Abstract
Background
Acne vulgaris is one of the most common disorders of the pilosebaceous unit. Although doxycycline is considered to be a first-line anti-acne antibiotic, various other antibiotics have been tried due to its adverse effects and contraindications. We performed a meta-analysis of randomized controlled trials (RCTs) that compared the efficacy of oral azithromycin pulse therapy with that of oral daily doxycycline in the management of moderate to severe acne vulgaris.
Methods
Five scientific databases (MEDLINE, EMBASE, Cochrane Library, SCOPUS, and Web of Science) were searched to identify relevant studies. A review of 1,341 publications produced six RCTs that met our predefined inclusion criteria. The clinical outcome measures were remaining acne lesion counts, patients' self-assessment of treatment, and the investigators' assessment of treatment after 12 weeks.
Results
We included six studies assessing 906 patients with moderate to severe acne vulgaris. Meta-analyses of clinical outcome measures revealed no significant difference between the two groups regarding remaining acne lesion counts (p=0.27), patients' self-assessment of treatment (p=0.67), and the investigators' assessment of treatment (p=0.32). The incidence of severe adverse events leading to the discontinuation of therapy was higher in the doxycycline daily therapy group when compared with the azithromycin pulse therapy group.
Conclusion
This study indicates that azithromycin pulse therapy is equivalent to doxycycline at 12 weeks in the efficacy of the treatment for moderate to severe acne vulgaris Therefore, oral azithromycin pulse therapy may be a good alternative to doxycycline in the management of acne for those unable to tolerate doxycycline.
Keywords: Acne vulgaris, Azithromycin, Doxycycline, Meta-analysis
INTRODUCTION
Acne, a follicular disorder involving the specialized pilosebaceous units in the skin, is one of the most common skin disorders treated by dermatologists. The major factors involved in the pathophysiology of acne are obstruction of follicles due to abnormal keratinization of infundibular epithelium, stimulation of sebum secretion by androgensensitive sebaceous glands, and inflammation induced by microbial colonization with Propionibacterium acnes1.
Systemic antibiotics have been the mainstay of treatment for moderate to severe acne vulgaris to date, and the effectiveness of several antibiotics, including oxytetracycline, minocycline, doxycycline and erythromycin, in treating acne has been established2. Although doxycycline is considered to be a first-line anti-acne antibiotic, it is known to have side effects, such as gastrointestinal symptoms, tooth discoloration, photosensitive reactions, pigmentation changes, and central nervous system effects3. Moreover, doxycycline has many contraindications and drug interactions. For example, it cannot be used during pregnancy or in children under 12 years of age. In addition, the use of doxycycline with isotretinoin, another effective agent in acne treatment, should be avoided because of the increased risk of benign intracranial hypertension4. Some authors have emphasized the efficacy of oral azithromycin pulse therapy in acne treatment5,6.
Azithromycin is an orally administered macrolide antimicrobial drug, structurally related to erythromycin, with an expanded spectrum of activity and improved pharmacokinetic features. Azithromycin is characterized by rapid uptake from the circulation, followed by slow release. The long elimination half-life from tissue permits less-frequent administration7. As acne runs a variable course with fluctuations, long-term therapy is often needed. Therefore, drugs with relatively long half-lives such as azithromycin can be useful in increasing patient compliance. In addition, azithromycin can be employed in combination with isotretinoin and can be used during pregnancy and childhood. The adverse effects of azithromycin are limited mainly to mild gastrointestinal discomfort and occur less frequently than with other antibiotics. However, few clinical studies have directly compared oral azithromycin pulse therapy with oral daily doxycycline in the management of acne. Therefore, we conducted a meta-analysis with the aim of comparing the efficacy of oral azithromycin pulse therapy with that of oral daily doxycycline in acne treatment using multiple randomized controlled trials (RCTs).
MATERIALS AND METHODS
This study followed the guidelines outlined in the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement (Moher et al.8, 2009) (Supplement 1).
Search strategy
A search was conducted of five scientific databases (MEDLINE, EMBASE, Cochrane Library, SCOPUS, and Web of Science) to identify studies in the literature that compared oral azithromycin pulse therapy with oral daily doxycycline in the management of acne. We searched MEDLINE (January 1, 1964 to December 4, 2016), EMBASE (January 1, 1947 to December 4, 2016), and Cochrane Library (January 1, 1966 to December 4, 2016) with no restriction on language or publication year. The following keywords and medical subject headings were used for the MEDLINE search: “acne vulgaris,” “azithromycin,” and “doxycycline.” The search strategies were developed using indices of the various databases based on the MEDLINE strategy (Supplement 2). In addition to the initial electronic search, manual searching for additional relevant publications was performed.
Study selection
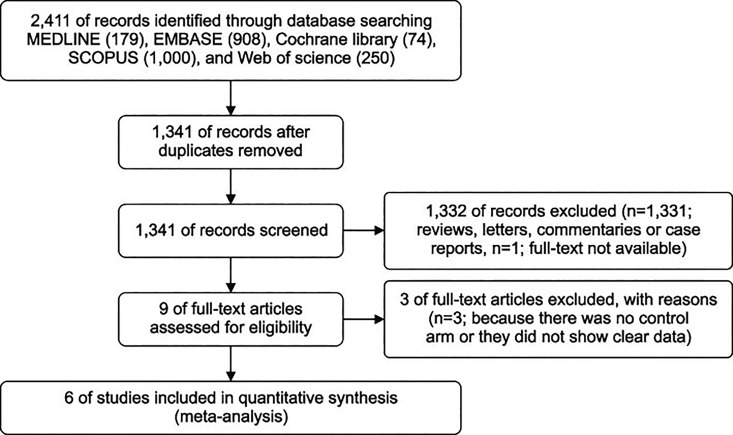
Two reviewers independently selected studies based on the following predefined inclusion criteria: 1) moderate or severe acne vulgaris diagnosed clinically or using validated diagnostic criteria; 2) comparison of the clinical outcomes of oral azithromycin pulse therapy and oral doxycycline daily therapy in moderate or severe acne vulgaris; 3) use of clinical outcomes, including the remaining acne lesion count and/or patients' self-assessment of treatment and/or investigators' assessment of lesions at the end of treatment, to evaluate efficacy; 4) maintenance of treatment for at least 3 months; 5) RCT design; and 6) availability of a full-text article. The two reviewers screened titles and abstracts to exclude reviews, letters, commentaries, and case reports. When a study was described in more than one publication, only the most recent or complete article was used. A full list of the exclusion criteria can be found in Fig. 1. Six studies were finally selected.
Fig. 1. Flow diagram of study identification, inclusion, and exclusion.
Data extraction
Two reviewers independently extracted data from the six studies using a predefined data extraction form. All disagreements were resolved by discussion. We extracted the following variables from the studies: 1) authors; 2) year of publication; 3) demographic characteristics of the study population (number, age); 4) inclusion criteria for moderate or severe acne vulgaris; 5) treatment protocol; 6) length of treatment; and 7) method of efficacy evaluation. The relevant clinical data were summarized separately according to the following outcomes: 1) remaining acne lesion count; 2) patients' self-assessment of treatment; and 3) investigators' assessment of treatment. We also evaluated safety outcomes by recording severe side effects that occurred during treatment in all included studies. We defined severe side effects as intolerable side effects that necessitated discontinuation of treatment.
Statistical analysis
We planned to perform a meta-analysis to compare the efficacy of oral azithromycin pulse therapy with that of oral daily doxycycline in the management of moderate to severe acne vulgaris. To do so, the clinical treatment outcome was measured according to the following data: remaining acne lesion count, patients' self-assessment of treatment, and investigators' assessment of treatment. Three studies involved inflammatory acne lesion counts, two included non-inflammatory acne lesion counts, two involved patient self-assessment, and all six included the investigators' assessment of treatment. These outcomes were pooled in this analysis. For remaining acne lesion counts, smaller numbers meant a better response to treatment. In evaluating the patient's self-assessment of treatment, favorable responses were defined as “excellent” and “good” ratings. In evaluating the investigators' assessment of treatment, treatment responses were expressed as percentages or by quantitative lesion scores on a 4-point scale (−1, worsened; 0, unchanged; 1, improved; and 2, clear). We defined an excellent response as “a reduction of 75% or more” or “improved or clear state.” Next, we defined a moderate response as “a reduction of 50% or more” or an “improved or clear state.” We conducted pooled analyses using random-effects weighting for meta-analyses of the outcomes reported by multiple studies that were sufficiently similar to justify combining results. However, if the clinical heterogeneity was too great, studies were not pooled. For dichotomous outcomes, we calculated risk ratios using the Mantel-Haenszel method. For continuous outcomes, we used weighted mean differences (WMDs) and 95% confidence intervals (CIs) with the inverse variance method. Heterogeneity in all meta-analyses was measured using I2, which indicates the proportion of variation in effect estimates across trials that is due to heterogeneity, rather than sampling error. I2 values >50% and p-values from the χ2 test <0.10 were taken to indicate a statistically large degree of heterogeneity among the included studies. If substantial statistical heterogeneity was noted (I2>50%), we planned to explore individual study characteristics and those of subgroups of the main body of evidence. We performed a sensitivity analysis according to the quality of individual studies and blinding of outcome assessment. All calculations were performed using Review Manager ver. 5.2 (The Cochrane Collaboration, Oxford, UK). This study is based on Cochrane Review Methods.
Assessment of risk of bias
The Cochrane Collaboration's risk of bias tool was used to assess the risk of bias in all included studies. The following items were assessed and recorded: random sequence generation (selection bias), allocation concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias), and selective reporting (reporting bias). Each of the included studies was rated as having low, unclear, or high bias based on these items (Supplement 3).
RESULTS
Identification of studies
The database search yielded 1,341 articles, of which 1,331 were excluded because the titles and abstracts indicated that they did not fulfill the selection criteria; an additional article was excluded because the full text was not available. We obtained the full text of the remaining nine articles. We subsequently identified six relevant studies after excluding three (two had no control group, and one did not provide enough data; Fig. 1). Ultimately, six studies were included in the meta-analysis.
Study characteristics and patients
Of the six studies, two were performed in Iran and one each was performed in India, Turkey, Poland, and Pakistan. The main characteristics of the studies are shown in Table 1. The six studies enrolled a total of 906 patients with moderate or severe acne vulgaris. Overall, 452 patients were assigned randomly to the azithromycin pulse therapy group, and the remaining 454 patients were assigned to the daily doxycycline therapy group. Patients assigned to the azithromycin pulse therapy group took 500 mg of azithromycin 1~3 times weekly or 4 times monthly. Patients in the daily doxycycline group took 100 mg of doxycycline once or twice daily.
Table 1. Characteristics of the six randomized controlled trials included in the final analysis.
| Study (year) | No. of patient | Age (yr) | Treatments protocol | Methods of evaluating efficacies | ||
|---|---|---|---|---|---|---|
| Azithromyci n group (n=452) | Doxycycline group (n=454) | Azithromycin group | Doxycycline group | |||
| Parsad et al. (2001)10 | 30 (6.6) | 30 (6.6) | ≥16 | Azithromycin 500 mg 4 d/mo+topical 0.05% tretinoin | 100 mg doxycycline once daily+topical 0.05% tretinoin cream | 1. Investigator's assessment of treatment using a 4 point scale |
| Kus et al. (2005)13 | 25 (5.5) | 26 (5.7) | 18~30 | Azithromycin 500 mg 3 d/wk (1st mo), 2 d/wk (2nd mo), once a week (3rd mo) | Doxycycline 100 mg twice a day (1st mo), once daily (2nd mo, 3rd mo) | 1. Facial inflammatory, non-inflammatory acne lesion counts |
| 2. Patient's own assessment of treatment using a 5 point scale | ||||||
| 3. Investigator's assessment of treatment (treatment responses were expressed as percentages) | ||||||
| Babaeinejad et al. (2011)12 | 50 (11.1) | 50 (11.0) | ≥13 | Azithromycin 500 mg 4 d/mo | 100 mg doxycycline once daily | 1. Investigator's assessment of treatment (treatment responses were expressed as percentages) |
| Maleszka et al. (2011)15 | 120 (26.5) | 120 (26.4) | ≥14 | Azithromycin 500 mg 3 d/wk (1st wk), followed by 500 mg weekly | 100 mg doxycycline twice a day (1st d), followed by 100 mg doxycycline once daily | 1. Facial inflammatory acne lesion counts |
| 2. Investigator's assessment of treatment (treatment responses were expressed as percentages) | ||||||
| Moravvej et al. (2012)14 | 34 (7.5) | 35 (7.7) | 18~30 | Azithromycin 500 mg 3 d/wk | 100 mg doxycycline daily | 1. Facial inflammatory, non-inflammatory acne lesion counts |
| 2. Patient's own assessment of treatment using a 5 point scale | ||||||
| 3. Investigator's assessment of treatment (treatment responses were expressed as percentages) | ||||||
| Ullah et al. (2014)16 | 193 (42.7) | 193 (42.5) | 14~30 | Azithromycin 500 mg 4 d/mo | 100 mg doxycycline daily | 1. Investigator's assessment of treatment (treatment responses were expressed as percentages) |
Studies defined “moderate acne vulgaris” by using specific tools or by measuring clinical findings. In one study, “moderate acne vulgaris” was defined according to Burke and Cunliffe's Leeds technique9,10; in another, recommendations from the Consensus Conference on Acne Classification were used11,12. In two studies, “moderate acne vulgaris” was diagnosed by counting inflammatory acne lesions and patients with at least 10 lesions were included13,14. In two other studies, “moderate acne vulgaris” was defined based on clinical findings15,16.
Inflammatory acne lesions were counted in three of the six studies. Of these13,14,15, non-inflammatory lesions (comedones) were also counted in two studies13,14. Two studies included patients' assessments of their treatment13,14, with improvement measured on a scale of 0~5 (0, worsening; 1, no change; 2, mild improvement; 3, moderate improvement; 4, good improvement; and 5, excellent improvement). Favorable patient responses were defined as “excellent” and “good” ratings. Investigators evaluated the response to treatment in all studies. Treatment responses were expressed as percentages in five studies12,13,14,15,16 and by quantitative lesion scores on a 4-point scale (−1, worsened; 0, unchanged; 1, improved; and 2, clear) in one study10. We defined a meaningful response as a score of 2. Initially, we defined an excellent response as “a reduction of 80% or more” in four studies12,13,14,16, “a reduction of 75% or more” in one study15, and an “improved or clear state” in one study10. Next, we defined a moderate response as “a reduction of 50% or more” in five studies12,13,14,15,16 and an “improved or clear state” in one study10. Each response was then analyzed individually.
Clinical treatment outcome measures
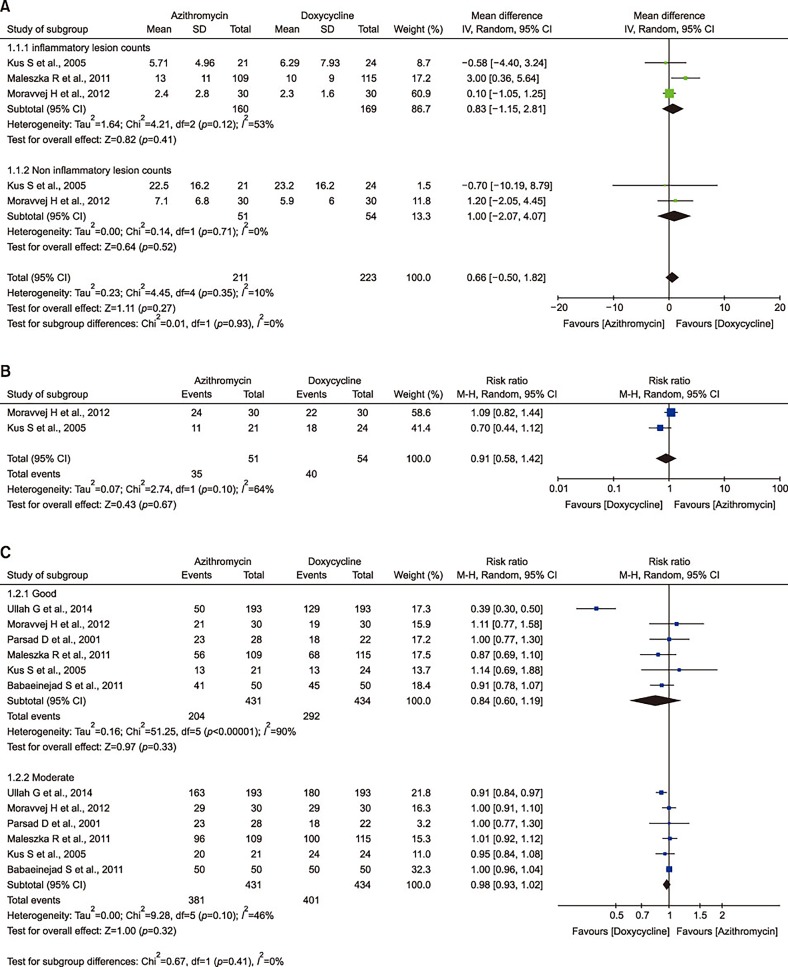
At 12 weeks, remaining inflammatory and non-inflammatory acne lesion profiles were similar in the azithromycin pulse therapy and doxycycline daily therapy groups, with no significant difference between groups and no heterogeneity (WMD, 0.66; 95% CI, −0.50~1.82; I2=10%; Fig. 2A). The meta-analysis of patients' self-assessment data from two studies revealed no significant difference between groups and moderate heterogeneity (relative risk [RR], 0.91; 95% CI, 0.58~1.42; I2=64%; Fig. 2B). Also, we conducted a meta-analysis of investigators' assessment of treatment in all six studies. Again, the analysis showed no significant difference between groups in both excellent and moderate response (excellent response: RR, 0.84; 95% CI, 0.60~1.19; I2=90%; moderate response: RR, 0.98; 95% CI, 0.93~1.02; I2=46%; Fig. 2C). The assessment outcomes are shown in Fig. 2.
Fig. 2. Forest plot of the meta-analysis for clinical outcome measures. (A) Remaining acne lesion counts. (B) Patient's self-assessment of treatment. (C) Investigator's assessment of treatment. SD: standard deviation, IV: inverse variance, CI: confidence interval, df: degree of freedom, M-H: Mantel-Haenszel.
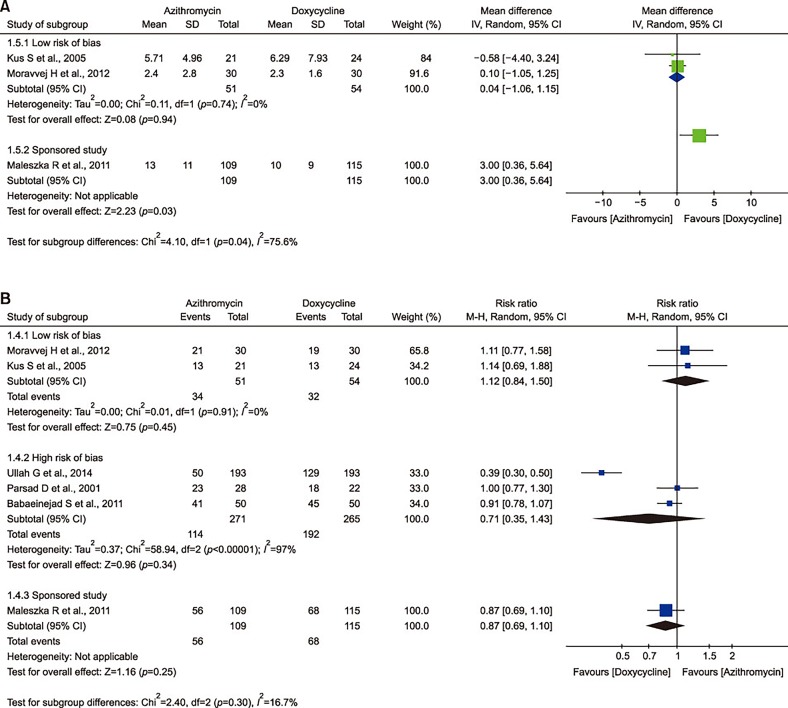
Sensitivity analysis outcomes
We conducted a sensitivity analysis of remaining inflammatory acne lesion counts and investigators' assessment of treatment according to the quality of individual studies and blinding of outcome assessment. The sensitivity analysis outcomes are shown in Fig. 3. The sensitivity analysis changed the direction of clinical outcomes, although it was not statistically significant. At 12 weeks, the remaining inflammatory acne lesion counts were similar in the azithromycin pulse therapy and doxycycline daily therapy groups, with no significant difference between groups (WMD, 0.83; 95% CI, −1.15~2.81; Fig 2A). Among them, two studies were assumed to have a low risk of bias and the other was a sponsored study. The individual sensitivity analysis outcomes showed the direction change (low risk of bias: WMD, 0.04; 95% CI, −1.06~1.15; sponsored study: WMD, 3.00; 95% CI, 0.36~5.64; Fig. 3A). Similarly, we performed a sensitivity analysis about the investigators' assessment of treatment. The meta-analysis of the six included studies showed no significant difference between groups (excellent response: RR, 0.84; 95% CI, 0.60~1.19; Fig. 2C). Among them, two studies were assumed to have a low risk of bias, three studies had a high risk of bias, and the other one was a sponsored study. The individual sensitivity analysis outcomes showed the direction change (low risk of bias: RR, 1.12; 95% CI, 0.84~1.50; high risk of bias: RR, 0.71; 95% CI, 0.35~1.43; sponsored study: RR, 0.87; 95% CI, 0.69~1.10; Fig. 3B).
Fig. 3. Forest plot of the meta-analysis for sensitivity analysis. (A) Remaining inflammatory acne lesion counts. (B) Investigator's assessment of treatment. SD: standard deviation, IV: inverse variance, CI: confidence interval, df: degree of freedom, M-H: Mantel-Haenszel.
Safety outcomes
We reviewed all side effects reported in the six studies. In general, the side effects were mild and transient, and did not require the discontinuation of therapy. For example, side effects included mild epigastric pain, diarrhea, vomiting, abdominal pain, constipation, malaise, and mild headache. However, some patients experienced intolerable side effects and subsequently discontinued therapy. Severe side effects are shown in Table 2. Severe side effects were defined as intolerable side effects that necessitated the discontinuation of treatment and included severe gastrointestinal discomfort, photosensitivity, vaginitis, and severe vertigo. Although a statistical analysis of these side effects was not performed, the incidence of severe adverse events was higher in the doxycycline daily therapy group than in the azithromycin pulse therapy group.
Table 2. Serious adverse events leading to the discontinuation of therapy.
| Severe side effect | Doxycycline | Azithromycin |
|---|---|---|
| Severe diarrhea | 0 | 4 |
| Severe nausea | 2 | 0 |
| Severe epigastric pain | 3 | 0 |
| Photosensitivity | 3 | 0 |
| Vaginitis | 2 | 0 |
| Abnormal blood cell count | 1 | 0 |
| Severe vertigo | 1 | 0 |
DISCUSSION
The results of our meta-analysis show that doxycycline daily therapy and azithromycin pulse therapy had similar efficacy in the treatment of moderate to severe acne vulgaris at 12 weeks, with no significant difference between groups. The clinical outcome measures included the remaining acne lesion count, patients' self-assessment of their treatment, and investigators' assessment of the treatment. In regards to safety outcomes, the doxycycline daily therapy group reported more severe adverse events than the azithromycin pulse therapy group. Even though it was not statistically significant, the meta-analysis of clinical outcome measures was weighed toward the doxycycline daily therapy group. Therefore, we conducted a sensitivity analysis of the remaining inflammatory acne lesion counts and investigators' assessment of treatment according to the quality of individual studies and blinding of outcome assessment. We chose these outcome measures for the sensitivity analysis because the blinding of outcome assessment can have a major influence on them. The sensitivity analysis changed the direction of the two clinical outcomes. Of the three studies13,14,15 evaluated for remaining inflammatory acne lesion counts, one study15 was a company-sponsored study and reported greater efficacy in the doxycycline daily therapy group. In contrast, two studies13,14 that showed their blinding of outcome assessment clearly reported more favorable efficacy in the azithromycin pulse therapy group. Similarly, of the six studies10,12,13,14,15,16 that evaluated the investigator's assessment of treatment, three studies10,12,16 that did not show their blinding of outcome assessment clearly reported more favorable efficacy in the doxycycline daily therapy group. In contrast, two studies13,14 that showed their blinding of outcome assessment clearly reported more favorable efficacy in the azithromycin pulse therapy group. The one company-sponsored study15 showed more favorable efficacy in the doxycycline daily therapy group. Sometimes, company-sponsored studies are significantly more likely to paint a rosy picture of the drug being evaluated than independent trials. Two studies12,16 did not report any side effects. Both of them reported more favorable efficacy in the doxycycline daily therapy group and were among the previous three studies that showed high detection bias. In light of this, there could also be reporting bias. Taken together, the high risk of blinding of outcome assessment of studies could have led to an overestimation of doxycycline efficacy in their assessment. Of all six studies, one study16 was distinctively heterogeneous compared with the other five. It reported the most favorable efficacy of doxycycline daily therapy among all six studies. However, the study did not report any adverse events and also did not describe its blinding of outcome assessment. This could have created reporting bias and thus led to an overestimation of doxycycline efficacy.
Antibiotics are a well-known mainstream treatment for acne because of their anti-inflammatory and antimicrobial properties. Systemic antibiotics have been proven to reduce not only, inflammatory, but also non-inflammatory, lesions of acne. Research has also shown that once P. acnes colonization occurs, those organisms liberate free fatty acids that are comedogenic, and thus yield non-inflammatory lesions17. Among various antibiotics, tetracycline and its derivatives are used widely in the treatment of acne vulgaris. Doxycycline is often preferred to other tetracyclines due to its safer side effect profiles, and it is among the most commonly prescribed antibiotics in the management of acne. Despite its overall safety record, doxycycline has fatal disadvantages. Sometimes, its use must be limited because it is contraindicated in females of childbearing age and children under 12 years of age. Also, doxycycline has been reported to have several side effects. The most common adverse events associated with doxycycline are gastrointestinal, including heartburn, nausea, vomiting, diarrhea, gastritis, and esophagitis. The second most commonly reported side effect is photosensitivity. In addition, several serious doxycycline-induced adverse reactions, such as pseudotumor cerebri and drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome, have emerged over the last few years. Although discontinuation of the medication yielded improvement in most reported cases, a few patients suffered from a permanent loss of visual acuity or loss of visual field18,19,20,21.
In the context of the fairly large number of adverse events related to tetracycline and its derivatives, some comparative clinical trials have shown that the tolerability profile of azithromycin is superior to that of tetracyclines13,16,22. Clinical isolates of P. acnes are highly susceptible to macrolide antibiotics. Although such antibiotics can effectively treat acne, they are not considered to be first-line drugs because of the risk of bacterial resistance23. Antibiotic resistance among P. acnes is increasing globally and may contribute significantly to treatment failure. Among the various macrolide antibiotics, P. acnes is more commonly resistant to erythromycin and clindamycin, and less so to azithromycin24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39. Moon et al.33 examined the antibiotic resistance profile of microbial strains isolated from Korean acne patients and reported that higher proportions of P. acnes isolates were resistant to clindamycin (30%) and erythromycin (26.7%) than to azithromycin (6.7%) and doxycycline (6.7%).
Also, azithromycin affords many advantages compared with other antibiotics. In terms of pharmacokinetics, azithromycin is known to be more stable in gastric acid than are older generation macrolides, including erythromycin, and it achieves rapid uptake from the circulation with a high tissue concentration following oral administration. Moreover, azithromycin has a long half-life, enabling less-frequent administration and making it suitable for use as pulse therapy, which can improve patient compliance and the development of P. acnes resistance; the dose is low. Several studies1,2,3 reported that pulse dosing was successful; however, no standard regimen is yet available6,10,40. Some studies4,5 have compared the efficacies of different pulse-dosing protocols and found no significant among-protocol difference in efficacy 41,42. Accordingly, although the treatment protocols differed slightly among included studies, we could not consider that this a major problem.
Furthermore, azithromycin is well tolerated and has a good safety record. Previously, Bakar et al.43 reported that the side effects of azithromycin were minimal and well tolerated in most patients treated for papulopustular rosacea. Kashkouli et al.44 also reported mild and temporary side effects, which did not require treatment, during treatment for meibomian gland dysfunction, whereas the doxycycline group had significantly more side effects. In the six studies included in the present meta-analysis, severe adverse events were detected more frequently in the doxycycline therapy group. Moreover, azithromycin has no major drug interaction. Of the anti-acne antibiotics used frequently, azithromycin is the most eligible for use in combination with isotretinoin. Previous studies showed that a combination of low-dose isotretinoin and oral azithromycin pulse therapy was effective in the treatment of severe acne. Combination therapy might yield synergistic effects and overcome the dose-dependent adverse effects of isotretinoin, as well as lower the incidence of relapse compared with monotherapy45,46. Azithromycin is not contraindicated in pregnancy, unlike tetracyclines; thus, it can be safely administered to women of childbearing age and to pregnant women with severe aggravated lesions, with no increased risk of congenital malformation or miscarriage47. Due to these advantages, azithromycin is expected to be a good alternative to conventional acne antibiotics. Many previous studies have demonstrated that azithromycin was effective in treating acne, with similar efficacy to that of doxycycline; our results are in line with these reports.
Our study has several limitations. First, only a small number of eligible studies were included. Second, detection and reporting biases may have been present. The inclusion of a greater number of high-quality RCTs is needed in future analyses.
In conclusion, the present work revealed significant evidence that azithromycin pulse therapy is a likely equivalent to daily doxycycline therapy in the management of moderate or severe acne vulgaris and may be a good alternative drug for patients who cannot tolerate tetracycline. In addition, reevaluation of the efficacy of azithromycin in treating acne would be helpful; azithromycin may be used widely with a better safety profile than other drugs, including doxycycline. To our knowledge, this is the first meta-analysis to compare the efficacy of oral azithromycin pulse therapy with that of oral daily doxycycline therapy in the treatment of acne vulgaris.
ACKNOWLEDGMENT
This work was supported by the Soonchunhyang University Research Fund.
Footnotes
CONFLICTS OF INTEREST: The authors have nothing to disclose.
SUPPLEMENTARY MATERIALS
Supplementary data can be found via http://anndermatol.org/src/sm/ad-30-417-s001.pdf.
PRISMA 2009 Checklist
Search strategy on MEDLINE, EMBASE, Cochrane Library, SCOPUS, and Web of Science
Risk of bias assessment of the included studies.
References
- 1.Pochi PE. The pathogenesis and treatment of acne. Annu Rev Med. 1990;41:187–198. doi: 10.1146/annurev.me.41.020190.001155. [DOI] [PubMed] [Google Scholar]
- 2.Layton AM. Optimal management of acne to prevent scarring and psychological sequelae. Am J Clin Dermatol. 2001;2:135–141. doi: 10.2165/00128071-200102030-00002. [DOI] [PubMed] [Google Scholar]
- 3.Smith K, Leyden JJ. Safety of doxycycline and minocycline: a systematic review. Clin Ther. 2005;27:1329–1342. doi: 10.1016/j.clinthera.2005.09.005. [DOI] [PubMed] [Google Scholar]
- 4.Lee AG. Pseudotumor cerebri after treatment with tetracycline and isotretinoin for acne. Cutis. 1995;55:165–168. [PubMed] [Google Scholar]
- 5.Gruber F, Grubisić-Greblo H, Kastelan M, Brajac I, Lenković M, Zamolo G. Azithromycin compared with minocycline in the treatment of acne comedonica and papulo-pustulosa. J Chemother. 1998;10:469–473. doi: 10.1179/joc.1998.10.6.469. [DOI] [PubMed] [Google Scholar]
- 6.Fernandez-Obregon AC. Azithromycin for the treatment of acne. Int J Dermatol. 2000;39:45–50. doi: 10.1046/j.1365-4362.2000.00749.x. [DOI] [PubMed] [Google Scholar]
- 7.Peters DH, Friedel HA, McTavish D. Azithromycin. A review of its antimicrobial activity, pharmacokinetic properties and clinical efficacy. Drugs. 1992;44:750–799. doi: 10.2165/00003495-199244050-00007. [DOI] [PubMed] [Google Scholar]
- 8.Moher D, Liberati A, Tetzlaff J, Altman DG PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62:1006–1012. doi: 10.1016/j.jclinepi.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 9.Burke BM, Cunliffe WJ. The assessment of acne vulgaris--the leeds technique. Br J Dermatol. 1984;111:83–92. doi: 10.1111/j.1365-2133.1984.tb04020.x. [DOI] [PubMed] [Google Scholar]
- 10.Parsad D, Pandhi R, Nagpal R, Negi KS. Azithromycin monthly pulse vs daily doxycycline in the treatment of acne vulgaris. J Dermatol. 2001;28:1–4. doi: 10.1111/j.1346-8138.2001.tb00077.x. [DOI] [PubMed] [Google Scholar]
- 11.Pochi PE, Shalita AR, Strauss JS, Webster SB, Cunliffe WJ, Katz HI, et al. Report of the consensus conference on acne classification. Washington, D.C., March 24 and 25, 1990. J Am Acad Dermatol. 1991;24:495–500. doi: 10.1016/s0190-9622(08)80076-x. [DOI] [PubMed] [Google Scholar]
- 12.Babaeinejad S, Khodaeiani E, Fouladi RF. Comparison of therapeutic effects of oral doxycycline and azithromycin in patients with moderate acne vulgaris: what is the role of age? J Dermatolog Treat. 2011;22:206–210. doi: 10.3109/09546631003762639. [DOI] [PubMed] [Google Scholar]
- 13.Kus S, Yucelten D, Aytug A. Comparison of efficacy of azithromycin vs. doxycycline in the treatment of acne vulgaris. Clin Exp Dermatol. 2005;30:215–220. doi: 10.1111/j.1365-2230.2005.01769.x. [DOI] [PubMed] [Google Scholar]
- 14.Moravvej H, Halim AM, Yousefi M, Givrad S. Efficacy of doxycycline versus azithromycin in the treatment of moderate facial acne vulgaris. Iran J Dermatol. 2012;15:7–10. [Google Scholar]
- 15.Maleszka R, Turek-Urasinska K, Oremus M, Vukovic J, Barsic B. Pulsed azithromycin treatment is as effective and safe as 2-week-longer daily doxycycline treatment of acne vulgaris: a randomized, double-blind, noninferiority study. Skinmed. 2011;9:86–94. [PubMed] [Google Scholar]
- 16.Ullah G, Noor SM, Bhatti Z, Ahmad M, Bangash AR. Comparison of oral azithromycin with oral doxycycline in the treatment of acne vulgaris. J Ayub Med Coll Abbottabad. 2014;26:64–67. [PubMed] [Google Scholar]
- 17.Lavker RM, Leyden JJ, McGinley KJ. The relationship between bacteria and the abnormal follicular keratinization in acne vulgaris. J Invest Dermatol. 1981;77:325–330. doi: 10.1111/1523-1747.ep12482524. [DOI] [PubMed] [Google Scholar]
- 18.Weinstein M, Laxer R, Debosz J, Somers G. Doxycycline-induced cutaneous inflammation with systemic symptoms in a patient with acne vulgaris. J Cutan Med Surg. 2013;17:283–286. doi: 10.2310/7750.2013.12085. [DOI] [PubMed] [Google Scholar]
- 19.Tabibian JH, Gutierrez MA. Doxycycline-induced pseudotumor cerebri. South Med J. 2009;102:310–311. doi: 10.1097/SMJ.0b013e31818f98f0. [DOI] [PubMed] [Google Scholar]
- 20.Friedman DI, Gordon LK, Egan RA, Jacobson DM, Pomeranz H, Harrison AR, et al. Doxycycline and intracranial hypertension. Neurology. 2004;62:2297–2299. doi: 10.1212/wnl.62.12.2297. [DOI] [PubMed] [Google Scholar]
- 21.Mailhol C, Tremeau-Martinage C, Paul C, Godel A, Lamant L, Giordano-Labadie F. [Severe drug hypersensitivity reaction (DRESS syndrome) to doxycycline] Ann Dermatol Venereol. 2010;137:40–43. doi: 10.1016/j.annder.2009.10.180. French. [DOI] [PubMed] [Google Scholar]
- 22.Singhi MK, Ghiya BC, Dhabhai RK. Comparison of oral azithromycin pulse with daily doxycycline in the treatment of acne vulgaris. Indian J Dermatol Venereol Leprol. 2003;69:274–276. [PubMed] [Google Scholar]
- 23.Zaenglein AL, Pathy AL, Schlosser BJ, Alikhan A, Baldwin HE, Berson DS, et al. Guidelines of care for the management of acne vulgaris. J Am Acad Dermatol. 2016;74:945–973.e33. doi: 10.1016/j.jaad.2015.12.037. [DOI] [PubMed] [Google Scholar]
- 24.Coates P, Vyakrnam S, Eady EA, Jones CE, Cove JH, Cunliffe WJ. Prevalence of antibiotic-resistant propionibacteria on the skin of acne patients: 10-year surveillance data and snapshot distribution study. Br J Dermatol. 2002;146:840–848. doi: 10.1046/j.1365-2133.2002.04690.x. [DOI] [PubMed] [Google Scholar]
- 25.Ross JI, Snelling AM, Carnegie E, Coates P, Cunliffe WJ, Bettoli V, et al. Antibiotic-resistant acne: lessons from Europe. Br J Dermatol. 2003;148:467–478. doi: 10.1046/j.1365-2133.2003.05067.x. [DOI] [PubMed] [Google Scholar]
- 26.Oprica C, Nord CE ESCMID Study Group on Antimicrobial Resistance in Anaerobic Bacteria. European surveillance study on the antibiotic susceptibility of propionibacterium acnes. Clin Microbiol Infect. 2005;11:204–213. doi: 10.1111/j.1469-0691.2004.01055.x. [DOI] [PubMed] [Google Scholar]
- 27.Dumont-Wallon G, Moyse D, Blouin E, Dréno B. Bacterial resistance in French acne patients. Int J Dermatol. 2010;49:283–288. doi: 10.1111/j.1365-4632.2009.04270.x. [DOI] [PubMed] [Google Scholar]
- 28.Bettoli V, Borghi A, Rossi R, Ferroni M, Rigolin F, Virgili A. Antibiotic resistance of propionibacteria. Four years' experience of a large number of cases in Italy. Dermatology. 2006;212:206–207. doi: 10.1159/000090665. [DOI] [PubMed] [Google Scholar]
- 29.Hassanzadeh P, Bahmani M, Mehrabani D. Bacterial resistance to antibiotics in acne vulgaris: an in vitro study. Indian J Dermatol. 2008;53:122–124. doi: 10.4103/0019-5154.43213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zandi S, Vares B, Abdollahi H. Determination of microbial agents of acne vulgaris and propionibacterium acnes antibiotic resistance in patients referred to dermatology clinics in Kerman, Iran. Jundishapur J Microbiol. 2011;4:17–22. [Google Scholar]
- 31.Luk NM, Hui M, Lee HC, Fu LH, Liu ZH, Lam LY, et al. Antibiotic-resistant propionibacterium acnes among acne patients in a regional skin centre in Hong Kong. J Eur Acad Dermatol Venereol. 2013;27:31–36. doi: 10.1111/j.1468-3083.2011.04351.x. [DOI] [PubMed] [Google Scholar]
- 32.Tan HH, Tan AW, Barkham T, Yan XY, Zhu M. Community-based study of acne vulgaris in adolescents in Singapore. Br J Dermatol. 2007;157:547–551. doi: 10.1111/j.1365-2133.2007.08087.x. [DOI] [PubMed] [Google Scholar]
- 33.Moon SH, Roh HS, Kim YH, Kim JE, Ko JY, Ro YS. Antibiotic resistance of microbial strains isolated from Korean acne patients. J Dermatol. 2012;39:833–837. doi: 10.1111/j.1346-8138.2012.01626.x. [DOI] [PubMed] [Google Scholar]
- 34.Abdel Fattah NS, Darwish YW. In vitro antibiotic susceptibility patterns of propionibacterium acnes isolated from acne patients: an Egyptian university hospital-based study. J Eur Acad Dermatol Venereol. 2013;27:1546–1551. doi: 10.1111/jdv.12057. [DOI] [PubMed] [Google Scholar]
- 35.Nakase K, Nakaminami H, Takenaka Y, Hayashi N, Kawashima M, Noguchi N. Relationship between the severity of acne vulgaris and antimicrobial resistance of bacteria isolated from acne lesions in a hospital in Japan. J Med Microbiol. 2014;63:721–728. doi: 10.1099/jmm.0.067611-0. [DOI] [PubMed] [Google Scholar]
- 36.Ishida N, Nakaminami H, Noguchi N, Kurokawa I, Nishijima S, Sasatsu M. Antimicrobial susceptibilities of Propionibacterium acnes isolated from patients with acne vulgaris. Microbiol Immunol. 2008;52:621–624. doi: 10.1111/j.1348-0421.2008.00081.x. [DOI] [PubMed] [Google Scholar]
- 37.Rodríguez-Cavallini E, Vargas-Dengo P. [Bacterial etiology and antibiotic susceptibility in patients with acne] Rev Biomed. 2004;15:101–106. Italian. [Google Scholar]
- 38.Schafer F, Fich F, Lam M, Gárate C, Wozniak A, Garcia P. Antimicrobial susceptibility and genetic characteristics of propionibacterium acnes isolated from patients with acne. Int J Dermatol. 2013;52:418–425. doi: 10.1111/j.1365-4632.2011.05371.x. [DOI] [PubMed] [Google Scholar]
- 39.Mendoza N, Hernandez PO, Tyring SK, Haitz KA, Motta A. Antimicrobial susceptibility of propionibacterium acnes isolates from acne patients in Colombia. Int J Dermatol. 2013;52:688–692. doi: 10.1111/j.1365-4632.2011.05403.x. [DOI] [PubMed] [Google Scholar]
- 40.Kapadia N, Talib A. Acne treated successfully with azithromycin. Int J Dermatol. 2004;43:766–767. doi: 10.1111/j.1365-4632.2004.02058.x. [DOI] [PubMed] [Google Scholar]
- 41.Naieni FF, Akrami H. Comparison of three different regimens of oral azithromycin in the treatment of acne vulgaris. Indian J Dermatol. 2006;51:255–257. [Google Scholar]
- 42.Basta-Juzbasić A, Lipozencić J, Oremović L, Kotrulja L, Gruber F, Brajac I, et al. A dose-finding study of azithromycin in the treatment of acne vulgaris. Acta Dermatovenerol Croat. 2007;15:141–147. [PubMed] [Google Scholar]
- 43.Bakar O, Demirçay Z, Gürbüz O. Therapeutic potential of azithromycin in rosacea. Int J Dermatol. 2004;43:151–154. doi: 10.1111/j.1365-4632.2004.01958.x. [DOI] [PubMed] [Google Scholar]
- 44.Kashkouli MB, Fazel AJ, Kiavash V, Nojomi M, Ghiasian L. Oral azithromycin versus doxycycline in meibomian gland dysfunction: a randomised double-masked open-label clinical trial. Br J Ophthalmol. 2015;99:199–204. doi: 10.1136/bjophthalmol-2014-305410. [DOI] [PubMed] [Google Scholar]
- 45.Hasibur MR, Meraj Z. Combination of low-dose isotretinoin and pulsed oral azithromycin for maximizing efficacy of acne treatment. Mymensingh Med J. 2013;22:42–48. [PubMed] [Google Scholar]
- 46.De D, Kanwar AJ. Combination of low-dose isotretinoin and pulsed oral azithromycin in the management of moderate to severe acne: a preliminary open-label, prospective, non-comparative, single-centre study. Clin Drug Investig. 2011;31:599–604. doi: 10.2165/11539570-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 47.Fuentelsaz V, Ara M, Corredera C, Lezcano V, Juberias P, Carapeto FJ. Rosacea fulminans in pregnancy: successful treatment with azithromycin. Clin Exp Dermatol. 2011;36:674–676. doi: 10.1111/j.1365-2230.2011.04042.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
PRISMA 2009 Checklist
Search strategy on MEDLINE, EMBASE, Cochrane Library, SCOPUS, and Web of Science
Risk of bias assessment of the included studies.