Abstract
Naturally-acquired antibody responses to malaria parasites are not only directed to protein antigens but also to carbohydrates on the surface of Plasmodium protozoa. Immunoglobulin M responses to α-galactose (α-Gal) (Galα1-3Galβ1-4GlcNAc-R)-containing glycoconjugates have been associated with protection from P. falciparum infection and, as a result, these molecules are under consideration as vaccine targets; however there are limited field studies in endemic populations. We assessed a wide breadth of isotype and subclass antibody response to α-Gal in children from Mozambique (South East Africa) and Ghana (West Africa) by quantitative suspension array technology. We showed that anti-α-Gal IgM, IgG and IgG1–4 levels vary mainly depending on the age of the child, and also differ in magnitude in the two sites. At an individual level, the intensity of malaria exposure to P. falciparum and maternally-transferred antibodies affected the magnitude of α-Gal responses. There was evidence for a possible protective role of anti-α-Gal IgG3 and IgG4 antibodies. However, the most consistent findings were that the magnitude of IgM responses to α-Gal was associated with protection against clinical malaria over a one-year follow up period, especially in the first months of life, while IgG levels correlated with malaria risk.
Introduction
Carbohydrates have not classically been considered to be significantly involved in adaptive immune responses, mostly being described as T cell-independent antigens that fail to induce immunological memory and immunoglobulin (Ig) class-switching1. However, studies of carbohydrate-based vaccines in mice have shown a dominant IgM response2 with some IgG production3. Since the early 1990s, naturally occurring glycoproteins4, glycolipids5, and even protein-free polysaccharides6 have been shown to be important components of the adaptive repertoire and, currently, polysaccharide-based conjugate vaccines are widely used to provide protective immunity against bacterial meningitis7. At present, there are no vaccines in use against complex human parasites, and there is a need to expand the pipeline of targets of protective immunity against malaria and other neglected diseases. The investigation of parasite glycosylation may provide new opportunities for the discovery of novel vaccine candidates against such diseases8.
The immune response against the malaria parasite Plasmodium falciparum has been mainly assessed against protein antigens. However, besides glycosylphosphatidylinositol (GPI) anchors9, the immunogenicity of carbohydrates allegedly located in the surface of this parasite is largely underappreciated since the parasite seems to have lost many of the genes required to elaborate complex carbohydrates10. Nevertheless, recent works showed the presence of precursors involved in glycoconjugate biosynthesis11,12 and identified new glycosylations in the parasite surface13–15. Some of these sugars modify important antigens in the fight against malaria, such as the circumsporozoite surface protein (CSP), which is the main component of the RTS,S vaccine16 and is O-fucosylated in malaria sporozoites. These post-translational modifications may alter protein antigenicity, being relevant for vaccine design.
It was recently demonstrated that antibodies against the classical α-Gal (Galα1-3Galβ1-4GlcNAc-R) epitopes confer protection against Plasmodium spp. infection, reducing malaria transmission by Anopheles mosquitoes17. This study showed that levels of IgG and IgM against α-Gal increased with age, and that IgM responses correlated with malaria incidence and were associated with protection against the disease17. On the contrary, IgG responses to α-Gal did not correlate with malaria exposure and were neither associated with protection17. Remarkably, other works have also reported the reduction of antigenicity of blood stage parasitic proteins after α-galactosidase treatment18. However, specific α-galactose containing glycans have never been isolated or structurally characterized in the malaria parasite.
Anti-α-Gal antibodies19 are produced against α-Gal epitopes, which are not expressed by humans due to the inactivation of the α-1,3-galactosyltransferase (α-1,3GT) in ancestral anthropoid primates20. Thus, anti-α-Gal antibodies are largely produced in response to cross-reactive epitopes present in commensal bacteria or food21,22, being the most abundant natural antibody in humans, constituting 1–5% of circulating IgM and IgG in healthy adults21. Anti α-Gal antibodies may also be produced in response to infection by pathogens expressing α-Gal, like the Gram-negative bacteria Salmonella spp. or the protozoan parasite Trypanosoma spp22–25. In fact, it has been argued that the selective pressure that removed this glycan from humans was exerted by an infectious agent like a virus, bacteria or protozoan expressing α-Gal epitopes, or an immunologically cross-reactive carbohydrate structure21,26.
In this study we investigated the anti-α-Gal response in children living in malaria-endemic areas of Mozambique (South East Africa) and Ghana (West Africa) who participated in clinical trials of the RTS,S/AS0 vaccine. We examined the effect of age, malaria transmission intensity (MTI) and other variables on anti-α-Gal IgM, IgG, IgG1, IgG2, IgG3 and IgG4 responses, and assessed their association with protection against clinical malaria and the factors affecting it.
Results
Pilot study of α-Gal IgG and IgM antibodies
IgM and IgG against α-Gal were first evaluated in children age 1–4 years from the RTS,S/AS02A phase 2b trial in Mozambique. Responses measured at the first visit (Month 0 [M0]) increased with age by 1.27 MFIs/year for IgM and by 1.48 MFIs/year for IgG (Table 1 and Supplementary Fig. 1). We observed a trend of IgG levels starting lower and increasing faster in Ilha Josina (cohort 2, high MTI) than in Manhiça (cohort 1, low MTI), reaching higher levels at age 4 years in Ilha Josina (Supplementary Fig. 1), however this trend was not statistically supported in the regression model, as site and age did not show a significant interaction (Table 1). These results suggest that IgM and IgG to α-Gal rise with age, and levels of IgM and IgG to α-Gal do not differ between neighborhoods of different MTI, or between malaria cases and controls in this small pilot study (data not shown).
Table 1.
Regression models to assess the effect of age on anti-α-Gal antibody levels and interaction with site in children aged 1 to 4 years old from Manhiça and Ilha Josina.
| Coefficient | Std. Error | t value | Pr(>|t|) | |
|---|---|---|---|---|
| IgM | ||||
| (Intercept) | 3.72402 | 0.15238 | 24.439 | <2e-16 |
| Age | 0.10476 | 0.04851 | 2.16 | 0.0358 |
| Site (Manhiça) | 0.13553 | 0.21321 | 0.636 | 0.528 |
| Age-site (Manhiça) interaction | −0.02768 | 0.06566 | −0.422 | 0.6752 |
| IgG | ||||
| (Intercept) | 3.48813 | 0.23936 | 14.573 | <2e-16 |
| Age | 0.17339 | 0.07619 | 2.276 | 0.0274 |
| Site (Manhiça) | 0.2264 | 0.33492 | 0.676 | 0.5023 |
| Age-site (Manhiça) interaction | −0.06506 | 0.10315 | −0.631 | 0.5312 |
Data correspond to samples collected at baseline (M0) from children participants in the Mozambican RTS,S phase 2b clinical trial.
Pattern of α-Gal antibody isotypes and subclasses in African children
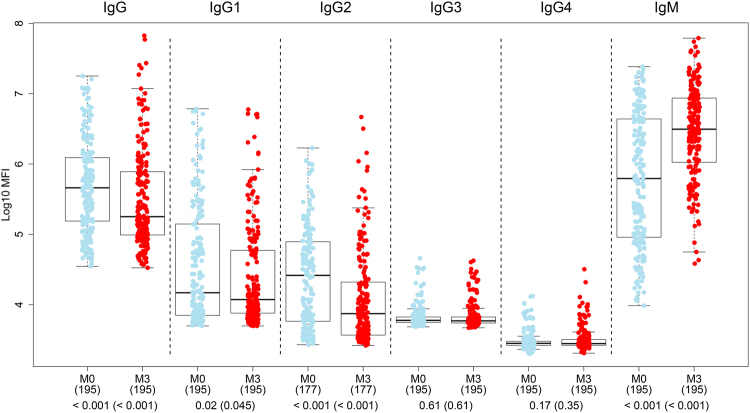
IgM, IgG and IgG1–4 against α-Gal were measured in children age ≤2 years from the RTS,S/AS01E phase 3 trial in Ghana and Mozambique, after confirming that vaccination did not have an effect on antibody response to α-Gal (Tables 2, 3 and S1). Thus, from here onwards, analyses were conducted regardless of vaccination group. IgM predominated over IgG responses. Among IgG subclasses, IgG1 and IgG2 tended to be higher than IgG3, and IgG4 was the lowest (Fig. 1). IgG, IgG1 and IgG2 were higher at the first study timepoint (M0) probably due to maternal transfer, and IgM was higher three months later (M3), reflecting continuous exposure to α-Gal.
Table 2.
Factors affecting the anti-α-Gal response at month 3.
| Antibody | Age* | Age cohort | Sex | Site | WAZ | HAZ | Hb | Exposure index | Maternal index | Prior episode† | Seasonǂ | Vaccine | IgG at M0 | IgM at M0 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Coef(CI) p-val | Coef(CI) p-val | Coef(CI) p-val | Coef(CI) p-val | Coef(CI) p-val | Coef(CI) p-val | Coef(CI) p-val | Coef(CI) p-val | Coef(CI) p-val | Coef(CI) p-val | Coef(CI) p-val | Coef(CI) p-val | Coef(CI) p-val | Coef(CI) p-val | |
| IgG | 4.16 (3.31;5.02) <0.001 | 403.47 (237.49;651.09) <0.001 | −13.71 (−45.39;36.34) 1 | 76.7 (11.52;180) 0.047 | −17.01 (−32.47;2) 0.38 | −4.84 (−22.02;16.12) 1 | −0.2 (−15.32;17.62) 1 | 6.24 (0.64;12.16) 0.14 | −7.33 (−12.39;1.97) 0.03 | 17.99 (−43.6;146.87) 1 | −10.38 (−66.78;141.74) 1 | 3.12 (−36.44;67.29) 1 | 449.62 (328.11;605.61) <0.001 | 138.22 (93.47;193.33) <0.001 |
| IgG1 | 2.64 (1.65;3.64) <0.001 | 189.97 (84.24;356.36) <0.001 | 2.49 (−36.25;64.75) 1 | 91.76 (19.18;208.53) 0.03 | −6.95 (−24.97;15.41) 1 | −6.96 (−24.32;14.39) 1 | −1.56 (−16.97;16.72) 1 | 2.07 (−3.56;8.03) 1 | −9.13 (−15.43;−2.35) 0.03 | −20.31 (−62.92;71.25) 1 | 26.21 (−54.86;252.9) 1 | −28.76 (−56.76;17.38) 1 | 189.1 (108.36;301.14) <0.001 | 75.7 (38.54;122.82) <0.001 |
| IgG2 | 3.15 (2.2;4.11) <0.001 | 173.79 (75.41;327.35) <0.001 | −17.39 (−48.12;31.52) 1 | 7.01 (−33.26;71.6) 0.78 | −7.91 (−25.31;13.53) 1 | −9.31 (−25.68;10.67) 1 | −1.6 (−16.44;15.87) 1 | 1.85 (−3.48;7.47) 1 | 0.02 (−5.72;6.11) 0.99 | 18.53 (−44.13;151.47) 1 | 2.8 (−62.52;181.97) 1 | −3.38 (−40.82;57.75) 1 | 332.76 (225.44;475.47) <0.001 | 70.85 (35.43;115.53) <0.001 |
| IgG3 | 0.84 (0.6;1.08) <0.001 | 54.04 (38.41;71.44) <0.001 | −2.26 (−13.52;10.48) 1 | 31.71 (16.96;48.32) <0.001 | 0.22 (−5.2;5.96) 1 | 2.72 (−2.61;8.33) 1 | −2.44 (−6.62;1.92) 1 | −0.06 (−1.51;1.42) 1 | −2.89 (−4.56;−1.19) 0.004 | −12.81 (−28.38;6.13) 1 | −10.96 (−31.68;16.05) 1 | 2.39 (−10.03;16.54) 1 | 15.29 (5.29;26.25) 0.007 | 21.22 (14.32;28.54) <0.001 |
| IgG4 | 0.77 (0.56;0.98) <0.001 | 43.15 (29.89;57.77) <0.001 | −3.69 (−13.62;7.39) 1 | 23.74 (11.18;37.72) <0.001 | 1.64 (−3.26;6.79) 1 | 2.51 (−2.23;7.49) 1 | −2.71 (−6.42;1.15) 0.68 | 0.26 (−1.04;1.57) 1 | −2.98 (−4.34;−1.6) <0.001 | −11.52 (−25.72;5.39) 0.85 | −14.58 (−32.47;8.07) 0.94 | 3.18 (−8.03;15.77) 1 | 10.14 (1.51;19.51) 0.03 | 18.13 (12.09;24.49) <0.001 |
| IgM | 4.3 (3.56;5.05) <0.001 | 609.34 (412.38;882) <0.001 | −36.58 (−58.33;−3.48) 0.2 | 102.99 (33.11;209.54) 0.006 | −21.63 (−35.18;−5.24) 0.07 | 4.85 (−12.83;26.11) 1 | −16.45 (−28.11;−2.9) 0.12 | 10.6 (5.32;16.13) <0.001 | −18.4 (−23.63;−12.82) <0.001 | −23.5 (−61.42;51.67) 1 | −57.25 (−82.84;6.54) 0.41 | 14.99 (−26.58;80.09) 1 | 49.35 (8.7;105.2) 0.03 | 208.53 (163.58;261.14) <0.001 |
Multivariable linear models including phase 3 participants from both age groups and sites together. The coefficients indicate % change for a unit change in the predictor (95% confidence intervals [CI]). P-values are adjusted for multiple testing through Benjamini-Hochberg and Holm; those significant are in bold.
*Continous age in weeks. Age cohort (children vs infants). Sex (male vs female). Site (Manhiça vs Kintampo). WAZ (Weight-for-Age Z-score). HAZ (Height-for-Age Z-score). Hb (Baseline hemoglobin (g/dL). Exposure index (baseline anti-P. falciparum exposure IgM levels). Maternal index (baseline maternally transferred antibodies). †Malaria episode between month 0 and month 3 (yes vs no). ǂMalaria transmission season at month 3 sample collection (low vs high). Vaccine (RTS,S vs comparator).
Table 3.
Factors affecting the anti-α-Gal response at month 3 stratified by age group.
| Antibody | Age* | Sex | Site | WAZ | HAZ | Hb | Exposure index | Maternal index | Prior episode† | Seasonǂ | vaccine | IgG at M0 | IgM at M0 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Coef(CI) p-val | Coef(CI) p-val | Coef(CI) p-val | Coef(CI) p-val | Coef(CI) p-val | Coef(CI) p-val | Coef(CI) p-val | Coef(CI) p-val | Coef(CI) p-val | Coef(CI) p-val | Coef(CI) p-val | Coef(CI) p-val | Coef(CI) p-val | |
| Infants | |||||||||||||
| IgG | 13.89 (−0.69;30.61) 0.31 | −22.34 (−46.73;13.21) 0.93 | 44.7 (−1.77;113.16) 0.31 | −5.4 (−21.29;13.7) 1 | 4.39 (−11.17;22.67) 1 | −0.73 (−15.88;17.14) 0.93 | −0.31 (−5.94;5.66) 1 | −4.08 (−10.61;2.92) 0.73 | 0.12 (−48.12;93.23) 1 | 96.96 (6.32;264.89) 0.19 | 19.03 (−20.16;77.48) 0.95 | 235.96 (150.48;350.62) <0.001 | −5.88 (−30.61;27.67) 1 |
| IgG1 | 7.63 (−11.33;30.65) 1 | −3.34 (−43.13;64.27) 1 | 56.1 (−9.3;168.67) 0.43 | −3.6 (−25.45;24.65) 1 | −4.63 (−23.92;19.55) 1 | −18.33 (−34.97;2.57) 0.49 | 0.66 (−7.18;9.17) 1 | −9.69 (−18.03;−0.49) 0.16 | −51.53 (−80.44;20.07) 0.47 | 115.22 (−9.57;412.24) 0.41 | −35.96 (−63.16;11.31) 0.68 | −12.27 (−47.94;47.86) 1 | −1.8 (−35.86;50.32) 1 |
| IgG2 | −7.24 (−20.69;8.47) 1 | −4.21 (−36.69;44.93) 1 | −26.77 (−51.99;11.71) 0.43 | −6.47 (−23.15;13.83) 1 | −4 (−19.18;14.03) 1 | 12.06 (−5.86;33.39) 0.72 | −3.94 (−9.63;2.1) 1 | 0.62 (−6.87;8.71) 1 | 113.08 (1.23;348.53) 0.26 | 67.49 (−15.07;230.3) 0.54 | 33.11 (−13.8;105.54) 0.86 | 114.92 (45.65;217.14) <0.001 | −27.37 (−47.97;1.38) 0.24 |
| IgG3 | 0.52 |(−1.09;2.16) 1 | 3.44 (−0.98;8.06) 0.64 | 4.37 (−0.23;9.18) 0.31 | 0.03 (−2.09;2.19) 1 | 1.35 (−0.53;3.25) 0.95 | −1.5 (−3.36;0.39) 0.58 | −0.14 (−0.81;0.54) 1 | −0.37 (−1.18;0.45) 0.75 | −2.87 (−10;4.82) 0.90 | 9.43 (1.91;17.5) 0.08 | 2.43 (−2.21;7.29) 0.92 | 2.59 (−1.75;7.12) 0.73 | −0.63 (−4.09;2.96) 1 |
| IgG4 | 0.88 (−0.24;2.02) 0.49 | −1.08 (−4.08;2.01) 1 | 2.6 (−0.59;5.9) 0.43 | −1.19 (−2.64;0.28) 0.67 | 0.08 (−1.23;1.41) 1 | −0.51 (−1.84;0.83) 0.9 | 0.02 (−0.45;0.49) 1 | −0.77 (−1.32;−0.22) 0.03 | −5.25 (−10.08;−0.15) 0.26 | 1.07 (−3.97;6.37) 1 | 2.26 (−0.99;5.61) 0.86 | 0.23 (−2.77;3.33) 1 | 2.67 (0.21;5.19) 0.17 |
| IgM | 49.05 (25.69;76.76) <0.001 | −50.77 (−69.89;−19.51) 0.03 | 278.48 (138.23;501.3) <0.001 | −16.91 (−34.95;6.13) 0.68 | 2.98 (−17.12;27.95) 1 | −16.08 (−32.63;4.53) 0.58 | 5.17 (−2.67;13.64) 1 | −16.68 (−23.74;−8.98) <0.001 | −48.17 (−78.36;24.15) 0.47 | 7.17 (−53.99;149.65) 1 | 31.29 (−23.14;124.27) 0.95 | 49.53 (−8.99;145.69) 0.44 | 119.91 (50.3;221.78) <0.001 |
| Children | |||||||||||||
| Antibody | Age* | Sex | Site | WAZ | HAZ | Hb | Exposure index | Maternal index | Prior episode† | Vaccine | IgG at M0 | IgM at M0 | |
| Coef(CI) p-val | Coef(CI) p-val | Coef(CI) p-val | Coef(CI) p-val | Coef(CI) p-val | Coef(CI) p-val | Coef(CI) p-val | Coef(CI) p-val | Coef(CI) p-val | Coef(CI) p-val | Coef(CI) p-val | Coef(CI) p-val | ||
| IgG | 4.46 (2.15;6.82) 0.001 | 21.57 (−44.06;164.22) 1 | 197.26 (41.24;525.65) 0.02 | −11.62 (−36.6;23.2) 1 | −27.07 (−48.29;2.87) 0.43 | 31.26 (3.14;67.04) 0.14 | −2.23 (−10.28;6.55) 1 | −7.33 (−17.6;4.21) 0.78 | 2.96 (−67.76;228.75) 1 | −14.86 (−62.48;93.21) 1 | 553.04 (407.38;740.51) <0.001 | 643.92 (247.07;1494.52) <0.001 | |
| IgG1 | 2.53 (0.1;5.02) 0.12 | 26.8 (−42.24;178.4) 1 | 196.13 (39.09;530.48) 0.02 | 2.21 (−27.09;43.29) 1 | −17.75 (−42.21;17.07) 1 | 33.39 (4.54;70.2) 0.13 | −5.67 (−13.48;2.83) 0.73 | −4.46 (−15.7;8.28) 0.93 | 5.06 (−67.62;240.84) 1 | −18.89 (−64.64;86.05) 1 | 398.63 (255.6;599.19) <0.001 | 226.21 (39.11;664.94) 0.02 | |
| IgG2 | 5.39 (2.83;8.02) <0.001 | −12.98 (−64.11;110.98) 1 | 118.5 (−7.74;417.5) 0.15 | 2.75 (−29.53;49.81) 1 | −23.1 (−47.82;13.33) 0.91 | 4.55 (−20.37;37.25) 1 | −2.87 (−11.64;6.77) 1 | −1.92 (−12.69;10.18) 0.93 | −43.84 (−83.92;96.14) 1 | −29.48 (−71.65;75.42) 1 | 491.83 (312.64;748.81) <0.001 | 481.29 (143.92;1285.23) <0.001 | |
| IgG3 | 0.01 (−0.74;0.76) 0.98 | −3.81 (−24.22;22.09) 1 | 87.77 (54.22;128.61) <0.001 | 5.94 (−4.29;17.26) 1 | 1.14 (−9.17;12.63) 1 | 3.87 (−3.7;12.05) 0.96 | −3.76 (−6.15;−1.32) <0.001 | −3.76 (−9.35;2.16) 0.78 | −27.28 (−48.73;3.14) 0.44 | 2.1 (−20.62;31.32) 1 | 19.74 (3.92;37.98) 0.03 | 10.43 (−15.58;44.46) 0.93 | |
| IgG4 | 0.35 (−0.33;1.03) 0.63 | −2.5 (−21.68;21.39) 1 | 64.9 (36.16;99.71) <0.001 | 9.34 (−0.26;19.88) 0.34 | 3.1 (−6.58;13.79) 1 | 1.4 (−5.45;8.74) 1 | −2.65 (−4.91;−0.32) 0.13 | −3.99 (−8.62;0.86) 0.51 | −22.36 (−43.77;7.22) 0.61 | 4.16 (−17.34;31.23) 1 | 13.5 (−0.56;29.55) 0.06 | 7.65 (−15.91;37.82) 0.93 | |
| IgM | 1.69 (0.61;2.79) 0.01 | 12.46 (−21.66;61.45) 1 | 35.76 (−5.09;94.2) 0.15 | −6.63 (−20.01;8.99) 1 | −8.23 (−21.99;7.96) 1 | 13.11 (1.06;26.59) 0.14 | −1.01 (−4.9;3.03) 1 | −6.73 (−12.46;−0.62) 0.19 | −22.59 (−54.82;32.63) 1 | −3.92 (−34.45;40.83) 1 | 36.13 (10.01;68.47) 0.02 | 183.54 (101.56;298.87) <0.001 | |
Multivariable linear models including phase 3 participants from both sites stratifying by age group. The coefficients indicate % change for a unit change in the predictor (95% confidence intervals). P-values were adjusted for multiple comparisons through Benjamini-Hochberg and Holm; those significant are in bold.
*Continous age in weeks. Age cohort (children vs infants). Sex (male vs female). Site (Manhiça vs Kintampo). WAZ (Weight-for-Age Z-score). HAZ (Height-for-Age Z-score). Hb (Baseline hemoglobin (g/dL). Exposure index (baseline anti-P. falciparum exposure IgM levels). Maternal index (baseline maternally transferred antibodies). †Malaria episode between month 0 and month 3 (yes vs no). ǂMalaria transmission season at month 3 sample collection (low vs high). Vaccine (RTS,S vs comparator).
Figure 1.
Antibody isotype and subclass responses to α-Gal by timepoint. Boxplots represent the median and interquartile ranges of IgM, IgG and IgG1–4 levels in infants and children from Manhiça and Kintampo (all together) participating in the RTS,S phase 3 trial, measured at the first recruitment visit (M0) and three months later (M3). Groups were compared through t-tests and p-values were adjusted for multiple comparisons through Benjamini-Hochberg and Holm (in parenthesis).
Effect of age on α-Gal antibody responses
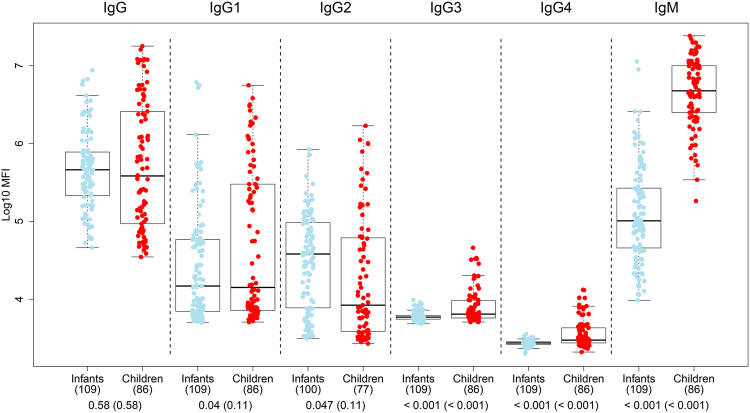
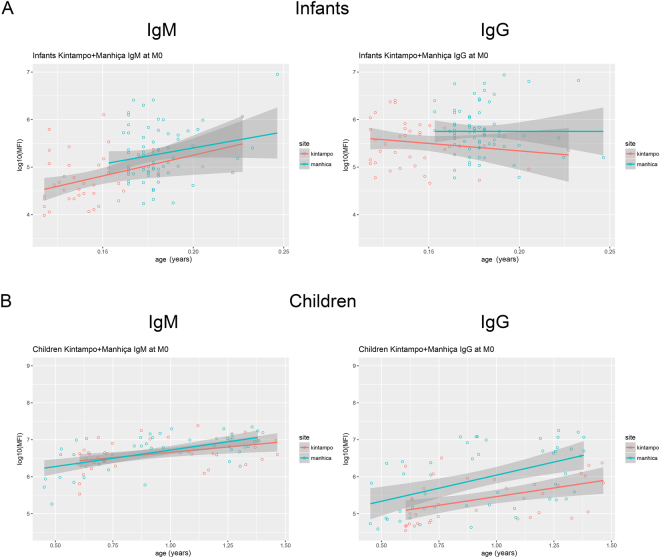
When comparing M0 α-Gal antibody levels between the age study groups, IgMs were higher in children (5–17 months old) than in infants (1.5–3 months old) (p < 0.001), whereas total IgGs were equal between them (p = 0.58) (Fig. 2). IgG1, IgG3 and IgG4 were higher in children and IgG2 in infants, although only IgG3 and IgG4 remained significant after adjusting by multiple comparisons (p < 0.001) (Fig. 2). When analyzing the effect of continuous age on IgM and IgG levels within each age cohort, IgM showed a strong increase in infants (11 × 107 MFIs/year) and a lower increase in children (3.77 MFIs/year) (Table 4 and Fig. 3). In contrast, IgG did not vary with age within the infants group, but increased 8.62 MFIs/year within the children group (Table 4 and Fig. 3). These results suggest that IgM increases from birth towards older ages, while total IgG does not increase during the initial months of life but an increase is already detected at age >5 months old. These observations were corroborated by multivariable linear regression models, showing that M3 levels of all six anti-α-Gal Ig increased with age as continuous or categorical (Table 2), but when stratifying by age group, IgM increased with age only in infants, while in children increments were observed for IgG, IgG2 and IgM (Table 3).
Figure 2.
Antibody isotype and subclass responses to α-Gal by age group. Comparison of levels of IgM, IgG and IgG1–4 between infants (1.5–3 months old) and children (5–17 months old), both sites together. Data correspond to samples collected at recruitment (M0) from participants in the RTS,S phase 3 clinical trial. Boxplots represent the median and interquartile range. Groups were compared through t-tests and p-values were adjusted for multiple comparisons through Benjamini-Hochberg and Holm (in parenthesis).
Table 4.
Regression models to assess the effect of age on anti-α-Gal antibody levels and interaction with site in infants (1.5–3 months old) and children (5–17 months old) from Manhiça and Kintampo.
| Coefficient | Std. Error | t value | Pr(>|t|) | |
|---|---|---|---|---|
| IgM | ||||
| Infants | ||||
| (Intercept) | 3.6632 | 0.5562 | 6.587 | 1.83E-09 |
| Age | 8.0381 | 3.8208 | 2.104 | 0.0378 |
| Manhiça | 0.3859 | 0.9327 | 0.414 | 0.6799 |
| Age-site (Manhiça) interaction | −1.2675 | 5.6345 | −0.225 | 0.8225 |
| IgG | ||||
| (Intercept) | 5.969 | 0.4852 | 12.302 | <2e-16 |
| Age | −3.1377 | 3.3335 | −0.941 | 0.349 |
| Manhiça | −0.2149 | 0.8137 | −0.264 | 0.792 |
| Age-site (Manhiça) interaction | 3.1261 | 4.9158 | 0.636 | 0.526 |
| IgM | ||||
| Children | ||||
| (Intercept) | 6.0856 | 0.2015 | 30.201 | <2e-16 |
| Age | 0.5762 | 0.2035 | 2.831 | 0.00584 |
| Manhiça | −0.2545 | 0.2701 | −0.942 | 0.34871 |
| Age-site (Manhiça) interaction | 0.3149 | 0.2721 | 1.158 | 0.25042 |
| IgG | ||||
| (Intercept) | 4.5273 | 0.3568 | 12.689 | <2e-16 |
| Age | 0.9355 | 0.3604 | 2.596 | 0.0112 |
| Manhiça | 0.1022 | 0.4782 | 0.214 | 0.8313 |
| Age-site (Manhiça) interaction | 0.4787 | 0.4817 | 0.994 | 0.3233 |
Data correspond to samples collected at baseline (M0) from participants in the RTS,S phase 3 clinical trial.
Figure 3.
Distribution of anti-α-Gal IgG and IgM levels (log10MFI) as a function of age (continuous) stratified by age cohort and site (Manhiça and Kintampo). (A) Infants (1.5–3 months old); (B) children (5–17 months old). Scatter plot data correspond to samples collected at baseline (M0) from participants in the RTS,S phase 3 clinical trial.
Furthermore, when comparing anti-α-Gal IgM, IgG and IgG1–4 subclass levels between time-points within each age group, we confirmed a significant increase of IgM from M0 to M3 in both age groups (p < 0.001) (Supplementary Fig. 2), being more marked in infants (also starting at lower basal levels) (Supplementary Fig. 3). IgG, IgG1, IgG2 and IgG3 levels decreased from M0 to M3 in infants (p < 0.001, p = 0.02, p < 0.001 and p = 0.01, respectively), and were recovered in children, with IgG levels being even higher at M3 than in M0 in this group (Supplementary Figs 2 and 3). This observation is compatible with a significant maternal transfer of anti-α-Gal IgG, IgG1, IgG2 and IgG3 to the newborn, corresponding to the levels measured in infants at M0, and a decay of these IgGs during the first months of life, evidenced by the lower M3 levels in infants. Overall, the increase of anti-α-Gal IgG and IgM levels in children compared to infants at M3 suggests a continued exposure to α-Gal.
Effect of MTI on α-Gal antibody responses
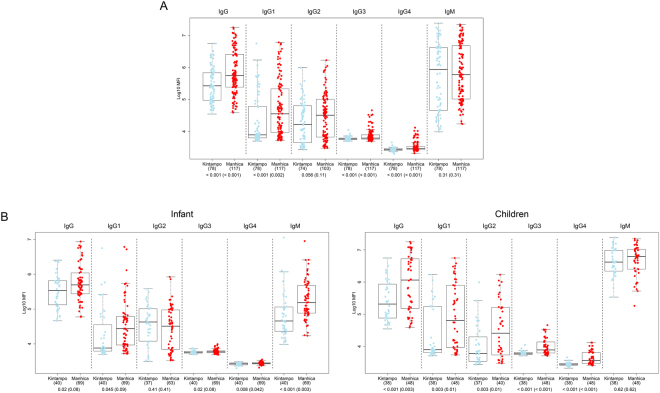
IgG, IgG1, IgG3 and IgG4 levels to α-Gal were significantly higher in Manhiça (low MTI) than Kintampo (high MTI) (p < 0.001, p = 0.002, p < 0.001 and p < 0.001, respectively) (Fig. 4A). When stratifying by age cohort, IgM and IgG4 were higher in infants (1.5–3 months) from Manhiça compared to Kintampo (p = 0.003 and p = 0.042, respectively), and total IgG, IgG1 and IgG3 showed a trend in the same direction (p = 0.08, p = 0.09 and p = 0.08, respectively) (Fig. 4B). Similarly, IgG, IgG1, IgG2, IgG3 and IgG4 were higher in children from Manhiça compared to Kintampo (p = 0.003, p = 0.01, p = 0.01, p < 0.001 and p < 0.001, respectively), but IgM did not show differences in this age group (Fig. 4B). Multivariable linear regression models also showed that IgG, IgG1, IgG3, IgG4 and IgM levels were higher in Manhiça compared to Kintampo (Table 2), but this was mostly for children, because when stratifying by age group, in infants only IgM was higher in Manhiça than Kintampo (Table 3).
Figure 4.
Anti-α-Gal antibody levels in Manhiça (Mozambique, low MTI) vs Kintampo (Ghana, high MTI). (A) Infants and children together. (B) Stratified by age group. Data correspond to samples collected at baseline (M0) from participants in the RTS,S phase 3 clinical trial. Boxplots represent the median and interquartile range. Groups were compared through t-tests and p-values were adjusted for multiple comparisons through Benjamini-Hochberg and Holm (in parenthesis). Infant: 1.5–3 months; Children: 5–17 months.
Effect of baseline malaria exposure and maternal antibodies on α-Gal antibody responses
The intensity of exposure to P. falciparum at M0, as indicated by antibody surrogate markers, was positively associated with anti-α-Gal IgM levels at M3 in multivariable linear regression models (Coeff [CI]: 10.6 [5.32; 16.13] p < 0.001) (Table 2). However, this effect disappeared when stratifying by age group (Table 3), probably because of the reduction in the sample size. Regarding IgG responses, P. falciparum exposure was negatively associated with anti-α-Gal IgG3 levels in children (−3.76 [−6.15; −1.32] p < 0.001) (Table 3). The models also showed a negative effect of P. falciparum maternally-transferred IgGs on anti-α-Gal IgG levels (−7.33 [−12.39; 1.97] p = 0.03), IgG1 (−9.13 [−15.43; 2.35] p = 0.03), IgG3 (−2.89 [−4.56; −1.19] p = 0.004), IgG4 (−2.98 [−4.34; −1.6] p < 0.001) and IgM (−18.4 [−23.63; −12.82] p < 0.001) (Table 2), but when stratifying by age group, this effect only remained significant for IgM in infants (−16.68 [−23.74; −8.98] p < 0.001) (Table 3), probably due to the reduced sample size.
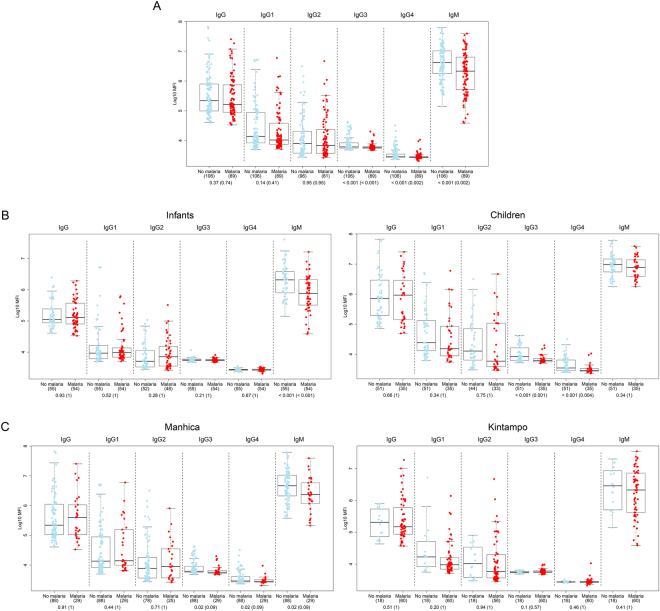
Effect of α-Gal antibodies in protection against clinical malaria
Anti-α-Gal IgM, IgG3 and IgG4 levels at M3 were higher in those subjects who did not have a clinical malaria episode over one year of follow up (p = 0.002, p < 0.001 and p = 0.002, respectively) (Fig. 5A). When stratifying by age group, IgM was higher only in infants (p < 0.001), and IgG3 and IgG4 only in children (p = 0.001 and p = 0.004) who did not subsequently develop clinical malaria (Fig. 5B). When looking at differences between cases and controls stratifying by site (but not age) (Fig. 5C), IgM, IgG3 and IgG4 were borderline significantly higher only in non-malaria controls from Manhiça (p = 0.09 for all).
Figure 5.
Anti-α-Gal antibody levels in cases (malaria) vs controls (no malaria). (A) Infants and children from both sites together. (B) Stratified by age group. (C) Stratified by site. Data correspond to samples collected at M3 (after the third vaccine dose and prior the 12 months of follow up) from children participants in the RTS,S phase 3 clinical trial. Cases were defined as children with at least one episode of clinical malaria during the 12 months of follow up. Boxplots represent the median and interquartile range. Groups were compared through t-tests and p-values were adjusted for multiple comparisons through Benjamini-Hochberg and Holm (in parenthesis). Infant: 1.5–3 months; Children: 5–17 months.
Logistic regression models were fitted including the covariates significantly associated to risk of clinical malaria, like being an infant, being immunized with a comparator vaccine, being from Kintampo, having had prior malaria episodes, and having higher M0 P. falciparum antibodies (indicative of malaria exposure and/or maternal antibodies). Univariate models showed a protective association of anti-α-Gal IgM (OR [CI] 0.43 [0.26; 0.68], p = 0.001), IgG3 (0.02 [0; 0.18], p < 0.001) and IgG4 (0.02 [0; 0.2], p = 0.001) with clinical malaria (Table 5). Stratifying by age group, anti-α-Gal IgM correlated with less risk of clinical malaria in infants (0.24 [0.1–0.52], p < 0.001), and anti-α-Gal IgG3 (0.02 [0; 0.18], p = 0.002) and IgG4 (0.01 [0; 0.18], p = 0.003) in children (Table 5). Stratified by site, anti-α-Gal IgM had a protective role only in Manhiça (0.36 [0.15; 0.78], p = 0.055) (Supplementary Table 2). Finally, multivariable stepwise regression models adjusting by the potential cofounders revealed a significant association of anti-α-Gal IgM (0.29 [0.1; 0.77], p = 0.02) with lower risk of clinical malaria in infants; and of anti-α-Gal IgG (7.99 [1.54; 58.03], p = 0.02) with higher risk of clinical malaria in children (Table 6).
Table 5.
Factors associated with risk of clinical malaria in univariate logistic regression models, showing odds ratios (OR) and 95% confidence intervals (CI).
| Antibody | Antibody levels | Age cohort | Sex | Site | WAZ | HAZ | Hb | Exposure index | Maternal antibodies | Prior episode† | Seasonǂ | Vaccine | IgG at M0 | IgM at M0 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR (CI) P-val | OR (CI) P-val | OR (CI) P-val | OR (CI) P-val | OR (CI) P-val | OR (CI) P-val | OR (CI) P-val | OR (CI) P-val | OR (CI) P-val | OR (CI) P-val | OR (CI) P-val | OR (CI) P-val | OR (CI) P-val | OR (CI) P-val | |
| All participants together | ||||||||||||||
| IgG | 0.83 (0.55;1.24) 0.74 | 0.74 (0.38;1.42) 1 | 1.24 (0.7;2.19) 1 | 0.1 (0.05;0.19) <0.001 | 0.73 (0.55;0.95) 0.059 | 0.75 (0.57;0.96) 0.1 | 0.91 (0.74;1.11) 1 | 1.18 (1.09;1.28) <0.001 | 1.39 (1.22;1.61) <0.001 | 4.55 (1.69;14.5) 0.01 | 0.66 (0.17;2.26) 1 | 0.64 (0.35;1.16) 0.7 | 0.7 (0.38;1.28) 1 | 0.8 (0.56;1.13) 1 |
| IgG1 | 0.74 (0.49;1.1) 0.41 | 0.78 (0.43;1.43) 1 | 1.26 (0.71;2.23) 1 | 0.1 (0.05;0.19) <0.001 | 0.73 (0.56;0.95) 0.059 | 0.74 (0.57;0.96) 0.1 | 0.9 (0.73;1.11) 1 | 1.17 (1.08;1.27) <0.001 | 1.39 (1.22;1.6) <0.001 | 4.38 (1.62; 13.95) 0.01 | 0.68 (0.17;2.36) 1 | 0.6 (0.33;1.1) 0.61 | 0.8 (0.49;1.29) 1 | 0.83 (0.6;1.14) 1 |
| IgG2 | 1.01 (0.65;1.57) 0.95 | 0.79 (0.42;1.48) 1 | 1.48 (0.82;2.7) 1 | 0.1 (0.05;0.2) <0.001 | 0.7 (0.52;0.92) 0.047 | 0.73 (0.55;0.94) 0.09 | 0.89 (0.72;1.09) 1 | 1.16 (1.07;1.26) <0.001 | 1.39 (1.22;1.61) <0.001 | 3.8 (1.38;12.25) 0.02 | 0.49 (0.1;1.82) 1 | 0.66 (0.35;1.23) 0.7 | 0.71 (0.39;1.26) 1 | 0.84 (0.6;1.16) 1 |
| IgG3 | 0.02 (0;0.18) <0.001 | 1.34 (0.69;2.65) 1 | 1.24 (0.69;2.24) 1 | 0.12 (0.06;0.23) <0.001 | 0.71 (0.52;0.93) 0.059 | 0.76 (0.58;0.99) 0.1 | 0.87 (0.7;1.08) 1 | 1.18 (1.09; 1.28) <0.001 | 1.34 (1.18;1.55) <0.001 | 3.97 (1.44;13.02) 0.02 | 0.57 (0.14;2) 1 | 0.64 (0.34;1.19) 0.7 | 0.87 (0.54;1.4) 1 | 1.03 (0.73;1.45) 1 |
| IgG4 | 0.02 (0;0.2) 0.001 | 1.21 (0.63;2.36) 1 | 1.18 (0.66;2.11) 1 | 0.11 (0.06;0.22) <0.001 | 0.72 (0.54;0.95) 0.059 | 0.76 (0.58;0.98) 0.1 | 0.87 (0.7;1.07) 1 | 1.17 (1.09;1.28) <0.001 | 1.35 (1.18;1.56) <0.001 | 3.99 (1.44;13.08) 0.02 | 0.53 (0.13;1.84) 1 | 0.64 (0.34;1.18) 0.7 | 0.82 (0.52;1.3) 1 | 1 (0.71;1.4) 1 |
| IgM | 0.43 (0.26;0.68) 0.001 | 1.87 (0.86;4.23) 0.7 | 1.07 (0.59;1.93) 1 | 0.11 (0.05;0.21) <0.001 | 0.65 (0.48;0.86) 0.01 | 0.75 (0.57;0.98) 0.1 | 0.84 (0.67;1.04) 0.6 | 1.27 (1.16;1.4) <0.001 | 1.32 (1.15;1.53) <0.001 | 4.43 (1.6;14.39) 0.01 | 0.47 (0.12;1.68) 1 | 0.65 (0.35;1.2) 0.7 | 0.82 (0.51;1.29) 1 | 1.44 (0.91;2.33) 0.7 |
| Antibody levels | Sex | Site | WAZ | HAZ | Hb | Exposure to malaria | Maternal antibodies | Prior episode† | Seasonǂ | vaccine | IgG at M0 | IgM at M0 | ||
| OR (CI) P-val | OR (CI) P-val | OR (CI) P-val | OR (CI) P-val | OR (CI) P-val | OR (CI) P-val | OR (CI) P-val | OR (CI) P-val | OR (CI) P-val | OR (CI) P-val | OR (CI) P-val | OR (CI) P-val | OR (CI) P-val | ||
| Infants | ||||||||||||||
| IgG | 1.04 (0.43;2.51) 1 | 1.31 (0.61;2.81) 1 | 0.13 (0.05;0.32) <0.001 | 0.84 (0.58;1.22) 1 | 0.72 (0.5;1) 0.28 | 1.12 (0.81;1.58) 1 | 1.16 (1.03;1.33) 0.07 | 1.35 (1.16;1.61) <0.001 | 4.61 (1.09;31.58) 0.22 | 0.53 (0.13;1.91) 1 | 0.89 (0.4;1.98) 1 | 0.98 (0.38;2.53) 1 | 0.69 (0.36;1.26) 1 | |
| IgG1 | 0.81 (0.41;1.52) 1 | 1.29 (0.61;2.77) 1 | 0.14 (0.06;0.35) <0.001 | 0.84 (0.57;1.21) 1 | 0.72 (0.5;1) 0.28 | 1.11 (0.79;1.57) 1 | 1.16 (1.03; 1.33) 0.07 | 1.35 (1.15;1.61) <0.001 | 4.45 (1.04;30.73) 0.22 | 0.58 (0.14;2.08) 1 | 0.86 (0.38;1.92) 1 | 0.99 (0.47;2.1) 1 | 0.68 (0.36;1.26) 1 | |
| IgG2 | 1.65 (0.68;4.17) 1 | 1.83 (0.82;4.15) 0.83 | 0.15 (0.06;0.38) <0.001 | 0.77 (0.52;1.13) 0.92 | 0.71 (0.49;1) 0.28 | 1.06 (0.76;1.51) 1 | 1.16 (1.03;1.34) 0.07 | 1.38 (1.17;1.66) <0.001 | 3.19 (0.67;22.94) 0.22 | 0.37 (0.07;1.46) 0.95 | 0.91 (0.39;2.13) 1 | 1.01 (0.42;2.41) 1 | 0.74 (0.37;1.44) 1 | |
| IgG3 | 0.01 (0;13.86) 1 | 1.41 (0.65;3.06) 1 | 0.15 (0.06;0.36) <0.001 | 0.84 (0.57;1.22) 1 | 0.74 (0.52;1.03) 0.28 | 1.09 (0.78;1.54) 1 | 1.16 (1.03;1.33) 0.07 | 1.35 (1.15;1.59) <0.001 | 4.39 (1.03;30.19) 0.22 | 0.64 (0.15;2.36) 1 | 0.94 (0.42;2.1) 1 | 1.07 (0.5;2.28) 1 | 0.68 (0.36;1.24) 1 | |
| IgG4 | 0.09 (0;4636.2) 1 | 1.28 (0.6;2.75) 1 | 0.14 (0.05;0.34) <0.001 | 0.83 (0.56;1.2) 1 | 0.72 (0.51;1) 0.28 | 1.12 (0.8;1.58) 1 | 1.16 (1.03;1.33) 0.07 | 1.37 (1.16;1.63) <0.001 | 4.58 (1.06;31.87) 0.22 | 0.55 (0.14;1.96) 1 | 0.92 (0.41;2.04) 1 | 1.01 (0.48;2.13) 1 | 0.69 (0.36;1.29) 1 | |
| IgM | 0.24 (0.1;0.52) <0.001 | 0.87 (0.37;1.98) 1 | 0.22 (0.08;0.57) 0.002 | 0.74 (0.48;1.1) 0.82 | 0.71 (0.48;1.01) 0.28 | 1.02 (0.71;1.46) 1 | 1.24 (1.08;1.44) 0.009 | 1.26 (1.07;1.5) 0.006 | 3.63 (0.79;26) 0.22 | 0.54 (0.13;2.02) 1 | 1.04 (0.44;2.46) 1 | 1.25 (0.56;2.82) 1 | 1.08 (0.54;2.23) 1 | |
| Antibody levels | Sex | Site | WAS | HAZ | Hb | Exposure to malaria | Maternal antibodies | Prior episode † | vaccine | IgG at M0 | IgM at M0 | |||
| OR (CI) P-val | OR (CI) P-val | OR (CI) P-val | OR (CI) P-val | OR (CI) P-val | OR (CI) P-val | OR (CI) P-val | OR (CI) P-val | OR (CI) P-val | OR (CI) P-val | OR (CI) P-val | OR (CI) P-val | |||
| Children | ||||||||||||||
| IgG | 0.88 (0.5;1.53) 1 | 1.16 (0.49;2.78) 1 | 0.02 (0;0.09) <0.001 | 0.59 (0.38;0.88) 0.043 | 0.79 (0.52;1.18) 1 | 0.71 (0.52;0.96) 0.14 | 1.29 (1.14;1.49) <0.001 | 1.6 (1.21;2.31) 0.001 | 4.78 (1.26;23.32) 0.12 | 0.4 (0.16;1) 0.25 | 0.23 (0.07;0.7) 0.05 | 1.27 (0.41;4.09) 1 | ||
| IgG1 | 0.76 (0.42;1.32) 1 | 1.18 (0.5;2.84) 1 | 0.03 (0.01;0.11) <0.001 | 0.6 (0.38;0.89) 0.043 | 0.79 (0.52;1.17) 1 | 0.73 (0.53;0.97) 0.15 | 1.29 (1.14;1.49) <0.001 | 1.6 (1.22;2.31) 0.001 | 4.89 (1.28;24.2) 0.12 | 0.39 (0.15;0.98) 0.25 | 0.55 (0.24;1.19) 0.5 | 1.25 (0.45;3.62) 1 | ||
| IgG2 | 0.91 (0.52;1.57) 1 | 1.09 (0.44;2.72) 1 | 0.04 (0.01;0.12) <0.001 | 0.59 (0.37;0.9) 0.043 | 0.75 (0.48;1.13) 1 | 0.73 (0.53;0.97) 0.15 | 1.28 (1.13;1.49) <0.001 | 1.54 (1.18;2.22) 0.002 | 4.34 (1.13;21.36) 0.12 | 0.39 (0.15;1) 0.25 | 0.46 (0.18;1.11) 0.42 | 1.31 (0.44;4.03) 1 | ||
| IgG3 | 0.02 (0;0.18) 0.002 | 1.11 (0.44;2.8) 1 | 0.04 (0.01;0.15) <0.001 | 0.56 (0.34;0.88) 0.043 | 0.78 (0.51;1.19) 1 | 0.74 (0.53;1) 0.15 | 1.24 (1.1;1.44) <0.001 | 1.51 (1.13;2.26) 0.007 | 3.41 (0.83;17.99) 0.15 | 0.36 (0.13;0.97) 0.25 | 0.78 (0.42;1.46) 0.61 | 1.44 (0.49;4.49) 1 | ||
| IgG4 | 0.01 (0;0.18) 0.003 | 1.06 (0.42; 2.66) 1 | 0.05 (0.01;0.16) <0.001 | 0.61 (0.38;0.93) 0.043 | 0.81 (0.53;1.22) 1 | 0.72 (0.51;0.97) 0.15 | 1.25 (1.1;1.45) <0.001 | 1.5 (1.11;2.25) 0.007 | 3.65 (0.88;19.45) 0.15 | 0.36 (0.13;0.97) 0.25 | 0.73 (0.4;1.32) 0.61 | 1.25 (0.45;3.64) 1 | ||
| IgM | 0.55 (0.16;1.82) 1 | 1.18 (0.5; 2.84) 1 | 0.04 (0.01;0.13) <0.001 | 0.58 (0.36;0.86) 0.041 | 0.79 (0.52;1.17) 1 | 0.73 (0.53;0.97) 0.15 | 1.29 (1.14;1.49) <0.001 | 1.72 (1.26;2.62) <0.001 | 4.54 (1.19;22.19) 0.12 | 0.4 (0.15;0.99) 0.25 | 0.64 (0.35;1.13) 0.5 | 1.68 (0.51;6.44) 1 | ||
Data from the phase 3 trial participants, including anti-α-Gal antibody data at M3 and covariates. The analysis was performed for all participants together and stratifying by age group (infants and children). Results show those factors that affect the risk of clinical malaria when anti-α-Gal antibodies are taken into account. P-values were adjusted for multiple comparisons through Benjamini-Hochberg and Holm, those significant are in bold.
Age cohort (children vs infants). Sex (male vs female). Site (Manhiça vs Kintampo). WAZ (Weight-for-Age Z-score). HAZ (Height-for-Age Z-score). Hb (Baseline hemoglobin (g/dL). Exposure index (baseline anti-P. falciparum exposure IgM levels). Maternal index (baseline maternally transferred antibodies). †Malaria episode between month 0 and month 3 (yes vs no). ǂMalaria transmission season at month 3 sample collection (low vs high). Vaccine (RTS,S vs comparator).
Table 6.
Association between anti-α-Gal antibody levels and risk of clinical malaria in multivariable logistic regression models.
| Antibody | All subjects together | Infants | Children | |||
|---|---|---|---|---|---|---|
| OR (CI) p-val | Covariates* | OR (CI) p-val | Covariates* | OR (CI) p-val | Covariates* | |
| IgG | 1.86 (1;3.5) 0.051 | Age, site, exposure | Site, exposure | 7.99 (1.54;58.03) 0.02 | Site, vaccine | |
| IgG1 | Age, site, exposure | Site, exposure | Site, vaccine | |||
| IgG2 | Age, site, exposure | Site, exposure | Site, vaccine | |||
| IgG3 | Age, site, exposure | Site, exposure | Site, vaccine | |||
| IgG4 | Age, site, exposure | Site, exposure | Site, vaccine | |||
| IgM | 0.38 (0.2;0.71) 0.003 | Site, exposure | 0.29 (0.1;0.77) 0.02 | Site, exposure | Site, vaccine | |
Data from phase 3 trial including all individuals together and stratified by age group, fitted including anti-α-Gal antibody data at M3 and adjusting by significant variables in univariate models to remove potential cofounding effects in the associations. P-values were adjusted for multiple comparisons. Data presented correspond to variables that were statistically significant.
*Covariates that in the multivariable analyses (backward and forward stepwise algorithms combined to obtain the model with the minimum akaike information criterion) were statistically significant. Age (Infants vs children); Site (Manhiça vs Kintampo); Exposure (malaria exposure antibody index); Vaccine (RTS,S vs comparator).
Discusion
We have assessed the IgM, IgG and IgG1–4 responses to α-Gal in children of different ages from two different African countries. Results show that anti-α-Gal IgM and IgG responses vary mainly depending on the age of the child and the location, but other factors like level of malaria exposure and maternally-transferred antibodies also affect them. Importantly, our data indicates that the magnitude of IgM responses to α-Gal is associated to protection against malaria, especially in the first months of life, while IgG levels may correlate with malaria risk. Our findings also point towards a possible protective role of anti-α-Gal IgG3 and IgG4 that needs to be better addressed in larger studies. Since antibodies against α-Gal are usually measured in Caucasian adults, and prior data on their levels in childhood are incomplete or even inexistent in African children19,27,28, our study provides novel and relevant information on anti-α-Gal antibody responses that are putative targets of immunity against several infectious diseases.
First, we provide additional insight into the age pattern of serological responses to this glycan. The anti-α-Gal IgM response in infants age 1.5 to 3 months started at very low levels but showed a rapid increase during the first months of life, reaching higher levels than IgG. This result is similar to Hamanova et al.28 on European children, and suggests exposure to α-Gal in the neonate and maintenance of this exposure over time. However, our data show an earlier and faster increase of α-Gal antibodies in African children. Exposure to α-Gal originates in the neonate gut microbiota, which is influenced by the mode of delivery, the gestational age and the mother breast milk microbiota, which in turn is influenced by maternal health29–31. All these factors are expected to be different between Europeans and Africans. Moreover, recent studies show that there is a significant effect of geographical variations in human milk microbiota composition30,32. Thus, geographical differences in human milk microbiota and exposure to pathogenic microbes could explain the differences in the anti-α-Gal IgM responses between European and African infants, and potentially among African regions.
Here, the α-Gal IgG response was already high in infants and did not increase during the first months of life. On the contrary, it tended to decrease, as evidenced when comparing Ig levels between M0 and M3 in this age group. On the other hand, in children (5 to 17 months old) IgG levels at M0 were similar to levels at M0 in infants, and increased towards M3. These results evidence a significant maternal transfer of anti-α-Gal IgG to the newborn, and a decay of this IgG during the first months of life, followed by an early and rapid increase. This suggests again a continued exposure to the glycan. These results are also similar to reports in European children28, although our data also suggest an earlier and faster increase of anti-α-Gal IgGs in African children compared to Europeans.
Overall, IgM and IgG to-α-Gal increased with age, however IgM reached higher levels than IgG, being the predominant response in children. This result is in agreement with previous works by Yilmaz et al. on subjects from 3 months to 25 years of age in Mali17. In that study, this observation was interpreted as indicative of P. falciparum infection failing to induce class switch of the anti-α-Gal Ig antibody response. However a higher IgM response than its correspondent IgG response is also observed against other polysaccharidae antigens, such as Streptococcus pneumoniae33, suggesting that overall the rate of IgM/IgG switching is not as fast for polysaccharide antigens as for protein antigens.
Second, we analyzed the effect of malaria endemicity on the anti-α-Gal response. When comparing anti-α-Gal IgM and IgG responses between two areas of high (Kintampo) and low (Manhiça) MTI, we observed that both antibodies were higher at lower MTI. This may suggest that other exposures besides malaria may be more important for their induction. It is known that, besides Plasmodium17, other pathogenic microbes express this glycan, like the protozoan parasites Leishmania spp. and Trypanosoma spp, the Gram-negative bacteria Salmonella spp., and some viruses22,23,34. Furthermore, common commensal bacteria in the midgut microbiota such as Escherichia spp., Klebsiella spp. and Serratia spp. also express α-Gal22. Also, exposure to different types of diet in both sites could be associated to the different anti-α-Gal responses. However, another possible explanation is that malaria infection affects the immune response to α-Gal in children living in high MTI. Previous studies show that P. falciparum malaria impairs the antibody response to polysaccharide vaccines (glycan antigens) but not responses to protein-based and whole parasite vaccines in children with malaria35. Young children (<3 years old) have immunologically immature spleens, mainly due to the still ongoing development of the marginal zone (MZ) B cell subset, which is the main responsible for the IgM response to polysaccharide antigens36,37. During malaria infection, the anatomy of the spleen becomes disorganized, with sometimes a complete dissolution of the MZ38,39. Accordingly, several studies have found a reduction of peripheral MZ-like B cells in patients with malaria40–42, which could explain the reduction in the IgM response in children with higher malaria exposure43 that may affect IgM response to α-Gal. However, in spite of the higher anti-α-Gal IgM response observed in the lower MTI site, the multivariable analysis showed that recent/current exposure to Plasmodium was positively associated to the levels of anti-α-Gal IgM, implying that malaria infection in fact induces IgM against α-Gal. These models also showed a negative effect of maternally transferred P. falciparum IgGs on the anti-α-Gal IgG and IgM responses in the offspring, suggesting an interference with anti-α-Gal antibody induction in children. A negative effect of maternal antibodies has been reported in the context of immune responses to vaccines44.
Third, we investigated the role of α-Gal antibodies in malaria risk or protection. Remarkably, anti-α-Gal IgM levels were higher in infants who did not subsequently develop any episode of malaria. Interestingly, this association was only observed in Manhiça in site-stratified analysis. The fact that this association was only observed in infants but not in children contrasts with the results by Yilmaz et al., where anti-α-Gal IgMs were associated to protection in Malian children >4 years old17. Disparity may result from several differences between the studies: (i) different samples sizes (195 in our study vs 695 in Mali study); (ii) separate countries with different levels of α-Gal exposure due to malaria and other pathogens; (iii) different follow up times (12 months in our study vs 6 months in Mali); (iv) different age ranges of subjects (1.5 to 17 months in our study vs 4 to 25 years in Mali); and, specially, due to the different ways to detect and define clinical malaria (passive case detection [PCD] defined by fever with any parasitemia in our study vs active case detection defined by fever with parasitemia ≥2500 parasites/mL in the Mali study).
Unlike IgM, anti-α-Gal IgG levels were associated with a higher risk of malaria in children, which suggests that a higher exposure to other pathogenic microbes containing α-Gal may increase the risk of a future malaria episode by, for example, deviating the immune response and/or causing a worst clinical outcome in co-infection. This result contrasts with the recent observation by Cabezas-Cruz et al. of a positive correlation of anti-α-Gal IgM and IgG with the lack of Plasmodium infection in individuals from Senegal45. However disparity of results may also be due to differences between the study site, age of participants and the study design.
We also investigated for the first time IgG1–4 subclass responses to α-Gal and observed new associations between certain subclasses and malaria protection. Interestingly, the pattern of IgG1–4 subclasses to α-Gal showed predominance of IgG1 and IgG2, followed by IgG3 and IgG4. This is different to the pattern against P. falciparum proteins, where IgG1 and IgG3 predominate and IgG2 and IgG4 are induced at much lower levels. Higher α-Gal IgG3 and IgG4 levels may correlate with malaria protection in children, also contrasting to what has been observed against protein antigens. Previous studies consistently show that cytophilic antibodies (IgG1 and IgG3) to protein antigens correlate more often with protection from malaria disease46–50. However, this may be different for glycan antigens. For example, IgG4 responses predominate against Schistosoma mansoni51 with many antigenic glycans on its surface52, and this subclass is associated with protection against S. haematobium53. IgG4 has been shown to be a blocking and tolerance-inducing “anti-allergenic” antibody54,55. Therefore its protective effect could be mediated through a tolerogenic response to the Plasmodium infection. However, IgG3 and IgG4 associations to malaria protection were lost in multivariable analysis and further studies with larger samples sizes are needed to better address this potential protective effect.
The study had some limitations, mostly related to the fact that it was performed with samples from the RTS,S clinical trial consisting on two age cohorts, forcing some design issues, e.g., the age range and the vaccination. Second, the unfeasibility to determine the exposure to other sources of α-Gal besides malaria, including other pathogens, commensal bacteria or food, which would have been helpful to understand why anti-α-Gal responses were higher in one site vs the other. Nevertheless, the fact the children from high MTI settings showed significantly lower levels of anti-α-Gal IgG and IgM compared to children living in lower MTI settings, might be a sign of an underlying impairment of the immune response to polysaccharide antigens in the context of high MTI. These data along with the observed reduction of MZ-like B cells in chronically exposed individuals40–42, the documented deficient antibody response to polysaccharide vaccines in children with malaria35 and the higher susceptibility of these children to invasive bacterial infections by polysaccharide encapsulated bacteria (as non-typhoid salmonella and S. pneumoniae)56,57, warrant further investigation.
Conclusions
Age and site affect the magnitude of anti-α-Gal IgM and IgG responses in African children. Levels of α-Gal IgG3, IgG4 and, particularly, IgM are associated with protection against clinical malaria, while total IgG levels correlate with malaria risk, supporting further investigations of α-Gal as a promising antigen target for future malaria vaccines.
Materials and Methods
Subjects and samples
Samples from African children participating in RTS,S/AS0 clinical trials were included in this analysis. First, a pilot study to assess age patterns of anti-α-Gal antibody immunogenicity in individuals age <5 years old was performed with serum samples from 104 Mozambican children of two cohorts exposed to different levels of MTI (Manhiça - low MTI, and Ilha Josina - high MTI), vaccinated with RTS,S/AS02 within a phase 2b trial58. This pilot was carried out to set up the α-Gal antibody assay and to confirm the age pattern of response previously described in Malian children17. A second larger study was performed to assess IgG subclasses and association between anti-α-Gal antibodies and malaria protection, and factors affecting it. This analysis included plasma and serum samples from 195 subjects enrolled in the RTS,S/AS01 phase 3 trial59 from two younger age groups (1.5–3 months [infants] and 5–17 months [children]), and two different African sites (Manhiça-Mozambique [low MTI] and Kintampo-Ghana [moderate-high MTI]), having 131 RTS,S-vaccinees and 66 comparator-vaccinees.
In both studies, samples were collected at the first study visit (recruitment, coinciding with baseline before vaccination, M0) and the second study timepoint three months later (M3, after three doses of vaccination). For the detection of clinical malaria cases (fever >37.5 °C with any parasitaemia), children were followed up by PCD starting 14 days after sample collection at M3 for the subsequent 12 months.
Antibody Luminex assay
Antibodies against α-Gal (Galα1-3 Galβ1-4GlcNAc-R-BSA, Dextra NGP0334) were measured by quantitative suspension array technology (qSAT) using the Luminex xMAP™ technology (Luminex Corp., Austin, Texas). α-Gal was covalently coupled to MagPlex beads and these were blocked with BSA. α-Gal-coupled beads were added to 96-well μClear® flat bottom plates (Greiner Bio-One) (1,000 microspheres/well) resuspended in 50 µL of PBS, 1% BSA, 0.05% Azide pH 7.4 (PBS-BN). The multiplex antigens panel also contained beads coupled to 32 P. falciparum protein constructs based on pre-erythrocytic (SSP2/TRAP, CelTOS, LSA-1, EXP-1) and erythrocytic (AMA-1, EBA-140, EBA-175, MSP-1, MSP-2, MSP-3, MSP-5, MSP-6, CyRPA, P41, PfRh1, PfRh2, PfRh4, var2csa) stage antigens analyzed as markers of malaria exposure and maternally-transferred antibodies.
Fifty µL of sample, positive control (serial dilutions of the WHO reference reagent for anti-malaria human serum NIBSC code 10/198 for the IgG assays; or a pool of samples with high IgM levels against P. falciparum for the IgM assay)60, negative control (individual plasma samples from malaria naïve Spanish adults) or PBS-BN (Blanks) were added to the wells and incubated with the beads at 4 °C overnight (ON) in a shaker protected from light. Plates were washed three times with 200 µL/well of PBS-Tween 20 0.05% using a manual magnetic washer. 100 µL of biotinylated secondary antibody were added diluted in PBS-BN as described61: anti-human IgG (Sigma), anti-human IgM (Sigma), anti-human IgG1 (Abcam) and anti-human IgG3 (Sigma). For IgG2 and IgG4 assays, secondary antibodies added were unconjugated mouse anti-human IgG4 (Thermo Fisher) and mouse anti-human IgG2 (Thermo Fisher), respectively, followed by biotinylated goat anti-mouse IgG (Sigma) in PBS-BN. All antibody incubations were performed at room temperature (RT) for 60 min, in agitation and protected from light. Next, 100 µL of streptavidin-R-phycoerythrin (Sigma) in PBS-BN were added to all wells and incubated 30 min, at RT, in agitation and protected from light. Plates were washed as before and beads were resuspended in 100 μL/well of PBS-BN. Plates were covered protected from light and stored at 4 °C ON to be read the next day using the Luminex xMAP® 100/200 analyser, and at least 50 microspheres per analyte were acquired per sample.
Test samples were assayed at 4 dilutions for IgG (500, 5000, 50,000 and 500,000), IgG1, IgG3 (100, 1000, 10,000 and 100,000) and IgM (100, 1000, 10,000 and 50,000), and 2 dilutions for IgG2 and IgG4 (50 and 500) to ensure that at least one dilution lie in the linear range of the respective standard curve. For IgG assays, 18 to 22 serial dilutions (1:2) of the positive control starting at 1:50 were used to perform subclass-specific standard curves. For the IgM assay, 18 serial dilutions (1:2) of a pool of samples from ISGlobal repository with high IgM levels against P. falciparum antigens were used. Blanks were added to each plate in triplicates for quality control purposes. Sample distribution across plates was designed ensuring a balanced distribution of site, age cohort and malaria cases. Data were captured using xPonent software, and antibody levels were measured as median fluorescence intensity (MFI).
Data analysis
Preprocessing
To stabilize the variance, the analysis was done on log10-transformed values of the MFI measurements. The positive control standard curve for each isotype/subclass-plate was estimated using the drLumi R package flow62. Standard curves were fitted in a 5-parameter logistic (5-PL) regression model, and data points were weighted by logarithmic variance. If the model did not converge, 4-PL or exponential regressions were fitted. The quality control for each plate was based on the estimation of the % coefficient of variation (CV) of the 3 blank controls. Blanks were also used to establish the antigen-isotype/subclass specific lower limits of quantification (LLOQ) and lower limits of detection (LLOD) calculated as the blanks mean +10 SD and blanks mean +3 SD, respectively63. The characteristics of the standard curves were visually inspected for quality control purposes. To select the sample working dilution (isotype/subclass and plate specific), an algorithm that detects the two points with the highest slope between them in the positive control sigmoidal curve was used. The slope was computed as:
The mean log10 MFI value of the two points was computed, and the nearest log10 MFI of the test sample and the corresponding dilution was selected. For IgG2 and IgG4 assays standard curves did not converge, then the first sample dilution was assigned. The log10 MFI of the selected dilution was corrected multiplying by its corresponding dilution factor. Blank background signal was not subtracted.
Statistical analysis
Descriptive comparisons of antibody levels between age groups, time points and sites were done by trajectory plots, boxplots representing the median and interquartile range (analyzed by t-tests), and dotplots with bars corresponding to the geometric mean and confidence intervals (CI) (analyzed by the Mann Whitney t-test). The effect of age was also evaluated through scatterplots and regression models and assessing its interaction with site.
The analysis of factors affecting levels of anti-α-Gal Ig at M3 was performed using data from children participating in the RTS,S phase 3 trial and applying multivariable linear regression models (Coefficient, 95% CI, p values). The predictors assessed were: age as continuous variable (weeks), age cohort (children vs infants), sex (male vs female), site (Manhiça vs Kintampo), baseline weight for age Z score (WAZ) and height for age Z score (HAZ), baseline hemoglobin levels (Hb), malaria episodes prior to M3 (yes vs no), malaria transmission season (low vs high), vaccination (RTS,S vs comparator), baseline α-Gal IgG levels, baseline α-Gal IgM levels, level of malaria exposure and maternally-transferred malaria antibodies. To define a P. falciparum exposure index, we selected 28 protein antigens in which IgM responses were M3 > M0 and thus acquired with age (e.g. children > infants) and exposure (e.g. Kintampo > Manhiça) (data not shown). Principal component analysis (PCA) was performed to construct the corresponding variables, and the first component (PC1) that explained 63% of the variability was selected to be used as a variable in the models. To define a P. falciparum maternal antibody index in subjects <10 months of age, we selected 17 antigens including two VAR2CSA pregnancy-specific antigen constructs which IgG responses were M0 > M3 and thus declined with age (e.g. infants > children) and were higher in infants from the high MTI site (e.g. Kintampo > Manhiça) (data not shown). We selected the first component that explained 54% of the variability and used that as a variable in the models.
The analysis of the association between anti-α-Gal antibody levels and clinical malaria was based on a case-control design. Univariate logistic regression models (odds ratio [OR], 95% CI, p values) with α-Gal antibody data at M3 as main predictor, including other covariates (same as above) and their interactions, were fitted to identify factors that affected malaria risk when α-Gal antibodies were taken into account. Covariates that were significant in the univariate models were included in the stepwise (forward and backward) multivariable models to remove potential cofounding effects. P-values were adjusted for multiple testing through Benjamini-Hochberg or Holm, depending on the analysis. None of the interactions were significant after adjusting for multiple comparisons, therefore they are not reported in the tables. All models were also performed stratifying by age group, by site, and by age and site at the same time. Significance was defined at the p < 0.05 level and analyses were performed with R.
Data availability
All data generated or analyzed during this study are included in this published article (and its Supplementary Information files).
Ethics Statement
All methods were performed in accordance with the relevant guidelines and regulations. Approval for the study protocol was obtained from the Ethical Committee of the Hospital Clínic in Barcelona (CEIC, Spain), the National Health and Bioethics Committee (CNBS, Mozambique), and the Ghana Health Service Ethical Review Committee (GHSERC, Ghana). Written informed consent was obtained from parents or guardians of participating children in accordance with the Declaration of Helsinki.
Electronic supplementary material
Acknowledgements
We are grateful to the volunteers and their families; the clinical, field and lab teams at the research institutions from the phase 2b and phase 3 trials, particularly Jahit Sacarlal and Pedro Alonso; the MAL067 Vaccine Immunology Consortium and Working Groups, particularly Nana Aba Williams and Núria Díez; the protein suppliers, David Lanar, Virander Chauhan, Chetan Chitnis, Deepak Gaur, Ross Coppel, David Cavanagh, Benoit Gamain, Evelina Angov, and James Beeson; the hyper-immune plasma suppliers (NIBSC, UK); ISGlobal is a member of the CERCA Program, Generalitat de Catalunya. NIH-NIAID (R01AI095789), PATH Malaria Vaccine Initiative (MVI), Ministerio de Economía y Competitividad (Instituto de Salud Carlos III, PI11/00423, and SAF2016-76080-R AEI/FEDER-UE), EviMalaR and AGAUR-Catalonia (2014 SGR991). European Commission funding for P.G. PhD.
Author Contributions
Wrote the first draft: R.A., C.D.; Conceived the study: R.A., G.P.G.-P., L.I., C.D.; Performed database management, statistical analysis and experimental design: I.U., N.B., N.C., A.A., H.S., J.J.C.; Collected samples and data and participated in the clinical trial: A.N., C.J., D.D., B.G., J.J.C.; Performed the experiments: I.U., M.V., A.J.; Coordinated the study: R.A., C.D.; Participated in the design of the analysis: R.A., C.D.; Contributed to the write up of the manuscript: I.U., G.P.G.-P., L.I.; All reviewed and approved the manuscript.
Competing Interests
The authors declare no competing interests.
Footnotes
Electronic supplementary material
Supplementary information accompanies this paper at 10.1038/s41598-018-28325-w.
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Luis Izquierdo, Email: luis.izquierdo@isglobal.org.
Carlota Dobaño, Email: carlota.dobano@isglobal.org.
References
- 1.Cobb BA, Kasper DL. Coming of age: carbohydrates and immunity. Eur J Immunol. 2005;35:352–356. doi: 10.1002/eji.200425889. [DOI] [PubMed] [Google Scholar]
- 2.Beuvery EC, van Rossum F, Nagel J. Comparison of the induction of immunoglobulin M and G antibodies in mice with purified pneumococcal type 3 and meningococcal group C polysaccharides and their protein conjugates. Infect Immun. 1982;37:15–22. doi: 10.1128/iai.37.1.15-22.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barrett DJ, Ammann AJ, Stenmark S, Wara DW. Immunoglobulin G and M antibodies to pneumococcal polysaccharides detected by enzyme-linked immunosorbent assay. Infect Immun. 1980;27:411–417. doi: 10.1128/iai.27.2.411-417.1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grundner C, et al. Factors limiting the immunogenicity of HIV-1gp120 envelope glycoproteins. Virology. 2004;330:233–248. doi: 10.1016/j.virol.2004.08.037. [DOI] [PubMed] [Google Scholar]
- 5.Godfrey DI, Kronenberg M. Going both ways: immune regulation via CD1d-dependent NKT cells. J Clin Invest. 2004;114:1379–1388. doi: 10.1172/JCI200423594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tzianabos AO, et al. T cells activated by zwitterionic molecules prevent abscesses induced by pathogenic bacteria. J Biol Chem. 2000;275:6733–6740. doi: 10.1074/jbc.275.10.6733. [DOI] [PubMed] [Google Scholar]
- 7.Trotter CL, Ramsay ME. Vaccination against meningococcal disease in Europe: review and recommendations for the use of conjugate vaccines. FEMS Microbiol Rev. 2007;31:101–107. doi: 10.1111/j.1574-6976.2006.00053.x. [DOI] [PubMed] [Google Scholar]
- 8.Rodrigues JA, et al. Parasite Glycobiology: A Bittersweet Symphony. PLoS Pathog. 2015;11:e1005169. doi: 10.1371/journal.ppat.1005169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Naik RS, Krishnegowda G, Ockenhouse CF, Gowda DC. Naturally elicited antibodies to glycosylphosphatidylinositols (GPIs) of Plasmodium falciparum require intact GPI structures for binding and are directed primarily against the conserved glycan moiety. Infect Immun. 2006;74:1412–1415. doi: 10.1128/IAI.74.2.1412-1415.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cova M, Rodrigues JA, Smith TK, Izquierdo L. Sugar activation and glycosylation in Plasmodium. Malar J. 2015;14:427. doi: 10.1186/s12936-015-0949-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sanz S, et al. Biosynthesis of GDP-fucose and other sugar nucleotides in the blood stages of Plasmodium falciparum. J Biol Chem. 2013;288:16506–16517. doi: 10.1074/jbc.M112.439828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lopez-Gutierrez B, Dinglasan RR, Izquierdo L. Sugar nucleotide quantification by liquid chromatography tandem mass spectrometry reveals a distinct profile in Plasmodium falciparum sexual stage parasites. Biochem J. 2017;474:897–905. doi: 10.1042/BCJ20161030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bushkin GG, et al. Suggestive evidence for Darwinian Selection against asparagine-linked glycans of Plasmodium falciparum and Toxoplasma gondii. Eukaryot Cell. 2010;9:228–241. doi: 10.1128/EC.00197-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Swearingen KE, et al. Interrogating the Plasmodium Sporozoite Surface: Identification of Surface-Exposed Proteins and Demonstration of Glycosylation on CSP and TRAP by Mass Spectrometry-Based Proteomics. PLoS Pathog. 2016;12:e1005606. doi: 10.1371/journal.ppat.1005606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sanz S, et al. The disruption of GDP-fucose de novo biosynthesis suggests the presence of a novel fucose-containing glycoconjugate in Plasmodium asexual blood stages. Sci Rep. 2016;6:37230. doi: 10.1038/srep37230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Agnandji ST, et al. A phase 3 trial of RTS,S/AS01 malaria vaccine in African infants. N Engl J Med. 2012;367:2284–2295. doi: 10.1056/NEJMoa1208394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yilmaz B, et al. Gut microbiota elicits a protective immune response against malaria transmission. Cell. 2014;159:1277–1289. doi: 10.1016/j.cell.2014.10.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ramasamy R, Reese RT. Terminal galactose residues and the antigenicity of Plasmodium falciparum glycoproteins. Mol Biochem Parasitol. 1986;19:91–101. doi: 10.1016/0166-6851(86)90113-1. [DOI] [PubMed] [Google Scholar]
- 19.Galili U, Rachmilewitz EA, Peleg A, Flechner I. A unique natural human IgG antibody with anti-alpha-galactosyl specificity. J Exp Med. 1984;160:1519–1531. doi: 10.1084/jem.160.5.1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Galili U, Swanson K. Gene sequences suggest inactivation of alpha-1,3-galactosyltransferase in catarrhines after the divergence of apes from monkeys. Proc Natl Acad Sci USA. 1991;88:7401–7404. doi: 10.1073/pnas.88.16.7401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Macher BA, Galili U. The Galalpha1,3Galbeta1,4GlcNAc-R (alpha-Gal) epitope: a carbohydrate of unique evolution and clinical relevance. Biochim Biophys Acta. 2008;1780:75–88. doi: 10.1016/j.bbagen.2007.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Galili U, Mandrell RE, Hamadeh RM, Shohet SB, Griffiss JM. Interaction between human natural anti-alpha-galactosyl immunoglobulin G and bacteria of the human flora. Infect Immun. 1988;56:1730–1737. doi: 10.1128/iai.56.7.1730-1737.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Avila JL, Rojas M, Galili U. Immunogenic Gal alpha 1-3Gal carbohydrate epitopes are present on pathogenic American Trypanosoma and Leishmania. J Immunol. 1989;142:2828–2834. [PubMed] [Google Scholar]
- 24.Almeida IC, Ferguson MA, Schenkman S, Travassos LR. Lytic anti-alpha-galactosyl antibodies from patients with chronic Chagas’ disease recognize novel O-linked oligosaccharides on mucin-like glycosyl-phosphatidylinositol-anchored glycoproteins of Trypanosoma cruzi. Biochem J. 1994;304(Pt 3):793–802. doi: 10.1042/bj3040793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Milani SR, Travassos LR. Anti-alpha-galactosyl antibodies in chagasic patients. Possible biological significance. Braz J Med Biol Res. 1988;21:1275–1286. [PubMed] [Google Scholar]
- 26.Bishop JR, Gagneux P. Evolution of carbohydrate antigens–microbial forces shaping host glycomes? Glycobiology. 2007;17:23R–34R. doi: 10.1093/glycob/cwm005. [DOI] [PubMed] [Google Scholar]
- 27.Doenz U, Nydegger UE, Kueng A, Carrel T, Mohacsi P. Anti-Galalpha1-3Gal IgM/IgG antibody levels in infants: do they have a clinical relevance in pediatric xenotransplantation? J Heart Lung Transplant. 2000;19:1108–1113. doi: 10.1016/S1053-2498(00)00196-0. [DOI] [PubMed] [Google Scholar]
- 28.Hamanova M, Chmelikova M, Nentwich I, Thon V, Lokaj J. Anti-Gal IgM, IgA and IgG natural antibodies in childhood. Immunol Lett. 2015;164:40–43. doi: 10.1016/j.imlet.2015.02.001. [DOI] [PubMed] [Google Scholar]
- 29.Cabrera-Rubio R, Mira-Pascual L, Mira A, Collado MC. Impact of mode of delivery on the milk microbiota composition of healthy women. J Dev Orig Health Dis. 2016;7:54–60. doi: 10.1017/S2040174415001397. [DOI] [PubMed] [Google Scholar]
- 30.Kumar H, et al. Distinct Patterns in Human Milk Microbiota and Fatty Acid Profiles Across Specific Geographic Locations. Front Microbiol. 2016;7:1619. doi: 10.3389/fmicb.2016.01619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Khodayar-Pardo P, Mira-Pascual L, Collado MC, Martinez-Costa C. Impact of lactation stage, gestational age and mode of delivery on breast milk microbiota. J Perinatol. 2014;34:599–605. doi: 10.1038/jp.2014.47. [DOI] [PubMed] [Google Scholar]
- 32.Gomez-Gallego C, et al. Breast Milk Polyamines and Microbiota Interactions: Impact of Mode of Delivery and Geographical Location. Ann Nutr Metab. 2017;70:184–190. doi: 10.1159/000457134. [DOI] [PubMed] [Google Scholar]
- 33.Parker AR, Allen S, Harding S. Concentration of anti-pneumococcal capsular polysaccharide IgM, IgG and IgA specific antibodies in adult blood donors. Pract Lab Med. 2016;5:1–5. doi: 10.1016/j.plabm.2016.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Takeuchi Y, et al. Sensitization of cells and retroviruses to human serum by (alpha 1-3) galactosyltransferase. Nature. 1996;379:85–88. doi: 10.1038/379085a0. [DOI] [PubMed] [Google Scholar]
- 35.Cunnington AJ, Riley EM. Suppression of vaccine responses by malaria: insignificant or overlooked? Expert Rev Vaccines. 2010;9:409–429. doi: 10.1586/erv.10.16. [DOI] [PubMed] [Google Scholar]
- 36.Timens W, Boes A, Rozeboom-Uiterwijk T, Poppema S. Immaturity of the human splenic marginal zone in infancy. Possible contribution to the deficient infant immune response. J Immunol. 1989;143:3200–3206. [PubMed] [Google Scholar]
- 37.Cerutti A, Cols M, Puga I. Marginal zone B cells: virtues of innate-like antibody-producing lymphocytes. Nat Rev Immunol. 2013;13:118–132. doi: 10.1038/nri3383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Urban BC, et al. Fatal Plasmodium falciparum malaria causes specific patterns of splenic architectural disorganization. Infect Immun. 2005;73:1986–1994. doi: 10.1128/IAI.73.4.1986-1994.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bockstal V, Geurts N, Magez S. Acute Disruption of Bone Marrow B Lymphopoiesis and Apoptosis of Transitional and Marginal Zone B Cells in the Spleen following a Blood-Stage Plasmodium chabaudi Infection in Mice. J Parasitol Res. 2011;2011:534697. doi: 10.1155/2011/534697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Requena P, et al. Pregnancy and malaria exposure are associated with changes in the B cell pool and in plasma eotaxin levels. J Immunol. 2014;193:2971–2983. doi: 10.4049/jimmunol.1401037. [DOI] [PubMed] [Google Scholar]
- 41.Ubillos I, et al. Chronic Exposure to Malaria Is Associated with Inhibitory and Activation Markers on Atypical Memory B Cells and Marginal Zone-Like B Cells. Front Immunol. 2017;8:966. doi: 10.3389/fimmu.2017.00966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Asito AS, et al. Suppression of circulating IgD + CD27+ memory B cells in infants living in a malaria-endemic region of Kenya. Malar J. 2011;10:362. doi: 10.1186/1475-2875-10-362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gomez-Perez GP, van Bruggen R, Grobusch MP, Dobano C. Plasmodium falciparum malaria and invasive bacterial co-infection in young African children: the dysfunctional spleen hypothesis. Malar J. 2014;13:335. doi: 10.1186/1475-2875-13-335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Edwards KM. Maternal antibodies and infant immune responses to vaccines. Vaccine. 2015;33:6469–6472. doi: 10.1016/j.vaccine.2015.07.085. [DOI] [PubMed] [Google Scholar]
- 45.Cabezas-Cruz A, et al. Effect of blood type on anti-alpha-Gal immunity and the incidence of infectious diseases. Exp Mol Med. 2017;49:e301. doi: 10.1038/emm.2016.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Aribot G, et al. Pattern of immunoglobulin isotype response to Plasmodium falciparum blood-stage antigens in individuals living in a holoendemic area of Senegal (Dielmo, west Africa) Am J Trop Med Hyg. 1996;54:449–457. doi: 10.4269/ajtmh.1996.54.449. [DOI] [PubMed] [Google Scholar]
- 47.Metzger WG, et al. Serum IgG3 to the Plasmodium falciparum merozoite surface protein 2 is strongly associated with a reduced prospective risk of malaria. Parasite Immunol. 2003;25:307–312. doi: 10.1046/j.1365-3024.2003.00636.x. [DOI] [PubMed] [Google Scholar]
- 48.Nebie I, et al. Humoral responses to Plasmodium falciparum blood-stage antigens and association with incidence of clinical malaria in children living in an area of seasonal malaria transmission in Burkina Faso, West Africa. Infect Immun. 2008;76:759–766. doi: 10.1128/IAI.01147-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Shi YP, et al. Natural immune response to the C-terminal 19-kilodalton domain of Plasmodium falciparum merozoite surface protein 1. Infect Immun. 1996;64:2716–2723. doi: 10.1128/iai.64.7.2716-2723.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Soe S, Theisen M, Roussilhon C, Aye KS, Druilhe P. Association between protection against clinical malaria and antibodies to merozoite surface antigens in an area of hyperendemicity in Myanmar: complementarity between responses to merozoite surface protein 3 and the 220-kilodalton glutamate-rich protein. Infect Immun. 2004;72:247–252. doi: 10.1128/IAI.72.1.247-252.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Boctor FN, Peter JB. IgG subclasses in human chronic schistosomiasis: over-production of schistosome-specific and non-specific IgG4. Clin Exp Immunol. 1990;82:574–578. doi: 10.1111/j.1365-2249.1990.tb05492.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Caulfield JP, Cianci CM, McDiarmid SS, Suyemitsu T, Schmid K. Ultrastructure, carbohydrate, and amino acid analysis of two preparations of the cercarial glycocalyx of Schistosoma mansoni. J Parasitol. 1987;73:514–522. doi: 10.2307/3282129. [DOI] [PubMed] [Google Scholar]
- 53.Hagan P, Blumenthal UJ, Dunn D, Simpson AJ, Wilkins HA. Human IgE, IgG4 and resistance to reinfection with Schistosoma haematobium. Nature. 1991;349:243–245. doi: 10.1038/349243a0. [DOI] [PubMed] [Google Scholar]
- 54.James LK, Till SJ. Potential Mechanisms for IgG4 Inhibition of Immediate Hypersensitivity Reactions. Curr Allergy Asthma Rep. 2016;16:23. doi: 10.1007/s11882-016-0600-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Santos AF, et al. IgG4 inhibits peanut-induced basophil and mast cell activation in peanut-tolerant children sensitized to peanut major allergens. J Allergy Clin Immunol. 2015;135:1249–1256. doi: 10.1016/j.jaci.2015.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Church J, Maitland K. Invasive bacterial co-infection in African children with Plasmodium falciparum malaria: a systematic review. BMC Med. 2014;12:31. doi: 10.1186/1741-7015-12-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bassat Q, et al. Severe malaria and concomitant bacteraemia in children admitted to a rural Mozambican hospital. Trop Med Int Health. 2009;14:1011–1019. doi: 10.1111/j.1365-3156.2009.02326.x. [DOI] [PubMed] [Google Scholar]
- 58.Aide P, et al. Four year immunogenicity of the RTS,S/AS02(A) malaria vaccine in Mozambican children during a phase IIb trial. Vaccine. 2011;29:6059–6067. doi: 10.1016/j.vaccine.2011.03.041. [DOI] [PubMed] [Google Scholar]
- 59.RTS, S.C.T.P Efficacy and safety of RTS,S/AS01 malaria vaccine with or without a booster dose in infants and children in Africa: final results of a phase 3, individually randomised, controlled trial. Lancet. 2015;386:31–45. doi: 10.1016/S0140-6736(15)60721-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bryan D, et al. The establishment of a WHO Reference Reagent for anti-malaria (Plasmodium falciparum) human serum. Malar J. 2017;16:314. doi: 10.1186/s12936-017-1958-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Vidal, M., Aguilar, M., Campo, J. J. & Dobaño, C. Development of quantitative suspension array assays for six immunoglobulin isotypes and subclasses to multiple Plasmodium falciparum antigens. Journal of Immunological Methods in press (2018). [DOI] [PMC free article] [PubMed]
- 62.Sanz, H. et al. drLumi: Multiplex Immunoassays Data Analysis. R package version 0.1.2. R package version 0.1.2 (2015).
- 63.Armbruster DA, Tillman MD, Hubbs LM. Limit of detection (LQD)/limit of quantitation (LOQ): comparison of the empirical and the statistical methods exemplified with GC-MS assays of abused drugs. Clin Chem. 1994;40:1233–1238. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analyzed during this study are included in this published article (and its Supplementary Information files).