Abstract
Behavioral interventions utilizing community health workers (CHWs) have demonstrated effectiveness in improving hypertension disparities in ethnic minority populations in the United States, but few have focused on Asian Americans. We assessed the efficacy of a CHW intervention to improve hypertension management among Filipino Americans with uncontrolled blood pressure (BP) in New York City (NYC) from 2011 to 2013. A total of 240 Filipino American individuals (112 in the treatment group and 128 in the control group) with uncontrolled hypertension (SBP ≥ 140 mmHg and/or DBP ≥ 90 mmHg) were recruited from community-based settings in NYC. Using a community-based participatory research approach, treatment participants received 4 educational workshops and 4 one-on-one visits with CHWs over a 4-month period, while control group participants received 1 educational workshop. Main outcome measures included BP control, changes in SBP and DBP, and changes in appointment keeping at 8-months. At 8-months, BP was controlled among a significantly greater percentage of treatment group participants (83.3%) compared to the control group (42.7%). The adjusted odds of controlled BP for the treatment group was 3.2 times the odds of the control group (P < 0.001). Both groups showed decreases in SBP and DBP, with greater decreases among treatment participants. Significant between-group differences were also demonstrated in adjusted analyses (P < 0.001). Individuals in the treatment group showed significant changes in appointment keeping. In conclusion, a community-based intervention delivered by CHWs can help improve BP and related factors among Filipino Americans with hypertension in NYC.
Keywords: Community-based participatory research, Community health workers, Minority health, Immigrants, Randomized controlled trial, Hypertension, Asian Americans
1. Introduction
Million Hearts© aims to prevent heart disease and stroke in the United States (US) by mobilizing public and private sectors around a core set of objectives, with particular attention on blood pressure (BP) control in minority populations (Department of Health and Human Services, n.d.). Disparities in hypertension among non-Hispanic blacks has been well-documented (Mensah et al., 2005; Ong et al., 2007; Centers for Disease Control and Prevention, 2005; Barnes et al., 2008). Research within Asian American communities is limited, yet a growing body of evidence indicates that compared to non-Hispanic whites, Filipino Americans experience a higher burden of hypertension (23.9–67%) (Barnes et al., 2008; Jose et al., 2013; Zhao et al., 2015; Bayog and Waters, 2017; Ma et al., 2017; Ye et al., 2009; Ursua et al., 2013; Ursua et al., 2014a) and lower rates of control (Zhao et al., 2015; Ursua et al., 2014a; Ea et al., 2018). Given the rapid population expansion of Filipino Americans in the US (38.9% increase between 2000 and 2010) (U.S. Census Bureau, 2012) as well as in regions such as New York City, (Federation AA, 2009) strategies to mitigate the burden of hypertension among Filipinos are warranted (Ursua et al., 2014b).
A cornerstone of Million Hearts© has been the dissemination of evidence-based, community-clinical linkage strategies, including the use of community health workers (CHWs). CHWs are frontline public health professionals with a close understanding of the communities they serve through shared racial/ethnic background, culture, language, socioeconomic status, and life experiences (American Public Health Association, 2014; Islam et al., 2015). They link community members to healthcare resources, provide culturally appropriate health coaching, and organize communities to improve physical and social well-being (USAID From the American People, n.d.). CHWs involved in chronic disease management provide social support and education on disease management (Adair et al., 2013; Katigbak et al., 2015; Lopez et al., 2017; Islam et al., 2018).
CHWs can improve hypertension control among low-income and minority populations (Katigbak et al., 2015; Islam et al., 2013a; Brownstein et al., 2005; Spencer et al., 2011; Islam et al., 2014; Islam et al., 2013b; Martinez et al., 2011; Brownstein et al., 2007). For example, CHW interventions have demonstrated significant improvements in BP control and self-management behaviors, including appointment keeping and antihypertensive medication adherence (Brownstein et al., 2007; Balcazar et al., 2009; Hess et al., 2007; Kim et al., 2016). To our knowledge, only our previous pilot work has examined the impact of a CHW intervention on hypertension control in the Filipino community; our findings showed a significant mean decrease in systolic blood pressure (SBP) (13.7 mmHg) and diastolic blood pressure (BP) (6.8 mmHg), weight (5.7 pounds), and body mass index (BMI) (1.1 kg/m2) (Ursua et al., 2014b). As Million Hearts© continues wide-scale dissemination efforts, models to improve BP control in populations like the Filipino community will be important in achieving goals set forth by the initiative.
Based on the encouraging findings from our pilot study, (Ursua et al., 2014b) we designed and conducted a study utilizing a community-based participatory research (CBPR) approach to test the effectiveness of a CHW intervention on hypertension-related outcomes among Filipino Americans with hypertension in New York City (NYC). We assess the efficacy of the intervention on BP control, SBP and DBP, and compliance to appointment keeping.
2. Methods
2.1. Study design
Project AsPIRE (Asian American Partnership in Research and Empowerment) is a CBPR study utilizing a randomized controlled trial design. Filipino American individuals with hypertension were assigned in a 1:1 ratio to a treatment or control group. The research protocol was approved by the NYU institutional review board, and all participants were provided with written informed consent before study enrollment. The study has been registered at ClinicalTrials.gov (Asian American Partnerships in Research and Empowerment (AsPIRE) NCT03100812).
2.2. Study setting and participants
Individuals self-identifying as Filipino (based on the screening question: “Are you of Filipino descent?”, aged 25–75, living in NYC, and hypertensive based either on the average value of the 2nd and 3rd BP measurements (≥140 mmHg for SBP or ≥ 90 mmHg for DBP if not diagnosed with diabetes, and ≥130 mmHg for SBP or ≥80 mmHg for DBP if diagnosed with diabetes) or on antihypertensive medication use (regardless of BP measurement) at screening were eligible for participation in the study. We excluded individuals who were on renal dialysis, had an acute or terminal illness or serious mental illness, had participated in a previous cardiovascular disease (CVD) study, or had a history of heart attack, stroke, or congestive heart failure. Eligibility age range was based on existing epidemiological data from previous studies examining hypertension among Filipino Americans (Stavig et al., 1988; Ryan et al., 2000; Grandinetti et al., 2005). We hoped to compare of our findings to the Filipino American population in other geographical areas. In addition, our coalition provided feedback on the increasing number of younger Filipino Americans diagnosed with hypertension. Recruitment occurred on a rolling basis from April 2011 through August 2012, and follow-up occurred 4-months and 8-months following baseline surveys.
2.3. Screening and randomization
In line with CBPR principles, we worked closely with our community partners to identify traditional and non-traditional venues and events frequented by Filipino community members. In addition, Census data was used to strategically sample in zip codes with large Filipino enclaves; faith, community, and business sites serving the Filipino community in those areas were engaged to host recruitment events. By using diverse sampling strategies, we minimized our risk of selection bias. Participants would also refer individuals in their personal network to meet with their CHWs to be screened for the study. At each recruitment event, staff or volunteers provided an explanation of the study and reviewed a consent form, confidentiality agreement, and liability release. After receiving study consent, a screening tool was administered by a licensed health professional. Three BP readings were taken five minutes apart on alternating arms. Height and weight measurements were taken. An exit interview was completed whereby trained staff provided health education related to the participants' risk factors, an explanation of the BP readings (the average of their 2nd and 3rd readings if BP was uncontrolled or untreated based on published guidelines), (National Heart Lung and Blood Institute, 2004) and an explanation of the study. Consent and screening took approximately 20 min.
A computer-generated randomization scheme was performed by the Project Coordinator, whereby individuals were placed into a predefined randomization table created by an outside Research Scientist. Individuals were stratified into a spreadsheet by age group (≤50 and >50) and sex to ensure equal distribution across the study arms; this stratification was based on the mean age of our previously sampled populations within this community, in order to obtain randomization groups of similar sizes.
2.4. Intervention
The CHW intervention was guided by the Health Belief Model (Champion and Skinner, 2008) and Social Support Theory (Lakey and Cohen, 2000). The intervention was delivered by four Filipino CHWs employed by the study's community partner, Kalusugan Coalition, Inc. All CHWs were Filipino immigrants, fluent in English, Tagalog, and Visayan languages. One CHW was male aged 39, and three were female (age range 50–65); all had at least a bachelor's degree. The majority of the CHWs lived in Queens, where the sample was recruited, and all had strong ties with the Filipino community. The CHWs participated in a 60-h core-competency training prior to the intervention start (Ruiz et al., 2012).
The study took place between March 2011 and April 2013. All participants met with the CHW for an orientation session; the CHW administered a baseline interview which included questions on demographics, risk factors, personal and family history of CVD, and baseline BP measurements. During the 4-month intervention, treatment group participants attended 4 monthly 90-min group or individual CHW-led health education sessions. The National Heart, Lung, and Blood Institute (NHLBI) Healthy Heart, Healthy Family curriculum, which has been culturally-adapted for the Filipino community, was utilized (National Heart Lung and Blood Institute, n.d.). The curriculum was modified to include 4 sessions: 1) heart disease and heart attack; 2) control of cholesterol and blood sugar; 3) physical activity, weight management, and BP control; and 4) nutrition and cigarette smoking. During each session, CHWs provided interactive health education to participants using adult learning techniques such as theatre of the oppressed, role playing activities, and other culturally appropriate games and activities. Sessions were predominantly conducted in English, as the majority of participants were fluent in English. However, phrases and idioms in specific languages were often used or incorporated by CHWs into session materials and health coaching efforts. Between sessions, CHWs followed up with participants through monthly one-on-one visits at convenient locations, including their homes, place of employment, or community-based settings. During these visits, CHWs developed individual goal-setting plans with participants, helping to link and negotiate participants' access to a primary care physician, providing social support, and assuring adherence to appointment keeping through accompaniment to the participants' physician appointments. The CHWs also made any necessary referrals to other services, such as mental health services or tobacco cessation. CHWs followed up with participants by phone as needed over the course of the intervention. All interactions with the study participants were documented in CHW progress notes and call logs to ensure fidelity to the study protocol, and the CHWs completed checklists that estimated the amount of time spent on key curriculum components.
Individuals in the control group attended only the first health education session, which was identical to the first session received by treatment group participants. Control group participants also received a wallet card with clinical readings and a referral to a primary care physician when necessary. No additional in-person or phone sessions were conducted with control group participants.
2.5. Measures
Throughout the intervention, BP was measured by CHWs using an Omron HEM-712C automatic BP monitor. Three BP measurements were taken after participants were seated for 5 min, each at least 5 min apart; the 2nd and 3rd measurements were averaged. Measurements were taken at baseline, 4-months, and 8-months. BP control was defined as BP <140/90 mmHg for non-diabetics, and BP <130/80 mm HG for individuals with diabetes (National Heart Lung and Blood Institute, 2004). Joint National Committee (JNC) 7 guidelines were used given the timeframe in which the intervention was implemented. Compliance to appointment keeping was measured using two questions adapted from the Hill-Bone Compliance to High Blood Pressure Therapy Scale (Kim et al., 2000) and two questions related to transportation issues. The mean score was calculated; scores ranged from 1 to 4 with 4 as the greatest compliance. We measured mean change in SBP and DBP and scale measurements between baseline and follow-up, as well as the proportion with controlled BP at each time-point.
Demographic variables, including sex, age, education, nativity, and years in US, were assessed at screening or baseline. Because 97% of participants spoke English well or very well, English fluency was not included in analyses. Approximately 65% of respondents did not report annual household income, thus income was not included in analysis. Additional variables collected at each time-point (screening/baseline, 4-month follow-up, and 8-month follow-up) included weight, BMI, current smoking, insurance, and having a regular health care professional.
2.6. Statistical analysis
Initial power calculations were based on BP control among participants in the pilot study phase, which observed that BP was under control for approximately 80% of participants at 4-month follow-up (Ursua et al., 2014b). Based on these results, we calculated our sample size using 80% power, 95% confidence level, and a 20% difference in BP between the two groups at 8-month follow-up. We estimated 91 participants per arm to allow detection of this difference, for a total of 182 total participants. Because our final sample included 78 treatment group participants and 103 control group participants with complete data at 8-month follow-up, we performed a new power analysis using 80% power, 95% confidence level, and a 30% difference between the two groups (50% under control for the control group and 80% under control for the treatment group). Our new analysis estimated 45 participants per arm, for a total of 90 participants.
Descriptive statistics (percents and means) compared demographics, self-reported health measures, and clinical indicators between groups at baseline using Pearson χ2 tests for categorical variables and the two-tailed Student t-test for continuous variables. To test within-group differences between baseline and 8-month follow-up, two-tailed paired t-tests and NcNemar tests were used for each outcome measure. To assess change across groups for each continuous outcome, we ran generalized estimating equation (GEE) models for repeated measures over time using proc. genmod, adjusting for study arm, time-point, and the study arm x time-point. Adjusted models included the following additional variables from baseline: age, sex, education, nativity, and years in the US; as well as the following time-varying variables: weight, current smoking, insurance, PCP, weekly recommended physical activity, adding salt to food after serving, and drinking alcohol. The study arm x time-point interaction tests the intervention effect, and the beta coefficients computed by GEE represent the change in slope both within the two study arms over time. For BP control, we ran GEE models using a binomial distribution; odds ratios were produced. An adjusted model included the same additional variables as in the continuous outcomes models. SAS version 9.4 (SAS Institute, Cary, NC) was used for all analyses.
3. Results
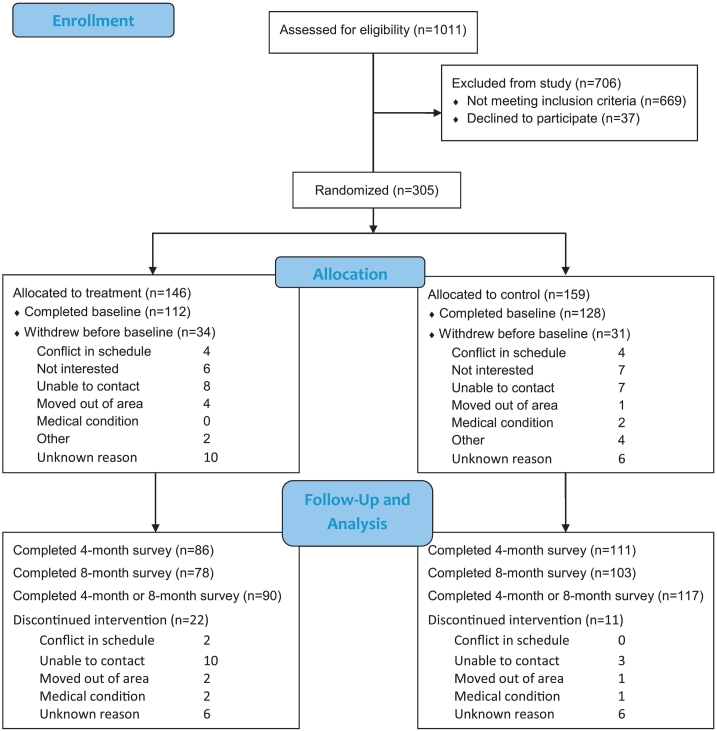
During the recruitment period, 1011 individuals were assessed for study eligibility. Sixty-six percent did not meet eligibility criteria and 4% refused to participate, mainly due to schedule conflicts or lack of interest (Fig. 1). Of 305 randomized participants, 79% completed the baseline survey. When comparing those who did and did not complete the baseline survey, no differences were found for sex, age, and employment for treatment or control groups. However, in the treatment group, participants completing baseline were more likely than participants not completing baseline to have public insurance, while participants not completing baseline were more likely to have private insurance (P = 0.012); and participants completing baseline were more likely than participants not completing baseline to have a previous diagnosis of hypertension (P = 0.010).
Fig. 1.
Study participant recruitment and retention for Project AsPIRE, 2011–2013.
A total of 90 individuals completed baseline and at least one follow-up survey in the treatment group (attrition rate = 19.6%), and a total of 117 individuals completed baseline surveys and at least one follow-up survey in the control group (attrition rate = 8.6%), see Fig. 1. Dropping out of the study was not significantly associated with age, gender, education, years lived in the US, marital status, previous diagnosis of hypertension, having a regular health provider, or health insurance for either group. When comparing those who dropped out of the intervention by study group, there was no significant difference in hypertension severity or diabetes diagnosis (comorbidity). Data available upon request.
3.1. Participant characteristics
The majority of participants were women (64.9%), and mean age was 53.9 years (SD = 10.4 years). The majority of individuals (99.6%) were born outside the US, and average residence in the US was 10.3 years (SD = 9.1 years). No significant differences were seen between study groups. Education was high, which reflects the education status of the Filipino population; according to 2016 American Community Survey data, 37.0% of individuals living in NYC have a college education, compared to 63.7% of Filipino Americans living in NYC (U.S. Census Bureau, 2016). See Table 1.
Table 1.
Baseline participant characteristics, Project AsPIRE, NYC, 2011–2013, n (%).
| Intervention (n = 112) | Control (n = 128) | P-value | |
|---|---|---|---|
| Age in years, mean ± SD | 53.9 (10.6) | 53.8 (10.3) | 0.953 |
| Age > 50 years | 77 (48.4) | 82 (51.6) | 0.444 |
| Sex | 0.208 | ||
| Women | 68 (60.7) | 87 (68.5) | |
| Men | 44 (39.3) | 40 (31.5) | |
| College graduate | 78 (73.6) | 102 (82.3) | 0.112 |
| Years in US, mean ± SD | 11.3 (9.4) | 9.4 (7.7) | 0.132 |
| Speaks English very well or well | 106 (95.5) | 125 (98.4) | 0.182 |
| Weight, lbs., mean ± SD | 146.2 (24.9) | 146.7 (23.2) | 0.873 |
| BMI, kg/m2, mean ± SD | 25.6 (3.2) | 25.9 (3.3) | 0.396 |
| Diabetes diagnosis | 31 (27.7) | 33 (25.8) | 0.740 |
| Current cigarette smoker | 8 (7.3) | 4 (3.2) | 0.157 |
| Health insurance | 41 (36.6) | 43 (34.4) | 0.723 |
| Regular doctor or health professional | 70 (64.2) | 75 (60.0) | 0.507 |
| Taking hypertension medication(s) | 64 (58.7) | 66 (52.8) | 0.364 |
| Adds salt to food after it is served | 30 (27.5) | 24 (19.2) | 0.124 |
| Alcohol Consumption | 0.628 | ||
| Rarely (on special occasions) | 14 (13.1) | 23 (19.5) | |
| Occasionally (Once a month) | 16 (15.0) | 18 (15.3) | |
| Once a week or more | 7 (6.5) | 8 (6.8) | |
| Does not drink alcohol | 70 (65.4) | 69 (58.5) | |
| Weekly Recommended Physical Activity | 0.422 | ||
| Does not exercise | 25 (22.5) | 20 (16.1) | |
| Less than recommended | 5 (4.5) | 5 (4.0) | |
| At least recommended | 81 (73.0) | 99 (79.8) | |
| Systolic BP, mean ± SD | 145.3 (15.2) | 143.6 (13.5) | 0.343 |
| Diastolic BP, mean ± SD | 83.3 (10.3) | 83.6 (9.4) | 0.822 |
| Controlled BP | 29 (25.9) | 28 (21.9) | 0.466 |
| Controlled BP (using diabetic definition) | 23 (20.5) | 20 (15.6) | 0.322 |
| Appointment keeping, mean ± SD | 3.6 (0.5) | 3.6 (0.5) | 0.867 |
Abbreviations: US, United States; BMI, body mass index; BP, blood pressure.
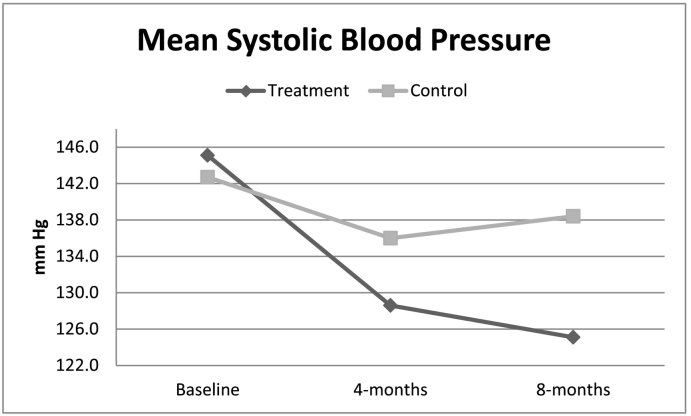
3.2. Blood pressure control
All primary study outcomes are detailed in Table 2. Mean (SD) SBP decreased significantly (−20.0 mmHg) in the treatment group from 145.1 (14.4) at baseline to 125.1 (12.8) at 8-months. Mean (SD) SBP in the control group decreased significantly (−4.3 mmHg) from 142.7 (13.2) at baseline to 138.4 (12.4) at 8-months (Fig. 2). GEE models present the difference in slope both within and between the study groups over time; the difference in SBP change between the two groups was 15.7 mmHg. Greater improvement in SBP was seen in the treatment group compared to the control group in unadjusted analysis using all available data; the difference in slopes was −7.7 (95% CI, −9.7, −5.7, P < 0.001) in unadjusted analysis. The intervention effect was seen after adjustment for all covariates, with a differences in slopes of −6.2 (P < 0.001).
Table 2.
Changes in outcomes at baseline, 4-month and 8-month follow-up for treatment and control groups, Project AsPIRE, NYC, 2011–2013.
| Treatment group, mean (SD) |
Control group, mean (SD) |
Intervention effect |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 4 Months | 8 Months | P-value BL-8 M | Baseline | 4 Months | 8 Months | P-value BL-8 M | Unadjusted | p-Value | Adjusteda | P-value | |
| Systolic BP, mm Hg | 145.1 (14.4) | 128.6 (15.0) | 125.1 (12.8) | <0.001 | 142.7 (13.2) | 136.0 (13.9) | 138.4 (12.4) | <0.001 | −7.7 (−9.7, −5.7) | <0.001 | −6.2 (−8.4, −4.0) | <0.001 |
| Diastolic BP, mm Hg | 84.5 (10.1) | 77.0 (8.6) | 77.1 (7.9) | <0.001 | 82.7 (9.5) | 80.7 (8.6) | 82.5 (7.4) | 0.829 | −2.8 (−4.1, −1.5) | <0.001 | −2.8 (−4.3, −1.4) | <0.001 |
| Controlled BP (diabetic definition), n (%) | 15 (19.2) | 54 (73.0) | 65 (83.3) | <0.001 | 18 (17.5) | 51 (50.5) | 44 (42.7) | <0.001 | 3.0 (2.0, 4.6) | <0.001 | 3.2 (1.9, 5.4) | <0.001 |
| Appointment keeping scale, 1–4, 4 = greatest compliance | 3.6 (0.5) | 3.8 (0.3) | 3.8 (0.3) | 0.004 | 3.6 (0.4) | 3.7 (0.4) | 3.7 (0.3) | 0.121 | 0.0 (−0.0, 0.1) | 0.266 | 0.01 (−0.1, 0.1) | 0.582 |
Abbreviations: BP, blood pressure.
Intervention effect reports the beta coefficient of the interaction of time point*intervention group for linear regression models. Odds ratios for study arm are reported for logistic models.
Sample sizes for BP outcomes: Control BL = 103, 4-mo = 101, 8-mo = 103; Intervention BL = 78, 4-mo = 74, 8-mo = 78.
Sample sizes for medication adherence: Control BL = 52, 4-mo = 46, 8-mo = 52; Intervention BL = 39, 4-mo = 37, 8-mo = 39.
Sample sizes for appointment keeping: Control BL = 73, 4-mo = 67, 8-mo = 73; Intervention BL = 55, 4-mo = 50, 8-mo = 55.
Adjusted for age, sex, education, nativity, years in US, time-varying: weightbody mass index, current smoking, insurance, PCP, recommended weekly physical activity, adding salt to food after serving, alcohol use.
Fig. 2.
Mean systolic blood pressure over time by group, Project AsPIRE, 2011–2013.
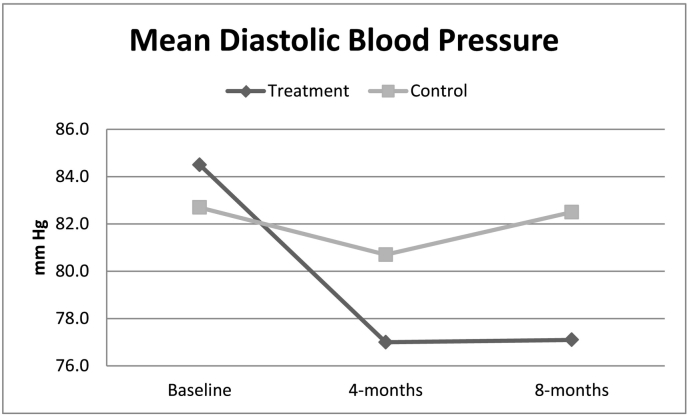
Mean (SD) DBP decreased significantly (−7.4 mmHg) in the treatment group from 84.5 (10.1) at baseline to 77.1 (7.9) at 8-months. Mean (SD) DBP did not decrease significantly in the control group (−0.2 mmHg) (Fig. 3). The difference in DBP change between the two groups was −7.2 mmHg. Greater improvement in DBP was seen in the treatment group compared to the control group in unadjusted analysis using all available data; the difference in slopes was −2.8 (95% CI, −4.1, −1.5, P < 0.001). The intervention effect was seen after adjustment for all covariates, with a difference in slopes of −2.8 (P < 0.001).
Fig. 3.
Mean diastolic blood pressure over time by group, Project AsPIRE, 2011–2013.
BP at 8-months was controlled among a significantly greater percent of individuals in the treatment group (83.3%) than in the control group (42.7%) (Table 2). The odds of controlled BP from baseline to 8-months for the treatment group was 3.0 times the odds of the control group in unadjusted analysis (95% CI, 2.0, 4.6, P < 0.001); the odds in adjusted analysis was 3.2 (95% CI, 1.9, 5.4, P < 0.001). At 8-month follow-up, 1.3% of treatment group participants were considered hypertension stage II and 9.0% hypertension stage I according to JNC-7 guidelines, (National Heart Lung and Blood Institute, 2004) compared to 4.9% and 46.6% of the control group, respectively (data not presented).
3.3. Appointment keeping
Among individuals completing the appointment keeping scale at baseline and 8-months, the treatment group saw a significant improvement in appointment keeping (3.6 to 3.8, P = 0.004), while a significant change was not seen for the control group. There was no evidence of an intervention effect on change in appointment keeping.
4. Discussion
In this population of Filipino Americans with hypertension, participants in both groups experienced improvements in SBP and DBP, although treatment participants were significantly more likely to experience SBP and DBP improvements after adjustments for other factors. Participants in the treatment group were more than twice as likely to report BP control at study follow-up, even after adjustment for other factors, demonstrating strong efficacy associated with the CHW intervention. The adjusted intervention effect was statistically significant for changes in controlled BP, SBP, and DBP.
To our knowledge, this represents the first community-based research study utilizing a randomized controlled study design to improve BP control in the Filipino community. This strong design is a key strength of our study, as prior studies on CHW efficacy have suffered from lack of rigor. The intervention effect on BP control is similar to or higher than that of other CHW interventions conducted in African American and Hispanic communities, (Hill et al., 2003; Levine et al., 2003; Morisky et al., 2002) suggesting that the CHW model may be a particularly important community-clinical linkage model to improve BP control in the Filipino hypertensive population. Findings that individuals retained in the intervention were more likely to be uninsured, younger, and better educated suggests that CHW effectiveness in BP control may be particularly salient for low socio-economic status populations that are disconnected from the healthcare system, aligning with the randomized controlled trial design.
Although the intervention effect on BP control and decreases in SBP and DBP were significant, control group participants also saw positive changes in BP outcomes. There was no difference in BP control outcomes or mean values of SBP and DBP between individuals in the control group who had contact with treatment group participants and those who did not. Thus, we surmise that the initial interaction of participants with study personnel at health screening events served as means of connecting control group participants' care; the control group's participation in the first session increased self-management of BP. Further, BP assessments received through screening control group participants at 4- and 8-month follow-ups may have prompted these individuals to be more cognizant of their BP management.
However, the intervention did not appear to have a significant effect on appointment-keeping. Our program was community-based, and CHWs were not integrated into clinical settings and did not have protocolized interactions with healthcare providers. Improvements in appointment keeping may be more driven by health systems and provider level factors; future research should test whether integration of CHWs with primary care teams can enhance these factors.
At the end of the intervention, treatment participants completed an evaluation of CHW attributes, functions and socio-cultural congruence. Individuals from the AsPIRE intervention rated their CHWs very highly, in terms of trust, respect, roles, and functions. For example, 83.5% of treatment participants reported that they trusted their CHW “a lot” when discussing health concerns, and 97.9% agreed or strongly agreed that the CHW helped to change their behaviors. Our previous work has demonstrated interpersonal attributes, along with CHWs roles in serving as a bridge to health and non-health resources and providing accessibility beyond health providers are highly valued to community members (Katigbak et al., 2015; Islam et al., 2017).
There were limitations of note. First, data regarding appointment keeping was self-reported and subject to bias. Second, differences in health insurance and a previous diagnosis of hypertension (non-significant) were found for the treatment group between individuals completing the baseline and withdrawing before the baseline, but not for the control group, suggesting that individuals with public insurance or previous knowledge of hypertension were more willing to participate in the intervention. Third, the study followed participants for eight months; thus, we cannot assess efficacy of the intervention on long-term BP control. Fourth, CHWs were unblinded to the randomization assignment. Finally, our findings may not be generalizable to other populations and settings, as this was a primarily foreign-born Filpino sample in NYC, also creating potential selection bias. However, the Filipino population in NYC is largely foreign-born (74% in 2016) (U.S. Census Bureau, 2016); given that our curriculum and protocols were adapted from NHLBI programs, we anticipate that the model can be replicated for other communities. Further, the trial design enhances confidence that the efficacy of the intervention can be attributed to CHWs efforts rather than external factors.
Our study findings provide compelling evidence for the promotion of CHW models in minority communities as a means of increasing BP control and reducing CVD disparities. Given that there has been significant policy and research discussion regarding the integration of CHWs into healthcare systems and opportunities for financing mechanisms to support sustainability of the model as the nation shifts towards value-based care, future analysis of CHW interventions should include an evaluation of cost-effectiveness and assessment of implementation factors that influence sustainability and scalability across different settings, including the adoption and maintenance of CHW efforts (Islam et al., 2015; Lopez et al., 2018; Islam et al., 2016). As efforts like Million Hearts© continue to advance community-clinical linkage models to improve CVD outcomes, programs and research that employ CHWs can play an important role in advancing population health equity.
Acknowledgments
Acknowledgments
This publication would not have been possible without the support of the staff, members, and leadership of the Kalusugan Coalition, Inc., who gave their time and expertise in designing and implementing the project. The authors would also like to thank the community health workers from the pilot round, Romerico Foz, Yves Nibungco, Hanalei Ramos, and Henry Soliveres. The authors are especially grateful to all the community members who participated in the study. We also thank Dr. Mariano Rey for the guidance, support, and leadership he provided to the study, and Bahman Tabaei and Stella Yi for statistical support.
This publication was made possible by grants U58DP005621 and U48DP005008 (Centers for Disease Control and Prevention), grants P60 MD000538 and R24MD001786 (NIH National Institute on Minority Health and Health Disparities), grant 1R01DK110048-01A1 (NIH National Institute of Diabetes and Digestive and Kidney Diseases), and grant UL1 TR001445 (National Center for Advancing Translational Sciences). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health and other supporters.
Conflict of interest
None.
Conflict of interest summary
To the best of our knowledge, no conflict of interest, financial or other, exists.
References
- Adair R., Wholey D.R., Christianson J., White K.M., Britt H., Lee S. Improving chronic disease care by adding laypersons to the primary care team: a parallel randomized trial. Ann. Intern. Med. 2013;159(3):176–184. doi: 10.7326/0003-4819-159-3-201308060-00007. [DOI] [PubMed] [Google Scholar]
- American Public Health Association Community Health Workers. 2014. https://www.apha.org/apha-communities/member-sections/community-health-workers [DOI] [PubMed]
- Balcazar H.G., Byrd T.L., Ortiz M., Tondapu S.R., Chavez M. A randomized community intervention to improve hypertension control among Mexican Americans: using the promotoras de salud community outreach model. J. Health Care Poor Underserved. 2009;20(4):1079–1094. doi: 10.1353/hpu.0.0209. [DOI] [PubMed] [Google Scholar]
- Barnes P.M., Adams P.F., Powell-Griner E. Health characteristics of the Asian adult population: United States, 2004–2006. Adv. Data. 2008;394:1–22. [PubMed] [Google Scholar]
- Bayog M.L., Waters C.M. Cardiometabolic risks, lifestyle health behaviors and heart disease in Filipino Americans. Eur. J. Cardiovasc. Nurs. 2017;16(6):522–529. doi: 10.1177/1474515117697886. [DOI] [PubMed] [Google Scholar]
- Brownstein J.N., Bone L.R., Dennison C.R., Hill M.N., Kim M.T., Levine D.M. Community health workers as interventionists in the prevention and control of heart disease and stroke. Am. J. Prev. Med. 2005;29(5 Suppl. 1):128–133. doi: 10.1016/j.amepre.2005.07.024. [DOI] [PubMed] [Google Scholar]
- Brownstein J.N., Chowdhury F.M., Norris S.L. Effectiveness of community health workers in the care of people with hypertension. Am. J. Prev. Med. 2007;32(5):435–447. doi: 10.1016/j.amepre.2007.01.011. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Racial/ethnic disparities in prevalence, treatment, and control of hypertension—United States, 1999–2002. MMWR Morb. Mortal. Wkly Rep. 2005;54(1):7–9. [PubMed] [Google Scholar]
- Champion V., Skinner C. Health Behavior and Health Education: Theory Research and Practice. 4th ed. Jossey-Bass; San Francisco, CA: 2008. The health belief model; pp. 45–66. [Google Scholar]
- Department of Health and Human Services Million Hearts. https://millionhearts.hhs.gov/
- Ea E.E., Colbert A., Turk M., Vaughan Dickson V. Self-care among Filipinos in the United States who have hypertension. Appl. Nurs. Res. 2018;39:71–76. doi: 10.1016/j.apnr.2017.11.002. [DOI] [PubMed] [Google Scholar]
- Federation AA Profile of New York City's Filipino Americans: 2005–2007. 2009. http://www.aafny.org/cic/briefs/filipino2009.pdf
- Grandinetti A., Chang H.K., Theriault A., Mor J. Metabolic syndrome in a multiethnic population in rural Hawaii. Ethn. Dis. 2005;15(2):233–237. [PubMed] [Google Scholar]
- Hess P.L., Reingold J.S., Jones J. Barbershops as hypertension detection, referral, and follow-up centers for black men. Hypertension. 2007;49(5):1040–1046. doi: 10.1161/HYPERTENSIONAHA.106.080432. [DOI] [PubMed] [Google Scholar]
- Hill M.N., Han H.R., Dennison C.R. Hypertension care and control in underserved urban African American men: behavioral and physiologic outcomes at 36 months. Am. J. Hypertens. 2003;16(11 Pt 1):906–913. doi: 10.1016/s0895-7061(03)01034-3. [DOI] [PubMed] [Google Scholar]
- Islam N.S., Wyatt L.C., Patel S.D. Evaluation of a community health worker pilot intervention to improve diabetes management in Bangladeshi immigrants with type 2 diabetes in New York City. Diabetes Educ. 2013;39(4):478–493. doi: 10.1177/0145721713491438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Islam N.S., Zanowiak J.M., Wyatt L.C. A randomized-controlled, pilot intervention on diabetes prevention and healthy lifestyles in the New York City Korean community. J. Community Health. 2013;38(6):1030–1041. doi: 10.1007/s10900-013-9711-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Islam N., Riley L., Wyatt L. Protocol for the DREAM project (diabetes research, education, and action for minorities): a randomized trial of a community health worker intervention to improve diabetic management and control among Bangladeshi adults in NYC. BMC Public Health. 2014;14:177. doi: 10.1186/1471-2458-14-177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Islam N., Nadkarni S.K., Zahn D., Skillman M., Kwon S.C., Trinh-Shevrin C. Integrating community health workers within patient protection and affordable care act implementation. J. Public Health Manag. Pract. 2015;21(1):42–50. doi: 10.1097/PHH.0000000000000084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Islam N., Nadkarni S.K., Peretz P. Integration of Community Health Workers into Healthcare Systems: The Time for New York State is Now! 2016. http://www.med.nyu.edu/prevention-research/sites/default/files/prevention-research2/NYU-CUNY%20PRC%20-%20Integration%20of%20CHWs%20into%20Primary%20Care%20Systems.pdf (October)
- Islam N., Shapiro E., Wyatt L. Evaluating community health workers' attributes, roles, and pathways of action in immigrant communities. Prev. Med. 2017;103:1–7. doi: 10.1016/j.ypmed.2017.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Islam N.S., Wyatt L.C., Taher M. A Culturally Tailored Community Health Worker Intervention Leads to Improvement in Patient-Centered Outcomes for Immigrant Patients With Type 2 Diabetes. Clin. Diabetes. 2018;36(2):100–111. doi: 10.2337/cd17-0068. https://www.ncbi.nlm.nih.gov/pubmed/29686448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jose P., Zhao B.N., Baek M., Chung S., Fortmann S., Palaniappan L. Variation in hypertension prevalence among Asian American subgroups: results from Pacs (Pan Asian Cohort Study) J. Am. Coll. Cardiol. 2013;61(10):E1349. [Google Scholar]
- Katigbak C., Van Devanter N., Islam N., Trinh-Shevrin C. Partners in health: a conceptual framework for the role of community health workers in facilitating patients' adoption of healthy behaviors. Am. J. Public Health. 2015;105(5):872–880. doi: 10.2105/AJPH.2014.302411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim M.T., Hill M.N., Bone L.R., Levine D.M. Development and testing of the hill-bone compliance to high blood pressure therapy scale. Prog. Cardiovasc. Nurs. 2000;15(3):90–96. doi: 10.1111/j.1751-7117.2000.tb00211.x. [DOI] [PubMed] [Google Scholar]
- Kim K., Choi J.S., Choi E. Effects of community-based health worker interventions to improve chronic disease management and care among vulnerable populations: a systematic review. Am. J. Public Health. 2016;106(4) doi: 10.2105/AJPH.2015.302987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lakey B., Cohen S. Social support theory and measurement. In: Cohen S., Underwood L., Gottlieb B., editors. Measuring and Intervening in Social Support. Oxford University Press; New York: 2000. [Google Scholar]
- Levine D.M., Bone L.R., Hill M.N. The effectiveness of a community/academic health center partnership in decreasing the level of blood pressure in an urban African-American population. Ethn. Dis. 2003;13(3):354–361. [PubMed] [Google Scholar]
- Lopez P.M., Zanowiak J., Goldfeld K. Protocol for project IMPACT (improving millions hearts for provider and community transformation): a quasi-experimental evaluation of an integrated electronic health record and community health worker intervention study to improve hypertension management among south Asian patients. BMC Health Serv. Res. 2017;17(1):810. doi: 10.1186/s12913-017-2767-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez P., Zanowiak J., Beane S., Islam N. A quasi-experimental evaluation of a community-clinical linkage study to improve hypertension management among South Asian Patients. BMC Health Serv. Res. 2018 doi: 10.1186/s12913-017-2767-1. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma G.X., Lee M., Bhimla A. Risk assessment and prevention of hypertension in Filipino Americans. J. Community Health. 2017;42(4):797–805. doi: 10.1007/s10900-017-0320-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez J., Ro M., Villa N.W., Powell W., Knickman J.R. Transforming the delivery of care in the post-health reform era: what role will community health workers play? Am. J. Public Health. 2011;101(12):e1–5. doi: 10.2105/AJPH.2011.300335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mensah G.A., Mokdad A.H., Ford E.S., Greenlund K.J., Croft J.B. State of disparities in cardiovascular health in the United States. Circulation. 2005;111(10):1233–1241. doi: 10.1161/01.CIR.0000158136.76824.04. [DOI] [PubMed] [Google Scholar]
- Morisky D.E., Lees N.B., Sharif B.A., Liu K.Y., Ward H.J. Reducing disparities in hypertension control: a community-based hypertension control project (CHIP) for an ethnically diverse population. Health Promot. Pract. 2002;3(2):264–275. [Google Scholar]
- National Heart Lung and Blood Institute . 2004. JNC 7 Complete Report: The Science Behind the New Guidelines. [Google Scholar]
- National Heart Lung and Blood Institute Healthy Heart, Healthy Family: A Community Health Worker's Manual for the Filipino Community. http://www.nhlbi.nih.gov/health-pro/resources/heart/filipino-health-manual/intro
- Ong K.L., Cheung B.M., Man Y.B., Lau C.P., Lam K.S. Prevalence, awareness, treatment, and control of hypertension among United States adults 1999-2004. Hypertension. 2007;49(1):69–75. doi: 10.1161/01.HYP.0000252676.46043.18. [DOI] [PubMed] [Google Scholar]
- Ruiz Y., Matos S., Kapadia S. Lessons learned from a community-academic initiative: the development of a core competency-based training for community-academic initiative community health workers. Am. J. Public Health. 2012;102(12):2372–2379. doi: 10.2105/AJPH.2011.300429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan C., Shaw R., Pliam M. Coronary heart disease in Filipino and Filipino-American patients: prevalence of risk factors and outcomes of treatment. J. Invasive Cardiol. 2000;12(3):134–139. [PubMed] [Google Scholar]
- Spencer M.S., Rosland A.M., Kieffer E.C. Effectiveness of a community health worker intervention among African American and Latino adults with type 2 diabetes: a randomized controlled trial. Am. J. Public Health. 2011;101(12):2253–2260. doi: 10.2105/AJPH.2010.300106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stavig G.R., Igra A., Leonard A.R. Hypertension and related health issues among Asians and Pacific Islanders in California. Public Health Rep. 1988;103(1):28–37. [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau The Asian Population: 2010. 2012. https://www.census.gov/prod/cen2010/briefs/c2010br-11.pdf
- U.S. Census Bureau Selected Population Profile in the United States, 2016 American Community Survey 1-Year Estimates. 2016. https://factfinder.census.gov/
- Ursua R.A., Islam N.S., Aguilar D.E. Predictors of hypertension among Filipino immigrants in the Northeast US. J. Community Health. 2013;38(5):847–855. doi: 10.1007/s10900-013-9689-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ursua R., Aguilar D., Wyatt L. Awareness, treatment and control of hypertension among Filipino immigrants. J. Gen. Intern. Med. 2014;29(3):455–462. doi: 10.1007/s11606-013-2629-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ursua R.A., Aguilar D.E., Wyatt L.C. A community health worker intervention to improve management of hypertension among Filipino Americans in New York and New Jersey: a pilot study. Ethn. Dis. 2014;24(1):67–76. [PMC free article] [PubMed] [Google Scholar]
- USAID From the American People Community and Formal Health System Support for Enhanced Community Health Worker Performance. http://www.coregroup.org/storage/Program_Learning/Community_Health_Workers/chw%20evidence%20summit%20final%20report-19dec2012.pdf
- Ye J., Rust G., Baltrus P., Daniels E. Cardiovascular risk factors among Asian Americans: results from a National Health Survey. Ann. Epidemiol. 2009;19(10):718–723. doi: 10.1016/j.annepidem.2009.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao B., Jose P.O., Pu J. Racial/ethnic differences in hypertension prevalence, treatment, and control for outpatients in northern California 2010-2012. Am. J. Hypertens. 2015;28(5):631–639. doi: 10.1093/ajh/hpu189. [DOI] [PMC free article] [PubMed] [Google Scholar]