Abstract
Pneumonia is an important cause of morbidity and mortality. Since 2014, the Health Insurance Review and Assessment Service (HIRA) has assessed the overall quality of care among hospitalized adult patients with community-acquired pneumonia (CAP) provided by all medical institutions in Korea. A committee of the Korea Academy of Tuberculosis and Respiratory Diseases developed the hospital inpatient quality measures set for CAP consisting of eight core measures and five monitoring measures. The composite measure score was calculated. The medical records of hospitalized adult patients ages 18 years or more with CAP from October to December 2014 were evaluated. The data of 523 hospitals (42 tertiary hospitals [8.0%], 256 general hospitals [49%], and 225 hospitals [43.0%]) and 15,432 cases (tertiary hospitals, 1,673 cases [10.8%]; general hospitals, 8,803 cases [57.1%]; hospitals, 4,956 cases [32.1%]) were analyzed. We found large variations among institutions in terms of performance of care measures for CAP. For the composite measure score, the mean value was 66.7 (tertiary hospitals, 98.5; general hospitals, 79.2; hospitals, 43.8). Despite significant differences in measure scores between tertiary, general hospitals and hospitals, no significant differences were found in mortality between hospitals. Further studies are needed to determine the care measures appropriate for CAP.
Keywords: Quality of Care, Pneumonia, Quality Improvement
Introduction
Community-acquired pneumonia (CAP) is one of the most common diseases worldwide. Pneumonia is also an important cause of morbidity and mortality, particularly in children and the elderly. According to the World Health Organization, pneumonia is the major cause of death in children, accounting for 16% of all deaths in children under 5 years of age in 20151. In the United States, pneumonia is the sixth most common cause of death. Two to three million cases of CAP per year resulted in 10 million visits to a physician, 500,000 hospitalizations, and 45,000 deaths2.
In Korea, pneumonia is the fifth ranked cause of death, with a mortality rate of 23.7/100,000 person years (PY) in 20143. Moreover, the mortality rate was 74 times higher (177.5/100,000 PY) in patients older than 65 years of age compared to those younger than 65 years (2.4/100,000 PY). As the aged population increases, the number of patients treated for pneumonia is also increasing along with a rapid rise in medical costs in Korea. Assessing the quality of care for patients with pneumonia is necessary because quality measure is related to patient outcomes. Assessment of pneumonia severity using oxygenation assessment, Pneumonia Severity Index (PSI) and CURB-65 enable the clinicians to initiate early and appropriate treatment including oxygen therapy4. Microbiologic testing is required because it can lead to a change in antibiotics therapy in up to 40% of patients with severe pneumonia5. Timely antibiotics administration is associated with lower risk of mortality6,7,8. Smoking cessation and pneumococcal vaccination are effective in preventing pneumonia9,10,11. The Health Insurance Review and Assessment Service (HIRA, Seoul, Korea), a government-affiliated agency that examines the accuracy of claims for National Health Insurance and National Medical Aid, evaluates the nationwide care status of hospitalized adult patients with CAP to assess and improve the quality of diagnosis and the treatment of pneumonia. This is the first study to report hospital performance for hospitalized patients with CAP in Korea. The aim of this evaluation was to assess the overall quality of care provided for hospitalized adult patients with CAP, and to use the quality measure as the basis for evaluating the treatment outcome of CAP.
Materials and methods
1. Study institutions
HIRA comprehensively analyzed the medical records of hospitalized adult patients with CAP from all of the health institutions that claimed five or more cases of hospitalization with CAP (except for nursing homes) from October to December 2014. HIRA classified the health institutions into three categories: hospital, general hospital, and tertiary hospital. A hospital is a medical facility with more than 30 beds where doctors, dentists, and oriental medical doctors perform medical treatments for hospitalized patients. A general hospital is a hospital with more than 100 beds. The following criteria should be met when defining a general hospital. In the case of 100 beds or more and less than 300 beds, there should be more than seven medical departments including Radiology, Anesthesiology, and Laboratory Medicine (Pathology as an alternative) and at least three medical courses of the following: Internal Medicine, Surgery, Pediatric Adolescents, and Obstetrics and Gynecology. Specialists should be assigned to each medical department. If there are more than 300 beds, there should be more than nine medical departments including Internal Medicine, Surgery, Pediatric Adolescents, Obstetrics and Gynecology, Radiology, Anesthesiology, Laboratory Medicine (Pathology as an alternative), Psychiatry, and Dentistry. Again, specialists should be assigned to each medical department. A tertiary hospital is a general hospital that has specialists assigned to more than 20 medical departments and is equipped with the manpower, facilities, and equipment prescribed by the Ordinance of the Ministry of Health and Welfare.
2. Study subjects
The study subjects comprised hospitalized adult patients aged 18 years or more with CAP and treated with intravenous antibiotics for a period of 3 days or more. Subjects were excluded if they had the following conditions: patients with hospital-acquired pneumonia, ventilator-associated pneumonia, postoperative pneumonia, or healthcare-associated pneumonia; patients whose treatment for pneumonia was delayed because of other acute illnesses such as emergency surgery; patients who were not administered intravenous antibiotics within 72 hours after hospitalization; patients who were transferred to the hospital after the initiation of intravenous antibiotics; patients who had a history of 2 or more days of hospitalization within a 90-day period; patients who were treated in a nursing home; patients receiving palliative care or hospice care; patients who had been diagnosed with malignant disease or had received anti-cancer therapy including chemotherapy and radiation therapy within a period of 3 months; patients who had an immunocompromised disease or received immunosuppressive therapy; patients who had been treated with high-dose steroids (20 mg/day for 2 weeks or more); patients undergoing dialysis eight times or more per month within a 30-day period; and patients with human immunodeficiency virus infection.
3. CAP hospital inpatient quality measure set
The hospital inpatient quality measure set for CAP was developed by a committee of the Korean Academy of Tuberculosis and Respiratory Diseases from June 2013 to February 2014.
The committee developed 15 measures consisting of eight core measures and five (additional) monitoring measures to evaluate the nationwide care status of hospitalized adult patients with CAP (Table 1). Measurement of arterial oxygenation (CAP1) is important in the initial evaluation of patients with CAP because hypoxemia has been associated with respiratory failure, intensive care unit admission and mortality12,13,14. PSI and CURB65 (CAP2), which are indicators of the severity of pneumonia, have been reported to be crucial for selection of appropriate location of treatment, initial empirical antimicrobial agents15,16. Sputum staining (CAP3), sputum culture (CAP4), and blood cultures prior to first intravenous antibiotics administration (CAP5) are recommended as a diagnostic method based on guidelines for pneumonia because they can be used to set the direction of initial treatment4.
Table 1. CAP hospital inpatient quality measure set.
| Measure | Measure name | Measure description | |
|---|---|---|---|
| Core | CAP 1 | Oxygenation assessment | Oxygenation assessment using either arterial blood gas or pulse oxymetry within 24 hours of hospital arrival |
| CAP 2 | Pneumonia severity assessment | Assessment of CAP severity using either PSI or CURB-65 within 24 hours of hospital arrival | |
| CAP 3 | Sputum smears | Evaluation of sputum smears within 24 hours of hospital arrival | |
| CAP 4 | Sputum cultures | Evaluation of sputum cultures within 24 hours of hospital arrival | |
| CAP 5 | Blood cultures prior to first intravenous antibiotics administration | Proportion of blood cultures obtained prior to first intravenous antibiotics administration of all blood cultures* | |
| CAP 6 | First dose of antibiotic within 8 hours | Proportion of administration of first dose of antibiotic within 8 hours of hospital arrival | |
| CAP 7 | Smoking cessation advice/counseling | Smoking cessation advice/counseling given to patients who have smoked within 1 year | |
| CAP 8 | Screening for pneumococcal vaccination | Screening for pneumococcal vaccination among patients 65 years of age and older | |
| Monitoring | CAP 9 | Median time from initial hospital arrival to first dose of antibiotic | Median time from initial hospital arrival to first dose of antibiotic |
| CAP 10 | Selection of appropriate initial antibiotics | Initial antibiotic selection consistent with current recommendation | |
| CAP 11 | Duration of intravenous antibiotic administration | Duration of intravenous antibiotic administration | |
| CAP 12 | 30-Day readmission rate | Readmission with CAP within 30 days after initial discharge | |
| CAP 13 | 30-Day mortality rate | Mortality within 30 days after hospitalization | |
*Denominator consists of hospitalized CAP patients who have had a blood culture.
CAP: community-acquired pneumonia; PSI: Pneumonia Severity Index.
First dose of antibiotic within 8 hours (CAP6), median time from initial hospital arrival to first dose of antibiotic (CAP9), selection of appropriate initial antibiotics (CAP10), duration of intravenous antibiotic administration (CAP11) are recommended based on guidelines for pneumonia8. Timely antibiotic affects prognosis and the mortality rates in patients with CAP17,18. Guideline-recommended antibiotics can reduce the risk of death from pneumonia up to 30% compared with non-guideline-recommended antibiotics19. Smoking cessation (CAP7) is helpful in preventing pneumonia8,20.
According to guidelines of the Advisory Council on Immunization Practices of the Centers for Disease Control and Prevention, the major preventive measures for CAP are use of pneumococcal vaccines21. Since 2013, pneumococcal vaccination (CAP8) has been included in the National Immunization Program for people over 65 years of age in Korea22. 30-Day readmission rate (CAP12) and 30-day mortality rate (CAP13) were included to assess the severity of pneumonia based on guidelines for pneumonia8.
4. Composite measure score
HIRA calculated the composite measure score in institutions that claimed 10 or more evaluated cases. The weighted value of each core measure was determined by the Pneumonia subcommittee centered on the experts recommended by each society according to clinical significance and it was finalized by the Medical Assessment Coordinating Committee (Table 2). The composite measure score was calculated by dividing the sum of the weighted core measures by the sum of the weighted values of the core measures:
Table 2. Weighted value of core measure.
| Measure | Measure name | Weighted value |
|---|---|---|
| CAP 1 | Oxygenation assessment | 2 |
| CAP 2 | Pneumonia severity assessment | 2 |
| CAP 3 | Sputum smears | 0.5 |
| CAP 4 | Sputum cultures | 0.5 |
| CAP 5 | Blood cultures prior to first intravenous antibiotics administration | 1.5 |
| CAP 6 | First dose of antibiotic within 8 hours | 2 |
| CAP 7 | Smoking cessation advice/counseling | 1 |
| CAP 8 | Screening for pneumococcal vaccination | 0.5 |
CAP: community-acquired pneumonia.
Results
1. Characteristics of the medical institutions and hospitalization cases
The analysis included data from 523 hospitals (42 tertiary hospitals [8.0%], 256 general hospitals [49%], and 225 hospitals [43.0%]). There were 15,432 evaluated cases (tertiary hospitals, 1,673 cases [10.8%]; general hospitals, 8,803 cases [57.1%]; hospitals, 4,956 cases [32.1%]). The estimated total medical cost was 31.8 billion won/28.5 million US dollars (USD) (tertiary hospitals, 5.1 billion won/4.5 million USD [16.0%]; general hospitals, 19.8 billion won/17.8 million USD [62.2%]; and hospitals, 6.9 billion won/6.2 million USD [21.8%]). Table 3 shows the admission route and regional distribution of cases. The most frequent admission routes were hospitalization on a general ward via the outpatient department (9,542 [61.8%]), followed by admission to a general ward via the emergency room (4,473 [29%]), and admission to the intensive care unit via the emergency room (1,166 [7.6%]). Gyeonggi-do was the highest ranked region (16.7%), followed by Seoul (11.7%) and Gyeongsangnam-do (10.9%).
Table 3. The admission routes and regional distribution.
| Total | Tertiary hospital | General hospital | Hospital | |
|---|---|---|---|---|
| Total | 15,432 (100) | 1,673 (10.8) | 8,803 (57.1) | 4,956 (32.1) |
| Admission route | ||||
| Outpatient | ||||
| GW | 9,542 (61.8) | 607 (3.9) | 5,140 (33.3) | 3,795 (24.6) |
| ICU | 251 (1.6) | 10 (0.1) | 159 (1.0) | 82 (0.5) |
| ER | ||||
| GW | 4,473 (29) | 889 (5.8) | 2,652 (17.2) | 932 (6.0) |
| ICU | 1,166 (7.6) | 167 (1.1) | 852 (5.5) | 147 (1.0) |
| Region | ||||
| Seoul | 1,803 (11.7) | 602 (3.9) | 980 (6.4) | 221 (1.4) |
| Busan | 961 (6.2) | 134 (0.9) | 583 (3.8) | 244 (1.6) |
| Incheon | 659 (4.3) | 156 (1.0) | 450 (2.9) | 53 (0.3) |
| Daegu | 898 (5.8) | 177 (1.1) | 277 (1.8) | 444 (2.9) |
| Gwangju | 872 (5.7) | 46 (0.3) | 655 (4.2) | 171 (1.1) |
| Daejeon | 420 (2.7) | 43 (0.3) | 342 (2.2) | 35 (0.2) |
| Ulsan | 272 (1.8) | 23 (0.1) | 119 (0.8) | 130 (0.8) |
| Gyeonggi | 2,583 (16.7) | 266 (1.7) | 1,659 (10.8) | 658 (4.3) |
| Gangwon | 715 (4.6) | 26 (0.2) | 454 (2.9) | 235 (1.5) |
| Chungbuk | 477 (3.1) | 25 (0.2) | 305 (2.0) | 147 (1.0) |
| Chungnam | 781 (5.1) | 88 (0.6) | 370 (2.4) | 323 (2.1) |
| Jeonbuk | 886 (5.7) | 31 (0.2) | 381 (2.5) | 474 (3.1) |
| Jeonnam | 1,185 (7.7) | 0 (0) | 620 (4.0) | 565 (3.7) |
| Gyeongbuk | 902 (5.8) | 0 (0) | 567 (3.7) | 335 (2.2) |
| Gyeongnam | 1,676 (10.9) | 56 (0.4) | 726 (4.7) | 894 (5.8) |
| Jeju | 330 (2.1) | 0 (0) | 315 (2.0) | 15 (0.1) |
| Sejong | 12 (0.1) | 0 (0) | 0 (0) | 12 (0.1) |
Values are presented as number (%).
GW: general ward; ICU: intensive care unit; ER: emergency room.
2. Participant demographics
Table 4 provides an overview of the participant demographics. More women were enrolled than men (8,062 cases [52.2%]). Study subjects older than 70 years of age accounted for 50% (7,449) of cases, those aged 70–79 years accounted for 24.2% (3,731) of cases, and subjects older than 80 years of age accounted for 24.1% (3,781) of cases.
Table 4. The demographics of study participants.
| Total | Tertiary hospital | General hospital | Hospital | |
|---|---|---|---|---|
| Total | 15,432 (100) | 1,673 (10.8) | 8,803 (57.1) | 4,956 (32.1) |
| Sex | ||||
| Male | 7,370 (47.8) | 946 (6.1) | 4,332 (28.1) | 2,092 (13.5) |
| Female | 8,062 (52.2) | 727 (4.7) | 4,471 (29.0) | 2,864 (18.6) |
| Age, yr | ||||
| 18–19 | 151 (1.0) | 15 (0.1) | 90 (0.6) | 46 (0.3) |
| 20–29 | 649 (4.2) | 62 (0.4) | 390 (2.5) | 197 (1.3) |
| 30–39 | 1,396 (9.0) | 144 (0.9) | 852 (5.5) | 400 (2.6) |
| 40–49 | 1,214 (7.9) | 115 (0.7) | 731 (4.7) | 358 (2.4) |
| 50–59 | 2,135 (13.8) | 255 (1.7) | 1,165 (7.5) | 715 (4.6) |
| 60–69 | 2,438 (15.8) | 319 (2.1) | 1,383 (9.0) | 736 (4.8) |
| 70–79 | 3,731 (24.2) | 443 (2.9) | 2,140 (13.9) | 1,148 (7.4) |
| ≥80 | 3,718 (24.1) | 320 (2.1) | 2,052 (13.3) | 1,346 (8.7) |
Values are presented as number (%).
3. Hospital CAP core measures
Table 5 shows the performance rates of the hospital CAP core measures. Five measures were obtained including data related to oxygenation assessment obtained from 523 institutions (100%), blood cultures taken before the initial administration of antibiotics obtained from 336 institutions (64.2%), smoking cessation counseling obtained from 138 institutions (26.4%), and screening for pneumococcal vaccination obtained from 469 institutions (89.7%). The variation in overall performance rate of the hospital CAP core measures was large, ranging from 53.7% to 93.1%. The performance rate was higher in terms of the administration of the first antibiotic dose within 8 hours from the time of hospital arrival (93.1%), smoking cessation counseling (92.2%), and blood cultures obtained prior to the first administration of antibiotics (85.2%). The performance rate was lower in terms of pneumonia severity assessment (56.3%) and screening for pneumococcal vaccination (53.7%).
Table 5. The performance of hospital CAP core measures.
| Measure name | No. of institutions | No. of cases | Performance rate of core measure (%) | ||||
|---|---|---|---|---|---|---|---|
| Total | Tertiary hospital | General hospital | Hospital | ||||
| CAP 1 | Oxygenation assessment | 523 | 15,432 | 68.1 | 99.5 | 81.9 | 33.0 |
| CAP 2 | Pneumonia severity assessment | 523 | 15,432 | 56.3 | 98.4 | 72.2 | 13.8 |
| CAP 3 | Sputum smears | 523 | 15,432 | 68.1 | 98.6 | 77.1 | 41.8 |
| CAP 4 | Sputum cultures | 523 | 15,432 | 70.2 | 98.7 | 79.5 | 44.2 |
| CAP 5 | Blood cultures prior to first intravenous antibiotics administration | 336 | 8,533 | 85.2 | 95.1 | 84.4 | 72.1 |
| CAP 6 | First dose of antibiotic within 8 hours | 523 | 15,432 | 93.1 | 97.8 | 93.9 | 90.0 |
| CAP 7 | Smoking cessation advice/counseling | 138 | 1,101 | 92.2 | 100.0 | 92.7 | 63.0 |
| CAP 8 | Screening for pneumococcal vaccination | 469 | 8,632 | 53.7 | 99.7 | 66.5 | 15.8 |
CAP: community-acquired pneumonia.
1) CAP 1. Oxygenation assessment within 24 hours of hospital arrival
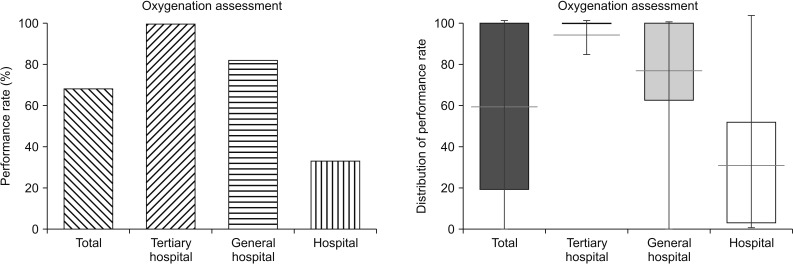
The overall performance rate of oxygenation assessment within 24 hours of arrival at hospital was 68.1%. Oxygenation assessment within 24 hours of hospital arrival varied greatly depending on the institution (tertiary hospitals, 99.5%; general hospitals, 81.9%; hospitals, 33.0%) (Figure 1). The minimum rate was 0% and the maximum rate was 100%. Among hospitals, in particular, the performance rate for oxygenation assessment was low with a large variation (mean, 30.6%; Q1, 3.6%; Q3, 51.5%) (Figure 1). Fifty-eight institutions had a minimum measure rate of zero (3 general hospitals and 55 hospitals).
Figure 1. Performance rates of oxygenation assessment according to institution.
2) CAP 2. Pneumonia severity assessment
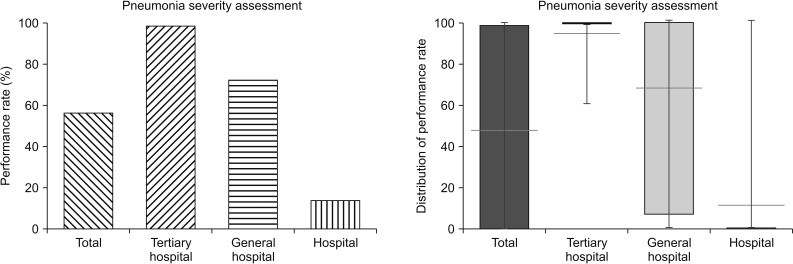
The overall performance rate for pneumonia severity assessment was 56.3%. This greatly varied depending on the institution (tertiary hospitals, 98.4%; general hospitals, 72.2%; hospitals, 13.8%) (Figure 2). The minimum rate was 0% and the maximum rate was 100%, indicating that pneumonia severity assessment is rarely performed in hospitals (Q1, 0%; Q3, 0%). Even general hospitals showed a large variation in the performance rate for pneumonia severity assessment (mean, 68.9%; Q1, 7.7%; Q3, 100%).
Figure 2. Performance rates of pneumonia severity assessment according to institution.
3) CAP 3. Sputum smear within 24 hours of arrival
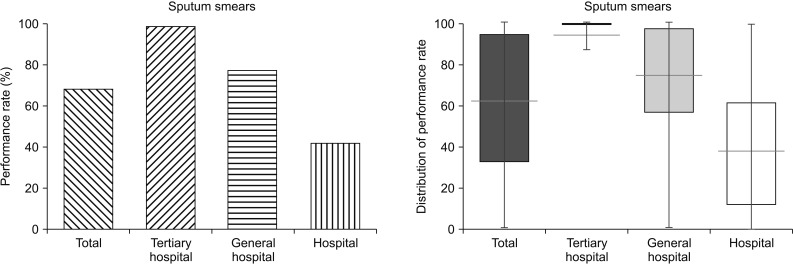
The overall performance rate of sputum smears performed within 24 hours of arrival at hospital was 68.1% (tertiary hospitals, 98.6%; general hospitals, 77.1%; hospitals, 41.8%) (Figure 3). This performance rate had a minimum of 0% and a maximum of 100%. The performance rate for sputum smears was low with a large variation among hospitals (mean, 39.9%; Q1, 12.5%; Q3, 60.9%).
Figure 3. Performance rates of sputum smears within 24 hours of hospital arrival according to institution.
4) CAP 4. Sputum culture within 24 hours of hospital arrival
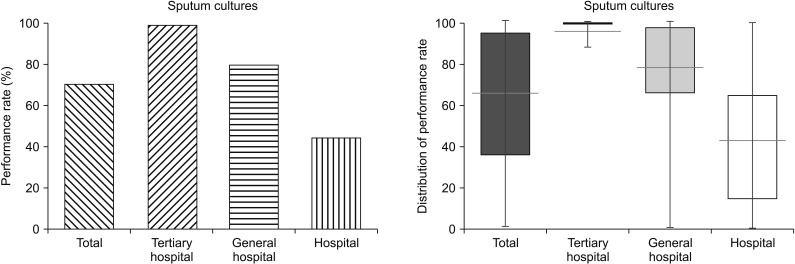
The overall performance rate of sputum cultures performed within 24 hours of arrival was 70.2% (tertiary hospitals, 98.7%; general hospitals, 79.5%; hospitals, 44.2%) (Figure 4). This performance rate had a minimum of 0% and a maximum of 100%. The performance rate for sputum cultures was low with a large variation among hospitals (mean, 42.0%; Q1, 15.4%; Q3, 64.3%).
Figure 4. The performance rates of sputum cultures performed within 24 hours of hospital arrival according to institution.
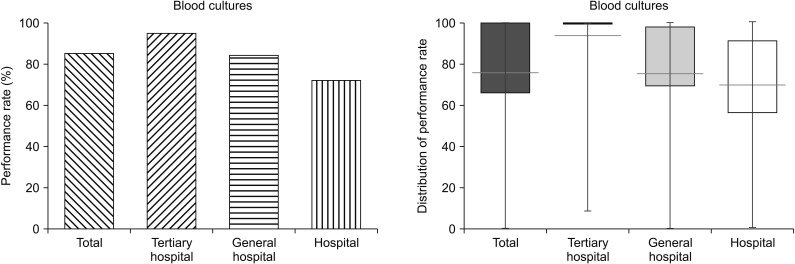
5) CAP 5. Blood culture prior to first intravenous antibiotic administration
Blood cultures taken prior to the initial administration of antibiotics accounted for 85.2% of all of the blood cultures (tertiary hospitals, 95.1%; general hospitals, 84.4%; hospitals, 72.1%) (Figure 5). This performance rate had a minimum of 0% and a maximum of 100%. Hospitals had a relatively high performance rate of blood cultures taken prior to the initial administration of antibiotics (mean, 69.3%; Q1, 57.1%; Q3, 90.9%).
Figure 5. Performance rates of blood cultures taken prior to the initial administration of antibiotics according to institution.
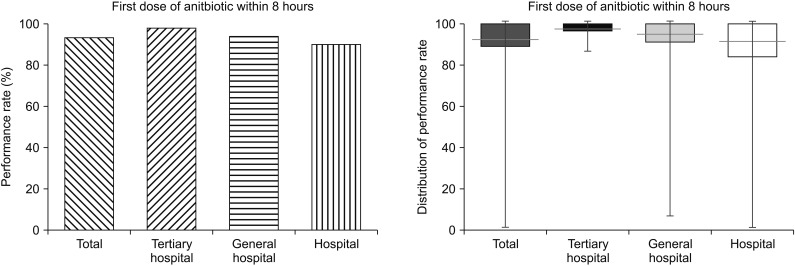
6) CAP 6. First dose of antibiotics administered within 8 hours of the time of hospital arrival
The percentage of CAP patients receiving their first dose of antibiotics within 8 hours of their arrival at hospital was 93.1%. Overall, this performance rate was the highest and had the least institutional variation (tertiary hospitals, 97.8%; general hospitals, 93.9%; hospitals, 90.0%) (Figure 6). This performance rate had a minimum of 0% and a maximum of 100%. Among hospitals, the performance rate was high with low variation (mean, 89.1%; Q1, 84.6%; Q3, 100.0%).
Figure 6. Performance rates of the administration of the first dose of antibiotics within 8 hours of the time of hospital arrival according to institution.
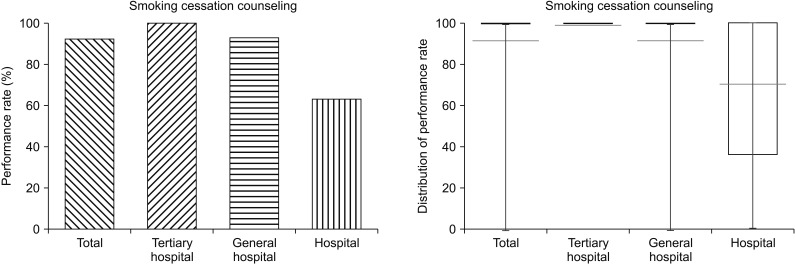
7) CAP 7. Smoking cessation counseling
The percentage of CAP patients with a history of smoking within a 1-year period who were offered smoking cessation counseling was 92.2%. This performance rate was lowest in hospitals (tertiary hospitals, 100.0%; general hospitals, 92.7%; hospitals, 63.0%) (Figure 7). The performance rate of smoking cessation counseling had a minimum of 0% and a maximum of 100%. There was a large variation in the performance rate among hospitals (mean, 68.5%; Q1, 36.7%; Q3, 100%).
Figure 7. Performance rates of smoking cessation counseling according to institution.
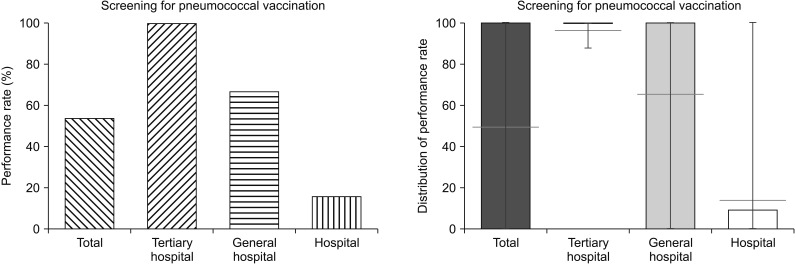
8) CAP 8. Screening for pneumococcal vaccination
The performance rate of screening for pneumococcal vaccination in patients aged 65 years and older was 53.7%. This performance rate greatly varied depending on the type of institution (tertiary hospitals, 99.7%; general hospitals, 66.5%; hospitals, 15.8%). There was a large difference in the performance rate between tertiary hospitals and hospitals (Figure 8). The performance rate of screening for pneumococcal vaccination had a minimum of 0% and a maximum of 100%. The performance rate was lowest in hospitals (mean, 15.5%; Q1, 0.0%; Q3, 8.7%). However, general hospitals had a large variation in the performance rate (mean, 65.3%; Q1, 0.0%; Q3, 100.0%). A total of 189 institutions had a minimum measurement rate of zero (62 general hospitals and 127 hospitals).
Figure 8. Performance rates of screening for pneumococcal vaccination according to institution.
4. Hospital CAP monitoring measures
1) CAP 9. Median time from initial hospital arrival to the first dose of antibiotics
The median time from the initial arrival at hospital to the hospitals, 175 minutes; general hospitals, 99 minutes; hospitals, 27 minutes) (Table 6). Fifty-nine institutions had a median value of less than zero (11 general hospitals and 48 hospitals).
Table 6. The result of monitoring measures.
| Monitoring measure | Measure name | No. of institutions | No. of cases | Result | |||
|---|---|---|---|---|---|---|---|
| Total | Tertiary hospital | General hospital | Hospital | ||||
| Process | Median time from initial hospital arrival to first dose of antibiotic, min | 520 | 15,240 | 83 | 175 | 99 | 27 |
| Selection of appropriate initial antibiotics, % | 523 | 15,432 | 81.9 | 92.7 | 84.6 | 73.3 | |
| Duration of intravenous antibiotic administration, day | 523 | 15,272 | 8 | 7 | 8 | 8 | |
| Outcome | 30-Day readmission rate, % | 520 | 13,114 | 2.0 | 1.1 | 2.3 | 1.8 |
| 30-Day mortality rate, % | 523 | 14,974 | 3.7 | 3.8 | 3.6 | 3.7 | |
2) CAP 10. Selection of appropriate initial antibiotics
The rate of appropriate intravenous antibiotic administration according to the recommendation of the treatment guideline was 81.9% (Table 6). Tertiary hospitals had a high rate of appropriate intravenous antibiotic administration (tertiary hospitals, 92.7%; general hospitals, 84.6%; hospitals, 73.3%).
3) CAP 11. Duration of intravenous antibiotic administration
The median duration of intravenous antibiotic administration for pneumonia was 8 days (Table 6). The duration of intravenous antibiotics in tertiary hospitals was lower by 1 day than that of general hospitals and hospitals.
4) CAP 12. Thirty-day readmission rate
The readmission rate within 30 days after pneumonia treatment was 2.0% (tertiary hospitals, 1.1%; general hospitals, 2.3%; hospitals, 1.8%) (Table 6). While the readmission rate of patients discharged after being hospitalized via the emergency room was high in tertiary hospitals, the readmission rate of patients discharged after hospitalization via the outpatient department was high in general hospitals and hospitals. The 30-day readmission rate was also high in subjects older than 70 years.
5) CAP 13. Thirty-day mortality rate
The mean 30-day mortality rate after admission was 3.7%. There was little difference between institutions in terms of 30-day mortality after admission (tertiary hospitals, 3.8%; general hospitals, 3.6%; hospitals, 3.7%) (Table 6). The mean mortality rate was 3.8% and the median mortality rate was 1.9%. The mortality rates of patients admitted to the intensive care unit and subjects older than 70 years were high.
5. Composite measure score
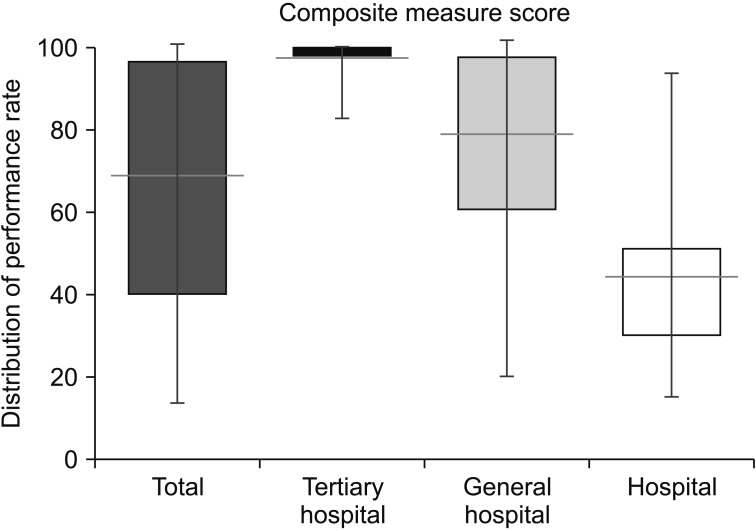
The composite measure score was calculated in 482 institutions (92.2%) with more than 10 evaluation cases, among a total of 523 institutions. The mean composite measure score was 66.7 (tertiary hospitals, 98.5; general hospitals, 79.2; hospitals, 43.8). There was a large variation in the composite measure score among institutions, ranging from 15.1 to 100.0 (Figure 9). The results of the quality measure set were publicly released for medical use and to allow data to be benchmarked by medical institutions.
Figure 9. Distribution of composite measure scores.
Discussion
Since the publication of process quality measures by Medicare in 2002 with the goal of improving health outcomes, the modification of these measures and the development of strategies to improve adherence have continued in the United States23,24. To the best of our knowledge, this is the first national report of care measures for CAP in Korea.
Eight core measures, a composite measure score reflecting the weighted value of each core measure, and five monitoring measures regarding CAP were examined. An evidence link between hospital-based core measures and safety goals related to patient outcomes was found to exist25. Oxygenation assessment should be performed with pulse oximetry or arterial blood gas because 10% of hypoxemic patients are asymptomatic26. A arterial partial pressure of oxygen level of less than 60 mm Hg, reflecting the severity of pneumonia, is associated with the 30-day mortality rate27. The guideline recommends that the CURB-65 criteria or the pneumonia severity index should be used as an objective criterion to determine whether or not patients require hospitalization and whether patients should be treated in the intensive care unit27.Microbiological testing such as sputum smears, sputum cultures, and blood cultures can lead to a change in antibiotic therapy in up to 40% of patients with severe pneumonia5. Timely administration of antibiotics is associated with a lower risk of mortality19. Smoking cessation counseling is effective for ending smoking9. Smokers are at risk for severe pneumonia and are two to three times more likely to experience pneumonia than non-smokers9. The pneumococcal vaccine is 40% effective for preventing pneumonia in high-risk patients10,11. Moreover, vaccination results in lower mortality and shorter hospitalization even in patients with pneumonia10,11. Monitoring measures such as the median time from the initial arrival at hospital to the administration of the first dose of antibiotics, the selection of appropriate initial antibiotics, and the duration of intravenous antibiotics are closely linked to the treatment effect26. 30-Day readmission rate, and 30-day mortality rate are other outcome measures. We assessed the overall performance rates of the quality measures and demonstrated the presence of variation among the performance rates across all measures.
Our report showed that the performance rates of the core measures varied and that the variation among each type of institution was large. Remarkably, the performance rate in hospitals was low and the variation within them was large, except for the performance rates of blood cultures taken prior to the first administration of antibiotics (72.1%) and the first dose of antibiotics administered within 8 hours of the time of hospital arrival (90%). Likewise, the composite measure score varied widely among the institutions (tertiary hospitals, 98.5; general hospitals, 79.2; hospitals, 43.8). There was a significant difference among the institutions in terms of the suitability of the initial selection of antibiotics (tertiary hospitals, 92.7%; general hospitals, 84.6%; hospitals, 73.3%) and the medical costs per case (tertiary hospitals, 2,410,000 Korean won; general hospitals, 2,020,000 Korean won; hospitals, 1,340,000 Korean won).
It is important that there are no significant differences in 30-day mortality between hospitals, although there are significant differences in several measure scores and medical costs. The severity of pneumonia may offset the effect of quality of care in tertiary hospitals. The reasons for this are unclear and need further analysis. The development of appropriate quality measurement tools that reflect the mortality is needed.
Previous studies monitored hospital performance and quality of care for single conditions over a specific period of time28,29,30. In the United States, a comprehensive analysis of the national trend in the Medicare core process measures for several diseases was reported31. The report documented the success of process improvement among all United States hospitals in the Centers for Medicare and Medicaid Services (CMS) core process measures for acute myocardial infarction, heart failure, and pneumonia from 2006 to 201131. Efforts to improve the measurement of performance by numerous national initiatives yielded a reduction in hospital-level variability and generally high performance during that period32,33,34. CMS has steadily continued to add to, modify, and publicly report these care measures to maintain the accuracy and reliability of the measures for quality improvement24.
As national efforts focusing on quality improvement have continued in Korea, hospital performance in quality measures for several conditions has begun to be publicly reported. The first evaluation of the quality of care for hospitalized adult patients with CAP (from October to December 2014) was followed by a secondary evaluation (from April to June 2016). Monitoring of the trend in performance measures over time should be continued because it is an important indicator of the success in achieving quality of care. Distinguishing and targeting lower-quality hospitals for quality improvement are expected to be beneficial in narrowing the gap between high-performing and low-performing hospitals. Modifying the existing measures and constructing novel ones is necessary to improve the accuracy and reliability of the measures for quality of care.
In conclusion, we documented the performance of care measures for CAP in 2014. We found diversity in the measures and large gaps among institutions in terms of performance of care measures. In particular, there was a lower level of performance in hospitals compared to tertiary hospitals and general hospitals. Nonetheless, there were no significant differences in mortality between hospitals. Determining the appropriate care measures for CAP and monitoring the trend in performance measures are needed.
Acknowledgments
We acknowledge the effort of the Health Insurance Review and Assessment Service.
Footnotes
Authors' Contributions: Conceptualization: Kang YA. Methodology: Hong JY. Writing - original draft preparation: Kang YA, Hong JY. Writing - review and editing: Kang YA, Hong JY. Approval of final manuscript: all authors.
Conflicts of Interest: No potential conflict of interest relevant to this article was reported.
References
- 1.World Health Organization. Pneumonia: Fact sheet [Internet] Geneva: World Health Organization; 2017. [cited 2017 Dec 31]. Available from: http://who.int/mediacentre/factsheets/fs331/en/2017. [Google Scholar]
- 2.Bartlett JG, Dowell SF, Mandell LA, File TM, Jr, Musher DM, Fine MJ. Practice guidelines for the management of community-acquired pneumonia in adults. Infectious Diseases Society of America. Clin Infect Dis. 2000;31:347–382. doi: 10.1086/313954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Korean Statistical Information Service. Statistical database: health/society/welfare [Internet] Daejeon: Statistivs Korea; 2017. [cited 2017 Dec 31]. Available from: http://kosis.kr/statisticsList/statisticsList_01List.jsp?vwcd=MT_ZTITLE&parentId=D2017. [Google Scholar]
- 4.Song JH, Jung KS, Kang MW, Kim DJ, Pai H, Suh GY, et al. Treatment guidelines for community-acquired pneumonia in Korea: an evidence-based approach to appropriate antimicrobial therapy. Tuberc Respir Dis. 2009;67:281–302. [Google Scholar]
- 5.Rello J, Bodi M, Mariscal D, Navarro M, Diaz E, Gallego M, et al. Microbiological testing and outcome of patients with severe community-acquired pneumonia. Chest. 2003;123:174–180. doi: 10.1378/chest.123.1.174. [DOI] [PubMed] [Google Scholar]
- 6.Houck PM, Bratzler DW, Nsa W, Ma A, Bartlett JG. Timing of antibiotic administration and outcomes for Medicare patients hospitalized with community-acquired pneumonia. Arch Intern Med. 2004;164:637–644. doi: 10.1001/archinte.164.6.637. [DOI] [PubMed] [Google Scholar]
- 7.Mitka M. JCAHO tweaks emergency departments' pneumonia treatment standards. JAMA. 2007;297:1758–1759. doi: 10.1001/jama.297.16.1758. [DOI] [PubMed] [Google Scholar]
- 8.Mandell LA, Wunderink RG, Anzueto A, Bartlett JG, Campbell GD, Dean NC, et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;44(Suppl 2):S27–S72. doi: 10.1086/511159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Murin S, Bilello KS. Respiratory tract infections: another reason not to smoke. Cleve Clin J Med. 2005;72:916–920. doi: 10.3949/ccjm.72.10.916. [DOI] [PubMed] [Google Scholar]
- 10.Ansaldi F, Turello V, Lai P, Bastone G, De Luca S, Rosselli R, et al. Effectiveness of a 23-valent polysaccharide vaccine in preventing pneumonia and non-invasive pneumococcal infection in elderly people: a large-scale retrospective cohort study. J Int Med Res. 2005;33:490–500. doi: 10.1177/147323000503300503. [DOI] [PubMed] [Google Scholar]
- 11.Vila-Corcoles A, Ochoa-Gondar O, Hospital I, Ansa X, Vilanova A, Rodriguez T, et al. Protective effects of the 23-valent pneumococcal polysaccharide vaccine in the elderly population: the EVAN-65 study. Clin Infect Dis. 2006;43:860–868. doi: 10.1086/507340. [DOI] [PubMed] [Google Scholar]
- 12.Fine MJ, Auble TE, Yealy DM, Hanusa BH, Weissfeld LA, Singer DE, et al. A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med. 1997;336:243–250. doi: 10.1056/NEJM199701233360402. [DOI] [PubMed] [Google Scholar]
- 13.Fine MJ, Smith MA, Carson CA, Mutha SS, Sankey SS, Weissfeld LA, et al. Prognosis and outcomes of patients with community-acquired pneumonia: a meta-analysis. JAMA. 1996;275:134–141. [PubMed] [Google Scholar]
- 14.Bowton DL, Scuderi PE, Haponik EF. The incidence and effect on outcome of hypoxemia in hospitalized medical patients. Am J Med. 1994;97:38–46. doi: 10.1016/0002-9343(94)90046-9. [DOI] [PubMed] [Google Scholar]
- 15.Fine MJ, Hough LJ, Medsger AR, Li YH, Ricci EM, Singer DE, et al. The hospital admission decision for patients with community-acquired pneumonia: results from the pneumonia Patient Outcomes Research Team cohort study. Arch Intern Med. 1997;157:36–44. [PubMed] [Google Scholar]
- 16.Lim WS, van der Eerden MM, Laing R, Boersma WG, Karalus N, Town GI, et al. Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax. 2003;58:377–382. doi: 10.1136/thorax.58.5.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yahav D, Leibovici L, Goldberg E, Bishara J, Paul M. Time to first antibiotic dose for patients hospitalised with community-acquired pneumonia. Int J Antimicrob Agents. 2013;41:410–413. doi: 10.1016/j.ijantimicag.2013.01.008. [DOI] [PubMed] [Google Scholar]
- 18.Bader MS, Abouchehade KA, Yi Y, Haroon B, Bishop LD, Hawboldt J. Antibiotic administration longer than eight hours after triage and mortality of community-acquired pneumonia in patients with diabetes mellitus. Eur J Clin Microbiol Infect Dis. 2011;30:881–886. doi: 10.1007/s10096-011-1171-8. [DOI] [PubMed] [Google Scholar]
- 19.Gleason PP, Meehan TP, Fine JM, Galusha DH, Fine MJ. Associations between initial antimicrobial therapy and medical outcomes for hospitalized elderly patients with pneumonia. Arch Intern Med. 1999;159:2562–2572. doi: 10.1001/archinte.159.21.2562. [DOI] [PubMed] [Google Scholar]
- 20.Cao B, Huang Y, She DY, Cheng QJ, Fan H, Tian XL, et al. Diagnosis and treatment of community-acquired pneumonia in adults: 2016 clinical practice guidelines by the Chinese Thoracic Society, Chinese Medical Association. Clin Respir J. 2018;12:1320–1360. doi: 10.1111/crj.12674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.The Advisory Committee on Immunization Practices (ACIP) Summary of recommendations for adult immunization [Internet] St. Paul: Immunization Action Coalition; 2011. [cited 2017 Dec 11]. Available from: http://www.immunize.org/catg.d/p2011.pdf. [Google Scholar]
- 22.The Korean Society of Infectious Diseases. Adult immunization guidelines [Internet] Seoul: The Korean Society of Infectious Diseases; 2017. [cited 2017 Dec 11]. Available from: http://www.ksid.or.kr/data/sub07.html. [Google Scholar]
- 23.Jha AK, Li Z, Orav EJ, Epstein AM. Care in U.S. hospitals: the Hospital Quality Alliance program. N Engl J Med. 2005;353:265–274. doi: 10.1056/NEJMsa051249. [DOI] [PubMed] [Google Scholar]
- 24.Hospital Inpatient Quality Reporting (IQR) [Internet] Kuwait City: QualityNet; 2017. [cited 2017 Dec 31]. Available from: https://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FQnetHomepage&cid=11381159871292014. [Google Scholar]
- 25.Masica AL, Richter KM, Convery P, Haydar Z. Linking joint commission inpatient core measures and national patient safety goals with evidence. Proc (Bayl Univ Med Cent) 2009;22:103–111. doi: 10.1080/08998280.2009.11928486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Levin KP, Hanusa BH, Rotondi A, Singer DE, Coley CM, Marrie TJ, et al. Arterial blood gas and pulse oximetry in initial management of patients with community-acquired pneumonia. J Gen Intern Med. 2001;16:590–598. doi: 10.1046/j.1525-1497.2001.016009590.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Song JH, Jung KS. Treatment guidelines for community-acquired pneumonia in Korea: an evidence-based approach to appropriate antimicrobial therapy. J Korean Med Assoc. 2010;53:20–42. [Google Scholar]
- 28.Chassin MR, Loeb JM, Schmaltz SP, Wachter RM. Accountability measures: using measurement to promote quality improvement. N Engl J Med. 2010;363:683–688. doi: 10.1056/NEJMsb1002320. [DOI] [PubMed] [Google Scholar]
- 29.Kumbhani DJ, Fonarow GC, Cannon CP, Hernandez AF, Peterson ED, Peacock WF, et al. Predictors of adherence to performance measures in patients with acute myocardial infarction. Am J Med. 2013;126:74.e1–74.e9. doi: 10.1016/j.amjmed.2012.02.025. [DOI] [PubMed] [Google Scholar]
- 30.Lee JS, Nsa W, Hausmann LR, Trivedi AN, Bratzler DW, Auden D, et al. Quality of care for elderly patients hospitalized for pneumonia in the United States, 2006 to 2010. JAMA Intern Med. 2014;174:1806–1814. doi: 10.1001/jamainternmed.2014.4501. [DOI] [PubMed] [Google Scholar]
- 31.Nuti SV, Wang Y, Masoudi FA, Bratzler DW, Bernheim SM, Murugiah K, et al. Improvements in the distribution of hospital performance for the care of patients with acute myocardial infarction, heart failure, and pneumonia, 2006-2011. Med Care. 2015;53:485–491. doi: 10.1097/MLR.0000000000000358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Marciniak TA, Ellerbeck EF, Radford MJ, Kresowik TF, Gold JA, Krumholz HM, et al. Improving the quality of care for Medicare patients with acute myocardial infarction: results from the Cooperative Cardiovascular Project. JAMA. 1998;279:1351–1357. doi: 10.1001/jama.279.17.1351. [DOI] [PubMed] [Google Scholar]
- 33.Larson JS, Muller A. Managing the quality of health care. J Health Hum Serv Adm. 2002;25:261–280. [PubMed] [Google Scholar]
- 34.Costante PA. AMAP: toward standardized physician quality data. American Medical Accreditation Program. N J Med. 1999;96:47–48. [PubMed] [Google Scholar]