Abstract
Objective: Bipolar disorder is highly comorbid with anxiety disorders, however current and lifetime comorbidity patterns of each anxiety disorder and their associated features are not well studied. Here, we aimed to conduct a meta-analysis and meta-regression study of current evidence.
Method: We searched PubMed to access relevant articles published until September 2015, using the keywords “Bipolar disorder” or “Affective Psychosis” or “manic depressive” separately with “generalized anxiety,” “panic disorder,” “social phobia,” “obsessive compulsive,” and “anxiety.” Variables for associated features and prevalence of anxiety disorders were carefully extracted.
Results: Lifetime any anxiety disorder comorbidity in BD was 40.5%; panic disorder (PD) 18.1%, generalized anxiety disorder (GAD) 13.3%, social anxiety disorder (SAD) 13.5% and obsessive compulsive disorder (OCD) 9.7%. Current any anxiety disorder comorbidity in BD is 38.2%; GAD is 15.2%, PD 13.3%, SAD 11.7%, and OCD 9.9%. When studies reporting data about comorbidities in BDI or BDII were analyzed separately, lifetime any anxiety disorder comorbidity in BDI and BDII were 38% and 34%, PD was 15% and 15%, GAD was 14% and 16.6%, SAD was 8% and 13%, OCD was 8% and 10%, respectively. Current any DSM anxiety disorder comorbidity in BDI or BDII were 31% and 37%, PD was 9% and 13%, GAD was 8% and 12%, SAD was 7% and 11%, and OCD was 8% and 7%, respectively. The percentage of manic patients and age of onset of BD tended to have a significant impact on anxiety disorders. Percentage of BD I patients significantly decreased the prevalence of panic disorder and social anxiety disorder. A higher rate of substance use disorder was associated with greater BD–SAD comorbidity. History of psychotic features significantly affected current PD and GAD.
Conclusions: Anxiety disorder comorbidity is high in BD with somewhat lower rates in BDI vs BDII. Age of onset, substance use disorders, and percentage of patients in a manic episode or with psychotic features influences anxiety disorder comorbidity.
Keywords: bipolar disorder, anxiety disorders, epidemiology, panic disorder, psychosis, substance-related disorders
Introduction
With an average 1% lifetime prevalence for bipolar disorder type I (BD I) and overall prevalence of almost 4% for bipolar spectrum disorders more broadly (1), BD is one of the most prevalent psychiatric disorders. On the other hand, it is also one of the most mutable disorders, comorbidity is the norm among patients diagnosed with BD and this may complicate the differential diagnosis as well as management (2–5). Given these challenges, it is important to understand the patterns of comorbidity and complex presentations in patients with BD.
Among BD comorbidities, anxiety disorders are second only to substance use disorders (SUD) (6–8), and in some reports even more common (9, 10). Only one study in a Chinese population found low anxiety disorder rates in BD patients (11). In addition, BD patients have higher rates of comorbid anxiety disorders compared to general population (2, 12, 13) and compared to unipolar depression patients (14, 15). The comorbidity of anxiety disorders in BD is not only common but also clinically significant because it can affect patient course and treatment response (16–21). Individual studies found an association of anxiety disorder comorbidity with earlier age of onset (22–24), increased symptom severity (17, 23), and multiple adverse outcomes in BD (17–19, 21, 23–47). BD patients diagnosed with anxiety may also need to be managed differently (48, 49). At a deeper level, it is not known whether the BD-anxiety disorder comorbidity represents a shared pathophysiology between two common psychiatric conditions, or a subgroup of patients with a genuinely different clinical condition which appears comorbidity. Ultimately, BD may come to be seen not only as a mood disorder but also as complex presentation with many nested circles involving anxiety, substance use, character pathology, and physical conditions (50).
Although there is a literature on the topic, the moderators of BD-anxiety disorder comorbidity and the variance in subgroups of anxiety disorders are not well studied due to the heterogeneity of BD and the heterogeneity in study methodology. Individual studies point out that unipolar mania patients may be less likely to be diagnosed with an anxiety disorder (51), and that BD type II (BD II) is found to be more related with anxiety symptoms (13, 36, 52) and it can be comparable to patients diagnosed with major depressive disorder (MDD) (14, 15, 52).
There is also the question of whether specific anxiety disorders are observed more often than others in BD patients, and which variables are important for comorbidity with each anxiety disorder. For example, association of specific anxiety disorders with gender, age at onset of BD, and substance use disorder may offer clues about the patterns of disorder emergence (10, 53–57). Finally, this research may point to risk factors such as traumatic life events or shared genetic vulnerability (53–56).
In this study, we conducted a systematic review and meta-analysis to answer the following questions about BD and anxiety disorder comorbidity: Question 1: What is the prevalence of lifetime and current anxiety disorder diagnosis in BD? We broke this question further to examine comorbidity patterns of commonly reported disorders: generalized anxiety disorder, panic disorder, obsessive compulsive disorder and social phobia. We also examined data from BD overall, as well as specifically in BD I and BD II. Question 2: How do moderators such as the mean age, marital status, gender, BD I ratio, educational level, age of onset of BD, current episode of BD, and presence of substance use disorders affect anxiety disorder comorbidity in BD? We sought to evaluate a large literature and identify patterns which may help provide new insights into the pathophysiology and clinical course of these common disorders.
Methods
Search strategy
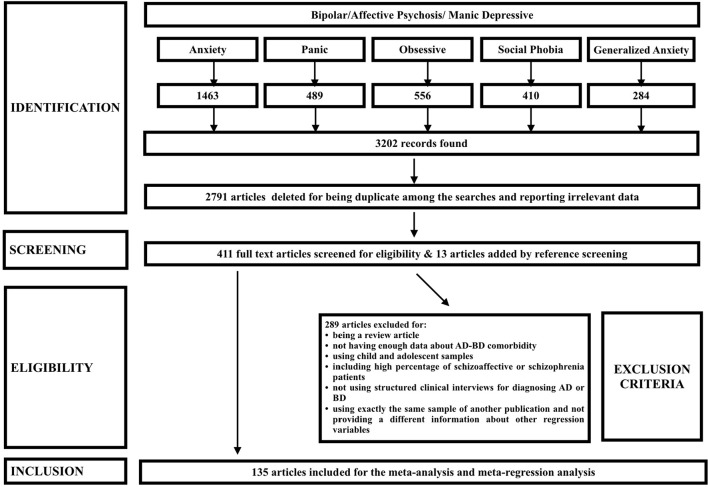
This study was designed and conducted in accordance with the MOOSE (58) and PRISMA (59) guidelines. We searched PubMed to access all relevant articles published until September 30th, 2015, starting from the first published viewable study in 1995. We used the keywords “Bipolar disorder” or “Affective Psychosis” or “manic depressive” separately with “generalized anxiety,” “panic disorder,” “social phobia,” “obsessive compulsive,” and “anxiety” to search for all relevant articles with this topic. All keywords were searched in the “Title/Abstract” of the articles. Only the articles that had an abstract or full text in published in English were included in the study (Figure 1).
Figure 1.
PRISMA flow of found studies based on the research and screening methods.
All abstracts were read to identify articles that have relevant prevalence data of any anxiety disorder in BD. If the abstract was inconclusive, the full article was accessed to ascertain whether relevant information was reported. Articles that reported data about prevalence of anxiety disorders were saved in full text for further evaluation. References of all original articles and reviews were checked for additional studies not previously accessed.
Study selection
Only original articles that diagnosed BD based on structured interviews [SCID, SADS- Schedule for Affective Disorders for Schizophrenia, DIGS (Diagnostic interview for genetic studies), CIDI or MINI] or on selected diagnostic criteria (both DSM-III and DSM-IV) were included. Studies that did not present conclusive data about BD—anxiety disorder comorbidity, review articles, studies on child and adolescent bipolar disorder patient samples, studies that were performed on data from health records/registries or hospital charts, studies that did not use structured clinical interviews for the diagnosis of anxiety disorders and diagnosed anxiety disorders based on scales, studies that reported data about the prevalence of “any anxiety disorder diagnosis” but did not define or clarify which disorders were concluded as “any anxiety disorder” were excluded.
Studies that presented data of comorbidity in a heterogenous sample of psychotic disorders (i.e., schizophrenia, schizoaffective disorder and bipolar disorder) were excluded, however, studies that included less than 5% of patients schizoaffective disorder in addition to BD were included because of potential overlap in DSM-III criteria. Samples consisting of one gender or samples with another disorder comorbidity in the whole sample (e.g., eating disorder or substance use disorder) were also included for the pooled analysis. Data about past history of intraepisode anxiety disorder were excluded (60, 61).
Data extraction
All relevant data about the prevalence and possible determinants of anxiety disorder comorbidity were extracted from each article by two authors (HYE, CMK, ASK, MY); HYE and ASK subsequently checked for the correctness of each data from each article. Extracted information included: name of the authors, name of the city and country where the sample was recruited, publication year, purpose of the study, how the research sample was defined and method of sampling, types of bipolarity in the sample (BD, Bipolar I, II) and percentage of BD I in the sample, sample size, number of individuals diagnosed with any anxiety disorder, generalized anxiety disorder, panic disorder, social phobia, and obsessive compulsive disorder in BD, BD I, BD II separately, mean age of the sample, age range, gender ratio, interview method, how bipolar disorder is diagnosed, if psychotic features are reported or not and percentage of patients with a history of psychotic symptoms, how anxiety disorder is diagnosed, if anxiety diagnosis is current, lifetime, last year or last month, definition for “any anxiety disorder,” episode of BD, BD age of onset, % of high school or higher graduates, marital status of the sample, BD family history, anxiety disorder family history, ADHD prevalence in the sample, and substance use disorder prevalence in the sample.
When a study did not report if the anxiety disorder diagnosis was current or lifetime, studies that used the MINI were coded as “current diagnosis”; “Diagnostic Interview for Genetic Studies” were coded as “lifetime.” A SCID diagnosis of anxiety disorders were coded as “lifetime” unless otherwise specified. A CIDI diagnosis of GAD was coded as last 12 months and defined as current, whereas a panic disorder diagnosis was coded as “lifetime,” unless reported otherwise except for Perich et al. (62), where diagnosis was stated as comorbid. Comorbidity reported as based on DSM-IV criteria was grouped in current diagnosis (44).
Studies were included to the analysis regardless of inpatient-outpatient populations or current episode of BD or BD type. However, % of patients in a manic episode were coded for use as a covariable in the meta-regression analysis.
Studies from the same clinics and research groups were examined for overlapping data and differences in reporting. In cases where two studies were performed on the same dataset (for example, Stanley Foundation, Step-BD, NESARC or JORVI study samples), the study with the most up to date data and the largest sample size was used in the analysis. Two authors agreed to use which data should be used in the study. In cases where meta-regression variable was presented in one article overlapping with a more up to date study, this variable and the prevalence for that study were only included in the meta-regression analysis of that variable, but not in the overall prevalence analysis.
Only studies that included all DSM-IV anxiety disorders in “any anxiety disorder” classification were coded for this variable. In cases where the prevalence of each anxiety disorder was reported separately, data were not summed for “any anxiety disorder” considering the possibility of comorbidity of anxiety disorders. If a study did not report which anxiety disorders they included in the any anxiety disorder definition but stated diagnosing anxiety disorder based on DSM-IV, it was assumed that data presented the overall prevalence of all anxiety disorders. Prevalence of substance use disorder comorbidity in the sample included both alcohol and substance use disorders, and due to lack of definition both current and lifetime prevalence data of SUD were pooled together in the meta-analysis.
Statistical analyses
Meta-analysis and meta-regression analysis were conducted using the Comprehensive Meta-analysis software licensed to Koc University. First, a publication bias analysis was conducted by visualization of the Funnel plots, Egger's test (63) and the Begg-Mazumdar Kendall's tau (64). Heterogeneity was assessed with the I2 and Q statistic for each analysis. Secondly, we conducted a meta-analysis using a random effects model for all the studies that included data about an anxiety disorder diagnosis in all types of BD. Data were analyzed separately for lifetime and current comorbidity. Second, we conducted a meta-analysis on BD I and BD II subgroups.
The meta-regression analyses were conducted for measuring the effect of possible variables on the heterogeneity of included studies. These variables included % of BD I patients in the sample, mean age of the sample, % of patients married, % of patients in a manic episode during the assessment, % of patients with a history of psychosis, % with high school or higher education, % of females in the sample, duration of BD, age of BD onset, % of patients diagnosed with ADHD, % of patients with a substance use disorder and family history of BD. For both lifetime and current comorbidity analyses, we conducted a univariate regression with random-effects model using mixed effect regression (unrestricted maximum likelihood). We could not analyze the effect of family history of anxiety disorders due to lack of adequate number of studies.
Results
Description of the included studies
After identification, screening and eligibility assessments, data from 152 studies published between 1995 and 2015 were included in the study and data from 135 articles were used for meta-analysis and meta-regression studies after excluding studies with overlapping samples. Figure 1 shows the PRISMA flow of selected studies. Sample sizes ranged from 20 to 3,766. Data from 121 studies were used for prevalence and data from 130 studies were used for meta-regression calculations. Number of studies and total sample sizes of each variable are presented in Tables 1–4.
Table 1.
Lifetime comorbidity of anxiety disorders in bipolar disorder.
| Lifetime Comorbidity | No of studies | No of Patients | Prevalence % (CI) | Heterogeneity I2 | Cochran Q (p-value) | References |
|---|---|---|---|---|---|---|
| Any anxiety disorder | 39 | 13,409 | 40.5 (36.0–45.2) | 96.09 | 971.7 (p < 0.0001) | (13, 16, 17, 19, 22, 30, 34, 39, 40, 42, 46, 47, 51, 55, 56, 76, 89–111) |
| Panic disorder | 63 | 14,890 | 18.1 (15.8–20.5) | 93.2 | 906.6 (p < 0.0001) | (2, 9, 11, 13, 15–19, 22, 30, 32, 34, 38, 42, 46, 47, 52, 57, 76, 77, 83–85, 89–92, 95–100, 102, 103, 106, 107, 109, 112–136) |
| Obsessive Compulsive Disorder | 52 | 14,253 | 9.7 (7.9–11.9) | 92 | 633.62 (p < 0.0001) | (2, 9, 11, 14–17, 19, 22, 32, 34, 38, 41, 42, 46, 47, 57, 76, 83–85, 89–92, 95–100, 106, 107, 112, 115–117, 119, 120, 124, 125, 127–132, 134–136) |
| Social Anxiety Disorder | 51 | 14,806 | 13.5 (11.3–16) | 93.34 | 751 (p < 0.0001) | (2, 9, 11, 15–17, 19, 22, 34, 38, 42, 46, 47, 52, 57, 76, 77, 83, 84, 89–91, 95–97, 99, 100, 102, 103, 106, 107, 109, 115–117, 119, 120, 124, 125, 127–132, 134–139) |
| Generalized Anxiety Disorder | 42 | 10,285 | 13.3 (10.7–16.5) | 94.8 | 801.82 (p < 0.0001) | (11, 15–17, 19, 22, 25, 26, 32, 34, 38, 42, 46, 47, 52, 76, 77, 84, 89–91, 95–99, 102, 103, 106, 107, 109, 115, 116, 119, 123, 124, 128, 129, 132, 134, 136, 137) |
Risk of bias and quality assessment
Publication bias assessment by inspection of the funnel plot revealed symmetrical distribution of the included studies. Egger's regression test [intercept: −1.29 (−4.7, 2.1), p-value: 0.44] and Kendall's tau with continuity correction test (tau: −0.0108, p-value: 0.92) also did not indicate a publication bias when data from studies on BD and any anxiety disorder comorbidity are analyzed.
Heterogeneity of the studies were calculated for each analysis and are presented in Tables 1, 2. For each analysis, included studies showed significant heterogeneity. All subgroup analysis revealed at least moderate heterogeneity of the studies (I2 > 80%) and most subgroup analysis revealed high heterogeneity (I2 > 90%) of the included studies (Tables 1, 2).
Table 2.
Current comorbidity of anxiety disorders in bipolar disorder.
| Current Comorbidity | No of studies | No of Patients | Prevalence % (CI) | Heterogeneity I2 | Cochran Q (p-value) | References |
|---|---|---|---|---|---|---|
| Any anxiety disorder | 30 | 10,590 | 38.2 (32.8–43.9) | 96.1 | 742.35 (p < 0.0001) | (6, 10, 16, 17, 19, 21, 42, 49, 54, 76, 90, 92, 93, 97, 107, 114, 122, 140–152) |
| Panic disorder | 34 | 7,394 | 13.3 (10.8–16.3) | 90.9 | 363.9 (p < 0.0001) | (10, 16, 19, 21, 28, 31, 42, 43, 49, 54, 62, 76, 90, 92, 93, 107, 114, 122, 126, 140, 142–145, 147, 149, 152–159) |
| Obsessive compulsive disorder | 32 | 7,134 | 9.9 (7.9–12.4) | 87.9 | 258.2 (p < 0.0001) | (10, 16, 19, 21, 28, 41, 42, 49, 54, 62, 76, 84, 90, 92, 93, 107, 114, 122, 126, 140, 142–145, 147, 152–154, 156–158, 160) |
| Social anxiety disorder | 23 | 5,361 | 11.7 (8.6–15.8) | 93.3 | 326.8 (p < 0.0001) | (10, 16, 19, 21, 28, 42, 49, 54, 76, 90, 93, 107, 122, 126, 140, 142, 143, 145, 147, 152, 154, 155, 158) |
| Generalized anxiety disorder | 28 | 6,529 | 15.2 (11–20) | 95.4 | 590.78 (p < 0.0001) | (10, 16, 19, 21, 28, 31, 42, 49, 54, 62, 76, 90, 93, 107, 122, 126, 127, 140, 142, 145, 147, 152–154, 156–159) |
Prevalence of anxiety disorders in bipolar disorder
We found that any DSM lifetime anxiety disorder comorbidity in BD is 40.5%; panic disorder comorbidity is at 18.1%, generalized anxiety disorder 13.3%, social anxiety disorder 13.5% and obsessive compulsive disorder 9.7% (Table 1). Any DSM current anxiety disorder comorbidity in BD is 38.2%; generalized anxiety disorder comorbidity is at 15.2%, panic disorder 13.3%, social anxiety disorder 11.7% and obsessive compulsive disorder 9.9% (Table 2).
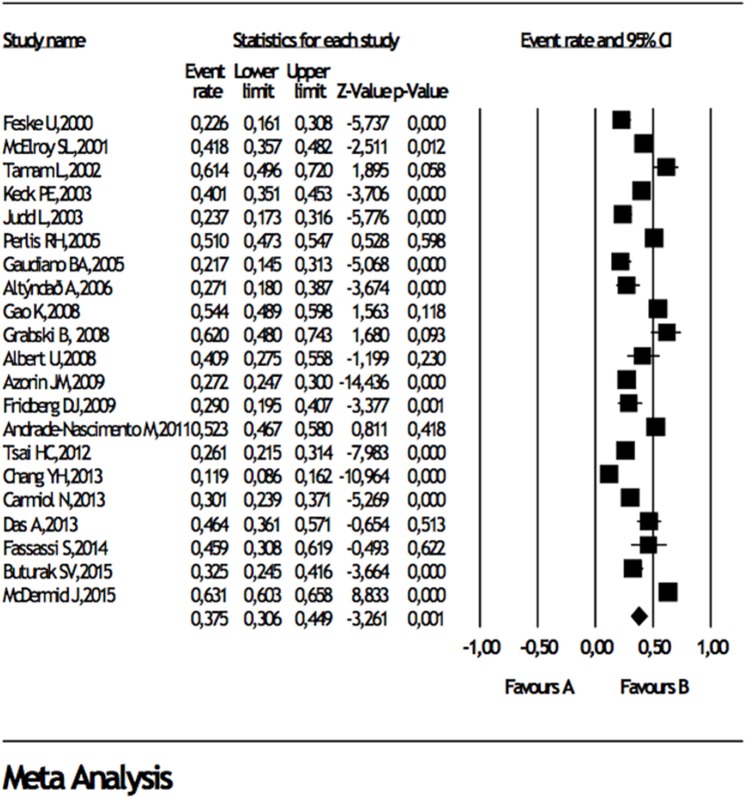
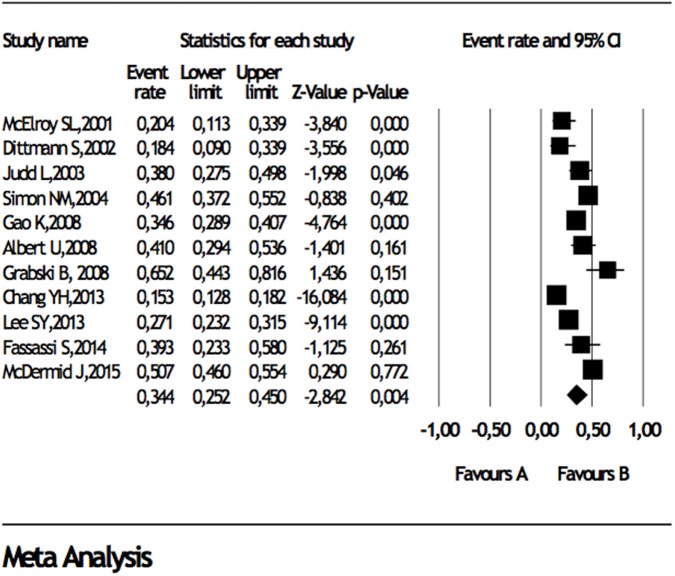
When studies reporting data about comorbidities in BD I or BD II were analyzed, separately, any DSM lifetime anxiety disorder comorbidity in BD I and BD II were 38 and 34%, panic disorder was 15 and 15%, generalized anxiety disorder was 14 and 16.6%, social anxiety disorder was 8 and 13%, obsessive compulsive disorder was 8% and 10%, respectively (Table 3), Forest plots for lifetime any anxiety disorder diagnosis in BD I and BD II are presented in Figure 2 and Figure 3, respectively. Any DSM current anxiety disorder comorbidity in BD I or BD II were 31 and 37%, panic disorder was 9 and 13%, generalized anxiety disorder was 8 and 12%, social anxiety disorder was 7 and 11%, and obsessive compulsive disorder was 8 and 7%, respectively (Table 4).
Table 3.
Lifetime comorbidity of anxiety disorders in bipolar disorder I and bipolar disorder II.
| Lifetime Comorbidity | BD I | BD II | ||||||
|---|---|---|---|---|---|---|---|---|
| No of studies | No of Patients | Prevalence % (CI) | References | No of studies | No of patients | Prevalence % (CI) | References | |
| Any anxiety disorder | 21 | 5,842 | 38 (31–45) | (13, 16, 17, 34, 42, 46, 51, 56, 76, 87, 90, 95, 98, 99, 101, 103, 105, 106, 109, 110, 161) | 11 | 2,171 | 34 (25–45) | (13, 27, 42, 55, 90, 98, 99, 105, 106, 109, 162) |
| Panic disorder | 26 | 5,831 | 15 (11–19) | (9, 11, 13, 16–18, 34, 42, 46, 52, 76, 84, 90, 95, 98, 99, 103, 106, 109, 112, 121, 125, 129, 134, 161, 163) | 15 | 1,823 | 15 (11–20) | (9, 11, 13, 27, 42, 52, 90, 98, 99, 106, 109, 121, 129, 136, 163) |
| Obsessive compulsive disorder | 21 | 4,133 | 8 (6–12) | (9, 11, 13, 16, 17, 34, 42, 46, 76, 84, 90, 95, 98, 99, 106, 112, 125, 129, 134, 161, 163) | 12 | 1,320 | 10 (7–14) | (9, 11, 13, 27, 42, 90, 98, 99, 106, 129, 136, 163) |
| Social anxiety disorder | 22 | 5,335 | 8 (6–12) | (9, 11, 13, 16, 17, 34, 42, 46, 52, 76, 84, 90, 95, 99, 103, 106, 109, 125, 129, 134, 161, 163) | 13 | 1,526 | 13 (9–16) | (9, 11, 13, 27, 42, 52, 90, 99, 106, 109, 129, 136, 163) |
| Generalized anxiety disorder | 20 | 4,968 | 14 (11–19) | (11, 13, 16, 17, 34, 42, 46, 52, 76, 84, 90, 95, 98, 99, 103, 106, 109, 129, 134, 161) | 12 | 1,516 | 16.6 (14–20) | (11, 13, 27, 42, 52, 90, 98, 99, 106, 109, 129, 136) |
Figure 2.
Forest plot for lifetime comorbidity of any anxiety disorder diagnosis in bipolar disorder I.
Figure 3.
Forest plot for lifetime comorbidity of any anxiety disorder diagnosis in bipolar disorder II.
Table 4.
Current comorbidity of anxiety disorders in bipolar disorder I and bipolar disorder II.
| Current Comorbidity | BD I | BD II | ||||||
|---|---|---|---|---|---|---|---|---|
| No of studies | No of Patients | Prevalence % (CI) | References | No of studies | No of Patients | Prevalence % (CI) | References | |
| Any anxiety disorder | 14 | 2,590 | 31 (24–39) | (16, 17, 21, 27, 29, 42, 76, 90, 93, 114, 143, 144, 150, 152) | 7 | 730 | 37 (26–48) | (27, 42, 90, 93, 114, 150, 152) |
| Panic disorder | 13 | 2,315 | 9 (6–14) | (16, 21, 27, 42, 76, 90, 93, 114, 143, 144, 152, 155, 158) | 6 | 651 | 13 (8–23) | (27, 42, 90, 93, 114, 152) |
| Obsessive compulsive disorder | 14 | 2,545 | 8 (5–13) | (16, 21, 27, 42, 76, 84, 90, 93, 114, 143, 144, 152, 153, 158) | 7 | 685 | 7 (3–15) | (27, 42, 90, 93, 114, 152, 153) |
| Social anxiety disorder | 10 | 2,153 | 7 (4–11) | (16, 27, 42, 76, 90, 93, 143, 152, 155, 158) | 5 | 544 | 11 (6–17) | (27, 42, 90, 93, 152) |
| Generalized anxiety disorder | 9 | 1,968 | 8 (4–14) | (16, 21, 27, 42, 76, 90, 93, 152, 158) | 5 | 544 | 12 (9–16) | (27, 42, 90, 93, 152) |
Meta-regression analysis
We conducted a univariate analysis using mixed effect regression (unrestricted maximum likelihood) analysis to explore the source of heterogeneity. We included many variables that may influence anxiety disorder - BD comorbidity and found that the percentage of patients in a manic episode in the sample significantly affected heterogeneity of the any anxiety disorder comorbidity in BD. This was true for both lifetime and current comorbidity (Z: −2.14 and Z: −2.02, p = 0.03 and p = 0.04, respectively) and there was also a trend for an inverse correlation for other lifetime anxiety disorders and significant negative correlations with current anxiety disorders as well. References for the studies used in meta-regression analysis of lifetime comorbidity are presented in supplementary Table 1 and references for the studies used in meta-regression analysis of current comorbidity are presented in supplementary Table 2.
The results of the univariate analysis for each covariate and anxiety disorder - BD lifetime and current comorbidity can be found in Tables 5, 6. Age of onset of BD tended to have a significant or near significant impact on other anxiety disorders as well (Z: −1.77, p = 0.076 for lifetime any anxiety disorder comorbidity, Z: −1.75, p = 0.08 for lifetime panic disorder comorbidity, Z: −1.52, p = 0.13 for lifetime panic disorder comorbidity, Z: −2.72, p = 0.006 for lifetime social anxiety disorder comorbidity, Z: −1.93, p = 0.053 for current any anxiety disorder, Z: −3.6, p = 0.0003 for current panic disorder comorbidity, Z: −1.73, p = 0.08 for current OCD comorbidity, Z: −3.85, p = 0.0001 for current SAD comorbidity). In addition, percentage of BD I patients significantly affected heterogeneity of the studies by decreasing the prevalence of panic disorder and social anxiety disorder (Z: −2.2, p = 0.026 and Z = −2.34, p = 0.019). Mean duration of illness and mean age of the study populations affected lifetime obsessive compulsive disorder comorbidity inversely (Z: −2.2, p = 0.02 and Z: −2.4, p = 0.01). However, mean duration of BD significantly predicted current panic disorder comorbidity (Z: 2.96, p = 0.003).% of patients with an ADHD diagnosis significantly predicted lifetime comorbidity of panic disorder (Z: 3.27 p = 0.001) and both lifetime and current OCD (Z: 3.17, p = 0.001, Z: 4.7, p < 0.00001). Here we note two of the stronger and intriguing findings from this table: first, the percentage of patients with a substance use disorder affected comorbidity of both current and lifetime social anxiety disorder (Z: 2.1, p = 0.03 and Z: 2.27, p = 0.02). In other words, a higher rate of substance use disorder was associated with greater BD—social anxiety disorder. Second, a history of psychotic features significantly affected current (but not lifetime) panic disorder and GAD (Z: −4.22, p = 0.00003 and Z: −2.94, p = 0.0003, respectively). In other words, BD patients with psychotic features tended to report lower rates of current BD—panic and generalized anxiety disorder comorbidity.
Table 5.
Analysis of possible associated features that may affect the heterogeneity of lifetime anxiety disorder comorbidity in bipolar disorder.
| Lifetime Comorbidity | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Any anxiety disorder | Panic disorder | Obsessive compulsive disorder | Social anxiety disorder | Generalized anxiety disorder | ||||||
| No of Studies | p-value | No of Studies | p-value | No of Studies | p-value | No of Studies | p-value | No of Studies | p-value | |
| % of BD I patients | 35 | 0.43 | 49 | 0.99 | 41 | 0.31 | 40 | 0.33 | 33 | 0.85 |
| Mean Age | 38 | 0.87 | 55 | 0.82 | 48 | 0.01 | 46 | 0.98 | 35 | 0.49 |
| % of Married patients | 17 | 0.07 | 23 | 0.25 | 18 | 0.60 | 22 | 0.52 | 17 | 0.65 |
| % of patients in a manic episode | 12 | 0.03 | 19 | 0.08 | 18 | 0.006 | 19 | 0.02 | 16 | 0.80 |
| % with a history of psychosis | 12 | 0.44 | 22 | 0.92 | 20 | 0.95 | 21 | 0.31 | 14 | 0.34 |
| % of high school and higher graduates | 7 | 0.28 | 10 | 0.22 | 8 | 0.28 | 9 | 0.30 | 8 | 0.17 |
| % of females | 37 | 0.91 | 54 | 0.07 | 46 | 0.48 | 45 | 0.87 | 35 | 0.38 |
| Duration of illness | 14 | 0.20 | 12 | 0.83 | 11 | 0.02 | 13 | 0.24 | 11 | 0.91 |
| Age of onset | 30 | 0.07 | 46 | 0.08 | 38 | 0.13 | 38 | 0.006 | 31 | 0.52 |
| % of patients with ADHD | 4 | 0.001 | 3 | 0.001 | 3 | 0.00002 | 3 | 0.9 | ||
| % of patients with SUD | 30 | 0.15 | 46 | 0.26 | 38 | 0.44 | 35 | 0.02 | 28 | 0.31 |
| Family history of BD | 7 | 0.1 | 10 | 0.05 | 9 | 0.74 | 9 | 0.56 | 6 | 0.72 |
The bold values indicate significant variables.
Table 6.
Analysis of possible associated features that may affect the heterogeneity of current anxiety disorder comorbidity in bipolar disorder.
| Current comorbidity | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Any anxiety disorder | Panic disorder | Obsessive compulsive disorder | Social anxiety disorder | Generalized anxiety disorder | ||||||
| No of studies | p-value | No of studies | p-value | No of studies | p-value | No of studies | p-value | No of studies | p-value | |
| % of BD I patients | 24 | 0.16 | 26 | 0.026 | 26 | 0.23 | 18 | 0.019 | 22 | 0.098 |
| Mean Age | 26 | 0.81 | 29 | 0.56 | 27 | 0.16 | 19 | 0.82 | 23 | 0.24 |
| % of Married patients | 13 | 0.63 | 12 | 0.41 | 12 | 0.84 | 9 | 0.64 | 11 | 0.25 |
| % of patients in a manic episode | 15 | 0.04 | 19 | 0.04 | 17 | 0.16 | 12 | 0.10 | 15 | 0.00005 |
| % with a history of psychosis | 6 | 0.61 | 9 | 0.00003 | 6 | 0.98 | 7 | 0.11 | 9 | 0.0003 |
| % of high school and higher graduates | 5 | 0.50 | 8 | 0.017 | 7 | 0.56 | 6 | 0.19 | 8 | 0.19 |
| % of females | 28 | 0.47 | 31 | 0.07 | 29 | 0.86 | 20 | 0.62 | 26 | 0.03 |
| Duration of illness | 8 | 0.53 | 10 | 0.003 | 9 | 0.52 | 9 | 0.45 | 10 | 0.09 |
| Age of onset | 20 | 0.05 | 22 | 0.0003 | 23 | 0.08 | 18 | 0.00011 | 19 | 0.16 |
| % of patients with ADHD | 4 | 0.90 | 4 | 0.0000 | 3 | 0.0000 | 4 | 0.35 | ||
| % of patients with SUD | 23 | 0.05 | 25 | 0.04 | 24 | 0.96 | 17 | 0.03 | 22 | 0.43 |
The bold values indicate significant variables.
Discussion
Design of the study
To our knowledge, this study is the most comprehensive and selective meta-analysis of anxiety disorder comorbidity in BD. Several design features distinguish our study from two recently published meta-analyses on a similar topic (65, 66), as follows. We accessed a very large number of published articles in this work and we examined studies with overlapping samples so as to include as much as unique data as possible. We discriminated reported current and lifetime prevalence of anxiety disorders in our analyses. We did not include studies that reported additive prevalence of subsets of anxiety disorders as “any anxiety disorder.” Also, though we noted these variables separately from all studies and used BD I proportion in the sample as a covariate, in case a study reported prevalences separately for BD I and other BD spectrums, we summed them all to model all BD group. Therefore, all BD group in this study does not stand for BD I alone as in Nabavi et al. (66). We also chose to define the current status of the patients as the percentage of patients in a manic episode, which distinguished our findings from the previous studies as Preti et al. (67) and Pavlova et al. (68). We believe these features provide a comprehensive look at the literature on this topic so far.
Prevalence of anxiety disorders in BD
We found that both lifetime and current anxiety disorder diagnosis are highly prevalent in BD patients. Generalized anxiety disorder and panic disorder are the most prevalent diagnoses, followed by social anxiety disorder and obsessive compulsive disorder. Our findings are in accordance with Nabavi et al. (66), but we found lower rates for anxiety disorders other than OCD, when compared to Pavlova et al. (65). Methodological differences, number of studies included in the analysis and data extraction methods are likely to be responsible for this variance. We also found that all anxiety disorder comorbidities are much higher than expected for the general population and even for disorders as schizophrenia (69, 70). This analysis continues to support a close association between bipolar disorder and anxiety disorders, above and beyond the usual associations seen between different kinds of psychopathology. There are likely to be shared environmental and neurobiological pathways for the co-occurrence of these two conditions. An anxiety disorder diagnosis may precede the diagnosis of BD, essentially as a prodromal feature (19). As environmental factors, early life adversities (71–73) and social rhytm disruptions (74) may all play a role for in both disorders and lead to increased HPA axis activity, which changes the excitability of the cortex and activation of relevant networks. In addition, amygdala, which is a core tuning center for both fear and reward networks that regulates emotion and anxiety is hyperactive in both disorders (74) which might predispose individuals to both anxiety symptoms and mood instability. Lastly, both disorders are associated with decreased executive functioning and prefrontal cortex activity, which may predispose to negative schema activation and decreased control and impaired perception over environmental concepts that includes both fear and social clues (74).
Lifetime and current anxiety-BD comorbidity
Because of the methodology and reported data categories of the included studies, studies included in the lifetime comorbidity analysis did not overlap with studies included in the current comorbidity analysis. Still, we found very consistent findings showing higher lifetime comorbidity compared to current comorbidity except for current GAD prevalance which was found to be higher than lifetime GAD comorbidity. Heterogeneity, sample size and used structural clinical interviews may have lead to this finding.
Comparison of BD I and BD II
In our meta-analysis, we found higher prevalence of anxiety disorders in BD II compared to BD I, except for lifetime any anxiety disorder diagnosis and a current OCD diagnosis. The increased lifetime prevalence of anxiety disorders in BD I may be due to higher rates of specific phobia or PTSD comorbidity in BD I which we did not analyze. There may also be a higher number of heterogeneous studies leading to this outcome for BD I. Our findings for anxiety disorder comorbidity in BD I vs. BD II are different from those of Pavlova et al. (65). In that paper, investigator pooled studies that concurrently include data for BD I and BD II to calculate a risk ratio for anxiety disorders. Here, we presented a prevalence analysis instead of a risk ratio calculation. We also conducted a meta-regression analysis to study the effect of BD I percentage in the sample on all studies for this purpose. This analysis can be thought as comparing BD I percentage to all other BD spectrum disorders. In this analysis, the proportion of BD I in the sample did not have a significant influence on the heterogeneity of lifetime comorbidity, but it did affect current panic and social anxiety disorder comorbidity. This finding indicates that the close relationship between BD and anxiety disorders is indeed seen across the bipolar spectrum with some modest differences between BD I and BD II. Nonetheless, the elevated rates of anxiety disorder comorbidity in BD II may be responsible for increased suicidality in this patient group (52).
Associated features of anxiety disorder comorbidity
Among the sociodemographic variables that we could included in the analysis, marital status of the patients did not influence either lifetime or current anxiety disorder comorbidity and educational level explained the heterogeneity for only current PD. Patients with a high school or higher education reported higher current panic disorder. For these two variables, we had dichotomized the variables to two groups while extracting the data from the articles for homogeneity, however this design may have limited our observation for a significant difference for the effect of these variables.
We found that age of onset is a significant covariate for anxiety disorder comorbidity. In our analysis, we took into account the mean age of onset for the sample. In a recent meta-analyses by Joslyn et al, data from 10 studies about the impact of early and adult onset of BD on severity measures of BD was examined and a 1.72-fold elevated anxiety disorder comorbidity risk was seen with earlier BD onset (75). The rest of the literature also supports the observation that early onset BD patients may be at higher risk of an anxiety disorder diagnosis (19, 30, 76, 77). Based on our findings, age of onset of bipolar disorder negatively correlates with almost all anxiety disorders. This finding may support the discussion that bipolar disorder patients may have subgroups based on the age of onset, where prevalance of anxiety disorders are higher in the earlier onsets, but may decrease with later onsets. Medications used for treatment and neurobiological changes related with age may lead to this finding. On the other hand, duration of illness mainly did not affect AD-BD comorbidity except for negatively correlation with lifetime OCD and positively correlation with current PD. Mean age of the sample was also not significant mostly. When findings about age of onset, duration of illness and mean age of the sample is combined, it can be concluded that the age of onset is a more significant determinant of anxiety disorder comorbidity compared to age of the participant and duration of illness.
The finding of elevated rates of anxiety disorder comorbidity in samples with higher proportion of patients in manic episode is intriguing. Percentage of patients in a manic episode significantly explained the heterogeneity of almost all lifetime and current anxiety disorders' comorbidity. Similarly, the proportion of patients with psychotic features affected rates of current (but not lifetime) panic and generalized anxiety disorder diagnoses. A history of psychosis is known to impart a worse outcome for BD (78) but it is not clear what the implication would be for a current anxiety disorder diagnosis. Patients experiencing mania or psychosis may be less likely to endorse anxiety symptoms, or to report them. We are not aware of a literature questioning the background of this finding.
Also, our findings highlight specific relationship between substance use disorders and social anxiety disorder comorbidity in BD. This relationship is reminiscent of the extensive literature on social anxiety and substance use disorder (79–81), and it is reassuring to observe it in our analysis. Lastly, even though the number of studies included in the analysis were very low because of the current published literature, ADHD comorbidity significantly increased reported anxiety disorders comorbidity. As discussed in the second discussion section, ADHD also shares common neurobiological pathways with anxiety and mood disorders on dysfunction of executive control and emotion regulation, studies assessing the ADHD-anxiety-mood disorders epidemiological significance and neurobiological overlaps are needed to clarify better treatment approaches to both disorders, as well.
Limitations of the study and current literature
Our study has some limitations. Most studies in our analysis are not population-based but rather recruited patients from outpatient or inpatient clinical services. In this context, they did not report a nonresponse rate, which reduces generalizability. Even though we tried to model clinical remission through the percentage of inpatients in the sample, our results may not be representative for intra-episode comorbidity. Most of the studies did not define what they meant by “current” disorder diagnosis except for Gao et al. (82). Studies mainly provided knowledge about mean age of onset (as opposed to a distribution), and this may not be reliable for most of the studies. Indeed, the age of onset definition varied across studies [e.g., (22, 83, 84)], define age of onset as the time point where the patient has enough symptoms to meet the diagnostic criteria of BD, whereas Edmonds et al. (85) defines as age at first professional contact, Goldstein and Levitt (86) defines as age of mania onset and Keck et al. (87) defines as age of first treatment. We did not have detailed data about educational levels in the samples, and therefore decided to generate a categorical variable of “high school or higher education.” Family history of anxiety disorder in the sample was not reported in most studies; we therefore could not include these variables in the regression analysis. Our meta-regression analysis is mainly a univariate analysis, which does not analyse the interaction of the various variables we assessed. Interaction of ADHD and SUD diagnosis on anxiety comorbidity and mood episodes of BD would be important to focus in new population studies.
Conclusion and future perspectives
The main findings of our study can be concluded as follows: 1: Anxiety disorder comorbidity is high in BD with somewhat lower rates in BD I vs. BD II, 2: Proportion of patients in a manic episode or with psychotic features influences anxiety disorder comorbidity, which may also explain lower rates in BD I, 3: Patients with an earlier age of BD onset report higher anxiety disorder comorbidity and age of onset for BD is a more important factor compared to duration of illness and current age for determining AD comorbidity, 4: Social anxiety comorbidity in BD is associated with substance use disorders, and 5: ADHD diagnosis in the population significantly influences anxiety disorder comorbidity.
Further research may analyze how current depressive and manic scores or suicidal ideation may change the diagnosis of current comorbidity of anxiety disorders and how the comorbidity of anxiety disorders may affect the treatment response. The effect of previous number of bipolar disorder episodes (both for manic, depressive or mixed states) or rapid cycling features, number of previous hospitalizations, lifetime suicide attempts, and association of anxiety disorder diagnosis with other comorbid medical diagnosis should also be studied. Anxiety disorders may also be related to different cognitive phenotypes when BD I and BD II are compared (44), role of anxiety disorders in clustering and subtyping of bipolar spectrum may be studied further. On the other hand, focusing on the neurobiology and shared environmental factors associated with AD and BD may pave the way for better future treatments. Finally, we need studies for the effect of medications on anxiety disorders comorbidity as seen in OCD-schizophrenia comorbidity (70, 88).
Author contributions
HY and DO have designed the study. HY, AK, CK, and MY have conducted the literature search and exclusion of the data. HY and AK conducted the statistical analysis. All authors contributed significantly to the discussion of the findings. HY, AK and DO wrote the manuscript. All authors approved the final version of the article.
Conflict of interest statement
DO was on a Scientific Advisory Board for Neurocrine Inc. in 2016. The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors gratefully acknowledge use of the services and facilities of the Koç University Research Center for Translational Medicine (KUTTAM), funded by the Republic of Turkey Ministry of Development. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Ministry of Development.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2018.00229/full#supplementary-material
References
- 1.Pini S, de Queiroz V, Pagnin D, Pezawas L, Angst J, Cassano GB, et al. Prevalence and burden of bipolar disorders in European countries. Eur Neuropsychopharmacol. (2005) 15:425–34. 10.1016/j.euroneuro.2005.04.011 [DOI] [PubMed] [Google Scholar]
- 2.Dilsaver SC, Benazzi F, Akiskal KK, Akiskal HS. Differential patterns of lifetime multiple anxiety disorder comorbidity between Latino adults with bipolar I and major depressive disorders. Bull Menninger Clin. (2008) 72:130–48. 10.1521/bumc.2008.72.2.130 [DOI] [PubMed] [Google Scholar]
- 3.Dilsaver SC, Akiskal HS, Akiskal KK, Benazzi F. Dose–response relationship between number of comorbid anxiety disorders in adolescent bipolar/unipolar disorders, and psychosis, suicidality, substance abuse and familiality. J Affect Disord. (2006) 96:249–58. 10.1016/j.jad.2006.07.008 [DOI] [PubMed] [Google Scholar]
- 4.Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry (2005) 62:617–27. 10.1001/archpsyc.62.6.617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Krishnan KRR. Psychiatric and medical comorbidities of bipolar disorder. Psychosomat Med. (2005) 67:1–8. 10.1097/01.psy.0000151489.36347.18 [DOI] [PubMed] [Google Scholar]
- 6.Asaad T, Okasha T, Ramy H, Fekry M, Zaki N, Azzam H, et al. Correlates of psychiatric co-morbidity in a sample of Egyptian patients with bipolar disorder. J Affect Disord. (2014) 166:347–52. 10.1016/j.jad.2014.04.050 [DOI] [PubMed] [Google Scholar]
- 7.Grant BF, Stinson FS, Hasin DS, Dawson DA, Chou SP, Ruan W, et al. Prevalence, correlates, and comorbidity of bipolar I disorder and axis I and II disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry (2005) 66:1205–15. 10.4088/JCP.v66n1001 [DOI] [PubMed] [Google Scholar]
- 8.Merikangas KR, Akiskal HS, Angst J, Greenberg PE, Hirschfeld RM, Petukhova M, et al. Lifetime and 12-month prevalence of bipolar spectrum disorder in the National Comorbidity Survey replication. Arch Gen Psychiatry (2007) 64:543–52. 10.1001/archpsyc.64.5.543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baek JH, Cha B, Moon E, Ha TH, Chang JS, Kim JH, et al. The effects of ethnic, social and cultural factors on axis I comorbidity of bipolar disorder: results from the clinical setting in Korea. J Affect Disord. (2014) 166:264–9. 10.1016/j.jad.2014.05.027 [DOI] [PubMed] [Google Scholar]
- 10.Paholpak S, Kongsakon R, Pattanakumjorn W, Kanokvut R, Wongsuriyadech W, Srisurapanont M. risk factors for an anxiety disorder comorbidity among Thai patients with bipolar disorder: results from the Thai Bipolar Disorder registry. Neuropsychiatr Dis Treat. (2014) 10:803. 10.2147/NDT.S57019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chang Y-H, Chen S-L, Chen S-H, Chu C-H, Lee S-Y, Yang H-F, et al. Low anxiety disorder comorbidity rate in bipolar disorders in Han Chinese in Taiwan. Prog Neuro-Psychopharmacol Biol Psychiatry (2012) 36:194–7. 10.1016/j.pnpbp.2011.09.013 [DOI] [PubMed] [Google Scholar]
- 12.Goldstein BI, Herrmann N, Shulman KI. Comorbidity in bipolar disorder among the elderly: results from an epidemiological community sample. Am J Psychiatry (2006) 163:319–21. 10.1176/appi.ajp.163.2.319 [DOI] [PubMed] [Google Scholar]
- 13.Judd LL, Akiskal HS, Schettler PJ, Coryell W, Maser J, Rice JA, et al. The comparative clinical phenotype and long term longitudinal episode course of bipolar I and II: a clinical spectrum or distinct disorders? J Affect Disord. (2003) 73:19–32. 10.1016/S0165-0327(02)00324-5 [DOI] [PubMed] [Google Scholar]
- 14.Chen Y-W, Dilsaver SC. Comorbidity for obsessive-compulsive disorder in bipolar and unipolar disorders. Psychiatry Res. (1995) 59:57–64. 10.1016/0165-1781(95)02752-1 [DOI] [PubMed] [Google Scholar]
- 15.Simon NM, Smoller JW, Fava M, Sachs G, Racette SR, Perlis R, et al. Comparing anxiety disorders and anxiety-related traits in bipolar disorder and unipolar depression. J Psychiatr Res. (2003) 37:187–92. 10.1016/S0022-3956(03)00021-9 [DOI] [PubMed] [Google Scholar]
- 16.Das A. Anxiety disorders in bipolar I mania: prevalence, effect on illness severity, and treatment implications. Indian J Psychol Med. (2013) 35:53. 10.4103/0253-7176.112202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gaudiano BA, Miller IW. Anxiety disorder comobidity in Bipolar I disorder: relationship to depression severity and treatment outcome. Depress Anxiety (2005) 21:71–7. 10.1002/da.20053 [DOI] [PubMed] [Google Scholar]
- 18.Toniolo RA, Caetano SC, da Silva PV, Lafer B. Clinical significance of lifetime panic disorder in the course of bipolar disorder type I. Compr Psychiatry (2009) 50:9–12. 10.1016/j.comppsych.2008.06.001 [DOI] [PubMed] [Google Scholar]
- 19.Zutshi A, Reddy YJ, Thennarasu K, Chandrashekhar C. Comorbidity of anxiety disorders in patients with remitted bipolar disorder. Eur Arch Psychiatry Clin Neurosci. (2006) 256:428–36. 10.1007/s00406-006-0658-2 [DOI] [PubMed] [Google Scholar]
- 20.Otto MW, Simon NM, Wisniewski SR, Miklowitz DJ, Kogan JN, Reilly-Harrington NA, et al. Prospective 12-month course of bipolar disorder in out-patients with and without comorbid anxiety disorders. Br J Psychiatry (2006) 189:20–5. 10.1192/bjp.bp.104.007773 [DOI] [PubMed] [Google Scholar]
- 21.Kim S-W, Berk L, Kulkarni J, Dodd S, de Castella A, Fitzgerald PB, et al. Impact of comorbid anxiety disorders and obsessive–compulsive disorder on 24-month clinical outcomes of bipolar I disorder. J Affect Disord. (2014) 166:243–8. 10.1016/j.jad.2014.05.017 [DOI] [PubMed] [Google Scholar]
- 22.Öngür D, Lin L, Cohen BM. Clinical characteristics influencing age at onset in psychotic disorders. Compr Psychiatry (2009) 50:13–9. 10.1016/j.comppsych.2008.06.002 [DOI] [PubMed] [Google Scholar]
- 23.Lee JH, Dunner DL. The effect of anxiety disorder comorbidity on treatment resistant bipolar disorders. Depress Anxiety (2008) 25:91–7. 10.1002/da.20279 [DOI] [PubMed] [Google Scholar]
- 24.Bauer MS, Altshuler L, Evans DR, Beresford T, Williford WO, Hauger R. Prevalence and distinct correlates of anxiety, substance, and combined comorbidity in a multi-site public sector sample with bipolar disorder. J Affect Disord. (2005) 85:301–15. 10.1016/j.jad.2004.11.009 [DOI] [PubMed] [Google Scholar]
- 25.Coryell W, Solomon DA, Fiedorowicz JG, Endicott J, Schettler PJ, Judd LL. Anxiety and outcome in bipolar disorder. Am J Psychiatry (2009) 166:1238–43. 10.1176/appi.ajp.2009.09020218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mantere O, Isometsä E, Ketokivi M, Kiviruusu O, Suominen K, Valtonen HM, et al. A prospective latent analyses study of psychiatric comorbidity of DSM-IV bipolar I and II disorders. Bipolar Disord. (2010) 12:271–84. 10.1111/j.1399-5618.2010.00810.x [DOI] [PubMed] [Google Scholar]
- 27.Simon NM, Otto MW, Wisniewski SR, Fossey M, Sagduyu K, Frank E, et al. Anxiety disorder comorbidity in bipolar disorder patients: data from the first 500 participants in the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD). Am J Psychiatry (2004) 161:2222–9. 10.1176/appi.ajp.161.12.2222 [DOI] [PubMed] [Google Scholar]
- 28.Nierenberg AA, Miyahara S, Spencer T, Wisniewski SR, Otto MW, Simon N, et al. Clinical and diagnostic implications of lifetime attention-deficit/hyperactivity disorder comorbidity in adults with bipolar disorder: data from the first 1000 STEP-BD participants. Biol Psychiatry (2005) 57:1467–73. 10.1016/j.biopsych.2005.01.036 [DOI] [PubMed] [Google Scholar]
- 29.Suttajit S, Paholpak S, Choovanicvong S, Kittiwattanagul K, Pratoomsri W, Srisurapanont M. Correlates of current suicide risk among Thai patients with bipolar I disorder: findings from the Thai Bipolar Disorder Registry. Neuropsychiatr Dis Treat. (2013) 9:1751. 10.2147/NDT.S52519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Moor S, Crowe M, Luty S, Carter J, Joyce PR. Effects of comorbidity and early age of onset in young people with Bipolar Disorder on self harming behaviour and suicide attempts. J Affect Disord. (2012) 136:1212–5. 10.1016/j.jad.2011.10.018 [DOI] [PubMed] [Google Scholar]
- 31.Neves FS, Malloy-Diniz LF, Corrêa H. Suicidal behavior in bipolar disorder: what is the influence of psychiatric comorbidities? J Clin Psychiatry (2009) 70:13–8. 10.4088/JCP.08m04037 [DOI] [PubMed] [Google Scholar]
- 32.Coryell W, Fiedorowicz JG, Solomon D, Leon AC, Rice JP, Keller MB. Effects of anxiety on the long-term course of depressive disorders. Br J Psychiatry (2012) 200:210–5. 10.1192/bjp.bp.110.081992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Azorin JM, Kaladjian A, Besnier N, Adida M, Hantouche EG, Lancrenon S, et al. “Folie circulaire” vs. “Folie à double forme”: contribution from a French national study. Eur Psychiatry (2011) 26:375–80. 10.1016/j.eurpsy.2009.12.025 [DOI] [PubMed] [Google Scholar]
- 34.Feske U, Frank E, Mallinger AG, Houck PR, Fagiolini A, Shear MK, et al. Anxiety as a correlate of response to the acute treatment of bipolar I disorder. Am J Psychiatry (2000) 157:956–62. 10.1176/appi.ajp.157.6.956 [DOI] [PubMed] [Google Scholar]
- 35.Weinstock LM, Gaudiano BA, Epstein-Lubow G, Tezanos K, Celis-deHoyos CE, Miller IW. Medication burden in bipolar disorder: a chart review of patients at psychiatric hospital admission. Psychiatry Res (2014) 216:24–30. 10.1016/j.psychres.2014.01.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Henry C, Van den Bulke D, Bellivier F, Etain B, Rouillon F, Leboyer M. Anxiety disorders in 318 bipolar patients: prevalence and impact on illness severity and response to mood stabilizer. J Clin Psychiatry (2003) 64:331–5. 10.4088/JCP.v64n0316 [DOI] [PubMed] [Google Scholar]
- 37.Taylor CT, Hirshfeld-Becker DR, Ostacher MJ, Chow CW, LeBeau RT, Pollack MH, et al. Anxiety is associated with impulsivity in bipolar disorder. J Anxiety Disord. (2008) 22:868–76. 10.1016/j.janxdis.2007.09.001 [DOI] [PubMed] [Google Scholar]
- 38.McElroy SL, Crow S, Biernacka JM, Winham S, Geske J, Barboza ABC, et al. Clinical phenotype of bipolar disorder with comorbid binge eating disorder. J Affect Disord. (2013) 150:981–6. 10.1016/j.jad.2013.05.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.McElroy SL, Frye MA, Hellemann G, Altshuler L, Leverich GS, Suppes T, et al. Prevalence and correlates of eating disorders in 875 patients with bipolar disorder. J Affect Disord. (2011) 128:191–8. 10.1016/j.jad.2010.06.037 [DOI] [PubMed] [Google Scholar]
- 40.Ostacher MJ, Nierenberg AA, Perlis RH, Eidelman P, Borrelli DJ, Tran TB, et al. The relationship between smoking and suicidal behavior, comorbidity, and course of illness in bipolar disorder. J Clin Psychiatry (2006) 67:1907–11. 10.4088/JCP.v67n1210 [DOI] [PubMed] [Google Scholar]
- 41.Magalhães PV, Kapczinski NS, Kapczinski F. Correlates and impact of obsessive-compulsive comorbidity in bipolar disorder. Compr Psychiatry (2010) 51:353–6. 10.1016/j.comppsych.2009.11.001 [DOI] [PubMed] [Google Scholar]
- 42.Albert U, Rosso G, Maina G, Bogetto F. Impact of anxiety disorder comorbidity on quality of life in euthymic bipolar disorder patients: differences between bipolar I and II subtypes. J Affect Disord. (2008) 105:297–303. 10.1016/j.jad.2007.05.020 [DOI] [PubMed] [Google Scholar]
- 43.Manenschijn L, Spijker AT, Koper JW, Jetten AM, Giltay EJ, Haffmans J, et al. Long-term cortisol in bipolar disorder: associations with age of onset and psychiatric co-morbidity. Psychoneuroendocrinology (2012) 37:1960–8. 10.1016/j.psyneuen.2012.04.010 [DOI] [PubMed] [Google Scholar]
- 44.Chang C-T, Chang Y-H, Wu JY-W, Lee S-Y, Chen S-L, Chen S-H, et al. Neuropsychological functions impairment in different subtypes of bipolar disorder with or without comorbid anxiety disorders. Psychiatry Res. (2012) 200:246–51. 10.1016/j.psychres.2012.06.012 [DOI] [PubMed] [Google Scholar]
- 45.Goldstein BI, Levitt AJ. Factors associated with temporal priority in comorbid bipolar I disorder and alcohol use disorders: results from the national epidemiologic survey on alcohol and related conditions. J Clin Psychiatry (2006) 67:643–9. 10.4088/JCP.v67n0416 [DOI] [PubMed] [Google Scholar]
- 46.Azorin JM, Kaladjian A, Adida M, Hantouche EG, Hameg A, Lancrenon S, et al. Psychopathological correlates of lifetime anxiety comorbidity in bipolar I patients: findings from a French national cohort. Psychopathology (2009) 42:380–6. 10.1159/000241193 [DOI] [PubMed] [Google Scholar]
- 47.Nery FG, Hatch JP, Glahn DC, Nicoletti MA, Monkul ES, Najt P, et al. Temperament and character traits in patients with bipolar disorder and associations with comorbid alcoholism or anxiety disorders. J Psychiatric Res. (2008) 42:569–77. 10.1016/j.jpsychires.2007.06.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Deckersbach T, Peters AT, Sylvia L, Urdahl A, Magalhães PV, Otto MW, et al. Do comorbid anxiety disorders moderate the effects of psychotherapy for bipolar disorder? Results from STEP-BD. Am J Psychiatry (2014) 171:178–86. 10.1176/appi.ajp.2013.13020225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hawke LD, Velyvis V, Parikh SV. Bipolar disorder with comorbid anxiety disorders: impact of comorbidity on treatment outcome in cognitive-behavioral therapy and psychoeducation. Int J Bipolar Disord. (2013) 1:15. 10.1186/2194-7511-1-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Malhi GS, Bargh DM, Cashman E, Frye MA, Gitlin M. The clinical management of bipolar disorder complexity using a stratified model. Bipolar Disord. (2012) 14:66–89. 10.1111/j.1399-5618.2012.00993.x [DOI] [PubMed] [Google Scholar]
- 51.Andrade-Nascimento M, Miranda-Scippa Â, Nery-Fernandes F, Kapczinski F, Quarantini LC. The identification of unipolar mania subtype based on anxiety comorbidity. J Affect Disord. (2011) 132:356–9. 10.1016/j.jad.2011.03.005 [DOI] [PubMed] [Google Scholar]
- 52.Rihmer Z, Szádóczky E, Füredi J, Kiss K, Papp Z. Anxiety disorders comorbidity in bipolar I, bipolar II and unipolar major depression: results from a population-based study in Hungary. J Affect Disord. (2001) 67:175–9. 10.1016/S0165-0327(01)00309-3 [DOI] [PubMed] [Google Scholar]
- 53.Kuiper S, McAulay C, McLean L, Malhi G. The relationship between bipolar disorders, anxiety, and trauma–implications for clinical practice. Aust. Psychiatry (2015) 23:378–81. 10.1177/1039856215588212 [DOI] [PubMed] [Google Scholar]
- 54.Kauer-Sant'Anna M, Frey BN, Andreazza AC, Ceresér KM, Gazalle FK, Tramontina J, et al. Anxiety comorbidity and quality of life in bipolar disorder patients. Can J Psychiatry (2007) 52:175–81. 10.1177/070674370705200309 [DOI] [PubMed] [Google Scholar]
- 55.Lee S-Y, Chen S-L, Wang Y-S, Chang Y-H, Huang S-Y, Tzeng N-S, et al. COMT and BDNF interacted in bipolar II disorder not comorbid with anxiety disorder. Behav Brain Res. (2013) 237:243–8. 10.1016/j.bbr.2012.09.039 [DOI] [PubMed] [Google Scholar]
- 56.Carmiol N, Peralta JM, Almasy L, Contreras J, Pacheco A, Escamilla MA, et al. Shared genetic factors influence risk for bipolar disorder and alcohol use disorders. Eur Psychiatry (2014) 29:282–7. 10.1016/j.eurpsy.2013.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Altshuler LL, Kupka RW, Hellemann G, Frye MA, Sugar CA, McElroy SL, et al. Gender and depressive symptoms in 711 patients with bipolar disorder evaluated prospectively in the Stanley Foundation bipolar treatment outcome network. Am J Psychiatry (2010) 167:708–15. 10.1176/appi.ajp.2009.09010105 [DOI] [PubMed] [Google Scholar]
- 58.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA (2000) 283:2008–12. 10.1001/jama.283.15.2008 [DOI] [PubMed] [Google Scholar]
- 59.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. (2009) 6:e1000097 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Dilsaver SC, Chen Y-W. Social phobia, panic disorder and suicidality in subjects with pure and depressive mania. J Affect Disord. (2003) 77:173–7. 10.1016/S0165-0327(02)00114-3 [DOI] [PubMed] [Google Scholar]
- 61.Dilsaver SC, Chen Y-W, Swann AC, Shoaib AM, Tsai-Dilsaver Y, Krajewski KJ. Suicidality, panic disorder and psychosis in bipolar depression, depressive-mania and pure-mania. Psychiatry Res. (1997) 73:47–56. [DOI] [PubMed] [Google Scholar]
- 62.Perich T, Mitchell PB, Loo C, Hadzi-Pavlovic D, Roberts G, Green M, et al. Cognitive styles and clinical correlates of childhood abuse in bipolar disorder. Bipolar Disord. (2014) 16:600–7. 10.1111/bdi.12212 [DOI] [PubMed] [Google Scholar]
- 63.Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ (1997) 315:629–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics (1994) 50:1088–101. [PubMed] [Google Scholar]
- 65.Pavlova B, Perlis RH, Alda M, Uher R. Lifetime prevalence of anxiety disorders in people with bipolar disorder: a systematic review and meta-analysis. Lancet Psychiatry (2015) 2:710–7. 10.1016/S2215-0366(15)00112-1 [DOI] [PubMed] [Google Scholar]
- 66.Nabavi B, Mitchell AJ, Nutt D. A lifetime prevalence of comorbidity between bipolar affective disorder and anxiety disorders: a meta-analysis of 52 interview-based studies of psychiatric population. Ebiomedicine (2015) 2:1405–19. 10.1016/j.ebiom.2015.09.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Preti A, Vrublevska J, Veroniki AA, Huedo-Medina TB, Fountoulakis KN. Prevalence, impact and treatment of generalised anxiety disorder in bipolar disorder: a systematic review and meta-analysis. Evid Based Mental Health (2016) 19:73–81. 10.1136/eb-2016-102412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Pavlova B, Perlis R, Mantere O, Sellgren C, Isometsä E, Mitchell P, et al. Prevalence of current anxiety disorders in people with bipolar disorder during euthymia: a meta-analysis. Psychol Med. (2017) 47:1107–15. 10.1017/S0033291716003135 [DOI] [PubMed] [Google Scholar]
- 69.Bandelow B, Michaelis S. Epidemiology of anxiety disorders in the 21st century. Dialogues Clin Neurosci. (2015) 17:327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Achim AM, Maziade M, Raymond É, Olivier D, Mérette C, Roy M-A. How prevalent are anxiety disorders in schizophrenia? A meta-analysis and critical review on a significant association. Schizophr Bull. (2009) 37:811–21. 10.1093/schbul/sbp148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Dualibe AL, Osório FL. Bipolar disorder and early emotional trauma: a critical literature review on indicators of prevalence rates and clinical outcomes. Harv Rev Psychiatry (2017) 25:198–208. 10.1097/HRP.0000000000000154 [DOI] [PubMed] [Google Scholar]
- 72.Coplan JD, Rozenboym AV, Fulton SL, Panthangi V, Tang J, Thiramangalakdi L, et al. Reduced left ventricular dimension and function following early life stress: a thrifty phenotype hypothesis engendering risk for mood and anxiety disorders. Neurobiol Stress (2017). 10.1016/j.ynstr.2017.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Cakir S, Tasdelen Durak R, Ozyildirim I, Ince E, Sar V. Childhood trauma and treatment outcome in bipolar disorder. J Trauma Dissoc. (2016) 17:397–409. 10.1080/15299732.2015.1132489 [DOI] [PubMed] [Google Scholar]
- 74.Iorfino F, Hickie IB, Lee RS, Lagopoulos J, Hermens DF. The underlying neurobiology of key functional domains in young people with mood and anxiety disorders: a systematic review. BMC Psychiatry (2016) 16:156. 10.1186/s12888-016-0852-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Joslyn C, Hawes DJ, Hunt C, Mitchell PB. Is age of onset associated with severity, prognosis, and clinical features in bipolar disorder? A meta-analytic review. Bipolar Disord. (2016) 18:389–403. 10.1111/bdi.12419 [DOI] [PubMed] [Google Scholar]
- 76.Tamam L, Ozpoyraz N. Comorbidity of anxiety disorder among patients with bipolar I disorder in remission. Psychopathology (2002) 35:203–9. 10.1159/000063824 [DOI] [PubMed] [Google Scholar]
- 77.Koyuncu A, Tükel R, Özyildirim I, Meteris H, Yazici O. Impact of obsessive-compulsive disorder comorbidity on the sociodemographic and clinical features of patients with bipolar disorder. Compr Psychiatry (2010) 51:293–7. 10.1016/j.comppsych.2009.07.006 [DOI] [PubMed] [Google Scholar]
- 78.Dell'Osso B, Camuri G, Cremaschi L, Dobrea C, Buoli M, Ketter TA, et al. Lifetime presence of psychotic symptoms in bipolar disorder is associated with less favorable socio-demographic and certain clinical features. Compr Psychiatry (2017) 76:169–76. 10.1016/j.comppsych.2017.04.005 [DOI] [PubMed] [Google Scholar]
- 79.Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, et al. Prevalence and co-occurrence of substance use disorders and independentmood and anxiety disorders: Results from the national epidemiologic survey on alcohol and relatedconditions. Arch Gen Psychiatry (2004) 61:807–16. 10.1001/archpsyc.61.8.807 [DOI] [PubMed] [Google Scholar]
- 80.Buckner JD, Schmidt NB, Lang AR, Small JW, Schlauch RC, Lewinsohn PM. Specificity of social anxiety disorder as a risk factor for alcohol and cannabis dependence. J Psychiatric Res. (2008) 42:230–9. 10.1016/j.jpsychires.2007.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Grant BF, Saha TD, Ruan WJ, Goldstein RB, Chou SP, Jung J, et al. Epidemiology of DSM-5 drug use disorder: results from the National Epidemiologic survey on alcohol and related conditions–III. JAMA Psychiatry (2016) 73:39–47. 10.1001/jamapsychiatry.2015.2132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Gao K, Wang Z, Chen J, Kemp DE, Chan PK, Conroy CM, et al. Should an assessment of Axis I comorbidity be included in the initial diagnostic assessment of mood disorders? Role of QIDS-16-SR total score in predicting number of Axis I comorbidity. J Affect Disord. (2013) 148:256–64. 10.1016/j.jad.2012.12.004 [DOI] [PubMed] [Google Scholar]
- 83.Schürhoff F, Bellivier F, Jouvent R, Mouren-Siméoni M-C, Bouvard M, Allilaire J-F, et al. Early and late onset bipolar disorders: two different forms of manic-depressive illness? J Affect Disord. (2000) 58:215–21. 10.1016/S0165-0327(99)00111-1 [DOI] [PubMed] [Google Scholar]
- 84.Strakowski SM, Sax KW, McElroy SL, Keck PE, Jr, Hawkins JM, West SA. Course of psychiatric and substance abuse syndromes co-occurring with bipolar disorder after a first psychiatric hospitalization. J Clin Psychiatry (1998) 59:465–71. [DOI] [PubMed] [Google Scholar]
- 85.Edmonds LK, Mosley BJ, Admiraal AJ, Olds RJ, Romans SE, Silverstone T, et al. Familial bipolar disorder: preliminary results from the Otago Familial Bipolar Genetic Study. Aust N Z J Psychiatry (1998) 32:823–9. [DOI] [PubMed] [Google Scholar]
- 86.Goldstein BI, Levitt AJ. The specific burden of comorbid anxiety disorders and of substance use disorders in bipolar I disorder. Bipolar Disord (2008) 10:67–78. 10.1111/j.1399-5618.2008.00461.x [DOI] [PubMed] [Google Scholar]
- 87.Keck PE, McElroy SL, Havens JR, Altshuler LL, Nolen WA, Frye MA, et al. Psychosis in bipolar disorder: phenomenology and impact on morbidity and course of illness. Compr Psychiatry (2003) 44:263–9. 10.1016/S0010-440X(03)00089-0 [DOI] [PubMed] [Google Scholar]
- 88.Swets M, Dekker J, van Emmerik-van Oortmerssen K, Smid GE, Smit F, de Haan L, et al. The obsessive compulsive spectrum in schizophrenia, a meta-analysis and meta-regression exploring prevalence rates. Schizophr Res. (2014) 152:458–68. 10.1016/j.schres.2013.10.033 [DOI] [PubMed] [Google Scholar]
- 89.Vieta E, Colom F, Martinez-Arán A, Benabarre A, Reinares M, Gastó C. Bipolar II disorder and comorbidity. Compr Psychiatry (2000) 41:339–43. 10.1053/comp.2000.9011 [DOI] [PubMed] [Google Scholar]
- 90.McElroy SL, Altshuler LL, Suppes T, Keck PE, Jr, Frye MA, Denicoff KD, et al. Axis I psychiatric comorbidity and its relationship to historical illness variables in 288 patients with bipolar disorder. Am J Psychiatry (2001) 158:420–6. 10.1176/appi.ajp.158.3.420 [DOI] [PubMed] [Google Scholar]
- 91.Perlis RH, Miyahara S, Marangell LB, Wisniewski SR, Ostacher M, DelBello MP, et al. Long-term implications of early onset in bipolar disorder: data from the first 1000 participants in the systematic treatment enhancement program for bipolar disorder (STEP-BD). Biol Psychiatry (2004) 55:875–81. 10.1016/j.biopsych.2004.01.022 [DOI] [PubMed] [Google Scholar]
- 92.Fenn HH, Bauer MS, Alshuler L, Evans DR, Williford WO, Kilbourne AM, et al. Medical comorbidity and health-related quality of life in bipolar disorder across the adult age span. J Affect Disord. (2005) 86:47–60. 10.1016/j.jad.2004.12.006 [DOI] [PubMed] [Google Scholar]
- 93.Mantere O, Melartin TK, Suominen K, Rytsälä HJ, Valtonen HM, Arvilommi P, et al. Differences in Axis I and II comorbidity between bipolar I and II disorders and major depressive disorder. J Clin. Psychiatry (2006) 67:584–93. 10.4088/JCP.v67n0409 [DOI] [PubMed] [Google Scholar]
- 94.Grunebaum MF, Galfalvy HC, Nichols CM, Caldeira NA, Sher L, Dervic K, et al. Aggression and substance abuse in bipolar disorder. Bipolar Disord. (2006) 8:496–502. 10.1111/j.1399-5618.2006.00349.x [DOI] [PubMed] [Google Scholar]
- 95.Altindag A, Yanik M, Nebioglu M. The comorbidity of anxiety disorders in bipolar I patients: prevalence and clinical correlates. Isr. J Psychiatry Relat. Sci. (2006) 43:10. [PubMed] [Google Scholar]
- 96.Perroud N, Baud P, Preisig M, Etain B, Bellivier F, Favre S, et al. Social phobia is associated with suicide attempt history in bipolar inpatients. Bipolar Disord. (2007) 9:713–21. 10.1111/j.1399-5618.2007.00471.x [DOI] [PubMed] [Google Scholar]
- 97.Nakagawa A, Grunebaum MF, Sullivan GM, Currier D, Ellis SP, Burke AK, et al. Comorbid anxiety in bipolar disorder: does it have an independent effect on suicidality? Bipolar Disord. (2008) 10:530–8. 10.1111/j.1399-5618.2008.00590.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Gao K, Tolliver BK, Kemp DE, Verduin ML, Ganocy SJ, Bilali S, et al. Differential interactions between comorbid anxiety disorders and substance use disorder in rapid cycling bipolar I or II disorder. J Affect Disord. (2008) 110:167–73. 10.1016/j.jad.2007.12.229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Grabski B, Dudek D, Datka W, Maczka G, Zieba A. Lifetime anxiety and substance use disorder comorbidity in bipolar disorder and its relationship to selected variables. Gender and bipolar subtype differences in comorbidity. Arch Psychiatry Psychother. (2008) 3:5–15. [Google Scholar]
- 100.Nwulia EA, Zandi PP, McInnis MG, DePaulo R, Jr, MacKinnon DF. Rapid switching of mood in families with familial bipolar disorder. Bipolar Disord. (2008) 10:597–606. 10.1111/j.1399-5618.2008.00600.x [DOI] [PubMed] [Google Scholar]
- 101.Fridberg DJ, Hetrick WP, Brenner CA, Shekhar A, Steffen AN, Malloy FW, et al. Relationships between auditory event-related potentials and mood state, medication, and comorbid psychiatric illness in patients with bipolar disorder. Bipolar Disord. (2009) 11:857–66. 10.1111/j.1399-5618.2009.00758.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Perich T, Manicavasagar V, Mitchell PB, Ball JR. Mindfulness, response styles and dysfunctional attitudes in bipolar disorder. J Affect Disord. (2011) 134:126–32. 10.1016/j.jad.2011.06.004 [DOI] [PubMed] [Google Scholar]
- 103.Tsai H-C, Lu M-K, Yang Y-K, Huang M-C, Yeh T-L, Chen W-J, et al. Empirically derived subgroups of bipolar I patients with different comorbidity patterns of anxiety and substance use disorders in Han Chinese population. J Affect Disord. (2012) 136:81–9. 10.1016/j.jad.2011.08.015 [DOI] [PubMed] [Google Scholar]
- 104.Drancourt N, Etain B, Lajnef M, Henry C, Raust A, Cochet B, et al. Duration of untreated bipolar disorder: missed opportunities on the long road to optimal treatment. Acta Psychiatr Scandinavica (2013) 127:136–44. 10.1111/j.1600-0447.2012.01917.x [DOI] [PubMed] [Google Scholar]
- 105.Chang Y-H, Lee S-Y, Chen S-L, Tzeng N-S, Wang T-Y, Lee IH, et al. Genetic variants of the BDNF and DRD3 genes in bipolar disorder comorbid with anxiety disorder. J Affect Disord. (2013) 151:967–72. 10.1016/j.jad.2013.08.017 [DOI] [PubMed] [Google Scholar]
- 106.Fassassi S, Vandeleur C, Aubry J-M, Castelao E, Preisig M. Prevalence and correlates of DSM-5 bipolar and related disorders and hyperthymic personality in the community. J Affect Disord. (2014) 167:198–205. 10.1016/j.jad.2014.06.004 [DOI] [PubMed] [Google Scholar]
- 107.Tasdemir A, Tamam L, Keskin N, Evlice YE. Assessment of co-morbidity of adult separation anxiety in patients with bipolar disorder. Nordic J Psychiatry (2016) 70:93–102. 10.3109/08039488.2015.1053098 [DOI] [PubMed] [Google Scholar]
- 108.Henry C, Etain B, Godin O, Dargel AA, Azorin J-M, Gard S, et al. Bipolar patients referred to specialized services of care: not resistant but impaired by sub-syndromal symptoms. Results from the FACE-BD cohort. Aust N Z J Psychiatry (2015) 49:898–905. 10.1177/0004867415585582 [DOI] [PubMed] [Google Scholar]
- 109.McDermid J, Sareen J, El-Gabalawy R, Pagura J, Spiwak R, Enns MW. Co-morbidity of bipolar disorder and borderline personality disorder: findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Compr Psychiatry (2015) 58:18–28. 10.1016/j.comppsych.2015.01.004 [DOI] [PubMed] [Google Scholar]
- 110.Buturak SV, Koçak OM. Effects of comorbid anxiety disorders on the course of bipolar disorder-I. Nordic J Psychiatry (2015) 69:552–6. 10.3109/08039488.2015.1014835 [DOI] [PubMed] [Google Scholar]
- 111.Azorin JM, Adida M, Belzeaux R. Predominant polarity in bipolar disorders: Further evidence for the role of affective temperaments. J Affect Disord. (2015) 182:57–63. 10.1016/j.jad.2015.04.037 [DOI] [PubMed] [Google Scholar]
- 112.Strakowski SM, Tohen M, Stoll AL, Faedda GL, Goodwin DC. Comorbidity in mania at first hospitalization. Am J Psychiatry (1992) 149:554–6. [DOI] [PubMed] [Google Scholar]
- 113.Chen Y-W, Dilsaver SC. Comorbidity of panic disorder in bipolar illness. Am J Psychiatry (1995) 152:280–2. [DOI] [PubMed] [Google Scholar]
- 114.MacKinnon DF, McMahon FJ, Simpson SG, McInnis MG, DePaulo JR. Panic disorder with familial bipolar disorder. Biol Psychiatry (1997) 42:90–5. [DOI] [PubMed] [Google Scholar]
- 115.Cosoff SJ, Julian Hafner R. The prevalence of comorbid anxiety in schizophrenia, schizoaffective disorder and bipolar disorder. Aust N Z J Psychiatry (1998) 32:67–72. [DOI] [PubMed] [Google Scholar]
- 116.Pini S, Dell'Osso L, Mastrocinque C, Marcacci G, Papasogli A, Vignoli S, et al. Axis I comorbidity in bipolar disorder with psychotic features. Br J Psychiatry (1999) 175:467–71. [DOI] [PubMed] [Google Scholar]
- 117.Rotondo A, Mazzanti C, Dell'Osso L, Rucci P, Sullivan P, Bouanani S, et al. Catechol o-methyltransferase, serotonin transporter, and tryptophan hydroxylase gene polymorphisms in bipolar disorder patients with and without comorbid panic disorder. Am J Psychiatry (2002) 159:23–9. 10.1176/appi.ajp.159.1.23 [DOI] [PubMed] [Google Scholar]
- 118.Pini S, Dell'Osso L, Amador XF, Mastrocinque C, Saettoni M, Cassano GB. Awareness of illness in patients with bipolar I disorder with or without comorbid anxiety disorders. Aust N Z J Psychiatry (2003) 37:355–61. 10.1046/j.1440-1614.2003.01188.x [DOI] [PubMed] [Google Scholar]
- 119.Slama F, Bellivier F, Henry C, Rousseva A, Etain B, Rouillon F, et al. Bipolar patients with suicidal behavior: toward the identification of a clinical subgroup. J Clin Psychiatry (2004) 65:1035–9. 10.4088/JCP.v65n0802 [DOI] [PubMed] [Google Scholar]
- 120.Joyce PR, Light KJ, Rowe SL, Kennedy MA. Bipolar disorder not otherwise specified: comparison with bipolar disorder I/II and major depression. Aust N Z J Psychiatry (2007) 41:843–9. 10.1080/00048670701579058 [DOI] [PubMed] [Google Scholar]
- 121.Mula M, Pini S, Monteleone P, Iazzetta P, Preve M, Tortorella A, et al. Different temperament and character dimensions correlate with panic disorder comorbidity in bipolar disorder and unipolar depression. J Anxiety Disord. (2008) 22:1421–6. 10.1016/j.janxdis.2008.02.004 [DOI] [PubMed] [Google Scholar]
- 122.Kennedy SH, McIntyre R, O'Donovan C, Milev R, Melledo J, Bisserbe J, et al. Frequency and Correlates of Gambling Problems in Depressed and Bipolar Outpatients. Belleville, ON: Mood Disorders Society of Canada; (2008). [Google Scholar]
- 123.Biffin F, Tahtalian S, Filia K, Fitzgerald PB, De Castella AR, Filia S, et al. The impact of age at onset of bipolar I disorder on functioning and clinical presentation. Acta Neuropsychiatr. (2009) 21:191–6. 10.1111/j.1601-5215.2009.00399.x [DOI] [PubMed] [Google Scholar]
- 124.Nery-Fernandes F, Quarantini LC, Galvão-De-Almeida A, Rocha MV, Kapczinski F, Miranda-Scippa Â. Lower rates of comorbidities in euthymic bipolar patients. World J Biol Psychiatry (2009) 10:474–9. 10.1080/15622970802688929 [DOI] [PubMed] [Google Scholar]
- 125.Perugi G, Medda P, Reis J, Rizzato S, Mariani MG, Mauri M. Clinical subtypes of severe bipolar mixed states. J Affect Disord. (2013) 151:1076–82. 10.1016/j.jad.2013.08.037 [DOI] [PubMed] [Google Scholar]
- 126.McIntyre RS, Kennedy SH, Soczynska JK, Nguyen HT, Bilkey TS, Woldeyohannes HO, et al. Attention-deficit/hyperactivity disorder in adults with bipolar disorder or major depressive disorder: results from the international mood disorders collaborative project. Prim Care Companion J Clin Psychiatry (2010) 12:e1–e7. 10.4088/PCC.09m00861gry [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Ortiz A, Cervantes P, Zlotnik G, Van De Velde C, Slaney C, Garnham J, et al. Cross-prevalence of migraine and bipolar disorder. Bipolar Disord. (2010) 12:397–403. 10.1111/j.1399-5618.2010.00832.x [DOI] [PubMed] [Google Scholar]
- 128.Parmentier C, Etain B, Yon L, Misson H, Mathieu F, Lajnef M, et al. Clinical and dimensional characteristics of euthymic bipolar patients with or without suicidal behavior. Eur Psychiatry (2012) 27:570–6. 10.1016/j.eurpsy.2011.05.005 [DOI] [PubMed] [Google Scholar]
- 129.Ibiloglu AO, Caykoylu A. The comorbidity of anxiety disorders in bipolar I and bipolar II patients among Turkish population. J Anxiety Disord. (2011) 25:661–7. 10.1016/j.janxdis.2011.02.008 [DOI] [PubMed] [Google Scholar]
- 130.Goes F, McCusker M, Bienvenu O, Mackinnon D, Mondimore F, Schweizer B, et al. Co-morbid anxiety disorders in bipolar disorder and major depression: familial aggregation and clinical characteristics of co-morbid panic disorder, social phobia, specific phobia and obsessive-compulsive disorder. Psychol Med. (2012) 42:1449–59. 10.1017/S0033291711002637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Mantere O, Suominen K, Valtonen HM, Arvilommi P, Leppämäki S, Paunio T, et al. Concomitants of family histories of mood disorders and alcoholism in a clinical cohort of patients with bipolar I and II disorder. J Nerv Mental Dis. (2012) 200:388–94. 10.1097/NMD.0b013e3182531f2e [DOI] [PubMed] [Google Scholar]
- 132.Mitchell P, Johnston AK, Frankland A, Slade T, Green M, Roberts G, et al. Bipolar disorder in a national survey using the World Mental Health Version of the composite international diagnostic interview: the impact of differing diagnostic algorithms. Acta Psychiatr Scandinavica (2013) 127:381–93. 10.1111/acps.12005 [DOI] [PubMed] [Google Scholar]
- 133.Young S, Pfaff D, Lewandowski KE, Ravichandran C, Cohen BM, Öngür D. Anxiety disorder comorbidity in bipolar disorder, schizophrenia and schizoaffective disorder. Psychopathology (2012) 46:176–85. 10.1159/000339556 [DOI] [PubMed] [Google Scholar]
- 134.Perugi G, Toni C, Maremmani I, Tusini G, Ramacciotti S, Madia A, et al. The influence of affective temperaments and psychopathological traits on the definition of bipolar disorder subtypes: a study on bipolar I Italian national sample. J Affect Disord. (2012) 136:e41–e9. 10.1016/j.jad.2009.12.027 [DOI] [PubMed] [Google Scholar]
- 135.Jen A, Saunders EFH, Ornstein RM, Kamali M, McInnis MG. Impulsivity, anxiety, and alcohol misuse in bipolar disorder comorbid with eating disorders. Int J Bipolar Disord. (2013) 1:13. 10.1186/2194-7511-1-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Fornaro M, De Berardis D, Iasevoli F, Pistorio ML, D'Angelo E, Mungo S, et al. Treatment adherence towards prescribed medications in bipolar-II acute depressed patients: relationship with cyclothymic temperament and “therapeutic sensation seeking” in response towards subjective intolerance to pain. J Affect Disord. (2013) 151:596–604. 10.1016/j.jad.2013.07.004 [DOI] [PubMed] [Google Scholar]
- 137.Goodwin RD, Hoven CW. Bipolar–panic comorbidity in the general population: prevalence and associated morbidity. J Affect Disord. (2002) 70:27–33. 10.1016/S0165-0327(01)00398-6 [DOI] [PubMed] [Google Scholar]
- 138.Ciapparelli A, Paggini R, Marazziti D, Carmassi C, Bianchi M, Taponecco C, et al. Comorbidity with axis I anxiety disorders in remitted psychotic patients 1 year after hospitalization. CNS Spectrums (2007) 12:913–9. 10.1017/S1092852900015704 [DOI] [PubMed] [Google Scholar]
- 139.Fournier JC, Cyranowski JM, Rucci P, Cassano GB, Frank E. The multiple dimensions of the social anxiety spectrum in mood disorders. J Psychiatr Res. (2012) 46:1223–30. 10.1016/j.jpsychires.2012.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Pini S, Cassano GB, Simonini E, Savino M, Russo A, Montgomery SA. Prevalence of anxiety disorders comorbidity in bipolar depression, unipolar depression and dysthymia. J Affect Disord. (1997) 42:145–53. [DOI] [PubMed] [Google Scholar]
- 141.Carter TDC, Mundo E, Parikh SV, Kennedy JL. Early age at onset as a risk factor for poor outcome of bipolar disorder. J Psychiatr Res. (2003) 37:297–303. 10.1016/S0022-3956(03)00052-9 [DOI] [PubMed] [Google Scholar]
- 142.MacQueen GM, Marriott M, Begin H, Robb J, Joffe RT, Young LT. Subsyndromal symptoms assessed in longitudinal, prospective follow-up of a cohort of patients with bipolar disorder. Bipolar Disord. (2003) 5:349–55. 10.1034/j.1399-5618.2003.00048.x [DOI] [PubMed] [Google Scholar]
- 143.Pashinian A, Faragian S, Levi A, Yeghiyan M, Gasparyan K, Weizman R, et al. Obsessive–compulsive disorder in bipolar disorder patients with first manic episode. J Affect Disord. (2006) 94:151–6. 10.1016/j.jad.2006.03.022 [DOI] [PubMed] [Google Scholar]
- 144.Benedetti A, Fagiolini A, Casamassima F, Mian MS, Adamovit A, Musetti L, et al. Gender differences in bipolar disorder type 1: a 48-week prospective follow-up of 72 patients treated in an Italian tertiary care center. J Nerv Mental Dis. (2007) 195:93–6. 10.1097/01.nmd.0000243781.67035.b1 [DOI] [PubMed] [Google Scholar]
- 145.Zimmerman M, Galione JN, Chelminski I, Young D, Dalrymple K, Ruggero CJ. Sustained unemployment in psychiatric outpatients with bipolar disorder: frequency and association with demographic variables and comorbid disorders. Bipolar Disord. (2010) 12:720–6. 10.1111/j.1399-5618.2010.00869.x [DOI] [PubMed] [Google Scholar]
- 146.Watson HJ, Swan A, Nathan PR. Psychiatric diagnosis and quality of life: the additional burden of psychiatric comorbidity. Compr Psychiatry (2011) 52:265–72. 10.1016/j.comppsych.2010.07.006 [DOI] [PubMed] [Google Scholar]
- 147.Bellani M, Hatch JP, Nicoletti MA, Ertola AE, Zunta-Soares G, Swann AC, et al. Does anxiety increase impulsivity in patients with bipolar disorder or major depressive disorder? J Psychiatr Res. (2012) 46:616–21. 10.1016/j.jpsychires.2012.01.016 [DOI] [PubMed] [Google Scholar]
- 148.Magalhães PV, Kapczinski F, Nierenberg AA, Deckersbach T, Weisinger D, Dodd S, et al. Illness burden and medical comorbidity in the systematic treatment enhancement program for bipolar disorder. Acta Psychiatr Scandinavica (2012) 125:303–8. 10.1111/j.1600-0447.2011.01794.x [DOI] [PubMed] [Google Scholar]
- 149.Bobo WV, Reilly-Harrington NA, Ketter TA, Brody BD, Kinrys G, Kemp DE, et al. Effect of adjunctive benzodiazepines on clinical outcomes in lithium-or quetiapine-treated outpatients with bipolar I or II disorder: results from the Bipolar CHOICE trial. J Affect Disord. (2014) 161:30–5. 10.1016/j.jad.2014.02.046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Dervic K, Garcia-Amador M, Sudol K, Freed P, Brent D, Mann J, et al. Bipolar I and II versus unipolar depression: clinical differences and impulsivity/aggression traits. Eur Psychiatry (2015) 30:106–13. 10.1016/j.eurpsy.2014.06.005 [DOI] [PubMed] [Google Scholar]
- 151.Sylvia LG, Thase ME, Reilly-Harrington NA, Salcedo S, Brody B, Kinrys G, et al. Psychotherapy use in bipolar disorder: Association with functioning and illness severity. Aust N Z J Psychiatry (2015) 49:453–61. 10.1177/0004867415569803 [DOI] [PubMed] [Google Scholar]
- 152.Angst J, Gamma A, Bowden C, Azorin J, Perugi G, Vieta E, et al. Evidence-based definitions of bipolar-I and bipolar-II disorders among 5,635 patients with major depressive episodes in the Bridge Study: validity and comorbidity. Eur Arch Psychiatry Clin Neurosci. (2013) 263:663–73. 10.1007/s00406-013-0393-4 [DOI] [PubMed] [Google Scholar]
- 153.Krüger S, Bräunig P, Cooke RG. Comorbidity of obsessive-compulsive disorder in recovered inpatients with bipolar disorder. Bipolar Disord. (2000) 2:71–4. 10.1034/j.1399-5618.2000.020111.x [DOI] [PubMed] [Google Scholar]
- 154.Mitchell PB, Slade T, Andrews G. Twelve-month prevalence and disability of DSM-IV bipolar disorder in an Australian general population survey. Psychol Med. (2004) 34:777–85. 10.1017/S0033291703001636 [DOI] [PubMed] [Google Scholar]
- 155.Vieta E, Colom F, Corbella B, Martínez-Arán A, Reinares M, Benabarre A, et al. Clinical correlates of psychiatric comorbidity in bipolar I patients. Bipolar Disord. (2001) 3:253–8. 10.1034/j.1399-5618.2001.30504.x [DOI] [PubMed] [Google Scholar]
- 156.Dell'Osso B, Buoli M, Bortolussi S, Camuri G, Vecchi V, Altamura AC. Patterns of Axis I comorbidity in relation to age in patients with Bipolar Disorder: a cross-sectional analysis. J Affect Disord. (2011) 130:318–22. 10.1016/j.jad.2010.10.008 [DOI] [PubMed] [Google Scholar]
- 157.Karaahmet E, Konuk N, Dalkilic A, Saracli O, Atasoy N, Kurçer MA, et al. The comorbidity of adult attention-deficit/hyperactivity disorder in bipolar disorder patients. Compr Psychiatry (2013) 54:549–55. 10.1016/j.comppsych.2012.11.005 [DOI] [PubMed] [Google Scholar]
- 158.Shashidhara M, Sushma B, Viswanath B, Math SB, Reddy YJ. Comorbid obsessive compulsive disorder in patients with bipolar-I disorder. J Affect Disord. (2015) 174:367–71. 10.1016/j.jad.2014.12.019 [DOI] [PubMed] [Google Scholar]
- 159.Couto T, Neves FS, Machado M, Vasconcelos AG, Correa H, Malloy-Diniz LF. Assessment of impulsivity in bipolar disorder (BD) in comorbidity with generalized anxiety disorder (GAD): revisiting the hypothesis of protective effect. Clin Neuropsychiatry (2012) 9:102–6. [Google Scholar]
- 160.McElroy SL, Strakowski SM, Keck PE, Tugrul KL, West SA, Lonczak HS. Differences and similarities in mixed and pure mania. Compr Psychiatry (1995) 36:187–94. [DOI] [PubMed] [Google Scholar]
- 161.Perlis RH, Delbello MP, Miyahara S, Wisniewski SR, Sachs GS, Nierenberg AA. Revisiting depressive-prone bipolar disorder: polarity of initial mood episode and disease course among bipolar I systematic treatment enhancement program for bipolar disorder participants. Biological Psychiatry (2005) 58:549–53. 10.1016/j.biopsych.2005.07.029 [DOI] [PubMed] [Google Scholar]
- 162.Dittmann S, Biedermann NC, Grunze H, Hummel B, Schärer LO, Kleindienst N, et al. The Stanley Foundation Bipolar Network: results of the naturalistic follow-up study after 2.5 years of follow-up in the German centres. Neuropsychobiology (2003) 46(Suppl. 1):2–9. 10.1159/000068018 [DOI] [PubMed] [Google Scholar]
- 163.Levander E, Frye MA, McElroy S, Suppes T, Grunze H, Nolen WA, et al. Alcoholism and anxiety in bipolar illness: differential lifetime anxiety comorbidity in bipolar I women with and without alcoholism. J Affect Disord. (2007) 101:211–7. 10.1016/j.jad.2006.11.023 [DOI] [PubMed] [Google Scholar]
- 164.Lembke A, Miklowitz DJ, Otto MW, Zhang H, Wisniewski SR, Sachs GS, et al. Psychosocial service utilization by patients with bipolar disorders: data from the first 500 participants in the Systematic Treatment Enhancement Program. J Psychiatr Pract. (2004) 10:81–7. 10.1097/00131746-200403000-00002 [DOI] [PubMed] [Google Scholar]
- 165.Leverich GS, Post RM, Keck PE, Altshuler LL, Frye MA, Kupka RW, et al. The poor prognosis of childhood-onset bipolar disorder. J Pediatr. (2007) 150:485–90. 10.1016/j.jpeds.2006.10.070 [DOI] [PubMed] [Google Scholar]
- 166.Valtonen HM, Suominen K, Haukka J, Mantere O, Arvilommi P, Leppämäki S, et al. Hopelessness across phases of bipolar I or II disorder: a prospective study. J Affect Disord. (2009) 115:11–7. 10.1016/j.jad.2008.06.013 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.