Abstract
Smoking is one of the primary causes of chronic obstructive pulmonary disease (COPD). Sustained active epithelial-mesenchymal transition (EMT) in COPD may explain the core pathophysiology of airway fibrosis and why lung cancer is so common among smokers. Interleukin (IL)-17A and growth/differentiation factor (GDF)15 have been reported to be biomarkers of COPD; however, the role of IL-17A and GDF15 in EMT remains unclear. The aim of the present study was to investigate the role of IL-17A and GDF15 in the pathogenesis of COPD. It was demonstrated that IL-17A and GDF15 are upregulated in patients with COPD, particularly those with a history of smoking. The results also revealed that IL-17A and GDF15 expression was negatively correlated with the epithelial marker epithelial-cadherin and positively correlated with the mesenchymal marker vimentin. Furthermore, treatment with cigarette smoke extract or IL-17A induced GDF15 expression. Combined treatment with IL-17A and GDF15 induced EMT in human small epithelial HSAEpiC cells in vitro. Collectively, the results of the present study suggest that IL-17A and GDF15-induced EMT serves an important role in the pathology of COPD.
Keywords: chronic obstructive pulmonary disease, epithelial-mesenchymal transition, interleukin, growth/differentiation factor
Introduction
Chronic obstructive pulmonary disease (COPD), which is characterised by poor reversible airflow limitation, is a major chronic lung disease and a global health problem (1,2). The alveolar response to noxious substances, including cigarette smoke, is considered to be a risk factor for the development of COPD (3); however, the underlying molecular mechanisms remain to be elucidated. Airway fibrosis has been reported to contribute to physiological airway dysfunction in COPD (4). Previous studies have suggested that epithelial-mesenchymal transition (EMT), a feature of lung fibrosis, may be important for the development of COPD (5–8). De-differentiation of the respiratory epithelium occurs via active EMT, however the underlying mechanism and the association between EMT and peribronchial fibrosis remain unclear (9). It was therefore hypothesised that de-differentiation of the COPD respiratory epithelium via EMT may serve a role in airway fibrosis and thereby in airway obstruction.
It has been reported that the airway epithelium provides frontline innate defence mechanisms as a physical barrier and via the secretion of protective factors. Interleukin (IL)-17A is an important cytokine that serves a vital role in a number of chronic inflammatory diseases (10,11). Previous studies have reported a greater number of IL-17A+ cells and increased IL-17A secretion in the submucosa of patients with COPD (12–14) and have also investigated the expression of IL-17A and IL-17F in the lung tissues of patients with stable COPD (15). Increased levels of growth differentiation factor 15 (GDF15) have been reported in the airway epithelium of smokers with COPD and in human airway epithelial cells exposed to cigarette smoke; as such, elevated GDF15 expression may contribute to the progression of COPD.
The aim of the present study was to elucidate the role of IL-17A and GDF15 in the pathogenesis of COPD. The results demonstrated that IL-17A and GDF15 are upregulated in patients with COPD, particularly in those with a history of smoking. IL-17A and GDF15 expression is negatively correlated with epithelial (E)-cadherin levels and positively correlated with the mesenchymal marker vimentin in clinical specimens. The results also revealed that treatment with cigarette smoke extract (CSE) and IL-17A was able to induce GDF15 expression, while increased IL-17A and GDF15 expression caused a corresponding increase in EMT in human small epithelial HSAEpiC cells in vitro. The results of the present study demonstrate that IL-17A and GDF15-induced EMT serves an important role in the pathology of COPD.
Materials and methods
Patients
A total of 143 patients with COPD (57 non-smokers, 86 smokers) and 75 patients without COPD (45 non-smokers, 30 smokers) were recruited from Hunan Provincial People's Hospital during (Changsha, Hunan Province, China) from March 2014 to September 2016. Patients were excluded from the present study if they exhibited acute and chronic pulmonary diseases, including bronchial asthma, bronchiectasis, interstitial lung disease, heart disease and autoimmune disease. Patients were also excluded if they possessed other systemic disorders, including orthopedic, neurologic or unstable cardiac diseases, which may interfere with results. Patients were recruited into the present study if they had not received glucocorticoid and antibiotics within the last 3 months. A total of 99 male and 44 female patients with COPD and average age of 56.4 years (range, 39–74 years) were recruited. In addition, 43 male and 32 female patients without COPD were recruited (average age, 52.5 years; range, 33–72 years). Lung tissue samples were obtained following lobectomy or pneumonectomy for various medical reasons, including solitary pulmonary nodules, peripheral space-occupying lesions and peripheral lung cancer. COPD was diagnosed according to the guidelines of the Global Initiative for Chronic Obstructive Lung Disease (16) as follows: Non-COPD, forced expiratory volume in 1 sec (FEV1)/forced vital capacity (FVC) ≥70% and FEV1 ≥70%; COPD, FEV1/FVC <70% and FEV1 <70%. Patients with a history of any other significant respiratory diseases were excluded. Non-smokers were defined as those who had smoked on average <1 cigarette/day for <1 year or had never smoked. Smokers were defined as patients who had a smoking history of ≥1 year and had smoked on average ≥300 cigarettes/year. None of the patients received corticosteroids prior to surgery. All experiments were approved by the Ethics Committee of Hunan Provincial People's Hospital and informed consent was obtained from all patients prior to specimen collection.
Immunohistochemistry
Immunohistochemical (IHC) staining for IL-17A and GDF15 proteins was performed using the labeled streptavidin-biotin method with an LSAB kit (Dako; Agilent Technologies, Inc., Santa Clara, CA, USA) according to the manufacturer's protocol. Surgical specimens were fixed using 10% neutral-buffered formalin. Following fixation for 24–48 h at room temperature, an initial 3–5 mm thick section was routinely processed, paraffin embedded, deparaffinized and rehydrated. 5-µm sections were then cut, placed on charged slides and dried in an oven for 1 h at 56–60°C. Sections were then stored in the dark at 2–8°C and used for the IHC assay. Sections were then immersed in 0.01 Mcitric buffer (pH 6.0) and preheated to 97°C, for 30 min. The slides were incubated with 3% hydrogen peroxide for 10 min at room temperature, followed by incubation in normal goat serum (cat. no. ab7481; Abcam, Cambridge, UK) for 10 min at room temperature. The slides were incubated with antibodies against IL-17A (ab217359; 1:200) and GDF15 (ab206414; 1:100; both Abcam) at 37°C for 1 h, followed by incubation in Biotin-SP (long spacer) AffiniPure Goat Anti-Rabbit Immunoglobulin G (IgG; 1:2,000; cat. no. 111-065-008; Jackson ImmunoResearch Laboratories, Inc., West Grove, PA, USA) for 10 min at room temperature and subsequently with streptavidin peroxidase for 10 min at room temperature. Diaminobenzidene was employed as the chromogen for 5 min at room temperature. Samples were then counterstained with hematoxylin at room temperature for 30 sec and coverslipped for microscopic examination (50I; light microscope; Nikon Corporation, Tokyo, Japan).
Cell culture
Human small airway epithelial cells (HSAEpiCs) were obtained from ScienCellResearch Laboratories, Inc. (San Diego, CA, USA; 3230) and cultured at 37°C in Small Airway Epithelial Cell Medium (cat. no. 3131; ScienCell Research Laboratories, Inc.) in a humidified atmosphere containing 5% carbon dioxide. To induce GDF15 overexpression, the recombinant expression vector pReceiver-Lv154 which contains the coding sequence of GDF15 (NM_004864) was bought from GeneCopoeia, Inc. (Rockville, MD, USA). Lipofectamine™ 3000 (Thermo Fisher Scientific, Inc., Waltham, MA, USA; cat. no. L3000015) was used to transfect cells with DNA complexes according to the manufacturer's protocol. Cells were harvested for RNA and protein extraction 72 h following transfection.
CSE preparation
CSE was prepared according to a previously published protocol (17). CSE was made from one brand of commercial cigarette (Baisha; Hunan Changsha Tobacco Industrial Co., Ltd., Changsha, China) bubbled through 12.5 ml of bronchial epithelium basal medium (cat. no. CC-3171; Lonza Group Ltd., Basel, Switzerland), which was filtered through a 0.2-mm pore filter. To ensure standardization between experiments and batches of CSE, the absorbance was measured at 320 nm on a spectrophotometer. An optical density of 1 was defined as 100%. CSE was frozen in single use aliquots at −20°C. According to previous reports, 1% CSE is the equivalent of 5 cigarettes/day, 3% is 15 cigarettes/day, 6% is 30 cigarettes/day and 10% is equal to 50 cigarettes/day, which corresponds to human daily exposure to cigarette smoke (18,19). The cytotoxicity of CSE on primary basal cells was measured using a Cytotoxicity Detection kit 1644793001; Roche Diagnostics GmbH, Mannheim, Germany).
Cell stimulation
Cells were seeded at a density of 1×106 onto 6-well plates and grown in bronchial epithelial growth medium (BEGM; Lonza Group Ltd.) supplemented with a BEGM™ BulletKit™ (cat. no. CC-3170; Lonza Group Ltd.) containing bovine pituitary extract, insulin, hydrocortisone, gentamycin/amphotericin, retinoic acid, transferrin, epinephrine and human epidermal growth factor (Lonza Group Ltd.). The medium was supplemented with heat-inactivated foetal bovine serum (cat. no. 10099141; Gibco; Thermo Fisher Scientific, Inc.; 10% in the growth medium or 1% in starvation medium). At confluence, cells were starved for 24 h (BEGM + 1% FBS), then treated daily with IL-17A 00 ng/ml) and CSE (10%) for 4 days, or treated with varying concentrations of IL7A (10, 25, 50, 100 ng/ml) or CSE (1, 2.5, 5, 10, 15%) for 3 days.
Reverse transcription-quantitative polymerase chain reaction (RT-qPCR)
Total RNA was extracted using TRIzol reagent (Invitrogen; Thermo Fisher Scientific, Inc., Waltham, MA, USA) according to the manufacturer's protocol. First strand cDNA was synthesised using Superscript II reverse transcriptase (Invitrogen; Thermo Fisher Scientific, Inc.). The reverse transcription temperature protocol was 42°C for 50 min, followed by 70°C for 15 min. Real-time PCR reactions were performed using the SYBR-Green Real time PCR Master Mix (Invitrogen; Thermo Fisher Scientific, Inc.) and PCR was performed using an ABI PRISM 7900 HT Sequence Detection System (Thermo Fisher Scientific, Inc.). The thermocycling conditions were as follows: 95°C for 5 min, followed by 95°C for 30 sec, 58°C for 30 sec and 40 cycles of 72°C for 10 sec. All reactions were performed in triplicate. Primers used for the amplification of the indicated genes are listed in Table I. Results were normalised to endogenous GAPDH and quantified using the 2−∆∆Cq method (20).
Table I.
Primers used in reverse transcription-quantitative polymerase chain reaction.
| Genes | Direction | Primer sequences (3′-5′) |
|---|---|---|
| Interleukin 17A | Forward | ACAACCGATCCACCTCACCTT |
| Reverse | CCCACGGACACCAGTATCTTCT | |
| Growth/differentiation factor 15 | Forward | GTTGCGGAAACGCTACGAGGA |
| Reverse | CGGAACAGAGCCCGGTGAAG | |
| Epithelial-cadherin | Forward | CGCATTGCCACATACACTCTCT |
| Reverse | GAGCACCTTCCATGACAGACC | |
| Neural-cadherin | Forward | TCAGTGGCGGAGATCCTACTG |
| Reverse | TTGACTGAGGCGGGTGCTGAA | |
| Vimentin | Forward | AACTAATCTGGATTCACTCCCTCTGC |
| Reverse | GAGAAGTTTCGTTGATAACCTGTC | |
| β-actin | Forward | AGGGGCCGGACTCGTCATACT |
| Reverse | GGCGGCACCACCATGTACCCT |
Western blot analysis
Cells were washed with PBS and lysed with RIPA lysis buffer (cat. no. 89900; Invitrogen; Thermo Fisher Scientific) containing a 10% protease inhibitor cocktail (cat. no. 78429; Thermo Fisher Scientific, Inc.) on ice for 30 min. Protein concentrations were determined using a BCA Protein Assay Reagent kit (Thermo Fisher Scientific, Inc.). Aliquots of cell lysates containing 20 µg protein were separated using 10% SDS-polyacrylamide gel and transferred to polyvinylidene difluoride membranes (Invitrogen; Thermo Fisher Scientific, Inc.). Subsequent to blocking with bovine serum albumin (Sigma-Aldrich; Merck KGaA; Darmstadt, Germany) at room temperature for 1 h, membranes were incubated at 4°C overnight with primary antibodies against the following: E-cadherin (1:500; cat. no. ab15148), N-cadherin (1:1,000; cat. no. ab18203), Vimentin (1:1,500; cat. no. ab137321). The anti-E-cadherin, N-cadherin and Vimentin antibodies were obtained from Abcam. Subsequently, membranes were washed with Tris-buffered saline and Tween-20 (Sigma-Aldrich; Merck KGaA) and incubated with horseradish peroxidase-conjugated anti-Rabbit IgG secondary antibodies (1:1,000; cat. no. A21253; Thermo Fisher Scientific, Inc.). Immunoreactive proteins were detected using an ECL kit (Pierce; Thermo Fisher Scientific, Inc.). The relative protein expression was analyzed using Image-Pro plus software 6.0 (Media Cybernetics Inc., Rockville, MD, USA). The expression of β-actin (1:5,000; cat. no. ab227387; Abcam) was used as an internal control to normalize the expressions of other proteins.
Statistical analysis
Data were analysed using SPSS v.17.0 (SPSS, Inc., Chicago, IL, USA) and are presented as the mean ± standard deviation. The non-parametric Mann Whitney U test was used for comparisons-between two groups. One-way analysis of variance with a post-hoc Tukey's test was used for comparisons between more than two groups. The correlation between gene expression levels was analysed using Pearson's correlation. P<0.05 was considered to indicate a statistically significant difference.
Results
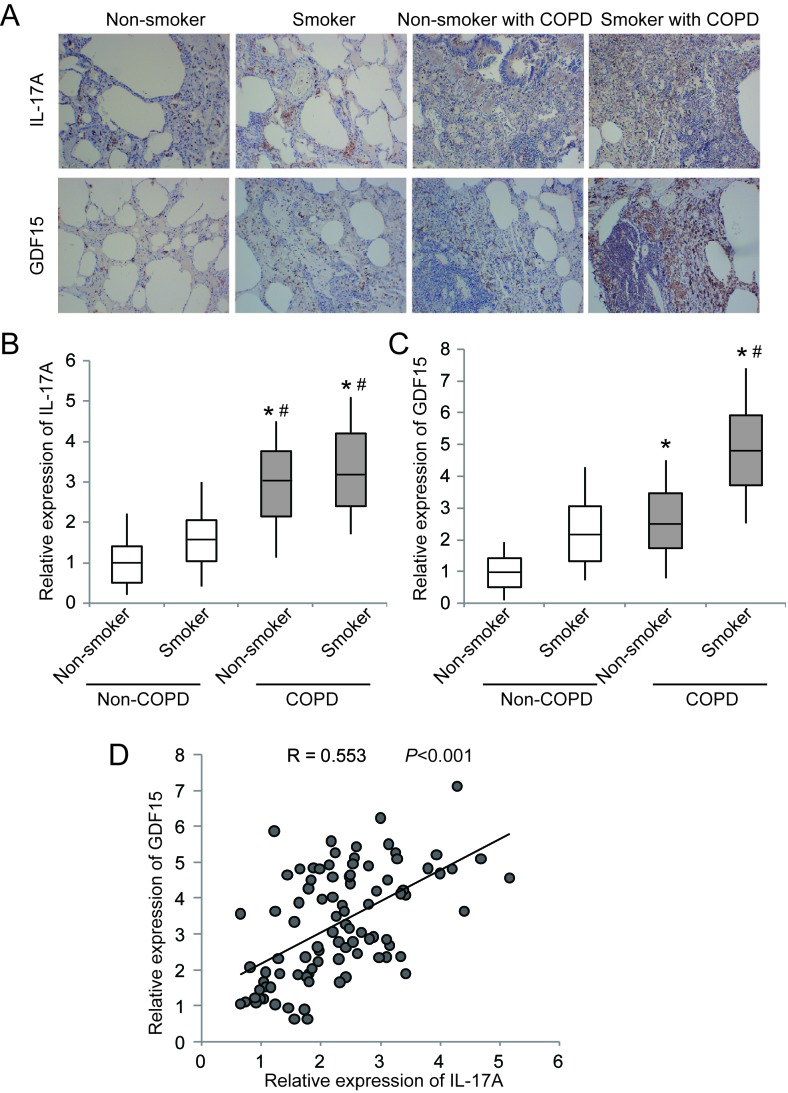
IL-17A and GDF15 are upregulated in the lung tissues of patients with COPD and a history of smoking
IHC staining and RT-qPCR were performed in 143 samples from patients with COPD and 75 samples from patients without COPD. The results of IHC staining demonstrated that IL-17A and GDF15 were markedly upregulated in lung tissues from patients with COPD compared with non-COPD tissues (Fig. 1A). RT-qPCR revealed that IL-17A and GDF15 expression was significantly increased in patients with COPD compared with patients who did not have COPD (Fig. 1B and C). Furthermore, the expression of IL-17A and GDF15 was significantly increased in smokers compared with non-smokers in the COPD and non-COPD groups (Fig. 1B and C). A significant positive correlation was identified between IL-17A and GDF15 expression (Fig. 1D). These results suggest that upregulated IL-17A and GDF15 expression may contribute to COPD development, particularly in patients with a history of smoking.
Figure 1.
Expression of IL-17A and GDF15 in patients with COPD. (A) Immunohistochemical staining of IL-17A and GDF15 in lung tissues. Reverse transcription-quantitative polymerase chain reaction was performed to assess the expression of (B) IL-17A and (C) GDF15 in lung tissue samples obtained from patients with COPD and patients without COPD. (D) IL-17A expression was positively correlated with GDF15 expression.*P<0.05 vs. non-COPD smokers and #P<0.05 vs. non-COPD non-smokers. IL, interleukin; GDF, growth/differentiation factor; COPD, chronic obstructive pulmonary disease.
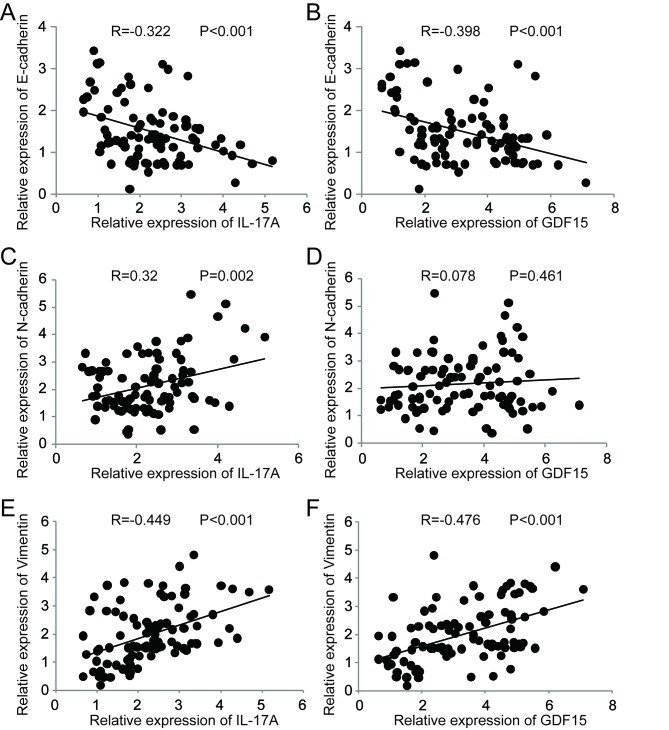
Correlation between IL-17A, GDF15 and EMT markers
A correlation analysis was performed to assess the association between IL-17A, GDF15 and EMT markers [E-cadherin, neural (N)-cadherin and vimentin] in clinical specimens (Fig. 2). IL-17A expression was significantly negatively correlated with E-cadherin (Fig. 2A), whereas it was significantly positively correlated with N-cadherin (Fig. 2C) and vimentin (Fig. 2E). GDF15 expressionwas significantly negatively correlated with E-cadherin (Fig. 2B) and significantly positively correlated with vimentin (Fig. 2F). No significant correlation was observed between GDF15 and N-cadherin expression (Fig. 2D). These results suggest a possible link between increased IL-17A and GDF15 expression and EMT during the development of COPD.
Figure 2.
Correlation between IL-17A, GDF15 and epithelial-mesenchymal transition biomarkers. (A) IL-17A and (B) GDF15 were negatively correlated with E-cadherin. (C) IL-17A was positively correlated with N-cadherin and (D) no significant correlation was observed between GDF15 and N-cadherin expression. (E) IL-17A and (F) GDF15 were positively correlated with vimentin expression. IL, interleukin; GDF, growth/differentiation factor; E-cadherin, epithelial cadherin; N-cadherin, neural cadherin.
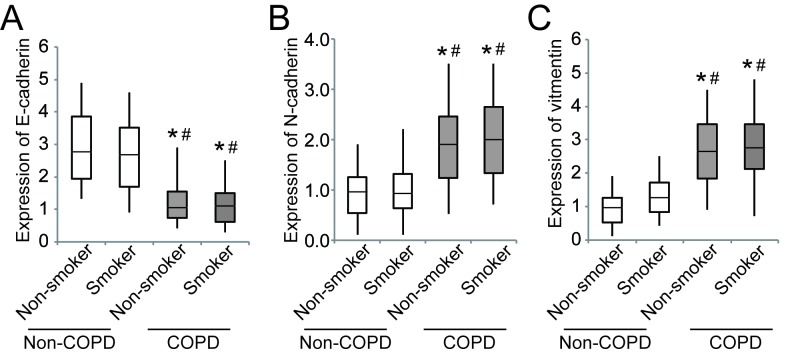
The expression of E-cadherin was significantly downregulated in patients with COPD compared to those without COPD, whereas N-cadherin and vimentin were significantly upregulated (Fig. 3).
Figure 3.
Expression of epithelial-mesenchymal transition biomarkers in patients with COPD. (A) E-cadherin, (B) N-cadherin and (C) vimentin expression in smokers and non-smokers with or without COPD. *P<0.05 vs. non-COPD smokers and #P<0.05 vs. non-COPD non-smokers. COPD, chronic obstructive pulmonary disease; E-cadherin, epithelial cadherin; N-cadherin, neural cadherin.
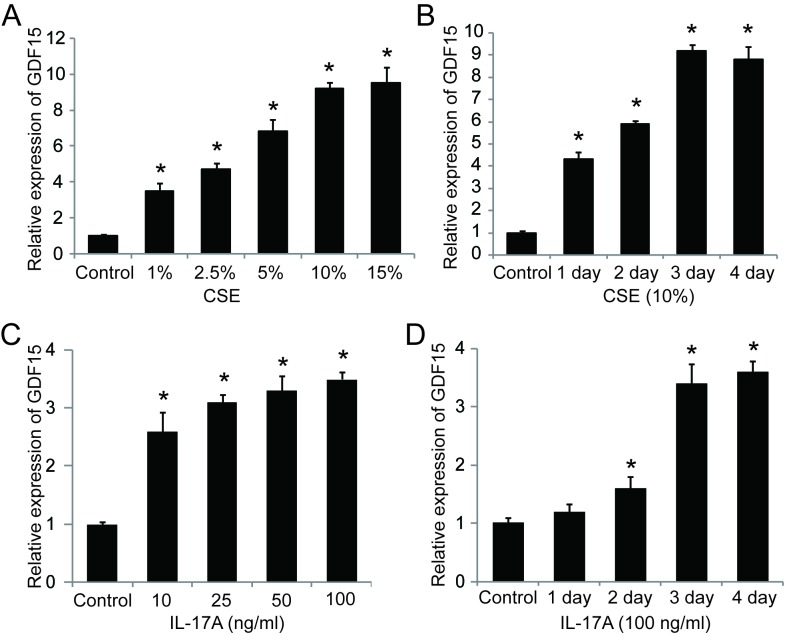
GDF15 is upregulated in CSE- and IL-17A-treated HSAEpiC cells
To address whether smoking affects GDF15 expression, HSAEpiCs were stimulated with CSE and assessed. The results demonstrated that the expression GDF15 mRNA significantly increased in a dose-dependent manner following CSE exposure for 3 days (Fig. 4A). Additionally, GDF15 expression increased significantly with exposure to 10% CSE in a time-dependent manner, reaching a peak following 3 days of exposure (Fig. 4B). It was also demonstrated that GDF15 expression was significantly upregulated by IL-17A in a dose- and time-dependent manner (Fig. 4C and D), suggesting that GDF15 expression is affected by both cigarette smoke exposure and IL-17A treatment in HSAEpiC cells.
Figure 4.
IL-17A and CSE induce GDF15 expression. (A) Cells were treated with 1, 2.5, 5, 10 or 15% CSE for 3 days. (B) Cells were treated with 10% CSE for 1, 2, 3 or 4 days. (C) Cells were treated with 10, 25, 50 or 100 ng/ml IL-17A for 3 days. (D) Cells were treated with 100 ng/ml IL-17A for 1, 2, 3 or 4 days. *P<0.05 vs. control. IL, interleukin; CSE, cigarette smoke extract; GDF, growth/differentiation factor.
IL-17A and GDF15 induce EMT in HSAEpiC cells
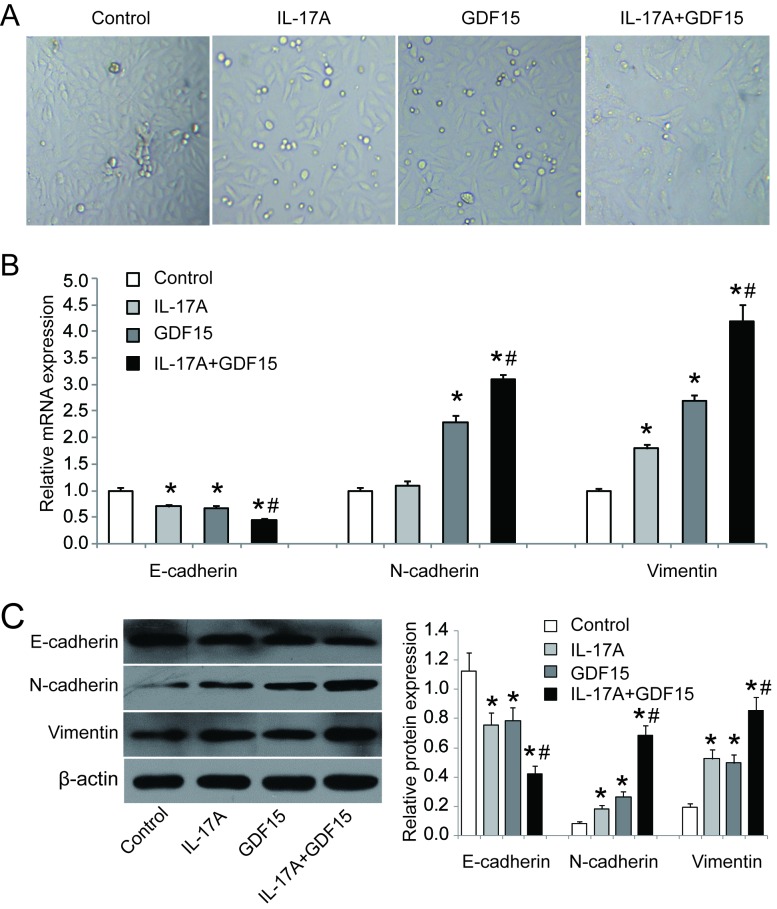
To investigate the role of IL-17A and GDF15 in EMT, HSAEpiC cells were transfected with a GDF15-overexpressing lentivirus and treated with IL-17A (100 ng/ml) for 3 days. The results revealed that HSAEpiC cells lost their honeycomb-like epithelial cell morphology and became spindle shape, which is indicative of EMT (Fig. 5A). RT-qPCR and western blotting were performed to assess the expression of EMT markers and the results demonstrated that E-cadherin was downregulated while N-cadherin and vimentin were upregulated in cells GDF15-overexpressing cells with or without IL-17A treatment compared with control cells (Fig. 5B and C). Furthermore, the combination of IL-17A treatment and GDF15 overexpression had a significantly greater effect on E-cadherin, N-cadherin and vimentin expression compared with GDF15 overexpression alone (Fig. 5B and C). These data suggest that IL-17A, in conjunction with GDF15, is able to induce EMT in HSAEpiC cells.
Figure 5.
IL-17A and GDF15 induce epithelial-mesenchymal transition in HSAEpiC cells. (A) Representative images of cell morphology following exposure to IL-17A and/or GDF15 for 3 days (magnification, ×200). Cells were exposed to IL-17A and/or GDF15 for 3 days and the expression of E-cadherin, N-cadherin and vimentin was measured using (B) reverse transcription-quantitative polymerase chain reaction and (C) western blotting. *P<0.05 vs. control; #P<0.05 vs. GDF15 alone. IL, interleukin; GDF, growth/differentiation factor; E-cadherin, epithelial cadherin; N-cadherin, neural cadherin.
Discussion
The results of the present study demonstrate that IL-17A and GDF15 are upregulated in patients with COPD, particularly in those with a history of smoking, and that IL-17A and GDF15 expression levels are positively correlated with EMT progression. Furthermore, IL-17A treatment in conjunction with CSE-induced GDF15 overexpression triggered EMT in HSAEpiC cells in vitro.
It has been reported that cigarette smoking contributes to lung remodelling and peribronchiolar fibrosis in the small airways, leading to airway obstruction (5). The formation of peribronchiolar fibrosis is associated with EMT (8), while CSE exposure is able to induce EMT in human bronchial epithelial cells (6). COPD has a complex aetiology and is characterised by a combination of airway and lung parenchymal damage (21). The earliest changes in the small airways appear to be due to active EMT, which is associated with a cascade of changes in the expression of regulators, including Smads, Twist and β-catenin (7). Proinflammatory cytokines, including tumour necrosis factor-α, interferon-γ and IL-17, serve an important role in the pathobiology of COPD (22). There is also evidence that high levels of the aforementioned cytokines are responsible for the clinical manifestations of COPD (22,23). Elevated IL-17 expression has been reported in the lungs of patients with COPD; this elevation was attributed to cigarette smoke exposure-dependent effects on the nuclear factor-κB and the phosphoinositide3-kinase pathways (24). Additionally, a combination of IL-17A and CSE stimulation has been reported to affect the proliferation of human epithelial cells and cigarette smoke increases T helper-17 immunity in the lung tissue of patients with COPD (15). In IL-17A knockout mice exposed to cigarette smoke, lymphoid neogenesis was attenuated and chemokine C-X-C motif ligand (CXCL)12 expression was reduced, suggesting that IL-17A contributes to COPD disease progression and the development of lymphoid follicles by activating CXCL12 (25).
It has been reported that the number of CD4+IL-17+ cells is higher in patients with COPD compared with non-smokers, as well as in healthy smokers compared with non-smokers (26). The increase in CD4+IL-17+ cells was positively correlated with pathological changes and airflow limitations (27,28). However, Freeman et al (23) reported a decrease in CD4+ and CD8+ T cells in the peripheral blood during acute exacerbations of COPD, indicating T cell extravasation into inflammatory sites. They also reported that GDF15 is a sensitive marker of cardiopulmonary stress that greatly increases during acute exacerbations of COPD (29). Elevated serum GDF15 levels have been demonstrated to independently predict adverse outcomes in patients with exacerbated COPD (30); furthermore, circulating GDF15 is inversely correlated with rectus femora's cross-sectional area and exercise capacity in patients with COPD (31). This suggests that GDF15 overexpression may be associated with a higher frequency of exacerbations and increased mortality in patients with COPD (32). Importantly, a GDF15 deficiency attenuated cigarette smoke-induced pulmonary inflammation (33) and disruption of GDF15 expression significantly inhibited CSE-induced airway epithelial senescence via activation of the Smad1 pathway (34). The results of the present study revealed that GDF15 expression in HSAEpiC cells was significantly upregulated by IL-17A in a dose- and time-dependent manner. Furthermore, IL-17A in conjunction with GDF15 activated EMT in HSAEpiC cells, which may explain the correlation between IL-17A, GDF15 and EMT markers in clinical specimens. In future studies, knocking out GDF15 and IL-17A is necessary to further determine whether GDF15 and IL-17A are effectors of smoking on COPD. Furthermore, whether monoclonal antibodies for GDF15 and IL-17A diminish the effects of tobacco on airway and lung parenchymal damage in vivo should be assessed in further studies.
In summary, the results of the present study highlight the role of IL-17A and GDF15 in the development of COPD following exposure to cigarette smoke. IL-17A and GDF15-induced EMT was demonstrated to serve an important role in the etiopathology of COPD, which suggests that IL-17A and GDF15 suppression may be an effective therapeutic treatment for COPD. However, more in vivo studies should be conducted in the future.
Acknowledgements
The authors would like to thank Mrs Merissa E. Garvey for language modifications.
Funding
The present study was supported by the Hunan Provincial Natural Science Foundation of China (grant no. 2015JJ2091), the Scientific Research Foundation from Ministry Education of Hunan Province of China (grant no. 15C0832) and the Hunan Provincial Health and Family planning commission of China (grant no. B2017078).
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Authors' contributions
GJ conceived and designed the experiments and wrote the manuscript; CTL performed the experiments and analyzed the data; WDZ contributed in collecting clinical tissue samples, performing the IHC assay and revising the manuscript.
Ethics approval and consent to participate
Ethical approval for the study was granted from the Hunan Provincial People's Hospital Ethics Committee and all patients gave written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3:e442. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sohal SS, Ward C, Danial W, Wood-Baker R, Walters EH. Recent advances in understanding inflammation and remodeling in the airways in chronic obstructive pulmonary disease. Expert Rev Respir Med. 2013;7:275–288. doi: 10.1586/ers.13.26. [DOI] [PubMed] [Google Scholar]
- 3.Hogg JC, Chu F, Utokaparch S, Woods R, Elliott WM, Buzatu L, Cherniack RM, Rogers RM, Sciurba FC, Coxson HO, Paré PD. The nature of small-airway obstruction in chronic obstructive pulmonary disease. N Engl J Med. 2004;350:2645–2653. doi: 10.1056/NEJMoa032158. [DOI] [PubMed] [Google Scholar]
- 4.Sohal SS, Walters EH. Role of epithelial mesenchymal transition (EMT) in chronic obstructive pulmonary disease (COPD) Respir Res. 2013;14:120. doi: 10.1186/1465-9921-14-120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Milara J, Peiró T, Serrano A, Cortijo J. Epithelial to mesenchymal transition is increased in patients with COPD and induced by cigarette smoke. Thorax. 2013;68:410–420. doi: 10.1136/thoraxjnl-2012-201761. [DOI] [PubMed] [Google Scholar]
- 6.Wang Q, Wang Y, Zhang Y, Zhang Y, Xiao W. The role of uPAR in epithelial-mesenchymal transition in small airway epithelium of patients with chronic obstructive pulmonary disease. Respir Res. 2013;14:67. doi: 10.1186/1465-9921-14-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nowrin K, Sohal SS, Peterson G, Patel R, Walters EH. Epithelial-mesenchymal transition as a fundamental underlying pathogenic process in COPD airways: Fibrosis, remodeling and cancer. Expert Rev Respir Med. 2014;8:547–559. doi: 10.1586/17476348.2014.948853. [DOI] [PubMed] [Google Scholar]
- 8.Sohal SS, Mahmood MQ, Walters EH. Clinical significance of epithelial mesenchymal transition (EMT) in chronic obstructive pulmonary disease (COPD): Potential target for prevention of airway fibrosis and lung cancer. Clin Transl Med. 2014;3:33. doi: 10.1186/s40169-014-0033-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gohy ST, Hupin C, Fregimilicka C, Detry BR, Bouzin C, Chevronay Gaide H, Lecocq M, Weynand B, Ladjemi MZ, Pierreux CE, et al. Imprinting of the COPD airway epithelium for dedifferentiation and mesenchymal transition. Eur Respir J. 2015;45:1258–1272. doi: 10.1183/09031936.00135814. [DOI] [PubMed] [Google Scholar]
- 10.Holgate ST. The sentinel role of the airway epithelium in asthma pathogenesis. Immunol Rev. 2011;242:205–219. doi: 10.1111/j.1600-065X.2011.01030.x. [DOI] [PubMed] [Google Scholar]
- 11.Isailovic N, Daigo K, Mantovani A, Selmi C. Interleukin-17 and innate immunity in infections and chronic inflammation. J Autoimmun. 2015;60:1–11. doi: 10.1016/j.jaut.2015.04.006. [DOI] [PubMed] [Google Scholar]
- 12.Di Stefano A, Caramori G, Gnemmi I, Contoli M, Vicari C, Capelli A, Magno F, D'Anna SE, Zanini A, Brun P, et al. T helper type 17-related cytokine expression is increased in the bronchial mucosa of stable chronic obstructive pulmonary disease patients. Clin Exp Immunol. 2009;157:316–324. doi: 10.1111/j.1365-2249.2009.03965.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Doe C, Bafadhel M, Siddiqui S, Desai D, Mistry V, Rugman P, McCormick M, Woods J, May R, Sleeman MA, et al. Expression of the T helper 17-associated cytokines IL-17A and IL-17F in asthma and COPD. Chest. 2010;138:1140–1147. doi: 10.1378/chest.09-3058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Eustace A, Smyth LJC, Mitchell L, Williamson K, Plumb J, Singh D. Identification of cells expressing IL-17A and IL-17F in the lungs of patients with COPD. Chest. 2011;139:1089–1100. doi: 10.1378/chest.10-0779. [DOI] [PubMed] [Google Scholar]
- 15.Montalbano AM, Riccobono L, Siena L, Chiappara G, Di Sano C, Anzalone G, Gagliardo R, Ricciardolo FLM, Sorbello V, Pipitone L, et al. Cigarette smoke affects IL-17A, IL-17F and IL-17 receptor expression in the lung tissue: Ex vivo and in vitro studies. Cytokine. 2015;76:391–402. doi: 10.1016/j.cyto.2015.07.013. [DOI] [PubMed] [Google Scholar]
- 16.Baker CL, Zou KH, Su J. Long-acting bronchodilator use after hospitalization for COPD: An observational study of health insurance claims data. Int J Chron Obstruct Pulmon Dis. 2014;9:431–439. doi: 10.2147/COPD.S59322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang G, Zhou H, Strulovici-Barel Y, Al-Hijji M, Ou X, Salit J, Walters MS, Staudt MR, Kaner RJ, Crystal RG. Role of OSGIN1 in mediating smoking-induced autophagy in the human airway epithelium. Autophagy. 2017;13:1205–1220. doi: 10.1080/15548627.2017.1301327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hogan AE, Corrigan MA, O'Reilly V, Gaoatswe G, O'Connell J, Doherty DG, Lynch L, O'Shea D. Cigarette smoke alters the invariant natural killer T cell function and may inhibit anti-tumor responses. Clin Immunol. 2011;140:229–235. doi: 10.1016/j.clim.2011.01.011. [DOI] [PubMed] [Google Scholar]
- 19.Kosmider B, Messier EM, Chu HW, Mason RJ. Human alveolar epithelial cell injury induced by cigarette smoke. PLoS One. 2011;6:e26059. doi: 10.1371/journal.pone.0026059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 21.Nowrin K, Sohal SS, Peterson G, Patel R, Walters EH. Epithelial-mesenchymal transition as a fundamental underlying pathogenic process in COPD airways: Fibrosis, remodeling and cancer. Expert Rev Respir Med. 2014;8:547–559. doi: 10.1586/17476348.2014.948853. [DOI] [PubMed] [Google Scholar]
- 22.Caramori G, Adcock IM, Di Stefano A, Chung KF. Cytokine inhibition in the treatment of COPD. Int J Chron Obstruct Pulmon Dis. 2014;9:397–412. doi: 10.2147/COPD.S42544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhang X, Zheng H, Zhang H, Ma W, Wang F, Liu C, He S. Increased interleukin (IL)-8 and decreased IL-17 production in chronic obstructive pulmonary disease (COPD) provoked by cigarette smoke. Cytokine. 2011;56:717–725. doi: 10.1016/j.cyto.2011.09.010. [DOI] [PubMed] [Google Scholar]
- 24.Chang Y, Al-Alwan L, Alshakfa S, Audusseau S, Mogas AK, Chouiali F, Nair P, Baglole CJ, Hamid Q, Eidelman DH. Upregulation of IL-17A/F from human lung tissue explants with cigarette smoke exposure: Implications for COPD. Respir Res. 2014;15:145. doi: 10.1186/s12931-014-0145-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Roos AB, Sandén C, Mori M, Bjermer L, Stampfli MR, Erjefält JS. IL-17A is elevated in End-stage chronic obstructive pulmonary disease and contributes to cigarette smoke-induced lymphoid neogenesis. Am J Respir Crit Care Med. 2015;191:1232–1241. doi: 10.1164/rccm.201410-1861OC. [DOI] [PubMed] [Google Scholar]
- 26.Zhang J, Chu S, Zhong X, Lao Q, He Z, Liang Y. Increased expression of CD4+IL-17+ cells in the lung tissue of patients with stable chronic obstructive pulmonary disease (COPD) and smokers. Int Immunopharmacol. 2013;15:58–66. doi: 10.1016/j.intimp.2012.10.018. [DOI] [PubMed] [Google Scholar]
- 27.Zhang J, Chu S, Zhong X, Lao Q, He Z, Liang Y. Increased expression of CD4+IL-17+ cells in the lung tissue of patients with stable chronic obstructive pulmonary disease (COPD) and smokers. Int Immunopharmacol. 2013;15:58–66. doi: 10.1016/j.intimp.2012.10.018. [DOI] [PubMed] [Google Scholar]
- 28.Jin Y, Wan Y, Chen G, Chen L, Zhang MQ, Deng L, Zhang JC, Xiong XZ, Xin JB. Treg/IL-17 ratio and Treg differentiation in patients with COPD. PLoS One. 2014;9:e111044. doi: 10.1371/journal.pone.0111044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wu Q, Jiang D, Chu HW. Cigarette smoke induces growth differentiation factor 15 production in human lung epithelial cells: Implication in mucin over-expression. Innate Immun. 2012;18:617–626. doi: 10.1177/1753425911429837. [DOI] [PubMed] [Google Scholar]
- 30.Kim M, Cha SI, Choi KJ, Shin KM, Lim JK, Yoo SS, Lee J, Lee SY, Kim CH, Park JY, et al. Prognostic value of serum growth differentiation factor-15 in patients with chronic obstructive pulmonary disease exacerbation. Tuberc Respir Dis (Seoul) 2014;77:243–250. doi: 10.4046/trd.2014.77.3.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Patel MS, Lee J, Baz M, Wells CE, Bloch S, Lewis A, Donaldson AV, Garfield BE, Hopkinson NS, Natanek A, et al. Growth differentiation factor-15 is associated with muscle mass in chronic obstructive pulmonary disease and promotes muscle wasting in vivo. J Cachexia Sarcopenia Muscle. 2016;7:436–448. doi: 10.1002/jcsm.12096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Husebo GR, Grønseth R, Lerner L, Gyuris J, Hardie JA, Bakke PS, Eagan TM. Growth differentiation factor-15 is a predictor of important disease outcomes in patients with COPD. Eur Respir J. 2017;49 doi: 10.1183/13993003.01298-2016. pii: 1601298. [DOI] [PubMed] [Google Scholar]
- 33.Verhamme FM, Seys LJ, De Smet EG, Provoost S, Janssens W, Elewaut D, Joos GF, Brusselle GG, Bracke KR. Elevated GDF-15 contributes to pulmonary inflammation upon cigarette smoke exposure. Mucosal Immunol. 2017;10:1400–1411. doi: 10.1038/mi.2017.3. [DOI] [PubMed] [Google Scholar]
- 34.Freeman CM, Martinez CH, Todt JC, Martinez FJ, Han MK, Thompson DL, McCloskey L, Curtis JL. Acute exacerbations of chronic obstructive pulmonary disease are associated with decreased CD4+ &; CD8+ T cells and increased growth &; differentiation factor-15 (GDF-15) in peripheral blood. Respir Res. 2015;16:94. doi: 10.1186/s12931-015-0251-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.