Abstract
Objective
The cost of care for diabetic foot ulcers is estimated to be more than $1.5 billion annually. The aim of this study was to analyze inpatient diabetic foot ulcer cost changes over time and to identify factors associated with these costs.
Methods
The Nationwide Inpatient Sample (2005–2010) was queried using the International Classification of Diseases, Ninth Revision codes for a primary diagnosis of foot ulceration. The primary outcomes were changes in adjusted total hospital charges and costs over time. Multivariable analysis was performed to assess relative increases (RIs) in hospital charges per patient in 2005 vs 2010 adjusting for demographic characteristics, income, comorbidities (Charlson Co-morbidity Index ≥3), insurance type, hospital characteristics, diagnostic imaging, revascularization, amputation, and length of stay.
Results
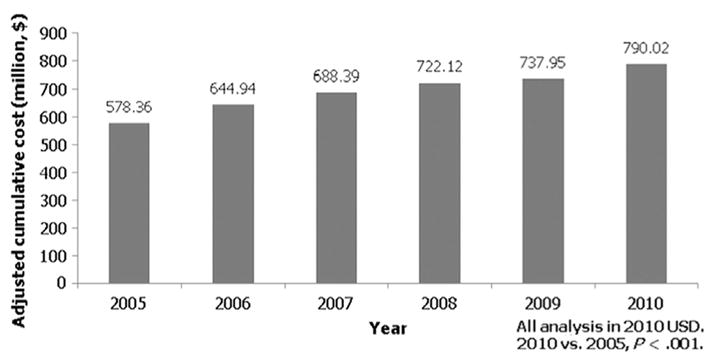
Overall, 336,641 patients were admitted with a primary diagnosis of diabetic foot ulceration (mean age, 62.9 ± 0.1 years, 59% male, 61% white race). The annual cumulative cost for inpatient treatment of diabetic foot ulcers increased significantly from 2005 to 2010 ($578,364,261 vs $790,017,704; P < .001). More patients were hospitalized (128.6 vs 152.8 per 100,000 hospitalizations; P < .001), and the mean adjusted cost per patient hospitalization increased significantly over time ($11,483 vs $13,258; P < .001). The proportion of nonelective admissions remained stable (25% vs 23%; P =.32) and there were no differences in mean hospital length of stay (7.0 ± 0.1 days vs 6.8 ± 0.1 days; P =.22). Minor (17.9% vs 20.6%; P < .001), but not major amputations (3.9% vs 4.2%; P = .27) increased over time. Based on multivariable analysis, the main factors contributing to the escalating cost per patient hospitalization included increased patient comorbidities (unadjusted mean difference 2005 vs 2010 $3303 [RI, 1.08] vs adjusted $15,220 [RI, 1.35]), open revascularization (unadjusted $15,145 [RI, 1.25] vs adjusted $30,759 [RI, 1.37]), endovascular revascularization (unadjusted $17,662 [RI, 1.29] vs adjusted $28.937 [RI, 1.38]), and minor amputations (unadjusted $9918 [RI, 1.24] vs adjusted $18,084 [RI, 1.33]) (P < .001, all).
Conclusions
Hospital charges and costs related to diabetic foot ulcers have increased significantly over time despite stable hospital length of stay and proportion of emergency admissions. Risk-adjusted analyses suggest that this change might be reflective of increasing charges associated with a progressively sicker patient population and attempts at limb salvage. Despite this, the overall incidence of major amputations remained stable.
Diabetes affects approximately 8% of the U.S. population, or nearly 24 million people in the United States.1 Diabetic foot ulcers are a common sequela of the disease and a significant cause of morbidity and mortality.2 Ulcer prevalence ranges from 0.65% in patients younger than 44 years of age to 1.3% in patients aged 75 years and older,3 and are the result of a well-described additive process that involves progressive neuropathy, minor trauma, ulceration, faulty healing, ischemia, and infection.4 Frequently, diabetic foot ulcers end in amputation; patients with diabetes have a 5-fold increase in odds of needing a limb amputation and a 3-fold increase in mortality compared with patients without diabetes.5
Overall, diabetes and diabetes-related problems are estimated to cost the United States $174 billion annually.1 An analysis of Medicare claims data suggests that the cost of care for diabetic foot ulcers, specifically, was more than $1.5 billion annually 15 years ago.6 The rate of hospitalization for diabetic foot ulcers has been steadily increasing since that time, and thus the current inflation-adjusted costs are likely much higher.3 The relative cost of care for a diabetic patient with a foot ulcer is estimated to be 5.4 times greater in the year after diagnosis than the cost of care for a similar patient with no ulcer.7 Furthermore, nearly 80% of these excess costs can be attributed to inpatient expenditures.6,8,9
Despite the magnitude of the diabetic foot ulcer problem, there are limited data reporting related trends in cost changes over recent years. In addition, a breakdown of the cost differential for the diagnosis and treatment of diabetic foot ulcers is not currently well described. The aim of this study was to analyze inpatient diabetic foot ulcer cost changes over time and to identify factors associated with these costs.
METHODS
Data source and inclusion criteria
The Healthcare Cost and Utilization Project Nationwide Inpatient Sample (NIS) was queried for all patients with diabetes who were admitted with a primary diagnosis of foot ulceration between January 1, 2005 and December 31, 2010. Eligible patients aged between 18 and 99 years were identified using the International Classification of Diseases, Ninth Revision codes (250.80–250.82, 440.23, 707.13–707.15). Patients with venous hypertension, gestational diabetes, or missing information for in-hospital mortality and cost were excluded. The Johns Hopkins Hospital Institutional Review Board approved this study prior to its initiation. Informed consent was waived as all data was obtained from the NIS, which is a publicly available source.
Variables
Data were collected on patient demographic characteristics (age, sex, race, household income quartile according to patient residential zip code, and insurance status), admitting hospital characteristics (teaching vs nonteaching status, hospital bed size, U.S. census region, urban vs rural location), admission details (elective vs nonelective admission, hospital length of stay), and relevant secondary diagnoses (critical limb ischemia, gangrene, osteomyelitis), diagnostic testing (X ray, computed tomography scan, magnetic resonance imaging, diagnostic angiogram), intervention (antibiotic use, endovascular revascularization, open revascularization, major amputation, minor amputation), and inpatient charges incurred per patient (Supplementary Table I, online only). Age was categorized into three predefined groups: 18 to 39 years, 40 to 64 years, and ≥65 years based on previously published reports.7 Insurance status was classified as “government,” “private/health maintenance organization,” or “uninsured.” Standard Charlson Comorbidity Index (CCI) scores (ie, without age adjustment) were calculated by using the International Classification of Diseases Program for Injury Categorization program.10 CCI scores are typically used to quantify prognosis of patients.11 Within our patient cohort, CCI scores were heavily skewed to the right, with a mean score of 2.3 and median score of 2. Based on the original article by Charlson et al,11 increasing patient comorbidity scores are associated with stepwise increases in the cumulative mortality attributable to comorbid disease (CCI score “0,” 12%; CCI score “1–2,” 26%; CCI score “3–4,” 52%; and CCI score “≥5,” 85%.) Therefore, for this analysis, CCI scores were dichotomized in to <3 and ≥3 to differentiate patients with mild or no comorbidity (scores 0–2) from those with moderate or severe comorbidity (scores ≥3). Other relevant comorbid conditions that were evaluated in this study include peripheral vascular disease, critical limb ischemia, gangrene, and osteomyelitis. Endovascular revascularization included percutaneous transluminal angioplasty and/or stent procedures. Open revascularization included inflow bypasses, infrainguinal bypasses, and multilevel bypasses. Major amputation was defined as below-knee amputation, knee disarticulation, or above-knee amputation. Minor amputation was defined as toe or foot amputations.
The main outcomes analyzed in this study were inpatient charges and cost. To obtain hospital costs, NIS provides a cost-to-charge ratio (CCR) file that can be merged with the core database. Each hospital in the database has one CCR value assigned to it. For the purposes of this study, every patient from a particular hospital was assigned that same CCR. By multiplying this ratio with total hospital charges incurred for each patient, cost per patient was able to be calculated.
Statistical analysis
Because the NIS is a 20% stratified sample of all short-term, nonfederal, community hospitals in the United States,12 applying sampling weights to the analysis allows U.S. population estimates to be estimated. Sampling weights calculated and provided by the Healthcare Cost and Utilization Project were applied at the beginning of the analysis. The study population was stratified in to six groups based on year of admission: 2005, 2006, 2007, 2008, 2009, and 2010. Patient demographic characteristics, visit, and hospital characteristics were analyzed for each year and described using weighted counts and proportions for categorical data, and means and standard errors for continuous data. The χ2 test was used to assess proportional differences in patient demographic characteristics, visit, and hospital characteristics across the years, and analysis of variance was conducted for comparison of means over the years. An a priori significance level of P < .05 was used. γ Distribution was specified in a generalized linear model to adjust for age group, sex, race, income quartile, insurance status, hospital teaching status, hospital bed size, hospital region, hospital location (urban/rural), critical limb ischemia, gangrene, osteomyelitis, CCI, nonelective admission, X ray, magnetic resonance imaging, computed tomography scan, antibiotic infusion, any endovascular revascularization, any open revascularization, minor amputation, major amputation, log-transformed hospital length of stay, and death, to obtain the estimated adjusted mean cost for the treatment of diabetic foot ulcers for each year between 2005 and 2010. γ Distribution was used in the adjusted analysis because costs and charges were highly skewed, and thus, this enabled the calculation of costs and charges in real-world monetary values so that meaningful estimates could be reported.13,14 Year 2005 was used as the reference year, to which the estimated adjusted mean cost for every subsequent year thereafter was compared.
All costs were adjusted for inflation and analyzed in 2010 U.S. dollars.15 Stata version 12.0 (StataCorp, College Station, Tex) was used for all analyses.
RESULTS
Patient demographic characteristics and admissions
Overall, 336,641 patients were admitted with a primary diagnosis of diabetic foot ulceration over the 6-year study period (mean age, 62.9 ± 0.1 years, 59% male, 61% white race). The median adjusted total hospital charges changed significantly over time for all patients regardless of demographic information, comorbidities, and insurance status (all, P < .001; Table I).
Table I.
Median adjusted total hospital charges per patient over time according to demographic characteristic (in 2010 U.S. dollars)
| Patient demographic characteristic | Year
|
P | |||||
|---|---|---|---|---|---|---|---|
| 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | ||
| Age, years | |||||||
| 18–39 | $17,474 | $19,807 | $20,238 | $23,202 | $24,859 | $27,609 | <.001 |
| 40–64 | $22,188 | $23,492 | $25,334 | $26,142 | $28,205 | $29,258 | <.001 |
| >65 | $21,632 | $23,634 | $24,356 | $26,613 | $28,344 | $28,738 | <.001 |
| Sex | |||||||
| Female | $20,466 | $22,224 | $22,682 | $25,205 | $26,466 | $27,415 | <.001 |
| Male | $22,570 | $24,060 | $25,949 | $26,704 | $28,910 | $29,863 | <.001 |
| Race | |||||||
| White | $22,127 | $23,798 | $25,291 | $25,988 | $27,802 | $28,096 | <.001 |
| Other | $24,271 | $25,534 | $27,616 | $28,817 | $31,772 | $32,119 | <.001 |
| Elective admission | $25,148 | $27,111 | $29,111 | $31,764 | $33,693 | $34,138 | <.001 |
| Comorbid conditions | |||||||
| Hypertension | $20,955 | $23,431 | $24,563 | $26,130 | $27,638 | $28,829 | <.001 |
| CAD | $22,769 | $24,472 | $24,899 | $28,220 | $28,925 | $29,600 | <.001 |
| CHF | $23,914 | $25,590 | $25,767 | $27,358 | $30,163 | $32,057 | <.001 |
| COPD | $16,831 | $18,515 | $22,860 | $20,007 | $21,692 | $21,823 | .83 |
| Neuropathy | $18,974 | $20,300 | $22,086 | $23,588 | $25,466 | $26,169 | <.001 |
| Dialysis | $22,639 | $26,208 | $27,597 | $27,683 | $31,444 | $33,789 | <.001 |
| PVD | $34,088 | $36,959 | $39,446 | $40,427 | $45,053 | $46,152 | <.001 |
| Critical limb ischemia | $34,695 | $37,453 | $40,132 | $41,247 | $46,244 | $47,049 | <.001 |
| Osteomyelitis | $28,020 | $31,484 | $33,836 | $34,276 | $36,920 | $36,920 | <.001 |
| Gangrene | $31,978 | $36,302 | $40,813 | $39,647 | $41,390 | $42,919 | <.001 |
| CCI >3 | $23,082 | $25,134 | $26,159 | $27,446 | $28,457 | $30,278 | <.001 |
| Primary payer | <.001 | ||||||
| Government | $21,540 | $23,507 | $24,598 | $26,343 | $28,001 | $29,222 | |
| Private/HMO | $22,318 | $23,413 | $24,367 | $26,038 | $28,626 | $28,436 | |
| Uninsured | $19,450 | $22,374 | $25,930 | $22,653 | $25,625 | $27,904 | |
CAD, Coronary artery disease; CCI, Charlson Comorbidity Index; CHF, congestive heart failure; COPD, chronic obstructive pulmonary disease; HMO, health maintenance organization; PVD, peripheral vascular disease.
Compared with 2005, patients admitted with diabetic foot ulcers in 2010 were sicker (CCI ≥3, 7.7% vs 22.2%; P < .001) and more frequently presented with osteomyelitis (29.3% vs 40.4%; P < .001). There were no differences in the proportion of patients presenting with critical limb ischemia (20.8% vs 19.1%; P = .15) or gangrene (12.5% vs 13.1%; P = .44). Hospital charges associated with having multiple comorbidities (CCI ≥3) increased from $23,082 per patient in 2005 to $30,278 per patient in 2010 (net increase of $7196 per patient; P < .001). Per-patient hospital charges similarly increased for osteomyelitis ($28,020 vs $36,920 per patient), critical limb ischemia ($34,695 vs $47,049 per patient), and gangrene ($31,978 vs $42,919 per patient) (all, P < .001; Table I). Hospital charges also significantly increased over time (2005 vs 2010) in patients with mild or no comorbidities (CCI <3; $21,534 vs $28,531 per patient), and in those without osteomyelitis ($18,711 vs $23,525 per patient), critical limb ischemia ($18,795 vs $25,486 per patient), or gangrene ($20,263 vs $27,045 per patient) (all, P < .001). The proportion of nonelective admissions remained stable (25.4% vs 23.2%; P = .32), and there were no differences in mean hospital length of stay over time (7.0 ± 0.1 days vs 6.8 ± 0.1 days; P = .22).
Hospital characteristics
Median hospital charges per diabetic foot ulcer admission increased significantly from 2005 to 2010 for all hospitals regardless of teaching status (teaching hospitals, $22,876 vs $29,639 per patient; nonteaching hospitals, $20,919 vs $28,131 per patient), or bed size (small, $18,229 vs $28,604 per patient; medium $18,407 vs $28,061 per patient; large $23,317 vs $29,169 per patient) (all, P < .001). Charges increased for hospitals in urban ($23,318 vs $30,662 per patient) and rural ($12,691 vs $18,112 per patient) settings in all geographic regions across the country (all, P < .001; Supplementary Table II, online only).
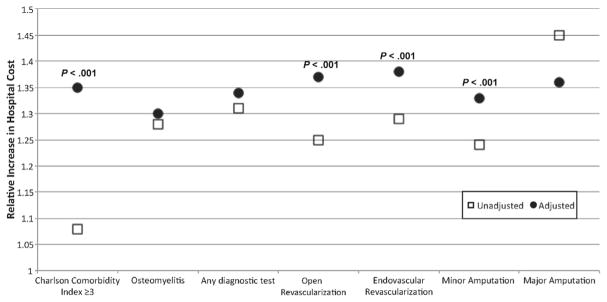
Cumulative hospital costs
The total cumulative hospital cost for inpatient treatment of diabetic foot ulcers between 2005 and 2010 was $4,152,130,094. The annual cumulative hospital costs for diabetic foot ulcers increased significantly from 2005 to 2010 ($578,364,261 vs $790,017,704; P < .001; Fig 1). More patients with diabetic foot ulcers were hospitalized over time (50,367 vs 59,588 patients; P < .001), accounting for a larger proportion of inpatient admissions overall (128.6 vs 152.8 per 100,000 hospitalizations; P < .001). The mean adjusted cost per patient hospitalization increased significantly ($11,483 vs $13,258; P < .001) (Table II).
Fig 1.
Risk-adjusted annual cumulative costs for inpatient treatment of diabetic foot ulcers in the United States increased significantly from 2005 to 2010 (P < .001).
Table II.
Trends in patient hospitalizations and adjusted hospital costs for diabetic foot ulcers over time (in 2010 U.S. dollars)
| Year
|
P | ||||||
|---|---|---|---|---|---|---|---|
| 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | ||
| Admissions per 100,000 hospitalizations | 128.6 | 139.4 | 144.0 | 143.9 | 145.4 | 152.8 | <.001 |
| Adjusted cost per patient, $ | 11,483 | 11,726 | 12,087 | 12,584 | 12,868 | 13,258 | <.001 |
Trends in diagnostic testing and interventions
The per-patient cost of diagnostic testing and interventions for diabetic foot ulcers increased significantly over time (Table III; Supplementary Table III, online only). The cost of antibiotic infusion therapy ($30,074 vs $37,860 per patient), open ($45,451 vs $56,117 per patient) and endovascular ($42,685 vs $63,007 per patient) revascularization procedures, and major ($38,008 vs $53,779 per patient) and minor ($29,928 vs $37,598 per patient) amputations all increased over the years (all, P < .001; Table III). Of note, patients underwent significantly fewer open revascularizations (7.1% vs 4.7%; P < .001) but more endovascular revascularizations in 2010 compared with 2005 (7.1% vs 8.7%; P = .008). Minor (17.9% vs 20.6%; P < .001), but not major amputations (3.9% vs 4.2%; P = .27) increased over time.
Table III.
Trends in median adjusted total hospital charges per patient for diagnostic testing and interventions for diabetic foot ulcers over time (in 2010 U.S. dollars)
| Year
|
P | ||||||
|---|---|---|---|---|---|---|---|
| 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | ||
| Any diagnostic test | $38,430 | $47,103 | $49,068 | $50,947 | $55,124 | $54,408 | <.001 |
| Antibiotic infusion | $30,074 | $32,794 | $34,108 | $38,059 | $41,977 | $37,860 | <.001 |
| Any revascularization | $43,468 | $45,862 | $51,109 | $50,947 | $58,204 | $59,911 | <.001 |
| Endovascular | $42,685 | $46,533 | $51,967 | $51,609 | $61,286 | $63,007 | <.001 |
| Open | $45,451 | $46,771 | $52,693 | $53,242 | $56,072 | $56,117 | <.001 |
| Amputation | |||||||
| Minor | $29,928 | $31,208 | $34,070 | $34,822 | $36,204 | $37,598 | <.001 |
| Major | $38,008 | $41,057 | $44,722 | $49,457 | $54,478 | $53,779 | <.001 |
| Death | $44,767 | $40,868 | $47,482 | $62,844 | $62,850 | $60,703 | .02 |
Factors contributing to relative increases in hospital costs over time
Based on multivariable analysis, the main factors contributing to the escalating cost per patient hospitalization for diabetic foot ulcers include increased patient comorbidities (CCI ≥3), open revascularization, endovascular revascularization, and minor amputations (P < .001; Fig 2). The relative effects of osteomyelitis, overall trends in diagnostic testing, and major amputations did not significantly change over time after risk adjustment (P = not significant; Table IV).
Fig 2.
Multivariable risk-adjusted analysis demonstrated that the main factors contributing to the escalating cost per patient hospitalization for diabetic foot ulcers included increased patient comorbidities, open revascularization, endovascular revascularization, and minor amputations (P < .001). Osteomyelitis, diagnostic testing, and major amputations did not significantly affect cost increases after risk-adjustment (P = not significant).
Table IV.
Multivariable analysis of factors contributing to relative increases in per-patient hospital costs from 2005 vs 2010
| Mean cost difference 2005 vs 2010
|
Relative increase in cost 2005 vs 2010
|
|||
|---|---|---|---|---|
| Unadjusted | Adjusted | Unadjusted | Adjusted | |
| CCI ≥3 | $3303 | $15,220 | 1.08 | 1.35a |
| Osteomyelitis | $11,244 | $13,852 | 1.28 | 1.3 |
| Any diagnostic test | $16,775 | $22,876 | 1.31 | 1.34 |
| Open revascularization | $15,145 | $30,759 | 1.25 | 1.37a |
| Endovascular revascularization | $17,662 | $28.937 | 1.29 | 1.38a |
| Minor amputation | $9918 | $18,084 | 1.24 | 1.33a |
| Major amputation | $23,794 | $24,996 | 1.45 | 1.35 |
CCI, Charlson Comorbidity Index.
Adjusted models control for age group, sex, race, income quartile, insurance status, hospital teaching status, hospital bed size, hospital region, hospital location (urban/rural), critical limb ischemia, gangrene, osteomyelitis, CCI ≥3, nonelective admission, X ray, magnetic resonance imaging, computed tomography scan, antibiotic infusion, any endovascular revascularization, any open revascularization, minor amputation, major amputation, log-transformed hospital length of stay, and death.
P < .001 for adjusted vs unadjusted relative increase in cost.
DISCUSSION
The cost of care for diabetic foot ulcers was estimated to be more than $1.5 billion annually based on 1995 to 1996 Medicare data.6 Because of the increasing prevalence of this disease,3 the current economic burden of caring for affected patients is significant. Minimal data exist that describe recent trends in hospital costs associated with diabetic foot ulcers over time. In the current study, we demonstrated that hospital charges related to diabetic foot ulcers have increased significantly between 2005 and 2010; that the cost increases are not reflective of increases in hospital stay or emergent admissions, and that the cost of treating sicker patients increased significantly. We also demonstrated that the overall incidence of major amputations has remained stable over time, despite an increased proportion of endovascular revascularization and minor amputation procedures.
Based on data from the Centers for Disease Control, hospital discharge rates related to diabetes have decreased by more than half from 1988 to 2009.3 In contrast, we report a nearly 20% increase in admissions for patients with a primary diagnosis of diabetic foot ulceration between 2005 and 2010 alone. These paradoxical findings might be reflective of an increasing understanding of the morbidity of foot ulcers, or the increased availability of limb salvage techniques including revascularization procedures with local wound care and/or minor amputations. There has been an increasing movement to improve patient and provider education on the diagnosis and management of diabetic foot ulcers, including a push for integrated limb salvage teams in a number of large academic centers.8,16–24 Multidisciplinary approaches to prevention, surveillance, and management of diabetic patients have been shown to effectively reduce major amputation rates by as much as 80%, particularly with the use of aggressive revascularization strategies.23,25,26 Because approximately 50% of the costs related to diabetic foot ulcerations are related to hospitalizations and amputations,27 such a multidisciplinary approach is now becoming the standard of care.28
Consistent with this notion, Goodney et al recently demonstrated that the rates of lower extremity endovascular interventions among Medicare beneficiaries increased significantly between 1996 and 2006, and open revascularization rates decreased by nearly half.29 We similarly found that among patients admitted with diabetic foot ulcers, endovascular revascularization procedures were performed more frequently in 2010 compared with 2005, but the proportion of open procedures decreased significantly. However, the incidence of major amputations appears to have remained stable over time within the diabetic population, compared with a 25% decrease in major amputations that has been reported in the overall Medicare population.29 This difference could be a reflection of the fact that the NIS includes patients of all age ranges, including those younger than 65 years of age who would have been excluded from the Medicare analysis, and/or our focus on a diabetic population. Goldberg et al cited amputation rates ranging between 24.4 to 48.0 per 1000 high-risk (≥3 comorbidities) diabetic patients within the Medicare population,30 which is similar to the 4.2% incidence of major amputations that we report. In addition, Anderson et al previously reported a relatively stable amputation rate between 1980 and 2000 despite significant increases in endovascular interventions using NIS data,31 which is consistent with our findings. Whether the stable incidence of major amputations in the setting of increasing minor amputations, vascular interventions, and hospital care that we report is a reflection of a lack of effect of limb salvage attempts or a sicker patient population is difficult to determine. Although hospital charges increased for patients with high (≥3) and low (<3) CCI scores, increased patient comorbidities was found to be one of the main factors contributing to the escalating cost per patient hospitalization in multivariable analysis. Certainly patients had more comorbidities and presented more frequently with osteomyelitis in 2010 compared with 2005, but a cause-and-effect relationship cannot be determined based on the data that are available for analysis in the NIS. Further studies investigating longitudinal trends in diabetic foot ulcer presentations over time are warranted to better address this important question.
In addition to confirming that the use of endovascular interventions has been increasing, we also demonstrated that this increase is associated with a significant increase in cost per patient hospitalization. Whether this increase is a reflection of increasing device costs, increases in the number of devices used per procedure, or other factors cannot be determined from this database. Minimal data exist reporting on the economic effect of limb salvage.22 A number of studies have examined the theoretic cost savings of a limb salvage team using Markov modeling, but all of them focused on early ulcer prevention strategies such as patient education, routine foot care, and proper foot care in their estimates, rather than performance of limb-salvage procedures specifically.32–36 Lower extremity amputations account for a disproportionately high portion of inpatient hospital costs related to diabetic ulcers,8 which is the impetus behind the limb salvage team concept. Although revascularization procedures, advanced wound care, and multimodal surveillance is recognized as expensive, the avoidance of costly major amputations is proposed as a means of reducing long-term costs.22 The cost of curative ulcer care has been shown to be anywhere from five to 30 times greater than the cost of preventive care depending on the severity of disease.37 However, our data suggest that the major short-term factors contributing to increasing costs of ulcer care include a progressively sicker patient population and increasing charges associated with limb salvage, rather than the inpatient charges associated with major amputation. In fact, the adjusted relative increase in hospital costs associated with major amputation was actually lower than the unadjusted costs in our study, suggesting that the unadjusted increases in costs associated with major amputation are attributable to other patient-, hospital-, or treatment-level variables included in the multivariable model. Treatment costs for diabetic foot ulcers are high regardless of amputation, totaling more than $13,000 per patient hospitalization as of 2010.
Of note, although we report a steady increase in hospital charges and admissions related to diabetic foot ulcers over time, the proportion of emergency admissions and overall hospital lengths of stay were stable. This was an unexpected finding based on previous reports suggesting that hospital length of stay is one of the most important factors affecting diabetic foot ulcer inpatient costs.17,36–39 Although one could argue that the trends we report reflect improvements in ulcer recognition, which would explain why hospital length of stay was largely unchanged, admitted patients had a progressively greater incidence of osteomyelitis over time. The reason for this trend is currently unclear, especially with the recent advocacy for improved diabetic care involving providers at all levels. Certain socioeconomic or insurance factors might play a role. In a study of nearly 700,000 patients with lower extremity ischemia, Eslami et al report a greater frequency of lower extremity amputation in nonwhite, low-income patients without commercial insurance.40 The authors attributed their findings to a lack of adequate primary care and/or vascular surgery access in disadvantaged populations. Consistent with this notion, we noted a significant association between hospital costs and patient health status; sicker patients had greater ulcer-related hospital costs, suggesting a possible association between poor access to primary care and more advanced disease. Increased hospital costs are likely reflective of an increased need for multimodal treatment in this group. There is an incremental increase in hospital utilization with increasing severity of ulcer disease,9,39 although the true effect of access to care on the epidemiology and costs of diabetic foot ulcers is unknown.
The limitations of our study include its retrospective design, use of a national database, and cost analysis based on administrative data. As is true for any study that depends on the accurate collection of data from a wide range of institutions, missing and inaccurately recorded information or variations in recognition and coding of certain diagnoses over time are possible. In addition, the deidentified nature of a national database precludes us from tracking patients who had multiple diabetic foot ulcer admissions over the study period. The NIS is the largest record of inpatient health care data in the United States and uses extremely strict data entry requirements,12 and our cohort size of >330,000 patients helps minimize potential errors that could result from missing data. Furthermore, diabetic foot ulceration is not strictly a disease of the elderly. Diabetic patients between 45 and 54 years of age have previously been identified as a high-risk population with an increased risk of amputation.41 Although other administrative databases, such as the Medicare database, might have more longitudinal data, the NIS captures national cost data for patients of all ages. Another limitation is that our cost analysis is based on hospital costs and charges that cannot capture specific procedure-level data, leaving us to make certain assumptions about the effect of diabetic foot ulcer treatment based on multivariable modeling and other techniques. Furthermore, we were unable to capture costs associated with outpatient and posthospital subacute and rehabilitation care using NIS data. However, the results of our analyses that focus on the costs of inpatient diabetic foot ulcer care are useful for formulating future studies that can more directly assess patient- and hospital-level costs using institutional data that allow for a more detailed cost breakdown.
CONCLUSIONS
Hospital costs associated with diabetic foot ulcers are extremely high and increasing over time despite stable hospital length of stay and proportion of emergency admissions. Risk-adjusted analyses suggest that this change might be reflective of increasing charges associated with a progressively sicker patient population and revascularization aimed at limb salvage. Despite this, the overall incidence of major amputations remained stable. Limb salvage approaches that focus on ulcer prevention and early diagnosis might be more cost effective than aggressive treatment and revascularization of patients with advanced disease, because the latter approach poses a significant economic cost burden. Further studies assessing the association between inpatient diabetic foot ulcer costs and outcomes are needed to formally address the efficacy of this approach.
Supplementary Material
Footnotes
Author conflict of interest: none.
Presented at the Forty-second Annual Symposium of the Society for Clinical Vascular Surgery, Carlsbad, Calif, March 18–22, 2014.
Additional material for this article may be found online at www.jvascsurg.org.
The editors and reviewers of this article have no relevant financial relationships to disclose per the JVS policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
AUTHOR CONTRIBUTIONS
Conception and design: CH, SS, CA
Analysis and interpretation: CH, SS, NM, BP, JF, JB, CA
Data collection: SS, CA
Writing the article: CH, SS, CA
Critical revision of the article: CH, SS, NM, BP, JF, JB, CA
Final approval of the article: CH, SS, NM, BP, JF, JB, CA
Statistical analysis: SS, CA
Obtained funding: Not applicable
Overall responsibility: CA
References
- 1.American Diabetes Association. Economic costs of diabetes in the U.S. 2007. Diabetes Care. 2008;31:596–615. doi: 10.2337/dc08-9017. [DOI] [PubMed] [Google Scholar]
- 2.Connor H. Some historical aspects of diabetic foot disease. Diabetes Metab Res Rev. 2008;24(Suppl 1):S7–13. doi: 10.1002/dmrr.838. [DOI] [PubMed] [Google Scholar]
- 3.Department of Health and Human Services. Centers for Disease Control and Prevention. [Accessed December 16, 2013];Diabetes data & trends. Available at: http://apps.nccd.cdc.gov/DDTSTRS/default.aspx.
- 4.Pecoraro RE, Reiber GE, Burgess EM. Pathways to diabetic limb amputation. Basis for prevention. Diabetes Care. 1990;13:513–21. doi: 10.2337/diacare.13.5.513. [DOI] [PubMed] [Google Scholar]
- 5.Jude EB, Oyibo SO, Chalmers N, Boulton AJ. Peripheral arterial disease in diabetic and nondiabetic patients: a comparison of severity and outcome. Diabetes Care. 2001;24:1433–7. doi: 10.2337/diacare.24.8.1433. [DOI] [PubMed] [Google Scholar]
- 6.Harrington C, Zagari MJ, Corea J, Klitenic J. A cost analysis of diabetic lower-extremity ulcers. Diabetes Care. 2000;23:1333–8. doi: 10.2337/diacare.23.9.1333. [DOI] [PubMed] [Google Scholar]
- 7.Ramsey SD, Newton K, Blough D, McCulloch DK, Sandhu N, Reiber GE, et al. Incidence, outcomes, and cost of foot ulcers in patients with diabetes. Diabetes Care. 1999;22:382–7. doi: 10.2337/diacare.22.3.382. [DOI] [PubMed] [Google Scholar]
- 8.Davis WA, Norman PE, Bruce DG, Davis TM. Predictors, consequences and costs of diabetes-related lower extremity amputation complicating type 2 diabetes: the Fremantle Diabetes Study. Diabetologia. 2006;49:2634–41. doi: 10.1007/s00125-006-0431-0. [DOI] [PubMed] [Google Scholar]
- 9.Holzer SE, Camerota A, Martens L, Cuerdon T, Crystal-Peters J, Zagari M. Costs and duration of care for lower extremity ulcers in patients with diabetes. Clin Ther. 1998;20:169–81. doi: 10.1016/s0149-2918(98)80044-1. [DOI] [PubMed] [Google Scholar]
- 10.IDEAS. ICDPIC: Stata module to provide methods for translating International Classification of Diseases (Ninth Revision) diagnosis codes into standard injury categories and/or scores. [Accessed April 27, 2013]; Available at: http://ideas.repec.org/c/boc/bocode/s457028.html#biblio.
- 11.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 12.Healthcare Cost and Utlization Project – HCUP. [Accessed December 2, 2012];Introduction to the HCUP Nationwide Inpatient Sample (NIS) 2010 Available at: http://www.hcup-us.ahrq.gov/db/nation/nis/NIS_Introduction_2010.jsp.
- 13.Dodd S, Bassi A, Bodger K, Williamson P. A comparison of multivariable regression models to analyse cost data. J Eval Clin Pract. 2006;12:76–86. doi: 10.1111/j.1365-2753.2006.00610.x. [DOI] [PubMed] [Google Scholar]
- 14.Manning WG, Mullahy J. Estimating log models: to transform or not to transform? J Health Econ. 2001;20:461–94. doi: 10.1016/s0167-6296(01)00086-8. [DOI] [PubMed] [Google Scholar]
- 15. [Accessed February 24, 2014];Consumer Price Index (CPI) Conversion Factors 1774 to estimated 2024 to Convert to Dollars of 2010. Available at: http://oregonstate.edu/cla/polisci/sites/default/files/faculty-research/sahr/inflation-conversion/pdf/cv2010.pdf.
- 16.LoGerfo FW, Gibbons GW, Pomposelli FB, Jr, Campbell DR, Miller A, Freeman DV, et al. Trends in the care of the diabetic foot. Expanded role of arterial reconstruction. Arch Surg. 1992;127:617–20. doi: 10.1001/archsurg.1992.01420050145019. discussion: 620–1. [DOI] [PubMed] [Google Scholar]
- 17.Gibbons GW, Marcaccio EJ, Jr, Burgess AM, Pomposelli FB, Jr, Freeman DV, Campbell DR, et al. Improved quality of diabetic foot care, 1984 vs 1990. Reduced length of stay and costs, insufficient reimbursement. Arch Surg. 1993;128:576–81. doi: 10.1001/archsurg.1993.01420170112017. [DOI] [PubMed] [Google Scholar]
- 18.Faglia E, Mantero M, Caminiti M, Caravaggi C, De Giglio R, Pritelli C, et al. Extensive use of peripheral angioplasty, particularly infrapopliteal, in the treatment of ischaemic diabetic foot ulcers: clinical results of a multicentric study of 221 consecutive diabetic subjects. J Intern Med. 2002;252:225–32. doi: 10.1046/j.1365-2796.2002.01015.x. [DOI] [PubMed] [Google Scholar]
- 19.Zayed H, Halawa M, Maillardet L, Sidhu PS, Edmonds M, Rashid H. Improving limb salvage rate in diabetic patients with critical leg ischaemia using a multidisciplinary approach. Int J Clin Pract. 2009;63:855–8. doi: 10.1111/j.1742-1241.2007.01608.x. [DOI] [PubMed] [Google Scholar]
- 20.Larsson J, Apelqvist J, Agardh CD, Stenstrom A. Decreasing incidence of major amputation in diabetic patients: a consequence of a multi-disciplinary foot care team approach? Diabet Med. 1995;12:770–6. doi: 10.1111/j.1464-5491.1995.tb02078.x. [DOI] [PubMed] [Google Scholar]
- 21.Van Gils CC, Wheeler LA, Mellstrom M, Brinton EA, Mason S, Wheeler CG. Amputation prevention by vascular surgery and podiatry collaboration in high-risk diabetic and nondiabetic patients. The Operation Desert Foot experience. Diabetes Care. 1999;22:678–83. doi: 10.2337/diacare.22.5.678. [DOI] [PubMed] [Google Scholar]
- 22.Driver VR, Fabbi M, Lavery LA, Gibbons G. The costs of diabetic foot: the economic case for the limb salvage team. J Vasc Surg. 2010;52(Suppl 3):17S–22S. doi: 10.1016/j.jvs.2010.06.003. [DOI] [PubMed] [Google Scholar]
- 23.Krishnan S, Nash F, Baker N, Fowler D, Rayman G. Reduction in diabetic amputations over 11 years in a defined U.K. population: benefits of multidisciplinary team work and continuous prospective audit. Diabetes Care. 2008;31:99–101. doi: 10.2337/dc07-1178. [DOI] [PubMed] [Google Scholar]
- 24.Anichini R, Zecchini F, Cerretini I, Meucci G, Fusilli D, Alviggi L, et al. Improvement of diabetic foot care after the Implementation of the International Consensus on the Diabetic Foot (ICDF): results of a 5-year prospective study. Diabetes Res Clin Pract. 2007;75:153–8. doi: 10.1016/j.diabres.2006.05.014. [DOI] [PubMed] [Google Scholar]
- 25.Driver VR, Madsen J, Goodman RA. Reducing amputation rates in patients with diabetes at a military medical center: the limb preservation service model. Diabetes Care. 2005;28:248–53. doi: 10.2337/diacare.28.2.248. [DOI] [PubMed] [Google Scholar]
- 26.Driver VR, Goodman RA, Fabbi M, French MA, Andersen CA. The impact of a podiatric lead limb preservation team on disease outcomes and risk prediction in the diabetic lower extremity: a retrospective cohort study. J Am Podiatr Med Assoc. 2010;100:235–41. doi: 10.7547/1000235. [DOI] [PubMed] [Google Scholar]
- 27.van Acker K, Léger P, Hartemann A, Chawla A, Siddiqui MK. Burden of diabetic foot disorders, guidelines for management, and disparities in implementation in Europe: a systematic literature review [published online ahead of print January 27, 2014] Diabetes Metab Res Rev. doi: 10.1002/dmrr.2523. [DOI] [PubMed] [Google Scholar]
- 28.Bakker K, Apelqvist J, Schaper NC. International Working Group on Diabetic Foot Editorial Board. Practical guidelines on the management and prevention of the diabetic foot 2011 Diabetes. Metab Res Rev. 2012;28(Suppl 1):225–31. doi: 10.1002/dmrr.2253. [DOI] [PubMed] [Google Scholar]
- 29.Goodney PP, Beck AW, Nagle J, Welch HG, Zwolak RM. National trends in lower extremity bypass surgery, endovascular interventions, and major amputations. J Vasc Surg. 2009;50:54–60. doi: 10.1016/j.jvs.2009.01.035. [DOI] [PubMed] [Google Scholar]
- 30.Goldberg JB, Goodney PP, Cronenwett JL, Baker F. The effect of risk and race on lower extremity amputations among Medicare diabetic patients. J Vasc Surg. 2012;56:1663–8. doi: 10.1016/j.jvs.2012.05.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Anderson PL, Gelijns A, Moskowitz A, Arons R, Gupta L, Weinberg A, et al. Understanding trends in inpatient surgical volume: vascular interventions, 1980–2000. J Vasc Surg. 2004;39:1200–8. doi: 10.1016/j.jvs.2004.02.039. [DOI] [PubMed] [Google Scholar]
- 32.Ragnarson Tennvall G, Apelqvist J. Prevention of diabetes-related foot ulcers and amputations: a cost-utility analysis based on Markov model simulations. Diabetologia. 2001;44:2077–87. doi: 10.1007/s001250100013. [DOI] [PubMed] [Google Scholar]
- 33.Ollendorf DA, Kotsanos JG, Wishner WJ, Friedman M, Cooper T, Bittoni M, et al. Potential economic benefits of lower-extremity amputation prevention strategies in diabetes. Diabetes Care. 1998;21:1240–5. doi: 10.2337/diacare.21.8.1240. [DOI] [PubMed] [Google Scholar]
- 34.Ortegon MM, Redekop WK, Niessen LW. Cost-effectiveness of prevention and treatment of the diabetic foot: a Markov analysis. Diabetes Care. 2004;27:901–7. doi: 10.2337/diacare.27.4.901. [DOI] [PubMed] [Google Scholar]
- 35.Horswell RL, Birke JA, Patout CA., Jr A staged management diabetes foot program versus standard care: a 1-year cost and utilization comparison in a state public hospital system. Arch Phys Med Rehabil. 2003;84:1743–6. doi: 10.1016/s0003-9993(03)00477-5. [DOI] [PubMed] [Google Scholar]
- 36.Matricali GA, Dereymaeker G, Muls E, Flour M, Mathieu C. Economic aspects of diabetic foot care in a multidisciplinary setting: a review. Diabetes Metab Res Rev. 2007;23:339–47. doi: 10.1002/dmrr.706. [DOI] [PubMed] [Google Scholar]
- 37.Van Acker K, Oleen-Burkey M, De Decker L, Vanmaele R, Van Schil P, Matricali G, et al. Cost and resource utilization for prevention and treatment of foot lesions in a diabetic foot clinic in Belgium. Diabetes Res Clin Pract. 2000;50:87–95. doi: 10.1016/s0168-8227(00)00157-1. [DOI] [PubMed] [Google Scholar]
- 38.Bouter KP, Storm AJ, de Groot RR, Uitslager R, Erkelens DW, Diepersloot RJ. The diabetic foot in Dutch hospitals: epidemiological features and clinical outcome. Eur J Med. 1993;2:215–8. [PubMed] [Google Scholar]
- 39.Apelqvist J, Ragnarson-Tennvall G, Persson U, Larsson J. Diabetic foot ulcers in a multidisciplinary setting. An economic analysis of primary healing and healing with amputation. J Intern Med. 1994;235:463–71. doi: 10.1111/j.1365-2796.1994.tb01104.x. [DOI] [PubMed] [Google Scholar]
- 40.Eslami MH, Zayaruzny M, Fitzgerald GA. The adverse effects of race, insurance status, and low income on the rate of amputation in patients presenting with lower extremity ischemia. J Vasc Surg. 2007;45:55–9. doi: 10.1016/j.jvs.2006.09.044. [DOI] [PubMed] [Google Scholar]
- 41.Chen HF, Ho CA, Li CY. Age and sex may significantly interact with diabetes on the risks of lower-extremity amputation and peripheral revascularization procedures: evidence from a cohort of a half-million diabetic patients. Diabetes Care. 2006;29:2409–14. doi: 10.2337/dc06-1343. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.