Abstract
Purpose
To describe a case of Achromobacter xylosoxidans keratitis with deep involvement of the corneal stroma and discuss its management.
Observations
A 73 year-old monocular male with infectious keratitis of the right eye was referred to the Wilmer Eye Institute after a month of empiric treatment with besifloxacin. On presentation, slit lamp examination of the right eye demonstrated a diffusely edematous cornea with three areas of corneal infiltrates and an overlying epithelial defect and a 1.3 mm hypopyon in the anterior chamber. The corneal culture performed grew A. xylosoxidans. Empiric antibiotic regimen was adjusted once corneal culture susceptibility results were available. Seven days later, slit lamp examination demonstrated a resolving epithelial defect, stable infiltrates, and resolution of the hypopyon. After approximately two months of follow up with his primary ophthalmologist, he was noted to have recurrent hypopyon and infiltrates and was referred back to Wilmer. Slit lamp examination again demonstrated an epithelial defect, diffuse corneal haze, deep stromal infiltrates, and a 1 mm hypopyon. Corneal infiltrates were too deep to culture. Ultimately, the patient underwent a therapeutic penetrating keratoplasty with anterior chamber washout resulting in improvement of vision.
Conclusions and importance
The indolent progression of A. xylosoxidans keratitis may predispose patients to delayed presentation and treatment. This can result in deep stromal infection that complicates management due to poor antibiotic penetration. Deep stromal infections in A. xylosoxidans keratitis warrant the consideration of intrastromal antibiotic injection or early therapeutic penetrating keratoplasty.
Keywords: Achromobacter, Alcaligenes, Bacterial keratitis, Penetrating keratoplasty
1. Introduction
Achromobacter xylosoxidans, formerly known as Alcaligenes xylosoxidans, is considered a rare cause of bacterial keratitis. Though most cases of A. xylosoxidans keratitis resolve with topical antibiotics,1 there are reported cases where A. xylosoxidans keratitis recurred after initial improvement and required a therapeutic penetrating keratoplasty (PK) for definitive treatment.2, 3, 4, 5 The detailed clinical history of such severe cases of A. xylosoxidans keratitis is not well described in the literature. We report a case of severe A. xylosoxidans keratitis with deep involvement of the corneal stroma that spanned a total of 4 months in a patient who had worsening of symptoms despite initial improvement with topical antibiotics and ultimately required therapeutic PK.
2. Case report
A 73 year-old monocular male presented with infectious keratitis of the right eye to his outside ophthalmologist. The left eye had no light perception due to advanced glaucoma. In the right eye, he had advanced glaucoma and had a trabeculectomy and cataract surgery 13 years ago. He was on suppressive oral valacyclovir and topical steroids for presumed herpes simplex virus (HSV) stromal keratitis. He also had some degree of corneal edema and recurrent epithelial defects that had been managed with a bandage contact lens. His baseline vision was 20/70 in this eye. The infectious keratitis was initially managed by his primary ophthalmologist with besifloxacin. He was referred to the Wilmer Eye Institute when he developed a new corneal infiltrate and hypopyon after a month of therapy.
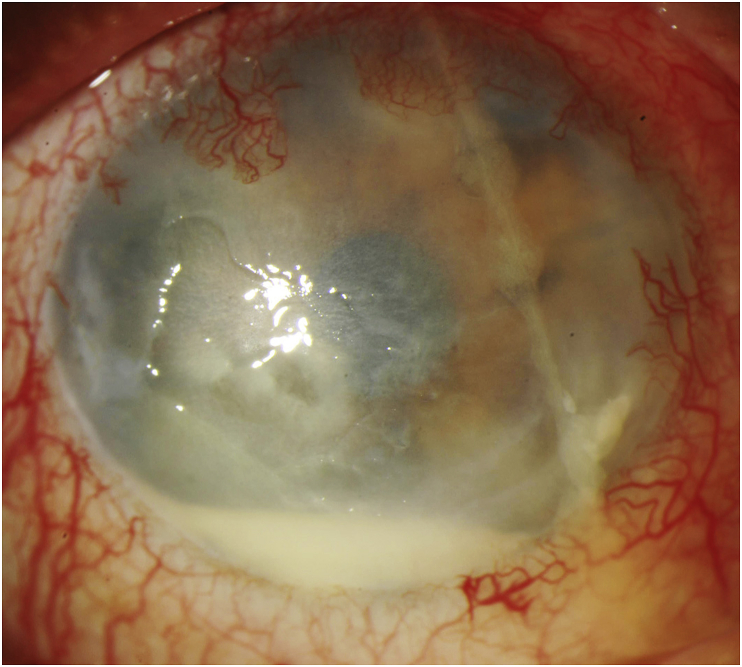
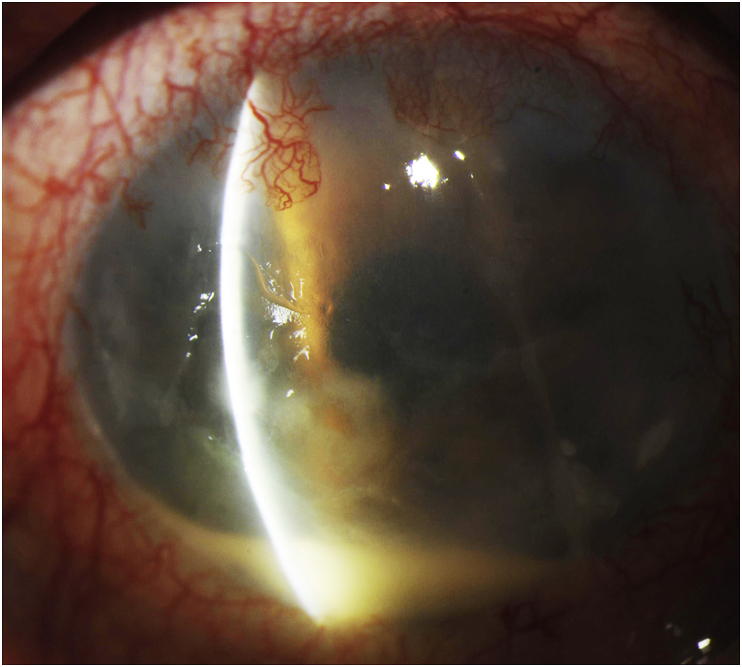
On presentation to Wilmer, the right eye had hand motion vision. Slit lamp examination of the right eye demonstrated a diffusely edematous cornea with three areas of corneal infiltrates, each with indistinct borders, and an overlying epithelial defect measuring 2.5 mm in width and 4 mm in height (Fig. 1, Fig. 2). He had a 1.3 mm hypopyon in the anterior chamber. Ophthalmic ultrasonogrophy demonstrated no vitritis to suggest endophthalmitis. Corneal cultures were obtained and hourly fortified vancomycin 25 mg/mL and tobramycin 14 mg/mL were empirically started. Due to his history of herpetic keratitis, treatment dose of oral valacyclovir was started and topical prednisolone was continued at four times a day.
Fig. 1.
Right eye slit lamp photograph – The slit-lamp exam demonstrates a diffusely edematous cornea with three areas of corneal infiltrates, an overlying epithelial defect measuring 2.5 mm in width and 4 mm in height, and a 1.3 mm hypopyon in the anterior chamber.
Fig. 2.
Right eye slit lamp photograph – The slit-lamp beam demonstrates the depth of the stromal infiltrate.
Five days later, the culture report revealed A. xylosoxidans that had resistance to tobramycin and gentamicin, intermediate susceptibility to ciprofloxacin and cefepime, and susceptibility to ceftazidime, imipenem, meropenem and trimethoprim and sulfamethoxazole.
Based on these sensitivities, fortified vancomycin and tobramycin were discontinued and the patient was started on topical polymyxin B sulfate-trimethoprim and ceftazidime 50 mg/mL. Oral valacyclovir and topical prednisolone was maintained.
Seven days later, the patient could still only see hand motion, but reported subjective improvement. Slit lamp examination demonstrated a resolving epithelial defect of 0.5 × 1 mm, stable infiltrates, and resolution of the hypopyon. The patient continued the antibiotic regimen and followed up with his primary ophthalmologist who was closer to his primary residence.
The patient was seen by his primary ophthalmologist on a weekly basis and compliant with the antibiotic regimen. One month later, his vision had improved to 20/400, which coincided with the resolution of the epithelial defect and a reduction in corneal haze. The antibiotics were discontinued one week later and the patient demonstrated slow clinical improvement at the follow up visit one week later. Two weeks after this visit, the patient was noted to have a recurrent epithelial defect with adjacent corneal infiltrate and a 0.5 mm hypopyon. Topical polymyxin B sulfate-trimethoprim and ceftazidime were restarted.
One week later, the patient returned to Wilmer for reevaluation. Slit lamp examination demonstrated an epithelial defect, diffuse corneal haze, deep stromal infiltrates, and a 1 mm hypopyon. Corneal infiltrates were too deep to culture. He was continued on polymyxin B sulfate-trimethoprim and ceftazidime 50 mg/mL based on previous culture results and susceptibility. Due to the concern for fungal keratitis given long term use of topical steroids, topical voriconazole was added. The treatment for bacterial keratitis was expanded to topical vancomycin and tobramycin. Additionally, oral valacyclovir was maintained and prednisolone was discontinued.
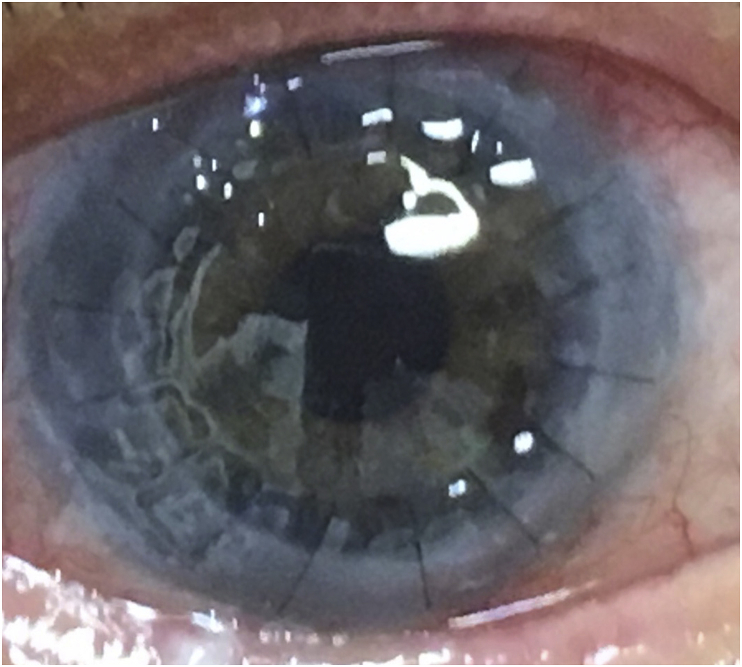
After 20 days on this regimen, the patient had no improvements in the epithelial defect, corneal infiltrates, or hypopyon. He then underwent a therapeutic PK with anterior chamber washout with intracameral injection of ceftazidime, vancomycin, and voriconazole. Cultures from the corneal button yielded moderate A. xylosoxidans growth with the same antibiotic susceptibility profile as the first culture. The patient was continued on polymyxin B sulfate-trimethoprim and ceftazidime post-operatively. Two months after the PK, the patient's vision improved to 20/150 uncorrected and pinholed to 20/60 and the graft remained clear (Fig. 3). At his last follow up visit seven months later, his uncorrected vision was 20/40.
Fig. 3.
Right eye slit lamp photograph – The corneal graft remained clear two months after penetrating keratoplasty.
3. Discussion
Achromobacter xylosoxidans is a gram-negative, water-borne organism that typically causes healthcare-associated infections in immunocompromised patients.6, 7, 8, 9 It is recognized as an emerging pathogen in patients with cystic fibrosis,10 a cause of bacteremia in cancer patients,9 and a co-inhabitant in catheter-associated urinary tract infections.11 A. xylosoxidans is a rare cause of ocular infections.
A. xylosoxidans can be confused with other nonfermentative, gram-negative rods, especially Pseudomonas species due to shared characteristics such as motility and biofilm formation.12 However, A. xylosoxidans has a peritrichous flagella, exhibits a different antibiotic susceptibility profile, and is less virulent than Pseudomonas.13 Because it is less virulent, A. xylosoxidans keratitis usually results in a less fulminant clinical course and may cause a delay in patients seeking medical attention.1,14 Various risk factors have been described for A. xylosoxidans keratitis including previous PK, topical corticosteroids use, and contact lens wear.1,2,14
Most cases of A. xylosoxidans keratitis can be successfully managed with topical antibiotics.1 The most common empiric antibiotic choices for bacterial keratitis, specifically fluoroquinolones and aminoglycosides, may not be effective against A. xylosoxidans keratitis as most A. xylosoxidans isolates are highly resistant to ciprofloxacin, gentamicin, and tobramycin.2 However, when the appropriate topical antibiotic therapy is used, A. xylosoxidans rarely leads to recurrences or a therapeutic PK.2, 3, 4, 5
The severity at presentation and clinical course of our patient can be attributed to his numerous risk factors, including chronic topical corticosteroids, HSV stromal keratitis, and contact lens wear, and his delayed presentation that allowed for deep penetration of infection. Despite initial clinical improvement after initiation of treatment with antibiotics guided by susceptibility results, the infection was persistent and resulted in recurrent hypopyon. When the infection did not improve with one month of further topical antibiotic treatment, a therapeutic PK was indicated.
Deep corneal penetration of infectious keratitis complicates management. A. xylosoxidans keratitis may result in deep infection through its indolent progression, that predisposes patients to delayed presentation and treatment, or penetration of the cornea, either iatrogenic or through injury. The affected eye of our patient acquired a deep stromal infection through a prolonged clinical course that could not be effectively treated with topical antibiotics. Two documented cases of penetration of the cornea leading to deep infection, a partial thickness corneal laceration and a post-PK eye, exhibited recurrence of infection despite topical antibiotics.4,5 Deep infection may result in poor antibiotic penetration, requiring more aggressive management. In the management of deep infectious keratitis refractory to topical antibiotics, intrastromal antibiotic injection may be an alternative to therapeutic PK.15 This may require repeated injections and was not performed in our patient because of his difficulty in following up due to living over 2 h away from our institution. Furthermore, it is important to note that this organism is often multi-drug resistant and difficult to treat.
4. Conclusions
This report highlights a severe case of A. xylosoxidans keratitis with deep involvement of the corneal stroma that could not be treated with topical antibiotics guided by susceptibility results and resulted in a therapeutic PK. The indolent progression of A. xylosoxidans keratitis may predispose patients to delayed presentation and delayed treatment. This can result in a deep corneal infection that complicates management through poor antibiotic penetration. Thus, deep infections in A. xylosoxidans keratitis warrant the consideration of intrastromal antibiotic injection or early therapeutic PK.
5. Patient consent
Consent to publish the case report was not obtained. This report does not contain any personal information that could lead to the identification of the patient.
Acknowledgments and disclosures
Funding
No funding or grant support.
Conflicts of interest
The authors have no financial disclosures.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Acknowledgements
None.
References
- 1.Reddy A.K., Garg P., Shah V., Gopinathan U. Clinical, microbiological profile and treatment outcome of ocular infections caused by Achromobacter xylosoxidans. Cornea. 2009;28(10):1100–1103. doi: 10.1097/ICO.0b013e3181a1658f. [DOI] [PubMed] [Google Scholar]
- 2.Spierer O., Monsalve P., O'Brien T. Clinical features, antibiotic susceptibility profiles, and outcomes of infectious keratitis caused by Achromobacter xylosoxidans. Cornea. 2016;35(5):626–630. doi: 10.1097/ICO.0000000000000798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Linke S.J., Skevas C., Richard G., Katz T. Bilateral Achromobacter xylosoxidans keratitis after laser in situ keratomileusis. J Cataract Refract Surg. 2010;36(6):1045–1047. doi: 10.1016/j.jcrs.2010.03.024. [DOI] [PubMed] [Google Scholar]
- 4.Huang Z.L., Chen Y.F., Chang S.W., Lin K.K., Hsiao C.H. Recurrent Alcaligenes xylosoxidans keratitis. Cornea. 2005;24(4):489–490. doi: 10.1097/01.ico.0000151562.17366.77. doi:00003226-200505000-00023 [pii] [DOI] [PubMed] [Google Scholar]
- 5.Pan T.H., Heidemann D.G., Dunn S.P., Chow C.Y., Gossage D. Delayed onset and recurrent Alcaligenes xylosoxidans keratitis. Cornea. 2000;19(2):243–245. doi: 10.1097/00003226-200003000-00022. [DOI] [PubMed] [Google Scholar]
- 6.Reverdy M.E., Freney J., Fleurette J. Nosocomial colonization and infection by Achromobacter xylosoxidans. J Clin Microbiol. 1984;19(2):140–143. doi: 10.1128/jcm.19.2.140-143.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gómez-Cerezo J., Suárez I., Ríos J.J. Achromobacter xylosoxidans bacteremia: a 10-year analysis of 54 cases. Eur J Clin Microbiol Infect Dis. 2003;22(6):360–363. doi: 10.1007/s10096-003-0925-3. [DOI] [PubMed] [Google Scholar]
- 8.Granowitz E.V., Keenholtz S.L. A pseudoepidemic of Alcaligenes xylosoxidans attributable to contaminated saline. Am J Infect Contr. 1998;26(2):146–148. doi: 10.1016/s0196-6553(98)80035-7. [DOI] [PubMed] [Google Scholar]
- 9.Aisenberg G., Rolston K.V., Safdar A. Bacteremia caused by Achromobacter and Alcaligenes species in 46 patients with cancer (1989-2003) Cancer. 2004;101(9):2134–2140. doi: 10.1002/cncr.20604. [DOI] [PubMed] [Google Scholar]
- 10.Talbot N.P., Flight W.G. Severe Achromobacter xylosoxidans infection and loss of sputum bacterial diversity in an adult patient with cystic fibrosis. Paediatr Respir Rev. 2016;20(suppl):27–29. doi: 10.1016/j.prrv.2016.06.011. [DOI] [PubMed] [Google Scholar]
- 11.Azevedo A.S., Almeida C., Melo L.F., Azevedo N.F. Impact of polymicrobial biofilms in catheter-associated urinary tract infections. Crit Rev Microbiol. 2017;43(4):423–439. doi: 10.1080/1040841X.2016.1240656. [DOI] [PubMed] [Google Scholar]
- 12.Igra-Siegman Y., Chmel H., Cobbs C. Clinical and laboratory characteristics of Achromobacter xylosoxidans infection. J Clin Microbiol. 1980;11(2):141–145. doi: 10.1128/jcm.11.2.141-145.1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yabuuchi E., Oyama A. Achromobacter xylosoxidans n. sp. from human ear discharge. Jpn J Microbiol. 1971;15(5):477–481. doi: 10.1111/j.1348-0421.1971.tb00607.x. [DOI] [PubMed] [Google Scholar]
- 14.Wiley L., Bridge D.R., Wiley L.A., Odom J.V., Elliott T., Olson J.C. Bacterial biofilm diversity in contact lens-related disease: emerging role of Achromobacter, Stenotrophomonas, and Delftia. Investig Ophthalmol Vis Sci. 2012;53(7):3896–3905. doi: 10.1167/iovs.11-8762. [DOI] [PubMed] [Google Scholar]
- 15.Liang S.Y.W., Lee G.A. Intrastromal injection of antibiotic agent in the management of recalcitrant bacterial keratitis. J Cataract Refract Surg. 2011;37(5):960–962. doi: 10.1016/j.jcrs.2011.03.005. [DOI] [PubMed] [Google Scholar]