Abstract
Background
The safety and efficacy of the Woven EndoBridge (WEB) for the treatment of naïve intracranial aneurysms has been confirmed.
Purpose
To analyze the safety and efficacy of the WEB in the treatment of recurrent aneurysms.
Methods
Anatomical and clinical results in consecutive patients with a recurrent aneurysm, who were treated using the WEB device in two French neurointerventional centers, were evaluated.
Results
Seventeen patients with 17 aneurysms were included. Treatment was feasible in 16 patients. In seven patients (41.2%), ancillary devices were used. Permanent morbidity due to a thromboembolic complication occurred in one patient (5.9%). There was no mortality. Follow-up angiographic studies were available for 15 patients after a mean of 12.1±6.1 months. Rates of complete occlusion, neck remnant, and aneurysm remnant were 33.3%, 40.0%, and 26.7%, respectively.
Conclusions
Treatment of recurrent aneurysms using the WEB device may be reasonably safe and effective.
Keywords: aneurysm, device, intervention, technique, material
Introduction
A drawback of aneurysm coiling remains the risk of aneurysm recurrence, which is estimated to happen in around 20% of cases, necessitating re-treatment in around 10%.1 Recurrence and re-treatment rates for previously clipped aneurysms are much less well studied but are thought to be lower.2 Although the decision about whether a recurrent aneurysm should be treated, and by which technique, varies between different physicians,3 it was shown that both coiling and clipping are feasible and reasonably safe options for this purpose.4 5
Rather high recurrence rates are reported with repeated coil occlusion of previously coiled aneurysms.5 Furthermore, endovascular treatment of recurrent aneurysms can be challenging owing to the often-unfavorable configuration of the aneurysm remnant; instead of a spherical shape, they often present the specific anatomical configuration of a wide neck combined with a shallow height, due to compacted coils in the aneurysm dome.
The WEB device (Woven EndoBridge aneurysm embolization system; Sequent Medical, Aliso Viejo, California, USA) may thus be a promising option for this purpose as it has a barrel shape, which should hypothetically conform optimally to the recurrent aneurysm sac. The safety and efficacy of this intrasaccular flow disrupter has been confirmed in several multicenter studies.6–15 To date, no reports exist on the feasibility and safety of treating recurrent aneurysms with this device. We present in this paper the combined experience of two high-volume neurointerventional centers.
Materials and methods
Patient population
This study was performed after approval of the local institutional review board and owing to its retrospective design, informed consent was waived.
After a thorough review of the institutional databases from January 2011 to December 2016, all patients who had undergone endovascular re-treatment of a recurrent aneurysm using the WEB device in the two participating centers were identified and included. At both institutions, the treatment indications were discussed in a multidisciplinary neurovascular meeting among neurosurgeons, vascular neurologists, and neuroradiologists. The WEB device was mainly chosen for recurrent aneurysms with a wide neck and an unfavorable configuration for coil occlusion.
For each patient and aneurysm, we collected the following data: age; sex; initial aneurysm status (ruptured or unruptured); aneurysm location; size of the initial aneurysm (maximal transverse diameter and height); neck diameter and size of the recurrent aneurysm (maximal transverse diameter and height); dome-to-neck and aspect ratio; number, date, and type of previous treatments; type and size of the WEB device; ancillary treatment methods, such as stents, coils, or remodeling balloons; preoperative clinical status measured on the modified Rankin Scale (mRS).
Interventional procedure
Senior interventional neuroradiologists performed the treatments with all patients under general anesthesia in a biplane angiosuite. Three-dimensional rotational angiography was performed to choose the working projection. Treatments were performed through the femoral access route with a triaxial approach.
Anticoagulation and antiplatelet medication was managed according to the center’s protocols. All interventions were performed after systemic administration of heparin (50 IU/kg of body weight). In both centers, embolization of asymptomatic, non-ruptured aneurysms is performed under routine acetylsalicylic acid administration, which is continued with a dose of 75–160 mg for 1 month after the treatment; dual antiplatelet therapy with acetylsalicylic acid and either 75 mg of clopidogrel or 180 mg of ticagrelor (the latter administered as a 90 mg dose in the morning and in the evening) per day is usually begun 3–7 days before the treatment if it is considered possible that intraluminal implants may be necessary. If no stent is placed, Plavix or ticagrelor is discontinued after the intervention. If a stent is applied during treatment, dual antiplatelet medication is typically maintained for 3 months after the procedure; after this period, acetylsalicylic acid is given for another 9 months as a single antiplatelet agent.
Complications and clinical follow-up
Complications—ischemic, hemorrhagic, and other types—were assessed during the procedure, within the hospital stay after the intervention, and during patient follow-up. In both participating centers, patient examinations performed by neurointerventionalists are regularly performed as an important part of patient follow-up. Clinical outcome was graded according to the mRS. Treatment morbidity was defined as any change in the mRS score compared with the score before the procedure.
Clinical and imaging follow-up
Imaging follow-up was performed using DSA and/or MR angiography according to institutional protocols—in general, a first DSA is scheduled at 3–6 months, with a second DSA 12–18 months after the procedure. We evaluated anatomic and clinical outcome at the latest available follow-up or before re-treatment of the target aneurysm.
Aneurysm occlusion
Follow-up aneurysm occlusion was graded by an independent interventional neuroradiologist from another institution (CM), who was not involved in the treatment of the study population. A three-grade scale, used in three large prospective multicenter studies, with the items complete occlusion, residual neck, and residual aneurysm, was applied.7 8 15 Opacification of the WEB device’s recess was graded as complete occlusion. Aneurysm occlusion was assessed on DSA studies.
Statistical analysis
Descriptive statistics were used. Numerical values are given as mean±SD.
Results
Patients and aneurysms
Seventeen patients (10 female, mean age 52.9±9 years; range 40–68 years) with 17 aneurysms were included. Eight aneurysms were located at the middle cerebral artery bifurcation, five at the basilar artery, three at the termination of the internal carotid artery and one at the posterior communicating artery. Twelve aneurysms presented initially with a rupture. Fifteen aneurysms were initially treated by coiling, one by clipping, and another one using a WEB device. Fourteen aneurysms were treated once before the re-treatment using the WEB, two aneurysms twice, and one aneurysm three times. The mean time from first treatment to re-treatment using the WEB was 84.2±86.2 months. Mean height and width of the initial aneurysm was 10±3.7 mm and 9±4 mm, respectively. The initial aneurysm size was not assessable in four patients as their initial treatment took place more than 15 years ago and pretreatment angiograms were not available. Mean height, width, and neck diameter of the recurrent aneurysm were 6.0±3 mm, 7.5±3.5 mm, and 5.3±2.4 mm, respectively. Twelve of 17 aneurysms (70.6%) had a neck diameter of ≥4 mm and were thus considered to be wide-necked.7 Detailed information on individual patients and aneurysm characteristics are given in table 1.
Table 1.
Patient and aneurysm characteristics
| No. | Localization (R/NR)* |
Initial aneurysm | Previous treatments (months before WEB treatment) | Aneurysm remnant before WEB treatment | WEB type | Other devices | |||
| Dome (mm) | Width (mm) | Neck (mm) | Dome (mm) | Width (mm) | |||||
| 1 | MCA (NR) | 6.0 | 7.0 | Coiling (12) | 2.6 | 5.4 | 6.4 | DL 6×3 mm | 4 Coils |
| 2 | ICA (R) | 13.1 | 8.4 | Coiling (38) | 5.3 | 3.6 | 8.2 | DL 7×5 mm | Stent |
| 3 | MCA (NR) | 16.4 | 17.5 | Coiling (17) | 10.0 | 13.5 | 14.9 | DL 11×9 mm | 4 Coils |
| 4 | MCA (R) | 7.3 | 4.2 | Coiling (67, 82) | 3.2 | 3.9 | 3.0 | SLS 4 mm | – |
| 5 | MCA (NR) | 10.1 | 8.9 | Coiling (60, 64) | 7.8 | 7.2 | 14.2 | SL 9×4 mm | Stent |
| 6 | BA (R) | N/A† | Coiling (247) | 3.7 | 6.5 | 7.4 | SL 6×3 mm | Balloon, 3 coils, stent | |
| 7 | ICA (NR) | 6.0 | 8.0 | Coiling (161) | 1.9 | 4.9 | 3.2 | SL 4×3 mm | – |
| 8 | BA (R) | N/A† | Coiling (73, 114, 205) | 4.0 | 5.5 | 4.5 | SL 6×3 mm | – | |
| 9 | BA (NR) | 8.4 | 6.3 | Coiling (13) | 3.6 | 2.4 | 4.4 | SL 5×3 mm | – |
| 10 | BA (R) | 11.5 | 9.2 | WEB (40) | 7.1 | 4.4 | 8.1 | SL 7×3 mm | Stent |
| 11 | MCA (R) | N/A† | Clipping (212) | 5.4 | 2.3 | 5.3 | SL 5×3 mm | – | |
| 12 | BA (R) | 6.2 | 7.6 | Coiling (28) | 5.0 | 5.0 | 7.7 | DL 4×4 mm | – |
| 13 | MCA (R) | 15.0 | 10.0 | Coiling (15) | 10.5 | 7.9 | 10.8 | DL 8×6 mm | Balloon |
| 14 | ICA (R) | N/A† | Coiling (216) | 4.8 | 6.1 | 9.5 | SLS 8 mm | – | |
| 15 | MCA (R) | 13.3 | 16.3 | Coiling (50) | 6.2 | 11.0 | 8.8 | SL 8×10 mm | – |
| 16 | PComA (R) | 6.0 | 4.0 | Coiling (29) | 4.0 | 4.0 | 3.8 | SL 4×3 mm | – |
| 17 | MCA (R) | 11.0 | 9.0 | Coiling (3) | 4.2 | 9.0 | 8.1 | SLS 7 mm | – |
*Ruptured/non-ruptured.
†Initial angiograms not available.
BA, basilar artery; ICA, internal carotid artery; MCA, middle cerebral artery; PComA, posterior communicating artery.
Treatment
Endovascular treatment of the recurrent aneurysm using the WEB device was possible in 16 of 17 aneurysms. Treatment failure was observed in one previously clipped middle cerebral artery aneurysm (patient 11) because the device could not be anchored in the aneurysm remnant without risking protrusion into the bifurcation branches. In seven patients (41.2%), ancillary devices (coils, stents, remodeling balloons) were applied (see table 1 for detailed information). Balloons and/or stents to prevent or reduce protrusion of the WEB into the parent artery were applied in four patients (23.5%). Coils were additionally used in the case of residual aneurysm perfusion in three patients (17.6%). Nine patients received dual antiplatelet therapy before treatment. Illustrative cases are shown in figures 1–3.
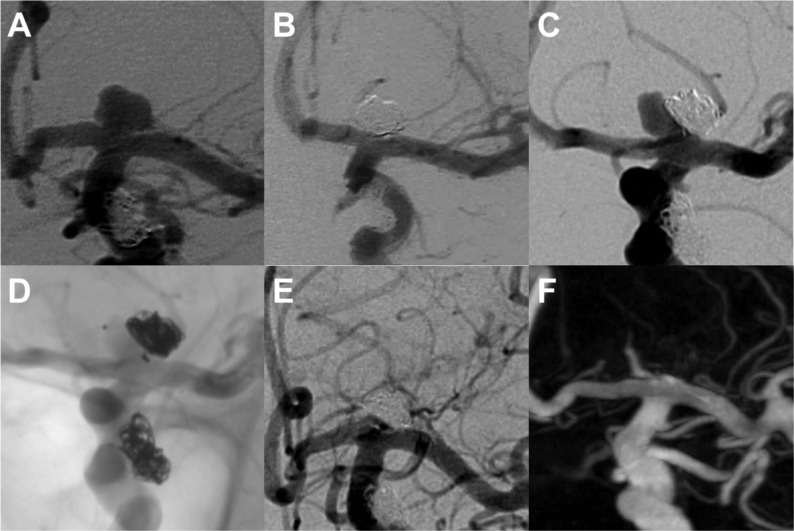
Figure 1.
Unruptured aneurysm of the left internal carotid artery (ICA) terminus (A), treated by coiling (B). About 14 years later, a large recurrence (C) was treated using a WEB SL (D). Control DSA (E) including 3D DSA (F with metal subtraction) after 11 months confirms complete occlusion. Note a second aneurysm of the intracranial ICA with stable occlusion after the initial endovascular treatment.
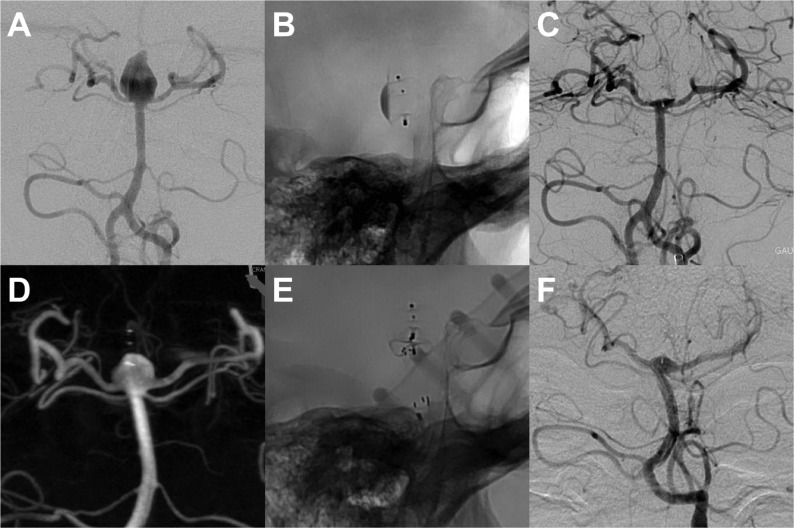
Figure 2.
Ruptured aneurysm (A) of the basilar apex that was treated with a WEB DL device in the acute phase. The profile projection in (B) depicts the device with contrast stasis in the mesh. The final result was a small neck remnant (C). A constantly growing aneurysm recurrence. (D) was treated 40 months later using a WEB SL device (E). For protection of the right P1 segment a self-expanding stent (Enterprise 4×16 mm) was placed. Follow-up after 7 months shows a small neck remnant (F).
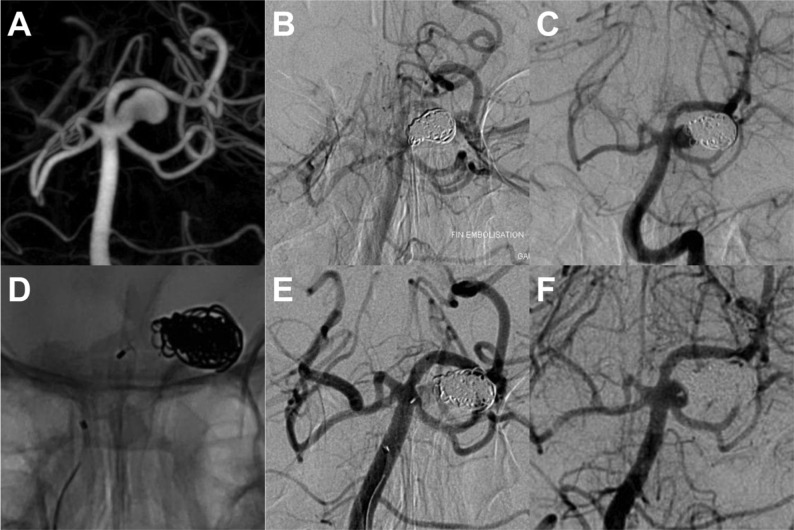
Figure 3.
Unruptured aneurysm of the basilar artery at the ostium of the left superior cerebellar artery (A). In a first session, the aneurysm was treated with the remodeling, resulting in complete occlusion (B). A growing aneurysm recurrence (C) was treated 13 months after the initial intervention by placing a WEB SL device (D). A late phase control run depicted a slowed down intra-aneurysmal blood circulation (E). Six-month DSA follow-up shows a neck remnant (F).
Complications
No hemorrhagic or technical complications occurred. Thromboembolic complications were observed in four of 17 patients (23.5%), three of whom (17.6%) reported neurological symptoms after treatment. However, permanent neurological deficit was present in only one patient (5.9%) with a modification of the mRS score from 0 to 1. One patient (5.9%) showed an amelioration of the mRS score from 3 to 2 during follow-up because he recovered from his initial hematoma caused by the aneurysm rupture. Additionally, one periprocedural intracranial vasospasm (5.9%) without clinical consequences occurred. We observed no treatment-related complications beyond the periprocedural period. One patient died 15 months after treatment owing to a non-small-cell lung cancer.
Anatomical results at follow-up
Mean follow-up after treatment was 12.1±6.1 months. Follow-up was missing in one patient who refused further imaging. The aneurysm in which treatment failed was excluded from further statistical analysis. At latest imaging follow-up 5 of 15 aneurysms followed up were completely occluded (33.3%), six showed a neck remnant (40%) and four an aneurysm remnant (26.7%). Two patients with aneurysm remnants at follow-up underwent re-treatment after 6 months and 5 months, respectively. Specific information about anatomical and clinical outcome is given in table 2.
Table 2.
Anatomical and clinical outcome
| No | Follow-up (months) | Aneurysm occlusion | Clinical outcome | |
| Follow-up | mRS score before treatment | mRS score at follow-up | ||
| 1 | 2 | Neck remnant | 0 | 0 |
| 2 | 24 | Neck remnant | 0 | 0 |
| 3 | 7 | Aneurysm remnant | 0 | 1 |
| 4 | 15 | Aneurysm remnant | 0 | 0 |
| 5 | 13 | Neck remnant | 0 | 0 |
| 6 | 18 | Complete occlusion | 0 | 0 |
| 7 | 11 | Complete occlusion | 0 | 0 |
| 8 | 12 | Complete occlusion | 1 | 1 |
| 9 | 6 | Neck remnant | 0 | 0 |
| 10 | 13 | Neck remnant | 1 | 1 |
| 11 | 12 | Treatment failure | 0 | 0 |
| 12 | 20 | Neck remnant | 0 | 0 |
| 13 | 18 | Aneurysm remnant | 3 | 2 |
| 14 | N/A* | N/A* | 0 | N/A* |
| 15 | 7 | Aneurysm remnant | 4 | 4 |
| 16 | 12 | Complete occlusion | 0 | 0 |
| 17 | 13 | Complete occlusion | 0 | 0 |
*No follow-up available.
mRS, modified Rankin scale.
Discussion
Our series is the first to show that the WEB device—either alone or in conjunction with other devices— can be used for the treatment of recurrent aneurysms with overall favorable anatomic and clinical results.
Complete occlusion and neck remnant at follow-up imaging was observed in 33.3% and 40.0% of all aneurysms, which can be considered a good result given the complex anatomy and the size of the aneurysm recurrences in our study population. These results are comparable to those of two multicenter studies investigating the WEB device for the treatment of naïve aneurysms, in which adequate occlusion (grouping complete occlusion and neck remnant in one category) was described in 79.3%8 at 1 year in the French Observatory and in 85.4% at 6 months in the WEBCAST study.7 In our study we evaluated aneurysm occlusion by using the three-grade scale previously used in three large prospective multicenter series.7 8 15 Although other scales have been proposed they are less frequently applied.16 17 It has been shown that opacification of the WEB’s recess is equivalent to complete occlusion, making grade AB in the four-grade WEB Occlusion Scale dispensable.18 Furthermore, reporting aneurysm occlusion with a three-grade scale may make comparison of the anatomical results using the WEB with historical coiling data more reliable.
The choice of the WEB device for re-treatment was mainly based on anatomical considerations—that is, when it was estimated that coiling of the recurrent aneurysm would not be reasonable owing to its configuration. Indeed, 70.6% of the aneurysms in the present series had wide neck (≥4 mm). However, endovascular coil occlusion—if technically possible—of previously coiled aneurysms remains a safe and effective option.19 Durable aneurysm occlusion after a second endovascular treatment was described in 50–84%4 5 19–22 in consecutive, mostly single-center, series.
In our series there was no mortality, two cases (11.8%) of transient and one case (5.9%) of permanent morbidity (mRS 1), the latter related to a thromboembolic event. Thromboembolic complications were seen in 23.5% of the patients (17.6% symptomatic), whereas no hemorrhagic complications occurred. The rate of thromboembolic complications is most probably attributable to the anatomic configuration of the aneurysm remnants, as only complex aneurysm remnants were chosen for treatment with the WEB that presented with a wide neck—a known risk factor for thrombus formation23—and a shallow depth due to compacted coils at the aneurysm dome; however, one has to bear in mind that only one patient had a permanent neurological deficit. Thromboembolic events, including any appearance of thrombus (symptomatic or asymptomatic), were observed in 15% of patients in the pooled patient population of the WEBCAST trial and the French Observatory.6 In a recent meta-analysis of the WEB device, the pooled rate of thromboembolic events was 8%.24
Endovascular treatment of recurrent intracranial aneurysms using coils is generally considered to be safe. A multicenter study concluded that endovascular re-treatment of recurrent aneurysms poses low risks for patients with a risk for death or permanent major disability of 1.3% per patient and 1.1% per procedure; the authors concluded that those risks might even be lower than those of the initial treatment.25 Henkes et al also corroborated this statement in a large single-center series in which permanent deficit and death was observed in 2.9% and 0.3% of patients during the first re-treatment of an aneurysm recurrence.5 On the other hand, 10% of permanent morbidity attributed to thromboembolic complications occurring in 20% of their patients was reported in a study by Park et al.26
In our series, ancillary devices were used in 41.2% of the patients (balloons and/or stents to prevent or reduce protrusion of the WEB in 23.5%; coils in case of residual aneurysm perfusion in 17.6%). This number is rather high and may reflect the complex anatomy of the recurrent aneurysms. In an analysis of the pooled populations of the French Observatory and the WEBCAST study, ancillary devices were used in 10%; however, that study population consisted predominantly of patients with naïve aneurysms.6
Owing to the small size of our sample it was not possible to perform a reliable analysis of aneurysm factors, such as the influence of the size of the sac or the neck on treatment results with the WEB device. In other studies, the initial aneurysm size was identified as the main predictor of stable occlusion after a second endovascular coil occlusion of a recurrent aneurysm.5 20 In their single-center series, Dorfer et al state that coiling of a recurrent aneurysm is more often successful if the mechanism of recanalization is coil compaction; conversely, they state that ‘real’ aneurysm regrowth makes endovascular treatment less likely.4 When using the WEB for the re-treatment of recurrent aneurysms one should pay attention to the appropriate sizing of the device, which is available in diameters of between 4 and 11 mm and heights from 3 to 9 mm, usually by a slight oversizing the lateral dimensions.
The question remains how to improve the results of the endovascular treatment for large recurrences and recurrent, initially large aneurysms. One possibility may be to use self-expanding stents as they may (a) facilitate endothelialization of the aneurysm neck and (b) modify aneurysm hemodynamics, either by a direct ‘flow-diverting effect’ of the stent mesh itself or by changing the angulation of the parent artery.27 Indeed, it was shown that stent implantation may reduce the rates of further recanalization at repeat embolization.28 Also, the use of flow diverters for the endovascular treatment of recurrent aneurysms was described with acceptable morbidity/mortality and encouraging occlusion rates.29 30 These devices, however, have been used rarely in bifurcation aneurysms, which constitute the major part of our study population.31 Most importantly the long-term effect of flow diverters on covered bifurcation branches and perforating arteries is not yet fully understood and includes risks associated with a prolonged dual antiplatelet regimen.
Clipping of recurrent aneurysms is a valuable alternative to endovascular therapy—in particular, for previously coiled aneurysms.4 32 33 However, also for this technique non-negligible morbidity and mortality rates have to be balanced with generally low hemorrhage rates.34 For previously clipped aneurysms, Kivelev et al observe that ‘dissection of the target area is commonly onerous’ because of ‘conglomeration of old clip(s), vessels, and surrounding brain or cranial nerves incorporated into tight scar tissue'.33 Interestingly, the only treatment attempt that failed in our series occurred in the single patient presenting with an aneurysm recurrence after clipping. Pierot et al stated in a small series from 1999 that endovascular treatment of postoperative aneurysm remnants is more technically challenging than treatment of naïve aneurysms.35 They hypothesized that because the clip is already in place or postoperative perianeurysmal scarring is present, the aneurysm remnant is more rigid, leading to stronger ‘kickback’ of the coil loops into the parent vessel.
Our study has some limitations, primarily its retrospective design and the relatively small patient population. Another limitation is that we did not consider the different mechanisms of aneurysm recurrence—that is, coil compaction versus aneurysm growth. Moreover, antiplatelet regimens were inhomogeneous in our study population, possibly affecting individual aneurysm occlusion and thromboembolic complications.
In conclusion, endovascular treatment of recurrent aneurysms using the WEB device is feasible and may be an effective and reasonably safe option. Possible indications for the WEB device in the treatment of recurrent aneurysms are summarized in box. Further research is warranted to identify those patients with a high likelihood of treatment success. An individualized approach remains necessary to define the best treatment for every patient. Possible options range from coiling with or without balloons and stents to intraluminal flow diversion and intrasaccular flow disruption to open surgery.
Box. Indications for the WEB device in recurrent aneurysms.
Bifurcation aneurysm
Recurrence after coiling
Coil compaction
Configuration suitable for WEB device
Footnotes
Contributors: MG: Substantial contributions to the conception or design of the work; acquisition, analysis and interpretation of data; drafting the work; final approval of the version to be published; agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. SS, ACJ, G-EM, CC, LP: Substantial contributions to the conception or design of the work; acquisition, analysis and interpretation of data for the work; revising the work critically for important intellectual content; final approval of the version to be published; agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. CM: Analysis and interpretation of data.
Competing interests: CC: Consultancy of Sequent Medical, MicroVention, Stryker and Codman. LP: Consultancy of Sequent Medical, MicroVention, Neuravi, Penumbra, Balt.
Ethics approval: This study was performed after approval of the local institutional review board and owing to its retrospective design, informed consent was waived.
Provenance and peer review: Not commissioned; externally peer reviewed.
Correction notice: Since this article was first published online first its open access status has been removed.
References
- 1. Ferns SP, Sprengers ME, van Rooij WJ, et al. Coiling of intracranial aneurysms: a systematic review on initial occlusion and reopening and retreatment rates. Stroke 2009;40:e523–9. 10.1161/STROKEAHA.109.553099 [DOI] [PubMed] [Google Scholar]
- 2. Tsutsumi K, Ueki K, Morita A, et al. Risk of aneurysm recurrence in patients with clipped cerebral aneurysms. Stroke 2001;32:1191–4. [DOI] [PubMed] [Google Scholar]
- 3. Daugherty WP, Rad AE, White JB, et al. Observer agreement regarding the necessity of retreatment of previously coiled recurrent cerebral aneurysms. AJNR Am J Neuroradiol 2011;32:566–9. 10.3174/ajnr.A2336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Dorfer C, Gruber A, Standhardt H, et al. Management of residual and recurrent aneurysms after initial endovascular treatment. Neurosurgery 2012;70:537–54. 10.1227/NEU.0b013e3182350da5 [DOI] [PubMed] [Google Scholar]
- 5. Henkes H, Fischer S, Liebig T, et al. Repeated endovascular coil occlusion in 350 of 2759 intracranial aneurysms: safety and effectiveness aspects. Neurosurgery 2006;58:224–32. 10.1227/01.NEU.0000194831.54183.3F [DOI] [PubMed] [Google Scholar]
- 6. Pierot L, Spelle L, Molyneux A, et al. Clinical and anatomical follow-up in patients with aneurysms treated with the WEB device: 1-year follow-up report in the cumulated population of 2 prospective, multicenter series (WEBCAST and French Observatory). Neurosurgery 2016;78:133–41. 10.1227/NEU.0000000000001106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Pierot L, Costalat V, Moret J, et al. Safety and efficacy of aneurysm treatment with WEB: results of the WEBCAST study. J Neurosurg 2016;124:1250–6. 10.3171/2015.2.JNS142634 [DOI] [PubMed] [Google Scholar]
- 8. Pierot L, Moret J, Turjman F, et al. WEB treatment of intracranial aneurysms: clinical and anatomic results in the French observatory. AJNR Am J Neuroradiol 2016;37:655–9. 10.3174/ajnr.A4578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Fiorella D, Molyneux A, Coon A, et al. Demographic, procedural and 30-day safety results from the WEB Intra-saccular Therapy Study (WEB-IT). J Neurointerv Surg 2017;9:1191–6. 10.1136/neurintsurg-2016-012841 [DOI] [PubMed] [Google Scholar]
- 10. Pierot L, Klisch J, Liebig T, et al. WEB-DL endovascular treatment of wide-neck bifurcation aneurysms: long-term results in a European series. AJNR Am J Neuroradiol 2015;36:2314–9. 10.3174/ajnr.A4445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Pierot L, Liebig T, Sychra V, et al. Intrasaccular flow-disruption treatment of intracranial aneurysms: preliminary results of a multicenter clinical study. AJNR Am J Neuroradiol 2012;33:1232–8. 10.3174/ajnr.A3191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Pierot L, Moret J, Turjman F, et al. WEB treatment of intracranial aneurysms: feasibility, complications, and 1-month safety results with the WEB DL and WEB SL/SLS in the French observatory. AJNR Am J Neuroradiol 2015;36:922–7. 10.3174/ajnr.A4230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Pierot L, Klisch J, Cognard C, et al. Endovascular WEB flow disruption in middle cerebral artery aneurysms: preliminary feasibility, clinical, and anatomical results in a multicenter study. Neurosurgery 2013;73:27–35. 10.1227/01.neu.0000429860.04276.c1 [DOI] [PubMed] [Google Scholar]
- 14. Pierot L, Arthur A, Spelle L, et al. Current evaluation of the safety and efficacy of aneurysm treatment with the WEB device. AJNR Am J Neuroradiol 2016;37:586–7. 10.3174/ajnr.A4702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Pierot L, Gubucz I, Buhk JH, et al. Safety and efficacy of aneurysm treatment with the WEB: results of the WEBCAST 2 study. AJNR Am J Neuroradiol 2017;38:1151–5. 10.3174/ajnr.A5178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Fiorella D, Arthur A, Byrne J, et al. Interobserver variability in the assessment of aneurysm occlusion with the WEB aneurysm embolization system. J Neurointerv Surg 2015;7:591–5. 10.1136/neurintsurg-2014-011251 [DOI] [PubMed] [Google Scholar]
- 17. Caroff J, Mihalea C, Tuilier T, et al. Occlusion assessment of intracranial aneurysms treated with the WEB device. Neuroradiology 2016;58:887–91. 10.1007/s00234-016-1715-9 [DOI] [PubMed] [Google Scholar]
- 18. Lubicz B, Klisch J, Gauvrit JY, et al. WEB-DL endovascular treatment of wide-neck bifurcation aneurysms: short- and midterm results in a European study. AJNR Am J Neuroradiol 2014;35:432–8. 10.3174/ajnr.A3869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Renowden SA, Koumellis P, Benes V, et al. Retreatment of previously embolized cerebral aneurysms: the risk of further coil embolization does not negate the advantage of the initial embolization. AJNR Am J Neuroradiol 2008;29:1401–4. 10.3174/ajnr.A1098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mascitelli JR, Oermann EK, De Leacy RA, et al. Predictors of treatment failure following coil embolization of intracranial aneurysms. J Clin Neurosci 2015;22:1275–81. 10.1016/j.jocn.2015.03.002 [DOI] [PubMed] [Google Scholar]
- 21. Slob MJ, Sluzewski M, van Rooij WJ, et al. Additional coiling of previously coiled cerebral aneurysms: clinical and angiographic results. AJNR Am J Neuroradiol 2004;25:1373–6. [PMC free article] [PubMed] [Google Scholar]
- 22. Sedat J, Chau Y, Moubarak K, et al. Endovascular treatment of recurrent coiled aneurysms: assessment of complications and rebleeding during a decade in a single center. Interv Neuroradiol 2012;18:14–9. 10.1177/159101991201800102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Soeda A, Sakai N, Sakai H, et al. Thromboembolic events associated with Guglielmi detachable coil embolization of asymptomatic cerebral aneurysms: evaluation of 66 consecutive cases with use of diffusion-weighted MR imaging. AJNR Am J Neuroradiol 2003;24:127–32. [PMC free article] [PubMed] [Google Scholar]
- 24. Asnafi S, Rouchaud A, Pierot L, et al. Efficacy and safety of the Woven EndoBridge (WEB) device for the treatment of intracranial aneurysms: a systematic review and meta-analysis. AJNR Am J Neuroradiol 2016;37:2287–92. 10.3174/ajnr.A4900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ringer AJ, Rodriguez-Mercado R, Veznedaroglu E, et al. Defining the risk of retreatment for aneurysm recurrence or residual after initial treatment by endovascular coiling: a multicenter study. Neurosurgery 2009;65:311–5. 10.1227/01.NEU.0000349922.05350.96 [DOI] [PubMed] [Google Scholar]
- 26. Park HK, Horowitz M, Jungreis C, et al. Periprocedural morbidity and mortality associated with endovascular treatment of intracranial aneurysms. AJNR Am J Neuroradiol 2005;26:506–14. [PMC free article] [PubMed] [Google Scholar]
- 27. Gao B, Baharoglu MI, Cohen AD, et al. Stent-assisted coiling of intracranial bifurcation aneurysms leads to immediate and delayed intracranial vascular angle remodeling. AJNR Am J Neuroradiol 2012;33:649–54. 10.3174/ajnr.A2841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Cho YD, Lee JY, Seo JH, et al. Does stent implantation improve the result of repeat embolization in recanalized aneurysms? Neurosurgery 2012;71 (2 Suppl Operative):ons253–9. 10.1227/NEU.0b013e3182647a97 [DOI] [PubMed] [Google Scholar]
- 29. Kühn AL, de Macedo Rodrigues K, Lozano JD, et al. Use of the Pipeline embolization device for recurrent and residual cerebral aneurysms: a safety and efficacy analysis with short-term follow-up. J Neurointerv Surg 2017;9:1208–13. 10.1136/neurintsurg-2016-012772 [DOI] [PubMed] [Google Scholar]
- 30. Benaissa A, Januel AC, Herbreteau D, et al. Endovascular treatment with flow diverters of recanalized and multitreated aneurysms initially treated by endovascular approach. J Neurointerv Surg 2015;7:44–9. 10.1136/neurintsurg-2013-011046 [DOI] [PubMed] [Google Scholar]
- 31. Gawlitza M, Januel AC, Tall P, et al. Flow diversion treatment of complex bifurcation aneurysms beyond the circle of Willis: a single-center series with special emphasis on covered cortical branches and perforating arteries. J Neurointerv Surg 2016;8:481–7. 10.1136/neurintsurg-2015-011682 [DOI] [PubMed] [Google Scholar]
- 32. Owen CM, Montemurro N, Lawton MT. Microsurgical management of residual and recurrent aneurysms after coiling and clipping: an experience with 97 patients. Neurosurgery 2015;62(Suppl 1):92–102. 10.1227/NEU.0000000000000791 [DOI] [PubMed] [Google Scholar]
- 33. Kivelev J, Tanikawa R, Noda K, et al. Open surgery for recurrent intracranial aneurysms: techniques and long-term outcomes. World Neurosurg 2016;96:1–9. 10.1016/j.wneu.2016.07.091 [DOI] [PubMed] [Google Scholar]
- 34. Crobeddu E, Lanzino G, Kallmes DF, et al. Review of 2 decades of aneurysm-recurrence literature, part 2: managing recurrence after endovascular coiling. AJNR Am J Neuroradiol 2013;34:481–5. 10.3174/ajnr.A2958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Pierot L, Boulin A, Visot A, et al. Postoperative aneurysm remnants: endovascular treatment as an alternative to further surgery. Neuroradiology 1999;41:315–9. 10.1007/s002340050755 [DOI] [PubMed] [Google Scholar]