Abstract
Objectives
Chronic diseases – including cancer, cardiovascular diseases, and metabolic conditions such as diabetes and obesity – account for over 60% of overall global mortality. Sedentary time increases the risk for chronic disease incidence and mortality, while moderate to vigorous physical activity is known to decrease risk. Most Americans spend at least half of their time sedentary, with a trend toward increasingly sedentary lifestyles, and few Americans achieve recommended levels of physical activity. Time spent outdoors has been associated with reduced sedentary time and increased physical activity among children/youth and the elderly, but few population-based studies have examined this relationship among working age adults who may face greater constraints on active, outdoor time.
Methods
This study examines the relationship between time spent outdoors, activity levels, and several chronic health conditions among a population-based sample of working age American adults in the National Health and Nutrition Examination Survey (NHANES) for 2009–2012.
Results
Findings provide evidence that time spent outdoors, on both work days and non-work days, is associated with less time spent sedentary and more time spent in moderate to vigorous physical activity. Further, findings indicate that time spent outdoors is associated with lower chronic disease risk; while these associations are partially explained by activity levels, controlling for activity levels does not fully attenuate the relationship between time outdoors and chronic disease risk.
Conclusions
While cross-sectional, study findings support the notion that increasing time spent outdoors could result in more active lifestyles and lower chronic disease risk. Future work should examine this relationship longitudinally to determine a causal direction. Additional work is also needed to identify mechanisms beyond physical activity, such as psychosocial stress, that could contribute to explaining the relationship between time spent outdoors and chronic disease risk.
INTRODUCTION
Chronic, non-communicable diseases account for over 60% of overall global mortality.1 In 2012, cardiovascular diseases, cancers, and diabetes accounted for 27.2 million deaths – nearly 50% of the 56 million deaths around the world.1 Ischemic heart disease is consistently ranked as the leading cause of death, with diabetes and several types of cancer among other top causes.2 Further, obesity rates, linked to risk of other chronic diseases, have nearly doubled since 1980.1 Among the top preventable causes of cardiovascular diseases, some cancers, and metabolic illnesses such as diabetes and obesity, is physical inactivity.
Sedentary time – time spent sitting or reclining – has been linked with increased risk of cancer incidence and mortality, type 2 diabetes incidence, cardiovascular disease mortality and all-cause mortality, even when controlling for levels of physical activity.3–6 Further, an analysis of National Health and Nutrition Examination Survey (NHANES) data revealed that Americans ages 12 years or older spend at least half of their time sedentary, with 6–11 year olds spending approximately 40% of their time sedentary.7 Additional estimates indicate that time spent sedentary is increasing among Americans, as well as globally,8 highlighting the need for approaches to reduce sedentary time and increase levels of physical activity.
Conversely, time spent in deliberate physical activity is known to have numerous health benefits, including reduced cancer and chronic disease risk and improvements in blood pressure, bone strength, aerobic fitness, strength and endurance, depression, and anxiety.9,10 Further, recent literature demonstrates that physical activity undertaken outdoors and/or in natural environments (sometimes termed “green exercise”) may have additional benefits, including improved mood, self-esteem, mental health, feelings of revitalization, feelings of energy, and social cohesion, and decreased blood pressure, stress, mental fatigue, tension, confusion, anger, and depression.11–16
Despite these known benefits, physical activity levels are low and new approaches to increasing activity levels are needed. Less than 50% of U.S. adults 18 years of age and over meet the physical activity guideline for aerobic activity and only 21% meet guidelines for both aerobic and resistance exercise.17 Although individual intervention efforts report positive results, participation is often based on self-selection and is more likely among some population groups than others, limiting generalizability and impact.18 Moreover, among those participating in physical activity interventions, results may be modest, and long-term maintenance of behavior change is often limited.19,20 Community wide campaigns have a wider reach and often target multiple levels of influence and a variety of relevant messages (e.g., use stairs; walk to school). Recent reviews suggest about a 4% increase in the percentage of people engaging in regular physical activity following such campaigns.21 Clearly, additional strategies are needed to help Americans move more.
One possible contributor to physical activity levels is the amount of time one spends outdoors. A number of studies in children and youth have linked time outdoors with higher moderate to vigorous physical activity (MVPA) levels, less time spent sedentary, and better cardiorespiratory fitness.22,23 One study indicated that while only 13% of youths’ time was spent outdoors, 30% of activity volume and 35% of MVPA was accumulated outside.24 These relationships indicate that time spent outdoors could be a valuable target for increasing activity levels and decreasing sedentary time among youth.
Some work has also addressed the relationship between outdoor time and health among older adults, 25–34 although this work has largely been undertaken in small samples of older adults. Kerr et al. found, in a study of 754 older adults, that individuals who undertook physical activity outdoors were more active than those who were active indoors, and that physical activity levels (but not activity location) were associated with self-rated health.34 Petersen et al. found that time out of home (a concept similar to time outdoors) was associated with improved cognitive function, physical ability, and emotional state among elders (n=85).28 Recently, Harada et al. demonstrated an association between outdoor time and steps per day among a sample (n=192) of older adults; they found that outdoor time was also associated with depression, but not with cardiorespiratory fitness, lower-extremity strength, or well-being, although steps per day was associated with these outcomes.27 In related work, Kono et al. have found that a higher frequency of going outdoors is associated with improved functional capacity, intellectual activity, and self-efficacy among older adults,29 as well as resulting in a reduced likelihood that an older adult’s activities of daily living (ADL) score decreases over time.30
However, few studies – particularly large, population-based studies – have examined the relationship between time spent outdoors, activity levels, and chronic conditions among adults, despite great interest in the (outdoor) built environment and its relationship to physical activity among adults.35 To address this gap, this study examines the relationships between time spent outdoors, activity levels, and several chronic conditions in a large, population-based sample of working age American adults. We specify two primary research questions: (1) Is time spent outdoors associated with activity levels (sedentary time, MVPA time) among a national sample of working age US adults? (2) Is time spent outdoors associated with chronic disease risk in the same population, and if so, is the association explained by activity levels?
METHODS
Data Source
This analysis included data from the National Health and Nutrition Examination Survey (NHANES) continuous surveys for 2009–2012 – a nationally representative, cross-sectional survey of the noninstitutionalized US population. Analysis was limited to individuals between the ages of 20 and 59, as they were eligible for the dermatology questionnaire, which queried time spent outdoors. The total number of individuals between the ages of 20 and 59 was 7,914. Sample sizes were reduced for each outcome examined based on data availability.
Measures
Predictors
Time spent outdoors during a typical work day and non-work day were measured with two questions: “The next questions ask about the time you spent outdoors during the past 30 days. By outdoors, I mean outside and not under any shade. How much time did you usually spend outdoors between 9 in the morning and 5 in the afternoon on the days that you worked or went to school?” and “During the past 30 days, how much time did you usually spend outdoors between 9 in the morning and 5 in the afternoon on the days when you were not working or going to school?” Time spent outdoors was grouped into time intervals: 30 minutes or less, 30 minutes to 1 hour, 1–2 hours, 2–3 hours, 3–4 hours, 4 – 5 hours, 5 – 6 hours, and 6 –8 hours.
Outcomes
Time spent sedentary was measured with a single question: “The following question is about sitting at work, at home, getting to and from places, or with friends, including time spent sitting at a desk, traveling in a car or bus, reading, playing cards, watching television, or using a computer. Do not include time spent sleeping. How much time do you usually spend sitting on a typical day?” Sedentary time was measured in minutes. It should be noted that this measure of sedentary time focused on time spent sitting, but did not specifically include time spent reclining.
Time spent in MVPA was measured using a combination of several questions. Respondents were asked whether they engaged in any vigorous intensity sports, fitness or recreational activities. If they answered yes, they were asked on how many days during a typical week they undertake vigorous exercise. They were then asked how many minutes they spend in vigorous activity on a typical day. To calculate the average daily minutes of vigorous PA, the number of days containing vigorous PA was multiplied by the average minutes of vigorous PA on a typical day to estimate weekly PA, and that number was divided by seven. A similar calculation was undertaken for moderate intensity activity. Average daily vigorous PA and average daily moderate PA were summed to result in a combined total estimate of minutes of MVPA per day per respondent. Respondents who answered that they engaged in no moderate or vigorous physical activity were assigned a value of zero MVPA minutes.
Chronic conditions examined included diabetes, cancer, body mass index (BMI) (as an indicator of overweight and obesity), and allostatic load. Cancer (ever diagnosed) and diabetes (taking insulin or diabetic pills) were assessed via self-report. BMI was derived from direct measurements of the subject’s height and weight. Allostatic load was defined, following previous work,36 as a continuous score based on a set of individual measures obtained through direct measurement and laboratory analysis: systolic blood pressure >= 140mm/hg, diastolic blood pressure >= 90 mm/hg, pulse > 90 beats per minute, total cholesterol >= 240 mg/dcl, HDL cholesterol < 50 mg/dL, BMI > 30 kg2/m, glycosylated hemoglobin >= 6.4%, and albumin < 4 g/dL. C-reactive protein could not be included as it was not available for the 2011–12 NHANES cohort. For each criterion met, a point was tallied. A point was added also for those taking prescription drugs for hypertension, high cholesterol, or high blood sugar/diabetes – as measured by self-report.
Statistical Analyses
Multivariable survey regression models were used to examine relationships between time spent outdoors and each outcome, controlling for a number of covariates: age group (20–39, 40–49, 50–59), sex (Male, Female), race and ethnicity (Non-Hispanic White, Mexican, Other Hispanic, Non-Hispanic Black, and Other Race – including Multiracial), income (poverty to income ratio as a continuous variable, calculated by dividing family income by the Department of Health and Human Services poverty guidelines specific to family size, year, and state), education (less than high school graduate, high school graduate or equivalent, some college or Associates degree, and college degree or more), marital status (Married, Divorced/Separated/Widowed, Never married, Living with partner) and employment status (Working at a job or business/With a job or business but not at work, Looking for work/Not working at a job or business). Further, relationships between time spent outdoors and chronic conditions were measured first without, and then with controlling for sedentary and MVPA time. Margins of covariate-adjusted regression coefficient estimates were calculated for relationships between time outdoors and sedentary and MVPA minutes, and the coefplot package in STATA was used to create graphical displays. All p-values associated with time outdoors as a categorical variable were adjusted for multiple (seven) comparisons using the conservative Bonferroni adjustment method. Finally, the overall trend was examined for each relationship tested by including the time outdoors predictor variables as continuous variables, using the midpoints of time outdoors categories, in hours (0.25, 0.75, 1.5, 2.67, 3.5, 4.5, 5.5 and 7). Analyses were undertaken using Stata/SE 14.2.
RESULTS
Sample characteristics are summarized in Table 1. Approximately half of the sample was between the ages of 20 and 39, with adults 40–49 and 50–59 making up approximately 25% of the sample each. Slightly over half of the sample was female, and fully 52% were married. The vast majority of participants were non-Hispanic White (63%), with smaller percentages of Mexican (10%), Other Hispanic (7%), Non-Hispanic Black (12%) and other racial and ethnic groups, including those who self-identified as multiracial (8%). Over 60% of the sample had at least some college education, and 72% were working. Fully 44% of the sample indicated that they spent 30 minutes or less outdoors on work days, while 20% reported spending less than 30 minutes outdoors on non-work days. With regard to chronic disease risk, 5% of the sample indicated they had ever been diagnosed with cancer or diabetes. The mean BMI was 28.7 (overweight) and the mean allostatic load score was 1.8. On a daily basis, individuals reported spending 6 hours sedentary and 25 minutes in MVPA.
Table 1.
Sample Characteristics
| Proportion/Mean [CI] | |
|---|---|
| Age category | |
| Age 20–39 | 0.49 [0.46, 0.52] |
| Age 40–49 | 0.26 [0.24, 0.28] |
| Age 50–59 | 0.25 [0.23, 0.27] |
| Sex | |
| Male | 0.49 [0.48, 0.51] |
| Female | 0.51 [0.49, 0.52] |
| Marital Status | |
| Married | 0.52 [0.49, 0.54] |
| Divorced/Separated/Widowed | 0.14 [0.13, 0.15] |
| Never married | 0.24 [0.21, 0.27] |
| Living with Partner | 0.10 [0.09, 0.11] |
| Race and Ethnicity | |
| Non-Hispanic White | 0.63 [0.58, 0.69] |
| Mexican American | 0.10 [0.07, 0.13] |
| Other Hispanic | 0.07 [0.05, 0.09] |
| Non-Hispanic Black | 0.12 [0.10, 0.15] |
| Other Race (Including Multiracial) | 0.08 [0.07, 0.10] |
| Education Level | |
| Less than High School Graduate | 0.17 [0.15, 0.19] |
| High school graduate/Equivalent | 0.21 [0.19, 0.23] |
| Some college or AA degree | 0.32 [0.30, 0.34] |
| College graduate or Above | 0.30 [0.27, 0.33] |
| Employment Status | |
| Working at a Job or Business/With a Job or Business, but Not at Work | 0.72 [0.70, 0.74] |
| Ratio of family income to poverty | 2.93 [2.80, 3.05] |
| Time Spent Outdoors (work days) | |
| 30 minutes or less | 0.44 [0.42, 0.46] |
| 30 minutes to 1 hour | 0.15 [0.14, 0.17] |
| 1–2 hours | 0.09 [0.08, 0.11] |
| 2–3 hours | 0.04 [0.04, 0.05] |
| 3–4 hours | 0.04 [0.04, 0.05] |
| 4–5 hours | 0.03 [0.03, 0.04] |
| 5–6 hours | 0.02 [0.02, 0.03] |
| 6–8 hours | 0.06 [0.05, 0.07] |
| Does not work or go to school | 0.11 [0.10, 0.12] |
| Time Spent Outdoors (non-work days) | |
| 30 minutes or less | 0.20 [0.18, 0.22] |
| 30 minutes to 1 hour | 0.17 [0.15, 0.18] |
| 1–2 hours | 0.21 [0.20, 0.23] |
| 2–3 hours | 0.12 [0.11, 0.13] |
| 3–4 hours | 0.12 [0.11, 0.13] |
| 4–5 hours | 0.07 [0.06, 0.09] |
| 5–6 hours | 0.05 [0.04, 0.06] |
| 6–8 hours | 0.05 [0.04, 0.06] |
| At work or school seven days a week | 0.01 [0.00, 0.01] |
| Cancer | |
| Yes | 0.05 [0.04, 0.06] |
| No | 0.95 [0.94, 0.95] |
| Diabetes | |
| Yes | 0.05 [0.04, 0.05] |
| No | 0.95 [0.95, 0.96] |
| BMI | 28.7 [28.4, 29.0] |
| Allostatic Load (score) | 1.80 [1.75, 1.85] |
| Sedentary minutes (daily) | 363.5 [353.0, 373.9] |
| MVPA minutes (daily) | 24.6 [22.5, 26.8] |
Our first research question was whether time spent outdoors is associated with activity levels. Model results (Figure 1, Table 2) indicate a significant relationship between time spent outdoors and time spent sedentary, with increasing intervals of time spent outdoors associated with fewer sedentary minutes during work days and non-work days, as compared to a reference group spending 30 minutes or less outdoors. A similar relationship was found for time spent outdoors and time spent in MVPA, with increasing time outdoors associated with more time in MVPA. Time spent outdoors on non-work days exhibited a stronger relationship with time in MVPA than outdoor time on work days. Trend analyses, reporting the parameter estimates from the adjusted models, indicated statistically significant relationships for non-work day time outdoors for both sedentary minutes (−9.7 minutes per hour of time outdoors, p<0.001) and MVPA minutes (1.98, p<0.001). For work day time, a trend was identified with sedentary minutes (−15.0, p<0.001), and a weaker trend was identified for MVPA minutes (0.99, p<0.05).
Figure 1.
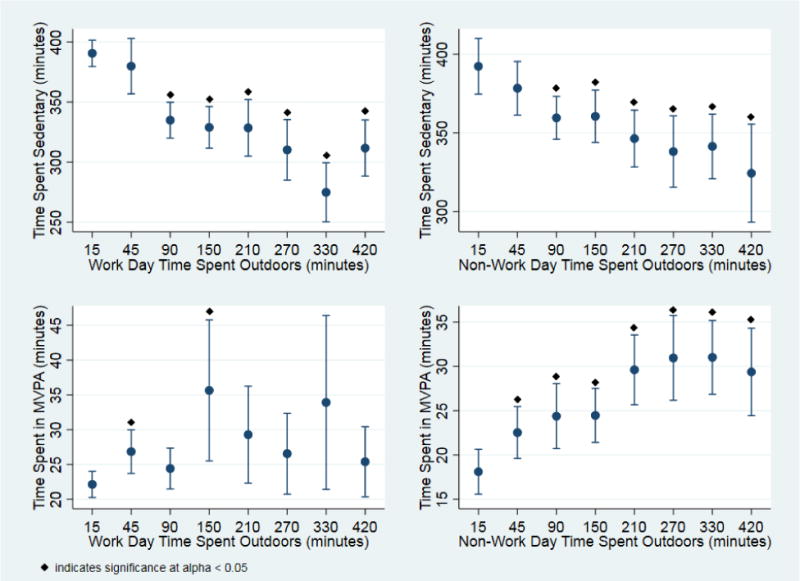
Time spent outdoors in relation to time spent sedentary and in MVPA
Table 2.
Time spent outdoors in relation to time spent sedentary and in MVPA
| Work Days n=6042 | Non-Work Days n=6958 | |
|---|---|---|
| Time Spent outdoors | Coefficient for sedentary minutes | Coefficient for sedentary minutes |
| 45 | −10.67 | −13.98 |
| 90 | −55.68** | −32.75** |
| 150 | −61.65** | −31.80** |
| 210 | −62.05** | −45.95** |
| 270 | −80.32** | −54.18** |
| 330 | −115.71** | −50.91** |
| 420 | −78.87** | −67.95** |
| Trend test | −15.03** | −9.65** |
| Time Spent outdoors | Coefficient for MVPA minutes | Coefficient for MVPA minutes |
| 45 | 4.71** | 4.43** |
| 90 | 2.28 | 6.28** |
| 150 | 13.51** | 6.36** |
| 210 | 7.15 | 11.50** |
| 270 | 4.41 | 12.85** |
| 330 | 11.78 | 12.92** |
| 420 | 3.25 | 11.27** |
| Trend test | 0.99* | 1.98** |
p<0.01
p<0.05
Additionally, we sought to determine whether time spent outdoors was associated with the risk of several chronic conditions – obesity (BMI), allostatic load, cancer, and diabetes – and whether any observed association could be explained by activity levels. As shown in Tables 3 and 4, associations between time spent outdoors and chronic conditions were identified for both work days and non-work days, though the magnitude of the associations was small. Non-work day time outdoors (Table 3) was associated with allostatic load, diabetes, and body mass index, but not cancer, in trend analyses. Work day time outdoors (Table 4) was associated with BMI, allostatic load and cancer in trend analyses, and diabetes only for one category. Significant associations were attenuated to a similar degree when controlling for sedentary and MVPA time for both work day and non-work day analyses, although the attenuation crossed the threshold of statistical significance for work days only.
Table 3.
Non-work day time spent outdoors in relation to chronic health conditions
| Body Mass Index (BMI) (n=6922, linear regression coefficient) | Allostatic Load Score (n=6955, linear regression coefficient) | Diabetes diagnosis (n=6974, odds ratio) | Cancer diagnosis (n=6954, odds ratio) | |||||
|---|---|---|---|---|---|---|---|---|
| Time Spent Outdoors on Non-Work Days | No control for activity level. | Controlled for sedentary and MVPA time | No control for activity level. | Controlled for sedentary and MVPA time | No control for activity level. | Controlled for sedentary and MVPA time | No control for activity level. | Controlled for sedentary and MVPA time |
| 30 minutes or less | Referent | Referent | Referent | Referent | Referent | Referent | Referent | Referent |
| 30 minutes to 1 hour | −0.32 | −0.23 | −0.08 | −0.07 | 0.84 | 0.88 | 0.72 | 0.75 |
| 2–3 hours | −0.74* | −0.57 | −0.14* | −0.11 | 0.35** | 0.38** | 0.83 | 0.88 |
| 3–4 hours | −0.66 | −0.39 | −0.16 | −0.11 | 0.58 | 0.65 | 0.45* | 0.49** |
| 4–5 hours | −1.43** | −1.12* | −0.28* | −0.22 | 0.46* | 0.53 | 0.91 | 0.98 |
| 5–6 hours | −0.69 | −0.41 | −0.12 | −0.06 | 0.39* | 0.41 | 0.88 | 0.94 |
| 6–8 hours | −1.61** | −1.29** | −0.35** | −0.29** | 0.58 | 0.66 | 0.38* | 0.41* |
| Overall trend per hour | −0.20** | −0.15** | −0.04** | −0.03** | 0.87* | 0.89* | 0.93 | 0.94 |
p<0.01
p<0.05
Table 4.
Work day time spent outdoors in relation to chronic health conditions
| Body Mass Index (BMI) (n=6018, linear regression coefficient) | Allostatic Load Score (n=5432, linear regression coefficient) | Diabetes diagnosis (n=6056, odds ratio) | Cancer diagnosis (n=6054, odds ratio) | |||||
|---|---|---|---|---|---|---|---|---|
| Time Spent Outdoors on Work Days | No control for activity level. | Controlled for sedentary and MVPA time | No control for activity level. | Controlled for sedentary and MVPA time | No control for activity level. | Controlled for sedentary and MVPA time | No control for activity level. | Controlled for sedentary and MVPA time |
| 30 minutes or less | Referent | Referent | Referent | Referent | Referent | Referent | Referent | Referent |
| 30 minutes to 1 hour | −0.35 | −0.26 | −0.08 | −0.06 | 0.81 | 0.84 | 0.86 | 0.87 |
| 1–2 hours | −0.48 | −0.22 | −0.01 | 0.03 | 1.51 | 1.64* | 1.05 | 1.11 |
| 2–3 hours | −0.91 | −0.56 | −0.10 | −0.04 | 0.58 | 0.68 | 0.88 | 0.96 |
| 3–4 hours | −0.92 | −0.60 | −0.04 | 0.02 | 1.23 | 1.37 | 0.37 | 0.40 |
| 4–5 hours | −0.43 | −0.09 | −0.07 | −0.01 | 0.31** | 0.35* | 1.15 | 1.25 |
| 5–6 hours | −0.77 | −0.22 | −0.27* | −0.16 | 0.53 | 0.66 | 0.06** | 0.07* |
| 6–8 hours | −1.03* | −0.77 | −0.26* | −0.21 | 0.82 | 0.92 | 0.41 | 0.43 |
| Overall trend per hour | −0.15** | −0.09 | −0.03* | −0.02 | 0.95 | 0.97 | 0.88* | 0.90 |
p<0.01
p<0.05
DISCUSSION
Time spent outdoors is known to be associated with physical activity among youth and older adults. The current study extends these findings using a large, population-based survey sample of working age U.S. adults. Based on NHANES data for adults ages 20–59, time spent outdoors on non-work days and work days was associated with less time spent in sedentary activities and more time engaged in MVPA. Trend tests indicated that an additional hour of time outdoors on non-work days was associated with a nine minute reduction in sedentary time and a two minute increase in MVPA time; for work days, an additional hour of outdoor time was associated with a sixteen minute reduction in sedentary time and a one minute increase in MVPA. Non-work day outdoor time was also related to BMI, allostatic load, and diabetes, even after controlling for activity levels. Work day time showed weaker associations, which were fully attenuated when controlling for activity levels.
Given low activity levels and modest impacts of current efforts to increase physical activity among American adults, establishing an association between time outdoors and activity levels has important implications for public health. If time spent outdoors is closely linked to activity levels among adults, and even directly to chronic disease risk, time spent outdoors may be a new target for interventions that seek to encourage adults to move more and/or reduce their risk for chronic diseases. In fact, some physicians have begun to prescribe time outdoors, particularly in nature, based on belief of a health benefit.37
Time outdoors as a “new target” could be advantageous for several reasons. First, an emphasis on time spent outdoors, as opposed to exercise, may address or circumnavigate barriers to the uptake and maintenance of active lifestyles. Messages that promote time outdoors may be more motivating or less intimidating to individuals who are not responsive to messages advocating exercise. Thus, prompting adults to spend more time outdoors may be an important first step in the effort to encourage more active lifestyles. Further, outdoor environments could provide opportunities for activities that feel enjoyable to individuals and don’t connote “exercise,” despite encouraging movement.38 Outdoor environments may also be more interesting or motivating for some individuals. Studies that individuals who participate in outdoor physical activity report greater feelings of positive engagement, revitalization, energy, mental well-being, enjoyment and satisfaction than those engaged in physical activity indoors, and declare a greater intent to repeat the activity later.15 These benefits may also address commonly reported barriers to physical activity among certain population groups. For example, psychoneurological symptoms, lack of motivation, and low energy are among the key barriers to physical activity reported by breast cancer survivors,39 and these barriers are known to be positively impacted by time spent outdoors, exposure to natural environments, and outdoor physical activity.
Further, evidence indicates that outdoor physical activity may have increased benefits over physical activity alone,11–16 and thus, targeting outdoor physical activity specifically may result in greater impact on chronic disease outcomes or result in other added benefits. Time spent outdoors and exposure to natural environments have been linked to reduced fatigue,40 and sleep disruptions,41 and improvements in mental health42,43 and cognitive function,44 as well as related biomarkers, including inflammatory markers.45 Our finding that the association between time outdoors on non-work days and chronic disease outcomes was not erased when controlling for activity levels could suggest additional mechanisms linking outdoor time to chronic disease risk. In particular, psychosocial stress could be an important additional pathway. Stress is known to be associated with obesity46–50 and diabetes,51–55 and allostatic load is conceived as a measure of cumulative stress over time.36,56,57 Thus, it is possible that stress, in addition to physical activity, mediates the relationship between time spent outdoors and chronic disease.
The stronger association for non-work day time (as compared to work day time) with MVPA indicates that non-work day leisure time was likely a significant source of MVPA among this population. Given that time outdoors during work days would have been between 9am and 5pm, which is a common day shift, it is likely that time outdoors on work days indicates for many people an outdoor occupation. Further, while the association between work day outdoor time and MVPA was weaker, the association between work day outdoor time and sedentary time was quite strong. These findings indicate that uses of outdoor time differ on work days and non-work days, and also highlight the importance of measurement. Because outdoor time before 9am and after 5pm was not included in the self-reported estimate of time spent outdoors, it is possible that work day time outdoors associated with MVPA was not captured because it took place outside of the 9–5 interval.
This study is subject to several limitations. First, questions measuring time outdoors were intended to measure sun exposure, and did not include early morning, evening or night time hours, or time spent in the shade. However, for the purposes of examining associations with physical activity, it would be ideal to consider time spent outdoors but in the shade (e.g., walking in a forest) and early morning and evening hours, which may be prime hours for physical activity among working age adults. Thus, results should be interpreted with these limitations in mind, as the measure constitutes a sample, but not a census, of time spent outdoors. Further, measures of sedentary time and MVPA did not distinguish between work days and non-work days, making it impossible to directly compare non-work day outdoor time with non-work day physical activity, for example. In addition, while the measure used to evaluate MVPA focused on recreational activity, other types of MVPA, including occupational activity, may also be relevant and are only captured in this study by the sedentary time variable, which measures time spent sitting and would exclude time spent active that was not recreational. The database also lacked information about the environments or seasons in which individuals spent time outdoors or engaged in different levels of activity. Finally, this cross-sectional study cannot infer causality, and there exists the possibility that reverse causation or a common third factor may have influenced study findings. It is likely that individuals with more active lifestyles will spend more time outdoors as a result of their planned physical activity. Future work should make use of longitudinal designs and incorporate qualitative methodologies to determine the direction of causality and motivations for spending time outdoors.
Results indicate that more time spent outdoors by adults was associated with progressively more activity. Results also indicate that more time spent outdoors may be associated with less chronic disease risk, including diagnosis of diabetes, allostatic load and body mass index. These findings are supported by other studies that have identified similar relationships among children and youth22–24 and older adults.25–34 The findings of this study support efforts to investigate time spent outdoors as a potential contributor to reducing sedentary time, increasing engagement in health enhancing physical activity, and, ultimately, reducing chronic disease risk among adults. Future work should consider the environments in which outdoor time is spent and the purpose of time spent outdoors (e.g. leisure versus occupational time). Future investigations would likely benefit from the use of more specific measurement approaches, including objectively measured physical activity via accelerometer, and objectively measured time spent outdoors, which has been most recently achieved through a combination of global positioning system (GPS), accelerometer and ambient light sensing technology.58 Longitudinal and experimental studies are needed to determine the direction of the association between time outdoors, activity levels, and chronic disease risk. Finally, it will be important to evaluate and consider the ways in which time spent outdoors could be encouraged through policy and programming, and how constraints such as safety or weather could be factored into such recommendations.
PUBLIC HEALTH IMPLICATIONS
Encouraging time spent outdoors may be an important strategy to reduce sedentary time, increase time spent in moderate to vigorous physical activity, and decrease risk for several chronic health conditions. Further study of how and why being outdoors may benefit health is needed.
Acknowledgments
The analyses were exempted by the Institutional Review Board at the Medical College of Wisconsin due to the use of public access data. This work is supported in part by the Advancing a Healthier Wisconsin Endowment and in part by the Clinical & Translational Science Institute of Southeast Wisconsin: NIH UL1RR031973.
Funding: This study was funded in part by the Advancing a Healthier Wisconsin Endowment and in part by the Clinical & Translational Science Institute of Southeast Wisconsin: NIH UL1RR031973.
Footnotes
Compliance with Ethical Standards
Conflict of Interest: Dr. Kirsten M. M. Beyer declares that she has no conflict of interest. Dr. Aniko Szabo declares that she has no conflict of interest. Ms. Kelly Hoormann declares that she has no conflict of interest. Dr. Melinda Stolley declares that she has no conflict of interest.
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The analyses were exempted by the Institutional Review Board at the Medical College of Wisconsin due to the use of public access data.
This article does not contain any studies with animals performed by any of the authors.
References
- 1.WHO. World Health. Vol. 176. 2014. Global status report on noncommunicable diseases 2014. [Google Scholar]
- 2.Wang H, Naghavi M, Allen C, et al. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1459–1544. doi: 10.1016/S0140-6736(16)31012-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Biswas A, Oh PI, Faulkner GE, et al. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: a systematic review and meta-analysis. Ann Intern Med. 2015;162(2):123–132. doi: 10.7326/M14-1651. [DOI] [PubMed] [Google Scholar]
- 4.Thorp AA, Owen N, Neuhaus M, Dunstan DW. Sedentary behaviors and subsequent health outcomes in adults: a systematic review of longitudinal studies, 1996–2011. Am J Prev Med. 2011;41(2):207–215. doi: 10.1016/j.amepre.2011.05.004. [DOI] [PubMed] [Google Scholar]
- 5.Schmid D, Leitzmann MF. Television viewing and time spent sedentary in relation to cancer risk: a meta-analysis. J Natl Cancer Inst. 2014;106(7) doi: 10.1093/jnci/dju098. Print 2014 Jul doi:10.1093/jnci/dju098 [doi] [DOI] [PubMed] [Google Scholar]
- 6.Wilmot EG, Edwardson CL, Achana FA, et al. Sedentary time in adults and the association with diabetes, cardiovascular disease and death: systematic review and meta-analysis. Diabetologia. 2012;55:2895–2905. doi: 10.1007/s00125-012-2677-z. [DOI] [PubMed] [Google Scholar]
- 7.Matthews CE, Chen KY, Freedson PS, et al. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am J Epidemiol. 2008;167(7):875–881. doi: 10.1093/aje/kwm390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ng SW, Popkin BM. Time use and physical activity: a shift away from movement across the globe. Obes Rev. 2012;13(8):659–680. doi: 10.1111/j.1467-789X.2011.00982.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Janssen I, LeBlanc AG. Review Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int J Behav Nutr Phys Act. 2010;7(40):1–16. doi: 10.1186/1479-5868-7-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moore SC, Lee I-M, Weiderpass E, et al. Association of leisure-time physical activity with risk of 26 types of cancer in 1.44 million adults. JAMA Intern Med. 2016;176(6):816–825. doi: 10.1001/jamainternmed.2016.1548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Barton J, Pretty J. What is the best dose of nature and green exercise for improving mental health? A multi-study analysis. Environ Sci Technol. 2010;44(10):3947–3955. doi: 10.1021/es903183r. [DOI] [PubMed] [Google Scholar]
- 12.Pretty J, Peacock J, Sellens M, Griffin M. The mental and physical health outcomes of green exercise. Int J Environ Health Res. 2005;15(5):319–337. doi: 10.1080/09603120500155963. [DOI] [PubMed] [Google Scholar]
- 13.Hug S-M, Hartig T, Hansmann R, Seeland K, Hornung R. Restorative qualities of indoor and outdoor exercise settings as predictors of exercise frequency. Health Place. 2009;15(4):971–980. doi: 10.1016/j.healthplace.2009.03.002. [DOI] [PubMed] [Google Scholar]
- 14.Mitchell R. Is physical activity in natural environments better for mental health than physical activity in other environments? Soc Sci Med. 2013;91:130–134. doi: 10.1016/j.socscimed.2012.04.012. [DOI] [PubMed] [Google Scholar]
- 15.Thompson Coon J, Boddy K, Stein K, Whear R, Barton J, Depledge MH. Does participating in physical activity in outdoor natural environments have a greater effect on physical and mental wellbeing than physical activity indoors? A systematic review. Environ Sci Technol. 2011;45(5):1761–1772. doi: 10.1021/es102947t. [DOI] [PubMed] [Google Scholar]
- 16.Hansmann R, Hug S-M, Seeland K. Restoration and stress relief through physical activities in forests and parks. Urban For Urban Green. 2007;6(4):213–225. [Google Scholar]
- 17.Ward BW, Clarke TC, Nugent CN, Schiller JS. Early release of selected estimates based on data from the 2015 National Health Interview Survey. Natl Cent Heal Stat. 2016 [Google Scholar]
- 18.Waters LA, Galichet B, Owen N, Eakin E. Who participates in physical activity intervention trials. J Phys Act Heal. 2011;8(1):85–103. doi: 10.1123/jpah.8.1.85. [DOI] [PubMed] [Google Scholar]
- 19.Tak EC, van Uffelen JG, Paw MJ, van Mechelen W, Hopman-Rock M. Adherence to exercise programs and determinants of maintenance in older adults with mild cognitive impairment. J Aging Phys Act. 2012;20(1):32–46. doi: 10.1123/japa.20.1.32. [DOI] [PubMed] [Google Scholar]
- 20.Findorff MJ, Wyman JF, Gross CR. Predictors of long-term exercise adherence in a community-based sample of older women. J Women’s Heal. 2009;18(11):1769–1776. doi: 10.1089/jwh.2008.1265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Prevention C for DC and. Strategies to prevent obesity and other chronic diseases: The CDC guide to strategies to increase physical activity in the community. Atlanta, GA US Dep Heal Hum Serv. 2011 [Google Scholar]
- 22.Gray C, Gibbons R, Larouche R, et al. What is the relationship between outdoor time and physical activity, sedentary behaviour, and physical fitness in children? A systematic review. Int J Environ Res Public Health. 2015;12(6):6455–6474. doi: 10.3390/ijerph120606455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schaefer L, Plotnikoff RC, Majumdar SR, et al. Outdoor time is associated with physical activity, sedentary time, and cardiorespiratory fitness in youth. J Pediatr. 2014;165(3):516–521. doi: 10.1016/j.jpeds.2014.05.029. [DOI] [PubMed] [Google Scholar]
- 24.Wheeler BW, Cooper AR, Page AS, Jago R. Greenspace and children’s physical activity: A GPS/GIS analysis of the PEACH project. Prev Med (Baltim) 2010;51:148–152. doi: 10.1016/j.ypmed.2010.06.001. [DOI] [PubMed] [Google Scholar]
- 25.Sugiyama T, Thompson CW. Outdoor environments, activity and the well-being of older people: Conceptualising environmental support. Environ Plan A. 2007;39(8):1943–1960. doi: 10.1068/a38226. [DOI] [Google Scholar]
- 26.Kerr J, Marshall S, Godbole S, et al. The relationship between outdoor activity and health in older adults using GPS. Int J Environ Res Public Health. 2012;9(12):4615–4625. doi: 10.3390/ijerph9124615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Harada K, Lee S, Lee S, et al. Objectively-measured outdoor time and physical and psychological function among older adults. Geriatr Gerontol Int. 2016 doi: 10.1111/ggi.12895. [DOI] [PubMed] [Google Scholar]
- 28.Petersen J, Austin D, Mattek N, Kaye J. Time out-of-home and cognitive, physical, and emotional wellbeing of older adults: A longitudinal mixed effects model. PLoS One. 2015;10(10) doi: 10.1371/journal.pone.0139643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kono A, Kai I, Sakato C, Rubenstein LZ. Frequency of going outdoors: a predictor of functional and psychosocial change among ambulatory frail elders living at home. J Gerontol A Biol Sci Med Sci. 2004;59(3):275–280. doi: 10.1093/GERONA/59.3.M275. [DOI] [PubMed] [Google Scholar]
- 30.Kono A, Kai I, Sakato C, Rubenstein LZ. Frequency of going outdoors predicts long-range functional change among ambulatory frail elders living at home. Arch Gerontol Geriatr. 2007;45(3):233–242. doi: 10.1016/j.archger.2006.10.013. [DOI] [PubMed] [Google Scholar]
- 31.Jacobs JM, Cohen A, Hammerman-Rozenberg R, Azoulay D, Maaravi Y, Stessman J. Going outdoors daily predicts long-term functional and health benefits among ambulatory older people. J Aging Health. 2008;20:259–272. doi: 10.1177/0898264308315427. [DOI] [PubMed] [Google Scholar]
- 32.Tsai L-T, Portegijs E, Rantakokko M, et al. The association between objectively measured physical activity and life-space mobility among older people. Scand J Med Sci Sports. 2015;25(4):e368–73. doi: 10.1111/sms.12337. [DOI] [PubMed] [Google Scholar]
- 33.Tsai L-T, Rantakokko M, Rantanen T, Viljanen A, Kauppinen M, Portegijs E. Objectively Measured Physical Activity and Changes in Life-Space Mobility Among Older People. J Gerontol A Biol Sci Med Sci. 2016;0(0):1–6. doi: 10.1093/gerona/glw042. [DOI] [PubMed] [Google Scholar]
- 34.Kerr J, Sallis JF, Saelens BE, et al. Outdoor physical activity and self rated health in older adults living in two regions of the US. Int J Behav Nutr Phys Act. 2012;9(1):89. doi: 10.1186/1479-5868-9-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.McCormack GR, Shiell A. In search of causality: a systematic review of the relationship between the built environment and physical activity among adults. Int J Behav Nutr Phys Act. 2011;8(1):1. doi: 10.1186/1479-5868-8-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Geronimus AT, Hicken M, Keene D, Bound J. “Weathering” and age patterns of allostatic load scores among blacks and whites in the United States. J Inf. 2006;96(5) doi: 10.2105/AJPH.2004.060749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Elizabeth Nisbet ML. Prescribing a Dose of Nature: Modern medicine is rediscovering the simple healing power of being outdoors. Altern J Canada’s Environ Voice. 2015 http://www.alternativesjournal.ca/sustainable-livi. http://www.alternativesjournal.ca/sustainable-living/prescribing-dose-nature.
- 38.Taverno Ross SE, Francis LA. Physical activity perceptions, context, barriers, and facilitators from a Hispanic child’s perspective. Int J Qual Stud Heal Well-being. 2016;11(31949) doi: 10.3402/qhw.v11.31949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Blaney JM, Lowe-Strong A, Rankin-Watt J, Campbell A, Gracey JH. Cancer survivors’ exercise barriers, facilitators and preferences in the context of fatigue, quality of life and physical activity participation: a questionnaire–survey. Psycho- Oncology. 2013;22(1):186–194. doi: 10.1002/pon.2072. [DOI] [PubMed] [Google Scholar]
- 40.Ryan RM, Weinstein N, Bernstein J, Brown KW, Mistretta L, Gagne M. Vitalizing effects of being outdoors and in nature. J Environ Psychol. 2010;30(2):159–168. [Google Scholar]
- 41.Astell-Burt T, Feng X, Kolt GS. Does access to neighbourhood green space promote a healthy duration of sleep? Novel findings from a cross-sectional study of 259 319 Australians. BMJ Open. 2013;3(8) doi: 10.1136/bmjopen-2013-003094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Alcock I, White MP, Wheeler BW, Fleming LE, Depledge MH. Longitudinal Effects on Mental Health of Moving to Greener and Less Green Urban Areas. Environ Sci Technol. 2014;48(2):1247–1255. doi: 10.1021/es403688w. [DOI] [PubMed] [Google Scholar]
- 43.Beyer KMM, Kaltenbach A, Szabo A, Bogar S, Nieto FJ, Malecki KM. Exposure to neighborhood green space and mental health: evidence from the survey of the health of Wisconsin. Int J Environ Res Public Health. 2014;11(3):3453–3472. doi: 10.3390/ijerph110303453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Faber Taylor A, Kuo FE. Children With Attention Deficits Concentrate Better After Walk in the Park. J Atten Disord. 2009;12(5):402–409. doi: 10.1177/1087054708323000. [DOI] [PubMed] [Google Scholar]
- 45.Song C, Ikei H, Miyazaki Y. Physiological effects of nature therapy: A review of the research in Japan. Int J Environ Res Public Health. 2016;13(8):781. doi: 10.3390/ijerph13080781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hamer M, Stamatakis E. Inflammation as an intermediate pathway in the association between psychosocial stress and obesity. Physiol Behav. 2008;94(4):536–539. doi: 10.1016/j.physbeh.2008.03.010. [DOI] [PubMed] [Google Scholar]
- 47.Coker AL, Bond SM, Pirisi LA. Life stressors are an important reason for women discontinuing follow-up care for cervical neoplasia. Cancer Epidemiol Biomarkers Prev. 2006;15(2):321–325. doi: 10.1158/1055-9965.EPI-05-0148. doi:15/2/321 [pii] [DOI] [PubMed] [Google Scholar]
- 48.Moore CJ, Cunningham SA. Social Position, Psychological Stress, and Obesity: A Systematic Review. J Acad Nutr Diet. 2012;112(4):518–526. doi: 10.1016/j.jand.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 49.Ayanian JZ, Block JP, He Y, Zaslavsky AM, Ding L. Psychosocial stress and change in weight among US adults. Am J Epidemiol. 2009;170(2):181–192. doi: 10.1093/aje/kwp104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Isasi CR, Parrinello CM, Jung MM, et al. Psychosocial stress is associated with obesity and diet quality in Hispanic/Latino adults. Ann Epidemiol. 2015;25(2):84–89. doi: 10.1016/j.annepidem.2014.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Heraclides A, Chandola T, Witte DR, Brunner EJ. Psychosocial stress at work doubles the risk of type 2 diabetes in middle-aged women: Evidence from the Whitehall II study. Diabetes Care. 2009;32(12):2230–2235. doi: 10.2337/dc09-0132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Annor FB, Roblin DW, Okosun IS, Goodman M. Work-related psychosocial stress and glycemic control among working adults with diabetes mellitus. Diabetes Metab Syndr. 2015;9(2):85–90. doi: 10.1016/j.dsx.2015.02.003. [DOI] [PubMed] [Google Scholar]
- 53.Hackett RA, Steptoe A. Psychosocial Factors in Diabetes and Cardiovascular Risk. Curr Cardiol Rep. 2016;18(10) doi: 10.1007/s11886-016-0771-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chida Y, Hamer M. An association of adverse psychosocial factors with diabetes mellitus: A meta-analytic review of longitudinal cohort studies. Diabetologia. 2008;51(12):2168–2178. doi: 10.1007/s00125-008-1154-1. [DOI] [PubMed] [Google Scholar]
- 55.Williams ED, Magliano DJ, Tapp RJ, Oldenburg BF, Shaw JE. Psychosocial stress predicts abnormal glucose metabolism: The Australian diabetes, obesity and lifestyle (ausdiab) study. Ann Behav Med. 2013;46(1):62–72. doi: 10.1007/s12160-013-9473-y. [DOI] [PubMed] [Google Scholar]
- 56.Seeman T, Epel E, Gruenewald T, Karlamangla A, McEwen BS. Socio- economic differentials in peripheral biology: Cumulative allostatic load. Ann N Y Acad Sci. 2010;1186(1):223–239. doi: 10.1111/j.1749-6632.2009.05341.x. [DOI] [PubMed] [Google Scholar]
- 57.Zalli A, Carvalho LA, Lin J, et al. Shorter telomeres with high telomerase activity are associated with raised allostatic load and impoverished psychosocial resources. Proc Natl Acad Sci U S A. 2014;111(12):4519–4524. doi: 10.1073/pnas.1322145111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Tandon PS, Saelens BE, Zhou C, Kerr J, Christakis DA. Indoor Versus Outdoor Time in Preschoolers at Child Care. Am J Prev Med. 2013;44(1):85–88. doi: 10.1016/j.amepre.2012.09.052. [DOI] [PubMed] [Google Scholar]


