Abstract
Background
Bone lengthening with an internal lengthening nail (ILN) avoids the need for external fixation and requires one less surgical procedure than lengthening over a nail (LON). However, LON has been shown to be superior to femoral internal lengthening using a mechanical nail. The magnetic ILN, a remote-controlled and magnet-driven device, may have overcome the weaknesses of earlier internal lengthening technology and may be superior to LON.
Questions/Purposes
(1) Is the magnetic ILN more accurate than LON for femoral lengthening? (2) Does the magnetic ILN demonstrate more precise distraction rate control than LON? (3) Does the magnetic ILN result in faster regenerate site healing, with more robust callus, than LON? (4) Does the magnetic ILN result in fewer complications, including impediments to knee motion, than LON?
Methods
We conducted a retrospective comparison of the records and radiographs of 21 consecutive patients with 22 femoral lengthenings using LONs and 35 consecutive patients with 40 femoral lengthenings using remote-controlled magnetic ILNs. Primary outcomes measured included accuracy, distraction rate precision, time to bony union, final knee range of motion, regenerate quality, and complications. The minimum follow-up times for the LON and ILN cohorts were 13 and 21 months, respectively.
Results
Patients treated with ILN had a lower post-treatment residual limb-length discrepancy (0.3 mm) than those treated with LON (3.6 mm). The rate of distraction was closer to the goal of 1 mm/day and more tightly controlled for the ILN cohort (1 mm/day) than that for the LON group (0.8 mm/day; SD, 0.2). Regenerate quality was not significantly different between the cohorts. Bone healing index for ILN was not statistically significant. Time to union was shorter in the ILN group (3.3 months) than that in the LON group (4.5 months). A lower percentage of patients experienced a complication in the ILN group (18%) than in the LON group (45%). Knee flexion at the end of distraction was greater for ILN patients (105°) than that for LON patients (88.8°), but this difference was no longer observed after 1 year.
Conclusions
Femoral lengthening with magnetic ILN was more accurate than with LON. The magnetic ILN comports the additional advantage of greater precision with distraction rate control and fewer complications. Both techniques afford reliable healing and do not significantly affect knee motion at the final follow-up. The magnetic ILN method showed no superiority in regenerate quality and healing rate.
Electronic supplementary material
The online version of this article (10.1007/s11420-017-9596-y) contains supplementary material, which is available to authorized users.
Keywords: internal lengthening nail, PRECICE, lengthening over a nail, limb lengthening
Introduction
External fixation has provided the stability and adjustability needed for successful femoral bone lengthening [5, 14, 26]. However, reliable, external fixation has been marred by patient dissatisfaction with pin site pain (and need for extended opioid use), infection (and antibiotic-related complications) [6, 8, 15], knee stiffness [2, 12, 16, 21], and the need for clothing modification [22]. The lengthening over a nail (LON) technique [29] was introduced to reduce the time patients needed to wear the external fixator by combining the simultaneous use of internal and external fixation, a concept called “integrated fixation” [1]. LON requires a two-stage surgical approach; the first surgery entails intramedullary (IM) nail insertion and external fixator (frame) application with pin insertion outside of the path of the nail. This is followed by a second surgery, at the completion of lengthening, to insert locking screws into the nail and remove the frame. The benefit is that the frame is no longer needed during the consolidation period (while the lengthened bone unites), reducing the external fixation index (EFI) (time in the frame). Integrated fixation has been shown to be safe and effective, despite the risk of deep infection from contaminated external fixation pins that are in close proximity to the internal implant [1, 4, 10, 13, 18, 20, 32].
The advantages of a fully implantable lengthening device are numerous [3, 11], but previous designs available in the USA were unreliable [23, 25, 34], making LON the preferred technique for femoral lengthening. The innovation of a magnetic internal lengthening nail (ILN) that utilizes an electromagnetic field (PRECICE®, NuVasive, Inc., Irvine, CA, USA) to accurately lengthen the femur has delivered such outstanding clinical results [6, 7, 19, 31, 33] that it merits further study and, specifically, a comparison with LON.
In this study, we asked the following questions: (1) Is the magnetic ILN method more accurate than the LON method in achieving the desired limb length? (2) Does the ILN demonstrate more precise distraction rate control compared with LON? (3) Does the regenerate site heal faster and with more robust callus when using the ILN? (4) Does the ILN result in fewer complications including impediments to knee motion when compared with LON?
Methods
We conducted a retrospective cohort study with institutional review board approval and in accordance with the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) guidelines. We reviewed the records and radiographs of a consecutive series of patients who underwent femoral LON between 2005 and 2009 and another consecutive series of those who underwent femoral lengthening using a magnetic remote-controlled ILN between 2012 and 2014. All procedures were performed by two fellowship-trained limb-lengthening and deformity surgeons at the same academic institution.
Two groups were identified using our patient registry. The indications for surgery were the same for both techniques and included shortening of the femur or lower extremity as a result of a posttraumatic incident or congenital, metabolic, or constitutional short stature (Table 1). Contraindications to surgery were active infection or irregular bone diameter or deformity that would prevent insertion of an intramedullary device.
Table 1.
Indication for surgery
| Etiology of femoral shortening | ILN (n) | LON (n) |
|---|---|---|
| Traumatic shortening (malunion) | 12 | 11 |
| Growth arrest | 2 | 2 |
| Metabolic | 4 | 2 |
| Congenital (unilateral) | 11 | 3 |
| Stature lengthening | 5 | 1 |
ILN internal lengthening nail, LON lengthening over nail
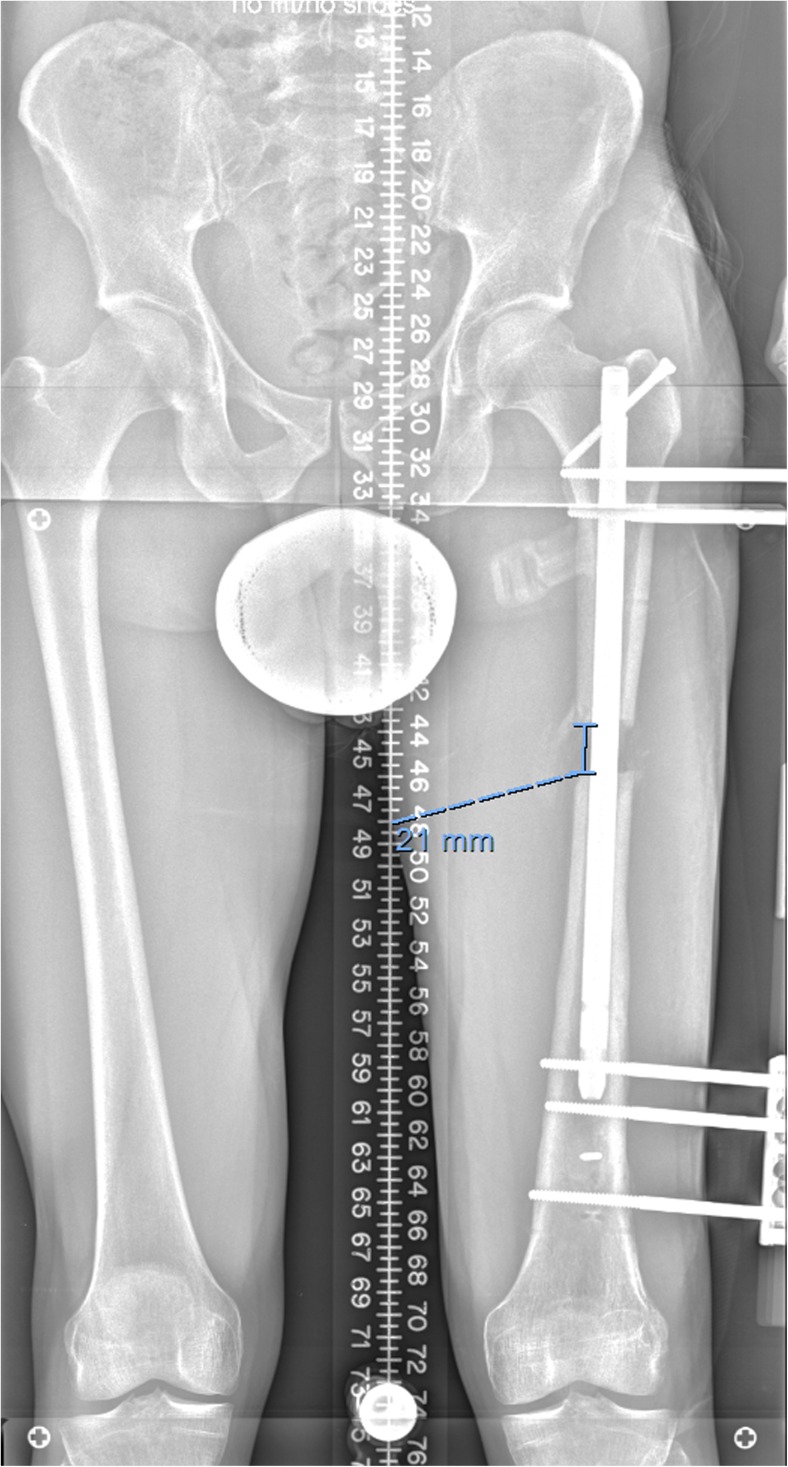
The preoperative evaluation was similar for both groups. Patients underwent a standard history and physical examination. Rotational deformity was identified with a prone examination and gait analysis. Standing anteroposterior (AP) lower extremity radiographs were obtained on 51-in. cassettes and measured in the picture archiving and communication system (PACS) with a calibration ball [17] (Fig. 1). AP and lateral radiographs were obtained of the affected femur and were measured in the same manner.
Fig. 1.
A 51-in. cassette shows both lower extremities including hip and ankle joints with an appropriate block under the short limb allowing for the accurate measurement of limb length.
The LON technique used was an antegrade nailing method similar to that described in previous studies [4, 18, 20, 25, 29]. The Schanz screws were 6-mm hydroxyapatite-coated tapered pins placed posteriorly to the nail in the lesser trochanter and in the distal femoral condyle (Fig. 2). The osteotomy was percutaneous using multiple drill holes followed by an osteotome. For children with open physes, a trochanteric entry point was used for the nail. The nail was locked proximally only. The frame used was a monolateral rail system (Biomet, Warsaw, IN, USA) (Fig. 3). The iliotibial band (ITB) was not released in these patients.
Fig. 2.
An intraoperative lateral fluoroscopy shot of the proximal femur shows two Schanz pins placed posterior to the intramedullary nail.
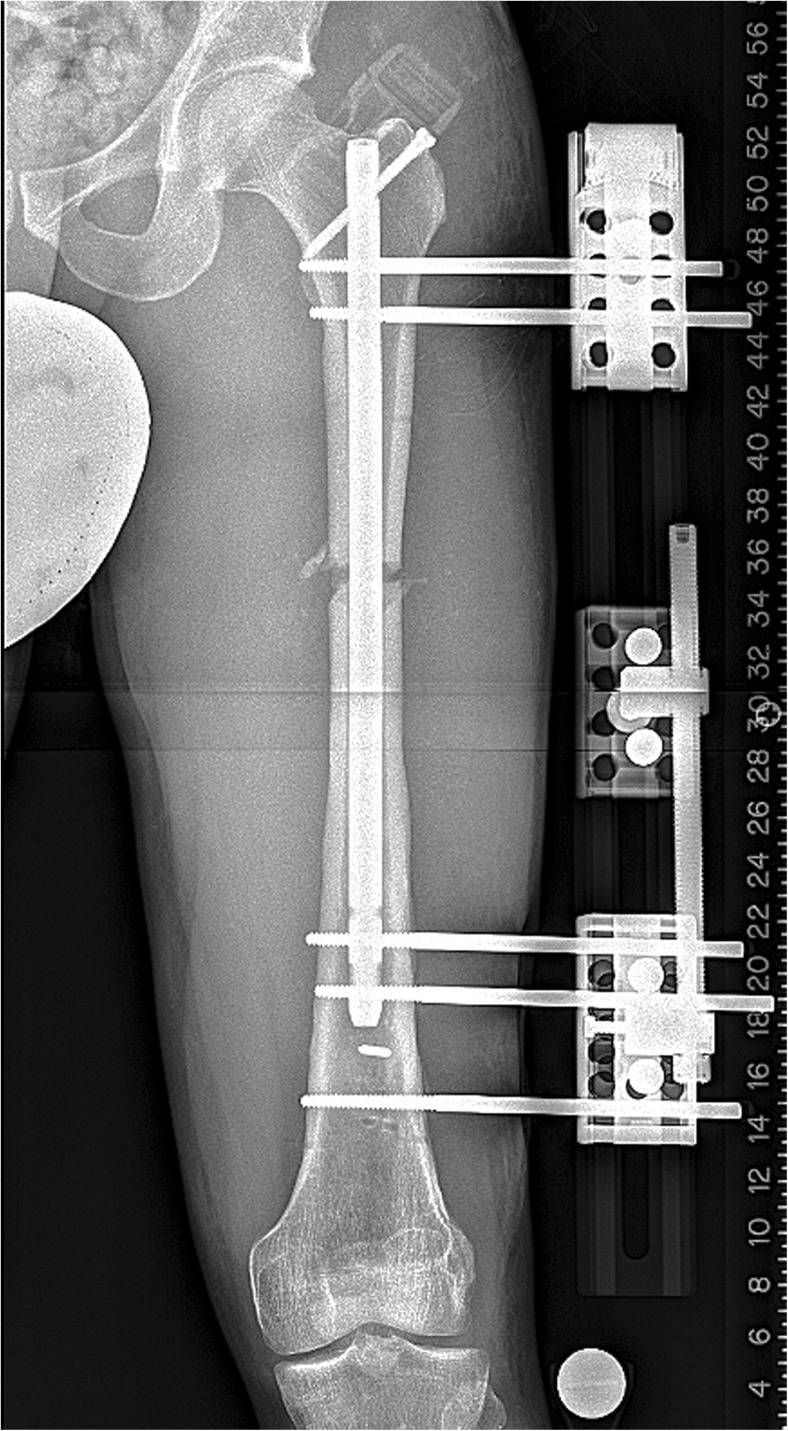
Fig. 3.
This AP radiograph shows a typical LON setup with the monolateral frame mounted parallel to the intramedullary nail and as close to the skin as safely possible.
For the magnetic ILN cohort, a well-described surgical technique, including both antegrade and retrograde nailing, was used [6, 7, 9, 19, 27, 28, 31, 33]. Steinmann pins or Schanz screws were placed posteriorly to the path of the ILN to mark rotational alignment. The osteotomy site was predrilled percutaneously. The canal was over-reamed 2 mm greater than the diameter of the nail and the reamings were noticed to extrude out through the drill holes. The corticotomy was completed with an osteotome. The PRECICE magnetic ILN was used. A separate, longitudinal incision was made along the lateral thigh 5 cm proximal to the superior pole of the patella. The ITB was cut across its fibers and the fractional lengthening extended along the anterior vastus fascia. The release was also extended posteriorly to include the lateral intramuscular septum. The decision to release the ITB in the ILN cohort but not in the LON patients was a change in practice decision. As the LON patients were all operated on prior to the invention of the ILN, we were not performing routine ITB release in lengthening patients. At the time the practice changed to use ILN, it also changed to include routine ITB release, with the reasoning that it would reduce pain, knee stiffness, and lengthening-induced deformity.
Postoperatively, patients received 23 h of IV antibiotics. Unless contraindicated, enoxaparin 40 mg daily was started on postoperative day (POD) two and continued for 14 days, at which point, aspirin 325 mg daily was used for another two weeks for venous thromboembolic prophylaxis. Physical therapy was ordered and focused on ambulation with weight-bearing restrictions. For LON patients, weight bearing as tolerated was allowed. For ILN patients, the weight bearing was dependent on the nail diameter (30, 50, or 70 lbs for 8.5-, 10.7-, and 12.5-mm nail diameters, respectively). Therapy included knee range of motion, emphasizing maintaining terminal extension. For LON patients, the frame was distracted at 1 mm/day starting on POD 5. For ILN patients, the lengthening started on POD 4 and proceeded at 1.32 mm/day (0.33 mm, 4 times/day) for 4 days, then slowed to 0.99 mm/day (0.33 mm, 3 times/day) thereafter.
Patients returned for an office visit every two weeks until the desired lengthening had been achieved. AP and lateral calibrated X-ray views of the femur were obtained at each visit. For the LON group, the distraction gap between bone ends (bony gap) was measured in millimeters, and the numbers of millimeters the patient distracted the frame were documented (Fig. 4). For the ILN group, the bony distraction gap was measured on both views and compared with the nail distraction gap (Fig. 5a, b). The quality of the regenerate was also assessed to confirm the best rate of distraction. Once the desired length was obtained, another standing 51-in. bilateral lower extremity film was taken to measure limb lengths and calculate residual limb-length discrepancy (LLD). In both groups, the IM nails were removed one year after surgery. In the ILN patients, the implanted magnet should be removed as per industry protocol. In the LON patients, concern about potential late infection due to some contamination of the internal implant by the half pins inspired universal IM nail removal.
Fig. 4.
The same patient is seen after 21 mm of distraction. The bony gap measured on the radiograph and then compared with the number of millimeters the patient recorded turning the frame distractor.
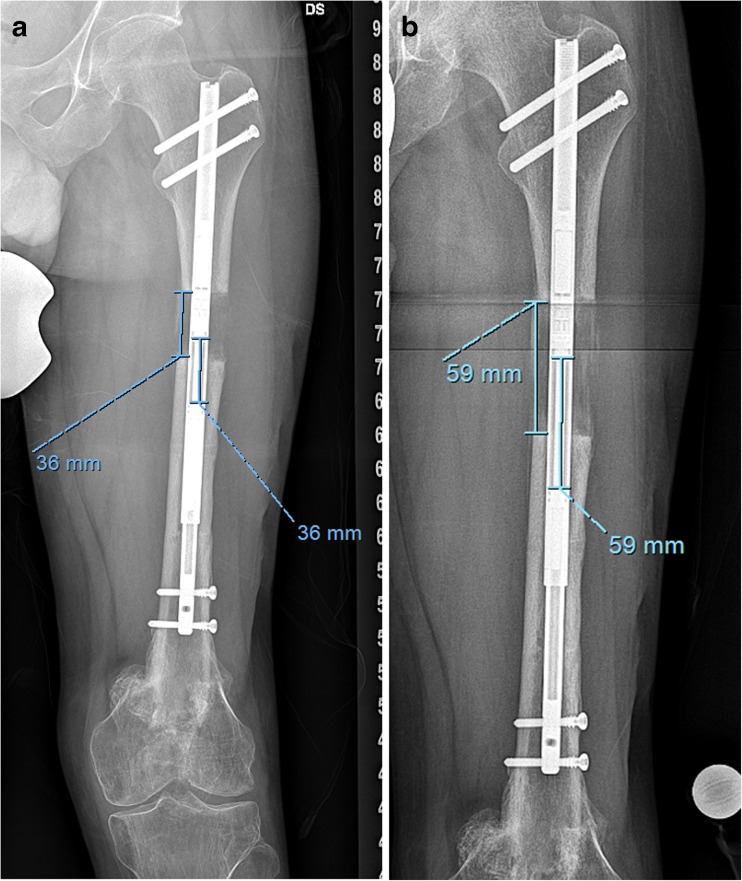
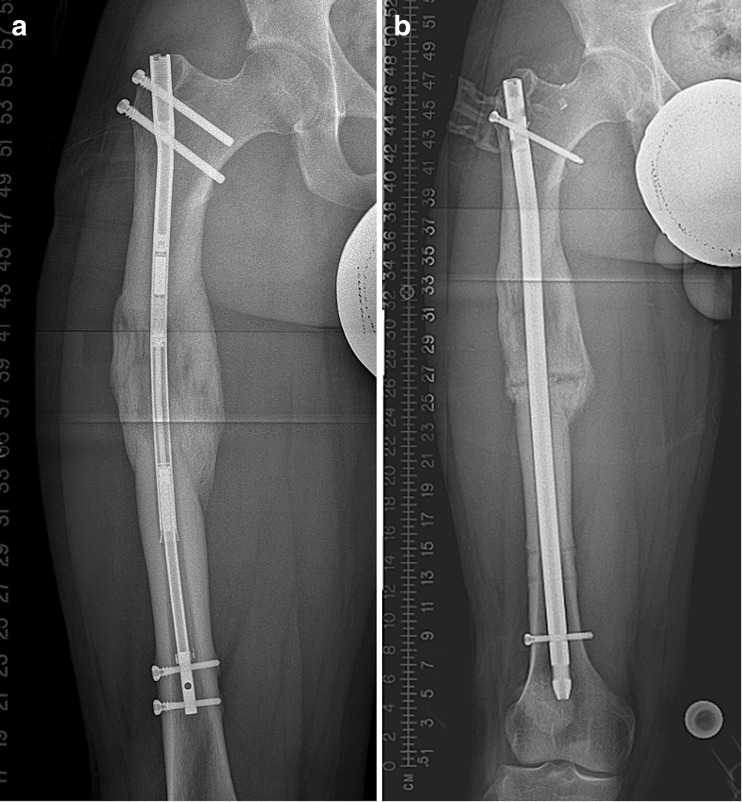
Fig. 5.
a The patient from Fig. 1 is seen at an interim follow-up visit after ILN lengthening. The amount of nail distraction is compared with the amount of bony gap. b The same patient at a later visit has the same comparison performed.
Chart review was used to record patient’s gender, age at time of surgery, etiology of shortening, and lengthening technique utilized (Table 2). Charted measurements of knee flexion and extension were collected at preoperative, end of distraction, and final follow-up time points. (The surgeon obtained these measurements in the office with a goniometer.) Union was defined as the time at which there was bridging bone on three of four cortices on the AP and lateral femur radiographs (Fig. 6a, b). From the radiographic record, the pre- and postoperative LLD and final length distracted were measured. The quality of the regenerate was measured by a single author on the radiographs obtained at eight weeks after surgery using a simplified modification of the method described by Li et al. [24, 25]. The regenerate types were graded as homogenous (A), heterogeneous (B), or sparse (C) based on their radiographic appearance at the eight-week postdistraction mark. The bone healing index, a measure of the rate at which bone heals after lengthening surgery, was also calculated. It is a simple calculation of time from osteotomy to full consolidation in months divided by the number of centimeters of length achieved. This currency can be used to compare techniques with that producing the lowest bone healing index being heralded as the best method. Complications encountered during treatment were recorded, including premature or delayed union, hardware failure, unintended angular deformity, knee contracture, leg-length discrepancy, unplanned surgery, or any other difficulties.
Table 2.
Patient demographics
| Characteristic | ILN | LON | p value | ||
|---|---|---|---|---|---|
| Mean or N | SD or % | Mean or N | SD or % | ||
| Age (years) | 29.7 | 13.6 | 32.4 | 14.2 | 0.487 |
| Gender | |||||
| M | 31 | 78% | 18 | 90% | 0.307 |
| F | 9 | 23% | 2 | 10% | |
| Side treated | |||||
| R | 20 | 50% | 8 | 40% | 0.464 |
| L | 20 | 50% | 12 | 60% | |
| Alcohol? | |||||
| N | 31 | 78% | 12 | 60% | 0.156 |
| Y | 9 | 23% | 8 | 40% | |
| Smoking (tobacco/e-cigarette)? | |||||
| N | 37 | 93% | 20 | 100% | 0.544 |
| Y | 3 | 8% | 0 | 0% | |
| Preop limb-length discrepancy (mm) | 26.8 | 23.5 | 43.3 | 20.4 | 0.007 |
ILN internal lengthening nail, LON lengthening over nail
Fig. 6.
a This AP radiograph of the same case as Figs. 2, 3, and 4, post-distal nail locking and frame removal, shows two cortices of bridging callus. b The lateral X-ray of the same patient shows bridging callus posteriorly but not anteriorly. With bony bridging on the posterior, medial, and lateral cortices, this patient is considered united.
Twenty-one patients with 22 femoral LON procedures and 35 patients with 40 femoral magnetic ILN lengthenings were identified. Two of the 21 patients in the LON group were lost to follow-up at three and four months post-frame removal, leaving 19 patients (20 femurs) in the group. One of the 35 patients in the ILN group was lost to follow-up after the first postoperative visit, leaving 34 patients (39 femurs). The minimum follow-up was 13 months (average, 27 months; range, 13–38 months) for the LON group and 21 months (average, 31 months; range, 21–43 months) for the ILN group.
Statistical Analysis, Study Size
Patient and surgical characteristics between the LON and magnetic ILN groups were evaluated using independent samples t tests for continuous variables and χ-square/Fisher’s exact tests for discrete factors. Continuous variables are reported as mean and standard deviation (SD), while discrete variables are reported as frequencies and percentages. To control for the differences in the distraction osteogenesis in patients, an additional stratified analysis was performed for patients who had a distraction rate of 1 mm or greater per day and those who had a distraction rate of less than 1 mm per day. Longitudinal analysis used generalized linear models to analyze range of motion outcomes of knee flexion and extension. Full factorial models were used to analyze the effect of time and study group. This modeling technique was used to maximize all observations from all patients, regardless of inconsistent data collection at follow-up. Parameter estimates were measured using maximum likelihood estimates. Statistical significance was defined as a p value that achieved 0.05 or below. All statistical analyses were performed using SPSS version 22.0 (IBM Corp., Armonk, NY, USA).
Results
In all cases, the goal was to lengthen the femur to the desired amount as determined preoperatively. The average preoperative LLD was 26.8 mm in the magnetic ILN group and 43.3 mm in the LON group (p = 0.007) (Table 2). (These numbers do not include stature-lengthening patients.) The femur was distracted 38.0 mm in the ILN group and 40.5 mm in the LON group (p = 0.666). (These statistics do include stature-lengthening patients.) The postoperative LLD (difference between desired length and final length) was 0.3 mm in the ILN group, and 3.6 mm in the LON cohort (p = 0.007) (Table 3).
Table 3.
Clinical characteristics
| Characteristic | ILN | LON | p value | ||
|---|---|---|---|---|---|
| Mean or N | SD or % | Mean or N | SD or % | ||
| Length distracted (mm) | 38.0 | 16.8 | 40.5 | 22.9 | 0.666 |
| Accuracy: mean residual limb-length discrepancy (mm) | 0.3 | 1.6 | 3.6 | 7.0 | 0.007 |
| Precision of distraction (mm) | 1.0 | 0.0 | 0.8 | 0.2 | < 0.001 |
| Modified Li score | |||||
| A (homogenous) | 35 | 88% | 14 | 70% | 0.082 |
| B (heterogeneous) | 5 | 12% | 4 | 20% | 0.565 |
| C (sparse) | 0 | 0% | 2 | 10% | 0.188 |
| Bone healing index (months/cm) | 1.0 | 0.5 | 1.4 | 0.8 | 0.101 |
| Time to union (months) | 3.3 | 1.0 | 4.5 | 1.7 | 0.001 |
| Nail diameter (mm) | 10.7 | 1.1 | 10.0 | 1.2 | 0.041 |
ILN internal lengthening nail, LON lengthening over nail
The precision of distraction rate control was calculated. For the LON group, the actual length distracted as measured between the bone ends (bony gap) was divided by the amount distracted on the external fixator (in millimeters). The calculated distraction ratio was 0.8 (SD, 0.2) in the LON group. For the ILN group, the actual length distracted as measured between the bone ends (bony gap) was divided by the amount the nail distracted. For the magnetic ILN group, the distraction ratio was 1 (SD, 0.2; p < 0.001). An additional stratified analysis was performed for patients who had a distraction rate of greater than and less than 1 mm/day which verified no skewness in distraction ratio within each group.
Our modified Li scores [24, 25] were homogenous (A), heterogeneous (B), or sparse (C). The scores were A in 88% and B in 12% of the magnetic ILN patients. In the LON group, the modified Li score was A in 70%, B in 20%, and C in 10% of patients. Although the ILN patients scored higher, the difference between these scores was not statistically significant (p = 0.082). The bone healing index was 1 in the magnetic ILN group versus 1.4 in the LON cohort (p = 0.101). Time to union was 3.3 months for the ILN cohort and 4.5 months in the LON group (p = 0.001). In all ILN cases, a minimum of 51 mm of the thick portion of the nail remained in the opposite fragment (mean, 96.3 mm; range, 51–160 mm), which is felt to be important for controlling the bone ends and preventing new deformities.
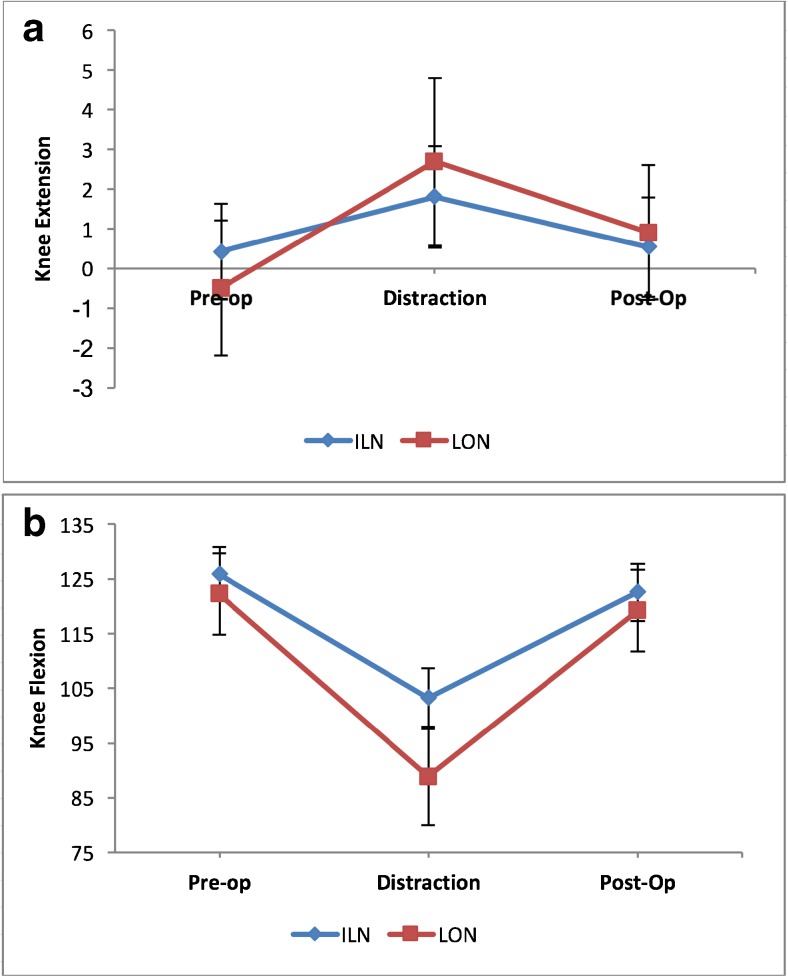
Complications occurred in 45% of patients in the LON group and 18% of patients in the ILN cohort (p = 0.027) (Table 4). Preoperative knee flexion was 122° in LON patients and 126° in ILN patients (p = 0.426) after removing two outliers in the LON cohort with knee extension contractures (one with a knee arthrodesis). Final postoperative knee flexion was 120° in LON patients (without outliers) and 123° in ILN patients (p = 0.464). When interim knee flexion at the end of distraction was analyzed, flexion was significantly greater for ILN patients (103°) than that for LON patients (89° without the same outliers) (p = 0.006) (Table 5; Fig. 7a, b).
Table 4.
Complications
| ILN | LON | |
|---|---|---|
| Delayed union | 1 | |
| Limb-length discrepancy | 1 | 1 |
| Varus deformity of regenerate | 2 | 1 |
| ILN fracture | 1 | |
| Premature consolidation | 2 | 2 |
| Unplanned surgeries | 5 | 4 |
| Skin dehiscence | 1 | |
| Excessive pain | 3 | |
| Knee contracture | 1 |
Patients with more than one complication were counted multiple times to illustrate the types of complications. Therefore, these numbers are not additive. Total number of complications in the ILN group was 7/39 limbs and in the LON group was 9/20 limbs
ILN internal lengthening nail, LON lengthening over nail
Table 5.
Knee range of motion
| Range of motion characteristic | ILN | LON | p value (between) | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| Knee extension | |||||
| Preoperative | 0.4 | 2.8 | − 0.5 | 3.6 | 0.385 |
| Distraction | 1.8 | 5.4 | 2.7 | 4.4 | 0.481 |
| Postoperative | 0.5 | 1.6 | 0.9 | 5.7 | 0.739 |
| p value (within) | 0.239 | 0.070 | |||
| Knee flexion | |||||
| Preoperative | 125.9 | 9.5 | 122.2 | 8.9 | 0.426 |
| Distraction | 103.3 | 25.2 | 88.8 | 20.0 | 0.006 |
| Postoperative | 122.6 | 14.9 | 119.2 | 11.5 | 0.464 |
| p value (within) | 0.000 | 0.000 | |||
| Knee arc of motion | |||||
| Preoperative | 125.5 | 9.5 | 116.3 | 29.9 | 0.145 |
| Distraction | 101.5 | 26.9 | 80.0 | 30.7 | 0.002 |
| Postoperative | 122.0 | 16.0 | 111.9 | 30.8 | 0.112 |
| p value (within) | 0.000 | 0.000 | |||
ILN internal lengthening nail, LON lengthening over nail
Fig. 7.
a This graphic representation of knee extension before, during, and after treatment shows more consistency in the magnetic ILN group. b This graphic representation of knee flexion before, during, and after treatment shows less variability in knee motion in the magnetic ILN group throughout treatment.
Discussion
Since implementing the ILN, we had observed that the magnetic ILN was quite accurate, exhibited excellent distraction rate control, produced a regenerate site with rapid healing and robust callus, and resulted in few complications. In this study, we sought to compare the magnetic ILN technique with a well-known and trusted method for distraction osteogenesis: the LON technique.
This study had a number of limitations. The study was performed in a retrospective, comparative manner with the two cohorts treated sequentially. There were more stature-lengthening patients and patients with congenital femoral shortening in the ILN cohort, resulting in suboptimal matching. Technical experience gained with the LON femoral-lengthening technique may have carried forward to greater facilitate the ILN method. Time to union was defined when three of four cortices were noted to be bridged on X-ray, which depends on the time of the office visit. This limitation affects both cohorts equally, though, and should not bias one group more than the other. Time to union is independent of lengthening distance, making bone healing index (time to union/length of regenerate bone) a more relevant parameter. Post-hoc power analysis determined that the sample size available for the study was adequately powered to find a statistically significant difference in time to union between the two study groups and a trend toward a difference in bone healing index. The quality of regenerate assessment and scoring was performed by only one observer. It would have been better to use two observers with multiple time points to calculate intra- and interobserver reliability. The ILN cohort had ITB releases while the LON cohort did not, making comparison of knee motion less reliable.
Our study showed the magnetic ILN to be highly accurate, allowing the desired length to be achieved with reliability. This accuracy corroborates the results reported in several other studies (Table 6). Lengthening with ILN was more accurate than lengthening using the LON technique.
Table 6.
Review of studies using the PRECICE nail
| Study | Type of study | Number of limbs | Accuracy of lengthening | Mean amount lengthened | Complications (number of events) |
|---|---|---|---|---|---|
| Paley et al. [30] | Retrospective | 65 total 54 femoral 2 fibula 8 tibial 1 humerus |
88.2%a | 44.1 mm | 26 total 3 nail breakages 1 premature consolidation 2 operator errors 4 dense regenerate 2 prominent hardwares 1 periprosthetic fracture 2 deep infection 3 failed regenerate 1 hematoma evacuation 3 soft tissue contractures 1 superficial infection 1 deep vein thrombosis 2 joint subluxations |
| Shabtai et al. [35] | Prospective | 21 total 16 femoral 5 tibial |
100%a | 44 mm | 7 total 4 delayed bone healing 1 hip contracture 1 hip subluxation 1 knee subluxation |
| Kirane et al. [19] | Retrospective | 25 total 17 femoral 8 tibial |
96%b | 35 mm | 7 total 1 implant failure 1 premature consolidation 2 delayed bone healing 2 delayed equinus contractures 1 toe clawing |
| Schiedel et al. [34] | Prospective | 26 total 20 femoral 6 tibial |
97%a | 37 mm | 4 total 2 nail breakages 1 nail failed to function 1 premature consolidation |
aAccuracy measured after total lengthening; accuracy = lengthening achieved/desired lengthening
bMeasured accuracy of distraction at each postoperative visit; accuracy = 100—absolute % error of distraction
The importance of lengthening with the proper rate and rhythm is well established. The unpredictable distraction rates of the intramedullary skeletal kinetic distractor were among the reasons the authors reverted to LON and may have contributed to problems with regenerate quality in some of those patients. Femoral lengthening with the magnetic ILN more precisely controlled the distraction rate than lengthening using the LON method. This is a distinct advantage of the ILN and is likely a result of elimination of cantilever inefficiencies inherent in the monolateral frames.
The difference in modified Li scores was not significant between cohorts. The technique of the osteotomy, the intramedullary canal reaming, and the presence of an IM rod were all constant across both methods.
The percentage of patients who experienced a complication did differ significantly between cohorts, and the types of complications encountered varied. Both groups had premature consolidations. The LON group had one case of skin breakdown around a pin site, two cases of premature consolidation (one with a varus deformity), and one case of knee flexion contracture. The ILN group had no wound-related complications, one case of delayed union, two cases of varus deformity, one case of over-lengthening, and one case of nail breakage. It is important to be vigilant for varus deformity, which occurs in both femoral-lengthening techniques. Over-reaming may allow either bone fragment to fall into varus. Trochanteric entry may facilitate varus nail insertion. The 8.5-mm-diameter ILN may bend slightly through the unsupported region to cause this deformity, as was the case with one of the above-reported complications (Fig. 8a, b). The case of over-lengthening was treated by reversing the motor for four days with no ill effect on healing or final limb length. The broken nail was likely a problem of the first generation of this nail, which had a seam between two portions of the upper part of the nail. This has been changed with the current generation of the nail, and we have not found any further incidents of this failure mode, albeit in the context of modest lengthenings. The finding that the ILN group had greater knee range of motion at the end of distraction was statistically significant; however, ITB release was performed routinely at the index surgery. This finding may be a marker for overall improved comfort during treatment with this method when compared with LON as observed by Landge et al. [22]. The IT band releases we performed on the ILN patients but not on the LON patients are a confounding variable. Furthermore, the total bone lengthening and therefore soft tissue tension was greater in the LON cohort, making knee motion at completion of distraction an unfair comparison. Although not technically a complication, the additional operation to lock the nail and remove the fixator at the end of the lengthening phase in patients treated with LON adds additional expense and general risk. The elimination of this operative intervention is a benefit of the ILN technique. Both groups had all nails removed eventually. While this additional surgery was a necessary part of both techniques, it had no effect on the imbalance in the total number of surgeries for each technique.
Fig. 8.
a This patient had a trochanteric entry 8.5-mm ILN that bent into varus. b This was remedied with a novel osteotomy and exchange nailing.
In conclusion, femoral lengthening with the magnetic ILN offers the limb-lengthening surgeon great accuracy in achieving lengthening goals and was more accurate than the LON technique. The ILN has more precise distraction rate control and fewer complications. The regenerate was not more robust and did not consolidate faster with ILN based on our sample size. Both techniques afford reliable healing and do not significantly affect knee motion at final follow-up. The ILN method maintains an acceptable risk of complications and obviates the need for the additional surgery requisite with LON. In our practice, these benefits have allowed us to replace LON with the magnetic ILN for nearly all cases requiring femoral lengthening.
Electronic Supplementary Material
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
Acknowledgements
We thank our research coordinator Eugene Borst for his help in managing the clinical data collection.
Compliance with Ethical Standards
Conflict of Interest
Anton M. Kurtz, MD, Jonathan R. Barclay, BS, and Joseph Nguyen, MPH, declare that they have no conflicts of interest. Austin T. Fragomen, MD, reports receiving personal fees from NuVasive, Smith and Nephew, and Synthes, outside the submitted work. S. Robert Rozbruch, MD, reports receiving personal fees from NuVasive, Smith and Nephew, and Stryker, outside the submitted work.
Human/Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2013.
Informed Consent
Informed consent was waived from all patients for being included in this study.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Footnotes
Level of Evidence: Therapeutic Study: Level III
Investigation performed at the Hospital for Special Surgery, New York, NY
Electronic supplementary material
The online version of this article (10.1007/s11420-017-9596-y) contains supplementary material, which is available to authorized users.
References
- 1.Bernstein M, Fragomen AT, Sabharwal S, Barclay J, Rozbruch SR. Does integrated fixation provide benefit in the reconstruction of posttraumatic tibial bone defects? Clin Orthop Relat Res. 2015;473(10):3143–3153. doi: 10.1007/s11999-015-4326-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bhave A, Shabtai L, Woelber E, Apelyan A, Paley D, Herzenberg JE. Muscle strength and knee range of motion after femoral lengthening. Acta Orthop. 2016;28:1–6. doi: 10.1080/17453674.2016.1262678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Black SR, Kwon MS, Cherkashin AM, Samchukov ML, Birch JG, Jo CH. Lengthening in congenital femoral deficiency: a comparison of circular external fixation and a motorized intramedullary nail. J Bone Joint Surg Am. 2015;97(17):1432–1440. doi: 10.2106/JBJS.N.00932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fernandes HP, Barronovo DG, Rodrigues FL, Hono M. Femur lengthening with monoplanar external fixator associated with locked intramedullary nail. Rev Bras Ortop. 2016;52(1):82–86. doi: 10.1016/j.rbo.2016.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fragomen AT, Rozbruch SR. The mechanics of external fixation. HSS J. 2007;3(1):13–29. doi: 10.1007/s11420-006-9025-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fragomen AT, Rozbruch SR. Lengthening of the femur with a remote controlled magnetic intramedullary nail: retrograde technique. JBJS Essent Surg Tech. 2016;6(2):e20. doi: 10.2106/JBJS.ST.15.00069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fragomen AT, Rozbruch SR. Lengthening and deformity correction about the knee using a magnetic internal lengthening nail. SICOT J. 2017;3(25):1–10. doi: 10.1051/sicotj/2017014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fragomen AT, Miller AO, Brause BD, Goldman V, Rozbruch SR. Prophylactic post operative antibiotics may not reduce pin site infections after external fixation. HSS J. 2017;13(2):165–170. doi: 10.1007/s11420-016-9539-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hammouda AI, Jauregui JJ, Gesheff MG, Standard SC, Conway JD, Herzenberg JE. Treatment of post traumatic femoral discrepancy with PRECICE magnetic powered intramedullary lengthening nails. J Orthop Trauma. 2017;31(7):369–374. doi: 10.1097/BOT.0000000000000828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harbacheuski R, Fragomen AT, Rozbruch SR. Does lengthening and plating shorten duration of external fixation? Clin Orthop Relat Res. 2012;470(6):1771–1781. doi: 10.1007/s11999-011-2178-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Horn J, Grimsrud Ø, Dagsgard AH, Huhnstock S, Steen H. Femoral lengthening with a motorized intramedullary nail. Acta Orthop. 2015;86:248–256. doi: 10.3109/17453674.2014.960647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hosalkar HS, Jones S, Chowdhury M, Hartley J, Hill RA. Quadricepsplasty for knee stiffness after femoral lengthening in congenital short femur. J Bone Joint Surg Br. 2003;85(2):261–264. doi: 10.1302/0301-620X.85B2.13144. [DOI] [PubMed] [Google Scholar]
- 13.Iobst CA, Dahl MT. Limb lengthening with submuscular plate stabilization: a case series and description of the technique. J Pediatr Orthop. 2007;27(5):504–509. doi: 10.1097/01.bpb.0000279020.96375.88. [DOI] [PubMed] [Google Scholar]
- 14.Kawoosa AA, Wani IH, Dar FA, Sultan A, Qazi M, Halwai MA. Deformity correction about knee with Ilizarov technique: accuracy of correction and effectiveness of gradual distraction after conventional straight cut osteotomy. Ortop Traumatol Rehabil. 2015;17(6):587–592. doi: 10.5604/15093492.1193011. [DOI] [PubMed] [Google Scholar]
- 15.Kazmers NH, Fragomen AT, Rozbruch SR. Prevention of pin site infection in external fixation: a review of the literature. Strat Trauma Limb Recon. 2016;11:75–85. doi: 10.1007/s11751-016-0256-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Khakharia S, Fragomen AT, Rozbruch SR. Limited quadsplasty for contracture during femoral lengthening. Clin Orthop Rel Res. 2009;467(11):2911–2917. doi: 10.1007/s11999-009-0951-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Khakharia S, Bigman D, Fragomen AT, Pavlov H, Rozbruch SR. Comparison of PACS and hard-copy 51-inch radiographs for measuring leg length and deformity. Clin Orthop Relat Res. 2011;469:244–250. doi: 10.1007/s11999-010-1460-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim HJ, Fragomen AT, Reinhardt K, Hutson JJ, Rozbruch SR. Lengthening of the femur over an existing IM nail. J Orthop Trauma. 2011;25:681–684. doi: 10.1097/BOT.0b013e3181f92d6e. [DOI] [PubMed] [Google Scholar]
- 19.Kirane YM, Fragomen AT, Rozbruch SR. Precision of the PRECICE internal bone lengthening nail. Clin Orthop Relat Res. 2014;472:3869–3878. doi: 10.1007/s11999-014-3575-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kocaoglu M, Eralp L, Bilen FE, Balci HI. Fixator-assisted acute femoral deformity correction and consecutive lengthening over an intramedullary nail. J Bone Joint Surg Am. 2009;91(1):152–159. doi: 10.2106/JBJS.H.00114. [DOI] [PubMed] [Google Scholar]
- 21.Koczewski P, Shadi M. Repair of the knee extension apparatus in the treatment of knee extension contracture after femoral lengthening. Chir Narzadow Ruchu Ortop Pol. 2005;70(2):91–96. [PubMed] [Google Scholar]
- 22.Landge V, Shabtai L, Gesheff M, Specht SC, Herzenberg JE. Patient Satisfaction After Limb Lengthening with Internal and External Devices. J Surg Orthop Adv. 2015;24(3):174–179. doi: 10.3113/JSOA.2015.0174. [DOI] [PubMed] [Google Scholar]
- 23.Lee DH, Ryu KJ, Song HR, Han SH. Complications of the Intramedullary Skeletal Kinetic Distractor (ISKD) in distraction osteogenesis. Clin Orthop Relat Res. 2014;472(12):3852–3859. doi: 10.1007/s11999-014-3547-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Li R, Saleh M, Yang L, Coulton L. Radiographic classification of osteogenesis during bone distraction. J Orthop Res. 2006;24:339–347. doi: 10.1002/jor.20026. [DOI] [PubMed] [Google Scholar]
- 25.Mahboubian S, Seah M, Fragomen AT, Rozbruch SR. Femoral lengthening with lengthening over a nail has fewer complications than intramedullary skeletal kinetic distraction. Clin Orthop Relat Res. 2012;470:1221–1231. doi: 10.1007/s11999-011-2204-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McCarthy JJ, Ranade A, Davidson RS. Pediatric deformity correction using a multiaxial correction fixator. Clin Orthop Relat Res. 2008;466(12):3011–3017. doi: 10.1007/s11999-008-0491-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Muthusamy S, Rozbruch SR, Fragomen AT. The use of blocking screws with internal lengthening nail and reverse rule of thumbs for blocking screws in limb lengthening and deformity correction surgery. Strategies Trauma Limb Reconstruct. 2016;11(3):199–205. doi: 10.1007/s11751-016-0265-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Paley D. PRECICE intramedullary limb lengthening system. Expert Rev Med Devices. 2015;12(3):231–249. doi: 10.1586/17434440.2015.1005604. [DOI] [PubMed] [Google Scholar]
- 29.Paley D, Herzenberg JE, Paremain G, Bhave A. Femoral lengthening over an intramedullary nail. A matched-case comparison with Ilizarov femoral lengthening. J Bone Joint Surg Am. 1997;79(10):1464–1480. doi: 10.2106/00004623-199710000-00003. [DOI] [PubMed] [Google Scholar]
- 30.Paley D, Harris M, Debiparshad K, Prince D. Limb lengthening by implantable limb lengthening devices. Tech Orthop. 2014;29(2):72–85. doi: 10.1097/BTO.0000000000000072. [DOI] [Google Scholar]
- 31.Rozbruch SR, Fragomen AT. Lengthening of the femur with a remote-controlled magnetic intramedullary nail: antegrade technique. JBJS Essential Surgical Techniques. 2016;6:e2–e2. doi: 10.2106/JBJS.ST.O.00063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rozbruch SR, Kleinman D, Fragomen A, Ilizarov S. Limb lengthening and then insertion of an intramedullary nail. A case matched comparison. Clin Orthop. 2008;466(12):2923–2932. doi: 10.1007/s11999-008-0509-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rozbruch SR, Birch JG, Dahl MT, Herzenberg JE. Motorized intramedullary nail for management of limb-length discrepancy and deformity. J Am Acad Orthop Surg. 2014;22:403–409. doi: 10.5435/JAAOS-22-07-403. [DOI] [PubMed] [Google Scholar]
- 34.Schiedel FM, Vogt B, Tretow HL, Schuhknecht B, Gosheger G, Horter MJ, Rödl R. How precise is the PRECICE compared to the ISKD in intramedullary limb lengthening? Reliability and safety in 26 procedures. Acta Orthop. 2014;85:293–298. doi: 10.3109/17453674.2014.913955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shabtai L, Specht SC, Standard SC, Herzenberg JE. Internal lengthening device for congenital femoral deficiency and fibular hemimelia. Clin Orthop Relat Res. 2014;472(12):3860–3868. doi: 10.1007/s11999-014-3572-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)