Abstract
Background
Hamstring injuries can present in numerous forms, some of which can lead to persistent pain, loss of function, and delay in return to sport. Although most are treated conservatively, proximal and distal tendon avulsion injuries have become more commonly treated with surgery. Distal semitendinosus avulsion injuries have been largely reported in the elite athlete population. While conservative management has been utilized, failure in this group can significantly impact a future career.
Purpose
The purpose of the manuscript is to describe our approach of surgical tendon excision for distal semitendinosus injury in an elite athlete.
Methods
We highlight a two-incision technique to isolate the avulsed tendon, followed by exteriorization and tendon excision. In addition, we provide insight on clinical and imaging findings to help guide management.
Results
This technique provides a reliable and effective surgical option for managing these rare injuries of the distal semitendinosus, along with outlining rehabilitation goals in the postoperative period.
Conclusion
In this setting, we present a detailed surgical technique to excise the injured distal semitendinosus tendon to promote recovery and potentially allow for earlier return to play.
Electronic supplementary material
The online version of this article (10.1007/s11420-017-9585-1) contains supplementary material, which is available to authorized users.
Keywords: Tendon excision, Distal semitendinosus
Introduction
Hamstring injuries are commonly encountered athletic injuries [1, 3, 4, 8, 12] and can account for the highest delay in return to play at the elite level [5, 6]. The injury mechanism for muscle belly strain is often related to concentric contraction while sprinting, whereas proximal and distal avulsion injuries are generally caused by eccentric overload. Skilled-position players are at the highest risk for injury, with distal semitendinosus avulsions almost exclusively seen in the elite athlete [5, 6]. Injury of the bicep femoris represents the most common hamstring injury, while distal semitendinosus injuries comprise 32% to 37% of the hamstring injury subset [2, 14]. Previously, Cooper et al. [4] had reported that tendon excision of distal semitendinosus ruptures in high-level athletes resulted in recovery at 6.8 weeks postoperatively, as compared to an average of 16.8 weeks in those managed conservatively. Distal avulsions of the semitendinosus from its pes anserinus insertion can cause recurrent symptoms if treated conservatively, as the disrupted length-tension relationship may lead to reinjury. However, tendon excision can provide a reliable treatment to prevent aberrant scarring and potential delay in return to sport. While surgical excision of the avulsed tendon has been successful in this clinical scenario, limited technical guidance exists on how to address these injuries. In this report, we present a detailed surgical approach for the management of distal semitendinosus injury in the elite athlete.
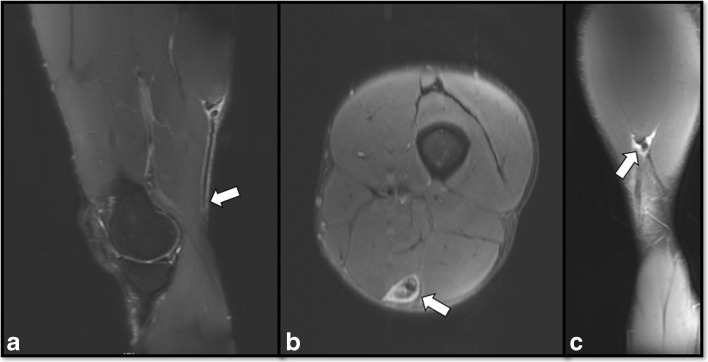
In this report, we profile a 25-year-old professional football player who sustained an acute distal hamstring injury while returning a punt during competitive gameplay. In order to prevent adhesion formation and potential delay in return to sport, the decision for operative management was made to excise the injured tendon to facilitate recovery. Magnetic resonance imaging (MRI) was used prior to surgery to assess the injury extent, which showed complete disruption and proximal retraction of the distal semitendinosus tendon (Fig. 1). In this scenario, surgery was performed 2 days post-injury.
Fig. 1.
Preoperative magnetic resonance imaging (MRI) depicting the distal semitendinosus injury. Sagittal T2, fat suppressed MRI image showing proximal retraction of the distal semitendinosus tendon (arrow) (a). Axial T2, fat suppressed MRI image showing injury to the semitendinosus with surrounding scar formation (arrow) (b). Coronal T2, fat suppressed MRI depicting the injury at the musculotendinous junction of the semitendinosus (arrow) (c).
Surgical Technique
The patient sustained the injury during rapid deceleration from a sprint while returning a punt. This led to immediate posteromedial thigh pain and pain limiting his ambulation. Further evaluation with MRI confirmed a diagnosis of a distal semitendinosus avulsion. While retraction can vary depending on the injury location and dynamic change based on contraction force, the semitendinosus tendon stump in this scenario was found to be 14 cm proximal to the popliteal crease. Given the physical demands of a professional athlete, the patient opted for surgical intervention with the target of an early return to sport. Given these goals, the patient was indicated for distal semitendinosus excision to aid in possible expedition of his recovery.
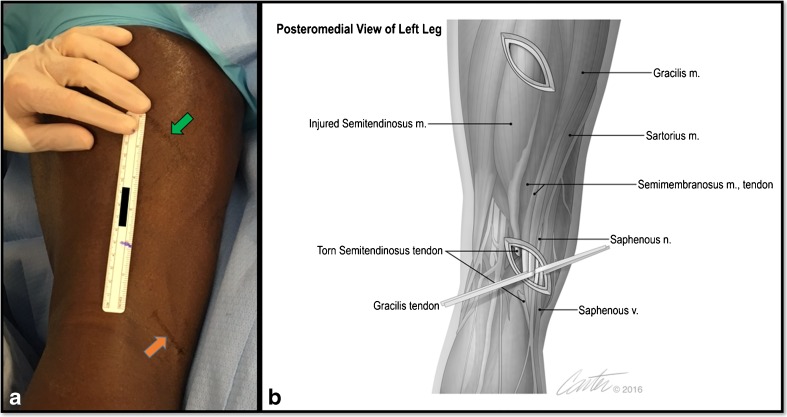
The operation was performed with the patient under general anesthesia in the prone position on a regular table. A thigh tourniquet was placed proximally but not inflated at any point during the procedure. A two-incision technique was used to isolate the ruptured semitendinosus. Using measurements obtained from the preoperative MRI, the location of the retracted distal semitendinosus stump and area immediately proximal to the musculotendinous junction were marked at the corresponding levels on the posteromedial thigh (Fig. 2). The muscle belly of the proximal hamstring can be palpated for the proximal incision; however, the distal incision is created based on the measured level of distal tendon retraction. In this case, the distal incision was marked at 14 cm above the popliteal crease over the posteromedial thigh, where the avulsed semitendinosus was measured on preoperative MRI.
Fig. 2.
A two-incision surgical technique is utilized for isolating the injured semitendinosus. Using preoperative measurements with magnetic resonance imaging, surgical incisions are marked at the level of the retracted distal tendon (orange arrow) and proximal musculotendinous junction (green arrow) of the semitendinosus over the posteromedial thigh (a). An artistic rendering of the surgical approach, with relevant anatomy encountered through both incisions (b).
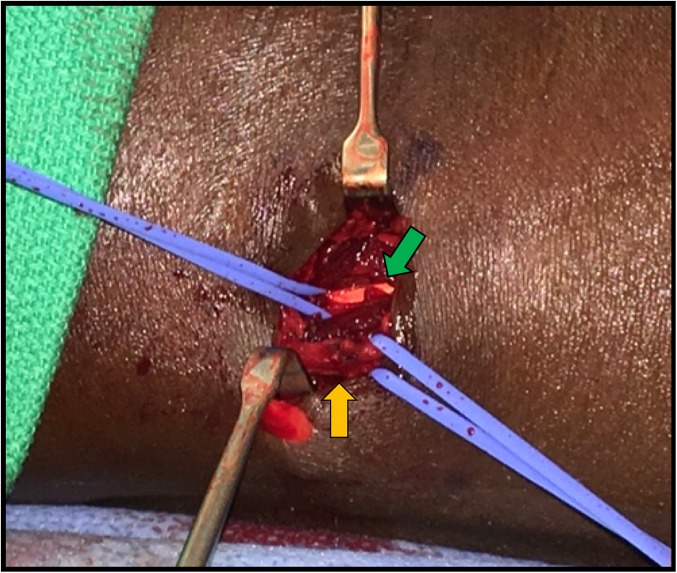
A distal oblique incision was first created over the posteromedial knee at the measured level of the avulsed tendon stump. Blunt dissection was used for the subcutaneous layers and the overlying popliteal fascia was sharply incised longitudinally. Care was taken to identify and preserve the gracilis tendon as well as the saphenous nerve, which is at risk with this approach (Fig. 3). The ruptured tendon stump was then identified superficially under the fascia, and present injury hematoma was evacuated.
Fig. 3.
Distal approach for identifying the injured distal semitendinosus tendon. This highlights the gracilis tendon (green arrow) and saphenous nerve and vein (orange arrow), which should be isolated and protected during dissection.
Notably, there is little tension present in the semitendinosus tendon after avulsion, which can create difficulty in being able to identify the structure by palpation. In the acute setting, the edema surrounding the tendon may also help direct dissection. However, significant edema is likely absent in the chronic setting, yet the retracted tendon is usually quite hypertrophied and potentially more easily palpable.
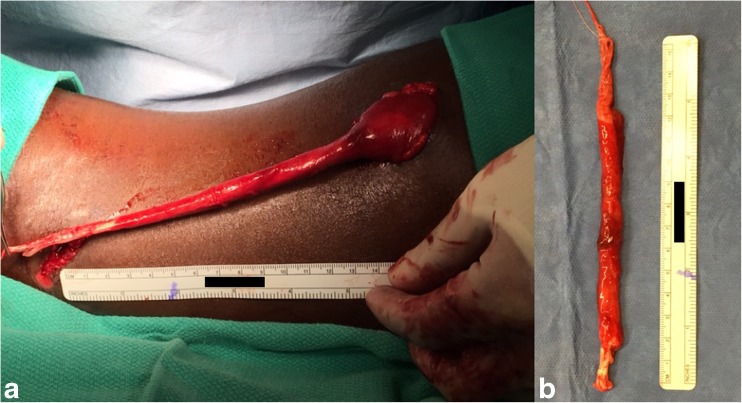
Using an Allis clamp to provide tension on the distal semitendinosus, mobilization of the avulsed tendon is performed. Surrounding adhesions or edematous tissue surrounding the injured tendon is removed, and the tendon is manually delivered out the distal skin incision. The tendon stump can then be tagged with nonabsorbable suture if needed to provide further traction. Attention is then turned to creating the proximal incision. By putting traction on the distal tendon, the course of the muscle becomes evident, also guiding the placement of the proximal incision. The proximal incision is made at a minimum of 15 cm proximal to the distal incision, to ensure that access is proximal to the myotendinosus junction. After the proximal incision is created and dissection of the fascia is performed, the semitendinosus muscle belly is identified superficially under the fascia. A right-angle hemostat was used to isolate the semitendinosus and exteriorize the distal extent of the muscle from the proximal incision (Fig. 4). Using a cautery device for hemostasis, the tendon stump is then excised at the level of the musculotendinous junction, leaving maximal muscle fibers. Using this incision immediately proximal to the myotendinosus junction allows for complete excision of the tendon. The course of the semitendinosus, between the two incisions, is then explored and cleared of any adhesions until there is unobstructed communication between both the proximal and distal incisions. This can be performed by providing retraction near the exposure. If present, surrounding fibrous tissue can be removed with cautery or sharp dissection after removal of the tendon. The use of irrigation of the semitendinosus tendon tract from the proximal incision can be used to confirm continuity and unimpeded flow to the distal incision. Complete removal of the hematoma in this tract may also modify the environment to reduce formation of fibrous tissue. This proximal muscle belly of the semitendinosus can then be gently placed back into the thigh at its resting tension.
Fig. 4.
Intraoperative images during tendon excision. The injured semitendinosus is exteriorized from the proximal incision to perform tenotomy at the musculotendinous junction (a). The excised tendon with minimizing proximal muscle disruption (b).
The wounds are thoroughly irrigated and closure is completed with 0 vicryl for fascia, 2–0 vicryl for the subcutaneous layer, and 4–0 prolene for subcuticular skin closure. Dry dressing and compressive wrap are placed with incorporation of a long narrow foam brick that provides additional compression along the distal course of the semitendinosus. A postoperative hinged brace is optional. A subfascial drain is recommended to prevent seroma formation, which can be subsequently discontinued at 12 to 24 h after surgery.
Postoperatively, we allow gentle active knee motion and gradual increase in weight bearing on crutches over a week. The compressive dressing is left in place for 3 to 5 days. Sutures are removed at 10 days. Following suture removal, there should be a rapid progression of activities with stationary bike exercises and achievement of full knee motion. In contrast to the generally accepted hamstring rehabilitation protocols, we recommend early hamstring stretching in order to prevent adhesions and to restore flexibility. A progressive strengthening program is begun when discomfort subsides. Once pain, motion, flexibility, and strength are improved to near-baseline levels with activities of daily living, then jogging is allowed. A functional dynamic brace on the field is initiated once the player is able to jog without discomfort. We also implement a dynamic elastic cord resistance program to increase work load, and slowly progress to full speed sprinting. Elastic resistance (including elastic bands or tubing) has been used for initiating muscle recruitment and activation, which are effective closed-chain exercises for rehabilitation [11]. The athlete should be able to sustain a high work load and maintain that ability for running at full speed without setback before return to play at an elite level.
Discussion
Surgical management of distal semitendinosus injuries has been rarely reported, most frequently in response to failed conservative management [4, 7, 10]. Formation of scarring, tendon hypertrophy, and surrounding adhesion post-injury can lead to persistent pain following injury. A fascial stricture in the popliteal region where the semitendinosus intersects with the semimembranosus tendon can be problematic in these select injuries. The difficulty with the resultant tendon hypertrophy and scarring is that it may intermittently cause symptoms when the athlete accelerates to full sprinting speed. Our experience is that a sudden setback in progression is due to reinjury because of scar formation in this area. While difficulty remains in predicting which athletes will be successful with nonoperative management, early intervention has provided reliable results for return to play [4]. In this report, we provide the surgical technique of distal semitendinosus excision along with rehabilitation goals for the elite athlete.
Cooper et al. [4] had shown that distal semitendinosus injuries had a 42% failure rate with nonoperative management. For those athletes who opted for surgical intervention with tendon excision returned to sport at 6.8 weeks. In addition, no clinical differences, including hamstring flexibility, were found at an average follow-up of 13 months. As previously suggested [13], we also advocate for removal of fibrous scar tissue and adhesions to allow for muscle-to-muscle healing in a tension-free environment. Removing any potential nidus for scarring can allow for early rehabilitation and has been suggested to prevent reinjury [13].
Sonnery-Cottert et al. [13] recently reported a case series of 10 professional athletes managed with operative intervention for recurrent hamstring injury. In this group, four had distal semitendinosus injuries that were treated by distal tenotomy with a stripping device. In this cohort of athletes, an average return to play was reported at 3.5 months. While good results were obtained, the caveat with this approach would be the inability to adequately address the post-injury adhesions and fibrotic formations along the course of the injured tendon. This may be especially relevant in the subacute or chronic setting. Also, the use of a stripping device for hamstring harvest does have an associated risk for iatrogenic nerve injury [9] and anecdotally may not be large enough to address the massively hypertrophied distal tendon in certain athletic populations.
We also comment on unpublished reports of soft tissue tenodesis of the semitendinosus to the nearby semimembranosus. This technique may incorporate increased scar formation with tendon healing after injury and potentially produce further symptoms. We do not recommend tenodesis, for concern that scar formation and hypertrophy may occur in the same region of the popliteal fascial stricture where the retracted avulsed tendon tends to rest and may scar after injury. In addition, this does not restore a normal length-tension relationship of the semitendinosus.
Potential risks associated with this technique include injury to the saphenous nerve and gracilis tendon, which can be encountered during dissection to the posteromedial thigh. In addition, hematoma formation can be problematic with creation of a void following tendon excision. As noted in our technique description, we find the use of foam compression over the posterior thigh to help in preventing hematoma during the initial postoperative period.
This approach provides a surgical option for management of acute and chronic distal semitendinosus injuries. Addressing fibrous adhesions and removing the distal tendon can help prevent scarring and may lead to reliable results with early return to play. We find this to be a reliable surgical technique and provide this report to help guide surgeons presented with this unique injury.
Electronic supplementary material
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
Compliance with Ethical Standards
Conflict of Interest
Brian J. Rebolledo, MD, and Timothy R. McAdams, MD, declare that they have no conflict of interest. Daniel E. Cooper, MD, reports receiving fees as a consultant from Arthrex and Stryker and royalties from Stryker.
Human/Animal Rights and Informed Consent
Exemption was granted from the Institutional Review Board at Stanford University, where the surgery was performed.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Footnotes
Level of Evidence: Level IV
Electronic supplementary material
The online version of this article (10.1007/s11420-017-9585-1) contains supplementary material, which is available to authorized users.
References
- 1.Ali K, Leland JM. Hamstring strains and tears in the athlete. Clin Sports Med. 2012;31:263–272. doi: 10.1016/j.csm.2011.11.001. [DOI] [PubMed] [Google Scholar]
- 2.Cohen SB, Towers JD, Zoga A, Irrgang JJ, Makda J, Deluca PF, Bradley JP. Hamstring injuries in professional football players: magnetic resonance imaging correlation with return to play. Sports Health. 2011;3:423–30. doi: 10.1177/1941738111403107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Comin J, Malliaras P, Baquie P, Barbour T, Connell D. Return to competitive play after hamstring injuries involving disruption of the central tendon. Am J Sports Med. 2013;41:111–5. doi: 10.1177/0363546512463679. [DOI] [PubMed] [Google Scholar]
- 4.Cooper DE, Conway JE. Distal semitendinosus ruptures in elite-level athletes: low success rates of nonoperative treatment. Am J Sports Med. 2010;38:1174–1178. doi: 10.1177/0363546509361016. [DOI] [PubMed] [Google Scholar]
- 5.Elliott MCCW, Zarins B, Powell JW, Kenyon CD. Hamstring muscle strains in professional football players: a 10-year review. Am J Sports Med. 2011;39:843–850. doi: 10.1177/0363546510394647. [DOI] [PubMed] [Google Scholar]
- 6.Feeley BT, Kennelly S, Barnes RP, Muller MS, Kelly BT, Rodeo SA, Warren RF. Epidemiology of National Football League training camp injuries from 1998 to 2007. Am J Sports Med. 2008;36:1597–1603. doi: 10.1177/0363546508316021. [DOI] [PubMed] [Google Scholar]
- 7.Lempainen L, Sarimo J, Mattila K, Heikkilä J, Orava S, Puddu G. Distal tears of the hamstring muscles: review of the literature and our results of surgical treatment. Br J Sports Med. 2007;41:80–83. doi: 10.1136/bjsm.2006.031211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Maniar N, Shield AJ, Williams MD, Timmins RG, Opar DA. Hamstring strength and flexibility after hamstring strain injury: a systematic review and meta-analysis. Br J Sports. 2016. doi:10.1136/bjsports-2015-095311. [DOI] [PubMed]
- 9.Sanders B, Rolf R, McClelland W, Xerogeanes J. Prevalence of saphenous nerve injury after autogenous hamstring harvest: an anatomic and clinical study of sartorial branch injury. Arthroscopy. 2007;23:956–963. doi: 10.1016/j.arthro.2007.03.099. [DOI] [PubMed] [Google Scholar]
- 10.Schilders E, Bismil Q, Sidhom S, Robinson P, Barwick T, Talbot C. Partial rupture of the distal semitendinosus tendon treated by tenotomy: a previously undescribed entity. Knee. 2006;13:45–47. doi: 10.1016/j.knee.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 11.Schulthies SS, Ricard MD, Alexander KJ, Myrer JW. An electromyographic investigation of 4 elastic-tubing closed kinetic chain exercises after anterior cruciate ligament reconstruction. J Athl Train. 1998;33:328–335. [PMC free article] [PubMed] [Google Scholar]
- 12.Shankar PR, Fields SK, Collins CL, Dick RW, Comstock RD. Epidemiology of high school and collegiate football injuries in the United States, 2005–2006. Am J Sports Med. 2007;35:1295–1303. doi: 10.1177/0363546507299745. [DOI] [PubMed] [Google Scholar]
- 13.Sonnery-Cottet B, Daggett M, Gardon R, Pupim B, Clechet J, Thaunat M. Surgical management of recurrent musculotendinous hamstring injury in professional athletes. Orthop J Sport Med. 2015;3:2325967115606393. doi: 10.1177/2325967115606393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Verrall GM, Slavotinek JP, Barnes PG, Fon GT. Diagnostic and prognostic value of clinical findings in 83 athletes with posterior thigh injury. Am J Sports Med. 2003;31:969–973. doi: 10.1177/03635465030310063701. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)