Introduction
Sporotrichosis is an infection caused by fungi of the Sporothrix complex, a very common plant saprophytes found in tropical and subtropical regions. Classically, transmission occurs after inoculation into the dermis or subcutaneous tissue through minor trauma during plant handling.1, 2 In Rio de Janeiro, most sporotrichosis cases are transmitted by infected cats.3 Most cases present with cutaneous lesions.2 Extracutaneous forms are uncommon.
This case report illustrates a rare presentation of the disease: primary conjunctival sporotrichosis transmitted by a cat, without presence of trauma, occurring exclusively in the bulbar conjunctiva.
Case report
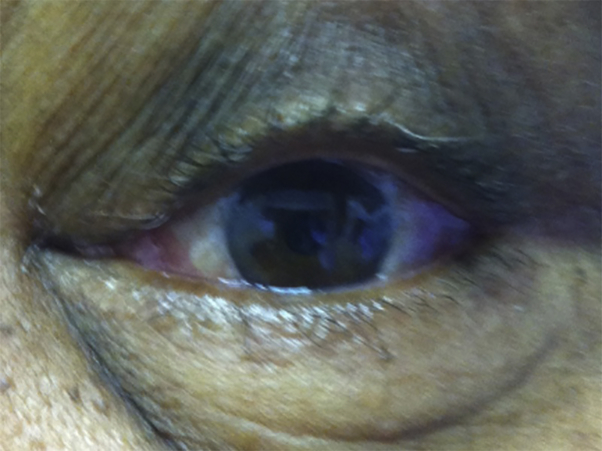
A 78-year-old woman was admitted to the hospital with edema, erythema, pain, and heat sensation in the left periorbital region with onset 15 days before admission. It evolved with pruritus, tearing, yellowish exudation, and reduction of visual acuity. The patient reported contact with a cat at home and denied local trauma, fever, or other symptoms. The patient had psoriasis, obesity, tabagism, hypertension, diabetes mellitus, mild cardiac insufficiency, and chronic renal disease. At admission, the patient presented with periorbital edema in the left eye (Figs 1 and 2), with intense reddish infiltration distributed throughout the entire bulbar conjunctiva but without infiltration of the palpebral conjunctiva. There were no palpable lymph nodes. Laboratory analyses at admission found hyperglycemia (glucose, 329 mg/dL); anemia (hemoglobin, 12.8 g/dL; hematocrit, 37.8%); leucocyte count of 6,300/mm³; platelet count of 225,000/mm³; and altered renal function (urea, 59 mg/dL; creatinine, 1.5 mg/dL; sodium, 131 mEq/L; potassium, 4 mEq/L). A skull magnetic resonance image showed infiltration of soft tissues of the left periorbital region and conjunctiva of the affected eye (Fig 3). Biopsies of the eyelid and bulbar conjunctiva were carried out with the material forwarded to histopathologic examination and culture. Histopathology of the conjunctiva tissue showed granuloma formation (Fig 4). After 4 days of culture, Sporothrix spp. growth occurred, restricted to the material of the conjunctiva. Oral treatment with 100 mg/d of itraconazole was initiated. After a month of treatment, major improvement was observed (Fig 5). A short time later, the patient died of acute myocardial infarction unrelated to the original presentation.
Fig 1.
Primary conjunctival sporotrichosis. Clinical presentation at admission: periorbital edema at left with infiltration of the bulbar conjunctiva.
Fig 2.
Primary conjunctival sporotrichosis. Clinical aspect at admission. Infiltration of the bulbar conjunctiva in detail.
Fig 3.
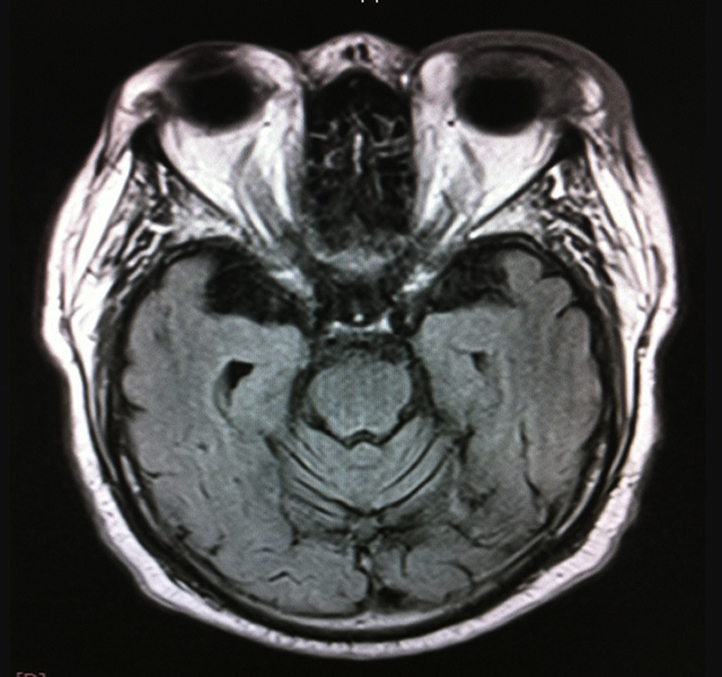
Skull magnetic resonance imaging. Infiltration of soft tissues of the left periorbital region and absence of intraocular lesions.
Fig 4.
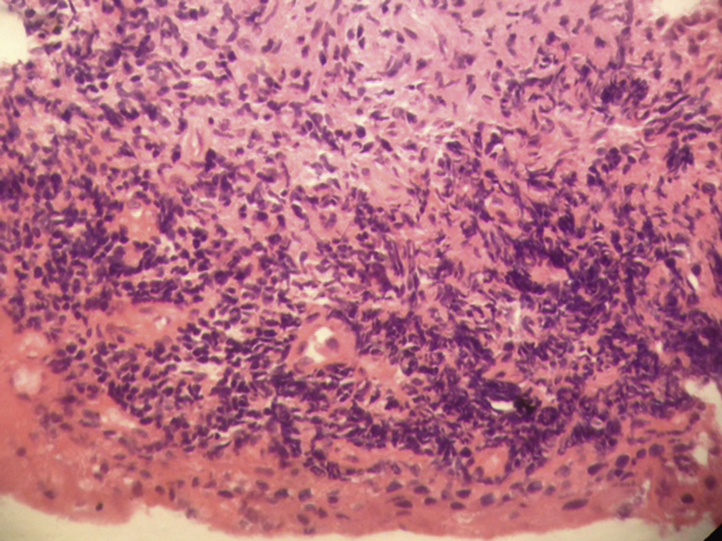
Histopathology of the bulbar conjunctival tissue shows granuloma formation. (Hematoxylin-eosin stain; original magnification: ×40.)
Fig 5.
Clinical aspect after 1 month of treatment. Improvement of the bulbar conjunctiva in detail.
Discussion
The lymphocutaneous form of sporotrichosis is the most common presentation of the disease, representing about 80% of cases. The extracutaneous form has been associated with immunosuppression.2, 4 Involvement of mucosa is uncommon but can be part of a disseminated presentation of the disease.2, 4 Ocular mucosa involvement presents commonly as Parinaud syndrome, an unilateral granulomatous conjunctivitis, with submandibular or preauricular lymphadenopathy. Atypical forms, as in this case without lymphadenopathy, have been described.5 In the scarce reported cases of primary conjunctival sporotrichosis, the palpebral conjunctiva is the most frequently affected area, and bulbar conjunctiva involvement, a very rare form, is described in only 2 cases in literature.6, 7 Involvement of the ocular conjunctiva is usually caused by local trauma, despite some few reported cases without.5, 6 Some hypotheses suggest primary inoculation, beginning from simple contact of the fungus with the mucosa, whereas others suggest inhalation of the agent with posterior hematogenic dissemination.2, 6 This case, with exuberant conjunctiva involvement, without other systemic signs, suggests transmission through primary fungus inoculation. Additionally, location in the bulbar conjunctiva, a region of difficult access for an animal to lick or for contact with infected feline lesions, may imply inoculation of the fungus through the patient's hands, without trauma, as in the case described by Hampton et al.8
Ocular sporotrichosis may be misdiagnosed because of its similarity to other conjunctivitis, which can result in a delay in the initiation of adequate therapy and in an increased risk of complications. Recently, 2 cases of symblepharon and conjunctival fibrosis were designated as sequelae of ocular sporotrichosis.9
The final diagnosis of the disease is carried out by the isolation of the fungus in culture.1, 2 Histopathologic examination may show pyogenic process and granulomas, and in some cases the fungus can be identified in the tissue.
The current epidemics in Rio de Janeiro have revealed an increase in atypical forms of the disease.7 Ocular sporotrichosis has been reported more recently in the city of Rio de Janeiro, affecting healthy individuals with age varying from 14 to 68 years.5, 6, 9
Almeida-Paes et al4 showed, through genotyping, that the Sporothrix brasiliensis is more associated with atypical forms of the disease when compared with Sporothrix schenckii.4 In this case, the species of the agent was not identified.
Itraconazole is the therapy of choice, providing good response in both lymphocutaneous and extra cutaneous forms. Potassium iodine can be used with good results but with frequent gastrointestinal side effects and possible repercussions in the thyroid function.10
Footnotes
Funding sources: None.
Conflicts of interest: None disclosed.
References
- 1.Ramos-e-Silva M., Vasconcelos C., Carneiro S., Cestari T. Sporotrichosis. Clin Dermatol. 2007;25:181–187. doi: 10.1016/j.clindermatol.2006.05.006. [DOI] [PubMed] [Google Scholar]
- 2.Barros M.B., de Almeida Paes R., Schubach A.O. Sporothrix schenckii and sporotrichosis. Clin Microbiol Rev. 2011;24(4):633–654. doi: 10.1128/CMR.00007-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Silva M.B., Costa M.M., Torres C.C. Urban sporotrichosis: a neglected epidemic in Rio de Janeiro, Brazil. Cad Saúde Pública. 2012;28(10):1867–1880. doi: 10.1590/s0102-311x2012001000006. [DOI] [PubMed] [Google Scholar]
- 4.Almeida-Paes R., de Oliveira M.M., Freitas D.F., do Valle A.C., Zancope-Oliveira R.M., Gutierrez-Galhardo M.C. Sporotrichosis in Rio de Janeiro, Brazil: Sporothrix brasiliensis is associated with atypical clinical presentations. PLoS Negl Trop Dis. 2014;8(9):e3094. doi: 10.1371/journal.pntd.0003094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ribeiro A.S., Bisol T., Menezes M.S. Parinaud's oculoglandular syndrome caused by Sporotrichosis. Rev Bras Oftalmol. 2010;69(5):317–322. [Google Scholar]
- 6.Schubach A.O., de Lima Barros M.B., Schubach T.M. Primary conjunctival sporotrichosis: two cases from a zoonotic epidemic in Rio de Janeiro, Brazil. Cornea. 2005;24(4):491–493. doi: 10.1097/01.ico.0000151504.26695.3e. [DOI] [PubMed] [Google Scholar]
- 7.Kashima T., Honma R., Kishi S., Hirato J. Bulbar conjunctival sporotrichosis presenting as a salmon-pink tumor. Cornea. 2010;29:573–576. doi: 10.1097/ICO.0b013e3181ba7039. [DOI] [PubMed] [Google Scholar]
- 8.Hampton D.E., Adesina A., Chodosh J. Conjunctival sporotrichosis in the absence of antecedent trauma. Cornea. 2002;21(8):831–833. doi: 10.1097/00003226-200211000-00021. [DOI] [PubMed] [Google Scholar]
- 9.Yamagata J.P., Rudolph F.B., Nobre M.C. Ocular sporotrichosis: A frequently misdiagnosed cause of granulomatous conjunctivitis in epidemic areas. Am J Ophthalmol Case Rep. 2017;8:35–38. doi: 10.1016/j.ajoc.2017.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kauffman C.A., Bustamante B., Chapman S.W., Pappas P.G. Clinical practice guidelines for the management of sporotrichosis: 2007 update by the Infectious Diseases Society of America. Clin Infect Dis. 2007;45(10):1255–1265. doi: 10.1086/522765. [DOI] [PubMed] [Google Scholar]