Abstract
It is well known that depression is associated with asthma symptoms. We assessed the combined effects of genetic factors and depression on asthma symptom severity using Bayesian network (BN) analysis. The common 100 top-ranked single-nucleotide polymorphisms (SNPs) were obtained from two genome-wide association studies of symptom severity in two childhood asthmatics trials (CAMP (Childhood Asthma Management Program) and CARE (Childhood Asthma Research and Education)). Using SNPs plus five discretized variables (depression, anxiety, age, sex, and race), we performed BN analysis in 529 CAMP subjects. We identified two nodes (depression and rs4672619 mapping to ERBB4 (Erb-B2 receptor tyrosine kinase 4)) that were within the Markov neighborhood of the symptom node in the network and then evaluated the interactive effects of depressive status and rs4672619 genotypes on asthma symptom severity. In childhood asthmatics with homozygous reference alleles, severe depression was related to less severe symptoms. However, in childhood asthmatics with heterozygous alleles and homozygous variant alleles, depression and symptom severity showed a positive correlation (interaction permutation P value = 0.019). We then tried to evaluate whether the interactive effects that we found were sustained in another independent cohort of elderly asthmatics. Contrary to the findings from childhood asthmatics, elderly asthmatics with homozygous reference alleles showed a positive correlation between depression and symptom severity, and elderly asthmatics with heterozygous alleles and homozygous variant alleles showed a negative correlation (interaction permutation P value = 0.003). In conclusion, we have identified a novel SNP, rs4672619, that shows interactive effects with depression on asthma symptom severity in childhood and elderly asthmatics in opposite directions.
Subject terms: Genetics, Asthma
Asthma: How genetic factors and depression affect symptom severity
A novel mutation affects how depression influences the severity of asthma symptoms, with opposite effects in children and the elderly. Depression is known to affect the severity of symptoms experienced by patients with chronic disorders, such as asthma. Heung-Woo Park at Seoul National University College of Medicine in South Korea and coworkers investigated how genetic factors might influence the interaction between depression and asthma. Using previously collected genetic data, the researchers identified a mutation linked with both asthma and depression. In children with the mutation, depression was linked to severe asthma symptoms; children with depression but without the mutation experienced milder symptoms. The researchers observed the opposite relationship in a group of elderly patients with asthma. They conclude that further study of this mutation could illuminate ways to improve asthma management strategies.
Introduction
A depressive disorder may influence the symptoms present in the course of a chronic illness. For example, the presence of depression was shown to be a stronger predictor of reporting diabetes symptoms than hemoglobin A1C level and was more highly associated with chest pain than objective measures of coronary artery disease severity1,2. Asthma is not an exception. Epidemiologic associations between depression and asthma symptoms have been recognized anecdotally for many years3–5. Dysregulation in key biologic systems, such as inflammation6, neuroendocrine dysregulation7, autonomic imbalance causing cholinergic activation8, and genetics dysregulation9, have been suggested as explanations of this co-occurrence.
A Bayesian network (BN) is a multivariate model of dependency among several variables, and the strength of the relationship between variables is represented by conditional probability distributions associated with each node10,11. BNs have been applied in a variety of settings for the purposes of probabilistic prediction, including predictions of asthma exacerbations and control12,13 and responses to short-acting bronchodilator and inhaled corticosteroids14,15. Given that depression is associated with asthma symptoms, we hypothesized that combining information from multiple SNPs, demographic factors, depression, and anxiety can yield models predictive of symptoms. Using BNs, we developed a predictive model and identified one candidate single-nucleotide polymorphism (SNP), rs4672619, that showed possible combined effects with depression upon asthma symptoms. Rs4672619 is located on the intron of the Erb-B2 receptor tyrosine kinase 4 (ERBB4) gene and showed interactive effects with depression on asthma symptom severity in children from the Childhood Asthma Management Program (CAMP) trial16. We confirmed that interactions between depression and rs4672619 in predicting asthma symptom severity were also noted in an independent cohort of elderly asthmatics, although the interactions were in the opposite direction.
Materials and methods
Each study was approved by the Institutional Review Board of the corresponding institution and informed consent was obtained from all study participants. Detailed methods are described in the supplementary material.
Identifying SNPs associated with asthma symptoms
To obtain reliable SNPs associated with asthma symptoms, we used the results of two genome-wide association study (GWAS) performed in the non-Hispanic white children with asthma enrolled in the CAMP trial (n = 438) and in the Childhood Asthma Research and Education (CARE) trials (n = 457). At baseline, all participants were asked to rate and score their asthma symptoms during the past 24 h on a diary card. Similar questions were used in both trials, and the symptom scores ranged from 0 (absent) to 3 (severe) in all trials16–18. Detailed methods of genome-wide SNP genotyping have been described elsewhere for CAMP19,20 and CARE21. A common set of SNP genotypes was obtained by imputation in each cohort using MaCH (version 1.0)22 and the 1000 Genomes Project EUR reference-phased haplotypes based on Phase 1 low coverage data (20101123 release). SNPs with minor allele frequency <1%, a Hardy–Weinberg equilibrium P < 0.001, and/or an imputation quality score <0.3 were excluded, resulting in a set of ~37 million variants per cohort. These data and quality control have been described previously23. The association of SNPs with asthma symptom scores at baseline was measured with a linear regression model as implemented in PLINK24 using additive genetic models. The regression models were adjusted for age and sex. From results of two GWAS, common SNPs with P values <0.05 showing same directionality were obtained. As information on depression and anxiety was available only in the CAMP trial, BN analysis was performed in the CAMP cohort. Among common SNPs, the 100 top-ranked SNPs based on P values of CAMP were forwarded to BN analysis.
BN analysis
We view the BN as primarily a hypothesis-generating step in the analysis. In the CAMP trial, measures of depression and anxiety status were collected at baseline and annually thereafter using the Children’s Depression Inventory25 and the Revised Children’s Manifest Anxiety26. Higher scores on each of these measures reflect increased problems. For better modeling, we drew 91 subjects with other ethnicities from the CAMP trial in addition to the 438 non-Hispanic white subjects, and resultantly, a total of 529 subjects who had a complete phenotype data set (symptom, depression, and anxiety scores) and genotype data were used for BN analysis. The baseline characteristics are presented in Table 1. We used the open-source software package bnlearn27 in the statistical and graphical environment R (http://www.r-project.org) for BN analysis. In BN analysis, we included 105 variables: 100 SNPs (homozygous minor alleles and heterozygous and homozygous major alleles); depression score (quartile 1–4); anxiety score (quartile 1–4); age (quartile 1–4); sex (male and female); and race (non-Hispanic white, African American, any Hispanic, and Asian). Prior distributions used were bnlearn defaults, and we learned a BN structure using bnlearn’s hill-climbing algorithm (a greedy optimizer for the Bayesian posterior probability of the data). Measuring the degree of confidence in a particular graphical feature is a key problem in inferring the network structure28. We quantified such a degree of confidence by generating 1000 network structures based on nonparametric bootstrap to the data and by estimating the relative frequency of the feature of interest28. Then, we removed undirected arcs and arcs with strength <0.1 from the BN inferred. A previous report showed that removing the arcs with strength <0.1 had a minimal effect on its classification accuracy29. According to the Markov blanket property of the BN, only the parents (nodes connected above), children (nodes connected below), and the other parents of those children are required to predict the behavior of a node30. We therefore selected the two nodes (depression and rs4672619) that were within the Markov blanket of the symptom node in BN and then performed interaction analysis. To calculate an adjusted P value, permutation tests for a linear model as implemented in the “lmPerm” R package31 was done.
Table 1.
Characteristics of childhood and elderly asthmatics
| Childhood asthmatics, N = 26 | Elderly asthmatics, N = 96 | |
|---|---|---|
| Age (years), median (IQR) | 8.8 (7.2–10.6) | 72.5 (70–77) |
| Male gender, number (%) | 332 (62.7) | 38 (39.6) |
| Symptom score, median (IQR) | 0.57 (0.14–1.00)a | 8 (6–10)b |
| Race, number (%) | ||
| Non-Hispanic white/African American/Hispanic/Asian | 389 (73.6)/58 (10.9)/40 (7.6)/42 (7.9) | 0 (0)/0 (0)/0 (0)/96 (100) |
| Cognitive function (score), median (IQR) | NA | 27 (24–29)c |
| Anxiety (score), median (IQR) | 10 (6–15) | NA |
| Depression (score), median (IQR) | 5 (2–10) | 19.5 (16–22) |
IQR interquartile range, NA not applicable
aRange 0–3
bRange 0–25
cRange, 0–30 (any score ≥24 points indicates normal cognition)
Evaluating the interactive effects in another cohort
We evaluated whether the interactive effects of depression status and rs4672619 genotypes on asthma symptom severity observed in the cohort of childhood asthmatics were sustained in another independent cohort. As no childhood cohort with both depression and genotype data was readily available, our evaluation was done in elderly asthmatics aged 65 years or older from a prospective, observational, and multi-centered cohort in Korea with the purpose of studying the natural history of asthma among elderly people32. The baseline characteristics are presented in Table 1. Symptom scores were measured using five questionnaires (range, 0–25; a higher score represents a more severe symptom), and depression status was assessed by the Korean version of the Geriatric Depression Scale Short Form (range, 0–30; a higher score represented more severe depression). Cognitive function was assessed using the Korean version of the Mini-Mental State Examination (range, 0–30; any score ≥27 points indicates a normal cognition). Details for symptom questionnaires are described in the online supplement. rs4672619 was genotyped, and the interactive effects between genotype and depression status on asthma symptom severity were evaluated.
Results
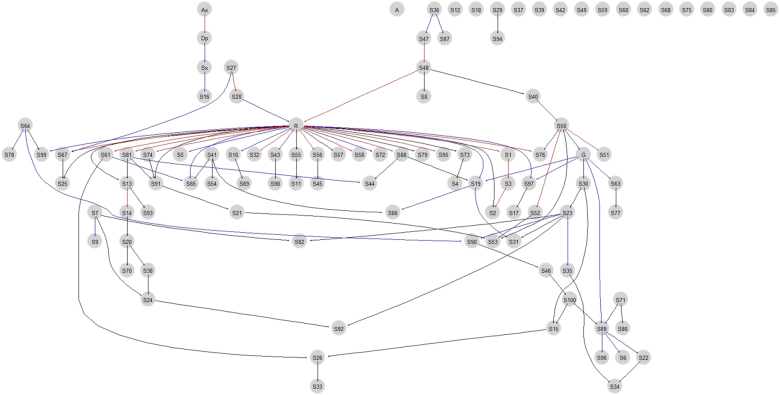
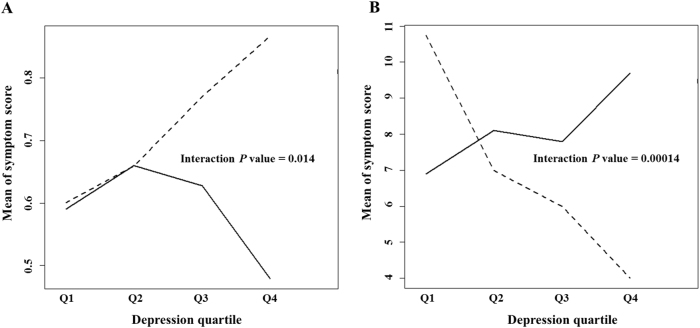
The lowest P value for GWAS analysis was 1.66 × 10−6 (rs2141189) in the CAMP trial and 1.52 × 10−6 (rs1429146) in the CARE trial. There were 413 common SNPs with P values <0.05 with the same directionality. Of these SNPs, the 100 top-ranked SNPs based on the CAMP P values (Supplementary Table 1) were selected and forwarded for BN analysis. Figure 1 shows the BN learned from the data of childhood asthmatics. We found two nodes directly attached to the asthma symptom (Sx node in Fig. 1): depression (Dp node in Fig. 1) and rs4672619 (S16 node in Fig. 1). The arc strengths between the Sx and Dp nodes and between the Sx and S16 nodes were 0.329 and 0.207, respectively. We then evaluated the interactive effects of depression severity and rs4672619 genotypes on asthma symptom severity in all CAMP subjects. As shown in Fig. 2a, in childhood asthmatics with homozygous reference alleles (frequency = 86.8%), severe depression was related to less severe asthma symptoms. However, in childhood asthmatics with heterozygous or homozygous variant alleles, depression and asthma symptom severity showed a positive correlation. The P values of the main effects were 0.009 for rs4672619 and 0.322 for depression, and the P value of the interaction was 0.014 (permutation P value = 0.019). rs4672619 was genotyped in 96 Korean elderly asthmatics, and we also found that the directions of correlations between depression status and asthma symptom severity differed according to rs4672619 genotypes (Fig. 2b). However, the direction of correlation was opposite to that of childhood asthmatics (Fig. 2). That is, elderly asthmatics with homozygous reference alleles (frequency = 92.4%) showed a positive correlation between depression and symptom severity. The P values of the main effects were 0.177 for rs4672619 and 0.125 for depression, and the P value of the interaction was 0.00014 (permutation P value = 0.003).
Fig. 1. Bayesian network inferred.
A Bayesian network learned from the data of childhood asthmatics with a Hill-Climbing algorithm. Edges represent conditional dependencies, and connected nodes represent variables that are conditionally dependent on each other. Red edges represent edges with an arc strength >0.5, blue edges represent edges with an arc strength between 0.2 and 0.5, and black edges represent edges with an arc strength between 0.1 and 0.2. Edges with an arc strength <0.1 were removed from the network. For a certain node, nodes connected above (parent nodes), nodes connected below (children nodes), and the other parent nodes of these children nodes form a Markov blanket, which is required to predict the behavior of that node. Thus, we evaluated the interactive effects of depression severity (parent of the Sx node) and rs4672619 (S16) genotypes (children of the Sx node) on asthma symptom severity (Sx node). A age quartile, Ax anxiety quartile, Dp depression quartile, G gender (male/female), Sx symptom severity quartile, R ethnicity (non-Hispanic white/African American/Hispanic/Asian), and S1-100 top-ranked 100 SNPs (S16, rs4672619)
Fig. 2. Interactive effects of rs4672619 genotypes and depression severity on asthma symptom severity in cohorts of childhood and elderly asthmatics.
a Childhood asthmatics. b Elderly asthmatics. Solid lines represent subjects with reference homozygous alleles of rs4672619, and dotted lines represent subjects with heterozygous or homozygous variant alleles of rs4672619. Q1 represents mild depression, and Q4 represents severe depression. The severity of asthma symptoms increases as symptom score increases
Discussion
Precise symptom perception would be an important component of asthma management, allowing asthmatics to use rescue medicine or seek medical help in a timely manner33. However, there may be a discrepancy between asthma symptom perception and lung function34. Therefore, asthma symptoms are a unique domain that should be evaluated for the proper management of asthma35. β2 Adrenergic receptor gene methylation was reported to be associated with decreased asthma severity in inner-city schoolchildren36, and genetic components are known to be involved in asthma symptom responses to medications37,38. In addition, a recent report showed that psychosocial factors, such as harsh parent–child conflict39 or targeted rejection40, caused severe symptoms in children with asthma by decreasing anti-inflammatory gene expression. These findings motivated us to assess the interactive effects of multiple SNPs mapped to multiple genes and depression severity on asthma symptoms. Using BNs to guide our investigation, we found that rs4672619 was directly attached to the symptom node. Further analysis has shown that rs4672619 genotypes showed significant interactive effects with depression severity on symptom severity in both childhood and elderly asthmatics.
rs4672619 is on an intron of the ERBB4 gene. ERBB4, along with its ligand neuregulin-1, is known to contribute to the pathophysiology of schizophrenia and bipolar disorders41,42. A recent Bayesian modeling approach identified several variants in ERBB4 with strong evidence for associations with childhood asthma43. Recent increases in the understanding of dyspnea, one of the important asthma symptoms, suggest that there may be interactions between biopsychological factors and dyspnea perception44. ERBB4 regulates a thalamic reticular nucleus to cortical inputs at levels that can support sensory selection while allowing behavioral flexibility45. In addition, crosstalk between the ErbB network and steroid hormone signaling pathway has been well known46 and severe, steroid-dependent asthmatics had depression more often than non-steroid-dependent asthmatics47. Taken together, rs4672619 is possibly involved in interactions between depression and asthma symptom severity by modulating symptom perception and steroid action.
One of the interesting findings of this study was that the direction of interactive effects of rs4672619 genotypes with depression severity on asthma symptoms was opposite between our childhood and elderly cohorts. The childhood asthmatics carrying two reference alleles showed significantly negative correlations between depression and symptoms scores, whereas elderly asthmatics with these alleles showed significantly positive correlations. Cognitive dysfunction, which is frequently encountered in elderly asthmatics48, might affect asthma symptom presentation. However, we found that the Mini-Mental State Examination scores of all elderly asthmatics were greater than 24 (Table 1), which suggested that they were cognitively competent49. Many investigators have agreed that elderly asthma differs considerably from non-elderly asthma and that aging lungs50, physiologic changes51, and immunosenescence52 are possible contributing factors. Likewise, the different interactive effects of rs4672619 genotypes and depression severity on asthma symptom severity between childhood and elderly asthmatics might come from the factors mentioned above. It is also possible that asthma symptom perception may be influenced by age, and a specific genetic mechanism regulating childhood asthma symptom severity may not carry over to old age. To date, no study has evaluated differences in the perception of asthma symptoms in childhood and elderly asthmatics. However, for childhood asthmatics, it was reported that adolescents (13–18 years) were more accurate in perceiving symptoms than school-age children (6–12 years)31 and that the accuracy for perceiving symptoms increased with age in children aged 7 to 17 years53. In our previous study, we found that genetic mechanisms underlying the symptomatic response to inhaled corticosteroids might be different between childhood and adult asthmatics36. Interestingly, recent reports showed that some genetic variations in ERBB4 showed age-by-genotype interactions on cortical brain morphology in a cohort of 3–20 year olds54, and age-dependent differences in ERBB4 expression were found in the brains of autistic patients55. These findings suggest that the genetic effects of ERBB4 may be different between childhood and elderly asthmatics, although we do not know whether the same differences exist in the lung.
Another plausible explanation is that the different interactive effects are due to ethnicity differences. Childhood asthmatics in this study were predominantly non-Hispanic white patients, and whereas elderly asthmatics were only Asian patients. Allele reversal at shared risk loci, the so-called flip-flop phenomenon, can be attributed to differences in the underlying genomic architectures at these loci according to ethnicity differences56. For example, a previous report showed that variants of ENND1B were associated with asthma in children, but the association in the African Americans was linked to the opposite allele of that associated with asthma in subjects of European ancestry57. Very little is known about ethnicity–gene interactions for ERBB4. Only one small-scale study conducted in non-Hispanic white and African-American schizophrenia patients reported that disease-associated SNPs on ERBB4 showed no ethnicity–genotype effects on ERBB4 splice-variant expression levels in the brain 58.
There are a few potential limitations in generalizing our findings. Inevitably, the main effect and interaction effect are often correlated. It is possible that the significant effect of rs4672619 genotypes might have affected the interactive effect of depression severity and rs4672619 genotypes on asthma symptom severity in childhood asthmatics. Next, we could not replicate our results in another pertinent cohort of childhood asthmatics. The opposite directions of the correlations in childhood and elderly asthmatics was interesting. However, we cannot completely exclude the possibility that our results may be due to chance alone (false-positive associations). In addition, further mechanistic studies are needed to confirm the age-specific or ethnicity-specific effects of rs4672619 on the ERBB4 gene. An incorporation of prior biological knowledge would help us overcome the reconstruction accuracy due to the complex nature of the network and the noise inherent in the data.
In conclusion, we have identified rs4672619, which showed significant interactive effects with depression severity on asthma symptom severity in both childhood and elderly asthmatics in opposite directions. This study is the first to show significant interactions between genetic factors and depression severity for asthma symptom severity. Our findings suggest that different strategies to decrease asthma symptom severity may be needed in these distinct age subsets of asthmatics.
Electronic supplementary material
Acknowledgements
This work was supported by the National Institutes of Health, US (R01 NR013391, R01 HL127332, and U01 HL065899) to K.G.T., by the Ministry of Health and Welfare, Republic of Korea (2008-E33028-00, 2009-E33022-00, and 2011-E33005-00) to H.-W.P., and by the Parker B. Francis Foundation to M.J.M.
Authors' contributions
H.-W.P. and K.G.T.: Conception and design of the study, data generation, analysis, interpretation, and preparation of the manuscript. W.-J.S. and S.-H.C.: Data generation and critical revision of the manuscript. M.J.M.: Data generation, analysis, interpretation, and preparation of the manuscript. F.M., D.M., and B.G.B.: Data generation, analysis, interpretation, and critical revision of the manuscript.
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Supplementary information accompanies this paper at 10.1038/s12276-018-0110-5.
References
- 1.Ludman EJ, et al. Depression and diabetes symptom burden. Gen. Hosp. Psychiatry. 2004;26:430–436. doi: 10.1016/j.genhosppsych.2004.08.010. [DOI] [PubMed] [Google Scholar]
- 2.Ruo B, et al. Depressive symptoms and health-related quality of life: the Heart and Soul Study. JAMA. 2003;290:215–221. doi: 10.1001/jama.290.2.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Janson C, Bjornsson E, Hetta J, Boman G. Anxiety and depression in relation to respiratory symptoms and asthma. Am. J. Respir. Crit. Care Med. 1994;149:930–934. doi: 10.1164/ajrccm.149.4.8143058. [DOI] [PubMed] [Google Scholar]
- 4.Rimington LD, Davies DH, Lowe D, Pearson MG. Relationship between anxiety, depression, and morbidity in adult asthma patients. Thorax. 2001;56:266–271. doi: 10.1136/thorax.56.4.266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Goldney RD, Ruffin R, Fisher LJ, Wilson DH. Asthma symptoms associated with depression and lower quality of life: a population survey. Med. J. Aust. 2003;178:437–441. doi: 10.5694/j.1326-5377.2003.tb05408.x. [DOI] [PubMed] [Google Scholar]
- 6.Shanahan L, Copeland WE, Worthman CM, Angold A, Costello EJ. Children with both asthma and depression are at risk for heightened inflammation. J. Pediatr. 2013;163:1443–1447. doi: 10.1016/j.jpeds.2013.06.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Van Lieshout RJ, Bienenstock J, MacQueen GM. A review of candidate pathways underlying the association between asthma and major depressive disorder. Psychosom. Med. 2009;71:187–195. doi: 10.1097/PSY.0b013e3181907012. [DOI] [PubMed] [Google Scholar]
- 8.Miller BD, Wood BL. Influence of specific emotional states on autonomic reactivity and pulmonary function in asthmatic children. J. Am. Acad. Child Adolesc. Psychiatry. 1997;36:669–677. doi: 10.1097/00004583-199705000-00018. [DOI] [PubMed] [Google Scholar]
- 9.Wamboldt MZ, Hewitt JK, Schmitz S. Familial association between allergic disorders and depression in adult Finnish twins. Am. J. Med. Genet. 2000;96:146–153. doi: 10.1002/(sici)1096-8628(20000403)96:2<146::aid-ajmg4>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 10.Shoemaker JS, Painter IS, Weir BS. Bayesian statistics in genetics: a guide for the uninitiated. Trends Genet. 1999;15:354–358. doi: 10.1016/s0168-9525(99)01751-5. [DOI] [PubMed] [Google Scholar]
- 11.Beaumont MA, Rannala B. The Bayesian revolution in genetics. Nat. Rev. Genet. 2004;5:251–261. doi: 10.1038/nrg1318. [DOI] [PubMed] [Google Scholar]
- 12.Farion KJ, Wilk S, Michalowski W, O’Sullivan D, Sayyad-Shirabad J. Comparing predictions made by a prediction model, clinical score, and physicians: pediatric asthma exacerbations in the emergency department. Appl. Clin. Inform. 2013;4:376–391. doi: 10.4338/ACI-2013-04-RA-0029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McGeachie MJ, et al. The metabolomics of asthma control: a promising link between genetics and disease. Immun. Inflamm. Dis. 2015;3:224–238. doi: 10.1002/iid3.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Himes BE, et al. Predicting response to short-acting bronchodilator medication using Bayesian networks. Pharmacogenomics. 2009;10:1393–1412. doi: 10.2217/pgs.09.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McGeachie MJ, et al. Predicting inhaled corticosteroid response in asthma with two associated SNPs. Pharm. J. 2013;13:306–311. doi: 10.1038/tpj.2012.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Childhood Asthma Management Program Research Group. The Childhood Asthma Management Program (CAMP): design, rationale, and methods. Control Clin. Trials. 1999;20:91–120. [PubMed] [Google Scholar]
- 17.Szefler SJ, et al. Characterization of within-subject responses to fluticasone and montelukast in childhood asthma. J. Allergy Clin. Immunol. 2005;115:233–242. doi: 10.1016/j.jaci.2004.11.014. [DOI] [PubMed] [Google Scholar]
- 18.Sorkness CA, et al. Long-term comparison of 3 controller regimens for mild-moderate persistent childhood asthma: the Pediatric Asthma Controller trial. J. Allergy Clin. Immunol. 2007;119:64–72. doi: 10.1016/j.jaci.2006.09.042. [DOI] [PubMed] [Google Scholar]
- 19.Murphy A, et al. Mapping of numerous disease-associated expression polymorphisms in primary peripheral blood CD4+ lymphocytes. Hum. Mol. Genet. 2010;19:4745–4757. doi: 10.1093/hmg/ddq392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Himes BE, et al. Genome-wide association analysis identifies PDE4D as an asthma-susceptibility gene. Am. J. Hum. Genet. 2009;84:581–593. doi: 10.1016/j.ajhg.2009.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Torgerson DG, et al. Meta-analysis of genome-wide association studies of asthma in ethnically diverse North American populations. Nat. Genet. 2011;43:887–892. doi: 10.1038/ng.888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Li Y, Willer CJ, Ding J, Scheet P, Abecasis GR. MaCH: using sequence and genotype data to estimate haplotypes and unobserved genotypes. Genet. Epidemiol. 2010;34:816–834. doi: 10.1002/gepi.20533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Croteau-Chonka DC, et al. Expression quantitative trait loci information improves predictive modeling of disease relevance of non-coding genetic variation. PLoS ONE. 2015;10:e0140758. doi: 10.1371/journal.pone.0140758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Purcell S, et al. PLINK: a tool set for whole-genome association and population-based linkage analyses. Am. J. Hum. Genet. 2007;81:559–575. doi: 10.1086/519795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kovacs M. Rating scales to assess depression in school aged children. Acta Paedopsychiatr. 1981;46:305–318. [PubMed] [Google Scholar]
- 26.Reynolds C, Richmond B. Revised Children’s Manifest Anxiety Scale (RCMAS) Los Angeles, CA: Western Psychological Services; 1985. [Google Scholar]
- 27.Scutari M. Learning Bayesian networks with the bnlearn R package. J. Stat. Softw. 2010;35:1–22. [Google Scholar]
- 28.Friedman, N., Goldszmidt, M., Wyner, A. Data analysis with Bayesian networks: a Bootstrap approach. In Proc 15th Conference on Uncertainty in Artificial Intelligence 206–215 (Morgan Kaufmann: San Francisco, CA, 1999).
- 29.Ratnapinda, P. & Druzdzel, M. J. An empirical evaluation of costs and benefits of simplifying Bayesian networks by removing weak arcs. In Proc 27th International Florida Artificial Intelligence Research Society Conference 508–511 (AAAI Press, Palo Alto, CA, 2014).
- 30.Ghosh JK, Delampady M, Samanta T. An Introduction to Bayesian Analysis Theory and Methods. Springer Texts in Statistics. New York, NY: Springer; 2006. [Google Scholar]
- 31.Wheeler B. lmPerm:Permutational tests for linear models. 2010. Available at: http://CRAN.R-project.org/package=lmPerm.
- 32.Park HW, et al. Prediction of asthma exacerbations in elderly adults: results of a 1-year prospective study. J. Am. Geriatr. Soc. 2013;61:1631–1632. doi: 10.1111/jgs.12434. [DOI] [PubMed] [Google Scholar]
- 33.Yoos HL, McMullen A. Symptom perception and evaluation in childhood asthma. Nurs. Res. 1999;48:2–8. doi: 10.1097/00006199-199901000-00002. [DOI] [PubMed] [Google Scholar]
- 34.Park HW, et al. Xenon ventilation computed tomography and the management of asthma in the elderly. Respirology. 2014;19:389–395. doi: 10.1111/resp.12242. [DOI] [PubMed] [Google Scholar]
- 35.The National Asthma Education and Prevention Program (NAEPP). National Asthma Education and Prevention Program Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma 2007. http://www.nhlbi.nih.gov/guidelines/asthma/asthgdln.pdf. Accessed 8 Dec 2016.
- 36.Gaffin JM, et al. β-2 adrenergic receptor gene methylation is associated with decreased asthma severity in inner-city schoolchildren: asthma and rhinitis. Clin. Exp. Allergy. 2014;44:681–689. doi: 10.1111/cea.12219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Park HW, et al. Genetic predictors associated with improvement of asthma symptoms in response to inhaled corticosteroids. J. Allergy Clin. Immunol. 2014;133:664–669. doi: 10.1016/j.jaci.2013.12.1042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mougey EB, et al. Pharmacogenetics of asthma controller treatment. Pharm. J. 2013;13:242–250. doi: 10.1038/tpj.2012.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ehrlich KB, Miller GE, Chen E. Harsh parent–child conflict is associated with decreased anti-inflammatory gene expression and increased symptom severity in children with asthma. Dev. Psychopathol. 2015;27:1547–1554. doi: 10.1017/S0954579415000930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Murphy ML, Slavich GM, Chen E, Miller GE. Targeted rejection predicts decreased anti-inflammatory gene expression and increased symptom severity in youth with asthma. Psychol. Sci. 2015;26:111–121. doi: 10.1177/0956797614556320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Maier W, Zobel A, Wagner M. Schizophrenia and bipolar disorder: differences and overlaps. Curr. Opin. Psychiatry. 2006;19:165–170. doi: 10.1097/01.yco.0000214342.52249.82. [DOI] [PubMed] [Google Scholar]
- 42.Wang N, et al. Downregulation of neuregulin 1-ErbB4 signaling in parvalbumin interneurons in the rat brain may contribute to the antidepressant properties of ketamine. J. Mol. Neurosci. 2014;54:211–218. doi: 10.1007/s12031-014-0277-8. [DOI] [PubMed] [Google Scholar]
- 43.Baurley JW, Conti DV. A scalable, knowledge-based analysis framework for genetic association studies. BMC Bioinform. 2013;14:312. doi: 10.1186/1471-2105-14-312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hayen A, Herigstad M, Pattinson KT. Understanding dyspnea as a complex individual experience. Maturitas. 2013;76:45–50. doi: 10.1016/j.maturitas.2013.06.005. [DOI] [PubMed] [Google Scholar]
- 45.Ahrens S, et al. ErbB4 regulation of a thalamic reticular nucleus circuit for sensory selection. Nat. Neurosci. 2015;18:104–111. doi: 10.1038/nn.3897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yarden Y, Sliwkowski MX. Untangling the ErbB signalling network. Nat. Rev. Mol. Cell. Biol. 2001;2:127–137. doi: 10.1038/35052073. [DOI] [PubMed] [Google Scholar]
- 47.Amelink M, et al. Anxiety, depression and personality traits in severe, prednisone-dependent asthma. Respir. Med. 2014;108:438–444. doi: 10.1016/j.rmed.2013.12.012. [DOI] [PubMed] [Google Scholar]
- 48.Ng TP, Chiam PC, Kua EH. Mental disorders and asthma in the elderly: a population-based study. Int. J. Geriatr. Psychiatry. 2007;22:668–674. doi: 10.1002/gps.1728. [DOI] [PubMed] [Google Scholar]
- 49.Tombaugh TN, McIntyre NJ. The Mini-Mental State Examination: a comprehensive review. J. Am. Geriatr. Soc. 1992;40:922–935. doi: 10.1111/j.1532-5415.1992.tb01992.x. [DOI] [PubMed] [Google Scholar]
- 50.Enright PL, Kronmal RA, Manolio TA, Schenker MB, Hyatt RE. Respiratory muscle strength in the elderly. Am. J. Respir. Crit. Care Med. 1994;149:430–438. doi: 10.1164/ajrccm.149.2.8306041. [DOI] [PubMed] [Google Scholar]
- 51.Knudson RJ, Lebowitz MD, Holberg CJ, Burrows B. Changes in the normal maximal expiratory flow volume curve with growth and aging. Am. Rev. Respir. Dis. 1983;127:725–734. doi: 10.1164/arrd.1983.127.6.725. [DOI] [PubMed] [Google Scholar]
- 52.Agarwal S, Busse PJ. Innate and adaptive immunosenescence. Ann. Allergy Asthma Immunol. 2010;104:183–190. doi: 10.1016/j.anai.2009.11.009. [DOI] [PubMed] [Google Scholar]
- 53.Kopel SJ, et al. Asthma symptom perception and obesity in children. Biol. Psychol. 2010;84:135–141. doi: 10.1016/j.biopsycho.2009.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Douet V, Chang L, Lee K, Ernst T. Pediatric Imaging, Neurocognition, and Genetics (PING) Consortium. ERBB4 polymorphism and family history of psychiatric disorders on age-related cortical changes in healthy children. Brain Imag. Behav. 2015;9:128–140. doi: 10.1007/s11682-015-9363-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chow ML, et al. Age-dependent brain gene expression and copy number anomalies in autism suggest distinct pathological processes at young versus mature ages. PLoS Genet. 2012;8:e1002592. doi: 10.1371/journal.pgen.1002592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lin PI, Vance JM, Pericak-Vance MA, Martin ER. No gene is an island: the flip-flop phenomenon. Am. J. Hum. Genet. 2007;80:531–538. doi: 10.1086/512133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sleiman PM, et al. Variants of DENND1B associated with asthma in children. N. Engl. J. Med. 2010;362:36–44. doi: 10.1056/NEJMoa0901867. [DOI] [PubMed] [Google Scholar]
- 58.Law AJ, Kleinman JE, Weinberger DR, Weickert CS. Disease-associated intronic variants in the ErbB4 gene are related to altered ErbB4 splice-variant expression in the brain in schizophrenia. Hum. Mol. Genet. 2007;16:129–141. doi: 10.1093/hmg/ddl449. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.