Abstract
Background and Objectives
Supervised lifestyle interventions, including dietary and exercise programs, may be infeasible to implement in real-world settings. Therefore, this study aimed to evaluate the effectiveness of a home-based lifestyle modification intervention on blood pressure (BP) management.
Methods
Eighty-five patients aged over 20 years and diagnosed with prehypertension or mild hypertension were randomly assigned to an advice-only comparison group (C group, n=28), a Dietary Approaches to Stop Hypertension (DASH) diet education group (D group, n=30), or a DASH and home-based exercise group (D+Ex group, n=27). The intervention lasted for 8 weeks. The primary outcome was the difference in office systolic blood pressure (SBP) before and after the study period (Trial registry at ClinicalTrials.gov, NCT01637909).
Results
Seventy-two participants (87.8%) completed the trial. The degree of change in office SBP did not significantly differ among the intervention groups; however, the D+Ex group demonstrated a tendency toward decreased SBP. Upon analysis of 24-hour ambulatory BP measurements, daytime ambulatory SBP was significantly lower in the D+Ex group (134 mmHg; 95% confidence interval [CI], 131 to 137; p=0.011) than in the C group (139.5 mmHg; 95% CI, 130.9 to 137), and daytime ambulatory SBP was significantly decreased in the D+Ex group (−5.2 mmHg; 95% CI, −8.3 to −2.1; p=0.011) compared to the C group (0.4 mmHg, 95% CI, −2.5 to 3.3).
Conclusions
In conclusion, lifestyle modification emphasizing both diet and exercise was effective for lowering BP and should be favored over diet-only modifications.
Keywords: Diet, Exercise, Hypertension, Lifestyle, Prehypertension
INTRODUCTION
Lifestyle modification has been proven as an effective treatment modality for hypertension, with major guidelines recommending it prior or concomitant to medical treatment for hypertension.1) Many studies have shown that lifestyle modifications such as dietary change, smoking cessation, and regular physical exercise reduce blood pressure (BP) and prevent hypertension and cardiovascular events.2),3),4) However, previous lifestyle modification studies have shown their effectiveness under the strict supervision of medical professionals. Rarely have studies shown the effectiveness of home-based lifestyle modification for hypertension management in a real-world setting, where performing a supervised diet and exercise treatment program is typically infeasible. In addition, suboptimal adherence is highly prevalent, with less than 10% of adults with hypertension being fully compliant with dietary recommendations and 35% compliant with exercise.5),6),7) Moreover, the effectiveness of dietary change and exercise on BP lowering in the Korean population has not been well defined. The aim of this study was to evaluate how a home-based lifestyle modification intervention without active monitoring, consisting of exercise education and recommendation of the Korean Dietary Approaches to Stop Hypertension (DASH) diet, affects BP in patients with prehypertension or mild hypertension.
METHODS
Study design and procedure
The Korean Lifestyle Modification on Hypertension study was approved by the Institutional Review Board at Yonsei University Health System (approval number: 4-2011-0305) and registered at ClinicalTrials.gov on 8 July 2012 (NCT01637909). The current study was a 3-armed randomized controlled trial. Potential participants were screened for eligibility via medical records review before their arrival at the clinic. At the time of their arrival at the clinic, a physician asked each patient whether they were willing to participate in the study after it has been explained to them. The research nurse explained the study in detail and obtained written informed consent.
Enrollment began in September 2011 and ended in November 2014. Baseline data including medical history, physical examination, and anthropometric data were assessed during 2 screening visits. Eligible participants were randomly assigned to one of the following groups: an advice-only comparison group (“Control,” C group); an intervention group receiving active dietary education from a certified nutritionist (“Diet,” D group); or an intervention group receiving the dietary intervention along with exercise education from an exercise specialist (“Diet and Exercise,” D+Ex group). After randomization, all participants were requested to visit at 1 week, at 4 weeks, and at 8 weeks. Twenty-four-hour ambulatory blood pressure monitoring (ABPM), central hemodynamics measurement, and laboratory analyses were performed at baseline and at the end of the study. Questionnaires regarding physical activity and diet were obtained before intervention at 1, 4, and 8 weeks. The D group received the dietary intervention at the randomization visit at 1 and 4 weeks. The D+Ex group received the exercise intervention at the randomization visit at 1 and at 4 weeks as well as the dietary intervention.
Study participants
All participants were over 20 years old. The inclusion criteria were as follows: 1) the participants who had not taken antihypertensive medication had systolic blood pressure (SBP) of 120−159 mmHg or diastolic blood pressure (DBP) of 80−99 mmHg; 2) the participants who had taken 1 or 2 antihypertensive medications had SBP of 140−159 mmHg or DBP of 90−99 mmHg. Major exclusion criteria were use of 3 or more antihypertensive medications; body mass index (BMI) less than 18.5 kg/m2 or greater than 45 kg/m2; evidence of target organ damage such as left ventricular hypertrophy, angina, heart failure, stroke, chronic kidney disease, peripheral artery disease, or retinopathy; cancer; or regular alcohol consumption exceeding 14 servings per week; pregnant women or women of child-bearing age who tested positive for human chorionic gonadotropin; breastfeeding women; individuals who could not read the consent; and individuals who had participated in another study within 3 months.
Sample size calculation
Initially, we hypothesized that dietary intervention would lower SBP by 11.5 mmHg with a standard deviation of 10 mmHg, and combination of dietary and exercise intervention would decrease SBP by 18 mmHg with a standard deviation of 15 mmHg, considering the additive effect of exercise on BP.8),9) Assuming a statistical power of 80% and dropout rate of 25%, the number of participants needed was determined to be 32 in the C group, 22 in the D group, and 22 in the D+Ex group, with the assumption that there would be more dropouts in the C group. Initially, the randomization was a simple 1:1:1 randomization. However, the interim analysis indicated that the dropout rate in the C group was lower than the initial assumption and there were discrepancies in age and gender. Therefore, the number of participants needed was recalculated to 28 participants in each group and the randomization method was changed to permuted 6 block randomizations.
Intervention
Dietary intervention
The dietary intervention involved active education of the enrolled participants based on the Korean modified DASH diet by a certified nutritionist at randomization visit, at 1 week, and at 4 weeks. Specifically, the participants in the D and D+Ex groups were advised to substitute processed white rice with whole grains such as barley. For protein, the participants were advised to consume chicken and fish instead of red meat. Additionally, consumption of nuts was recommended, whereas processed foods containing high fructose corn syrup were discouraged. We recommended reducing salt intake by advising the participants to abstain from adding table salt to their meals and adding salt during cooking. Participants were advised to abstain from consuming pickles and condiments, which are the main source of excess salt in the Korean population.
Exercise intervention (home-based)
Participants in the D+Ex group were provided with an exercise diary, a pedometer (DMC-03; Shinwoo Electronics Company Ltd., Seoul, Korea) and 2 exercise DVDs. Participants also received 15 minutes of exercise education, as well as instruction in the use of the pedometer and exercise diary at randomization visit at 1 and 4 weeks. The exercise DVDs consisted of 2 different exercise programs containing either 5 (mild intensity) or 7 (moderate intensity) different exercises, primarily core exercise and low-intensity resistance exercise using their own bodyweight or a 500-mL water bottle. Participants were asked to follow the exercise DVD in a circuit training manner (3 circuits of 5 or 7 exercises). Participants were encouraged to walk more than 10,000 steps daily. The number of steps walked as well as circuit exercise performed following the DVD were recorded in the exercise diary. Furthermore, participants were encouraged to participate in aerobic exercises such as hiking, biking, and swimming. The exercise specialist made a weekly phone call to encourage participants to exercise as recommended and also answer any questions raised by participants. At the end of the study, participants returned their exercise diaries to the exercise specialist, who provided further counseling on exercise based on the exercise diary. Participants in the C and D groups were instructed to maintain their usual activities.
Usual advice treatment
Participants in the C group received usual care and advice on lifestyle modification from their physician based on guidelines for the management of arterial hypertension. No additional education session on diet or exercise was provided, and participants were asked to maintain their usual daily lifestyle.
Primary outcome measurement
The primary outcome of the current study was office BP. Office BP was determined according to the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC-7) guidelines. After participants sat quietly for 5 minutes, 2 BP measurements were obtained 5 minutes apart with a validated automated sphygmomanometer (HEM-7080IT; Omron Healthcare, Kyoto, Japan) at each visit.
Secondary and other outcome measurements
Twenty-four-hour ABPM was performed using a Takeda TM-2430 instrument (A&D Medical, Tokyo, Japan) with readings taken every 30 minutes. Daytime and nighttime periods were defined according to information provided by the patient. Ambulatory BP readings were averaged for 24 hours, daytime, and nighttime.
Central hemodynamics were evaluated in the sitting position after 10 minutes of rest using the SphygmoCor system (AtCor Medical, Sydney, Australia). A high-fidelity micromanometer (Millar Instruments, Houston, TX, USA) was used to record peripheral pressure waveforms from the radial arteries, as reported previously.10),11) Central SBP, DBP, pulse pressure, augmentation pressure, forward wave amplitude, and augmentation index (AI) were acquired from the aortic pressure waveform analyses.
Height and weight were measured using standard methodology, while the subject was wearing light indoor clothing without shoes, and rounded up to the nearest 0.1 cm using a stadiometer. Body composition was measured using an Omron Karada Scan Body Fat Analyzer (HBF-359; Omron, Tokyo, Japan). Waist circumference was measured at the navel and recorded to the nearest centimeter (cm).12)
Physical activity was assessed by using the Godin Leisure-Time Exercise Questionnaire and 7-Day Physical Activity Recall at randomization at 1, 4, and 8 weeks. Three fitness tests were performed at baseline and at the end of the study: maximal oxygen consumption test, push-up test, and hand grip strength test. A graded maximal treadmill test was performed using a treadmill (T2100; GE Healthcare, Seoul, Korea) with a gas analyzer and electrocardiograph. The modified Bruce protocol was used for all participants. For the push-up test, the participants were asked to complete as many standard pushups as possible in 2 minutes, while maintaining proper form (on the toes while keeping the back and knees straight for men, and kneeling while keeping the back straight for women). Hand grip strength was measured with a Takei A5401 hand grip dynamometer (Takei Scientific Instruments, Niigata, Japan) in both hands.
To investigate dietary sodium intake, a 125-item dish-frequency questionnaire (DFQ) was used at the first screening visit at 1, 4, and at the end of the study, which was developed to estimate habitual sodium intake by assessing intakes of individual dishes commonly eaten by Koreans, who usually enjoy soups, stews, and pickled vegetables such as kimchi.13) When the actual sodium intake from soup or stew was calculated, sodium content in the leftover broth was subtracted from the total sodium content of the food.14) Data on energy, carbohydrate, protein, fat, cholesterol, dietary fiber, potassium, magnesium, and calcium intake from the diet were assessed by using 24-hour dietary recall. Twenty-four-hour urine collection was also performed for the measurement of sodium, potassium, phosphorus, and urea nitrogen. Each of these measurements was obtained at baseline and at 8 weeks.
Statistical analysis
Data were analyzed by using the intent-to-treat principle, with missing values managed with last-observation-carried-forward imputation. Per-protocol analysis was performed as a sensitivity analysis, and the results are shown in the supplementary data (Supplementary Tables 1, 2, 3, 4, 5, Supplementary Figures 1, 2). For each variable, the change from baseline to 8 weeks was calculated. Group differences in continuous variables were analyzed with a one-way analysis of variance (ANOVA) and a post hoc test using Tukey's honest significant difference (HSD) test. Analysis of covariance was performed to analyze differences in BP at the end of the study and in change of BP adjusting for age, sex, and baseline BP. To examine within-group paired data, a paired t-test was used. Categorical variables were summarized as numbers and percentages of the group total. Pearson's χ2 test was performed to compare categorical variables. Data analysis was performed using SPSS version 23.0 for Windows (IBM Corp., Armonk, NY, USA). The p values of <0.05 were considered statistically significant.
RESULTS
Study population
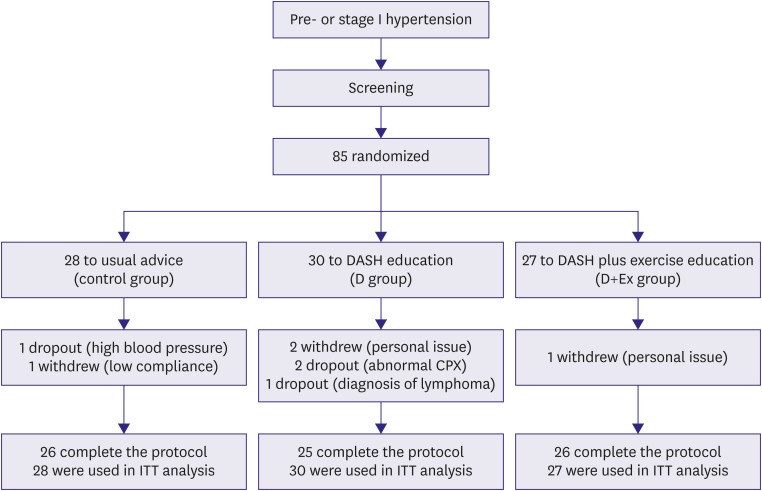
A total of 87 patients participated in the study. Among these 87 participants, 72 (87.8%) completed the study. The flow of the participants throughout the trial is shown in Figure 1.
Figure 1.
Participant flow chart of the Korean LifeStyle Modification on Hypertension study.
C group = advice-only comparison group; CPX = cardiopulmonary exercise test; D group = diet education group; D+Ex group = diet and exercise education group; DASH = Dietary Approaches to Stop Hypertension; ITT = intention-to-treat.
Baseline characteristics
Participants' mean age was 45.1±13 years, 78% were men, and 82% were either overweight or obese. Waist circumference was higher in the D+Ex group (Table 1). Renal function and other metabolic profiles did not differ among the 3 groups. All patients had either prehypertension or stage I hypertension, with mean office SBP and DBP of 134.5±10.0 mmHg and 86.0±7.8 mmHg, respectively. The mean office SBP and DBP values did not statistically differ among the 3 groups (Table 1). There were no differences in the types of hypertension and antihypertensive medications among the 3 groups (Supplementary Table 6).
Table 1. Baseline characteristics of study subjects.
| C group (n=28) | D group (n=30) | D+Exgroup (n=27) | p value across all groups | p value* | |||
|---|---|---|---|---|---|---|---|
| C vs. D | C vs. D+Ex | ||||||
| Age (year) | 43.4±14.5 | 43.0±13.5 | 49.1±10.1 | 0.145 | 0.993 | 0.228 | |
| Male | 21 (75) | 20 (66.7) | 25 (92.6) | 0.124 | |||
| BMI (kg/m2) | 24.6±2.5 | 25.7±4.3 | 26.8±3.0 | 0.054 | 0.39 | 0.042 | |
| Waist (cm) | 88.4±7.0 | 91.3±11.2 | 94.7±7.3 | 0.032 | 0.419 | 0.024 | |
| BUN (mg/dL) | 13.7±3.2 | 12.9±3.1 | 14.1±2.9 | 0.346 | 0.561 | 0.34 | |
| Creatinine (mg/dL) | 0.9±0.2 | 0.8±0.1 | 0.9±0.1 | 0.026 | 0.299 | 0.426 | |
| eGFR (mL/min/1.73 m2) | 94.8±15.4 | 97.8±12.7 | 89.9±15.6 | 0.125 | 0.717 | 0.423 | |
| Na (mmol/L) | 141.6±1.6 | 141.8±1.8 | 140.9±1.6 | 0.126 | 0.933 | 0.262 | |
| K (mmol/L) | 4.5±0.4 | 4.4±0.3 | 4.4±0.3 | 0.421 | 0.886 | 0.397 | |
| Total cholesterol (mg/dL) | 181.4±28.1 | 190.7±40.1 | 193±34.6 | 0.418 | 0.564 | 0.429 | |
| LDL cholesterol (mg/dL) | 100.6±28.4 | 115.9±30.8 | 110.7±35.6 | 0.184 | 0.07 | 0.244 | |
| HDL cholesterol (mg/dL) | 49.4±15.9 | 50.6±13.7 | 44.9±10.5 | 0.259 | 0.941 | 0.436 | |
| Triglyceride (mg/dL) | 126.9±80.8 | 120.8±62.0 | 213.2±256.5 | 0.053 | 0.988 | 0.107 | |
| Glucose (mg/dL) | 98.4±13.0 | 97.7±9.6 | 102.3±13.9 | 0.324 | 0.975 | 0.466 | |
| Office BP (mmHg) | |||||||
| SBP | 134.5±10.0 | 135.3±11.8 | 139.3±13.2 | 0.272 | 0.963 | 0.288 | |
| DBP | 86.0±7.8 | 86.7±9.2 | 88.7±7.3 | 0.443 | 0.932 | 0.431 | |
| ABPM (mmHg) | |||||||
| 24-hour SBP | 131.8±8.1 | 133.6±11.2 | 135.2±9.4 | 0.198 | 0.707 | 0.333 | |
| 24-hour DBP | 82.3±6.0 | 83.0±6.8 | 85.3±6.3 | 0.082 | 0.876 | 0.146 | |
| Daytime SBP | 137.4±7.4 | 139.4±10.5 | 140.6±10.9 | 0.224 | 0.668 | 0.373 | |
| Daytime DBP | 86.3±5.5 | 87.7±7.6 | 90.3±8.0 | 0.04 | 0.667 | 0.075 | |
| Nighttime SBP | 117.8±13.4 | 120.5±15.1 | 121.1±12.0 | 0.363 | 0.674 | 0.567 | |
| Nighttime DBP | 72.9±8.9 | 72.3±7.4 | 75.0±7.3 | 0.312 | 0.954 | 0.488 | |
Data are presented as mean±SD or number (%). Continuous variables were compared with one-way ANOVA. Categorical variables were compared with linear-by-linear association test.
ABPM = ambulatory blood pressure monitoring; ANOVA = analysis of variance; BMI = body mass index; BP = blood pressure; BUN = blood urea nitrogen; C group = advice-only comparison group; D group = diet education group; D+Ex group = diet and exercise education group; DBP = diastolic blood pressure; eGFR = estimated glomerular filtration rate; HDL = high-density lipoprotein; HSD = honest significant difference; LDL = low-density lipoprotein; SBP = systolic blood pressure; SD = standard deviation.
*Tukey HSD.
Effects of intervention on BP
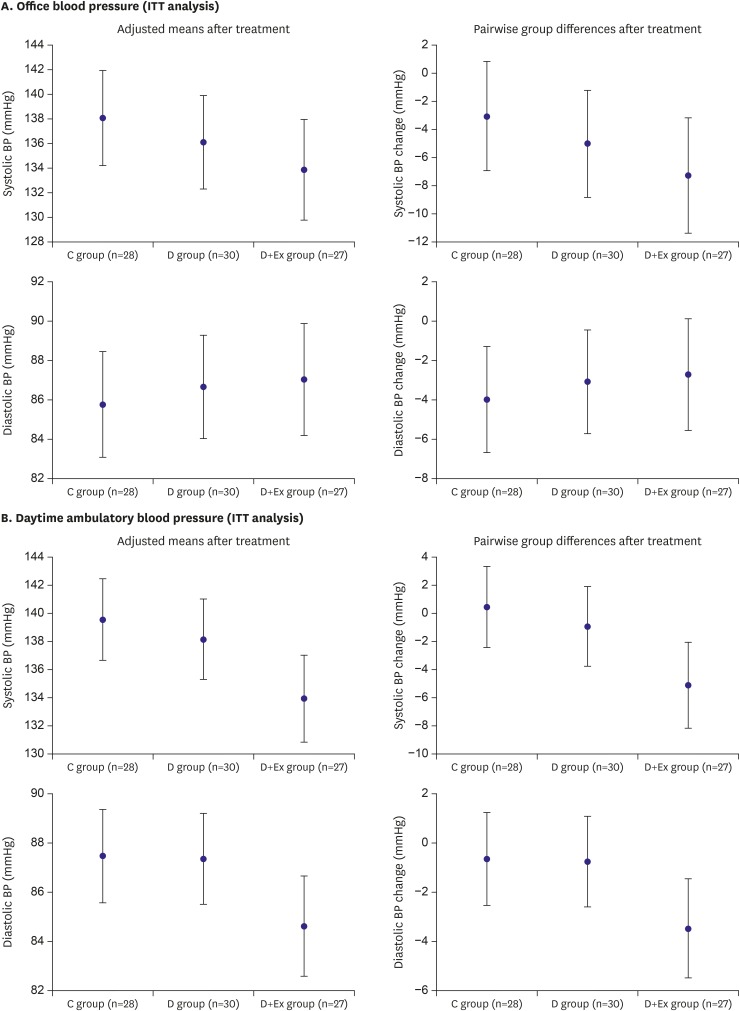
There was no difference in the magnitude of change in office SBP and DBP after the intervention among 3 groups (Table 2). Office SBP and DBP did not differ among the 3 groups after adjustment for age, sex, and baseline office BP (Figure 2A). Although there was no difference in ambulatory BP measurements at 8 weeks among 3 groups (Supplementary Table 7), the analysis of ABPM revealed significant reductions of daytime ambulatory SBP and DBP and a tendency for significant reduction of nighttime ambulatory SBP in the D+Ex group (Table 2). At 8 weeks, daytime ambulatory SBP and DBP were significantly lower in the D+Ex group than in the C group after adjustment for age, sex, and baseline daytime ambulatory BP (Figure 2B). In addition, the reduction of daytime ambulatory SBP was significant and that of daytime ambulatory DBP showed marginal significance in the D+Ex group compared to the C group in pairwise analyses for intergroup differences adjusting for age, sex, and baseline ambulatory BP (Figure 2B). However, daytime ambulatory SBP and DBP were not lower in the D group than in the C group, and the magnitude of BP reduction did not significantly differ between the D and C groups. Additionally, the D+Ex group showed a tendency towards higher achievement of BP control but without statistical significance (Supplementary Figure 3).
Table 2. BP change during the study period.
| C group | D group | D+Ex group | ||||
|---|---|---|---|---|---|---|
| Difference | p value | Difference | p value | Difference | p value | |
| Office SBP | 2.0±10.0 | 0.319 | 0.7±9.6 | 0.677 | −3.6±15.3 | 0.238 |
| Office DBP | −1.4±7.3 | 0.334 | 0.4±8.2 | 0.809 | −1.0±8.0 | 0.507 |
| 24-hour SBP | 0.9±6.5 | 0.459 | −1.6±7.4 | 0.248 | −5.1±7.1 | 0.001 |
| 24-hour DBP | 0.5±4.8 | 0.610 | −0.7±4.6 | 0.393 | −2.7±4.9 | 0.009 |
| Daytime SBP | 0.8±7.6 | 0.588 | −1.1±7.4 | 0.438 | −5.4±8.8 | 0.003 |
| Daytime DBP | −0.1±5.4 | 0.944 | −0.8±4.8 | 0.384 | −4.1±6.8 | 0.004 |
| Nighttime SBP | 0.5±11.6 | 0.834 | −3.1±11.5 | 0.147 | −3.7±9.6 | 0.056 |
| Nighttime DBP | 0.4±7.4 | 0.781 | −1.0±6.6 | 0.412 | −1.2±6.9 | 0.366 |
Data are presented as mean±SD. Differences between baseline and at 8 weeks were compared with paired t-test.
BP = blood pressure; C group = advice-only comparison group; D group = diet education group; D+Ex = diet and exercise education group; DBP = diastolic blood pressure; SBP = systolic blood pressure.
Figure 2.
Comparison of post-intervention means and 95% CI for office BP and daytime ambulatory BP using an ANCOVA model adjusted for age, sex, and pre-intervention BP. (A) The left panels show the differences between both intervention groups and the control group were insignificant for office SBP (p=0.347) and DBP (p=0.801). The right panels show the comparison of mean differences and 95% CI between the intervention groups using an ANCOVA model adjusted for age, sex, and pre-intervention office SBP. (B) The left panels show the difference between both intervention groups and the control group was significant for daytime ambulatory SBP (p=0.034) and insignificant for daytime ambulatory DBP (p=0.097). The right panels show the comparison of mean differences and 95% CI between the intervention groups using an ANCOVA model adjusted for age, sex, and pre-intervention daytime ambulatory SBP.
ANCOVA = analysis of covariance; BP = blood pressure; C group = advice-only comparison group; CI = confidence interval; DBP = diastolic blood pressure; D group = diet education group; D+Ex group = diet and exercise education group; ITT = intention-to-treat; SBP = systolic blood pressure.
Central hemodynamics were evaluated at baseline and at 8 weeks (Supplementary Table 8). Central BP, augmentation index, and pulse wave velocities did not change from baseline in all 3 groups. The degree of change after intervention did not differ among the groups.
Intervention effects on other variables
Table 3 shows changes in lifestyle variables during the 8-week study period in each group and mean differences between groups at 8 weeks. Waist circumference was significantly reduced in both the D and D+Ex groups compared with the C group. Self-reported sodium intake decreased significantly in all 3 groups at 8 weeks compared to baseline, with the change in the D group showing marginal significance and the change in the D+Ex group being significant compared to the C group. However, the reduction of urinary sodium excretion was only significant in the D+Ex group, and the magnitude of the change in the D+Ex group demonstrated borderline significant difference compared to that of the C group. Other urinary excretory variables did not show any significant differences.
Table 3. Interventional outcomes at baseline and at 8 weeks by randomization group.
| C group (n=28) | D group (n=30) | D+Exgroup (n=27) | p value across all groups | p value* | |||
|---|---|---|---|---|---|---|---|
| C vs. D | C vs. D+Ex | ||||||
| Weight (kg) | |||||||
| Baseline | 69.9±9.2 | 72.8±15.2 | 76.6±10.7 | 0.131 | 0.631 | 0.110 | |
| At 8 weeks | 70.0±9.2 | 72.5±14.5 | 75.8±10.9 | 0.197 | 0.701 | 0.171 | |
| Change | 0.0±1.6 | −0.4±2.1 | −0.8±1.7† | 0.240 | 0.671 | 0.210 | |
| Waist (cm) | |||||||
| Baseline | 88.4±7.0 | 91.3±11.2 | 94.7±7.3 | 0.032 | 0.419 | 0.024 | |
| At 8 weeks | 88.5±7.6 | 89.8±11.3 | 93.0±7.2 | 0.166 | 0.841 | 0.157 | |
| Change | 0.1±3.0 | −1.5±2.6† | −1.8±2.3† | 0.021 | 0.061 | 0.029 | |
| Sodium intake (g/day) | |||||||
| Baseline | 4.6±1.9 | 4.1±1.7 | 4.9±1.9 | 0.235 | 0.49 | 0.856 | |
| At 8 weeks | 4.1±1.9 | 2.8±1.6 | 3.0±1.5 | 0.011 | 0.012 | 0.055 | |
| Change | −0.5±1.3† | −1.3±1.4† | −1.9±1.7† | 0.006 | 0.068 | 0.001 | |
| 24-hour urinary sodium excretion (mmol/24 hr) | |||||||
| Baseline | 147.3±63.3 | 143.4±62.6 | 178.7±50.6 | 0.058 | 0.977 | 0.991 | |
| At 8 weeks | 137.2±52.0 | 140.3±60.6 | 139.2±59.2 | 0.979 | 0.839 | 0.896 | |
| Change | −10.1±62.3 | −3.2±48.4 | −39.5±68.0† | 0.061 | 0.662 | 0.072 | |
| 24-hour urinary potassium excretion (mmol/24 hr) | |||||||
| Baseline | 54.5±19.5 | 50.9±19.8 | 55.4±14.6 | 0.616 | 0.73 | 0.985 | |
| At 8 weeks | 52.0±23.5 | 47.9±25.3 | 52.2±26.1 | 0.756 | 0.53 | 0.974 | |
| Change | −2.5±24.9 | −3.0±17.7 | −3.1±22.2 | 0.994 | 0.928 | 0.920 | |
| 24-hour urinary phosphorus excretion (mg/24 hr) | |||||||
| Baseline | 761.5±250.5 | 803.9±303.7 | 790.9±257.7 | 0.834 | 0.825 | 0.916 | |
| At 8 weeks | 756.7±260.2 | 737.3±318.2 | 728.9±302.1 | 0.938 | 0.803 | 0.728 | |
| Change | −4.9±264.9 | −66.7±248.1 | −62.0±284.0 | 0.623 | 0.378 | 0.427 | |
| 24-hour urinary urea nitrogen excretion (g/24 hr) | |||||||
| Baseline | 9.3±3.3 | 9.0±3.1 | 9.6±3.0 | 0.781 | 0.817 | 0.69 | |
| At 8 weeks | 8.9±2.8 | 8.4±3.6 | 8.2±3.1 | 0.654 | 0.505 | 0.377 | |
| Change | −0.4±3.1 | −0.6±2.6 | −1.4±3.7 | 0.438 | 0.745 | 0.217 | |
Data are presented as mean±SD. Continuous variables were compared with one-way ANOVA.
ANOVA = analysis of variance; C group = advice-only comparison group; D group = diet education group; D+Ex group = diet and exercise education group; HSD = honest significant difference; SD = standard deviation.
*Tukey HSD; †p<0.05 for change between baseline and at 8 weeks determined by paired t-test.
Table 4 shows variables relevant to exercise capacity at baseline and at 8 weeks in each group. Initial cardiopulmonary fitness and muscular strength were similar across groups. At 8 weeks, the changes in aerobic capacity, determined by the maximal amount of oxygen (VO2 peak) during cardiopulmonary exercise test, did not significantly differ among the groups, and that of the C group increased slightly compared to baseline. Although the change of VO2 peak did not differ across groups, heart rate in the recovery phase of the step test decreased significantly compared to that at baseline (−5.8 beats/min; 95% confidence interval [CI], −2 to −9.7 beats/min; p=0.005) in the D+Ex group. However, the changes in heart rate in the recovery phase of the step test were not statistically significant in the other groups or significantly different across the groups. In the D+Ex group, parameters of resistance exercise, namely hand grip strength and push-up, were significantly improved compared to baseline. However, the changes in resistance exercise parameters did not significantly differ among the 3 groups.
Table 4. Variables related to exercise capacity at baseline and at 8 weeks by randomization group.
| C group (n=28) | D group (n=30) | D+Ex group (n=27) | p value across all groups | p value* | ||||
|---|---|---|---|---|---|---|---|---|
| C vs. D | C vs. D+Ex | |||||||
| Cardiopulmonary fitness test | ||||||||
| VO2 peak (mL/kg/min) | ||||||||
| Baseline | 33.0±5.9 | 30.5±6.5 | 32.0±5.3 | 0.282 | 0.255 | 0.809 | ||
| At 8 weeks | 34.6±6.0 | 31.5±5.4 | 32.8±5.5 | 0.124 | 0.104 | 0.651 | ||
| Change | 1.6±3.6† | 1.0±6.0 | 0.8±3.2 | 0.792 | 0.868 | 0.793 | ||
| Metabolic equivalents | ||||||||
| Baseline | 9.5±1.8 | 8.9±1.4 | 9.1±1.6 | 0.354 | 0.336 | 0.602 | ||
| At 8 weeks | 9.9±1.7 | 9.0±1.5 | 9.4±1.6 | 0.128 | 0.107 | 0.494 | ||
| Change | 0.4±1.3 | 0.1±1.2 | 0.3±1.0 | 0.656 | 0.644 | 0.964 | ||
| VE/VCO2 slope | ||||||||
| Baseline | 27.2±3.4 | 26.9±5.2 | 26.2±5.8 | 0.767 | 0.978 | 0.758 | ||
| At 8 weeks | 27.7±3.7 | 27.7±2.8 | 27.6±2.4 | 0.994 | 0.998 | 0.994 | ||
| Change | 1.2±3.3 | 0.1±3.7 | 1.4±6.5 | 0.594 | 0.696 | 0.992 | ||
| Step test (heart rate at recovery) | ||||||||
| Baseline | 89.7±12.6 | 90.7±17.3 | 89.3±11.3 | 0.929 | 0.959 | 0.995 | ||
| At 8 weeks | 87.3±14.8 | 89.2±15.7 | 83.5±9.1 | 0.295 | 0.86 | 0.563 | ||
| Change | −2.4±11.7 | −1.5±12.4 | −5.8±9.6† | 0.339 | 0.955 | 0.508 | ||
| Muscle strength test | ||||||||
| Push up (/min) | ||||||||
| Baseline | 17.6±12.4 | 19.9±20.8 | 19.1±13.9 | 0.864 | 0.854 | 0.941 | ||
| At 8 weeks | 19.5±13.5 | 20.0±20.8 | 24.5±18.1 | 0.656 | 0.995 | 0.679 | ||
| Change | 1.9±3.9† | 0.1±5.8 | 5.4±6.7† | 0.002 | 0.427 | 0.06 | ||
| Hand grip (kg) | ||||||||
| Baseline | 34.9±8.7 | 33.2±8.8 | 38±9.8 | 0.14 | 0.752 | 0.424 | ||
| At 8 weeks | 34.5±10.0 | 33.2±11.0 | 40.2±10.2 | 0.032 | 0.879 | 0.112 | ||
| Change | −0.4±3.5 | 0.0±8.3 | 2.2±3.4† | 0.186 | 0.962 | 0.205 | ||
Data are presented as mean±SD. Continuous variables were compared with one-way ANOVA.
ANOVA = analysis of variance; C group = advice-only comparison group; D group = diet education group; D+Ex group = diet and exercise education group; SD = standard deviation; VO2 peak = maximal amount of oxygen; VE/VCO2 = ventilatory equivalent ratio for carbon dioxide.
*Tukey HSD; †p<0.05 for change between baseline and at 8 weeks determined by paired t-test.
DISCUSSION
The present study demonstrated that, first, the usual recommendation of lifestyle modification by the attending physician in an office may be insufficient to reduce BP. Second, the compliance with dietary modifications based on education by a nutritionist is insufficient in the usual office setting. Third, both active dietary education and exercise education are needed for effective reduction of BP. In contrast to other lifestyle modification studies, lifestyle modification without active monitoring, which is more consistent with real-word practice, was performed in this study.
The DASH diet was devised for the prevention and management of hypertension. It is known to reduce SBP by 6 to 11 mmHg in patients with prehypertension and stage I hypertension.15) The DASH-sodium diet has been shown to have an additional SBP lowering effect of 7.2 mmHg, which is equal to adding one antihypertensive drug.8) The culturally modified DASH diet for Koreans has shown efficacy in BP lowering, as it reduced SBP by 4.5 mmHg and DBP by 2.6 mmHg.16) As such, the Korean modified DASH diet was used as the dietary program in this study. However, implementation of the DASH diet and sodium intake reduction in the current study did not result in significant lowering of ABPM BP or office BP in the D group. To verify participants' compliance to the dietary intervention, sodium intake and urinary sodium excretion were assessed. Although self-reported sodium intake decreased compared to baseline, 24-hour urinary sodium excretion did not decrease and was similar to that of the C group. This finding may imply that dietary patterns are not easily altered by basic education. Previous studies where dietary advice for DASH is given in real-world settings have shown a low level of compliance.17) In a study by Couch et al.,18) 21% of participants achieved the DASH target for fruits, vegetables, and saturated fat in a 3-month randomized trial. The Premier trial, a representative study showing the effect of lifestyle modification on BP, evaluated change in BP over 18 months and found that compliance with lifestyle changes decreased between the 6- and 18-month follow-up visits. While the Premier trial revealed that behavioral changes can be sustained over long periods, it conversely suggests that persistent or intensive intervention is needed for improved hypertension management results.19) In the early phase of the Premier trial, participants kept in close contact with an interventionist to acquire behavioral skills related to the lifestyle guidelines and to establish goals for lifestyle change.20) By contrast, our results demonstrated that a relatively less intensive intervention, which educates participants to modify their dietary habits voluntarily without close contact during the inter-visit period, is insufficient to control BP. The results from this study support the practice of persistent, close contact and active monitoring by an interventionist to maintain good compliance.
In contrast to the DASH diet alone, DASH diet plus exercise was able to significantly reduce daytime ambulatory SBP in this study. Aerobic or resistant exercise has been shown to control BP and regular exercise is recommended for the primary prevention of hypertension.21),22) In this study, participants were encouraged to participate in at least 150 minutes per week of aerobic exercise and daily participation in strengthening exercise by following an exercise DVD. No improvement in aerobic capacity was observed; however, upper body muscle strength and endurance were improved after the intervention, suggesting that participants complied with the mild- to moderate-resistance strengthening exercise. Notably, significant and definite BP lowering effects of exercise in combination with dietary intervention were observed. Previous studies have shown that effective exercise intervention is associated with increased VO2 peak or reduced resting heart rate.9) Interestingly however, in the present study, ABPM BP in the D+Ex group was significantly reduced despite the absence of significant improvement in VO2 peak. Therefore, we speculate that the reduction in ambulatory BP in the D+Ex group resulted from various other factors. For example, waist circumference decreased significantly in the D+Ex group compared to the other groups. The reduction of abdominal obesity and visceral fat, which is known to play an important role in hypertension, may have significantly influenced the ambulatory BP reduction in the D+Ex group.23) Improvement in endothelial function, oxidative stress, and autonomic function may be some other plausible explanations for the beneficial effect of exercise.24) Although the measurements related to aerobic exercise did not change from baseline at 8 weeks, the change in muscle strength was significant in only the D+Ex group. Strengthening exercise is known as an effective training modality to reduce resting BP. Multiple adaptations in vasculature, cardiac structure, and the autonomic nervous system are likely to be responsible for the significant ambulatory BP reduction in the D+Ex group.24)
DASH diet and/or exercise, when implemented as an unmonitored education program alone, might not be as efficacious as active, monitored intervention. As most lifestyle interventions in clinical practice are unmonitored education programs, the findings from this study may have important clinical implications. A previous study also reported the lack of efficacy of lifestyle modification for BP control in the primary care setting.25) Therefore, it should be emphasized that more active cognitive-behavioral strategies such as psychological support, goal setting, and group-mediated cognitive behavior intervention could improve patient adherence for better outcomes in terms of behavioral change.26-28) We speculate that the reason for significant reduction in ambulatory BP and urinary sodium only in the D+Ex group and not in the D group despite receiving the same dietary education might be that additional exercise education induced participants to care more about their health behavior and to practice lifestyle modification more actively. This finding supports the notion that total behavioral modification, rather than focusing on modifying a single behavioral target, is important for improving the efficacy of lifestyle modification. There is limited scientific evidence on the relative benefit of interventions targeting a single behavior versus multiple behaviors, but most studies that performed interventions on multiple behaviors reported positive results,29) which is consistent with the result of this study. To evaluate this hypothesis, further research investigating changes in compliance to dietary education by simultaneous exercise education might be required.
This study has some limitations. First, although patients were randomly assigned to intervention groups, more obese patients and more male patients were included in the D+Ex group. Thus, randomization bias may have affected the results. However, there was no difference in proportion of participants with prehypertension or hypertension (Supplementary Table 6) and BP reduction was significant in the D+Ex group after adjustment for baseline BP, age, and sex. In addition, subgroup analysis of participants with prehypertension showed similar results with that of the total study participants (Supplementary Table 9). Second, patient adherence was not analyzed, because the specific aim of this study was to evaluate the effect of unmonitored lifestyle modification on BP. In terms of exercise intervention, all participants were asked to submit their exercise diary, however, only about 70% of participants returned their exercise diary. Therefore, we cannot calculate exact amount of exercise dose and estimate adherence. In lifestyle modifications to manage hypertension, compliance is a very challenging issue. If data could indicate a difference in BP reduction according to adherence level, this study would be more powerful. Third, this intervention failed to achieve the primary endpoint, the reduction of office BP. This limitation may have resulted from the BP change in this study being smaller than the BP reduction that had been assumed for sample size estimation, thus leaving the study underpowered. Nonetheless, it is a meaningful result that BP reduction on ABPM was observed in patients who received dietary and exercise education.
In conclusion, unmonitored lifestyle modification through diet and exercise, but not diet alone, was effective for lowering BP. Lifestyle modification emphasizing both dietary modification and exercise should be encouraged.
Footnotes
Funding: This work was supported by a grant from the Korean Health Technology R&D Project, Ministry of Health and Welfare, Republic of Korea (HI13C0715) and by a research grant from Sanofi-Aventis Korea Company (4-2011-0305).
Conflict of Interest: The authors have no financial conflicts of interest.
- Conceptualization: Jeon JY, Park S.
- Data curation: Hong SH, Lee M, Park S.
- Formal analysis: Lee CJ, Kim JY, Jeon JY.
- Funding acquisition: Park S.
- Investigation: Shim E, Jeon JY, Park S.
- Methodology: Kim JY, Shim E, Hong SH, Jeon JY.
- Project administration: Park S.
- Resources: Lee M.
- Supervision: Jeon JY, Park S.
- Validation: Shim E, Jeon JY.
- Visualization: Lee CJ.
- Writing - original draft: Lee CJ, Kim JY, Park S.
- Writing - review & editing: Park S.
SUPPLEMENTARY MATERIALS
Baseline characteristics of study subjects (PP analysis)
Interventional outcomes at baseline and at 8 weeks by randomization group (PP analysis)
Variables related to exercise capacity at baseline and at 8 weeks by randomization group (PP analysis)
BP change during the study period (PP analysis)
The change of central hemodynamics during the study period (PP analysis)
Baseline types of hypertension and antihypertensive medications (ITT analysis)
Ambulatory BP at 8 weeks (ITT analysis)
The change of central hemodynamics during study period (ITT analysis)
BP change during the study period among subject with prehypertension
Comparison of post-intervention means and 95% CI for office BP and daytime ambulatory BP using an ANCOVA model adjusted for age, sex, and pre-intervention BP in the PP dataset.
Percentage of patients with controlled daytime ambulatory BP at 8 weeks according to intervention group among patients with uncontrolled daytime BP at baseline in the PP set.
Percentage of patients with controlled daytime ambulatory BP at 8 weeks according to intervention group among patients with uncontrolled daytime BP at baseline.
References
- 1.Weber MA, Schiffrin EL, White WB, et al. Clinical practice guidelines for the management of hypertension in the community a statement by the American Society of Hypertension and the International Society of Hypertension. J Hypertens. 2014;32:3–15. doi: 10.1097/HJH.0000000000000065. [DOI] [PubMed] [Google Scholar]
- 2.Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) Eur Heart J. 2013;34:2159–2219. doi: 10.1093/eurheartj/eht151. [DOI] [PubMed] [Google Scholar]
- 3.Eckel RH, Jakicic JM, Ard JD, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129:S76–S99. doi: 10.1161/01.cir.0000437740.48606.d1. [DOI] [PubMed] [Google Scholar]
- 4.Whelton SP, Chin A, Xin X, He J. Effect of aerobic exercise on blood pressure: a meta-analysis of randomized, controlled trials. Ann Intern Med. 2002;136:493–503. doi: 10.7326/0003-4819-136-7-200204020-00006. [DOI] [PubMed] [Google Scholar]
- 5.Friedberg JP, Rodriguez MA, Watsula ME, et al. Effectiveness of a tailored behavioral intervention to improve hypertension control: primary outcomes of a randomized controlled trial. Hypertension. 2015;65:440–446. doi: 10.1161/HYPERTENSIONAHA.114.03483. [DOI] [PubMed] [Google Scholar]
- 6.Parikh A, Lipsitz SR, Natarajan S. Association between a DASH-like diet and mortality in adults with hypertension: findings from a population-based follow-up study. Am J Hypertens. 2009;22:409–416. doi: 10.1038/ajh.2009.10. [DOI] [PubMed] [Google Scholar]
- 7.Bassett DR, Jr, Fitzhugh EC, Crespo CJ, King GA, McLaughlin JE. Physical activity and ethnic differences in hypertension prevalence in the United States. Prev Med. 2002;34:179–186. doi: 10.1006/pmed.2001.0969. [DOI] [PubMed] [Google Scholar]
- 8.Sacks FM, Svetkey LP, Vollmer WM, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med. 2001;344:3–10. doi: 10.1056/NEJM200101043440101. [DOI] [PubMed] [Google Scholar]
- 9.Cornelissen VA, Fagard RH. Effects of endurance training on blood pressure, blood pressure-regulating mechanisms, and cardiovascular risk factors. Hypertension. 2005;46:667–675. doi: 10.1161/01.HYP.0000184225.05629.51. [DOI] [PubMed] [Google Scholar]
- 10.Weber T, Auer J, O'Rourke MF, et al. Arterial stiffness, wave reflections, and the risk of coronary artery disease. Circulation. 2004;109:184–189. doi: 10.1161/01.CIR.0000105767.94169.E3. [DOI] [PubMed] [Google Scholar]
- 11.Weber T, O'Rourke MF, Ammer M, Kvas E, Punzengruber C, Eber B. Arterial stiffness and arterial wave reflections are associated with systolic and diastolic function in patients with normal ejection fraction. Am J Hypertens. 2008;21:1194–1202. doi: 10.1038/ajh.2008.277. [DOI] [PubMed] [Google Scholar]
- 12.World Health Organization. Waist circumference and waist-hip ratio: report of a WHO expert consultation, Geneva, 8-11 December 2008. Geneva: World Health Organization; 2011. [Google Scholar]
- 13.Son SM, Park YS, Lim WJ, Kim SB, Jeong YS. Development and evaluation of validity of short Dish Frequency Questionnaire (DFQ) for estimation of habitual sodium intake for Korean adults. Korean J Community Nutr. 2007;12:838–853. [Google Scholar]
- 14.Son SM, Park YS, Lim HJ, Kim SB, Jeong YS. Sodium intakes of Korean adults with 24-hour urine analysis and Dish Frequency Questionnaire and comparison of sodium intakes according to the regional area and dish group. Korean J Community Nutr. 2007;12:545–558. [Google Scholar]
- 15.Moore TJ, Conlin PR, Ard J, Svetkey LP. DASH (Dietary Approaches to Stop Hypertension) diet is effective treatment for stage 1 isolated systolic hypertension. Hypertension. 2001;38:155–158. doi: 10.1161/01.hyp.38.2.155. [DOI] [PubMed] [Google Scholar]
- 16.Kim H, Song HJ, Han HR, Kim KB, Kim MT. Translation and validation of the dietary approaches to stop hypertension for koreans intervention: culturally tailored dietary guidelines for Korean Americans with high blood pressure. J Cardiovasc Nurs. 2013;28:514–523. doi: 10.1097/JCN.0b013e318262c0c1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kwan MW, Wong MC, Wang HH, et al. Compliance with the Dietary Approaches to Stop Hypertension (DASH) diet: a systematic review. PLoS One. 2013;8:e78412. doi: 10.1371/journal.pone.0078412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Couch SC, Saelens BE, Levin L, Dart K, Falciglia G, Daniels SR. The efficacy of a clinic-based behavioral nutrition intervention emphasizing a DASH-type diet for adolescents with elevated blood pressure. J Pediatr. 2008;152:494–501. doi: 10.1016/j.jpeds.2007.09.022. [DOI] [PubMed] [Google Scholar]
- 19.Elmer PJ, Obarzanek E, Vollmer WM, et al. Effects of comprehensive lifestyle modification on diet, weight, physical fitness, and blood pressure control: 18-month results of a randomized trial. Ann Intern Med. 2006;144:485–495. doi: 10.7326/0003-4819-144-7-200604040-00007. [DOI] [PubMed] [Google Scholar]
- 20.Funk KL, Elmer PJ, Stevens VJ, et al. PREMIER--a trial of lifestyle interventions for blood pressure control: intervention design and rationale. Health Promot Pract. 2008;9:271–280. doi: 10.1177/1524839906289035. [DOI] [PubMed] [Google Scholar]
- 21.ESH/ESC Task Force for the Management of Arterial Hypertension. 2013 practice guidelines for the management of arterial hypertension of the European Society of Hypertension (ESH) and the European Society of Cardiology (ESC): ESH/ESC Task Force for the Management of Arterial Hypertension. J Hypertens. 2013;31:1925–1938. doi: 10.1097/HJH.0b013e328364ca4c. [DOI] [PubMed] [Google Scholar]
- 22.Sharman JE, La Gerche A, Coombes JS. Exercise and cardiovascular risk in patients with hypertension. Am J Hypertens. 2015;28:147–158. doi: 10.1093/ajh/hpu191. [DOI] [PubMed] [Google Scholar]
- 23.Guagnano MT, Ballone E, Colagrande V, et al. Large waist circumference and risk of hypertension. Int J Obes Relat Metab Disord. 2001;25:1360–1364. doi: 10.1038/sj.ijo.0801722. [DOI] [PubMed] [Google Scholar]
- 24.Millar PJ, McGowan CL, Cornelissen VA, Araujo CG, Swaine IL. Evidence for the role of isometric exercise training in reducing blood pressure: potential mechanisms and future directions. Sports Med. 2014;44:345–356. doi: 10.1007/s40279-013-0118-x. [DOI] [PubMed] [Google Scholar]
- 25.Petrella RJ, Lattanzio CN, Shapiro S, Overend T. Improving aerobic fitness in older adults: effects of a physician-based exercise counseling and prescription program. Can Fam Physician. 2010;56:e191–200. [PMC free article] [PubMed] [Google Scholar]
- 26.Nothwehr F, Yang J. Goal setting frequency and the use of behavioral strategies related to diet and physical activity. Health Educ Res. 2007;22:532–538. doi: 10.1093/her/cyl117. [DOI] [PubMed] [Google Scholar]
- 27.Shilts MK, Horowitz M, Townsend MS. Goal setting as a strategy for dietary and physical activity behavior change: a review of the literature. Am J Health Promot. 2004;19:81–93. doi: 10.4278/0890-1171-19.2.81. [DOI] [PubMed] [Google Scholar]
- 28.Kabaroff JL, Eys MA, Schinke RJ, Eger T. The analysis of a group-mediated cognitive-behavioral corporate physical activity intervention. Work. 2013;44:423–433. doi: 10.3233/WOR-2012-1379. [DOI] [PubMed] [Google Scholar]
- 29.Artinian NT, Fletcher GF, Mozaffarian D, et al. Interventions to promote physical activity and dietary lifestyle changes for cardiovascular risk factor reduction in adults: a scientific statement from the American Heart Association. Circulation. 2010;122:406–441. doi: 10.1161/CIR.0b013e3181e8edf1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Baseline characteristics of study subjects (PP analysis)
Interventional outcomes at baseline and at 8 weeks by randomization group (PP analysis)
Variables related to exercise capacity at baseline and at 8 weeks by randomization group (PP analysis)
BP change during the study period (PP analysis)
The change of central hemodynamics during the study period (PP analysis)
Baseline types of hypertension and antihypertensive medications (ITT analysis)
Ambulatory BP at 8 weeks (ITT analysis)
The change of central hemodynamics during study period (ITT analysis)
BP change during the study period among subject with prehypertension
Comparison of post-intervention means and 95% CI for office BP and daytime ambulatory BP using an ANCOVA model adjusted for age, sex, and pre-intervention BP in the PP dataset.
Percentage of patients with controlled daytime ambulatory BP at 8 weeks according to intervention group among patients with uncontrolled daytime BP at baseline in the PP set.
Percentage of patients with controlled daytime ambulatory BP at 8 weeks according to intervention group among patients with uncontrolled daytime BP at baseline.