Abstract
Background:
Advanced cancer patients experience several physical or psychological symptoms which require palliative care for alleviation.
Purpose:
To assess the prevalence and intensity of symptoms among cancer patients receiving palliative care in a Greek hospital and to examine the association between reported symptoms and social clinical and demographic characteristics.
Material-methods:
This descriptive research was conducted during a six-month period using a convenient sample of 123 advanced cancer patients. All participants were assessed for their symptoms using the Edmonton Symptom Assessment System (ESAS) with a questionnaire covering demographic and clinical characteristics.
Results:
The mean age was 63.8± 10.8 years, with lung and breast (58.5% and 11.4%, respectively) as the most common primary cancer types. The most severe symptoms were fatigue, sleep disturbance, dyspnea, depression and anxiety. Negative correlations were revealed between age and the following symptoms: pain (r = -0.354, p = 0.001), fatigue (r = -0.280, p = 0.002), nausea (r = -0.178, p = 0.049), anorexia (r = -0.188, p = 0.038), dyspnea (r = -0.251, p = 0.005), and depression (r = -0.223, p = 0.013). Advanced breast cancer patients scored higher in pain, fatigue and dyspnea compared to those with other cancers.
Conclusions:
Hospitalized cancer patients in Greece experience several symptoms during the last months of their life. These are influenced by demographic characteristics. Appropriate interventions are strongly advised with appropriate recognition and evaluation of symptoms by health professionals.
Keywords: End stage cancer symptoms, palliative care, symptom management, cancer patients
Introduction
Cancer is one of the main causes of worldwide morbidity and mortality according to the World Health Organization (WHO) and the International Agency for Research on Cancer (IARC). It is estimated that there will be about a 70% increase in cancer-related incidents over the next two decades. In addition, cancer is the second most important cause of death globally and is responsible for nearly 1 in 6 deaths (Stewart, 2014). In Greece, cancer is the second leading cause of death following cardiovascular diseases. It is worth mentioning that there has been an increase in deaths resulting from cancer in individuals aged over 75 years, and men in Greece, as in Europe, are exhibiting higher rates of incidents than women (Bray et al., 2013; Ferlay et al., 2013)
End stage cancer patients are particularly vulnerable, as they experience a wide range of complex symptoms and problems due to the illness itself as well as the use of therapeutic approaches (Fan et al., 2007). These symptoms require interdisciplinary collaboration of a group of doctors and other health professionals of different specialties in order to be addressed (Lee, 2002). The incidence of symptoms varies depending on the type of malignancy. For practical reasons, end stage symptoms can be divided into the following four main categories: physical, psychological, social, and spiritual (Bekelman et al., 2009; Onyeka, 2010). The most frequent symptoms are fatigue, pain, lack of energy, weakness, loss of appetite, and these are reported in at least in 50% of cancer patients (Teunissen et al., 2007).
The main purpose of palliative care is the management of symptoms experienced by end stage cancer patients. According to WHO, palliative care is a healthcare approach that aims to provide relief from symptoms as well as improve quality of life (QoL) of the patients. Palliative care includes relief from pain and other distressing symptoms (Borasio, 2011). Despite the urgent need for facilities to provide palliative care, their integration to the health system varies from country to another. A study, which was conducted in 2013 regarding the provision of palliative care, found that only a few countries such as Australia, Austria, Belgium, Canada, France, Germany, Hong Kong, U.K., U.S. had advanced provision and integration of palliative care. Greece was classified among the countries that had isolated provision of palliative care along with countries such as Angola, Armenia, Bulgaria, Egypt, Estonia, and others (Lynch et al., 2013).
Despite remarkable advances in medicine, especially in cancer treatment, cancer patients continue to face many challenges and have to deal with many cancer or cancer treatment related symptoms (Delgado-Guay et al., 2008). Current studies are focusing on various aspects of those symptoms such as prevalence, intensity, relief from those symptoms, and effectiveness of interventions. Solano et al., (2006), in a systematic review, reported that there are a set of 11 symptoms with high prevalence in advanced cancer patients as well as in other chronic and life threating diseases. These are pain, depression, anxiety, confusion, fatigue, breathlessness, insomnia, nausea, constipation, diarrhea, and anorexia. The prevalence of these symptoms was found to vary between 3–29% (Diarrhea) up to 35–96% (pain). In another study, it was found that symptoms such as anorexia, fatigue, cough, dyspnea, pain, overall symptomatic distress was found to have a great effect on normal activity and global QoL of cancer patients (Kao et al., 2012). A more recent study examined the longitudinal assessment of symptoms in cancer patients in a palliative care unit. It was found that the most prevalent symptoms were pain, anorexia and constipation. Also, it was found that gender and primary cancer sites influenced the severity of symptoms (Tai et al., 2016)
There is also research that focuses more on the effectiveness of complementary intervention along with palliative care for the management of cancer related symptoms and patients’ QoL. All these studies, however, provided conflicting results, with some interventions and treatments proving to be non-effective (Bruera et al., 2003 a). Some of them improved the QoL of patients, but failed to manage or improve cancer related symptoms (Bakitas et al., 2009). While there were others that focused on patients’ participation (Bruera et al., 2003 b), implementation of palliative care consultation (Yennurajalingam et al., 2011), or early palliative referral for advanced cancer patients (Zimmermann et al., 2014). These approaches reported more efficient management of symptoms and seemed to improve the QoL of advanced cancer patients.
Although the assessment of cancer or cancer treatment related symptoms is essential to the provision of palliative care, as well as the measurement of the quality of provided care, yet sometimes it is neglected. Specific studies are being conducted in Greece are that are focusing on the psychological aspects and symptoms of cancer such as resilience, anxiety and depression (Fradelos et al., 2017; Mystakidou et al., 2004; Mystakidou et al., 2006), while others are looking into a specific reported symptom like fatigue, or a specific type of cancer like breast cancer (Lavdaniti et al., 2006) or nausea and vomiting (Lavdaniti and Tsitsis, 2014). The above reasons stimulated the researchers’ interest in investigating the phenomenon further, and they decided to study the symptoms of advanced cancer patients in hospitals.
Thus, purpose of this study is to assess the prevalence and the intensity of most frequent reporting symptoms among cancer patients receiving palliative care in hospital and to examine the association between reported symptoms and social clinical and demographic characteristics.
Materials and Methods
Participants
This study was descriptive and non-experimental. It was conducted at the general hospital of Greece, a comprehensive tertiary cancer unit located in Thessaloniki a major city of Northern Greece. In this study a convenience sample of advanced cancer patients was collected, during hospitalization. The sample consisted of 123 evaluable patients. The inclusion criteria were: patients had to have been diagnosed with advanced cancer, at least 18 years old, and a native Greek-speaking. Patients with any confusion, uncontrolled psychiatric disease, cognitive dysfunction, or any other disabling disease that could hinder their ability to answer the study questionnaires were not eligible to participate. All patients sign in and score the Edmonton Symptom Assessment System (ESAS) based on their symptoms at the time of completion. The completed ESAS scores are forwarded to the medical or nursing team for review at the patient’s appointment; the needs identified by the results guide the care provided. The survey has lasted from April to September 2016.
Procedure
The study was approved by the General Assembly of Nursing Department in Alexander Technological Education Institute of Thessaloniki, which acted as an ethics committee. A member of a research team approached all potential participants who met the inclusion criteria and introduced to the aim of the study. A confidential letter was distributed to these potential participants to inform them about the study and participants’ rights. Confidential statements were then collected from the patients who agreed to participate, following which they were given the questionnaire. A total of 130 patients were invited to participate in the study, and 123 agreed to do so (94%).
Instrument
The Edmonton Symptom Assessment System (ESAS) was implemented in this study. The ESAS is a self-report measure for assessing the intensity of nine symptoms (pain, fatigue, nausea, anxiety, depression, drowsiness, anorexia, well-being, dyspnea, and sleep disturbance) in cancer care (Bruera et al., 1991). The severity of each symptom is rated from 0 to 10, with 0 indicating that the symptom is absent and 10 describing the worst possible severity (Kang et al., 2013). The total symptom distress score (TSDS) represents the sum of all ESAS symptoms (from 0 to 100) (Zimmermann et al., 2014). Moreover, the questionnaire includes the following patients’ demographics and clinical characteristics: gender, age, marital status, living alone, occupation, insurance agency, education level, place of residence, type of cancer and comorbidities.
Statistical analysis
Descriptive statistical data were summarized as frequencies and percentages for categorical variables, means (standard deviations, SD), median and mode for symptom scores and other continuous variables such as age. Internal consistency of instrument was assessed using Cronbach’s alpha coefficient, and a value between 0.70 and 0.90 was considered adequate (Terwee et al., 2007). Data of our analysis followed the normal distribution and parametric test were performed. In order to find differences among symptoms and categorical or ordinal variables, student’s t-test and analysis of variances was realized respectively. Pearson correlation coefficient was performed to find differences among age and symptoms. A 2-tailed P value of < .05 indicated statistical significance. All statistical analyses were performed using the SPSS software
Results
Table 1 summarizes the demographic and clinical characteristics of the study population. The 123 evaluable patients had a mean age of 63.8 (S.D. 10.8) years; 65% were male. The majority of the sample (66.7%) was married and only 15.4% lived alone. Also, 39.8% of patients were retired and the same rate was private employee. Percentage of 43.9% was completed the primary school and 55.3% lived in urban area. As far as the clinical characteristics, the most common primary cancer types were lung cancer (58.5%) and breast cancer (11.4%). The majority of patients suffered from hypertension (35.8%) and diabetes mellitus (23.6%).
Table 1.
Patient Characteristics
| Number | Percentage (%) | ||
|---|---|---|---|
| Gender | Male | 80 | 65 |
| Female | 43 | 35 | |
| Mean age = 63.8 (S.D. 10.8) years | |||
| Family status | Unmarried | 18 | 14.6 |
| Married | 82 | 66.7 | |
| Divorced | 14 | 11.4 | |
| Widower | 9 | 7.3 | |
| Live alone | Yes | 19 | 15.4 |
| No | 104 | 84.6 | |
| Occupation | Unemployed | 7 | 5.7 |
| Private employee | 49 | 39.8 | |
| Public employee | 11 | 8.9 | |
| Housewife | 3 | 2.4 | |
| Retired | 49 | 39.8 | |
| Other | 4 | 3.3 | |
| Educational level | Illiterate | 6 | 4.9 |
| Primary | 85 | 69.1 | |
| Secondary | 9 | 7.3 | |
| Tertiary | 23 | 18.7 | |
The internal consistency of the ESAS was measured by calculating Cronbach alpha (Chang et al., 2000). The overall Cronbach alpha for the ESAS instrument in our sample was 0.749. Also, Cronbach’s alpha ranged from 0.705 (fatigue) to 0.741 (anxiety).
The mean score on the ESAS as a whole was 54.4, which indicates that the average response on each ESAS item was roughly 5 out of 10, demonstrating that patients with cancer in this sample generally score at the moderate of the response range (0–10, with 10 representing worse symptoms) on each item. Fatigue, sleep disturbance, dyspnea, depression and anxiety were scored ≥7 points, meaning severe symptoms (Table 2).
Table 2.
Response Frequencies for the Edmonton Symptom Assessment System
| Pain | Fatigue | Sleep disturbance | Nausea | Anorexia | Dyspnea | Depression | Anxiety | Well-being | |
|---|---|---|---|---|---|---|---|---|---|
| Mean | 4.58 | 6.74 | 5.46 | 3.73 | 4.8 | 5.43 | 8.66 | 8.54 | 5.06 |
| Median | 5 | 8 | 7 | 0 | 5 | 7 | 9 | 9 | 5 |
In the Table 3, the patients’ answers by symptoms (as percentage) are presented. The majority of patients declared worst possible severity in all symptoms except from well-being. Moreover, the half and over of our sample had severe symptoms in the following: pain, sleep disturbance, dyspnea, depression and anxiety (Figure 1).
Table 3.
Patients’ Answers by Symptoms (as Percentage)
| Score | Pain | Fatigue | Sleep disturbance | Nausea | Anorexia | Dyspnea | Depression | Anxiety | Well-being |
|---|---|---|---|---|---|---|---|---|---|
| Absent | 41.5 | 18.7 | 31.7 | 56.9 | 45.5 | 37.4 | 0.8 | 1.6 | 1.6 |
| 1 | 0.8 | ||||||||
| 2 | 1.6 | 0.8 | 6.5 | ||||||
| 3 | 0.8 | 1.6 | 17.9 | ||||||
| 4 | 1.6 | 0.8 | 17.9 | ||||||
| 5 | 11.4 | 7.3 | 11.4 | 4.9 | 4.1 | 4.1 | 8.9 | 8.1 | 19.5 |
| 6 | 5.7 | 7.3 | 2.4 | 0.8 | 1.6 | 1.6 | 1.6 | 5.7 | |
| 7 | 9.8 | 15.4 | 6.5 | 4.1 | 3.3 | 7.3 | 8.1 | 8.9 | 13.8 |
| 8 | 8.1 | 8.9 | 12.2 | 7.3 | 7.3 | 12.2 | 19.5 | 24.4 | 9.8 |
| 9 | 2.4 | 3.3 | 3.3 | 1.6 | 5.7 | 3.3 | 11.4 | 7.3 | 4.9 |
| Worst possible | 21.1 | 38.2 | 29.3 | 24.4 | 31.7 | 33.3 | 49.6 | 48 | 1.6 |
Figure 1.
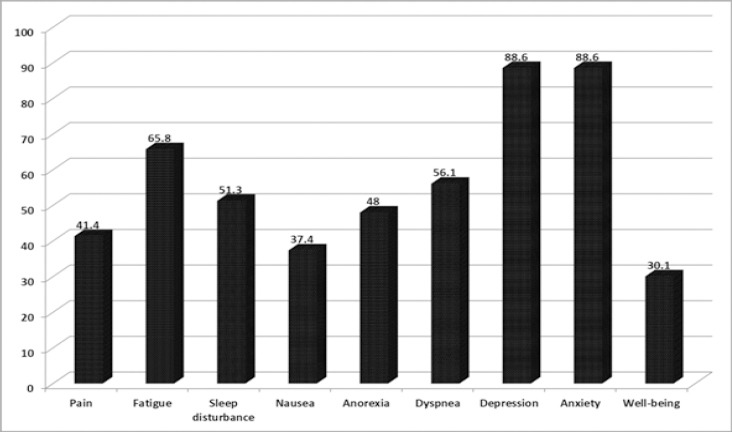
Percent of Patient Reported Severe Symptom Burden (≥7)
Statistically significant differences were found among some symptoms and demographic characteristics of the sample. Specifically, the mean value of well-being for women is 5.5 (±2.3) while for men is lower (4.7 ±2) with statistically significant difference (p=0.049). Negative correlations were revealed between age and the following symptoms: pain (r = -0.354, p = 0.001), fatigue (r = -0.280, p = 0.002), nausea (r = -0.178, p = 0.049), anorexia (r = -0.188, p = 0.038), dyspnea (r = -0.251, p = 0.005), depression (r = -0.223, p = 0.013) and total symptom distress score (r = -0.331, p = 0.001). Unmarried, married and divorced patients scored higher in fatigue than patients in widowhood (Table 4). Moreover, our findings revealed that if educational level increases then patients’ anxiety increases (table 4). Also, patients who lived in semi-urban area scored lower (3.7 ±1.5) their well-being than those who lived in rural area (5.3±2) (p =0.045).
Table 4.
Significant Symptoms by Patients’ Demographic Characteristics
| Fatigue | P value | ||
|---|---|---|---|
| Family status | Mean | S. D. | |
| Unmarried | 7.28 | 3.3 | 0.027 |
| Married | 6.8 | 3.55 | 0.021 |
| Divorced | 8 | 2.8 | 0.009 |
| Widower | 3.11 | 4.7 | Reference |
| Anxiety | |||
| Educational level | |||
| Illiterate | 5.17 | 4.49 | Reference |
| Primary | 4.73 | 4.5 | 0.017 |
| Secondary | 8.22 | 3.23 | 0.019 |
| Tertiary | 7 | 3.93 | 0.011 |
Regarding the differences among cancer and symptoms, patients with breast cancer were more likely to score higher in pain, fatigue, dyspnea and total symptom distress score compared to patients with other cancer such as pancreatic cancer, prostate cancer e.t.c. (Figure 2).
Figure 2.
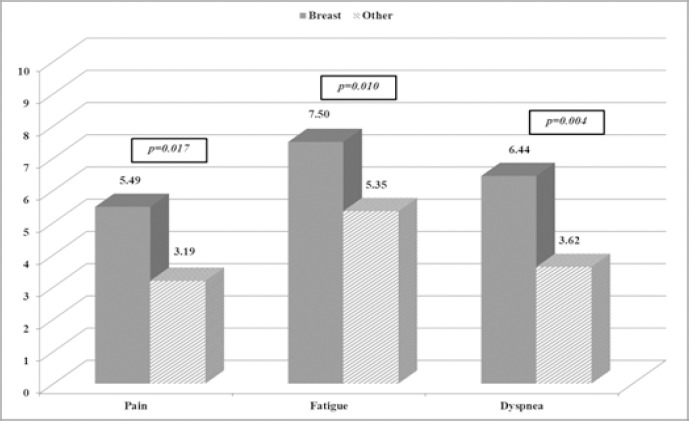
Significant Symptoms between Breast Cancer and Other Cancer
Discussion
The purpose of this study was to assess the prevalence and severity of symptoms that experience advanced hospitalized cancer patients received palliative care in northern Greece and to examine the possible relationship of those symptoms with clinical and demographic characteristics. While the symptom burden considers being moderate for the patients of our study, the majority of them are characterized by the high prevalence of depression, anxiety and fatigue.
Assessment of common symptoms during palliative care must be a key priority and can contribute to an organization’s integrated care plan. Addressing those symptoms can improve the patients’ QoL and well-being, providing them with comfort and peace. Symptom screening and assessment with the help of an appropriate instrument can help healthcare providers such as nurses and physician adequately screen, assess and manage such symptoms (Pereira et al., 2016). Brief instruments like ESAS, which was used in the current study, can help in obtaining vital information regarding cancer related symptomatology over a short period, and can help organize optimal healthcare (Chang et al., 2000).
The ESAS score of the present study can be categorized as moderate, and this is consistent with the findings of another study that assessed symptoms in advanced cancer patients and used the same scale (Follwell et al., 2009). Our study, in addition, reported higher scores in depression, anxiety, fatigue, sleep disturbance, while nausea, pain and anorexia registered lesser scores and had lower mean scores. These results are not consistent with those of Tai et al., (2016), who found that pain, anorexia, constipation were the most common symptoms, and those of Kwon et al., (2013), who reported the higher mean scores in anorexia, fatigue and drowsiness. Also, they were not consistent with the findings of a study, conducted in Canada in 2009, which reported fatigue, anorexia and pain were the most prevalent and severe symptoms (Follwell et al., 2009). This difference may be attributed to the different study population, the use of different questionnaires, and generally to differences in study design. The studies are not structured in an identical way, and hence there is a need to investigate the symptoms experienced by advanced cancer patients in Greece.
It is worth mentioning that fatigue is one of the most prevalent and severe symptoms in this study as well as the aforementioned studies, although there are differences in the prevalence of other symptoms. This is explained by the fact that fatigue is one of the most common symptoms in advanced cancer patients. (Teunissen et al., 2007; Kao et al., 2012)
Another interesting result is that anxiety and depression were present in the study population and recorded high prevalence (88.6%). The existence of these symptoms is an expected outcome because anxiety and depression are well-documented symptoms in advanced cancer patients in Greece (Mystakidou et al., 2004; Mystakidou et al., 2006) and in other recent studies across the world (Arrieta et al., 2012; Wilson et al., 2017). The result that, however, that was most surprising us was the high prevalence of these two symptoms that contrasted with the results of other studies. Lower prevalence of depression (32.9 %) and anxiety (34.1 %) was reported in non-small lung cancer patients (Arrieta et al., 2012), and the prevalence of psychiatric disorder in end stage cancer patients reached 52.2% (Wilson et al., 2017). This difference may be attributed to our assumption that ESAS cannot be considered as the appropriate tool for diagnosing depression and anxiety and cannot replace clinical interview. Undoubtedly, there is a need for further research in Greece in order to draw safe conclusions about these two symptoms among in this particular group of patients.
Furthermore, this study found that age and gender affected several symptoms. These findings are similar to the findings of other studies (Walsh et al., 2000; Tai et al., 2016). Although these studies had larger samples, the similar results once again strengthen the assumption that advanced cancer patients suffer from various physical and psychological symptoms. (Tai et al., 2016). Also, it was found that educational level increases patients’ anxiety. This is explained by the assumption that patients with advanced educational degrees are likely to focus on QoL. This is the cause for increased anxiety (Hui et al., 2012). Patients with advanced breast cancer experienced more severe pain, fatigue, dyspnea, and total symptom distress than the other advanced cancer patients. This is an expected outcome because these symptoms are the most common during the final months of life of these patients (Bien et al., 2016). On the other hand, this difference may be attributed to other factors such as breast cancer, which is the second most common form of cancer in this population, and the assumption that different primary cancer sites have different symptoms in the final months (Tai et al., 2016). There is a need for further research in Greece in order to identify the factors affecting the symptoms of advanced cancer patients.
This study has certain limitations. One of them is the use of a convenience sample, and the fact that the data collection was conducted in a single hospital in a major Greek city. Also, the correlations and comparisons between the questionnaire items and clinical, demographic characteristics had to be limited, specifically on account of the small sample. This was in contrast to the other studies, whose larger sample allowed for correlations and comparisons with the sample demographics and clinical characteristics.
In conclusion, this study confirmed the presence of symptoms such as depression, anxiety, fatigue, and sleep disturbance in hospitalized cancer patients in Greece. In addition, age and gender are associated with some symptoms, and it was also found that educational status affected anxiety. The results are very important for Greek nurses and other health professionals, with a view to recognizing and assessing symptoms in advanced cancer patients. Recognition and evaluation of these symptoms by health professionals can lead to improved continuity of care.
Funding
This study was not funded.
Conflict of Interest
The authors declare that there is no conflict of interests regarding the publication of this paper.
Acknowledgments
The authors would like to thank all patients who participated in the study.
References
- 1.Arrieta Ó, Angulo L, Núñez-Valencia C, et al. Association of depression and anxiety on quality of life, treatment adherence, and prognosis in patients with advanced non-small cell lung cancer. Ann Surg Oncol. 2012;20:1941–8. doi: 10.1245/s10434-012-2793-5. [DOI] [PubMed] [Google Scholar]
- 2.Bakitas M, Lyons K, Hegel M, et al. Effects of apalliative care intervention on clinical outcomes in patients with advanced cancer. JAMA. 2009;302:741. doi: 10.1001/jama.2009.1198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bekelman DB, Rumsfeld JS, Havranek EP, et al. Symptom burden, depression, and spiritual well-being:a comparison of heart failure and advanced cancer patients. J Gen Intern Med. 2009;24:592–8. doi: 10.1007/s11606-009-0931-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bien M. Metastatic breast cancer:understanding the symptoms. 2016. [Accessed November 7 2017]. Available at: www.healthine.com .
- 5.Borasio G. Translating the World Health Organization definition of palliative care into scientific practice. Palliat Support Care. 2011;9:1–2. doi: 10.1017/S1478951510000489. [DOI] [PubMed] [Google Scholar]
- 6.Bray F, Ren JS, Masuyer E, Ferlay J. Estimates of global cancer prevalence for 27 sites in the adult population in 2008. Int J Cancer. 2013;132:1133–45. doi: 10.1002/ijc.27711. [DOI] [PubMed] [Google Scholar]
- 7.Bruera E, Kuehn N, Miller MJ, et al. The Edmonton Symptom Assessment System (ESAS):a simple method for the assessment of palliative care patients. J Palliat Care. 1991;7:6–9. [PubMed] [Google Scholar]
- 8.Bruera E, Strasser F, Palmer J, et al. Effect of fish oil on appetite and other symptoms in patients with advanced cancer and anorexia/cachexia:A double-blind, placebo-controlled study. J Clin Oncol. 2003a;21:129–34. doi: 10.1200/JCO.2003.01.101. [DOI] [PubMed] [Google Scholar]
- 9.Bruera E, Driver L, Barnes E, et al. Patient-controlled methylphenidate for the management of fatigue in patients with advanced cancer: A preliminary report. J Clin Oncol. 2003b;21:4439–43. doi: 10.1200/JCO.2003.06.156. [DOI] [PubMed] [Google Scholar]
- 10.Chang V, Hwang S, Feuerman M. Validation of the edmonton symptom assessment scale. Cancer. 2000;88:2164–71. doi: 10.1002/(sici)1097-0142(20000501)88:9<2164::aid-cncr24>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 11.Delgado-Guay M, Parsons H, Li Z, et al. Symptom distress in advanced cancer patients with anxiety and depression in the palliative care setting. Support Care Cancer. 2008;17:573–9. doi: 10.1007/s00520-008-0529-7. [DOI] [PubMed] [Google Scholar]
- 12.Fan G, Filipczak L, Chow E. Symptom clusters in cancer patients:a review of the literature. Curr Oncol. 2007;14:173–9. doi: 10.3747/co.2007.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ferlay J, Steliarova-Foucher E, Lortet-Tieulent J, et al. Cancer incidence and mortality patterns in Europe:estimates for 40 countries in 2012. Eur J Cancer. 2013;49:1374–403. doi: 10.1016/j.ejca.2012.12.027. [DOI] [PubMed] [Google Scholar]
- 14.Follwell M, Burman D, Le L, et al. Phase II study of an outpatient palliative care intervention in patients with metastatic cancer. J Clin Oncol. 2009;27:206–13. doi: 10.1200/JCO.2008.17.7568. [DOI] [PubMed] [Google Scholar]
- 15.Fradelos EC, Papathanasiou IV, Veneti A, et al. Psychological distress and resilience in women diagnosed with breast cancer in Greece. Asian Pac J Cancer Prev. 2017;18:2545–50. doi: 10.22034/APJCP.2017.18.9.2545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hui D, Kilgore K, Fellman B, et al. Development and cross-validation of the in-hospital mortality prediction in advanced cancerpatients score:a preliminary study. J Palliat Med. 2012;15:902–9. doi: 10.1089/jpm.2011.0437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kao S, Vardy J, Harvie R, et al. Health-related quality of life and inflammatory markers in malignant pleural mesothelioma. Support Care Cancer. 2012;21:697–705. doi: 10.1007/s00520-012-1569-6. [DOI] [PubMed] [Google Scholar]
- 18.Kang JH, Kwon JH, Hui D, et al. Changes in symptom intensity among cancer patients receiving outpatient palliative care. J Pain Symptom Manage. 2013;46:652–60. doi: 10.1016/j.jpainsymman.2012.11.009. [DOI] [PubMed] [Google Scholar]
- 19.Kwon J, Nam S, Koh S, et al. Validation of the edmonton symptom assessment system in Korean patients with cancer. J Pain Symptom Manage. 2013;46:947–56. doi: 10.1016/j.jpainsymman.2013.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lavdaniti M, Patiraki E, Dafni U, et al. Prospective assessment of fatigue and health status in Greek patients with breast cancer undergoing adjuvant radiotherapy. Oncol Nurs Forum. 2006;33:603–10. doi: 10.1188/06.ONF.603-610. [DOI] [PubMed] [Google Scholar]
- 21.Lavdaniti M, Tsitsis N. Investigation of nausea and vomiting in cancer patients undergoing chemotherapy. Health Psychol Res. 2014;2:1550. doi: 10.4081/hpr.2014.1550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee DH. Approach to end of life care. Ochsner J. 2002;4:98–103. [PMC free article] [PubMed] [Google Scholar]
- 23.Lynch T, Connor S, Clark D. Mapping levels of palliative care development:a global update. J Pain Symptom Manage. 2013;45:1094–106. doi: 10.1016/j.jpainsymman.2012.05.011. [DOI] [PubMed] [Google Scholar]
- 24.Mystakidou K, Tsilika E, Parpa E, et al. The hospital anxiety and depression scale in Greek cancer patients:psychometric analyses and applicability. Support Care Cancer. 2004;12:821–5. doi: 10.1007/s00520-004-0698-y. [DOI] [PubMed] [Google Scholar]
- 25.Mystakidou K, Parpa E, Katsouda E, et al. The role of physical and psychological symptoms in desire for death:a study of terminally ill cancer patients. Psychooncology. 2006;15:355–60. doi: 10.1002/pon.972. [DOI] [PubMed] [Google Scholar]
- 26.Onyeka TC. Psychosocial issues in palliative care:a review of five cases. Indian J Pall Care. 2010;16:123–8. doi: 10.4103/0973-1075.73642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pereira J, Chasen M, Molloy S, et al. Cancer care professionals'attitudes toward systematic standardized symptom assessment and the Edmonton Symptom Assessment System after large-scale population-based implementation in Ontario, Canada. J Pain Symptom Manage. 2016;51:662–72. doi: 10.1016/j.jpainsymman.2015.11.023. [DOI] [PubMed] [Google Scholar]
- 28.Teunissen SC, Wesker W, Kruitwagen C, et al. Symptom prevalence in patients with incurable cancer:a systematic review. J Pain Symptom Manage. 2007;34:94–104. doi: 10.1016/j.jpainsymman.2006.10.015. [DOI] [PubMed] [Google Scholar]
- 29.Terwee CB, Bot SDM, de Boer MR, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 2007;60:34–42. doi: 10.1016/j.jclinepi.2006.03.012. [DOI] [PubMed] [Google Scholar]
- 30.Solano J, Gomes B, Higginson I. A comparison of symptom prevalence in far advanced cancer, AIDS, heart disease, chronic obstructive pulmonary disease and renal disease. J Pain Symptom Manage. 2006;31:58–69. doi: 10.1016/j.jpainsymman.2005.06.007. [DOI] [PubMed] [Google Scholar]
- 31.Stewart B, Wild CP. World Cancer Report 2014. Lyon: IARC Press; 2014. pp. 297–301. [Google Scholar]
- 32.Tai S, Lee C, Wu C, et al. Symptom severity of patients with advanced cancer in palliative care unit:longitudinal assessments of symptoms improvement. BMC Palliat Care. 2016;15:32. doi: 10.1186/s12904-016-0105-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yennurajalingam S, Urbauer D, Casper K, et al. Impact of a palliative care consultation team on cancer-related symptoms in advanced cancer patients referred to an outpatient supportive care clinic. J Pain Symptom Manage. 2011;41:49–56. doi: 10.1016/j.jpainsymman.2010.03.017. [DOI] [PubMed] [Google Scholar]
- 34.Walsh D, Donnelly S, Rybicki L. The symptoms of advanced cancer:relationship to age, gender, and performance status in 1,000 patients. Support Care Cancer. 2000;8:175–9. doi: 10.1007/s005200050281. [DOI] [PubMed] [Google Scholar]
- 35.Wilson K, Dalgleish T, Chochinov H, et al. Mental disorders and the desire for death in patients receiving palliative care for cancer. BMJ Support Palliat Care. 2016;6:170–7. doi: 10.1136/bmjspcare-2013-000604. [DOI] [PubMed] [Google Scholar]
- 36.Zimmermann C, Swami N, Krzyzanowska M, et al. Early palliative care for patients with advanced cancer:a cluster-randomised controlled trial. Lancet. 2014;383:1721–30. doi: 10.1016/S0140-6736(13)62416-2. [DOI] [PubMed] [Google Scholar]


