Abstract
Background:
Cervical cancer is the second most common cancer in women worldwide; early detection can play a key role in reducing the associated morbidity. The objective of this study was to systematically assess the effects of educational interventions on cervical cancer screening (CCS) behavior of women.
Methods:
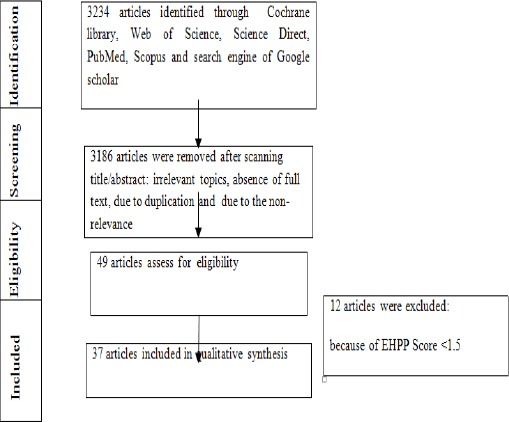
In this review the Cochrane library, Web of Science, Science Direct, PubMed, Scopus and search engine of Google scholar were searched for all interventional studies (trails, pre- and post-test or quasi-experimental) published in 2000-2017 for a systematic review, The search was based on the following keywords: cervix cancer, uterine cervical neoplasms, screening, prevention and control, Papanicolaou Test, pap test, pap smear, education, intervention, systematic review. Due to the heterogeneity of the data, a qualitative analysis was performed.
Results:
Thirty seven articles with 15,658 female participants in different parts of world were included in the review. About three quarters of the articles covered behavior change interventions. About one fourth of the articles were based on health education methods. The heath belief model is the most popular used framework for cervical cancer screening interventions. The results of our study showed that different health education methods (such as calls, mailed postcards, mother/daughter education. consultation sessions, picture books, videos, PowerPoint slides, small group discussions, educational brochures, radio broadcast education, lecture presentations, tailored counseling and a fact sheet, Self-learning package, face-to- face interviews and etc) are effective in modifying cervical cancer screening behavior of women.
Conclusions:
Our results showed that the different interventions and health behavior change frameworks provide an effective base for cervical cancer prevention. Heath providers can chose educational methods based on the particular client situations.
Keywords: Cervical cancer, screening, systematic review, prevention, Pap test, cervical neoplasm
Introduction
Cervical Cancer is one of the most common malignancies in women (Nwankwo et al., 2011). It is estimated that in all over the worldwide about 1.4 million women are living with Cervical cancer (second most after the breast cancer), the cervical cancer is the second most common cancer in women worldwide, also it is the leading cause of cancer death in some developing countries (Organization, 2015).
Screening can reduce both the mortality and incidence of cervical cancer (Mishra et al., 2011). The World Health Organization knows cervical cancer as a preventable disease in women (Bleggi et al., 2003). The treatment of cervical cancer is less effective because the sign and symptom of this cancer does not appear until the advance stages. The cause of cervical cancer is the Human Papilloma Virus (HPV) (Group, 1995). The epidemiologic risk factors of this cancer are onset of coitus in young ages, history of sexually transmitted disease, larger number of sexual partners, use of contraceptive methods, history of smoking, parity and chronic immunosuppression (Partridge et al., 2014). Now in the developed countries CCS is carried out by cytological examination of a the Pap test (Hanaa, 2014; Koliopoulos et al., 2010). Women’s decisions regarding CCS are affected by many factors including: sociocultural factors (Johnsonet al., 2008), cancer awareness (Austoker et al., 2009), knowledge (Nwankwo et al., 2011), attitudes (Reis et al., 2012) and women’s beliefs (Esin et al., 2011), lack of encouragement (Fernández-Esquer and Cardenas-Turanzas, 2004), providers’ attitudes (McFarland, 2003), recommendation from health professionals (Chan et al., 2016) and etc.
The world health education mentioned that “Health education is an exchange of information with the purpose of increasing awareness and knowledge about how to keep healthy and prevent diseases (such as cervical cancer), including information about resources that are available and the benefits of accessing services” (Health, Diseases, and Promotion, 2006). Evidence showed that Education by raising awareness, improving accessibility to services, increasing individuals’ efficacy and empowering over future choices can enhance the demand for preventative health services (Sabates and Feinstein, 2006).
Systematic reviews aimed to generate new knowledge and provide a rigorously reviewed summary of relevant literature on a specific question and synthesize the results of these literature (Wallace et al., 2014), because of the importance of the CCS, and lack of overall articles on effectiveness of educational interventions in this issue, this study was carried out to systematically assess the effect of Educational Interventions to improve cervical cancer screening (CCS) behavior of women.
Materials and Methods
Search Strategy
This study is a systematic review conducted to determine the effect of educational interventions on CCS behavior of women, in this study we assess all published articles (Trails, pre- and post-test design or quasi-experimental) from July 2000 to May 2017 in English language. We searched from Cochrane library, Web of Science, Science Direct, PubMed, Scopus and search engine of Google scholar. The search was based on the following search terms: cervix cancer, Uterine Cervical Neoplasms, screening, prevention and control, Papanicolaou test, Pap test, Pap smear, education, intervention, systematic review.
Criteria for considering studies for this review Selection of studies
Two authors reviewed the eligibility of interventional design studies and also evaluated the risk of bias and the data for included articles such as information on the study population, country of origin, the number of participants in each group, study design, aim, measurement tools, the type of educational intervention, and adverse effect of each intervention and main results of study was extracted.
Types of Participants
All educational intervention studies (Trails, pre- and post-test or quasi-experimental) with inclusion criteria of women without a previous cervix cancer diagnosis.
Types of Interventions
All intervention studies (Trails, pre and post-test or quasi-experimental) involving educational intervention versus usual care or versus without educational intervention.
Types of Comparator/control
No intervention or usual care.
Types of Outcome measures
Educational interventions based on different health models adverse outcomes related to false positive findings of symptoms (such as decreased quality of life/increased anxiety and any of the adverse outcomes) assessed by any validated scale.
Risk of Bias
The EPHPP is a generic tool used to evaluate a variety of intervention study designs. This tool assesses six domains: selection bias, study design, confounders, blinding, data collection method and withdrawals/dropouts. According Guidelines for this tool each domain is rated as weak (1 point), moderate (2 points) and strong (3 points) and domain scores are averaged to provide the total score. The maximum total score per study is 3.00. Based on their total score, quality of studies is rated as weak (1.00–1.50), moderate (1.51–2.50) or strong (2.51–3.00) (Armijo-Olivo et al., 2012; Deeks et al., 2003; Thomas et al., 2004). Search in databases was performed by two researchers; the abstracts were first assessed and then some articles underwent final assessment according to EPHPP and inclusion criteria (including published from 2000 through May 2017 included an intervention based) and Exclusion criteria (Full-text not accessible, Studies not demonstrating a clear research methodology).
Data analysis
In this review due to the heterogeneity of the data, qualitative analysis was used.
Results
In this review study thirty seven articles with 15658 female participants included. 38.8 % of studies were from Asia, 13.8% from Europe, 33.3% from Americas and 13.8% from Africa. Table 1 showed the Characteristics of included studies.
Table 1.
Characteristics of Health Belief Model and Trans Theoretical Model and Theory of Reasoned Action based Studies
| study | Design/sample/model | location | Intervention | Outcome | quality rating EPHPP | model |
|---|---|---|---|---|---|---|
| Kocaöz et al (2017) (Champion et al., 2006) | semi-experimental n=342 | Turkey | 20 min theoretical and practical education about cervix cancer | In this study in the 6 months after the education 33.6% of women had a pap smear test and there were significantly increasing in pap smear benefits motivation subscale and significantly decreasing in pap smear barriers subscale. | Moderate | |
| Shobeiri et al, (2016)(Shobeiri et al., 2016) | Quasi-Experimental N=330 | Iran | The intervention included two 45-60 minutes consultation sessions in the form of consulting. The control group did not receive any training | There was significant increase in all variables of HBM and mean score of knowledge in intervention group (P<0.001). | Moderate | |
| Daryani et al,(2015) | quasi-experimental | Iran | Intervention group received education sessions for 1.5 hours was held in practical displays, films, lectures and questions & answers | The result showed that there was significantly difference in women’s practice and in between two groups (p<0.05). Also in the intervention group. before and after intervention In case group there was a significant difference in terms of HBM constructs (P<0.0001), | Moderate | |
| (Daryani et al., 2015) | the intervention (N = 60) or control (N = 60) | 2)control group received no intervention | ||||
| Taghi Pour shoorijeh et al,(2015) (shoorijeh Leila et al.) | quasi-experimental Experimental group N=60/ Control group N=60 | Iran | Educational slides | after educational intervention there was significantly increase in mean scores of perceived susceptibility and severity, perceived benefits and barriers, self-efficacy and cues to action in internal and external dimensions in intervention group. | Moderate | |
| Hanaa, A.A et al (2014) (Hanaa, 2014) | Experimental design 314 married female students intervention group =157 and CON =157 | Egypt | Self -learning package about CCS | Regarding knowledge dimension there was high difference between two group (p<0.05). In the intervention group the mean scores of perceived susceptibility and severity Of cervical cancer and perceived benefits of early detection and HPV vaccination were significantly higher than CON. | Moderate | |
| Guvenc et al , (2013) (Guvenc et al., 2013) | quasi-experimental n= 2,500 women | Turkey | 1-stage nursing intervention was distribution of the study’s educational brochure, by apartment building doormen 2-stage nursing intervention (telephone interviews) 3-stage nursing intervention (face-to- face interviews) | The result showed that Of the 144 who did not have Pap test after telephone interviews, 54 were then interviewed face-to-face, and 37.0% decided to accept free Pap test. A total of 668 women had accepted free Pap test uptake by the end of the intervention. | Moderate | Health belief model |
| Bebis et al , (2012)(Bebis et al., 2012) | RCT Intervention group=75 CON=75 | Turkey | Educational conference (45 minutes) about Cervical cancer and Papanicolaou test in study group | There was statistically significant between two group in the score of knowledge (p<0.05) and There were statistically lower levels of susceptibility to cervical cancer score , lower levels of perceived benefit and lower levels of perceived barriers to Papanicolaou test score (P < 0.05). | Moderate | |
| Pirzadeh & Amidi Mazaheri et al (2012) (Pirzadeh & Mazaheri, 2012) | quasi-experimental 70 women Intervention group = 35 CON=35 | Iran | educational session lasted 45–60 min about cervical cancer and its screening | The results showed that after intervention HBM variables includes (perceived susceptibility and severity, perceived benefits, and barriers) had significantly difference between two groups(P < 0.001). | Moderate | |
| Karimy et al,(2011) | quasi-experimental | Iran | educational program in three sessions based on Health Belief Model | The results showed that in intervention group the mean score of self-efficacy, susceptibility, severity, benefit and barriers perceived and performance of pap smear test were significantly increased (p<0.05). | Moderate | |
| (Karimy, Gallali, Niknami, Aminshokravi, & Tavafian, 2012) | 60 participants each: the experiment (intervention) group and the control | |||||
| Shojaeizadeh et al,(2011) (Shojaeizadeh et al., 2011) | quasi-experimental n=70 | Iran | The participants were divided in to seven 10- member groups. For each group, 2-hour training session was held twice. In each session, various training methods were used (lectures, question, and answer, showing slides and group discussion). | There was significantly increase in scores of perceived susceptibility, severity, benefits, and barriers and participants’ knowledge | Moderate | |
| Park et al, (2005) | non-equivalent control group post-test | Korea | The core contents of the program reflected the results of a previous qualitative study conducted through focus groups to explore cognitive and affective attributes that women experience related to Pap test | Participants in the experimental group had significantly higher scores on perceived benefits of Pap tests, knowledge of cervical cancer, lower scores on procedural and cognitive barriers to testing(p<0.05). Results showed the Improvement in elf-efficacy, strong intention to have the pap test and advanced stages of behavior adoption (p < .01). | Strong | |
| (Park et al., 2005) | Intervention group = 48 CON=48 | |||||
| Jibaja-Weiss et al, (2003) | RCT | Houston | 1) personalized form (PF) letter( containing generic cancer information | The results showed 1 year after the intervention that personalized form-letter group was significantly more likely to have undergone a Pap testing (p<0.05). | strong | Health Belief Model |
| (Jibaja-Weiss et al., 2003) | N=1574 Teilored letter=524 personalized form (PF) letter=460 con=499 | 2)personalized tailored (PT) letter containing minimally tailored individualized risk factor information about breast and cervical cancer screening | ||||
| Krok-Schoen et al, (2016) (Krok-Schoen et al., 2016) | randomized controlled trial 90 women | USA | received all components for the intervention (both visits, both phone calls, and 4 mailed postcards) | At visit 1 woman in the preparation and contemplation stages reported more barriers than women in the precontemplation stage. At visit 2, the number of reported barriers declined, and a higher number of barriers were reported by those n the early stages of change. | strong | |
| Hou et al, (2005) (Hou, 2005) | pretest–posttest design n = 424 | Taiwan | phone educational intervention | Result showed that at the end of the program women in the intervention group were 2.31 more likely and in contemplation stage4.18 were more likely to receive a CCS . | Moderate | Trans theoretical Model |
| Abdullah et al , (2013) (Abdullah & Su, 2013) | cluster randomized controlled trial intervention group =199 and CON =199 | Malaysia | intervention group: A call–recall program The control group received usual care from the existing program. | Results showed that In both groups, pre-contemplation stage was had the highest proportion of changes in all stages. An intervention group showed two times more in the action stage than control group (OR= 2.44) At 24 weeks. | Strong | |
| Coronado Interis et al, (2016)`(Coronado Interis et al., 2015) | pre-test/post-test design n=225 | Jamaica | Intervention sessions were conducted one-to-one and in groups of up to 30 women. Presentations lasted approximately 15 min for both methods of delivery | 6 month after intervention statistically significant increases in the percentage of questions correctly answered and in participants’ intention to CCS.40.7% of women screened for cervical cancer | Moderate | TTM/HBM |
| Maxwell et al,(2003)(Maxwell et al., 2003) | randomized trial n=444 intervention=213 CON=234 | Los Angeles County | Small group discussion intervention with Educational intervention sessions by physicians and nurses. | The results showed that screening rates in study group were moderate increased. | Moderate | Health Belief Model Theory of Reasoned Action/Planned Behavior Pre- cede Model |
RCT, Randomized Clinical Trials
Figure 1 showed the Flowchart of articles selection. About three forth of articles are based on behavior change interventions. twelve article utilized a HBM base and, 1 article used HBM and TTM bases, 1 used HBM and TPB, 1 used Preceed, Proced model bases, 3 used TTM, 2 SCT, 2 used PMT (1). About one fourth of articles are based on Health education methods without framework theory based. The result of our study showed that different Health education methods (such as calls, mailed postcards, mother/daughter education. Consultation sessions, video, PowerPoint slide, small group discussion, educational brochure, radio broadcasts education, lecture presentations, tailored counseling and a fact sheet, Self -learning package, face-to- face interviews and …) are effective in CCS behavior of women. Table 1 showed the characteristics of Health belief model and Trans theoretical Model based studies. Table 2 showed the characteristics of included studies based on Protection Motivation Theory, PRECEDE-PROCEED MODEL. Table 3 showed the characteristics of included studies based on Health education methods without framework theory based.
Figure 1.
Flowchart of Articles Selection
Table 2.
Characteristics of Included Studies Based on Protection Motivation Theory, Precede-Proceed Model
| study | Design/sample/model | location | Intervention | Outcome | quality rating EPHPP | model |
|---|---|---|---|---|---|---|
| Ghahremani et al,(2015) | quasi-experimental | Iran | Training classes were conducted for the health volunteers through three 120-minute sessions using PowerPoint slide show and educational pamphlets and booklets. | In the intervention group the mean scores of perceived vulnerability, severity, fear, response-costs, intention , and self-efficacy statistically significant increased(P<0.001). but there was no significant difference regarding response efficacy after the intervention (P=0.06). The rate of uptake Pap test increased by about 62.9% among the intervention group. | Moderate | Protection Motivation Theory(PMT) |
| (Ghahremani et al., 2016) | Intervention group (n=210)/Control - group (n=210) | |||||
| Dehdari et al,(2014) (Dehdari et al., 2014) | quasi-randomized controlled trial intervention group =97 and CON =103 | Iran | The educational intervention includes four 60-minute sessions during a four-week period. At the end of last session, an instructional booklet was given to the participants. | In the intervention group the mean scores of self-efficacy and intention variables were significantly higher than CON (p<0.05). But the result showed that there were No significant differences in the perceived severity, response cost, response efficacy, and fear. In the intervention group Higher percent of women had obtained first and second Pap smear compared to the CON. | Moderate | |
| Katz et al, (2007) (Katz et al., 2007) | randomized trial Intervention group = 453 CON=444 | North Carolina | The intervention group received an educational program about mammography delivered by a health advisor, and the CON received a physician letter/brochure about Pap tests. | The rate of CCS significantly increased in both group | Strong | Precede-Proceed Model |
| Peterson et al, (2012) (Peterson et al., 2012) | RCT Intervention group = 80 CON=76 | Oregon | The education program include 90-120 minute small-group workshop / structured telephone support for 6 months (with five monthly calls attempted, Control group participants received general health promotion | The intervention group statistically significant received more Pap tests than the CON (intervention 61%, control 27%, n = 71). | strong | |
| Tomas Nuno et al (2011) (Nuno et al., 2011) | RCT Intervention group (n = 183)/Usual care group (n = 188) | U.S.–Mexico | The educational intervention trained by promotora in 2-h group session | the intervention group 1.5 times more likely to report having pap testing although this was not statistically significant (95% CI = 0.9–2.6). | Strong | social cognitive theory |
RCT, Randomized Clinical Trials
Table 3.
Characteristics of Included Studies Based on Health Education Methods Without Framework Theory Based
| study | Design/sample/model | location | Intervention | Outcome | quality rating EPHPP |
|---|---|---|---|---|---|
| Gana et al, (2016)`(Gana et al., 2016) | quasi-experimental the intervention (N = 93) or control (N = 93 | Nigeria | During the intervention phase, health education was provided on cervical cancer, Pap smear test with emphasis on its benefit and procedure and on proximate health institutions that provide such services to the intervention group. | After intervention there was a statistically significant difference in cervical cancer awareness (p<0.05) , but the rate of pap testing marginally increased (p>05) | Moderate |
| Thompson et al, (2016) (Thompson et al., 2017) | RCT video delivered to participants’ homes; n =150 video plus a home-based educational session; n = 146 usual care; n=147 | Latinas | 1)the control arm (usual care) did not receive any intervention 2) Participants in the low-intensity intervention (video) arm were mailed a culturally appropriate Spanish-language video based on a curriculum developed with community-based 3) The high-intensity arm received a promotoraled educational session in their home. | The results showed that pap testing in the high- intensity arm Significantly higher than low-intensity arm and the usual-care arm (P<.001) | Strong |
| Patricia et al, (2016) (Obulaney et al., 2016) | quasi-experimental design N = 41 | US | mall group, mother/daughter educational intervention | The result of this study showed that knowledge-based test item Significantly improved (p<0.05),the mothers hpv vaccine intention significantly change (p<0.005) | Moderate |
| Rosser et al,(2015) | the intervention (N = 207) or control (N = 212) | Kenya | The educational intervention includes a brief health talk on cervical cancer. | The result showed that the mean score of Knowledge in the intervention group significantly increased (p<0.05) however there was no significantly increase in uptake of pap screening | Strong |
| Abiodun et al,(2014) | Quasi-experimental | Nigeria | Health education intervention used a movie on cervical cancer and screening/ The intervention group received health education on cervical cancer and screening while the control group received education on breast cancer and screening. The control group also received health education on cervical cancer and screening after the post intervention study. | The result showed that Health education had significant effect on the awareness of CCS (p < 0.0001). Also in the intervention group The mean score of knowledge, perception and uptake of cervical screening were improved. | |
| (Abiodun et al., 2014) | Experimental group N=350 Control group N=350 | Moderate | |||
| Lai et al (2014) (Gahremani nasab et al., 2014) | quasi-experimental n=200 (100 in each group) | Taiwan | Intervention group: Six-hour discussion sessions were offered either with Facebook-assisted or in-person discussions after class. | In the intervention group there were significantly greater improvement in knowledge and attitudes score after intervention. | Moderate |
| Choi (2013) (Moodi et al., 2011) | pre-test/post-test design n=57 intervention group =30 and CON =27 | korea | 4-week program ( in 50-minute sessions once a week) The control group received no intervention | The results of this study showed that the cervical cancer preventive program was effective in increasing perceived susceptibility, knowledge and CCS. | strong |
| Marek et al , (2012) (Marek et al., 2012) | educational intervention study Experimental group / n=89 Control group/n=128 | Baranya County, Hungary | The educational intervention was undertaken by a trained health educator (first author) during the students’ regular classes | The results showed that awareness about cervical cancer, causal relationship between cervical cancer and HPV and perception of HPV vaccination , health-related beliefs significantly increased in intervention group (p<0.05) | Moderate |
| Love et al , (2012) | quasi-experimental | Thailand | the intervention group received Entertainment-education video | No uniform differences were showed between two groups. In Both educational Knowledge and attitudes score increased. | Moderate |
| (Love & Tanjasiri, 2012) | intervention group / n=263 CON=253 | (video) and the control group received brochure | |||
| Brien et al, (2010) (O’Brien et al., 2010) | randomized trial Intervention group = 60 CON=60 | Philadelphia | The educational intervention consisted of two workshops (3-hour, 4 and 10 women in each group) which were led by a pair of promotoras. | There were statistically significant differences in Pap smear test (65% vs. 36%), knowledge about cervical cancer (5.4 vs. 3.5), and self-efficacy (4.7 vs. 4.0) between the two group . | Moderate |
| Wright et al, (2010) (Wright et al., 2010) | quasi-experimental Intervention group = 175 CON=175 | Nigeria | the intervention group received sessions of community- based educational messages | Three was low level of cervical cancer Knowledge at baseline (15% versus 6.9% CON). in the intervention/experimental group there were Significant increase in proportions on awareness of cervical cancer (61.7%). | Moderate |
| study | Design/sample/model | location | Intervention | Outcome | quality rating EPHPP |
| Choe et al (2009) (Guvenc et al., 2011) | randomized trial n=130 deaf women | California | Intervention group received cervical cancer education video | In the intervention group by viewing of the in-depth video, obtained significantly more cancer knowledge than the CON. | Moderate |
| Perkins et al, (2007) (Perkins et al., 2007) | pre-/ post-test design control groups n = 124, n = 243; intervention group n = 233 | Honduras | radio broadcasts education and lecture presentations | The radio broadcast increased the proportion of knowledge of women about cervical cancer. And also improved pap test behavior of women | Moderate |
| Holloway et al (2003) (Moodi et al., 2011) | RCT N=1890 intervention=772 CON=1118 | Wales | a brief specific counseling session | In the intervention arm at the 5year follow-up, fewer women had attended for CCS sooner than recommended recall. | Moderate |
| Taylor et al, (2002) (Taylor et al., 2002) | RCT High-intensity intervention=161 Low-intensity intervention=161 CON=160 | North America | 1) The CON received usual care. 2)The outreach worker intervention group received an educational brochure, tailored counseling and a fact sheet 3) The direct mail intervention group received materials by mail | 39% of women in outreach group, 25% in the direct mail group and 15% in the CON reported Pap testing in the interval between randomization and follow-up data collection (P<.001 for outreach worker vs CON, P = .03 for direct mail vs CON, and P = .02 for outreach worker vs direct mail). | strong |
Behavior change based interventions Health belief model (HBM)
Kocaöz et al., (2017) and Champion et al., (2006) in their study reported that professional education program have positive effect on pap test behavior of women. Shobeiri and Roshanaei, (2016) reported that HBM-based education had a key role on changing women’s beliefs about CCS. Taghi Pour shoorijeh et al, (2015) reported that HBM based intervention can enhance the awareness and uptake of pap test. Daryani et al., (2015) showed that education based on HBM was effective in enhancing women’s performance about CCS. Guvenc and Yenen, (2013) reported that three-stage nursing intervention could help to increase participation of Turkish women in Pap testing. Bebis et al., (2012) reported that HBM educational based model significantly increased the knowledge, perceived susceptibility cervical cancer and barriers of pap testing. Pirzadeh and Mazaheri, (2012) reported that HBM based educational intervention promote CCS behavior of women. Shojaeizadeh et al., (2011) concluded that HBM based health education can enhance women’s knowledge and health beliefs and CCS behaviors. In Karimy et al., (2011) study theories and models of changing of individuals’ behavior is effective programs on CCS. The results of Park and Chung, (2005) study showed that cognition-emotion focused program have a role on women’s decisions to have Pap smear. The results Jibaja-Weiss et al., (2003) showed that one year after the intervention that personalized form-letter group was significantly more likely to have undergone a Pap testing.
Social cognitive theory (SCT)
Peterson et al., (2010) reported that among mobility impairments women PATHS intervention enhanced the pap testing. Nuno et al., (2011) reported that a promotora-based education enhace the CCS behavior of Hispanic women.
Trans Theoretical Model (TTM)
In Krok-Schoen et al., (2016) study showed during the intervention 63% of the Ohio Appalachian women had forward stage movement. Hou et al., (2005) reported that at the end of the program women in the intervention group were 2.31 more likely and in contemplation stage 4.18 were more likely to receive a CCS. In Abdullah and Su, (2013) study results showed that in both groups, pre-contemplation stage was had the highest proportion of changes in all stages.
Precede-Proceed Model
Katz et al., (2007) reported that implementation of ROSE project (which was designed to improve breast cancer screening in Carolina) significantly increased The rate of CCS in both group of participants.
Protection Motivation Theory (PMT)
In the Dehdari et al., (2014) study the results showed that in the intervention group the mean scores of self-efficacy and intention variables were significantly higher than CON (p<0.05); But the result showed that there were No significant differences in the perceived severity, response cost, response efficacy, and fear. In the intervention group higher percent of women had obtained first and second Pap smear compared to the CON. The result of Ghahremani et al., (2015) study showed that educational based on PMT is effective in pap testing among participants. PMT was introduced by Rogers as a predictive theoretical model of health behaviors. This theory proposes that two appraisal processes, i.e. threat and coping appraisal, occur when the individual receives threatening information. Threat appraisal is associated with a maladaptive response. It involves the perceived severity of a threatening event and personal vulnerability to the proposed threat (Dehdari et al., 2014).
Combined model
Maxwell et al., (2003) reported that small group community-based education base on Health Belief Model, the Theory of Reasoned Action/Planned Behavior and the Precede Model only effective in increasing CCS among participants who had very low baseline CCS rates. Coronado et al., (2016) reported that the knowledge and intention to CCS of participants based on HBM/TTM theory education intervention significantly increased.
Health education methods
In Gana et al., (2016) educational program increased cervical cancer and Pap test awareness however, even after intervention the uptake of Pap testing remained low. In Thompson et al., (2016) study results showed that in-home, promotora-led educational intervention improving CCS. in Patricia et al., (2016) study the awareness and intention of mothers were changed after their daughter education (Obulaney et al., 2016). Rosser et al., (2015) reported that the educational intervention could help to increase knowledge and awareness about CCS, however it did not result in higher CCS rates. Hanaa et al., (2014) reported that after self-learning educational package the perceive and knowledge of intervention group increased and the 53.5% of the intervention group compared with 5.7% of the CON intent to do pap test. The result Abiodun et al., (2014) showed that health education had significant effect on the awareness of CCS (p < 0.0001). Also in the intervention group the mean score of knowledge, perception and uptake of cervical screening were improved. Lai et al., (2014) and Gahremani-nasab et al., (2014) reported that School-based education had positive effect on cervical cancer prevention. Choi, (2013) and Moodi et al., (2011) in their study reported that education program with picture book, lecture and discussion significantly improved the knowledge and CCS of Korean women. Marek et al., (2012) reported that, school-based, educational intervention effective in improving knowledge, beliefs and attitudes. Love and Tanjasiri, (2012) reported that entertainment-education video and brochure could help to increasing knowledge and attitudes. In O’Brien et al., (2010) study promotora-led intervention significantly improved pap test using rate also could help to increase self-efficacy and cervical cancer knowledge of women. Wright et al., (2010) reported that Community Education improved the cervical cancer awareness of women. Choe et al., (2009) and Guvenc et al., (2011) reported that education by video in deaf women improved the cervical cancer knowledge. Perkins et al., (2007) reported that community-based educational intervention with lecture presentations and radio broadcasts increase CCS behavior of women. Holloway et al., (2003) and Moodi et al., (2011) reported that the intervention had a substantial benefit for CCS. In Taylor et al., (2002) study 39% of women in outreach group, 25% in the direct mail group and 15% in the CON reported Pap testing in the interval between randomization and follow-up data collection.
Discussion
Cervical cancer is a common women cancer our study systematically assess the effect of Educational Interventions to improve cervical cancer screening (CCS) behavior of women. The result of our study showed that educational interventions based on health behavior change theories could help to improve CCS behavior of women in different part of the world. Theories of health behavior change indicates that increasing self-regulation skills and developing knowledge and beliefs lead to the change of health behavior (Ryan, 2009). The result of a review showed that behavioral interventions example mailed or telephone reminders increased pap test usage by 18.8% (Yabroff et al., 2003). Roncancio et al, (2013) reported that Theory of Planned Behavior Model is a useful model for understanding CCS intentions. Coronado et al., (2015) reported that theory-based education intervention lead to increasing knowledge and promoting awareness and increasing screening rates.
The result of our study showed that different health education methods (such as calls, mailed postcards, mother/daughter education, consultation sessions, video, PowerPoint slide, small group discussion, educational brochure, radio broadcasts education, lecture presentations, tailored counseling and a fact sheet, Self -learning package, face-to- face interviews and …) are effective in CCS behavior of women. The evidence show that an educational intervention can help to reduce barriers of CCS and subsequently can help to increase CCS rate (Coronado et al., 2015). Soares and Silva, (2016) in their review about interventions that facilitate adherence to Pap smear exam reported that use of case manager; media outreach work; telephone call; invitation letter increase women’s knowledge about CCS. Lu et al., (2012) in their systematic review about interventions to increase breast and cervical cancer screening uptake in Asian women reported that the combination workplace-based group education programs with mobile screening services and attending screening are effective in promotion breast and cervical cancer screening uptake. Roy et al., (2008) in the systematic review reported that use of client reminders, one-on-one education and small media improve cervical cancer screening behavior of women (Baron et al., 2008). Sabatino et al., (2012) in their systematic review reported that client reminders and one-on-one education and reducing structural barriers improve the CCS behavior (Spadea et al., 2010). In another systematic review reported that community demand for screening increased with education by: Mass media, Client reminders and recall, Client incentives, Laws to increase screening, Reducing structural barriers, Reducing client out-of-pocket costs, Provider assessment and feedback (Baron et al., 2008). Evidence show that organized screening programs can improve the cervical cancer screening (Spadea et al., 2010).
Limitation
Our study did not include the ‘grey’ literature so Future research need to survey this literature.
In conclusion, different interventional and health behavior change framework models are effective method in cervical cancer prevention. Heath providers can chose educational method based on the client situations.
Compliance with Ethical Standards
Funding Information: Funding information is not applicable / No funding was received.
Disclosure of potential conflicts of interest
The authors declare that they have no conflict of interest.
Informed consent
For this review study Informed consent is not required.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors
References
- 1.Abdullah F, Su TT. Applying the transtheoretical model to evaluate the effect of a call–recall program in enhancing Pap smear practice:A cluster randomized trial. Prev Med. 2013;57:83–6. doi: 10.1016/j.ypmed.2013.02.001. [DOI] [PubMed] [Google Scholar]
- 2.Abiodun OA, Olu-Abiodun OO, Sotunsa JO, Oluwole FA. Impact of health education intervention on knowledge and perception of cervical cancer and cervical screening uptake among adult women in rural communities in Nigeria. BMC Public Health. 2014;14:814. doi: 10.1186/1471-2458-14-814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Armijo OS, Stiles R, Hagen NA, Biondo PD, Cummings GG. Assessment of study quality for systematic reviews:a comparison of the cochrane collaboration risk of bias tool and the effective public health practice project quality assessment tool:methodological research. J Eval Clin Pract. 2012;18:12–8. doi: 10.1111/j.1365-2753.2010.01516.x. [DOI] [PubMed] [Google Scholar]
- 4.Austoker J, Bankhead C, Forbes LJL, et al. Interventions to promote cancer awareness and early presentation:systematic review. Br J Cancer. 2009;101:31–9. doi: 10.1038/sj.bjc.6605388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baron RC, Rimer BK, Breslow RA, et al. Client-directed interventions to increase community demand for breast, cervical, and colorectal cancer screening:a systematic review. Am J Prev Med. 2008;35:34–55. doi: 10.1016/j.amepre.2008.04.002. [DOI] [PubMed] [Google Scholar]
- 6.Baron RC, Rimer BK, Coates RJ, et al. Methods for conducting systematic reviews of evidence on effectiveness and economic efficiency of interventions to increase screening for breast, cervical, and colorectal cancers. Am J Prev Med. 2008;35:26–33. doi: 10.1016/j.amepre.2008.04.003. [DOI] [PubMed] [Google Scholar]
- 7.Bebis HR, Nesrin Y, Tulay BD, Unal AB, Serkan D. Effect of health education about cervical cancer and papanicolaou testing on the behavior, knowledge, and beliefs of Turkish women. Int J Gynecol Cancer. 2012;22:1407–12. doi: 10.1097/IGC.0b013e318263f04c. [DOI] [PubMed] [Google Scholar]
- 8.Bleggi T, Luiz F, Werner B, et al. Cervical cancer screening program of Paraná:Cost-effective model in a developing country. Diagn Cytopathol. 2003;29:49–54. doi: 10.1002/dc.10269. [DOI] [PubMed] [Google Scholar]
- 9.Champion VL, Springston JK, Zollinger TW, et al. Comparison of three interventions to increase mammography screening in low income African American women. Cancer Detect Prev. 2006;30:535–44. doi: 10.1016/j.cdp.2006.10.003. [DOI] [PubMed] [Google Scholar]
- 10.Chan CWH, Choi KC, Wong RS, et al. Examining the cervical screening behaviour of women aged 50 or above and its predicting factors:A population-based survey. Int J Environ Res Public Health. 2016;13:1195. doi: 10.3390/ijerph13121195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Coronado I, Evelyn A, Chidinma P, Aung M, Jolly PE. Increasing cervical cancer awareness and screening in Jamaica:Effectiveness of a theory-based educational intervention. Int J Environ Res Public Health. 2015;13:53. doi: 10.3390/ijerph13010053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Daryani S, Shojaeezadeh D, Yazdani Charati J, Batebi A, Naghibi A. The effect of education based on health belief model on women's practice about pap smear test. J Cancer Policy. 2015;8:51–6. [Google Scholar]
- 13.Deeks JJ, Dinnes J, D'amico R, et al. Evaluating non-randomised intervention studies. Health Technol Assess. 2003;7:1–173. doi: 10.3310/hta7270. [DOI] [PubMed] [Google Scholar]
- 14.Dehdari T, Hassani L, Hajizadeh E, et al. Effects of an educational intervention based on the protection motivation theory and implementation intentions on first and second pap test practice in Iran. Asian Pac J Cancer Prev. 2014;15:7257–61. doi: 10.7314/apjcp.2014.15.17.7257. [DOI] [PubMed] [Google Scholar]
- 15.Esin MN, Bulduk S, Ardic A. Beliefs about cervical cancer screening among Turkish married women. J Cancer Edu. 2011;26:510–15. doi: 10.1007/s13187-011-0198-y. [DOI] [PubMed] [Google Scholar]
- 16.Fernández E, Maria E, Cardenas TM. Cervical cancer screening among Latinas recently immigrated to the United States. Prev Med. 2004;38:529–35. doi: 10.1016/j.ypmed.2003.12.009. [DOI] [PubMed] [Google Scholar]
- 17.Gahremani-Nasab P, Shahnazi M, Farshbaf-Khalili A, Ganbari S. Factors related to cervical cancer screening among women referring to health centers in Tabriz, Iran 2012. Iran J Obstet Gynecol Infertil. 2014;16:15–24. [Google Scholar]
- 18.Gana GJ, Oche MO, Ango JT, Raji MO, Okafoagu NC. Effect of an educational program on awareness of cervical cancer and uptake of Pap smear among market women in Niger State, North Central Nigeria. J Public Health Epidemiol. 2016;8:211–19. [Google Scholar]
- 19.Ghahremani L, Harami ZK, Kaveh MH, Keshavarzi S. Investigation of the role of training health volunteers in promoting pap smear test use among Iranian women based on the protection motivation theory. Asian Pac J Cancer Prev. 2016;17:1157–62. [PubMed] [Google Scholar]
- 20.Group IARC Working. Human papilloma viruses, IARC Monograph on the evaluation of carcinogenic risks to humans. Lyon, France: International Agency for Research on Cancer; 1995. p. 65. [Google Scholar]
- 21.Guvenc G, Akyu A, Açikel CH. Health belief model scale for cervical cancer and Pap smear test:psychometric testing. J Adv Nurs. 2011;67:428–37. doi: 10.1111/j.1365-2648.2010.05450.x. [DOI] [PubMed] [Google Scholar]
- 22.Guvenc G, Akyuz A, Yenen MC. Effectiveness of nursing interventions to increase pap smear test screening. Res Nurs Health. 2013;36:146–57. doi: 10.1002/nur.21526. [DOI] [PubMed] [Google Scholar]
- 23.Hanaa AA Y, EL Sayed HA. Effect of self learning package based on health belief model on cervical cancer prevention among female university students. J Nurs Health Sci. 2014;3:77–88. [Google Scholar]
- 24.Health World health organization reproductive, diseases, world health organization chronic, and promotion, health. Comprehensive cervical cancer control:a guide to essential practice: World Health Organization. 2006 [PubMed] [Google Scholar]
- 25.Hou Su I. Stage of adoption and impact of direct-mail communications with and without phone intervention on Chinese women's cervical smear screening behavior. Prev Med. 2005;41:749–56. doi: 10.1016/j.ypmed.2005.07.011. [DOI] [PubMed] [Google Scholar]
- 26.Jibaja W, Maria L, Volk RJ, et al. Tailored messages for breast and cervical cancer screening of low-income and minority women using medical records data. Patient Educ Couns. 2003;50:123–32. doi: 10.1016/s0738-3991(02)00119-2. [DOI] [PubMed] [Google Scholar]
- 27.Johnson CE, Mues KE, Mayne SL, Kiblawi AN. Cervical cancer screening among immigrants and ethnic minorities:a systematic review using the health belief model. J Low Genit Tract Dis. 2008;12:232–41. doi: 10.1097/LGT.0b013e31815d8d88. [DOI] [PubMed] [Google Scholar]
- 28.Karimy M, Gallali M, Niknami SH, Aminshokravi F, Tavafian SS. The effect of health education program based on health belief model on the performance of Pap smear test among women referring to health care centers in Zarandieh. J Jahrom Univ Med Sci. 2012;10:53–9. [Google Scholar]
- 29.Katz ML, Tatum CM, Degraffinreid CR, Dickinson S, Paskett ED. Do cervical cancer screening rates increase in association with an intervention designed to increase mammography usage? J Womens Health. 2007;16:24–35. doi: 10.1089/jwh.2006.0071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Koliopoulos G, Nyaga VN, Santesso N, et al. Cytology versus HPV testing for cervical cancer screening in the general population. Cochrane Database Syst Rev. 2010 doi: 10.1002/14651858.CD008587.pub2. doi:10.1002/14651858CD008587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Krok S, Jessica L, Oliveri JM, et al. Evaluating the stage of change model to a cervical cancer screening intervention among Ohio Appalachian women. Women Health. 2016;56:468–86. doi: 10.1080/03630242.2015.1101736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Love GD, Tanjasiri SP. Using entertainment-education to promote cervical cancer screening in Thai women. J Cancer Edu. 2012;27:585–90. doi: 10.1007/s13187-012-0369-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lu M, Moritz S, Lorenzetti D, et al. A systematic review of interventions to increase breast and cervical cancer screening uptake among Asian women. BMC Public Health. 2012;12:413. doi: 10.1186/1471-2458-12-413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Marek E, Dergez T, Rebek-Nagy G, et al. Effect of an educational intervention on Hungarian adolescents'awareness, beliefs and attitudes on the prevention of cervical cancer. Vaccine. 2012;30:6824–32. doi: 10.1016/j.vaccine.2012.09.012. [DOI] [PubMed] [Google Scholar]
- 35.Maxwell AE, Bastani R, Vida P, Warda US. Results of a randomized trial to increase breast and cervical cancer screening among Filipino American women. Prev Med. 2003;37:102–9. doi: 10.1016/s0091-7435(03)00088-4. [DOI] [PubMed] [Google Scholar]
- 36.Mc Farland DM. Cervical cancer and pap smear screening in Botswana:knowledge and perceptions. Int Nurs Rev. 2003;50:167–75. doi: 10.1046/j.1466-7657.2003.00195.x. [DOI] [PubMed] [Google Scholar]
- 37.Mishra GA, Pimple SA, Shastri SS. An overview of prevention and early detection of cervical cancers. Indian Indian J Med Paediatr Oncol. 2011;32:125. doi: 10.4103/0971-5851.92808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Moodi MM, Baladi M, Sharifirad GR, et al. Evaluation of breast self-examination program using Health Belief Model in female students. J Isfahan Univ Med Sci. 2011;16:316. [PMC free article] [PubMed] [Google Scholar]
- 39.Nuno T, Martinez ME, Harris R, Garcia F. A promotora-administered group education intervention to promote breast and cervical cancer screening in a rural community along the U.S.-Mexico border:a randomized controlled trial. Cancer Causes Control. 2011;22:367–74. doi: 10.1007/s10552-010-9705-4. [DOI] [PubMed] [Google Scholar]
- 40.Nwankwo KC, Aniebue UU, Aguwa EN, Anarado AN, Agunwah E. Knowledge attitudes and practices of cervical cancer screening among urban and rural Nigerian women:a call for education and mass screening. Eur J Cancer Care. 2011;20:362–7. doi: 10.1111/j.1365-2354.2009.01175.x. [DOI] [PubMed] [Google Scholar]
- 41.O'Brien MJ, Halbert CH, Bixby R, et al. Community health worker intervention to decrease cervical cancer disparities in Hispanic women. J Gen Intern Med. 2010;25:1186–92. doi: 10.1007/s11606-010-1434-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Obulaney PA, Gilliland I, Cassells H. Increasing cervical cancer and human papillomavirus prevention knowledge and HPV vaccine uptake through mother/daughter education. J Community Health Res. 2016;33:54–67. doi: 10.1080/07370016.2016.1120595. [DOI] [PubMed] [Google Scholar]
- 43.Organization World Health. Strategic framework for the comprehensive control of cancer cervix in South-East Asia Region. 2015 [Google Scholar]
- 44.Park S, Chang SB, Chung CW. Effects of a cognition-emotion focused program to increase public participation in Papanicolaou smear screening. Public Health Nurs. 2005;22:289–98. doi: 10.1111/j.0737-1209.2005.220404.x. [DOI] [PubMed] [Google Scholar]
- 45.Partridge EE, Abu-Rustum N, Giuliano A, et al. Cervical cancer screening. J Natl Compr Canc Netw. 2014;12:333–41. doi: 10.6004/jnccn.2014.0035. [DOI] [PubMed] [Google Scholar]
- 46.Perkins RB, Langrish S, Stern LJ, Simon CJ. A community-based education program about cervical cancer improves knowledge and screening behavior in Honduran women. Rev Panam Salud Publica. 2007;22:187–93. doi: 10.1590/s1020-49892007000800005. [DOI] [PubMed] [Google Scholar]
- 47.Peterson JJ, Suzuki R, Walsh ES, Buckley DI, Krahn GL. Improving cancer screening among women with mobility impairments:Randomized controlled trial of a participatory workshop intervention. Am J Health Promot. 2012;26:212–16. doi: 10.4278/ajhp.100701-ARB-226. [DOI] [PubMed] [Google Scholar]
- 48.Pirzadeh AM, Maryam A. The effect of education on women's practice based on the health belief model about pap smear test. Int J Prev Med. 2012;3:585–90. [PMC free article] [PubMed] [Google Scholar]
- 49.Reis N, Bebis H, Kose S, et al. Knowledge, behavior and beliefs related to cervical cancer and screening among Turkish women. Asian Pac J Cancer Prev. 2012;13:1463–70. doi: 10.7314/apjcp.2012.13.4.1463. [DOI] [PubMed] [Google Scholar]
- 50.Roncancio AM, Ward KK, Fernandez ME. Understanding cervical cancer screening intentions among Latinas using an expanded theory of planned behavior model. Int J Behav Med. 2013;39:66–72. doi: 10.1080/08964289.2013.799452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rosser JI, Njoroge B, Huchko MJ. Changing knowledge, attitudes, and behaviors regarding cervical cancer screening:The effects of an educational intervention in rural Kenya. Patient Educ Couns. 2015;98:884–9. doi: 10.1016/j.pec.2015.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ryan P. Integrated theory of health behavior change:background and intervention development. Clin Nurse Spec. 2009;23:161. doi: 10.1097/NUR.0b013e3181a42373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sabates R, Feinstein L. The role of education in the uptake of preventative health care:the case of cervical screening in Britain. Soc Sci Med. 2006;62:2998–3010. doi: 10.1016/j.socscimed.2005.11.032. [DOI] [PubMed] [Google Scholar]
- 54.Shobeiri F, Javad MT, Parsa P, Roshanaei G. Effects of group training based on the health belief model on knowledge and behavior regarding the pap smear test in Iranian women:a quasi-experimental study. Asian Pac J Cancer Prev. 2016;17:2871–6. [PubMed] [Google Scholar]
- 55.Shojaeizadeh D, Hashemi SZ, Moeini B, Poorolajal J. The effect of educational program on increasing cervical cancer screening behavior among women in Hamadan, Iran:Applying health belief model. J Res Health Sci. 2011;11:20–5. [PubMed] [Google Scholar]
- 56.shoorijeh L, Taghi-Pour S, Abedini LH, Ghanbarnejad A. The impact of educational interventions based on the health belief model (Hbm) pap smear test in women referred to health centers of Bandar Abbas. I JABER. 2015;13:3579–90. [Google Scholar]
- 57.Soares MBO, Silva SRd. Interventions that facilitate adherence to Pap smear exam:integrative review. Rev Bras Enferm. 2016;69:404–14. doi: 10.1590/0034-7167.2016690226i. [DOI] [PubMed] [Google Scholar]
- 58.Spadea T, Bellini S, Kunst A, Stirbu I, Costa G. The impact of interventions to improve attendance in female cancer screening among lower socioeconomic groups:a review. Prev Medi. 2010;50:159–64. doi: 10.1016/j.ypmed.2010.01.007. [DOI] [PubMed] [Google Scholar]
- 59.Taylor VM, Hislop TG, Jackson JC, et al. A randomized controlled trial of interventions to promote cervical cancer screening among Chinese women in North America. J Nat Cancer Inst. 2002;94:670–7. doi: 10.1093/jnci/94.9.670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Thomas BH, Ciliska D, Dobbins M, Micucci S. A process for systematically reviewing the literature:providing the research evidence for public health nursing interventions. Worldviews Evid Based Nurs. 2004;1:176–84. doi: 10.1111/j.1524-475X.2004.04006.x. [DOI] [PubMed] [Google Scholar]
- 61.Thompson B, Carosso EA, Jhingan E, et al. Results of a randomized controlled trial to increase cervical cancer screening among rural Latinas. Cancer. 2017;123:666–74. doi: 10.1002/cncr.30399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wallace J, Byrne C, Clarke M. Improving the uptake of systematic reviews:a systematic review of intervention effectiveness and relevance. BMJ Open. 2014;4:e005834. doi: 10.1136/bmjopen-2014-005834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wright KO, Kuyinu YA, Faduyile FA. Community education on cervical cancer amongst market women in an urban area of Lagos, Nigeria. Asian Pac J Cancer Prev. 2010;11:137–40. [PubMed] [Google Scholar]
- 64.Yabroff KR, Mangan P, Mandelblatt J. Effectiveness of interventions to increase Papanicolaou smear use. J Am Board Fam Pract. 2003;16:188–203. doi: 10.3122/jabfm.16.3.188. [DOI] [PubMed] [Google Scholar]


