Abstract
Background:
In women, breast cancer accounts for 30 percent of all cancers and it is the second leading cause of mortality. Mammography is considered an effective procedure to detect early breast cancer recommended by World Health Organization. This study was aimed to evaluate breast cancer screening determinants in women referred to health centers of Urmia for mammography in 2017.
Materials and Methods:
In this descriptive-analytic cross-sectional study, 348 women referred to health centers of Urmia were selected using multistage sampling. Data were collected using a standard questionnaire for mammography screening determinants, with a checklist including demographic characteristics, family, social and economic factors and midwifery background. Analysis was with SPSS software version 20for descriptive and inferential statistic tests, P<0.05 being considered significant.
Results:
The proportion performing mammography was 12%. Significant relationships were noted with income, menopause status, a history of breast cancer in close relatives, beliefs, inaccessibility, knowledge, cues to action, emotions, self-care, and life priorities (P<0.05). There were no significant links with age at marriage, first age of delivery, number of children, duration of breastfeeding, status of residency, education, marital status, occupation, history of breastfeeding, and previous breast problems (P>0.05).
Conclusions:
The findings of this study showed that the status of breast cancer screening in participating women was not satisfactory. Therefore, promotion of screening methods by health policy makers in Iran is necessary and given that reliance solely on education is not sufficient, it is essential to pay attention to barriers and eliminate them.
Keywords: Screening tests, breast cancer, mammography
Introduction
Nowadays, cancer is one of the most important health problems in the world (Siegel et al., 2015). Breast cancer is the most common diagnosed cancer among women (DeSantis et al., 2014), so that 23% of newly diagnosed cases of cancer are breast cancer (Jemal et al., 2011). According to the Iranian Cancer Institute, 24.4% of all cancers assigned to breast cancer among Iranian women (Harirchi et al., 2011). One out eight women are likely to suffer from this malignancy during their lifetime and more than one million and one hundred thousand women annually involve with breast cancer in the world (Anderson, 2006). The five-year survival rate among newly diagnosed women with breast cancer is 89% in the United States (Morse et al., 2014). In contrast, the treatment rate of breast cancer in low-income countries is estimated to be less than 40% (Coleman et al., 2008). Also, the development age of breast cancer in Iran is 10 years younger than developed countries, which 70% are diagnosed in the advanced stage leading to early death (Rafiemanesh et al., 2016).
Cancer screening tests play a major role in reduction of cancer-related mortality (Dündar et al., 2006). The purpose of screening programs is to diagnose the disease after it begins and before it can lead to clinical symptoms (Khaleghnezhad and Khaleghnezhad, 2008). An appropriate way to detect early and timely breast cancer including understanding early signs and symptoms, participating in screening for breast cancer, such as breast self-examination and periodic screening by physicians, midwives and mammography performers. According to the American Cancer Society’s recommendation, breast self-examination, clinical breast examinations and mammography are three effective methods for secondary prevention of breast cancer (Khani et al., 2008).
Mammography is currently the most important screening method for breast cancer in the world (Hersch et al., 2013). The mammography’s sensitivity to diagnose mammary gland is 80-85% (Hatefnia et al., 2010), and although screening with mammography has limitations such as high false-positive results, but it remains the most effective method for early detection of breast cancer in an unpredictable stage (Friedewald et al., 2014). In breast cancer screening program, it is recommended that at the age of 40 years, a basic mammography be performed and, if there is no problem, be repeated every two years. If a family member has breast cancer, starting a mammography is recommended 5 years earlier than usual program (Nojomi et al., 2014).
Research shows that people’s knowledge, attitudes and believes about cancer can have widespread effects on participation, prevention activities and early detection, as well as decisions about treatment (Kwok et al., 2010; Sessa et al., 2008). Health believes are concepts and ideas that a person accepts as a fact, and health behaviors are the result of these believes (Abbas Zadeh et al., 2011). Although, early detection of breast cancer is effective in the survival rate, but many women still do not carry out screening tests (Regan and Durvasula, 2008). Often, there is a difference between the recommendations and the actual use of mammography (Griva et al., 2011). In western countries, due to the use of these methods among the majority of women, the mortality rate has been greatly reduced (Ries et al., 2006). Unfortunately, these methods are still not widely used by most physicians and women in most of the treatment centers in developing countries (Khani, et al., 2008; Lu, 1995). In the study of Alam et al. in Saudi Arabia showed that knowledge of 82% of women about the benefits of breast self-examination was high and 61% of women had high knowledge about mammography, but less than half (41.2%) had breast self-examination and only 18.2% had a non-diagnostic mammography (Alam, 2006). Various studies have shown that knowledge and attitude about breast cancer screening methods and the availability of such services in the health care system provide a series of challenges for early diagnosis and treatment of breast cancer (Assefa, 2011; Sullivan and Chiarelli, 2009; Odusanya, 2001).
Factors related to the screening of women’s common cancers have been studied very limited in Iran, especially in Urmia. Therefore, the necessity to reflect on this problem in order to promote breast cancer control is necessary and, as well as the specificity of mammography in early diagnosis of breast cancer, the prevention role in the death, the importance of reproductive health as human rights and the consideration of women as vulnerable groups in this view, encouraging women to perform screening tests for breast cancer is necessary. This encouragement requires a major change in their behavioral patterns and this change was affected by various factors such as personal, socioeconomic and family risk factors. Therefore, this study was conducted to determine the determinants of breast cancer screening with mammography in women referred to health centers in Urmia.
Materials and Methods
This descriptive-analytic cross-sectional study conducted on 348 women reffered health centers in Urmia city based on their social, economic and cultural status. Then, 26 health centers were classified as high level according to the socioeconomic and cultural status, 19 health centers as moderate level according to the socioeconomic and cultural status, and 20 health centers as low level. In this study, ten health centers in Urmia were randomly selected through lottery at three high, moderate and low levels of socioeconomic and cultural status. Then, four centers were randomly selected from the high level, three centers from the moderate level and three centers were from the low level. The number of each cluster was selected according to the population covered by the relevant regions and centers, and 70% of the samples (269 samples) were from urban health centers and 30% of samples (115 samples) were selected from rural health centers. Inclusion criteria were included age of 30-60, having read and write literacy and ability of verbal communication. The sample size was calculated 348 using the following formula (1):
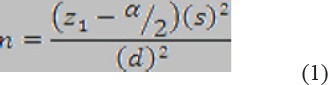
And according to standard deviation of cannas Kwok et al. (2016) (Kwok et al., 2016) equals to 0.29, where confidence interval (CI) of 95% and estimating error (d) of 0.1 and Z shows standard normal distribution. The data collection tool was a standard questionnaire for breast cancer screening with mammography which its validity and reliability was determined by Moghadam Tabrizi et al. (1396), and an information form including 19 questions about demographic characteristics, socioeconomic, family factors and midwifery risk factors. The questionnaire has 34 items and 7 factors that the related question of knowledge factor with correct answer scores 1 and in the absence of the answer or the wrong answer scores zero, 6 other factors score based on the Likert scale (completely agree, agree, I have no idea, disagree, completely disagree).
The first factor is “believes” with 7 questions (score range: 7-35), the second factor “accessibility” with 6 questions (score range: 6-30), the third factor “knowledge” with 3 questions, the fourth factor “ cue to action” with 5 questions (score range: 5 -25), the fifth factor was “emotions” with 4 questions (score range: 4-20), factor 6 “Self-care” with 4 questions (score range: 4-20) and factor 7 “ lack of priorities in life “ with 5 questions (score range: 5-25). The questionnaire has 7 factors of beliefs, accessbility, knowledge, cue to action, emotions, self-care and life priorities. The Cronbach’s alpha coefficient of the questionnaire was 0.78 and the internal group correlation coefficient was 0.91 in two measurements with two weeks interval (Nourizadeh et al., 2017).
The objectives of the study were explained to all participants and all of them accepted to participate and were assured of the confidentiality of their individual information as well as the voluntary nature of participating in the study to leave freely this study.
Demographic characteristics and family, social factors (age, place of residence, educational level, marital status), economic status (occupation, income, household size), risk factors (history of breast cancer, history of cancer in first degree relatives, history of breastfeeding, menopause, etc. were also extracted from the information form. Finally, the data were analyzed using SPSS software version 20, and descriptive and inferential statistic tests (chi-square and independent t-test) were used. P<0.05 was considered significance.
Results
The results showed that the mean age of the subjects was 43.25 ± 5.36. The marriage age of the participants and the number of the participants were 21.26 ± 2.74 and 2.88 ± 1.34, respectively. The age of the first delivery was 22.92 ± 2.80 and the average time of breastfeeding was 5.8 ± 1.76 months, and the mean age of menopause was 47.76 ± 1.80 (Table 1).
Table 1.
Quantitative Demographic Characteristics in Women Participating in This Study
| Qualitative variable | Mean± SD |
|---|---|
| Age | 43.25±5.36 |
| Age of marriage | 21.26±2.74 |
| Number of child | 2.88±1.34 |
| Age of first delivery | 22.90±2.80 |
| Duration of breastfeeding | 5.88±1.76 |
| Age of menopause | 47.76±1.70 |
The majority of participants (70%) were residents of urban area. Regarding the level of education, 45.1% of them had diploma and 4.9% of them were illiterate. Most of the subjects (66.3%) were married During the analysis of midwifery history, it was shown that 68.5% of the subjects had a history of breastfeding, and the majority of subjects (69.5%) did not have menopause. Thirty percent of subjects who had a problem in their breast had referred to a doctor regardless of their type of problem, while 20% of the subjects had avoided referral to the doctor, despite the feeling of a problem in their breast. Breast pain was experienced as the most common problem by 57.8% of participants. The history of breast cancer in the first-degree relatives was reported by 17% of the subjects. In this study, 12% of subjects never had mammography, and 88% had at least one mammography, while doctors contributed as the main source of information and encouragement of screening (Table 2).
Table 2.
Qualitative demographic characteristics in women participating in this study
| Variable | Frequency (Percent) | Variable | Frequency (Percent) | ||
|---|---|---|---|---|---|
| Place of residence | Urban | 269 (70) | History of breast problem | Yes with reference to the doctor | 115 (29.9) |
| Rural | 115 (30) | Yes without reference to the doctor | 77 (20.1) | ||
| Level of education | Illiterate | 19 (4.9) | No without history of problem | 192 (50) | |
| Under diploma | 134 (34.9) | Type of experienced problem | Breast pain | 111 (57.8) | |
| Diploma | 173 (45.1) | Breast benign disease | 60 (31.3) | ||
| College | 58 (15.1) | Breast malignant Disease | 18 (9.4) | ||
| Marital status | Single | 108 (28) | Others | 3 (1.6) | |
| Married | 256 (66.3) | History of breast problems in close relatives | Yes | 65 (16.9) | |
| Divorced | 8 (2.1) | No | 319 (82.6) | ||
| Widow | 12 (3.1) | History of mammography | Yes | 46 (12) | |
| Occupation | Housekeeper | 268 (69.8) | No | 338 (88) | |
| Employee | 116 (30.2) | Source of information and encouragement of screening | Midwiferies of health centers | 12 (26.1) | |
| History of breastfeeding | Yes | 263 (68.5) | Doctor | 16 (34.8) | |
| No | 121 (31.5) | Media | 5 (10.9) | ||
| History of menopause | Yes | 117 (30.5) | Books and magazines | 1 (2.2) | |
| No | 267 (69.5) | Patient person | 3 (6.5) | ||
| Economic status | Less than enough | 95 (34.7) | Web and virtual space | 5 (10.9) | |
| Moderate | 174 (45.3) | Friends | 3 (6.5) | ||
| More than enough | 115 (29.9) | In-person training | 1 (2.2) |
Regarding the effective factors on the performing mammography in women participating in this study, there was a significant relationship between the determinants of screening with mammography including believes, knowledge, cue to action, emotions, self-care, life priorities (P < 0.001) and inaccessibility (P= 0.006). Also, there was a significant relationship between menopausal status and performing mammography (P = 0.01) and between the history of previous breast problems and performing mammography (P < 0.001). There was a significant relationship between income status and performing mammography (P = 0.03) (Table 3).
Table 3.
Facotrs Affecting Mammography in Women Participating in This Study
| Variables | Mammography | |
|---|---|---|
| T | P-Value | |
| Age | 1.53 | 0.12 |
| Age of marriage | -1.53 | 0.12 |
| Age of first delivery | -1.22 | 0.22 |
| Number of child | 0.12 | 0.9 |
| Breastfeeding time | -0.36 | 0.71 |
| Age of menopause | -1.19 | 0.23 |
| Believes | -17 | P<0.001 |
| Inaccessibility | -9.96 | 0.006 |
| Knowledge (question 1) | 7.99 | P<0.001 |
| Knowledge (question 2) | 9.87 | P<0.001 |
| Knowledge (question 3) | 13.35 | P<0.001 |
| Cue to action | 9.44 | P<0.001 |
| Emotions | -16.25 | P<0.001 |
| Self-care | 7.76 | P<0.001 |
| Life priority | -15.52 | P<0.001 |
| Residence status | - | 0.88 |
| Education status | - | 0.96 |
| Marital status | - | 0.4 |
| Occupation status | - | 0.16 |
| History of breastfeeding | - | 0.61 |
| Menopause status | - | 0.01 |
| Income status | - | 0.02 |
| Insurance status | - | 0.25 |
| History of breast problems in past | - | 0.72 |
| Type of breast problem | - | 0.62 |
| History of breast problems in close relatives | - | P<0.001 |
Discussion
The results of the present study showed that only 12% of women performed mammography, and approximately 20% of them avoided referral to the doctor after feeling of breast problems, and 88% of participants never had mammographyin their lifetime. In the study of Tavakolian et al., (2015) less than 18% of women had mammography, while more than half of the participants never reffered to the doctor for examination, and 82 % of paricipants had not mammography (Tavakolian et al., 2015). In the study of Okobia in Nigeria, breast cancer screening behaviors were not performed in none of the participants (Okobia et al., 2006) Also, the study of Heidari et al., (2008) in Zahedan, Farshbaf et al., (2009) in Tabriz and Petro-Nustus, and Mikhail (2002) in Jordan were consistent with the present study While Eisinger et al., (2008) in France showed that 92.5% of women aged 50-74 years had at least one mammography, the reason for the difference was likely related to the age groups of study, so that participants were in the ages of 40-75 years, In this range, the majority of women refer to mammography, while women in our study were in the ages of 30- 60 years.
In this study, the physician’s advice was identified as the strongest source of information and encouragement for performing mammography. In the study of Farshbaf et al., (2009) more than half of those who performed mammography were encouraged by gyncologists. On the other hand, a study of Vazifeshenas et al., (2007) confirmed the poor performance of midwives working in health centers for breast screening. In the present study, the performance of midwives and health providers was not desirable in performing mammography, while one of the roles of midwives is to encourage all women to perform breast self-examination and follow screening recommendations (Moghadam, 1998).
In our study, kowledge was related to mammography as an personal factor and mammography was observed in people with high level of knowledge. In the study of Dundar et al., (2006) and Hurris et al., (2003) there was a positive correlation between knowledge and benefits of screening behaviors, and those who do not participate in breast screening tests are not more likely informed with the benefits and importance of screening tests and mammography which are consistent with the results of our study.
In studying the socioeconomic level of the participants in the study, there was no relationship between the education and the occupation of women with mammography. This finding was consistent with the study of Farshbaf et al., (2009) and SalimiPormehr et al., (2010), while there was a significant relationship between women’s education and occupation with breast self-examination in these studies.
Also, the present study showed that the economic status of individuals was related to performing mammography; the study of Farshbaf et al., (2006), Abedian et al., (2006) and Yücel et al., (2005) showed that high level and better economic status increse breast screening and mammography costs are one of the most important barriers for performing mammography.
The present study showed that there was a significant relationship between the history of cancer in first degree relatives and performing mammography. A study conducted by Lee-Lin et al., (2007) and Heidari et al., (2008) reported that the strongest companion factor for performing mammography and breast self-examination was history of breast cancer in a family. The esults of present study were inconsistwnt with the study of Salemi etal. Its cause can be seen in the difference between the percentage of familial history of cancer in this study, so that, SalimiPormehr et al., (2010) reported a history of cancer in relatives up to 1.7% and in our study was 26%. In the present study, there was no significant relationship between the risk factors for breast cancer including the history of breast cancer and the age of the first delivery, history of breastfeeding and the number of children with breast cancer screening tests.
Regarding the history of breast problems in a person and performing mammography, the results of the present study were consistent with the study of SalimiPormehr et al., (2010) because showed that clinical examination and mammography were related to the history of benign diseases. Perhaps the reason for this inconsistency is that in the current study, half of the subjects had a history of breast problem and breast pain, while in the study of SalimiPormehr et al., (2010) less than 5% of the subjects had previous breast problems. It seems that due to the report of breast pain as the most common problem in mammary glands, the lack of perceived susceptibility does not affect screening behaviors (Hatefnia and Niknami, 2013). Also, in this study women involving with menopause had more mammography, meaning that there was a significant relationship between menopause and mammography, which was consistent with the results of Tavakolian et al., (2015). which showed that breast self-examination in young age group (less than 30 years) and performing mammography with menopause were more compare to other age groups (Tavakolian et al., 2015).
Regarding breast cancer screening determinants, the results of this study showed that there was a significant relationship between women’s health believes and mammography. The findings of the studies conducted by Laporta et al., (2017) and Abedian et al., (2006) revealed that the majority of participants believed that breast self-examination was sufficient to find breast problems and performing mammograms is completely unnecessary, such believes can endanger the health of women in any society, so providing information about the benefits of mammography and the importance and accuracy of early diagnosis of breast cancer is necessary, so believes of individuals are one of the main determinants of one’s behavior health.
In the present study, there was a significant relationship between inaccessability including difficulty in taking turns, expensive costs, far distance and lack of appropriate insurance, lack of knowledge about mammography centers, crowded or inadequate centers and performing mammography. This conclusion was consistent with the study by Keshavarz et al., (2012) because the high cost of examinations and mammography were the most common cause. Also, in the study of Farshbaf et al., (2009) spending too much time in centers was recognized as an important reason for not performing breast cancer screening tests in women.
In the study of Tavakolian et al., (2015) and Qaed Amini et al., (2007) the geographical factors and far distances between home and breast screening centers were important factors influencing mammography. Several studies have been conducted on the impact of financial variables on access to health services. In the study of Kaufman et al., (2006) patients who pay their treatment form theirselve pocket have more likely tendency to cancel their surgery more than those who were insured and supported with governmental insurence. Therefore, if governmental -private sponsorship be created in community, access to healthcare services will be increased.
In this study, there was a significant relationship between cue to action and mammography. As explained earlier, the recommendation of the health team is the most stimulant for referring patients to mammography and other breast cancer screening tests (Jones et al., 2014). Due to the tendency of individuals to access information from the internet and cyberspace and the possibility of access to incorrect and invalid information published in such spaces, social media must declare the importance of early detection of breast cancer and mammography as the best available test for cancer detection. Unfortunately, according to the results of the present study, the media was not considered in terms of information sources.
The present study showed that there was a signifcant relationship between emotion and mammography. The results of Fang et al., (2007), Tejeda et al., (2009); and Farmer et al., (2007); Reported that the fear of the probable occurrence of cancerous tumors was the most important barrier for performing mammography (Farmer et al., 2007; Tejeda et al., 2009; Zheng et al., 2006), as well as fear of pain and a feeling of shame and embarrassment during the examination, fear of death and fear of negative emotions affect the mammography (Keshavarz et al., 2012; Stoll et al., 2015).
This study showed that there was a significant relationship between self-care and mammography. A study have shown that people who have higher levels of perceived health, in other words, have higher health motivation, are more involved in self-care activities (Wang et al., 2004).
The most important self-care behaviors include healthy dietary behaviors, proper physical activity and accountability in terms of health status, so that these behaviors are recognized as the most important strategy to prevent non-communicable diseases, especially breast cancer (Azadbakht et al., 2014). There are three important and influential factors in adopting or not adopting self-care behaviors, such as mammography, which include personal, behavioral and social factors (Shakibazadeh, 2014). Personal factors are in fact a value that a person considers for himself and cares for his own and follows screening behaviors for early diagnosis of the disease, belief factor anomg patients is also important in control of disease because think that their fate depends on external factors, such as luck and chance or believe that they have a fundamental role in determining theirselve health status (Runowicz et al., 2016).
According to the results, there was a significant relationship between life priorities (as the last discussed variable) and mammography. The results of other studies were consistent with the present study and factors such as conflicts with other life problems, other physical illnesses, conflict with problems of family members and high occupations and lack of sufficient time were barriers for performing mammography (Farmer et al., 2007; Stoll et al., 2015).
Limitations of the study
The small sample size of include studies are potential limitation of this study. There is still need to further studies to access additional information about breast cancer screening determinants with mammography. Another limitations of the current study, were low of the same study in this field and low of the health cnters surveyed in Urmia city.
In conclusion, according to the results, it is needed to emphasize on the culture of health care in order to increase the frequency of mammography and other breast cancer screening tests. The results of this study reveal the need of reproductive health specialists to emphasize on the teaching and promoting screening methods. To increase the use of a healthcare behavior, solely relying on education is not useful. It is recommended to pay attention other barriers and remove them. Certainly, these goals will certainly not be achieved without the development of long-term and continuous plans.
Conflict of Interest
The authors delacred that there was no conflict of interst in this study.
Acknowledgements
This article is the result of a research project approved by ethical committee and research deputy of the faculty of nursing and midwifery. The authors would like to thank the the deputy of Health of Urmia University of Medical Sciences as well as the cooperation of the participants, so that it was not possible to do without their cooperation.
References
- 1.Abbaszadeh A, Taebi M, Simin K, Haghdost A. The relationship of health beliefs of Kermanian women and participation in mammography. J Qual Res Health Sci. 2011;10:9–17. [Google Scholar]
- 2.Abedian K, Shah Hosseini Z, Adeli M. Survey of health beliefs of women about performing mammography in the health servic centers of Sari. J Mazandaran Uni Med Sci. 2006;16:90–8. [Google Scholar]
- 3.Alam A. Knowledge of breast cancer and its risk and protective factors among women in Riyadh. Annals of Saudi medicine. 2006;26:272. doi: 10.5144/0256-4947.2006.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anderson Benjamin O. Breast healthcare and cancer control in limited-resource countries:a framework for change. Nat Clin Pract Oncol. 2006;3:4–5. doi: 10.1038/ncponc0397. [DOI] [PubMed] [Google Scholar]
- 5.Assefa M. Assessment of types and treatment pattern of cancer in TASH radiotherapy center:retrospective study. A thesis submitted to the school of graduate studies of AAU in partial fulfillment of the requirements for the degree of master of science in pharmacoepidemiology and social pharmacy, Addis Ababa. 2011. https://pdfs.semanticscholar.org/add5/b462c9⅚c9155c50ec73446b6f86928dc7.pdf .
- 6.Azadbakht M, Garmaroodi GH, Taheri Tanjani P, et al. Health promoting self-care behaviors and its related factors in elderly:application of health belief model. J Educ Community Health. 2014;1:20–9. [Google Scholar]
- 7.Coleman MP, Quaresma M, Berrino F, et al. Cancer survival in five continents:a worldwide population-based study (CONCORD) Lancet Oncol. 2008;9:730–56. doi: 10.1016/S1470-2045(08)70179-7. [DOI] [PubMed] [Google Scholar]
- 8.DeSantis C, Ma J, Bryan L, Jemal A. Breast cancer statistics 2013. CA Cancer J Clin. 2014;64:52–62. doi: 10.3322/caac.21203. [DOI] [PubMed] [Google Scholar]
- 9.Dündar P, Erbay O, Dilek O. The knowledge and attitudes of breast self-examination and mammography in a group of women in a rural area in western Turkey. BMC Cancer. 2006;6:43. doi: 10.1186/1471-2407-6-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dündar P, Özmen D, Öztürk B, et al. The knowledge and attitudes of breast self-examination and mammography in a group of women in a rural area in western Turkey. BMC Cancer. 2006;6:1. doi: 10.1186/1471-2407-6-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Eisinger F, Blay JY, Morere JF, et al. Cancer screening in France:subjects'and physicians'attitudes. Cancer Causes Control. 2008;19:431–4. doi: 10.1007/s10552-007-9102-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Farmer D, Reddick B, Jackson SH. Psychosocial correlates of mammography screening in older African American women. Paper presented at the Oncology nursing forum. Oncol Nurs Forum. 2007;34:117–23. doi: 10.1188/07.ONF.117-123. [DOI] [PubMed] [Google Scholar]
- 13.Farshbaf KH, Shahnazi M, Ghahvehchi A, Torabi Sh. Performance conditions of breast cancer screening methods and its efficient factors among women referring to health centers of Tabriz. Iran J Nurs Res. 2009;4:27–38. [Google Scholar]
- 14.Friedewald SM, Rafferty EA, Rose SL, et al. Breast cancer screening using tomosynthesis in combination with digital mammography. JAMA. 2014;311:2499–507. doi: 10.1001/jama.2014.6095. [DOI] [PubMed] [Google Scholar]
- 15.Griva F, Anagnostopoulos F, Gourounti K, Kolokotroni P, Koutrouli N. Mammography screening within the context of the theory of planned behavior:The role of personality traits and personal factors. Int J Psychol Studies. 2013;5:98. [Google Scholar]
- 16.Harirchi I, Kolahdoozan S, Karbakhsh M, et al. Twenty years of breast cancer in Iran:downstaging without a formal screening program. Ann Oncol. 2011;22:93–7. doi: 10.1093/annonc/mdq303. [DOI] [PubMed] [Google Scholar]
- 17.Harris Dawne M, Miller Jane E, Davis Diane M. Racial differences in breast cancer screening, knowledge and compliance. J Nat Med Asso. 2003;95:693. [PMC free article] [PubMed] [Google Scholar]
- 18.Hatefnia E, Niknami SH. Predictors of mammography among employed women by hbm model. J Rostamineh. 2013;5:47–56. [Google Scholar]
- 19.Hatefnia E, Niknami S, Bazargan M, et al. Correlates of mammography utilization among working Muslim Iranian women. Health Care Women Int. 2010;31:499–514. doi: 10.1080/07399331003725507. [DOI] [PubMed] [Google Scholar]
- 20.Heidari Z, Mahmoudzadeh-Sagheb HR, Sakhavar N. Breast cancer screening knowledge and practice among women in southeast of Iran. Acta Med Iranica. 2008;46:321–8. [Google Scholar]
- 21.Hersch J, Jansen J, Barratt A, et al. Women's views on overdiagnosis in breast cancer screening:a qualitative study. BMJ. 2013;346:158. doi: 10.1136/bmj.f158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jemal A, Bray F, Center MM, et al. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- 23.Jones CE, Maben J, Jack RH, et al. A systematic review of barriers to early presentation and diagnosis with breast cancer among black women. BMJ Open. 2014;4:e004076. doi: 10.1136/bmjopen-2013-004076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kaufman W, Chavez AS, Skipper B, Kaufman A. Effect of high up front charges on access to surgery for poor patients at a public hospital in New Mexico. Int J Equity Health. 2006;5:6. doi: 10.1186/1475-9276-5-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Keshavarz Z, Simbar M, Ramezankhan A, Alavi MH. Factors influencing the behavior of female-workers in the reproductive age regarding breast and cervical cancer screening based on the integrated model of planned behavior and self-efficacy: A qualitative approach. J Sch Pub Health Inst Pub Health Res. 2012;9:23–36. [Google Scholar]
- 26.Khaleghnezhad Tabari N, Khaleghnezhad Tabari A. The assessment of knowledge, attitude and behavior towards breast cancer screening methods among female teachers in Tehran. Iran J Surg. 2008;16:46–54. [Google Scholar]
- 27.Khani H, Moslemizadeh N, Montazeri A, Godazandeh Ga, Ghorbani A. Breast cancer prevention:knowledge, attitudes and practices among iranian health workers in southern coastwise of the caspian sea in 2006: a multi center study. Iran Quart J Breast Dis. 2008;2:28–37. [Google Scholar]
- 28.Kwok C, Endrawes G, Lee CF. Breast cancer screening beliefs questionnaire:Psychometric properties assessment of the Arabic version. Eur J Oncol Nurs. 2016;20:42–8. doi: 10.1016/j.ejon.2015.08.003. [DOI] [PubMed] [Google Scholar]
- 29.Kwok C, Fethney J, White K. Chinese breast cancer screening beliefs questionnaire:development and psychometric testing with Chinese-Australian women. J Adv Nurs. 2010;66:191–200. doi: 10.1111/j.1365-2648.2009.05177.x. [DOI] [PubMed] [Google Scholar]
- 30.LaPorta J, McClowry R, McIntosh L, et al. Addressing barriers to breast cancer screening:Where to intervene to increase mammogram completion rates. 2017 [Google Scholar]
- 31.Lee LF, Menon U, Pett M, et al. Breast cancer beliefs and mammography screening practices among Chinese American immigrants. J Obstet Gynecol Neonatal Nurs. 2007;36:212–21. doi: 10.1111/j.1552-6909.2007.00141.x. [DOI] [PubMed] [Google Scholar]
- 32.Lu ZYJ. Variables associated with breast self-examination among Chinese women. Cancer Nurs. 1995;18:29–34. [PubMed] [Google Scholar]
- 33.Mai V, Sullivan T, Chiarelli AM. Breast cancer screening program in Canada:successes and challenges. Salud Publica Mex. 2009;51:228–35. doi: 10.1590/s0036-36342009000800013. [DOI] [PubMed] [Google Scholar]
- 34.Moghadam F. Teachers knowledge and attitude of breast self-examination in high schools of Khoy city. MCS thesis in midwifery, Faculty of Nursing and midwifery, Tabriz University of medical science. 1998 [Google Scholar]
- 35.Morse EP, Maegga B, Joseph G, Miesfeldt S. Breast cancer knowledge, beliefs, and screening practices among women seeking care at district hospitals in Dar Es Salaam, Tanzania. Breast Cancer. 2014;8:73. doi: 10.4137/BCBCR.S13745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nojomi M, Namiranian N, Myers RE, Razavi-Ratki SK, Alborzi F. Factors associated with breast cancer screening decision stage among women in Tehran, Iran. Int J Prev Med. 2014;5:196. [PMC free article] [PubMed] [Google Scholar]
- 37.Nourizadeh R, Moghaddam TF, Vahdati S. Development and psychometric testing of an instrument to measure determinants of mammography. Payesh. 2017;16:603–12. [Google Scholar]
- 38.Okobia MN, Bunker CH, Okonofua FE, Osime U. Knowledge, attitude and practice of Nigerian women towards breast cancer:a cross-sectional study. World J Surg Oncol. 2006;4:11. doi: 10.1186/1477-7819-4-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Petro-Nustus W, Mikhail BI. Factors associated with breast self-examination among Jordanian women. Public Health Nurs. 2002;19:263–71. doi: 10.1046/j.1525-1446.2002.19406.x. [DOI] [PubMed] [Google Scholar]
- 40.Qaed Amini R. Justice in access to health services:solutions and challenges (2007 May Paper presented at the 5th annual conference of the students of health care management. Iran: Tabriz University of Medical Sciences; 2007. [Google Scholar]
- 41.Rafiemanesh H, Salehiniya H, Lotfi Z. Breast cancer in Iranian woman:incidence by age group, morphology and trends. Asian Pac J Cancer Prev. 2016;17:1393–7. doi: 10.7314/apjcp.2016.17.3.1393. [DOI] [PubMed] [Google Scholar]
- 42.Regan PC, Durvasula RS. Predictors of breast cancer screening in Asian and Latina university students. Coll Stud J. 2008;42:1152. [Google Scholar]
- 43.Ries LA, Harkins D, Krapcho M, et al. SEER cancer statistics review. 2006:1975–2003. [Google Scholar]
- 44.Runowicz CD, Leach CR, Henry NL, et al. American cancer society/American society of clinical oncology breast cancer survivorship care guideline. CA Cancer J Clin. 2016;66:43–73. doi: 10.3322/caac.21319. [DOI] [PubMed] [Google Scholar]
- 45.SalimiPormehr S, Kariman N, Sheykhan Z, AlaviMajd H. Investigation of breast cancer screening tests performance and affecting factors in women referred to Ardebil's health and medical centers 2009. J Ardabil Uni Med Sci. 2010;10:310–18. [Google Scholar]
- 46.Odusanya O. Breast cancer:knowledge, attitudes, and practices of female schoolteachers in Lagos, Nigeria. Breast J. 2001;7:171–5. doi: 10.1046/j.1524-4741.1998.410062.x-i1. [DOI] [PubMed] [Google Scholar]
- 47.Sessa A, Abbate R, Di Giuseppe G, Marinelli P, Angelillo IF. Knowledge, attitudes, and preventive practices about colorectal cancer among adults in an area of Southern Italy. BMC Cancer. 2008;8:1. doi: 10.1186/1471-2407-8-171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Shakibazadeh E. Using commercial marketing approach to deliver health and prevention:helping to promote self-care. J Hayat. 2014;20:1–5. [Google Scholar]
- 49.Siegel R, Miller K, Jemal A. Cancer statistics 2015. CA Cancer J Clin. 2015;65:5–29. doi: 10.3322/caac.21254. [DOI] [PubMed] [Google Scholar]
- 50.Stoll C, Roberts S, Cheng MR, et al. Barriers to mammography among inadequately screened women. Health Educ Behav. 2015;42:8–15. doi: 10.1177/1090198114529589. [DOI] [PubMed] [Google Scholar]
- 51.Tavakolian L, Boniadi F, Malekzadeh E. The investigation of factors associated with breast cancer screening among Kazeroon women aged 20-65 in 2013. Nurs J Vulnerable. 2015;1:17–31. [Google Scholar]
- 52.Tejeda S, Thompson B, Coronado GD, Martin DP. Barriers and facilitators related to mammography use among lower educated Mexican women in the USA. Soc Sci Med. 2009;68:832–39. doi: 10.1016/j.socscimed.2008.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Vazifeshenas R, Shahnazi M, Tavakol Z. Practice of the midwives occupied in health centers of Tabriz about breast cancer screening methods. Paper presented at the Proceedings of the of 1st congress of life quality and health promotion (oral) 2007 [Google Scholar]
- 54.Wang HH, Wang RH, Shieh C. Self-care and well-being model for elderly women:A comparison of rural and urban areas. Kaohsiung J Med Sci. 2004;20:63–8. doi: 10.1016/S1607-551X(09)70086-5. [DOI] [PubMed] [Google Scholar]
- 55.Yücel A, Degirmenci B, Acar M, et al. Knowledge about breast cancer and mammography in breast cancer screening among women awaiting mammography. Turk J Med Sci. 2005;35:35–42. [Google Scholar]
- 56.Zheng YF, Saito T, Takahashi M, Ishibashi T, Kai I. Factors associated with intentions to adhere to colorectal cancer screening follow-up exams. BMC Public Health. 2006;6:272. doi: 10.1186/1471-2458-6-272. [DOI] [PMC free article] [PubMed] [Google Scholar]


