Introduction
The term dysplastic nevus derives from Greek (dys = abnormal) and (plasis = growth) and was coined to describe a distinct entity harbouring, in its name, a potential harm to the host [1]. In 1992, the National Institutes of Health Consensus Conference proposed to replace the term with “nevus with architectural disorder with and without cytologic atypia” [2]. However, the old terminology continues to be widely used. By inserting dysplastic nevus as an intermediate melanocytic lesion within the histologic morphobiologic spectrum of benign versus malignant lesions, it was felt that a diagnostic “comfort zone” was provided where diagnostic uncertainty on behalf of the pathologist may, in turn, guarantee re-excision of the lesion by the clinician [3, 4].
Histopathologic Criteria
The World Health Organization (WHO) in 1991 defined dysplastic nevus as a histologic entity which is distinct from common nevi, and with the diagnosis requiring both of two major criteria (basilar proliferation of atypical melanocytes extending three rete ridges beyond the dermal component; organization of proliferation in lentiginous or epithelioid cell pattern), and at least two of the minor criteria (lamellar or concentric eosinophilic fibrosis; neovascularization; inflammatory response; fusion of rete ridges) [5]. Duke University added a three-level grading of cytologic atypia into mild, moderate, and severe. This was based on nuclear size, morphology, euchromatism, nucleoli prominence, as well as cell diameter when compared to basal keratinocytes [6] (Fig. 1). Issues arise in the setting of a diagnosis of dysplastic nevus with severe atypia, which harbours the risk of misdiagnosing a melanoma in situ [7].
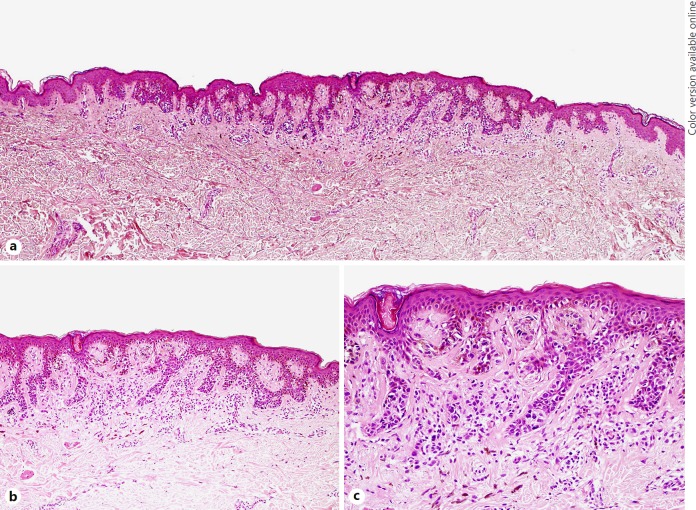
Fig. 1.
Dysplastic nevus. a Fairly well-circumscribed lentiginous and nested melanocytic proliferation extending three rete ridges beyond the dermal component (original magnification ×40). b The lesion exhibits elongation and fusion of the rete ridges, concentric and lamellar papillary dermal fibroplasia, a patchy lymphoid cell infiltrate, and occasional melanophages (original magnification ×100). c Mild to moderate cytologic atypia (original magnification ×200).
Problems of Diagnostic Reproducibility
Pathologists rely on visual interpretation for diagnosing melanocytic lesions. However, there is great variation amongst pathologists, particularly within the spectrum ranging from dysplastic nevi with moderate atypia to early melanoma; such criteria are neither reproducible nor accurate [8]. This is due to the overlapping morphologic features shared by common nevi and melanoma [7], which makes the interpretation of dysplastic nevi cum bersome. Further complexity arises when a dysplastic nevus is adjacent to an early melanoma in situ, and the question is whether they may represent part of a morphobiologic continuum or not (Fig. 2, 3). Ultimately, grading atypia (mild, moderate, severe) is highly subjective, with low interobserver agreement [9].
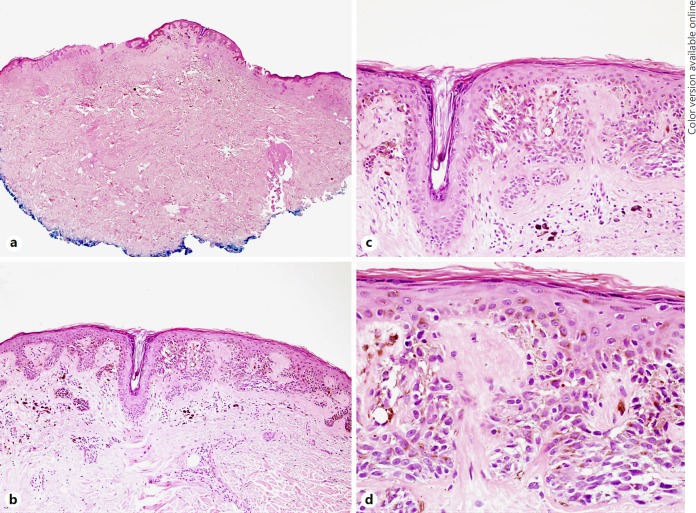
Fig. 2.
Excision of a clinically and dermoscopically diagnosed dysplastic nevus. a Scanning magnification showing a well-demarcated melanocytic proliferation in the centre of the specimen (original magnification ×20). b–d At higher magnification, the lesion exhibits features of a dysplastic nevus with moderate atypia (original magnifications b ×100, c ×200, d ×400).
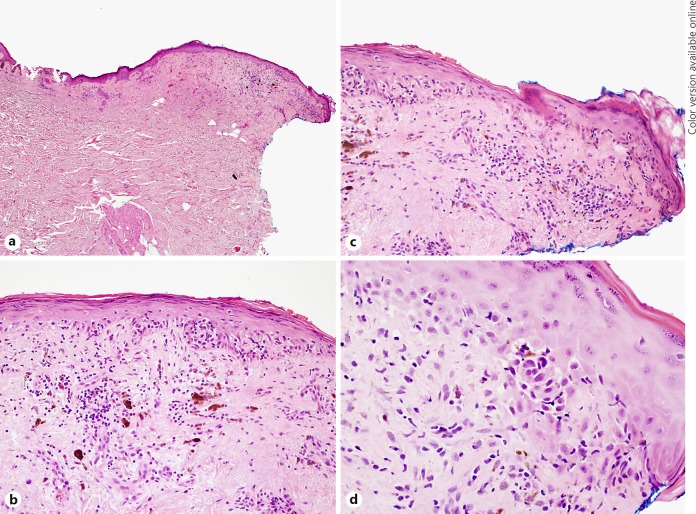
Fig. 3.
Area adjacent to the dysplastic nevus with melanoma in situ. a Scanning magnification of the same histologic section as in Figure 2 showing loss of rete ridges with epidermal thinning and papillary dermal fibrosis, suggestive of possible regression (original magnification ×40). b, c At higher magnification, an irregular lentiginous and nested melanocytic proliferation with scattered lymphocytes and melanophages with papillary dermal fibrosis is observed extending to the peripheral margin (original magnifications ×200). d Deeper sections of the peripheral margin further disclose the atypical intraepidermal melanocytes of melanoma in situ. No invasive component was identified in numerous sections evaluated (original magnification ×400).
New Genetic Insights
Numerous studies have been undertaken to identify molecular features distinguishing dysplastic nevi from common nevi and melanoma [1]. In an attempt to overcome the limitations of low interobserver agreement in the diagnosis of dysplastic nevi, a study has been undertaken to assess whether the morphologic features of dysplastic nevi are genetically driven and whether morphology may be the reflection of a genetic alteration, with the ultimate risk of progression to melanoma [10]. Shain et al. [10] showed that there is a sequence of genetic alternations during melanoma development, and that those melanocytic lesions with one or more pathogenic alterations, such as dysplastic nevi, in their evolutionary model fall into the “intermediate” category.
The Re-Excision Controversy
Given the above considerations, the histopathologic diagnosis of a dysplastic nevus impacts patient management. While it is generally accepted that mildly atypical dysplastic nevi which do not resemble melanoma do not require further treatment [7], recent studies have shown low recurrence rates of dysplastic nevi with moderate atypia and positive histologic margins [9, 11] and of dysplastic nevi with severe atypia [12], thus suggesting that re-excision may not be required [9, 11, 12]. Others advocate an upfront clear margin policy in the re-excision of dysplastic nevi with a margin biopsy of 2.0 mm [13] or with complete shave removal with clear margins [14]. It has also been suggested that the use of a non-grading histologic diagnostic approach of dysplastic nevi may decrease the excision rate [15].
Nevertheless, providing an objective interpretation of a dysplastic nevus with severe atypia at the light microscopic level still remains difficult, given its borderline morphology potentially representing the early counterpart of the morphobiologic continuum with melanoma [4, 16].
Conclusion
It is hoped that the recent advances in genetics will shed light on the knowledge of dysplastic nevus and resolve its morphologic conundrum distinguishing it from melanoma. Incompletely excised dysplastic nevi with moderate and severe architectural and cytologic atypia, in the setting of appropriate clinicopathologic correlation, should be best managed by complete re-excision.
Statement of Ethics
The author has no ethical conflicts to disclose.
Disclosure Statement
The author has no conflicts of interest to declare.
References
- 1.Duffy K, Grossman D. The dysplastic nevus: from historical perspective to management in the modern era: Part I. Historical, histologic, and clinical aspects. J Am Acad Dermatol. 2012;67(1) doi: 10.1016/j.jaad.2012.02.047. e1–1.e16; quiz 1.e17–1.e18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.NIH Consensus Conference Diagnosis and treatment of early melanoma. JAMA. 1992;268(3):1314–1319. doi: 10.1001/jama.1992.03490100112037. [DOI] [PubMed] [Google Scholar]
- 3.Kittler H, Tschandl P. Dysplastic nevus: why this term should be abandoned in dermatoscopy. Dermatol Clin. 2013;31:579–588. doi: 10.1016/j.det.2013.06.009. viii. [DOI] [PubMed] [Google Scholar]
- 4.Rosendahl CO, Grant-Kels JM, Que SK. Dysplastic nevus: fact and fiction. J Am Acad Dermatol. 2015;73:507–512. doi: 10.1016/j.jaad.2015.04.029. [DOI] [PubMed] [Google Scholar]
- 5.Clemente C, Cochran AJ, Elder DE, Levene A, MacKie RM, Mihm MC, Rilke F, Cascinelli N, Fitzpatrick TB, Sober AJ. Histopathologic diagnosis of dysplastic nevi: concordance among pathologists convened by the World Health Organization Melanoma Programme. Hum Pathol. 1991;22:313–319. doi: 10.1016/0046-8177(91)90078-4. [DOI] [PubMed] [Google Scholar]
- 6.Shea CR, Vollmer RT, Prieto VG. Correlating architectural disorder and cytologic atypia in Clark (dysplastic) melanocytic nevi. Hum Pathol. 1999;30:500–505. doi: 10.1016/s0046-8177(99)90191-0. [DOI] [PubMed] [Google Scholar]
- 7.Duffy K, Grossman D, The dysplastic nevus: from historical perspective to management in the modern era: Part II Molecular aspects and clinical management. J Am Acad Dermatol. 2012;67(19):e1–19. doi: 10.1016/j.jaad.2012.03.013. e12; quiz 19.e31–19.e32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Elmore JG, Barnhill RL, Elder DE, Longton GM, Pepe MS, Reisch LM, Carney PA, Titus LJ, Nelson HD, Onega T, Tosteson ANA, Weinstock MA, Knezevich SR, Piepkorn MW. Pathologists' diagnosis of invasive melanoma and melanocytic proliferations: observer accuracy and reproducibility study. BMJ. 2017;357 doi: 10.1136/bmj.j2813. j2813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hiscox B, Hardin MR, Orengo IF, Rosen T, Mir M, Diwan AH. Recurrence of moderately dysplastic nevi with positive histologic margins. J Am Acad Dermatol. 2017;76:527–530. doi: 10.1016/j.jaad.2016.09.009. [DOI] [PubMed] [Google Scholar]
- 10.Shain AH, Yeh I, Kovalyshyn I, Sriharan A, Talevich E, Gagnon A, Dummer R, North J, Pincus L, Ruben B, Rickaby W, D'Arrigo C, Robson A, Bastian BC. The genetic evolution of melanoma from precursor lesions. N Engl J Med. 2015;373:1926–1936. doi: 10.1056/NEJMoa1502583. [DOI] [PubMed] [Google Scholar]
- 11.Hiscox B, Hardin MR, Orengo IF, Rosen T, Mir M, Diwan AH. Reply: Do moderately dysplastic nevi with positive histologic margins need to be reexcised? J Am Acad Dermatol. 2017;77 doi: 10.1016/j.jaad.2017.05.011. e85. [DOI] [PubMed] [Google Scholar]
- 12.Engeln K, Peters K, Ho J, Jedrych J, Winger D, Ferris LK, Patton T. Dysplastic nevi with severe atypia: long-term outcomes in patients with and without re-excision. J Am Acad Dermatol. 2017;76:244–249. doi: 10.1016/j.jaad.2016.08.054. [DOI] [PubMed] [Google Scholar]
- 13.Terushkin V, Ng E, Stein JA, Katz S, Cohen DE, Meehan S, Polsky D. A prospective study evaluating the utility of a 2-mm biopsy margin for complete removal of histologically atypical (dysplastic) nevi. J Am Acad Dermatol. 2017;77:1096–1099. doi: 10.1016/j.jaad.2017.07.016. [DOI] [PubMed] [Google Scholar]
- 14.Maghari A. Dysplastic (or atypical) nevi showing moderate or severe atypia with clear margins on the shave removal specimens are most likely completely excised. J Cutan Med Surg. 2017;21:42–47. doi: 10.1177/1203475416661313. [DOI] [PubMed] [Google Scholar]
- 15.Lozeau DF, Farber MJ, Lee JB. A nongrading histologic approach to Clark (dysplastic) nevi: a potential to decrease the excision rate. J Am Acad Dermatol. 2016;74:68–74. doi: 10.1016/j.jaad.2015.09.030. [DOI] [PubMed] [Google Scholar]
- 16.Cockerell CJ. Counterpoint: The “dysplastic” nevus: what I do and do not believe. J Am Acad Dermatol. 2015;73:515–517. doi: 10.1016/j.jaad.2015.05.037. [DOI] [PubMed] [Google Scholar]