Abstract
Background
We evaluated the changes in mean arterial pressure (MAP) and heart rate (HR), and the anesthetic and hemostatic effects, after injection of 2% lidocaine containing various concentrations of epinephrine in rats and mice to determine the appropriate concentration of epinephrine in various anesthetic mixtures.
Methods
Rats and mice were randomly allocated to experimental groups: 2% lidocaine without epinephrine (L0), 2% lidocaine with epinephrine 1:200,000 (L200), 1:100,000 (L100), and 1:80,000 (L80). Changes in MAP and HR after administration of the anesthetic mixture were evaluated using a physiological recording system in rats. Onset and duration of local anesthesia was evaluated by pricking the hind paw of mice. A spectrophotometric hemoglobin assay was used to quantify the hemostatic effect.
Results
MAP increased in response to epinephrine in a dose-dependent manner; it was significantly higher in the L80 group than in the L0 group at 5 min post-administration. The HR was relatively lower in the L0 group than in the L80 group. The time required for onset of action was < 1 min in all evaluation groups. The duration of action and hemostatic effect of the local anesthetic were significantly better in the L200, L100, and L80 groups than in the L0 group.
Conclusion
L200 demonstrated relatively stable MAP and HR values with satisfactory efficacy and hemostatic effect. L200 might be a better local anesthetic for dental patients in terms of anesthetic efficacy and safety.
Keywords: Arterial Pressure, Epinephrine, Hemostasis, Lidocaine, Local Anesthetics
INTRODUCTION
Lidocaine is one of the preferred local anesthetic agents in the field of dentistry. The advantages of lidocaine include its quick onset, acceptable duration of action, and excellent safety profile. Despite rare occurrence of toxicity, excessive doses of lidocaine influence function of the cardiovascular and central nervous systems in a dose-dependent manner [1]. Addition of epinephrine to lidocaine reduces the local blood flow, resulting in vasoconstriction, and rapid onset and increased duration of action, by decreasing systemic absorption of lidocaine [2]. The provision of a clear operative field due to reduced bleeding at the operating site is another beneficial effect of using vasoconstrictors. However, unfavorable hemodynamic changes such as tachycardia, increased blood pressure (BP), and cardiac contraction force can be observed due to systemic absorption of exogenous epinephrine in the local anesthetic, especially in subjects with hypertension [3,4]. Low concentration of epinephrine is preferred in patients for whom it may be desirable to limit the epinephrine burden, such as those with cardiovascular diseases.
There are different views regarding optimal concentration level of epinephrine in lidocaine for safety and efficacy in dentistry. Comparative studies have reported effects of local anesthetics and concentrations of lidocaine [5,6]. Although the degree of anesthesia for inferior alveolar nerve block was not statistically different among the treatment groups of 1:50,000, 1:80,000, and 1:100,000 epinephrine with 2% lidocaine [7], the effect of 1:200,000 epinephrine with 2% lidocaine has not been established yet. In this study, we compared changes of hemodynamic variables after administration of various epinephrine concentrations contained in 2% lidocaine in rats. In addition, local anesthetic and hemostatic effects of lidocaine containing various concentrations of epinephrine were investigated in mice.
MATERIALS AND METHODS
1. Animals
Male Sprague-Dawley rats (Orient Bio Inc., Gyunggi-do, Korea) with 300–350 g body weight, and male ICR mice (Orient Bio Inc., Gyeonggi-do, Korea) with 30–35 g body weight were housed in specific pathogen-free barrier cages with free access to food and water. The cages were covered with soft bedding and maintained in an environmental room equipped with programmed 12-h light cycle (7 am / 7 pm) at constant temperature (23℃) and humidity (50%). All experimental procedures were performed according to the ethical guidelines for the use of animals in research of the International Association for the Study of Pain. The study protocol was reviewed and approved by the Institutional Animal Care and Use Committee of Seoul National University (SNU130104-3-1). Rescue analgesia was provided with tramadol. Investigators were blinded to experimental groups during the entire course of study.
Rats and mice were randomly allocated to four groups each, according to concentration of epinephrine added to 2% lidocaine using a table of random numbers: 2% lidocaine without epinephrine (L0), 2% lidocaine with 1:200,000 epinephrine (L200), 2% epinephrine with 1:100,000 epinephrine (L100), and 2% epinephrine with 1:80,000 epinephrine (L80). Changes in BP and heart rate (HR) were observed after administration of lidocaine containing different concentrations of epinephrine in all groups of rats. Onset and duration of anesthetics and degree of bleeding from incision site were evaluated in all groups of mice. Lidocaine containing various concentrations of epinephrine was supplied by Huons Co., Ltd. (Gyunggi-do, Korea). Lidocaine cartridges were covered with a white strip to blind investigators from information on the anesthetic solution.
2. Measurement of BP and HR
Rats (n = 9–10 per group) were anesthetized with intraperitoneal injection of urethane (1.5 g/kg) (Sigma-Aldrich, St Louis, MO, U.S.A.) and placed on a heating pad (Homeothermic Blanket System, Harvard Apparatus, Holliston, MA) to maintain constant rectal temperature (37 ± 0.5℃). Catheters were placed in the left carotid artery for measurement of systemic arterial BP (IWX214 Data Recorder, iWorx/CB Sciences Inc., Dover, NH, U.S.A.). After system calibration and 10-min equilibration period, baseline values for arterial BP and HR were measured. Subsequently, lidocaine (7 mg/kg) containing a selected concentration of epinephrine was injected over 1 min into the mandibular gingivobuccal fold, using a 31-gauge needle. BP and HR were continuously measured for 10-min after administration of the anesthetic mixture. Alterations in arterial pressure and HR were expressed as percent change from the mean arterial pressure (MAP) and HR at baseline, respectively, of each study subject.
3. Local anesthetic effect
To examine local anesthetic effect of each mixture, pricking mechanical stimuli with a 10 g of von Frey filament (North Coast Medical Inc., Morgan Hill, CA. U.S.A.) were applied to the plantar surface of the hind paw [8] of mice. Each mouse (n = 10 per group) was placed on a metal mesh floor to allow habituation for 20 min. Mice with signs of hypersensitivity or freezing reactions to the von Frey test were excluded from the experiment. Lidocaine (7 mg/kg) containing any concentration of epinephrine were injected into the subcutaneous tissue on the plantar surface of the hind paw with slow infiltration using a 31-gauge needle, followed by mechanical stimulation every 30 s using a von Frey filament, with a strength that bends the filament slightly.
4. Analysis of hemostatic effect
Mice (n = 11 per group) were anesthetized with intra-peritoneal injection of urethane (1.5 g/kg). Lidocaine (7 mg/kg) containing known concentration of epinephrine was administered in the right thigh region with slow infiltration using a 31-gauge needle. At 2-min after administration, thigh muscles were cut to 1-cm length with #11 scalpel blade. Capillary bleeding from the incised muscle was absorbed for 3 min using filter paper of size 3 mm × 30 mm (Advantec no. 2; Toyo Roshi Kaisha Ltd., Tokyo, Japan) that were pre-treated by soaking in 0.04% heparinized saline to prevent blood coagulation during the experiment. The hemolyzed red blood cell lysate was isolated from the filter paper using Cyto Buster Protein Extraction Reagent (Novagen, Madison, WI, U.S.A), overnight. The released hemoglobin in the supernatant was quantified at 540 nm using a microplate reader (PowerWave X340, BioTek Instruments Inc., Winooski, VT, U.S.A.).
5. Statistical analysis
Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS) software (version 21.0, SPSS Inc., Chicago, IL, U.S.A.). MAP and HR were analyzed using one-way ANOVA followed by Tukey post hoc test. Kruskal-Wallis test followed by Dunn's multiple comparisons test was used for analysis of the local anesthetic and hemostatic effects. All data are expressed as mean ± SD. P < 0.05 was considered statistically significant.
RESULTS
1. Measurement of MAP and HR
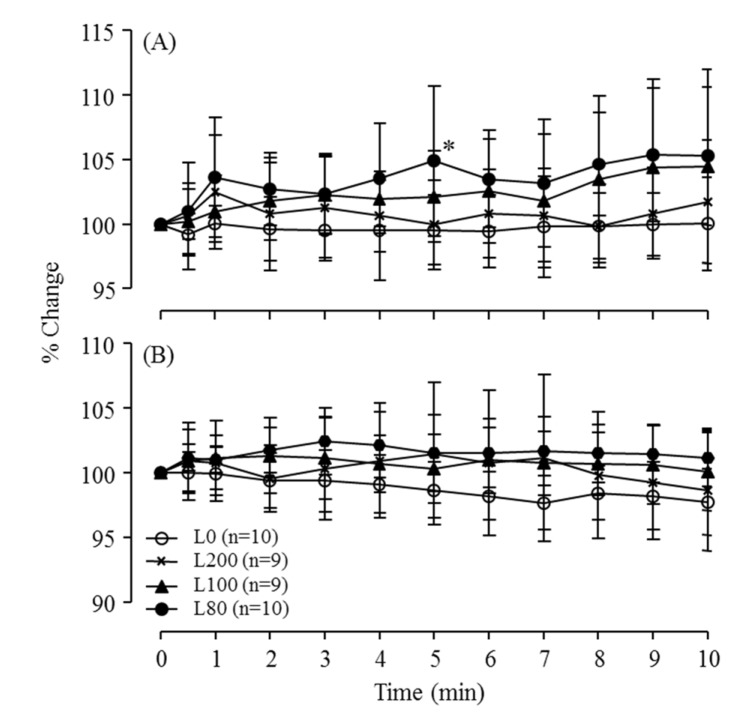
To evaluate effect of lidocaine-epinephrine mixture on the cardiovascular system in rats, we analyzed time-dependent changes in the MAP and HR. The effect of anesthetic mixture for 10 min after administration on the MAP in rats is illustrated in Fig. 1(A). Increasing concentration of epinephrine showed positive correlation with the degree of MAP increase. Five minutes after administration of anesthetic mixture, the MAP of the L80 group was significantly increased compared to that of the L0 group (P < 0.05). A concentration-dependent increase in MAP by epinephrine-lidocaine mixtures was observed in all groups.
Fig. 1. Percent change of mean arterial pressure (A) and heart rate (B) in rats after injection of 2% lidocaine without or with various concentrations of epinephrine. *P < 0.05 vs. L0 (one-way ANOVA followed by Tukey post hoc test). Results are presented as mean ± SD.
The percent change in HR for 10 min post-administration is shown in Fig. 1(B). The HR of L0 showed gradual decrease; whereas, that of L100 and L80 showed slight increase, without significant group-wise difference.
2. Local anesthetic effect
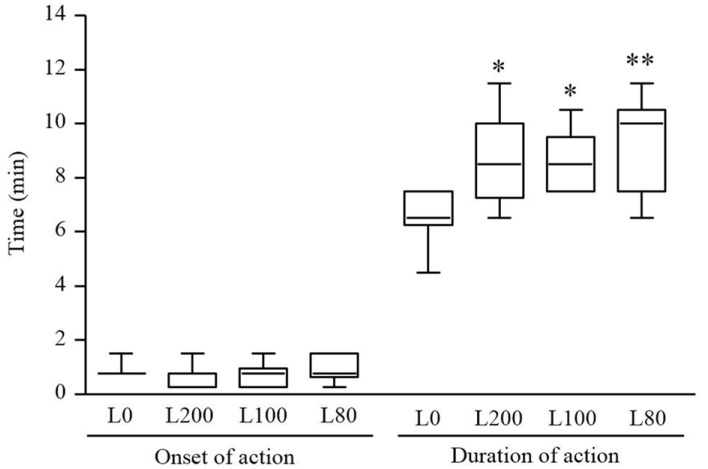
To determine the effect of epinephrine on the onset and duration of anesthetic action, in all mice, the hind paw was pricked with a von Frey filament after administration of an anesthetic mixture. In each group, the onset of anesthetic action was < 1 min; and the duration of action of L200, L100, and L80 was significantly greater than that in L0 (Fig. 2).
Fig. 2. Onset and duration of local anesthetic action in mice injected with 2% lidocaine without or with various concentrations of epinephrine. N = 10 per group. *P < 0.05 and **P < 0.01 vs. L0 (Kruskal-Wallis test followed by Dunn's multiple comparisons test). Results are presented as median, interquartile range, and full range.
3. Analysis of hemostatic effect
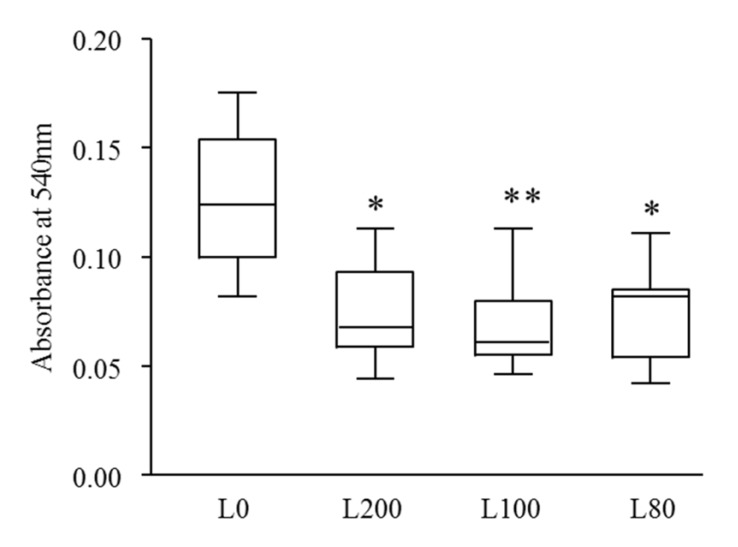
To investigate the hemostatic effect of lidocaine without or with various concentrations of epinephrine, the amount of capillary bleeding from the incision site at the mouse thigh for 3 min was measured. The absorbance at 540 nm was significantly lower in L200, L100, and L80 than that in L0 (Fig. 3).
Fig. 3. Hemostatic effect on mice after injection of 2% lidocaine without or with various concentrations of epinephrine. N = 11 per group. *P < 0.05 and **P < 0.01 vs. L0 (Kruskal-Wallis test followed by Dunn's multiple comparisons test). Results are presented as median, interquartile range, and full range.
DISCUSSION
In this study, the effect of various concentrations of epinephrine in 2% lidocaine on the hemodynamics, anesthetic effect, and hemostasis was investigated. L200 showed consistent low values of MAP and HR than L100 or L80. The duration of anesthesia and hemostatic effect of L200, L100, or L80 were superior to those of the epinephrine free group, L0.
In modern society, the need for dental treatment has increased due to change of eating habits, elongation of life expectancy, and pursuit of better quality of life; thus, importance of anesthetics has been emphasized. Indiscreet usage of anesthetics is harmful to vital organs in our body and could be life threatening [9,10]. It may be necessary to select the optimal concentration of epinephrine in local anesthetics according to the health conditions of individual patients.
Lidocaine containing 1:80,000 or 1:100,000 epinephrine has been widely used for local anesthesia in dentistry. Lidocaine, an amide-type local anesthetic agent that has been in use since 1948, is less efficient in duration and effectiveness than tetracaine. However, it is adequate for use in dental treatments with mild toxicity [11,12]. For sustained anesthesia and hemostasis in surgical patients, in general, lidocaine is mixed with a small amount of epinephrine [13,14]. Bader et al. [4] reported that epinephrine concentrations of 1:80 000 and 1:100,000 in the dental local anesthetic cartridge are unnecessarily high. Because epinephrine is a hormone and a neurotransmitter, intra-operative over dose may cause elevated BP and HR due to stimulation of the sympathetic nerve system [15,16].
We estimated the biological safety of lidocaine with 1:200,000 epinephrine through evaluation of hemodynamic parameters in an animal model. Fig. 1(A) presents the changes of BP in each group at 1-min intervals for 10 min after injection. Evaluation of BP is one of the most sensitive assays for the response to epinephrine levels. In this study, MAP was increased in response to epinephrine in a dose-dependent manner. It suggests that the epinephrine contained in L100 or L80 could be the cause of the raised BP.
There was no change in HR in the L200 and L100 groups; however, the HR was slightly increased in the L80 group, while that in the L0 group was decreased. Salonen et al. [17] and Meechan et al. [18] demonstrated absence of hemodynamic response to lidocaine with epinephrine in healthy young patients. In addition, Niwa et al. [19] reported that intraoral injection of 1.8 mL of 2% lidocaine with 1:80,000 epinephrine was safe in patients with cardiovascular disease; however, the volume of epinephrine used in their study was less than that used clinically. Kohler et al. [20] reported that negative cardiovascular effects could be followed by systemic absorption of drug in some patients with cardiac diseases. In our study, the maximum local anesthetic lidocaine dosage was 7 mg/kg. Administration of L100 or L80 with a large volume might lead to adverse effects in patients with cardiac diseases. Gerlach et al. [21] suggested that epinephrine-containing anesthetics should be used under consideration of the cardiac condition of each patient; thus, minimum dosage of epinephrine is indicated in patients with significant cardiac diseases.
Despite differences in MAP or HR values based on the epinephrine concentration, all treatments containing epinephrine had extended duration of anesthetic action than that of L0. Wakita et al. [22] conducted the pinprick test and von Frey test in the medial antecubital skin for evaluation of anesthetic effect of 2% lidocaine with 1:80,000, 1:160,000, and 1:320,000 epinephrine. Level of pricking pain using the visual analogue scale was significantly lower compared with baseline values in the groups with 1:80,000 and 1:160,000 epinephrine, but not in groups with 2% lidocaine alone or 1:320,000 epinephrine.
Reduced bleeding was observed in groups containing epinephrine compared to that in L0. Injected epinephrine at the surgical site can reduce bleeding by stimulating the α1 adrenergic receptors [23,24]. L200 had comparable hemostatic effect with L100 and L80, which indicated that the local anesthetic effect of L200 may be sufficient for use in clinical dental treatment.
This study has several limitations. First, the study was conducted in an experimental animal model. In the patient's model, the degree of bleeding is quite extensive depending on the surgical site, procedure, and operating time. However, in a previous study comparing L200 and L80 in human subjects, L200 had better safety with regard to hemodynamic parameters than that of L80 [25]. In this study, the hemostatic effect was evaluated in an objective manner by using consistent procedure. Second, Sprague-Dawley rats used in this study were healthy. Adverse effects induced by epinephrine are more common in subjects with cardiovascular diseases. Further studies using cardiovascular disease animal model, such as rats with spontaneous hypertension, are needed. Third, vital signs were recorded for up to 10 min after injection due to consistency in findings for 5 min. Hence, observation of different tendency in hemodynamic change after 10 min is possible.
Our results indicated that the L100 and L80 local anesthetic mixtures containing higher concentration of epinephrine, showed unfavorable hemodynamic changes including increases in MAP and HR. L0, plain lidocaine, had short duration of anesthetic action. L200 demonstrated relatively stable MAP and HR values with satisfactory action duration and hemostatic effect. In conclusion, L200 might be a better local anesthetic for dental patients in terms of anesthetic efficacy and safety.
ACKNOWLEDGMENTS
This work was supported by Huons Co., Ltd. Korea.
Footnotes
DECLARATION OF INTERESTS: All authors declared no conflict of interest.
References
- 1.Faccenda KA, Finucane BT. Complications of regional anaesthesia incidence and prevention. Drug Saf. 2001;24:413–442. doi: 10.2165/00002018-200124060-00002. [DOI] [PubMed] [Google Scholar]
- 2.Hersh EV, Giannakopoulos H, Levin LM, Secreto S, Moore PA, Peterson C, et al. The pharmacokinetics and cardiovascular effects of high-dose articaine with 1:100,000 and 1:200,000 epinephrine. J Am Dent Assoc. 2006;137:1562–1571. doi: 10.14219/jada.archive.2006.0092. [DOI] [PubMed] [Google Scholar]
- 3.Sano K. Vasoconstrictors in local anesthesia. Dental Diamond. 1988;23:62–65. [Google Scholar]
- 4.Bader JD, Bonito AJ, Shugars DA. A systematic review of cardiovascular effects of epinephrine on hypertensive dental patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93:647–653. doi: 10.1067/moe.2002.123866. [DOI] [PubMed] [Google Scholar]
- 5.Boonsiriseth K, Chaimanakarn S, Chewpreecha P, Nonpassopon N, Khanijou M, Ping B, et al. 4% lidocaine versus 4% articaine for inferior alveolar nerve block in impacted lower third molar surgery. J Dent Anesth Pain Med. 2017;17:29–35. doi: 10.17245/jdapm.2017.17.1.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ping B, Kiattavorncharoen S, Durward C, Im P, Saengsirinavin C, Wongsirichat N. Hemodynamic changes associated with a novel concentration of lidocaine hcl for impacted lower third molar surgery. J Dent Anesth Pain Med. 2015;15:121–128. doi: 10.17245/jdapm.2015.15.3.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dagher FB, Yared GM, Machtou P. An evaluation of 2% lidocaine with different concentrations of epinephrine for inferior alveolar nerve block. J Endod. 1997;23:178–180. doi: 10.1016/S0099-2399(97)80271-3. [DOI] [PubMed] [Google Scholar]
- 8.Lee JY, Shin TJ, Choi JM, Seo KS, Kim HJ, Yoon TG, et al. Antinociceptive curcuminoid, kms4034, effects on inflammatory and neuropathic pain likely via modulating trpv1 in mice. Br J Anaesth. 2013;111:667–672. doi: 10.1093/bja/aet176. [DOI] [PubMed] [Google Scholar]
- 9.Daublander M, Muller R, Lipp MD. The incidence of complications associated with local anesthesia in dentistry. Anesth Prog. 1997;44:132–141. [PMC free article] [PubMed] [Google Scholar]
- 10.Kaufman E, Goharian S, Katz Y. Adverse reactions triggered by dental local anesthetics: A clinical survey. Anesth Prog. 2000;47:134–138. [PMC free article] [PubMed] [Google Scholar]
- 11.McLure HA, Rubin AP. Review of local anaesthetic agents. Minerva Anestesiol. 2005;71:59–74. [PubMed] [Google Scholar]
- 12.Sobanko JF, Miller CJ, Alster TS. Topical anesthetics for dermatologic procedures: A review. Dermatol Surg. 2012;38:709–721. doi: 10.1111/j.1524-4725.2011.02271.x. [DOI] [PubMed] [Google Scholar]
- 13.Carvalho B, Fuller A, Brummel C, Cohen SE. Local infiltration of epinephrine-containing lidocaine with bicarbonate reduces superficial bleeding and pain during labor epidural catheter insertion: A randomized trial. Int J Obstet Anesth. 2007;16:116–121. doi: 10.1016/j.ijoa.2006.09.006. [DOI] [PubMed] [Google Scholar]
- 14.Ghali S, Knox KR, Verbesey J, Scarpidis U, Izadi K, Ganchi PA. Effects of lidocaine and epinephrine on cutaneous blood flow. J Plast Reconstr Aesthet Surg. 2008;61:1226–1231. doi: 10.1016/j.bjps.2007.09.011. [DOI] [PubMed] [Google Scholar]
- 15.Serrera Figallo MA, Velazquez Cayon RT, Torres Lagares D, Corcuera Flores JR, Machuca Portillo G. Use of anesthetics associated to vasoconstrictors for dentistry in patients with cardiopathies. Review of the literature published in the last decade. J Clin Exp Dent. 2012;4:e107–e111. doi: 10.4317/jced.50590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Neema C, Kapur S. Epinephrine toxicity: An avoidable fatal complication due to iatrogenic overdose. Sri Lankan J Aanesthesiol. 2013;21:72–73. [Google Scholar]
- 17.Salonen M, Forssell H, Scheinin M. Local dental anaesthesia with lidocaine and adrenaline. Effects on plasma catecholamines, heart rate and blood pressure. Int J Oral Maxillofac Surg. 1988;17:392–394. doi: 10.1016/s0901-5027(88)80071-7. [DOI] [PubMed] [Google Scholar]
- 18.Meechan JG, Parry G, Rattray DT, Thomason JM. Effects of dental local anaesthetics in cardiac transplant recipients. Br Dent J. 2002;192:161–163. doi: 10.1038/sj.bdj.4801323. [DOI] [PubMed] [Google Scholar]
- 19.Niwa H, Sugimura M, Satoh Y, Tanimoto A. Cardiovascular response to epinephrine-containing local anesthesia in patients with cardiovascular disease. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92:610–616. doi: 10.1067/moe.2001.118903. [DOI] [PubMed] [Google Scholar]
- 20.Knoll-Kohler E, Frie A, Becker J, Ohlendorf D. Changes in plasma epinephrine concentration after dental infiltration anesthesia with different doses of epinephrine. J Dent Res. 1989;68:1098–1101. doi: 10.1177/00220345890680060801. [DOI] [PubMed] [Google Scholar]
- 21.Gerlach RF, Santos JETd, Escobar CAB. The use of epinephrine-containing anesthetic solutions in cardiac patients: A survey. Rev Odontol Univ São Paulo. 1998;12:349–353. [Google Scholar]
- 22.Wakita R, Oono Y, Oogami S, Hayashi S, Umino M. The relation between epinephrine concentration and the anesthetic effect of lidocaine iontophoresis. Pain Pract. 2009;9:115–121. doi: 10.1111/j.1533-2500.2008.00252.x. [DOI] [PubMed] [Google Scholar]
- 23.Haas DA. An update on local anesthetics in dentistry. J Can Dent Assoc. 2002;68:546–551. [PubMed] [Google Scholar]
- 24.Yagiela JA. Vasoconstrictor agents for local anesthesia. Anesth Prog. 1995;42:116–120. [PMC free article] [PubMed] [Google Scholar]
- 25.Karm MH, Park FD, Kang M, Kim HJ, Kang JW, Kim S, et al. Comparison of the efficacy and safety of 2% lidocaine hcl with different epinephrine concentration for local anesthesia in participants undergoing surgical extraction of impacted mandibular third molars: A multicenter, randomized, double-blind, crossover, phase iv trial. Medicine. 2017;96:e6753. doi: 10.1097/MD.0000000000006753. [DOI] [PMC free article] [PubMed] [Google Scholar]