Abstract
Objective
Borderline personality disorder is the prototypical disorder of emotion reactivity and dysregulation, yet there remains limited understanding of its neurocognitive correlates. Two mechanisms that may underlie anomalous reactivity to negative stimuli in borderline patients are impairment in habituation or exaggerated sensitization of activity of the neural salience network, including amygdala, anterior insula (AI), and dorsal anterior cingulate cortex (dACC). The present study attempted to reveal the most plausible mechanism by examining the effect of repeated exposure to emotional images both within and across sessions.
Method
26 borderline patients, 25 avoidant personality disorder patients included as a psychopathological control group, and 24 healthy controls viewed 5 presentations of the same set of negative and neutral images at each of two sessions separated by approximately 3 days, as functional MRI data were acquired. Salience network activity, as measured by blood-oxygen-level dependent signal in anatomically-defined regions-of-interest across the salience network, was compared across groups for each presentation on each of the two study sessions. Self-reported negative affect was also measured for each trial.
Results
Salience network activity showed a main effect of within-session habituation across all groups and sessions. However, a group-by-session interaction was present, such that only borderline patients showed increased salience network activity to the images re-encountered at the second session, and this increased salience network sensitization predicted greater sensitization in self-reported negative affect.
Conclusions
These results elucidate the neural mechanisms by which borderline patients appraise negative social situations as exaggeratedly salient and suggest potential neurocognitive intervention targets.
Borderline personality disorder is characterized by hyper-reactivity to emotional stimuli, severe affective instability, impaired interpersonal relationships, and emotion dysregulation (1-4). The emotional dysregulation has great significance clinically, impacting social functioning, life satisfaction, and identity (1, 5). Although recent work has begun to elucidate the neurobiological correlates underlying emotional hypersensitivity in borderline patients in single sessions (6, 7), an important unanswered question investigated here concerns whether and how these responses are affected as the same negative stimuli are re-encountered. This question is of particular ecological relevance because emotionally salient situations typically present themselves not once, but recurrently over a span of days or longer.
One adaptive, typical response to repeated negative stimulus presentation, over the short or long term, is habituation (8, 9), which relies upon well-established mechanisms at the cellular level involving depression of synaptic transmission (10, 11). Cellular response habituation represents an important physiological mechanism implicated in psychological processes like extinction of conditioned responses (12). While few studies of extinction learning using classical conditioning paradigms exist in borderline personality disorder, one recent study has pointed to delayed extinction in borderline patients (13). Further, and importantly, habituation has been implicated as a key mechanism of action for many desensitization-based psychotherapies, including prolonged exposure therapy (14, 15).
Indeed, for some people, and under some circumstances, responses do not decrease with repeated presentation, but rather increase (i.e. sensitize). One useful theoretical framework views psychological and physiological responses to repeated stimulation as a dual-process: a plasticity of response that involves separable component processes of habituation and sensitization (8). While the tendency toward habituation responses is dependent on factors including the number of identical repetitions, the tendency toward sensitization responses is increased for repeated stimuli that are particularly aversive (i.e. particularly salient) to the recipient of the stimulation (16). We were thus interested to examine the longitudinal profile of psychological and neurophysiological responses to repeated presentation of negative stimuli that were particularly germane to the phenomenology of borderline personality disorder. We also examined these processes in both healthy adult controls as well as avoidant personality disorder patients, who as a near-neighbor personality disorder involving hypersensitivity to negative evaluation (17) as well as intermediate negative emotional reactivity relative to borderline patients and healthy controls (18), represented a psychopathological control group. While comparative behavioral evidence is minimal, both borderline and avoidant patients have failed to exhibit habituation of negative affect self-reports in response to a single repetition of a negative image in an individual session, in contrast to healthy controls (18).
Given that the intense shifts in affect which characterize borderline personality disorder pertain to external or internal cues perceived as meaningful, we chose to focus upon activation of the neural salience network (19), comprised of the amygdala, anterior insula (AI), and dorsal anterior cingulate cortex (dACC). The salience network is involved in integrating sensory, emotional, and cognitive information in order to filter out and amplify information through both bottom-up and top-down means (19-21). The amygdala is a key player in this regard, with a prominent role in assessing the salience (and in the case of negative information, threat value) of a stimulus (22, 23). The AI has been implicated in highly diverse psychological functions related to salience including sensory integration and awareness (20, 24). Further, dACC has been associated with cognitive control, performance monitoring, and executive attention (22, 25).
Among borderline patients and healthy controls, a recent meta-analysis of neuroimaging studies of reactivity to emotional stimuli has shown that, of the salience network regions noted above, the most consistent findings have been observed in the amygdala, with most studies indicating hyper-activation of the amygdala during appraisal of emotional stimuli (i.e. faces and scenes) in borderline patients relative to healthy controls (6). A second recent neuroimaging meta-analysis of borderline versus healthy activation differences during emotion processing has likewise indicated consistent evidence for amygdala hyper-activation in borderline patients (26). Meta-analysis results of borderline versus healthy group differences in emotion reactivity in AI and ACC have been more mixed (6, 26). In the AI, the quantitative meta-analysis (26) indicated hyper-activation in borderline patients relative to healthy controls, whereas two of the nine studies included in the other meta-analysis (6) reported hypo-activation of anterior insula in borderline patients relative to healthy controls, with the other seven not indicating a result in that region.
While a relatively small but growing number of functional neuroimaging studies have examined borderline patients, only two functional neuroimaging studies have examined avoidant personality disorder patients in any context, finding evidence for hyper-activation of the amygdala during anticipation of engaging in emotion regulation in avoidant patients relative to healthy controls (27) as well as under-recruitment of the dACC in avoidant patients relative to healthy controls in the context of habituation to a single repetition of a negative stimulus (18). Borderline patients were likewise shown to exhibit hypo-activation of dACC relative to healthy controls in this single repetition habituation paradigm (18).
Thus, given the clinical relevance of examining habituation processes over a longer time course than a single repetition of a negative stimulus, our principal focus in the present study was to test whether and how borderline patients differed from avoidant patients and healthy controls in terms of longitudinal habituation and sensitization to several presentations of a negative stimulus over multiple days, as measured by both functional magnetic resonance imaging (fMRI) and trial-by-trial self-reports of negative affect. In terms of neural activity, our primary interest concerned habituation or sensitization of the salience network as a whole, with the component regions noted above (amygdala, AI, dACC) defined anatomically and independently of study data. We predicted that negative affect reports and salience network activity would show hyper-activation in borderline patients relative to avoidant patients and healthy controls, manifesting either as diminished longitudinal response habituation or anomalous longitudinal response sensitization to negative stimuli.
Method
Participants
We recruited 30 borderline patients, 31 avoidant patients, and 33 healthy control participants from outpatient clinics at the Mount Sinai Medical Center and the James J. Peters VA Medical Center in New York City as well as from newspaper and online advertisements. All participants provided written informed consent after procedures were fully explained. Exclusions due to motion, signal quality, and related issues are detailed in Supplemental Material. In total, 4 borderline patients, 6 avoidant patients, and 9 healthy controls were excluded, yielding an analyzable total of 26 borderline patients (mean age = 37.0 years; 15 female), 25 avoidant patients (mean age = 37.2 years; 13 female), and 24 healthy controls (mean age = 32.6 years; 11 female). There were no significant age differences by group (F(2,72)=1.92, p=0.15, n.s.; all pairwise t-tests n.s.), and there was no significant differences in gender ratio (χ2 (2,75)=0.70, p=0.70, n.s.). The groups did not differ in years of education (borderline patients: 14.6 ± 2.4; avoidant patients: 14.3 ± 2.8; healthy controls: 15.6 ± 3.3; all pairwise two-tailed t-tests n.s.).
Borderline participants met DSM-IV criteria for borderline personality disorder, including the affective instability criterion. Avoidant participants met DSM-IV criteria for avoidant personality disorder but not criteria for borderline personality disorder. Borderline and avoidant participants did not meet DSM-IV criteria for past or present bipolar I disorder, schizophrenia, or schizoaffective disorder. Avoidant participants did not meet criteria for past or present PTSD. Borderline and avoidant participant comorbidities are given in Supplemental Material. Participants had to be psychotropic medication free for 2 weeks (6 weeks in the case of fluoxetine). Healthy participants did not meet DSM-IV criteria for any axis I or axis II disorder. Diagnostic assessments were obtained using the Structured Clinical Interview for DSM-IV–Patient Edition and the Structured Clinical Interview for DSM-IV Axis II Personality Disorders. Our group has achieved an interrater reliability of 0.81 for diagnosing borderline personality disorder.
Materials
A total of 30 negative and 30 neutral images were used. All images (negative and neutral) were social, depicting two or more people interacting. All negative images contained themes specifically relevant to borderline personality disorder, including interpersonal rejection, sadness, frustration, anger, and violence. Images were drawn from the Empathy Picture System (28) and online image repositories and rated using the Self-Assessment Manikin (29) for comparability (see Supplemental Material).
Task Design
Participants completed a habituation task during fMRI scanning at two separate sessions. At Session 1, participants saw 5 presentations of each of the 30 negative and 30 neutral task images, divided into 3 equally-sized functional runs of 10 negative images (with 5 presentations of each) and 10 neutral images (with 5 presentations of each). Thus, 100 total image presentations occurred per each of the 3 runs (50 image presentations per valence per run), and 300 total image presentations occurred overall at Session 1. Image presentation order was pseudorandomly counterbalanced across participants. Each trial consisted of an image presentation (3 s), a negative affect rating (3 s), and a brief fixation interval (1 s). During image presentation, participants were instructed to simply look and respond naturally to each image, keeping their eyes on it the entire time. During the negative affect rating period, participants were instructed to provide a rating of their current level of negative affect on a scale of 1-5 (1=least negative; 5=most negative).
Session 2 followed Session 1 by approximately 3 days. At Session 2, participants returned to the fMRI scanner and viewed the same images presented in the original order that they had seen at Session 1.
Data Acquisition and Analysis
Self-Reported Negative Affect
Self-reported negative affect ratings were acquired using a 5-button response glove during fMRI scanning and recorded using E-Prime software (Psychology Software Tools, Inc.). Self-reported affect data were analyzed using linear mixed models incorporating fixed effect estimates for Group (borderline, avoidant, healthy control), Session (1 and 2), Valence (negative and neutral), and Presentation Order (presentation 1, 2, 3, 4, 5), and their interactions, and a random effect consisting of an intercept for each participant.
Functional MRI
Whole-brain fMRI data were acquired using a 3.0T Philips Achieva scanner (see Supplemental Material for acquisition and preprocessing information). A random-effects general linear model (GLM) was computed with regressors corresponding to the interaction of three conditions (Session, Valence, and Presentation Order; see Supplemental Material for details, including for the exploratory whole-brain analysis).
Anatomical Definitions of Salience Network Regions-of-Interest (ROI’s)
As our primary hypotheses concerned activation of a priori-defined regions of the salience network, we defined ROI’s for right and left amygdala, right and left AI, and dACC using standard anatomical atlases (30, 31). Details of each ROI are given in Supplemental Material.
As our hypotheses principally concerned salience network activity as a whole, in order to provide a unified test of our hypotheses, we constructed a network activity estimate. While component anatomically-defined ROI’s varied in size (see Supplemental Material), all five ROI’s were hypothesized to contribute equally to salience network activity. Therefore, salience network activity was defined as the average of activity estimates for each of the five component ROI’s (i.e. right and left amygdala, right and left AI, and dACC). Neural activity was further examined within each ROI in particular. Neural activity was then analyzed using linear mixed models using the factors described above for analysis of self-reported negative affect ratings.
Results
Self-Reported Negative Affect
Figure 1 shows negative affect self-reports during the habituation task. As expected, a main effect of Valence was present (negative>neutral), F(1,1368)=2814.31, p<0.01. There was no significant effect of Presentation Order, F(4,1368)=0.15, n.s., indicating that there was little within-session habituation overall. However, a marginal main effect of Session was present (Session 2 < Session 1), F(1,1368)=3.18, p<0.08, indicating global habituation across sessions. Further, a marginal Group-by-Valence interaction was present, F(2,1368)=2.70, p<0.07.
Figure 1.
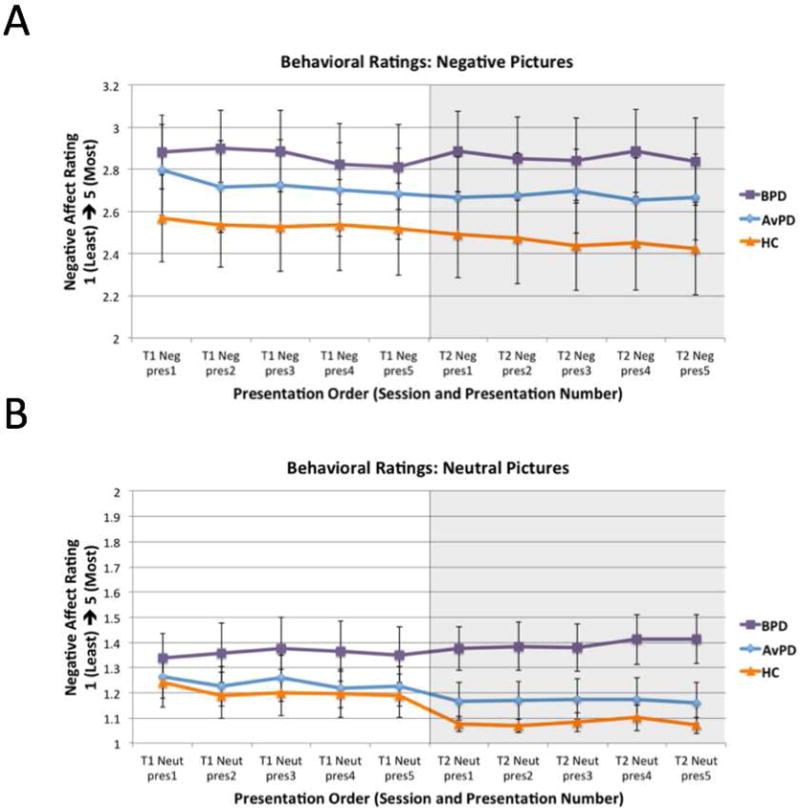
Negative affect ratings (A: negative images; B: neutral images). T1 refers to Session 1 and T2 refers to Session 2. Pres refers to Presentation Order.
In order to unpack this interaction, and given our hypotheses concerning responses to negative images in particular, we examined responses in each valence individually. Among negative images (Figure 1A), there was a main effect of Session, indicating habituation across sessions overall, F(1,648)=8.73, p<0.01. Further, a marginal Group-by-Session interaction was present, indicating a trend toward borderline patients having shown less change over time (i.e. diminished habituation) relative to the other groups, F(2,648)=2.50, p<0.09. This is illustrated by within-group comparisons showing change over time was not significant for borderline patients (either from the first to last presentation [t(25)=0.51, p=0.62, two-tailed, n.s.; Bayes factor (32) = 0.15; Bayes factor <1, indicating that the null finding is not driven by data insensitivity], nor from the average of the first session to the second [t(25)=0.00, p=0.99, two-tailed, n.s.; Bayes factor (32) = 0.11]), whereas a decrease in negativity over time from the first to last presentation was significant in healthy controls, t(23)=2.27, p<0.04, two-tailed. Avoidant patients showed a trend toward Session 1 habituation, t(24)=1.88, p<0.08, two-tailed, but no between-session habituation, t(24)=0.71, p=0.48, two-tailed, n.s, nor a difference from first to last presentation, t(24)=1.38, p=0.18, two-tailed.
Among neutral images (Figure 1B), there was similarly a main effect of Session, F(1,648)=16.46, p<0.01, indicating global between-session habituation. In addition, there was a significant Group-by-Session interaction, F(2,648)=13.16, p<0.01. Here too, the healthy controls showed a marginal decrease in negative affect from first to last presentation (t(23)=1.97, p<0.07, two-tailed), and the avoidant patients also showed a marginal decrease (t(23)=2.06, p=0.06, two-tailed), whereas the borderline patients instead showed an anomalous trend toward sensitization over time (t(25)=1.45, p=0.09, one-tailed).
fMRI
Salience Network Activity
In order to examine habituation and sensitization processes in the brain, we examined overall activity of the salience network (Figure 2). In addition to a main effect of Valence (negative>neutral), F(1,1368)=16.37, p<0.01, there was a main effect of Presentation Order, F(4,1368)=11.55, p<0.01, reflecting significant within-session habituation overall across all groups (see Supplemental Material). Further, there was a significant Valence-by-Presentation Order interaction, F(4,1368)=2.50, p<0.05, indicating greater within-session habituation for negative images relative to neutral images overall.
Figure 2.
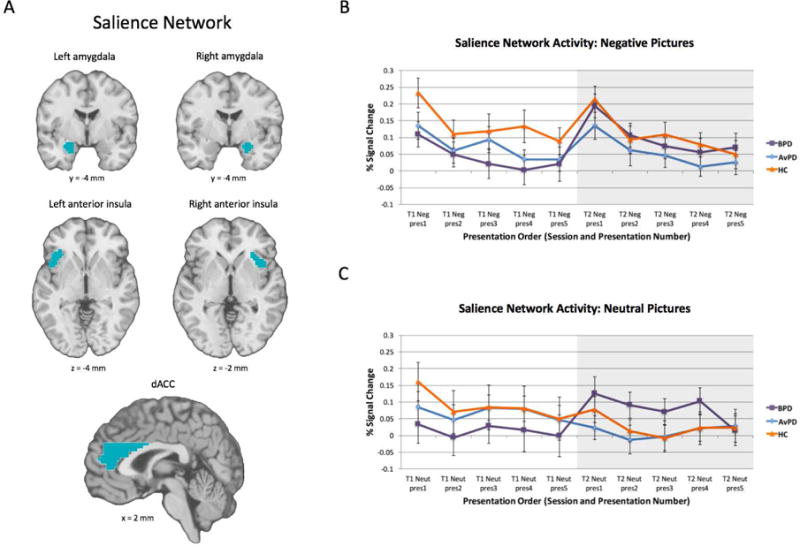
Salience network activity during the longitudinal habituation task. (A: network component ROI definitions; B: activity for negative images; C: activity for neutral images). T1 refers to Session 1 and T2 refers to Session 2. Pres refers to Presentation Order.
Importantly, there was also a significant Group-by-Session interaction, F(2,1368)=14.74, p<0.01, with borderline patients showing anomalous between-session sensitization overall. Given our particular hypotheses regarding responses to negative images, we investigated this interaction in each valence separately. Indeed, this anomalous between-session sensitization of salience network activity was present for both negative images alone, F(2,648)=6.90, p<0.01, as well as neutral images alone, F(2,648)=8.16, p<0.01. Among negative images, this interaction is illustrated by an anomalous trend toward elevated salience network activity across sessions (i.e. between-session sensitization) in borderline patients, t(25)=1.69, p<0.06, one-tailed, whereas there was no change in activity across sessions for healthy controls (t(23)=0.81, n.s.) or avoidant patients (t(24)=0.44, n.s.).
As an exploratory analysis, we further examined self-reported negative affect and salience network activity in avoidant patients as a function of presence or absence of comorbidity with social phobia (i.e. the comorbidity with the largest sample size across participants, as 11 avoidant patients were comorbid with social phobia; see Supplemental Material and Figure S1).
Salience Network Component ROI’s
While our primary interest was in assessing activity of the salience network overall, we further investigated activity in each of the anatomically-defined salience network component ROI’s individually (see Supplemental Material and Figures S2-S6 for right amygdala, left amygdala, right AI, left AI, and dACC activity, respectively). As described in greater detail in Supplemental Material, these results further characterize the salience network results above, with broadly consistent results across regions, but evidence of a laterality asymmetry. Specifically, activity in right amygdala, right AI, and dACC illustrated the Group-by-Session interaction indicated above with anomalous between-session sensitization of response in borderline patients, whereas left amygdala and left AI activity did not show significant change across sessions in borderline patients (see Supplemental Material).
Correlation between self-reported negative affect and salience network activity among borderline patients
In addition, a brain-behavior correlation was observed among borderline patients, with greater longitudinal sensitization of salience network activity (i.e. greater average activity in Session 2 relative to Session 1 for negative images) predicting greater longitudinal sensitization of self-reported negative affect ratings defined in the same way, r=0.38, p<0.03, one-tailed (Figure 3).
Figure 3.
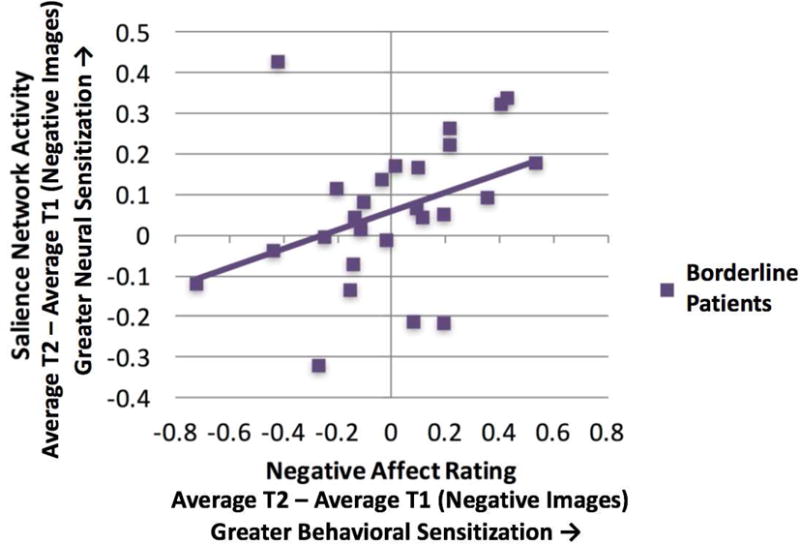
Among borderline patients, greater longitudinal sensitization of salience network activity for negative images predicts greater longitudinal sensitization of self-reported negative affect.
Exploratory Whole-Brain Analysis
No additional regions met multiple comparison correction criteria for significant sensitization or habituation across sessions for either valence in any group (see Supplemental Material).
Discussion
In this study, we examined anomalies in within and between-session habituation and sensitization, dual processes that are clinically relevant to the phenomenology of borderline personality disorder, in borderline patients, avoidant personality disorder patients, and healthy controls. Given prior work examining emotional reactivity to negative stimuli in borderline patients and healthy controls, we hypothesized that self-reports of negative affect and activity of the salience network (i.e. including amygdala, anterior insula, and dACC; 19, 21) would be differentially recruited across groups with regard to their habituation and sensitization profile, in particular by reflecting either diminished habituation or exaggerated sensitization in the borderline group.
While the current results support comparable habituation responses across groups within-session, we found evidence of diminished habituation and anomalous sensitization in borderline patients between sessions. The self-reported negative affect data supported this hypothesis in that borderline patients showed diminished habituation of response across sessions for both negative and neutral social images (i.e. diminished habituation in response to negative images, and, for neutral images, an anomalous marginal trend toward increase in self-reported negative affect over the course of the experiment). Further, salience network activity supported our hypothesis regarding anomalous longitudinal sensitization in borderline patients. While all groups exhibited initial within-session habituation, only borderline patients showed a between-session rise in salience network activity. As further validation of the current fMRI results, we found evidence that, between sessions, behavioral sensitization (i.e. increased negative affect reports) predicted salience network sensitization in borderline patients. These results are consistent with the salience network’s role in assigning value and importance to environmental stimuli (19, 21-23).
Interestingly, this between-session salience network sensitization pattern was also observed for neutral images, potentially suggesting top-down negative emotion generation in borderline patients, whereby even neutral social stimuli are appraised as relatively negative (33, 34). Thus, the longitudinal sensitization observed for borderline patients among neutral as well as negative social stimuli may reflect anomalous negative appraisal processes in borderline patients, inferring negativity in social situations where it does not objectively exist. This interpretation is consistent with the observed self-reported negative affect data for neutral images, which showed diminished habituation and anomalously negative overall negative affect reports for neutral images in borderline patients relative to the other groups.
While our primary focus was on activity of the salience network as a whole, it is noteworthy that laterality played a role in the salience network results. Between-session sensitization effects in borderline patients were observed in only one laterality for amygdala and AI (i.e. only in the right but not left hemisphere). At the same time, an exploratory laterality analysis indicated that left hemisphere responses to the social picture stimuli used in this experiment in these regions were stronger overall than right hemisphere responses across groups and valences. While some evidence in healthy adults has suggested that the right hemisphere may be relatively attuned to negative (versus positive) stimulus processing (35-37), some quantitative meta-analyses have called the reliability of this effect into question (38), and, consistent with the current laterality results, a true account may be more nuanced (39) and depend on person factors (e.g. group) as well as context.
The need for the use of appropriate clinical control groups has been highlighted in the literature in order to establish psychopathological specificity (6). Here, we examined avoidant personality disorder patients in parallel with borderline patients and healthy controls. Prior work has shown avoidant patients to exhibit intermediate negative reactivity relative to borderline patients and healthy controls (18), which is also supported in the present negative affect results. However, overall avoidant patients showed longitudinal neural response profiles in the salience network that resembled those of healthy controls rather than borderline patients. While clinically near-neighbor, avoidant and borderline personality disorders may draw upon somewhat divergent neural networks (18). Additionally, from a dimensional perspective, avoidant personality disorder may not have reached the threshold for maladaptive reactivity that’s associated with anomalous sensitization in the manner shown by borderline patients.
Further, while this was not a conditioning study, the present salience network results in borderline patients may be relevant to the phenomenon of spontaneous recovery in extinction paradigms (12, 13, 40). Although borderline patients showed initial habituation responses that paralleled those of avoidant patients and healthy controls, the anomalous sensitization exhibited by borderline patients may be reflective of the reemergence of a salience response to particularly population-relevant stimuli following a delay of approximately 3 days.
In conclusion, the present work suggests that borderline patients may ascribe hyper-salient significance to repeated negative social stimuli via hyper-activation of the neural salience network. Awareness of evidence for longitudinal sensitization in borderline patients may have implications for the psychotherapy of borderline personality disorder. For example, it may help patients and psychotherapists to better understand and prepare for the not uncommon experience that when salient emotional episodes are revisited in successive psychotherapy sessions of borderline patients, reactions intensify rather than subside. This could have implications for the optimal timing of therapeutic interventions or militate against treatment approaches predicated heavily upon systematic desensitization strategies.
Supplementary Material
Acknowledgments
This work was supported by NIH grant R01 MH077813 to HWK, NIH grant F32 MH105119 to BTD, and the James J Peters VA Medical Center.
Footnotes
Disclosures
The authors report no financial relationships with commercial interests.
References
- 1.Skodol AE, Gunderson JG, Pfohl B, Widiger TA, Livesley WJ, Siever LJ. The borderline diagnosis I: psychopathology, comorbidity, and personality structure. Biological psychiatry. 2002;51:936–950. doi: 10.1016/s0006-3223(02)01324-0. [DOI] [PubMed] [Google Scholar]
- 2.Skodol AE, Siever LJ, Livesley WJ, Gunderson JG, Pfohl B, Widiger TA. The borderline diagnosis II: biology, genetics, and clinical course. Biological psychiatry. 2002;51:951–963. doi: 10.1016/s0006-3223(02)01325-2. [DOI] [PubMed] [Google Scholar]
- 3.Tomko RL, Trull TJ, Wood PK, Sher KJ. Characteristics of borderline personality disorder in a community sample: comorbidity, treatment utilization, and general functioning. Journal of personality disorders. 2014;28:734–750. doi: 10.1521/pedi_2012_26_093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Carpenter RW, Trull TJ. Components of emotion dysregulation in borderline personality disorder: a review. Curr Psychiatry Rep. 2013;15:335. doi: 10.1007/s11920-012-0335-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Koenigsberg HW, Harvey PD, Mitropoulou V, Schmeidler J, New AS, Goodman M, Silverman JM, Serby M, Schopick F, Siever LJ. Characterizing affective instability in borderline personality disorder. The American journal of psychiatry. 2002;159:784–788. doi: 10.1176/appi.ajp.159.5.784. [DOI] [PubMed] [Google Scholar]
- 6.van Zutphen L, Siep N, Jacob GA, Goebel R, Arntz A. Emotional sensitivity, emotion regulation and impulsivity in borderline personality disorder: a critical review of fMRI studies. Neurosci Biobehav Rev. 2015;51:64–76. doi: 10.1016/j.neubiorev.2015.01.001. [DOI] [PubMed] [Google Scholar]
- 7.Hazlett EA, Zhang J, New AS, Zelmanova Y, Goldstein KE, Haznedar MM, Meyerson D, Goodman M, Siever LJ, Chu KW. Potentiated amygdala response to repeated emotional pictures in borderline personality disorder. Biological psychiatry. 2012;72:448–456. doi: 10.1016/j.biopsych.2012.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Groves PM, Thompson RF. Habituation: a dual-process theory. Psychological review. 1970;77:419–450. doi: 10.1037/h0029810. [DOI] [PubMed] [Google Scholar]
- 9.Thompson RF, Spencer WA. Habituation: a model phenomenon for the study of neuronal substrates of behavior. Psychological review. 1966;73:16–43. doi: 10.1037/h0022681. [DOI] [PubMed] [Google Scholar]
- 10.Castellucci V, Kandel ER. A quantal analysis of the synaptic depression underlying habituation of the gill-withdrawal reflex in Aplysia. Proceedings of the National Academy of Sciences of the United States of America. 1974;71:5004–5008. doi: 10.1073/pnas.71.12.5004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Castellucci V, Pinsker H, Kupfermann I, Kandel ER. Neuronal mechanisms of habituation and dishabituation of the gill-withdrawal reflex in Aplysia. Science. 1970;167:1745–1748. doi: 10.1126/science.167.3926.1745. [DOI] [PubMed] [Google Scholar]
- 12.McSweeney FK, Swindell S. Common processes may contribute to extinction and habituation. J Gen Psychol. 2002;129:364–400. doi: 10.1080/00221300209602103. [DOI] [PubMed] [Google Scholar]
- 13.Krause-Utz A, Keibel-Mauchnik J, Ebner-Priemer U, Bohus M, Schmahl C. Classical conditioning in borderline personality disorder: an fMRI study. Eur Arch Psychiatry Clin Neurosci. 2016;266:291–305. doi: 10.1007/s00406-015-0593-1. [DOI] [PubMed] [Google Scholar]
- 14.Foa EB. Prolonged exposure therapy: past, present, and future. Depress Anxiety. 2011;28:1043–1047. doi: 10.1002/da.20907. [DOI] [PubMed] [Google Scholar]
- 15.Sripada RK, Rauch SA. Between-session and within-session habituation in Prolonged Exposure Therapy for posttraumatic stress disorder: a hierarchical linear modeling approach. J Anxiety Disord. 2015;30:81–87. doi: 10.1016/j.janxdis.2015.01.002. [DOI] [PubMed] [Google Scholar]
- 16.Hinde RA. Animal behavior: A synthesis of ethology and comparative psychology. New York: McGraw-Hill; 1966. [Google Scholar]
- 17.Sanislow CA, Bartolini EE, Zoloth EC. Avoidant personality disorder in Encyclopedia of Human Behavior Edited by Ramachandran VS. 2nd. San Diego: Academic Press; 2012. pp. 257–266. [Google Scholar]
- 18.Koenigsberg HW, Denny BT, Fan J, Liu X, Guerreri S, Mayson SJ, Rimsky L, New AS, Goodman M, Siever LJ. The neural correlates of anomalous habituation to negative emotional pictures in borderline and avoidant personality disorder patients. The American journal of psychiatry. 2014;171:82–90. doi: 10.1176/appi.ajp.2013.13070852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Menon V. Salience network in Brain Mapping: An Encyclopedic Reference Edited by Toga AW. Oxford, UK: Academic Press: Elsevier; 2015. pp. 597–611. [Google Scholar]
- 20.Craig AD. How do you feel–now? The anterior insula and human awareness. Nat Rev Neurosci. 2009;10:59–70. doi: 10.1038/nrn2555. [DOI] [PubMed] [Google Scholar]
- 21.Menon V, Uddin LQ. Saliency, switching, attention and control: a network model of insula function. Brain structure & function. 2010;214:655–667. doi: 10.1007/s00429-010-0262-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ochsner KN, Silvers JA, Buhle JT. Functional imaging studies of emotion regulation: a synthetic review and evolving model of the cognitive control of emotion. Annals of the New York Academy of Sciences. 2012;1251:E1–24. doi: 10.1111/j.1749-6632.2012.06751.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.LeDoux J. The emotional brain, fear, and the amygdala. Cell Mol Neurobiol. 2003;23:727–738. doi: 10.1023/A:1025048802629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Craig AD. Interoception: the sense of the physiological condition of the body. Curr Opin Neurobiol. 2003;13:500–505. doi: 10.1016/s0959-4388(03)00090-4. [DOI] [PubMed] [Google Scholar]
- 25.Fan J, McCandliss BD, Fossella J, Flombaum JI, Posner MI. The activation of attentional networks. NeuroImage. 2005;26:471–479. doi: 10.1016/j.neuroimage.2005.02.004. [DOI] [PubMed] [Google Scholar]
- 26.Schulze L, Schmahl C, Niedtfeld I. Neural Correlates of Disturbed Emotion Processing in Borderline Personality Disorder: A Multimodal Meta-Analysis. Biological psychiatry. 2016;79:97–106. doi: 10.1016/j.biopsych.2015.03.027. [DOI] [PubMed] [Google Scholar]
- 27.Denny BT, Fan J, Liu X, Ochsner KN, Guerreri S, Mayson SJ, Rimsky L, McMaster A, New AS, Goodman M, Siever LJ, Koenigsberg HW. Elevated amygdala activity during reappraisal anticipation predicts anxiety in avoidant personality disorder. J Affect Disord. 2015;172:1–7. doi: 10.1016/j.jad.2014.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Geday J, Gjedde A, Boldsen AS, Kupers R. Emotional valence modulates activity in the posterior fusiform gyrus and inferior medial prefrontal cortex in social perception. NeuroImage. 2003;18:675–684. doi: 10.1016/s1053-8119(02)00038-1. [DOI] [PubMed] [Google Scholar]
- 29.Bradley MM, Lang PJ. Measuring emotion: the Self-Assessment Manikin and the Semantic Differential. J Behav Ther Exp Psychiatry. 1994;25:49–59. doi: 10.1016/0005-7916(94)90063-9. [DOI] [PubMed] [Google Scholar]
- 30.Maldjian JA, Laurienti PJ, Kraft RA, Burdette JH. An automated method for neuroanatomic and cytoarchitectonic atlas-based interrogation of fMRI data sets. NeuroImage. 2003;19:1233–1239. doi: 10.1016/s1053-8119(03)00169-1. [DOI] [PubMed] [Google Scholar]
- 31.Lancaster JL, Woldorff MG, Parsons LM, Liotti M, Freitas CS, Rainey L, Kochunov PV, Nickerson D, Mikiten SA, Fox PT. Automated Talairach atlas labels for functional brain mapping. Human brain mapping. 2000;10:120–131. doi: 10.1002/1097-0193(200007)10:3<120::AID-HBM30>3.0.CO;2-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dienes Z. Using Bayes to get the most out of non-significant results. Front Psychol. 2014;5:781. doi: 10.3389/fpsyg.2014.00781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ochsner KN, Ray RR, Hughes B, McRae K, Cooper JC, Weber J, Gabrieli JD, Gross JJ. Bottom-up and top-down processes in emotion generation: common and distinct neural mechanisms. Psychological science. 2009;20:1322–1331. doi: 10.1111/j.1467-9280.2009.02459.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Donegan NH, Sanislow CA, Blumberg HP, Fulbright RK, Lacadie C, Skudlarski P, Gore JC, Olson IR, McGlashan TH, Wexler BE. Amygdala hyperreactivity in borderline personality disorder: implications for emotional dysregulation. Biological psychiatry. 2003;54:1284–1293. doi: 10.1016/s0006-3223(03)00636-x. [DOI] [PubMed] [Google Scholar]
- 35.Davidson RJ. Anterior cerebral asymmetry and the nature of emotion. Brain Cogn. 1992;20:125–151. doi: 10.1016/0278-2626(92)90065-t. [DOI] [PubMed] [Google Scholar]
- 36.Davidson RJ, Irwin W. The functional neuroanatomy of emotion and affective style. Trends in cognitive sciences. 1999;3:11–21. doi: 10.1016/s1364-6613(98)01265-0. [DOI] [PubMed] [Google Scholar]
- 37.Lichtenstein-Vidne L, Gabay S, Cohen N, Henik A. Lateralisation of emotions: evidence from pupil size measurement. Cogn Emot. 2017;31:699–711. doi: 10.1080/02699931.2016.1164668. [DOI] [PubMed] [Google Scholar]
- 38.Wager TD, Phan KL, Liberzon I, Taylor SF. Valence, gender, and lateralization of functional brain anatomy in emotion: a meta-analysis of findings from neuroimaging. NeuroImage. 2003;19:513–531. doi: 10.1016/s1053-8119(03)00078-8. [DOI] [PubMed] [Google Scholar]
- 39.Lindquist KA, Wager TD, Kober H, Bliss-Moreau E, Barrett LF. The brain basis of emotion: a meta-analytic review. Behav Brain Sci. 2012;35:121–143. doi: 10.1017/S0140525X11000446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Estes WK. Statistical theory of spontaneous recovery and regression. Psychological review. 1955;62:145–154. doi: 10.1037/h0048509. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


