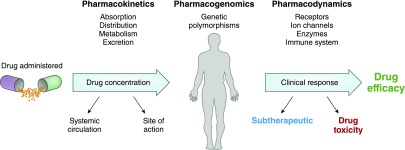
Drugs form the cornerstone of treatment for a plethora of diseases, including kidney disease and its common comorbid conditions. Patients with kidney disease are routinely prescribed numerous drugs simultaneously. For instance, patients with CKD not dependent on dialysis are prescribed a mean of six to 12 medications (1), whereas patients with ESKD take a median number of 19 pills per day, with 25% of patients with ESKD taking >25 medications daily (2). Hospitalized patients with AKI are also exposed to a large number of medications. Several factors affect the clinical pharmacology of drugs in humans, including pharmacokinetics, pharmacogenetics, and pharmacodynamics (Figure 1). Impaired kidney function leads to changes in pharmacokinetics and pharmacodynamics; thus, commonly used drugs frequently exhibit altered risk-benefit profiles in patients with CKD (3). Unfortunately, clinical trials are notorious for excluding patients with kidney disease (4,5), often leading to a lack of data to inform drug selection and dosing and forcing clinicians to extrapolate clinical data derived from the general population to patients with CKD. It is no surprise then that patients with CKD experience increased rates of adverse drug events and toxicity compared with those with normal kidney function (6). There is even less pharmacologic data available to clinicians on patients with AKI (7). These issues underscore the importance of “Nephropharmacology for the Clinician,” the latest educational series to appear in the Clinical Journal of the American Society of Nephrology (CJASN).
Figure 1.
Several factors affect clinical pharmacology in humans.
We believe that this series fills an important gap in the nephropharmacology literature, providing reviews of topics that generally fit into four categories (Table 1). The series begins with this issue of the CJASN, providing the first of several reviews covering basic principles of clinical pharmacology in kidney disease, including clinically applied pharmacokinetics, pharmacodynamics, and pharmacogenomics. The second group of reviews relates to fundamentally important pharmacologic considerations in kidney disease, including kidney function estimates for drug dosing, medication safety principles, common drug nephrotoxicities, and use of technology to prevent nephrotoxicity. Underpinning the series is a collection of reviews that comprise the third group and present clinical pharmacologic aspects of commonly used drug classes from a nephrocentric perspective. The series concludes with reviews of emerging issues in nephropharmacology, including use of biosimilars and the regulatory perspective on drug development.
Table 1.
Topics to be included in the educational series “Nephropharmacology for the Clinician”
| Review Categories and Topics |
|---|
| Basic principles |
| Pharmacokinetics |
| Pharmacodynamics |
| Pharmacogenomics |
| Fundamentally important considerations in nephropharmacology |
| Kidney function estimates for drug dosing |
| Medication safety principles and practice |
| Pharmacology behind common drug nephrotoxicities |
| EMR alerts to prevent drug nephrotoxicity |
| Contemporary perspectives on drug use in kidney disease |
| Pain management |
| Anticoagulants |
| Diuretics |
| Antihypertensives |
| HIV therapy |
| Antibiotics |
| Emerging topics |
| Biosimilars |
| Regulatory perspective |
EMR, electronic medical record.
The editors have assembled a team of highly regarded physicians, clinical pharmacologists, researchers, and regulatory scientists to contribute to this important educational series. The reviews are intentionally brief but comprehensive, contemporary, and clinically applied. We anticipate that the series will be a vital resource for clinical practitioners and trainees alike related to basic principles and considerations that are fundamentally important in the use of drugs in patients with kidney disease.
Disclosures
None.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
See related article, “Clinical Pharmacokinetics in Kidney Disease: Fundamental Principles,” on pages 1085–1095.
References
- 1.Burnier M, Pruijm M, Wuerzner G, Santschi V: Drug adherence in chronic kidney diseases and dialysis. Nephrol Dial Transplant 30: 39–44, 2015 [DOI] [PubMed] [Google Scholar]
- 2.Chiu YW, Teitelbaum I, Misra M, de Leon EM, Adzize T, Mehrotra R: Pill burden, adherence, hyperphosphatemia, and quality of life in maintenance dialysis patients. Clin J Am Soc Nephrol 4: 1089–1096, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Matzke GR, Aronoff GR, Atkinson AJ Jr, Bennett WM, Decker BS, Eckardt KU, Golper T, Grabe DW, Kasiske B, Keller F, Kielstein JT, Mehta R, Mueller BA, Pasko DA, Schaefer F, Sica DA, Inker LA, Umans JG, Murray P: Drug dosing consideration in patients with acute and chronic kidney disease-a clinical update from Kidney Disease: Improving Global Outcomes (KDIGO). Kidney Int 80: 1122–1137, 2011 [DOI] [PubMed] [Google Scholar]
- 4.Coca SG, Krumholz HM, Garg AX, Parikh CR: Underrepresentation of renal disease in randomized controlled trials of cardiovascular disease. JAMA 296: 1377–1384, 2006 [DOI] [PubMed] [Google Scholar]
- 5.Konstantinidis I, Nadkarni GN, Yacoub R, Saha A, Simoes P, Parikh CR, Coca SG: Representation of patients with kidney disease in trials of cardiovascular interventions: An updated systematic review. JAMA Intern Med 176: 121–124, 2016 [DOI] [PubMed] [Google Scholar]
- 6.Hug BL, Witkowski DJ, Sox CM, Keohane CA, Seger DL, Yoon C, Matheny ME, Bates DW: Occurrence of adverse, often preventable, events in community hospitals involving nephrotoxic drugs or those excreted by the kidney. Kidney Int 76: 1192–1198, 2009 [DOI] [PubMed] [Google Scholar]
- 7.Goldstein SL, Nolin TD: Lack of drug dosing guidelines for critically ill patients receiving continuous renal replacement therapy. Clin Pharmacol Ther 96: 159–161, 2014 [DOI] [PubMed] [Google Scholar]