Abstract
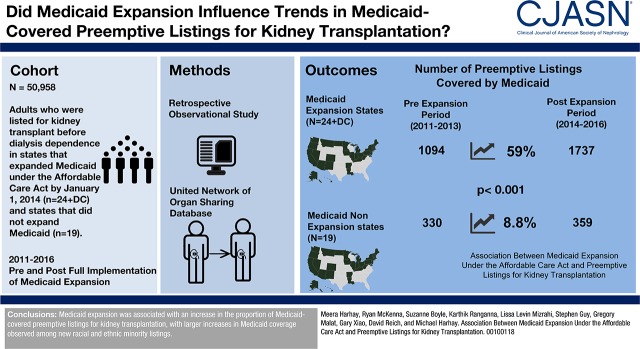
Background and objectives
Before 2014, low-income individuals in the United States with non–dialysis-dependent CKD had fewer options to attain health insurance, limiting their opportunities to be preemptively wait-listed for kidney transplantation. We examined whether expanding Medicaid under the Affordable Care Act was associated with differences in the number of individuals who were pre-emptively wait-listed with Medicaid coverage.
Design, setting, participants, & measurements
Using the United Network of Organ Sharing database, we performed a retrospective observational study of adults (age≥18 years) listed for kidney transplantation before dialysis dependence between January 1, 2011–December 31, 2013 (pre-Medicaid expansion) and January 1, 2014–December 31, 2016 (post-Medicaid expansion). In multinomial logistic regression models, we compared trends in insurance types used for pre-emptive wait-listing in states that did and did not expand Medicaid with a difference-in-differences approach.
Results
States that fully implemented Medicaid expansion on January 1, 2014 (“expansion states,” n=24 and the District of Columbia) had a 59% relative increase in Medicaid-covered pre-emptive listings from the pre-expansion to postexpansion period (from 1094 to 1737 listings), compared with an 8.8% relative increase (from 330 to 359 listings) among 19 Medicaid nonexpansion states (P<0.001). From the pre- to postexpansion period, the adjusted proportion of listings with Medicaid coverage decreased by 0.3 percentage points among nonexpansion states (from 4.0% to 3.7%, P=0.09), and increased by 3.0 percentage points among expansion states (from 7.0% to 10.0%, P<0.001). Medicaid expansion was associated with absolute increases in Medicaid coverage by 1.4 percentage points among white listings, 4.0 percentage points among black listings, 5.9 percentage points among Hispanic listings, and 5.3 percentage points among other listings (P<0.001 for all comparisons).
Conclusions
Medicaid expansion was associated with an increase in the proportion of new pre-emptive listings for kidney transplantation with Medicaid coverage, with larger increases in Medicaid coverage among racial and ethnic minority listings than among white listings.
Keywords: Adult; Ethnic Groups; European Continental Ancestry Group; Hispanic Americans; Humans; Insurance, Health; kidney transplantation; Logistic Models; Medicaid; Patient Protection and Affordable Care Act; renal dialysis; Renal Insufficiency, Chronic; Retrospective Studies; United States
Introduction
January 1, 2014 marked the beginning of full implementation of Medicaid expansion in the United States under the Patient Protection and Affordable Care Act (ACA). On this date, the federal government enhanced funding to states that elected to expand Medicaid to cover low-income adults at or below 138% of the federal poverty level, and instated other policies to streamline Medicaid applications and promote outreach (1,2). To date, Medicaid expansion has provided insurance coverage to 11 million previously uninsured individuals (3). Studies are needed to determine the extent to which these national gains in insurance coverage may have implications for existing disparities in the care of low-income patients with CKD (4).
Because individuals with CKD can accrue additional waiting time for kidney transplantation if they are wait-listed before starting chronic dialysis (5), pre-emptive wait-listing is a recommended strategy to minimize pretransplant dialysis exposure (6,7). However, access to the kidney transplant waiting list is generally contingent on having health insurance coverage (8–10). Before the ACA, younger, low-income adults with non–dialysis-dependent CKD had more limited options for insurance coverage in the United States, a factor that has been linked to the substantial socioeconomic and racial disparities in pre-emptive wait-listing (9,11). To date, states that expanded Medicaid under the ACA have substantially closed the gap in insurance coverage among low-income adults and minorities, with nearly double the number of newly insured individuals under the ACA coming from states that expanded Medicaid than from nonexpansion states (12.3 million versus 6.9 million, respectively) (12–15). However, little is known as to how Medicaid expansion may have also influenced socioeconomic and racial trends in pre-emptive kidney transplantation wait-listing.
The goal of this study was to determine whether Medicaid expansion under the ACA was associated with differences in the number of individuals who were pre-emptively wait-listed for kidney transplantation with Medicaid coverage. Using national data over a 6-year period, we compared trends in the insurance types used for pre-emptive listing among United States states that did and did not expand Medicaid under the ACA. We also examined whether there was evidence of differences in the association of Medicaid expansion on the insurance types used for pre-emptive listings of racial and ethnic minority transplant candidates compared with listings of white transplant candidates.
Materials and Methods
Study Population
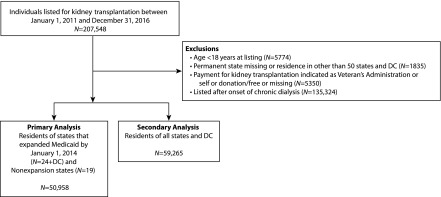
We used the United Network for Organ Sharing’s standard transplant analytic file to identify the study population, which included all adults (≥18 years of age) pre-emptively listed (i.e., listed before dialysis onset) for kidney transplantation in the United States between January 1, 2011 and December 31, 2016. We excluded candidates with missing or non–insurance-based payment for transplantation, residents of United States territories, and those with missing data on their state of residence (see Figure 1, cohort inclusion diagram).
Figure 1.
The cohort included all pre-emptive adult listings for kidney transplantation in the United States between 2011–2016 with non-missing data on state of residence and insurance coverage. DC, District of Columbia.
In our primary analyses, to facilitate comparisons between state groupings over similar pre- and postexposure periods, we compared listings in states that fully implemented Medicaid expansion as of January 1, 2014 (n=24 and the District of Columbia [DC]) to those that did not during the study period (n=19) (16,17), excluding the seven states that implemented Medicaid expansion after January 1, 2014 and before December 31, 2016 (see Supplemental Table 1). In secondary analyses, we compared listings from all states that fully implemented Medicaid expansion during the study period (n=31 states and DC) to the 19 states that did not, on the basis of the date that full expansion was implemented in each state (17). The primary analysis included 50,958 pre-emptive listings, and the secondary analysis included 59,265 pre-emptive listings.
The Drexel University institutional review board approved the study. The clinical and research activities being reported are consistent with the Principles of the Declaration of Istanbul as outlined in the “Declaration of Istanbul on Organ Trafficking and Transplant Tourism.”
Exposure
Our primary exposure was full implementation of Medicaid expansion under the ACA to include low-income adults at or below 138% of the federal poverty level. Before January 1, 2014, some states elected to implement varying levels of Medicaid expansion under the ACA (“early expansion states,” n=5 and DC) (18). However, in contrast to the 2014 expansion, these early expansions were limited to each state’s Federal Medical Assistance Percentage, and varied widely in the eligibility thresholds chosen by states for expanded coverage (18). January 1, 2014 also marked the onset of other ACA policies, including streamlined Medicaid applications and outreach, that greatly affected uptake of the policy (see Supplemental Figure 1, Supplemental Table 2) (19,20). Therefore, we included early expansion states in our primary and secondary analyses, and considered January 1, 2014 as the date of fully implemented Medicaid expansion in these states.
Outcome of Pre-Emptive Medicaid Listing
Our primary outcome was the proportion of pre-emptive listings with Medicaid coverage.
Statistical Analyses
Categoric variables (e.g., sex) were described by their frequencies. Continuous variables (e.g., age) were described by their medians and ranges. Binary variables were compared between groups using chi-squared tests. To compare continuous variables between groups, we used the Wilcoxon rank-sum or Kruskal–Wallis tests, as appropriate.
First, we compared national trends in insurance types used for pre-emptive listings among states that fully implemented Medicaid expansion on January 1, 2014 (n=24 and DC) to those that did not adopt expansion during the study period (n=19) by estimating a race-adjusted multinomial logistic regression model of pre-emptive listing insurance types (Medicaid, private, and Medicare) within each quarter (3-month period [e.g., the first quarter of each year spans January through March]) of our study period. Next, in order to determine the overall associations of Medicaid expansion on Medicaid coverage for pre-emptive listing, we compared the adjusted proportion (i.e., predicted probability) of pre-emptive listings with Medicaid coverage between January 1, 2011 and December 31, 2013 (pre-expansion) to the adjusted proportion of pre-emptive listings with Medicaid coverage between January 1, 2014 and December 31, 2016 (postexpansion) among states that did and did not expand Medicaid by January 1, 2014 using a difference-in-differences approach (21). Finally, to examine whether Medicaid expansion was associated with differences in the proportion of pre-emptive listings with Medicaid coverage by race/ethnicity, we used a triple-difference estimation strategy to consider the interactions of race, Medicaid expansion, and the pre- and post- periods in multivariable multinomial logistic regression models.
In a secondary analysis, we included all states that fully implemented Medicaid expansion under the ACA during our study period (n=31 and DC) to states that did not implement expansion (n=19), and standardized the date of expansion for each state. In race-adjusted multinomial logistic regression models, we compared the adjusted proportion of pre-emptive listings with Medicaid coverage by the number of quarters before and after implementation of Medicaid expansion.
In the Supplemental Appendix, we provide more details on our analysis strategy, as well as additional descriptive analyses and robustness checks. In all analyses, we accounted for potential clustering by transplant center with robust standard errors. All analyses were performed using STATA/MP version 14 for Mac (College Station, TX).
Missing Data
Data were missing for state of residence among <0.04% of the study cohort, and payment information was missing among <0.3% of the cohort. All analyses included only individuals with nonmissing data on race/ethnicity, state of residence, and payment information.
Results
Among 59,265 individuals who were pre-emptively listed during the study period (Figure 1), 55% (n=32,670) were residents of states that fully implemented Medicaid expansion on January 1, 2014 (“expansion states”) and 31% (n=18,288) were residents of nonexpansion states. An additional 8307 (14%) were residents of seven states that adopted Medicaid expansion between January 1, 2014 and the end of the study period (“late-expansion states”) (17).
Table 1 displays characteristics of individuals listed in expansion states versus nonexpansion states in the pre- and postexpansion periods, respectively (n=50,958). Compared with the pre-expansion period, there was a 59% relative increase in pre-emptive Medicaid-covered listings in the postexpansion period among states that expanded Medicaid as of January 1, 2014 (from 1094 to 1737 listings), compared with an 8.8% relative increase among states that did not expand Medicaid (from 330 to 359 listings). Among pre-emptive listings covered by Medicaid (Table 2), the proportions of white listings were similar in the pre- and postexpansion periods in nonexpansion states (from 40% to 40%, P=0.96), and decreased in expansion states (from 36% to 32%, P=0.03). In the postexpansion period, the proportion of pre-emptive Medicaid-covered listings with current employment increased from 16% to 20% in nonexpansion states (P=0.26), and from 22% to 29% in expansion states (P<0.01). The proportion of pre-emptive Medicaid listings that were functionally independent, defined as ≥80% on the Karnofsky Performance Status Scale (22), decreased in nonexpansion states (from 66% to 63%, P=0.28) and increased in expansion states (from 68% to 73%, P=0.02).
Table 1.
Characteristics of pre-emptively listed candidates in nonexpansion and expansion states, pre- and postexpansion
| Characteristic | January 1, 2011–December 31, 2013 | January 1, 2014–December 31, 2016 | ||
|---|---|---|---|---|
| Nonexpansion State (n=19) | Expansion Statea (n=24+DC) | Nonexpansion State (n=19) | Expansion Statea (n=24+DC) | |
| n=8487 | n=15,525 | n=9801 | n=17,145 | |
| Age at listing, yr | 55 (44, 63) | 55 (45, 63) | 54 (44, 63) | 55 (45, 63) |
| Race/ethnicity | ||||
| White | 5429 (64) | 9090 (59) | 6005 (61) | 9697 (57) |
| Black | 1910 (23) | 2551 (16) | 2193 (22) | 2794 (16) |
| Hispanic | 775 (9) | 1998 (13) | 1020 (10) | 2358 (14) |
| Other | 373 (4) | 1886 (12) | 583 (6) | 2296 (13) |
| Male | 4762 (56) | 8964 (58) | 5451 (56) | 9975 (58) |
| BMI kg/m2 | 28.8 (25.1, 32.9) | 28.4 (24.8, 32.5) | 28.7 (25.1, 32.7) | 28.4 (24.7, 32.6) |
| Diabetes status | ||||
| Nondiabetic | 5651 (67) | 10,088 (65) | 6567 (67) | 11,052 (65) |
| Diabetic | 2826 (33) | 5417 (35) | 3229 (33) | 6088 (36) |
| Unknown | 10 (0.1) | 20 (0.1) | 5 (0.1) | 5 (<1) |
| Insurance coverage | ||||
| Medicare | 2463 (29) | 3961 (26) | 2726 (28) | 4415 (26) |
| Medicaid | 330 (4) | 1094 (7) | 359 (4) | 1737 (10) |
| Private | 5694 (67) | 10,470 (67) | 6716 (69) | 10,993 (64) |
| United States citizen | 8319 (98) | 14,785 (95) | 9511 (97) | 16,071 (94) |
| Education level | ||||
| Less than high school | 226 (3) | 635 (4) | 221 (2) | 706 (4) |
| High school graduate | 4971 (59) | 8741 (56) | 5329 (54) | 9456 (55) |
| ≥College graduate | 3020 (36) | 5646 (36) | 3798 (39) | 6664 (39) |
| Missing/unknown | 270 (3) | 503 (3) | 453 (5) | 319 (2) |
| Prior transplant | 1121 (13) | 2056 (13) | 1193 (12) | 2122 (12) |
| Employed | ||||
| No | 3838 (45) | 7387 (48) | 4278 (44) | 7914 (46) |
| Yes | 4435 (52) | 7884 (51) | 5329 (54) | 9061 (53) |
| Unknown | 214 (3) | 254 (2) | 194 (2) | 170 (1) |
| Independent functionb | ||||
| No | 1849 (22) | 2372 (15) | 2120 (22) | 2616 (15) |
| Yes | 6515 (77) | 12,508 (81) | 7428 (76) | 14,200 (83) |
| Missing | 123 (1) | 645 (4) | 253 (3) | 329 (2) |
Values presented as median (interquartile range) and n (%). DC, District of Columbia; BMI, body mass index.
Excludes seven states that implemented Medicaid expansion between January 1, 2014 and December 31, 2016.
Defined as Karnofsky Performance Status Scale ≥80%.
Table 2.
Characteristics of pre-emptively listed candidates with Medicaid coverage in nonexpansion and expansion states, pre- and postexpansion
| Characteristic | January 1, 2011–December 31, 2013 | January 1, 2014–December 31, 2016 | ||
|---|---|---|---|---|
| Nonexpansion State (n=19) | Expansion Statea (n=24+DC) | Nonexpansion State (n=19) | Expansion Statea (n=24+DC) | |
| n=330 | n=1094 | n=359 | n=1737 | |
| Age at listing, yr | 44 (32, 55) | 48 (36, 58) | 45 (35, 54) | 48 (36, 57) |
| Race/ethnicity | ||||
| White | 133 (40) | 388 (36) | 144 (40) | 549 (32) |
| Black | 128 (39) | 282 (26) | 142 (40) | 422 (24) |
| Hispanic | 58 (18) | 289 (26) | 50 (14) | 480 (28) |
| Other | 11 (3) | 135 (12) | 23 (6) | 286 (17) |
| Male | 161 (49) | 540 (49) | 157 (44) | 913 (53) |
| BMI (kg/m2) | 29.0 (24.3, 34.0) | 28.3 (24.4, 32.9) | 28.8 (24.6, 33.2) | 28.4 (24.3, 32.6) |
| Diabetes states | ||||
| Nondiabetic | 224 (70) | 699 (64) | 223 (62) | 1094 (63) |
| Diabetic | 106 (32) | 394 (36) | 136 (38) | 642 (37) |
| Missing | 0 (0.0) | 1 (0.1) | 0 (0.0) | 1 (0.1) |
| United States citizen | 317 (96) | 936 (86) | 339 (94) | 1440 (83) |
| Educational attainment | ||||
| Less than high school | 27 (8) | 150 (14) | 25 (7) | 213 (12) |
| High school graduate | 255 (77) | 732 (67) | 263 (73) | 1208 (70) |
| ≥College graduate | 39 (12) | 154 (14) | 54 (15) | 283 (16) |
| Missing/unknown | 9 (3) | 58 (5) | 17 (5) | 33 (2) |
| Prior organ transplant | 45 (14) | 152 (14) | 42 (12) | 173 (10) |
| Employed | ||||
| No | 256 (78) | 818 (75) | 276 (77) | 1214 (70) |
| Yes | 54 (16) | 237 (22) | 73 (20) | 507 (29) |
| Unknown | 20 (6) | 39 (4) | 10 (3) | 16 (1) |
| Independent functionb | ||||
| No | 99 (30) | 305 (28) | 122 (34) | 426 (25) |
| Yes | 219 (66) | 740 (68) | 226 (63) | 1271 (73) |
| Unknown | 12 (4) | 49 (5) | 11 (3) | 40 (2) |
Values presented as median (interquartile range) and n (%). DC, District of Columbia; BMI, body mass index.
Excludes seven states that implemented Medicaid expansion between January 1, 2014 and December 31, 2016.
Defined as Karnofsky Performance Status Scale ≥80%.
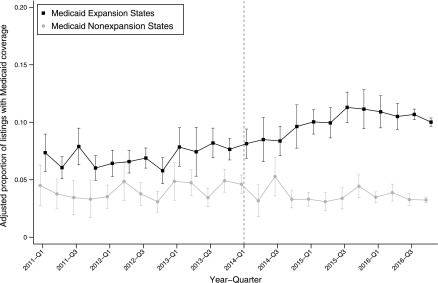
Trends in Pre-Emptive Listings Covered by Medicaid among Medicaid Expansion and Nonexpansion States
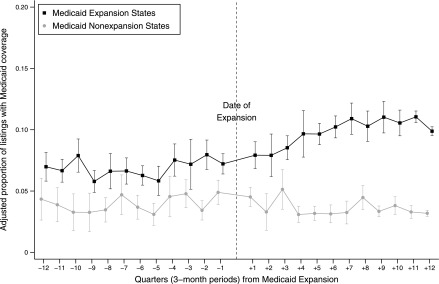
Figure 2 displays trends in the proportions of pre-emptive listings with Medicaid coverage from January 1, 2011 to December 31, 2016 among Medicaid expansion states and nonexpansion states, respectively. From January 1, 2013 to December 31, 2013, there was no statistically significant change in the proportion of pre-emptive listings with Medicaid coverage among expansion state listings (from 7.9% to 7.6%, P=0.95) or nonexpansion state listings (from 4.9% to 4.9%, P=0.80) (difference-in-differences of 0.3%, P=0.78). From January 1, 2014 to December 31, 2014, expansion states had a 1.5 percentage-point increase in the proportion of pre-emptive listings with Medicaid coverage (from 8.1% to 9.6%, P=0.02), compared with nonexpansion states that had a 1.3 percentage-point decrease in the proportion of pre-emptive listings with Medicaid coverage (from 4.6% to 3.3%, P<0.01) (difference-in-differences of 2.8 percentage points, P<0.001). The difference in proportions of pre-emptive listings with Medicaid coverage between expansion and nonexpansion states was sustained throughout the postexpansion study period.
Figure 2.
Medicaid expansion by January 1, 2014 was associated with an increase in pre-emptive listings with Medicaid coverage. This figure displays results from a race-adjusted multinomial logistic regression model for insurance type at listing comparing 19 nonexpansion states to states that expanded Medicaid on January 1, 2014 (n=24+DC). Only Medicaid listings are displayed. The dashed line indicates January 1, 2014. The point estimate for each quarter indicates the adjusted proportion of all pre-emptive listings in that quarter that was Medicaid-covered. Thus, this figure shows changes in the proportion of Medicaid-covered pre-emptive listings over the course of the study period. Black squares represent adjusted proportions of Medicaid-covered pre-emptive listings in Medicaid expansion states, with 95% confidence intervals. Gray circles represent adjusted proportions of Medicaid-covered pre-emptive listings in nonexpansion states, with 95% confidence intervals. Q1, Quarter 1; Q3, Quarter 3.
Association between Medicaid Expansion and Pre-Emptive Listing with Medicaid Coverage in the Pre- and Postexpansion Periods
Table 3 displays results of a race-adjusted multinomial logistic regression difference-in-differences model that compared pre- and postexpansion proportions of pre-emptive listings with Medicaid, Medicare, and private coverage in expansion and nonexpansion states, respectively. From the pre- to postexpansion period, there was no statistically significant difference in the proportion of pre-emptive listings with Medicaid coverage in nonexpansion states (4.0% versus 3.7%, P=0.09), compared with a 3.0 percentage-point increase in pre-emptive listings with Medicaid coverage in expansion states (from 7.0% to 10.0%, P<0.001) (difference-in-differences of 3.3 percentage points, P<0.001).
Table 3.
Results of multivariable multinomial logistic regression difference-in-differences model for pre-emptive listing insurance types
| Insurance Type, State Expansion Status | Adjusteda Probability of Insurance Type for Pre-emptive Listing, % (95% CI) | Proportional Difference, % (95% CI) | ||
|---|---|---|---|---|
| Pre-Expansion Period | Postexpansion Period | Between Periods | In Difference | |
| Medicaid, nonexpansion states | 4.0 (3.5 to 4.5) | 3.7 (3.3 to 4.1) | −0.3 (−0.7 to 0.1) | reference |
| Medicaid, expansion states | 7.0 (6.1 to 8.0) | 10.0 (8.8 to 11.1) | 3.0 (2.4 to 3.4)b | 3.2 (2.7 to 3.8)b |
| Medicare, nonexpansion states | 28.4 (23.3 to 33.6) | 27.4 (24.7 to 30.1) | −1.0 (−3.6% to 1.6%) | reference |
| Medicare, expansion states | 25.7 (21.1 to 30.3) | 26.1 (23.3 to 28.9) | 0.4 (−1.5 to 2.3) | 1.4 (0.04 to 2.8)c |
| Private, nonexpansion states | 67.5 (62.1 to 73.0) | 68.9 (65.8 to 72.0) | 1.3 (−1.1 to 3.9) | reference |
| Private, expansion states | 67.2 (61.8 to 72.7) | 64.0 (60.0 to 67.9) | −3.3 (−4.9 to −1.7)b | −4.7 (−6.1 to −3.1)b |
95% CI, 95% confidence interval.
Adjusted for race, with transplant center cluster-robust standard errors.
P<0.001.
P<0.05.
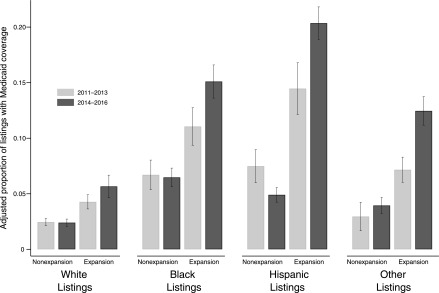
Association between Medicaid Expansion and Pre-Emptive Listing with Medicaid Coverage by Race/Ethnicity
In nonexpansion states, compared with the pre-expansion period, there were no differences in the postexpansion period in the proportion of candidates with Medicaid coverage among white pre-emptive listings (from 2.4% to 2.4%, P=0.80), black pre-emptive listings (from 6.7% to 6.5%, P=0.58), or among pre-emptive listings of other races/ethnicities (from 3.0% to 4.0%, P=0.20). There was a 2.6 percentage-point decrease in the proportion of pre-emptive listings with Medicaid coverage among Hispanic listings in nonexpansion states (from 7.5% to 4.9%, P=0.003). Among expansion states, compared with the pre-expansion period, the proportion of pre-emptive listings with Medicaid coverage increased in the postexpansion period by 1.4 percentage points among white listings (from 4.3% to 5.7%, P<0.001), 4.0 percentage points among black listings (from 11.1% to 15.1%, P<0.001), 5.9 percentage points among Hispanic listings (from 14.5% to 20.4%, P<0.001), and 5.3 percentage points among listings of other races/ethnicities (from 7.2% to 12.5%, P<0.001) (Figure 3) (see Supplemental Figure 3 for within-race comparisons of all insurance types).
Figure 3.
Medicaid expansion was associated with larger percentage-point increases in Medicaid coverage for pre-emptive listing among racial and ethnic minority listings compared to white listings. This figure displays results from a race-adjusted multinomial logistic regression model for insurance type at listing comparing 19 nonexpansion states to states that expanded Medicaid on January 1, 2014 (n=24+DC). The estimates were derived from the triple interaction of race/ethnicity, Medicaid expansion state, and pre- and postexpansion period. Each bar represents the adjusted proportion, with 95% confidence intervals, of Medicaid-covered listings within each listed race/ethnicity group in expansion states and nonexpansion states, respectively. Light gray bars represent the adjusted pre-expansion proportions, and dark gray bars represent postexpansion adjusted proportions.
Secondary Trends Analysis Including All States that Implemented Medicaid Expansion
Figure 4 displays race-adjusted trends in Medicaid coverage for pre-emptive listings by the number of quarters (3-month periods) before and after implementation of Medicaid expansion, comparing all states that expanded Medicaid during the study period (n=31+DC) (17), to 19 states that did not expand Medicaid (total sample n=59,265, see Supplemental Table 2 for descriptive comparisons). From the first quarter after Medicaid expansion to the fourth quarter, states that expanded Medicaid had a 2.1 percentage-point increase in the proportion of pre-emptive listings with Medicaid coverage (from 7.6% to 9.7% P=0.003), compared with a 1.7 percentage-point decrease in the proportion of pre-emptive listings with Medicaid coverage among states that did not expand Medicaid (from 4.7% to 3.0%, P<0.001) (difference-in-differences of 3.8 percentage points, P<0.001).
Figure 4.
Including all states that expanded Medicaid by their dates of expansion, Medicaid expansion was associated with an increase in pre-emptive listings with Medicaid coverage. This figure displays results from a race-adjusted multinomial logistic regression model for insurance type at listing comparing 19 nonexpansion states to 31 expansion and late-expansion states and the District of Columbia. To account for different calendar dates of Medicaid expansion, results are presented as the number of quarters before and after a standardized Medicaid expansion date, where the date of Medicaid expansion adoption is set to equal zero. The point estimate for each quarter indicates the adjusted proportion of all pre-emptive listings in that quarter that was Medicaid-covered. The dashed line indicates the calendar date of Medicaid expansion. Black squares represent proportions of Medicaid-covered pre-emptive listings in Medicaid expansion states, with 95% confidence intervals. Gray circles represent proportions of Medicaid-covered pre-emptive listings in nonexpansion states, with 95% confidence intervals.
Results of Sensitivity Analysis
Similar trends in pre-emptive Medicaid-covered listings were observed in analyses that excluded early expansion states (Supplemental Figure 5) (18). Results were also robust in other sensitivity analyses, including models comparing only early expansion states (n=5 and DC) and late expansion states (n=7), respectively, to nonexpansion states (see Supplemental Material).
Discussion
This nationally representative study found that full implementation of Medicaid expansion under the ACA was associated with an increase in the proportion of pre-emptive listings for kidney transplantation with Medicaid coverage. Further, expansion was associated with larger proportional increases in Medicaid coverage among racial and ethnic minority listings compared with white listings.
Lack of insurance is a known barrier to CKD awareness, predialysis nephrology care, and access to the kidney transplant waiting list (9,10,23–25). Recent changes to the national deceased donor kidney allocation system have increased rates of transplantation for individuals who are wait-listed after long dialysis durations (26). However, pre-emptive wait-listing for waiting time accrual remains an effective and recommended strategy to minimize pretransplant dialysis exposure in the new system (27–29). Our study suggests that states that expanded access to public insurance provided more low-income patients with CKD with the resources required for pre-emptive wait-listing. In states that did not expand Medicaid, millions of individuals with incomes too high to qualify for Medicaid and too low to receive subsidized private insurance remain uninsured (30,31). Given this coverage gap, it is uncertain if low-income individuals with CKD in nonexpansion states have had equivalent opportunities to accrue pre-emptive waiting time for kidney transplantation. Prior studies have shown that states with expanded access to public insurance demonstrate higher utilization of health services, including CKD care, among low-income individuals and minorities (32–35). With respect to cost, policies that promote shorter periods of dialysis exposure among individuals who rely on public insurance may have positive implications for United States spending for chronic dialysis (36,37), which currently exceeds 30 billion dollars yearly (38).
Medicaid expansion has accounted for approximately 60% of the gains in insurance coverage under the ACA (39), and both previously Medicaid-eligible and newly eligible individuals have gained insurance under Medicaid expansion (18,39). Before expansion, access to Medicaid for younger low-income adults was generally restricted to pregnant women, those with disabilities, and some parents (40). These restrictions may explain why traditional Medicaid beneficiaries have historically comprised a minority of pre-emptively listed kidney transplant candidates (7,9,41). In contrast, Medicaid expansion beneficiaries may represent a distinct, healthier population of potentially eligible kidney transplant candidates (30,42). For example, we found that Medicaid-covered listings in expansion states were more likely to be employed and functionally independent than those in nonexpansion states. However, despite expanded access to public insurance coverage, low-income individuals may continue to experience suboptimal access to care and quality of care compared with those with other coverage options (43–45). Therefore, it is likely that additional efforts will be needed on the part of nephrologists and transplant providers to ensure that pre-emptive waiting time accrual among Medicaid expansion beneficiaries also translates to optimal transplant outcomes in this vulnerable population.
Our study found that Medicaid expansion was associated with a larger increase in Medicaid coverage among minority pre-emptive listings than among white pre-emptive listings. Before the ACA, the known racial disparities in predialysis nephrology care and access to kidney transplantation in the United States were strongly linked to income inequalities and unequal access to insurance coverage options (9,46). Numerous non-Medicaid ACA provisions, such as federal subsidies for private insurance and health insurance exchanges, have increased private insurance coverage nationwide (39). However, racial and ethnic minorities have benefited disproportionately from Medicaid expansion (30,42), and states that have adopted Medicaid expansion have narrowed racial disparities in health services utilization to a greater extent than nonexpansion states (15,47). Further, racial minorities comprise more than half of the 2.3 million individuals who remain uninsured as a result of the Medicaid nonexpansion coverage gap for low-income adults (31). Given substantially higher incidence rates of ESKD among minorities compared with whites (38,48), this coverage gap may represent a persistent driver of racial disparities in predialysis CKD care in the United States (4).
Our study has several strengths, including the ability to analyze nationally representative data over a 6-year time period to assess trends in pre-emptive kidney transplant wait-listing. However, our study must be considered with respect to its limitations. First, our retrospective study design may be vulnerable to selection bias if the overall source population of potentially eligible kidney transplant candidates significantly changed in expansion or nonexpansion states during the study period. Second, our study lacks individual-level data on income level, changes in access to insurance, and patterns of health care utilization. Third, it is likely that states that partially expanded Medicaid earlier than 2014 differed in important, unmeasured ways from states that expanded Medicaid on and after January 1, 2014, and their inclusion may impart a conservative bias on our difference-in-differences estimates (18). However, our findings were robust to sensitivity analyses that excluded these early expansion states. Another limitation of our study is that it cannot disentangle Medicaid expansion from the effects of other ACA provisions and national initiatives, such as the new kidney allocation system, that may have also exerted influences on United States wait-listing practices. Finally, because our results represent early trends in listing patterns after Medicaid expansion, studies are needed to observe whether these patterns persist in the changing political landscape (40,49), and whether they affect kidney transplant outcomes.
In summary, this study found evidence that implementation of Medicaid expansion was associated with an increase in the proportion of pre-emptive listings for kidney transplantation with Medicaid coverage, with larger increases in Medicaid coverage among minority listings than white listings. Future studies are needed to determine whether long-term transplant outcomes differ among candidates who were listed with expanded Medicaid coverage compared with those with other coverage options.
Disclosures
None.
Supplementary Material
Acknowledgments
M.N.H. is supported by a grant (K23DK105207) from the National Institutes of Health/National Institutes of Diabetes and Digestive and Kidney Diseases. This study used data from the Organ Procurement and Transplantation Network (OPTN). The OPTN data system includes data on all donors, wait-listed candidates, and transplant recipients in the United States, submitted by the members of the OPTN, and has been described elsewhere. The Health Resources and Services Administration, US Department of Health and Human Services provides oversight to the activities of the OPTN contractor. This work was supported in part by Health Resources and Services Administration contract 234-2005-37011C.
The content is the responsibility of the authors alone and does not necessarily reflect the views or policies of the Department of Health and Human Services or the Department of Veterans Affairs, nor does mention of trade names, commercial products, or organizations imply endorsement by the US Government.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
See related editorial, “The Affordable Care Act, Kidney Transplant Access, and Kidney Disease Care in the United States,” on pages 982–983.
This article contains supplemental material online at http://cjasn.asnjournals.org/lookup/suppl/doi:10.2215/CJN.00100118/-/DCSupplemental.
References
- 1.Sommers BD, Maylone B, Blendon RJ, Orav EJ, Epstein AM: Three-year impacts of the affordable care act: Improved medical care And health among low-income adults. Health Aff (Millwood) 36: 1119–1128, 2017 [DOI] [PubMed] [Google Scholar]
- 2.Heberlein M, Brooks T, Artiga S, Stephens J: Getting into gear for 2014: Shifting new medicaid eligibility and enrollment policies into drive, Washington, DC, The Kaiser Commission on Medicaid and the Uninsured, 2013. Available at: https://www.kff.org/medicaid/report/getting-into-gear-for-2014-shifting-new-medicaid-eligibility-and-enrollment-policies-into-drive/. Accessed March 9, 2018
- 3.Obamacare enrollment numbers, 2017. Available at: https://obamacarefacts.com/sign-ups/obamacare-enrollment-numbers/. Accessed January 1, 2018
- 4.Trivedi AN, Sommers BD: The affordable care act, medicaid expansion, and disparities in kidney disease. Clin J Am Soc Nephrol 13: 480–482, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Israni AK, Salkowski N, Gustafson S, Snyder JJ, Friedewald JJ, Formica RN, Wang X, Shteyn E, Cherikh W, Stewart D, Samana CJ, Chung A, Hart A, Kasiske BL: New national allocation policy for deceased donor kidneys in the United States and possible effect on patient outcomes. J Am Soc Nephrol 25: 1842–1848, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schold JD, Sehgal AR, Srinivas TR, Poggio ED, Navaneethan SD, Kaplan B: Marked variation of the association of ESRD duration before and after wait listing on kidney transplant outcomes. Am J Transplant 10: 2008–2016, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kasiske BL, Snyder JJ, Matas AJ, Ellison MD, Gill JS, Kausz AT: Preemptive kidney transplantation: The advantage and the advantaged. J Am Soc Nephrol 13: 1358–1364, 2002 [DOI] [PubMed] [Google Scholar]
- 8.Joshi S, Gaynor JJ, Bayers S, Guerra G, Eldefrawy A, Chediak Z, Companioni L, Sageshima J, Chen L, Kupin W, Roth D, Mattiazzi A, Burke GW 3rd, Ciancio G: Disparities among Blacks, Hispanics, and Whites in time from starting dialysis to kidney transplant waitlisting. Transplantation 95: 309–318, 2013 [DOI] [PubMed] [Google Scholar]
- 9.Keith D, Ashby VB, Port FK, Leichtman AB: Insurance type and minority status associated with large disparities in prelisting dialysis among candidates for kidney transplantation. Clin J Am Soc Nephrol 3: 463–470, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Herring AA, Woolhandler S, Himmelstein DU: Insurance status of U.S. organ donors and transplant recipients: The uninsured give, but rarely receive. Int J Health Serv 38: 641–652, 2008 [DOI] [PubMed] [Google Scholar]
- 11.Tuot DS, Grubbs V: Chronic kidney disease care in the US safety net. Adv Chronic Kidney Dis 22: 66–73, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hayes SL, Riley P, Radley DC, McCarthy D. Reducing racial and ethnic disparities in access to care: Has the affordable care act made a difference? Issue Brief (Commonw Fund) 2017: 1–14, 2017 [PubMed] [Google Scholar]
- 13.Lipton BJ, Decker SL, Sommers BD: The affordable care act appears to have narrowed racial and ethnic disparities in insurance coverage and access to care among young adults [published online ahead of print April 1, 2017]. Med Care Res Rev doi: 10.1177/1077558717706575 [DOI] [PubMed] [Google Scholar]
- 14.Garrett B, Gangopadhyaya A: Who gained health insurance coverage under the ACA, and where do they live? 2016. Available at: https://www.urban.org/sites/default/files/publication/86761/2001041-who-gained-health-insurance-coverage-under-the-aca-and-where-do-they-live.pdf. Accessed March 16, 2018
- 15.Chen J, Vargas-Bustamante A, Mortensen K, Ortega AN: Racial and ethnic disparities in health care access and utilization under the affordable care act. Med Care 54: 140–146, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Oliveira GH, Al-Kindi SG, Simon DI: Implementation of the affordable care act and solid-organ transplantation listings in the United States. JAMA Cardiol 1: 737–738, 2016 [DOI] [PubMed] [Google Scholar]
- 17.Henry J: Kaiser family foundation. Status of state action on the medicaid expansion secision, 2017. Available at: https://www.kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D. Accessed December 31, 2017
- 18.Sommers BD, Arntson E, Kenney GM, Epstein AM: Lessons from early Medicaid expansions under health reform: Interviews with Medicaid officials. Medicare Medicaid Res Rev 3: E1–E19, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McKenna RM: Treatment use, sources of payment, and financial barriers to treatment among individuals with opioid use disorder following the national implementation of the ACA. Drug Alcohol Depend 179: 87–92, 2017 [DOI] [PubMed] [Google Scholar]
- 20.Sommers BD, Gordon S, Somers S, Ingram C, Epstein AM: Medicaid on the eve of expansion: A survey of state Medicaid officials on the Affordable Care Act. Am J Law Med 40: 253–279, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dimick JB, Ryan AM: Methods for evaluating changes in health care policy: The difference-in-differences approach. JAMA 312: 2401–2402, 2014 [DOI] [PubMed] [Google Scholar]
- 22.Karnofsky DA, Burchenal JH: The clinical evaluation of chemotherapeutic agents in cancer. In: Evaluation of Chemotherapeutic Agents, edited by MacLeod CM, New York, Columbia University Press, 1949 [Google Scholar]
- 23.Jurkovitz CT, Li S, Norris KC, Saab G, Bomback AS, Whaley-Connell AT, McCullough PA; KEEP Investigators : Association between lack of health insurance and risk of death and ESRD: Results from the Kidney Early Evaluation Program (KEEP). Am J Kidney Dis 61[Suppl 2]: S24–S32, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Johansen KL, Zhang R, Huang Y, Patzer RE, Kutner NG: Association of race and insurance type with delayed assessment for kidney transplantation among patients initiating dialysis in the United States. Clin J Am Soc Nephrol 7: 1490–1497, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shah A, Fried LF, Chen SC, Qiu Y, Li S, Cavanaugh KL, Norris KC, Whaley-Connell AT, McCullough PA, Mehrotra R; KEEP Investigators : Associations between access to care and awareness of CKD. Am J Kidney Dis 59[Suppl 2]: S16–S23, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Melanson TA, Hockenberry JM, Plantinga L, Basu M, Pastan S, Mohan S, Howard DH, Patzer RE: New kidney allocation system associated with increased rates of transplants among Black and Hispanic patients. Health Aff (Millwood) 36: 1078–1085, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Organ Procurement and Transplantation Network Minority Affairs Committee: Educational guidance on patient referral to kidney transplantation, 2015. Available at: https://optn.transplant.hrsa.gov/resources/guidance/educational-guidance-on-patient-referral-to-kidney-transplantation/. Accessed January 21, 2018
- 28.Goldfarb-Rumyantzev A, Hurdle JF, Scandling J, Wang Z, Baird B, Barenbaum L, Cheung AK: Duration of end-stage renal disease and kidney transplant outcome. Nephrol Dial Transplant 20: 167–175, 2005 [DOI] [PubMed] [Google Scholar]
- 29.Haller MC, Kainz A, Baer H, Oberbauer R: Dialysis vintage and outcomes after kidney transplantation: A retrospective cohort study. Clin J Am Soc Nephrol 12: 122–130, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McMorrow S, Long SK, Kenney GM, Anderson N: Uninsurance disparities have narrowed for Black and Hispanic adults under the affordable care act. Health Aff (Millwood) 34: 1774–1778, 2015 [DOI] [PubMed] [Google Scholar]
- 31.Garfield R, Damico A: The coverage gap: Uninsured poor adults in states that do not expand medicaid, 2017. Available at: https://www.kff.org/uninsured/issue-brief/the-coverage-gap-uninsured-poor-adults-in-states-that-do-not-expand-medicaid/. Accessed March 15, 2018
- 32.Sommers BD, Blendon RJ, Orav EJ, Epstein AM: Changes in utilization and health among low-income adults after medicaid expansion or expanded private insurance. JAMA Intern Med 176: 1501–1509, 2016 [DOI] [PubMed] [Google Scholar]
- 33.Wherry LR, Miller S: Early coverage, access, utilization, and health effects associated with the affordable care act medicaid expansions: A quasi-experimental Study. Ann Intern Med 164: 795–803, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yan G, Cheung AK, Greene T, Yu AJ, Oliver MN, Yu W, Ma JZ, Norris KC: Interstate variation in receipt of nephrologist care in US patients approaching ESRD: Race, age, and state characteristics. Clin J Am Soc Nephrol 10: 1979–1988, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kurella-Tamura M, Goldstein BA, Hall YN, Mitani AA, Winkelmayer WC: State medicaid coverage, ESRD incidence, and access to care. J Am Soc Nephrol 25: 1321–1329, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Held PJ, McCormick F, Ojo A, Roberts JP: A cost-benefit analysis of government compensation of kidney donors. Am J Transplant 16: 877–885, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gill JS, Tonelli M: Penny wise, pound foolish? Coverage limits on immunosuppression after kidney transplantation. N Engl J Med 366: 586–589, 2012 [DOI] [PubMed] [Google Scholar]
- 38.Saran R, Robinson B, Abbott KC, Agodoa LY, Albertus P, Ayanian J, Balkrishnan R, Bragg-Gresham J, Cao J, Chen JL, Cope E, Dharmarajan S, Dietrich X, Eckard A, Eggers PW, Gaber C, Gillen D, Gipson D, Gu H, Hailpern SM, Hall YN, Han Y, He K, Hebert H, Helmuth M, Herman W, Heung M, Hutton D, Jacobsen SJ, Ji N, Jin Y, Kalantar-Zadeh K, Kapke A, Katz R, Kovesdy CP, Kurtz V, Lavalee D, Li Y, Lu Y, McCullough K, Molnar MZ, Montez-Rath M, Morgenstern H, Mu Q, Mukhopadhyay P, Nallamothu B, Nguyen DV, Norris KC, O'Hare AM, Obi Y, Pearson J, Pisoni R, Plattner B, Port FK, Potukuchi P, Rao P, Ratkowiak K, Ravel V, Ray D, Rhee CM, Schaubel DE, Selewski DT, Shaw S, Shi J, Shieu M, Sim JJ, Song P, Soohoo M, Steffick D, Streja E, Tamura MK, Tentori F, Tilea A, Tong L, Turf M, Wang D, Wang M, Woodside K, Wyncott A, Xin X, Zang W, Zepel L, Zhang S, Zho H, Hirth RA, Shahinian V. US renal data system 2016 annual data report: Epidemiology of kidney disease in the United States. Am J Kidney Dis. 69[3 Suppl 1]: A7–A8, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Frean M, Gruber J, Sommers BD: Premium subsidies, the mandate, and medicaid expansion: Coverage effects of the affordable care act. J Health Econ 53: 72–86, 2017 [DOI] [PubMed] [Google Scholar]
- 40.Sommers BD, Grabowski DC: What is medicaid? More than meets the eye. JAMA 318: 695–696, 2017 [DOI] [PubMed] [Google Scholar]
- 41.Kasiske BL, London W, Ellison MD: Race and socioeconomic factors influencing early placement on the kidney transplant waiting list. J Am Soc Nephrol 9: 2142–2147, 1998 [DOI] [PubMed] [Google Scholar]
- 42.McMorrow S, Kenney GM, Long SK, Anderson N: Uninsurance among young adults continues to decline, particularly in Medicaid expansion states. Health Aff (Millwood) 34: 616–620, 2015 [DOI] [PubMed] [Google Scholar]
- 43.Alcalá HE, Roby DH, Grande DT, McKenna RM, Ortega AN: Insurance type and access to health care providers and appointments under the affordable care act. Med Care 56: 186–192, 2018 [DOI] [PubMed] [Google Scholar]
- 44.McMorrow S, Long SK, Fogel A: Primary care providers ordered fewer preventive services for women with medicaid than for women with private coverage. Health Aff (Millwood) 34: 1001–1009, 2015 [DOI] [PubMed] [Google Scholar]
- 45.Evans RW, Applegate WH, Briscoe DM, Cohen DJ, Rorick CC, Murphy BT, et al. : Cost-related immunosuppressive medication nonadherence among kidney transplant recipients. Clin J Am Soc Nephrol 5: 2323–2328, 2010. [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Patzer RE, Amaral S, Wasse H, Volkova N, Kleinbaum D, McClellan WM: Neighborhood poverty and racial disparities in kidney transplant waitlisting. J Am Soc Nephrol 20: 1333–1340, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cole MB, Galárraga O, Wilson IB, Wright B, Trivedi AN: At federally funded health centers, medicaid expansion was associated with improved quality of care. Health Aff (Millwood) 36: 40–48, 2017 [DOI] [PubMed] [Google Scholar]
- 48.Albertus P, Morgenstern H, Robinson B, Saran R: Risk of ESRD in the United States. Am J Kidney Dis 68: 862–872, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sommers BD, Clark KL, Epstein AM: Early changes in health insurance coverage under the Trump administration. N Engl J Med 378: 1061–1063, 2018 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.