Abstract
Background
Parkinson's disease (PD) is a neurodegenerative disorder that affects human voluntary movements. Tremor is one of the most common symptoms of PD and is expressed as involuntary oscillation of the body. Tremors can be analysed in the frequency domain.
Objective
The aim of the current study was to examine selected tremor parameters (frequency, root mean square, and approximated entropy) in order to quantify the characteristics of patients diagnosed with PD, compared to a healthy control group, and to compare the parameters by dividing the subjects according to UPDRS assessment.
Methods
The subjects were divided into two groups: a group of people diagnosed with PD (n = 19) and a control group consisting of healthy volunteers (CO = 12). Each subject performed motor tasks specific to certain tremors: the finger-to-nose test. Each subject performed a motor task three times. A nine degree of freedom (DOF) wireless inertial measurement unit was used for the measurement of upper limb motor tasks. For the quantitative estimation of kinetic and postural tremors, dominant frequency, root means square, and approximation entropy were selected and calculated from the measured angular velocity and linear acceleration signals. A one-way ANOVA with a significance level of α = 0.05 was used to test the null hypothesis that the means of the tremor metrics were the same between the PD and CO groups.
Results
Statistically significant differences between PD patients and control groups were observed in ApEn acceleration signal of kinetic tremor, ApEn angular velocity signal of kinetic tremor, ApEn angular velocity of postural tremor, frequency acceleration signal of postural tremor, and RMS angular speed kinetic tremor.
Conclusion
Application of inertial measurement units for clinical research of patients and PD tremor evaluation allows providing quantitative information for diagnostic purposes, during screening in a clinical setting that differentiates between PD patients and controls.
1. Introduction
Parkinson's disease (PD) is a disorder of certain nerve cells in the part of the brain that produces dopamine. PD usually begins in middle or later life (after age 50) [1]. PD is the second most common neurodegenerative movement disorder [2]. Tremor, in addition to rigidity, bradykinesia, and postural instability, is generally considered to be one of the cardinal features of PD [3].
Tremor is defined as rhythmical and involuntary oscillatory movement of a body part; detection of tremors plays a crucial role in the management and treatment of PD patients. There are three types of PD tremor:
rest tremor, which occurs in a body segment while this body segment is relaxed;
action (kinetic) tremor, which is associated with any voluntary movement;
postural tremor, which occurs when a person maintains a position against gravity, such as holding their arms outstretched.
Postural or action tremors can happen together with rest tremors, but with different frequencies. A rest tremor can occur with a postural tremor, but disappears during an action tremor task [4].
The Unified Parkinson's Disease Rating Scale (UPDRS) allows evaluation of motor and nonmotor symptoms in PD. This scale has standardised movements and tasks; thus, doctors do not need to use any special devices to evaluate specific movements. The severity of the disease is evaluated only according to the competence of the doctor. Each motor task is rated from 0 to 4, where 0 is normal and 4 is severe.
Various motion capture equipment can be used to quantify tremors. An accelerometer is one of the most commonly used sensors for tremor detection [5]. Electromyography (EMG) is also used to detect tremors of the limbs [6], and laser displacement sensors can be used to measure and quantify tremors [7]. There are also systems that allow the registration of tremors and the parameters associated with disease rating scales [8]. Inertial measurement units (IMUs) are increasingly used to detect tremors, as they combine several types of sensors: accelerometers, gyroscopes, and magnetometers. In some studies, angular velocity is used to quantify tremors instead of the acceleration signal [9].
PD can be diagnosed incorrectly and can be confused with other diseases such as essential tremor (ET) [10]. Therefore, studies use data classification techniques to discriminate different diseases. A support vector machine has been used successfully to classify PD and ET tremor characteristics [11]. Classical statistical techniques such as binary logistic linear regression and linear discriminant analysis can also be applied [12]. Researchers often use artificial neural network methods which can automatically detect PD resting tremor using EMG and a recurrent neural network classifier [13].
Tremor signal analysis can be divided into several types: time-domain analysis [14], spectral analysis [15], time-frequency analysis [16], and nonlinear analysis [17].
Amplitude and frequency are the main parameters that describe a tremor [18]. These parameters allow researchers to distinguish between different types of tremors and to assess the severity of the disease. Fast Fourier transformation is used to obtain frequency characteristics. This is a mathematical technique for transforming a signal from the time domain to the frequency domain. Most research analyses only a single limb, usually the one that is most affected, or analyses one segment of the upper limb. Further studies often use a combination of parameters in order to separate PD patients from the control group. In addition, quantification of tremors is often performed using a dominant frequency, which is calculated using the power spectral density function or root mean square (RMS). One of the most commonly used nonlinear analysis parameters is the approximated entropy, which allows estimation of the complexity of the signal.
The aim of the current study was to examine selected parameters (dominant frequency (f), root mean square (RMS), and approximated entropy (ApEn)) in order to quantify the characteristics of patients with PD, compared to a control group, and to compare the parameters by dividing the subjects according to UPDRS assessment (kinetic or postural tremor). Finally, this study aimed to compare which side and segment (s) were most affected.
2. Materials and Methods
The data were collected at the Vilnius University Hospital “Santaros Klinikos” Centre of Neurology. Subjects were divided into two groups: a group of subjects diagnosed with PD and healthy subjects. The control subjects did not have any illnesses and injuries that would impair movement or coordination. The inclusion criterions were person older than 18 years of age, able to walk independently without assisting devices, and disease severity, according to the Hoehn and Yahr scale, at 2-3. The exclusion criterions were cardiologic pathologies and other diseases that would impair movement. The experimental protocol was approved by the local ethical committee and all the subjects gave their written informed consent before participating. Subject data are presented in Table 1.
Table 1.
Demographic and clinical characteristic of subjects.
| Group | n | Total UDPRS score (mean ± SD) | UPDRS III score (mean ± SD) | Age (mean ± SD) | Hoehn and Yahr scale score (mean ± SD) |
|---|---|---|---|---|---|
| PD | 19 (M/F: 8/11) | 40.21 ± 15.97 | 28.42 ± 11.21 | 61.53 ± 10.81 | 2.10 ± 0.54 |
| CO | 12 (M/F: 6/6) | — | — | 57.83 ± 7.58 | — |
M, male; F, female.
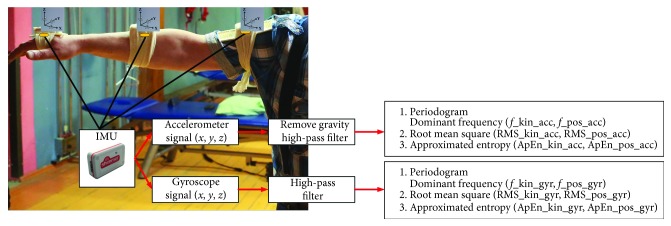
A nine degree of freedom (DOF) wireless inertial measurement unit (Shimmer Research, Dublin, Ireland) was used for the measurement of upper limb motor tasks. Six wireless sensors were attached to the subjects' right and left arm, forearm, and hand (Figure 1).
Figure 1.
Placement of the inertial measurement unit (IMU) sensors on the upper extremity and the calculation algorithm.
Each sensor measured linear acceleration (three-axis acceleration, FreeScale MM7361, and accelerometer limit ± 6 g), angular velocity (three-axis gyroscope, InvenSense 500 MEMs Gyro, angular velocity limit ± 500°/s, and sensibility 2 mV/°), and magnetic heading (three-axis magnetometer, Honeywell HMX5843, and input field boundaries = −0.7–4.5 Ga). The data from the sensors were received via a Bluetooth wireless connection, at a sampling frequency (Fs) of 51.2 Hz, and were stored on a computer.
Each subject performed motor tasks specific to certain tremors: the finger-to-nose test for examining kinetic tremor features and holding an outstretched arm for examination of postural tremor features. Each subject performed a motor task three times.
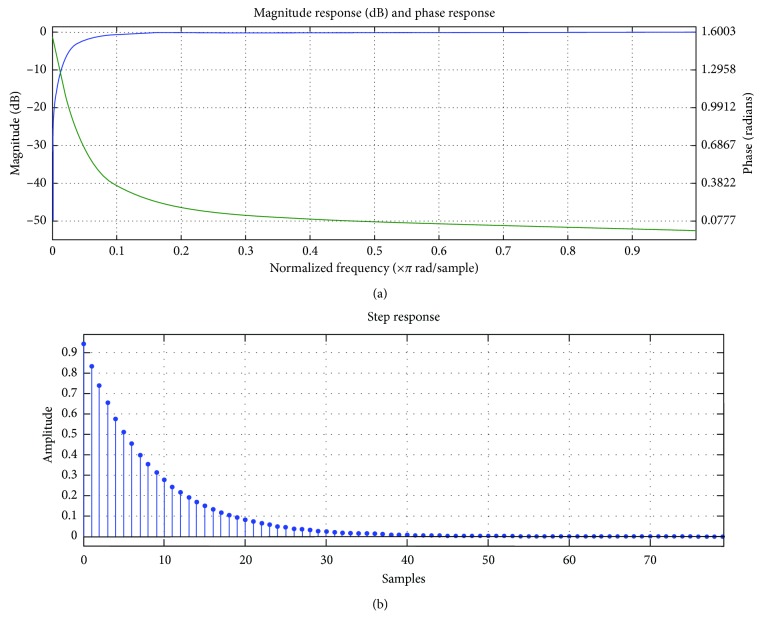
Data processing was performed using Matlab (MathWorks, Inc., 2013). Prior to the analysis, all data recordings were high-pass filtered with a cut-off frequency of 1 Hz (1st order Butterworth filter). The cut-off frequency was chosen considering the digital signal processing to the IMU. Further, the gravitational component was removed from the acceleration signal. Figure 2 shows time and frequency response of a digital filter.
Figure 2.
(a) Frequency-domain digital filter; (b) time-domain digital filter.
For the quantitative estimation of kinetic and postural tremors, several parameters were selected and calculated from the measured angular velocity and linear acceleration signals:
Dominant frequency (frequency kinetic tremor acceleration signal (f_kin_acc), frequency postural tremor acceleration signal (f_pos_acc), frequency kinetic tremor gyroscope signal (f_kin_gyr), and frequency postural tremor gyroscope signal (f_pos_gyr))
Root mean square (RMS kinetic tremor acceleration signal (RMS_kin_acc), RMS postural tremor acceleration signal (RMS_pos_acc), RMS kinetic tremor gyroscope signal (RMS_kin_gyr), and RMS postural tremor gyroscope signal (RMS_pos_gyr))
Approximated entropy (ApEn kinetic tremor acceleration signal (ApEn_kin_acc), ApEn postural tremor acceleration signal (ApEn_pos_acc), ApEn kinetic tremor gyroscope signal (ApEn_kin_gyr), and ApEn postural tremor gyroscope signal (ApEn_pos_gyr)).
Spectral analysis was performed to identify dominant frequencies. The signal strength in a specific frequency spectrum is shown using power spectral density (PSD). The dominant frequency of a tremor is evident as a visible peak in the PSD [19]. A periodogram was used for the evaluation of PSD. A periodogram is a nonparametric estimate of power spectral density, which is based on the Fourier transform of the based estimate of the autocorrelation sequence. A rectangular window is used for calculating the PSD. A periodogram is defined as
| (1) |
where xL(n) is the signal, L is the length, and FS is the sampling frequencies.
If the dominant frequency in different axes is not the same, the valid dominant frequency in the axis with the highest peak power is regarded as the dominant frequency of all axes.
Approximate entropy (ApEn) is a technique that quantifies the degree of irregularity and the unpredictability of fluctuations in time series data [20]. This is a popular tool for analysing the complexity of time series data, especially in clinical research. Low ApEn values indicate predictability and high regularity of time series data, whereas high ApEn values indicate incalculable and random time series data. In this study, we calculated ApEn values for all data sets using m = 2 and r = 0.45 of SD of the individual subjects' time series. This value is recommended [21], and ApEn is defined as
| (2) |
where Sn gives a sequence consisting of N instantaneous measurements, m specifies the pattern length, r defines the criterion of similarity, and Cim(r) is the fraction of patterns of length m that is similar to the pattern of the same length that starts at interval i.
RMS is used to evaluate intensity of tremors. RMS interprets actual vibration levels, while PSD results indicate the dominant frequency that contributes the most to the tremor. Because tremors are based on a dominant frequency, the advantages of PSD compared to a statistical measure (quadratic mean) are that it isolates the tremor signals from noise and other movements, by analysis of the frequency dimension, and it provides a squared value for the signals.
Data from PD patients were divided into groups according to a clinical assessment: Right 0, Right 1, Left 0, and Left 1. Statistical analysis of the metrics was performed using IBM's SPSS v22 software. A one-way ANOVA with a significance level of α = 0.05 was used to test the null hypothesis that the means of the tremor metrics were the same between the PD and CO groups.
3. Results
Significant differences (α < 0.05) between the PD and CO groups are shown in Tables 2–4 (bold values have statistical significance).
Table 2.
Comparison of approximation entropy between PD and CO.
| Segment | Group | ApEn_kin_acc (mean ± SD) | ApEn_pos_acc (mean ± SD) | ApEn_kin_gyr (mean ± SD) | ApEn_pos_gyr (mean ± SD) |
|---|---|---|---|---|---|
| Right upper arm | CO | 0.452 ± 0.139 | 0.967 ± 0.168 | 0.394 ± 0.107 | 0.455 ± 0.188 |
| PD | 0.578 ± 0.208 | 0.947 ± 0.154 | 0.416 ± 0.175 | 0.552 ± 0.135 | |
|
| |||||
| Left upper arm | CO | 0.368 ± 0.195 | 0.991 ± 0.153 | 0.329 ± 0.097 | 0.541 ± 0.223 |
| PD | 0.552 ± 0.198 | 0.860 ± 0.181 | 0.475 ± 0.119 | 0.577 ± 0.168 | |
|
| |||||
| Right forearm | CO | 0.240 ± 0.081 | 0.859 ± 0.201 | 0.383 ± 0.178 | 0.429 ± 0.151 |
| PD | 0.387 ± 0.194 | 0.906 ± 0.217 | 0.375 ± 0.098 | 0.573 ± 0.197 | |
|
| |||||
| Left forearm | CO | 0.297 ± 0.115 | 0.891 ± 0.229 | 0.279 ± 0.069 | 0.516 ± 0.183 |
| PD | 0.491 ± 0.227 | 0.858 ± 0.281 | 0.369 ± 0.104 | 0.579 ± 0.200 | |
|
| |||||
| Right hand | CO | 0.343 ± 0.112 | 0.776 ± 0.156 | 0.283 ± 0.070 | 0.402 ± 0.124 |
| PD | 0.400 ± 0.181 | 0.762 ± 0.210 | 0.311 ± 0.139 | 0.494 ± 0.179 | |
|
| |||||
| Left hand | CO | 0.373 ± 0.111 | 0.804 ± 0.180 | 0.291 ± 0.095 | 0.463 ± 0.180 |
| PD | 0.447 ± 0.155 | 0.754 ± 0.194 | 0.321 ± 0.103 | 0.482 ± 0.169 | |
Table 3.
Comparison of root mean square between PD and CO.
| Segment | Group | RMS_kin_acc (mean ± SD) | RMS_pos_acc (mean ± SD) | RMS_kin_gyr (mean ± SD) | RMS_pos_gyr (mean ± SD) |
|---|---|---|---|---|---|
| Right upper arm | CO | 1.617 ± 0.958 | 0.275 ± 0.095 | 34.078 ± 19.754 | 0.394 ± 0.107 |
| PD | 1.629 ± 1.007 | 0.267 ± 0.159 | 36.018 ± 21.575 | 0.416 ± 0.175 | |
|
| |||||
| Left upper arm | CO | 2.349 ± 1.595 | 0.256 ± 0.130 | 43.031 ± 20.821 | 0.329 ± 0.097 |
| PD | 1.576 ± 1.008 | 0.317 ± 0.289 | 31.536 ± 16.057 | 0.475 ± 0.119 | |
|
| |||||
| Right forearm | CO | 1.909 ± 1.006 | 0.344 ± 0.198 | 45.722 ± 23.602 | 0.383 ± 0.178 |
| PD | 1.772 ± 0.882 | 0.281 ± 0.157 | 42.203 ± 16.655 | 0.375 ± 0.098 | |
|
| |||||
| Left forearm | CO | 1.834 ± 0.831 | 0.271 ± 0.215 | 63.640 ± 25.549 | 0.279 ± 0.069 |
| PD | 1.469 ± 0.794 | 0.239 ± 0.101 | 44.170 ± 16.903 | 0.369 ± 0.104 | |
|
| |||||
| Right hand | CO | 2.429 ± 1.350 | 0.392 ± 0.204 | 70.972 ± 39.044 | 0.283 ± 0.070 |
| PD | 2.703 ± 1.587 | 0.395 ± 0.209 | 86.217 ± 48.488 | 0.310 ± 0.139 | |
|
| |||||
| Left hand | CO | 2.446 ± 1.588 | 0.377 ± 0.283 | 70.419 ± 35.286 | 0.290 ± 0.095 |
| PD | 2.462 ± 1.230 | 0.476 ± 0.406 | 88.970 ± 44.162 | 0.321 ± 0.103 | |
As can be seen, selected parameters (ApEn, dominant frequency, and RMS) allowed us to distinguish between PD and CO groups. Therefore, these parameters allow quantification of tremor characteristics.
Table 4.
Comparison of dominant frequencies between PD and CO.
| Segment | Group | f _kin_acc (mean ± SD) | f _pos_acc (mean ± SD) | f _kin_gyr (mean ± SD) | f _pos_gyr (mean ± SD) |
|---|---|---|---|---|---|
| Right upper arm | CO | 3.278 ± 1.565 | 6.558 ± 3.213 | 2.175 ± 0.752 | 4.164 ± 2.162 |
| PD | 3.516 ± 2.094 | 7.610 ± 2.730 | 2.519 ± 1.075 | 5.715 ± 2.836 | |
|
| |||||
| Left upper arm | CO | 3.101 ± 1.374 | 5.788 ± 2.775 | 2.007 ± 0.866 | 3.195 ± 1.633 |
| PD | 3.925 ± 1.882 | 7.588 ± 3.627 | 2.814 ± 1.377 | 5.421 ± 2.081 | |
|
| |||||
| Right forearm | CO | 1.534 ± 0.396 | 3.196 ± 1.949 | 1.829 ± 0.623 | 2.693 ± 1.662 |
| PD | 1.878 ± 0.890 | 5.234 ± 2.947 | 2.364 ± 1.405 | 4.248 ± 2.654 | |
|
| |||||
| Left forearm | CO | 1.944 ± 0.827 | 3.958 ± 3.373 | 2.079 ± 0.749 | 2.639 ± 1.834 |
| PD | 2.173 ± 1.112 | 6.617 ± 4.504 | 2.722 ± 2.155 | 5.074 ± 2.841 | |
|
| |||||
| Right hand | CO | 1.750 ± 0.415 | 2.287 ± 1.771 | 1.296 ± 0.649 | 2.316 ± 2.062 |
| PD | 1.653 ± 0.488 | 3.857 ± 2.682 | 1.037 ± 0.347 | 3.484 ± 2.400 | |
|
| |||||
| Left hand | CO | 1.939 ± 0.656 | 4.009 ± 3.151 | 1.548 ± 0.723 | 2.396 ± 1.211 |
| PD | 1.882 ± 1.014 | 2.892 ± 1.889 | 1.662 ± 1.726 | 3.333 ± 2.479 | |
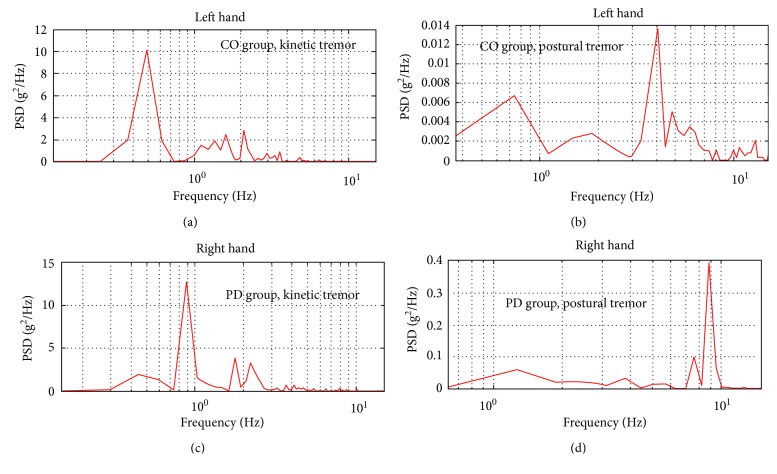
Data from PD patients were further divided into groups according UPDRS clinical assessment (action or postural tremor of hand and UPDRS III motor task 21). This motor task is evaluated in numbers from 0 to 4 (0: no tremor; 4: severe tremor). This motor task is assessed by the right and left side of subjects. This assessment was received from a doctor. Clinical assessment was performed, and the upper limbs from both sides were evaluated; each segment was then scored (upper arm, forearm arm, and hand). Each participant was classified according to the clinical assessment (Right 0 (n = 14), Right 1 (n = 4), Left 0 (n = 14), and Left 1 (n = 4)). The data were grouped as follows: Left 0 versus Left 1 and Right 0 versus Right 1. Figure 3 shows the PSD calculation from the acceleration signal.
Figure 3.
The power spectrum based power spectral density (PSD) plot. (a, b) Postural and kinetic tremor in the CO group; (c, d) kinetic and postural tremor in the PD group.
Statistically significant differences between the PD groups with regard to the UPDRS assessment are shown in Table 5 (bold values have statistical significance).
Table 5.
Tremor parameters between the PD groups with regard to the UPDRS assessment.
| Parameter | Segment | Right 0 (mean ± SD) | Right 1 (mean ± SD) | Segment | Left 0 (mean ± SD) | Left 1 (mean ± SD) |
|---|---|---|---|---|---|---|
| f_kin_gyr | Right upper arm | 2.486 ± 0.891 | 3.077 ± 1.423 | Left upper arm | 2.804 ± 1.303 | 3.335 ± 1.551 |
| Right forearm | 2.082 ± 1.189 | 2.842 ± 1.915 | Left forearm | 2.354 ± 1.388 | 2.756 ± 3.245 | |
| Right hand | 1.063 ± 0.378 | 0.890 ± 0.236 | Left hand | 1.160 ± 0.363 | 1.954 ± 2.140 | |
|
| ||||||
| f_kin_acc | Right upper arm | 3.800 ± 2.234 | 3.177 ± 1.361 | Left upper arm | 3.512 ± 1.514 | 4.146 ± 1.568 |
| Right forearm | 1.940 ± 0.982 | 1.759 ± 0.693 | Left forearm | 2.561 ± 0.914 | 1.232 ± 0.994 | |
| Right hand | 1.709 ± 0.528 | 1.585 ± 0.336 | Left hand | 2.103 ± 1.101 | 1.277 ± 0.198 | |
|
| ||||||
| f_post_gyr | Right upper arm | 5.730 ± 2.901 | 6.835 ± 1.654 | Left upper arm | 5.111 ± 1.802 | 7.224 ± 2.090 |
| Right forearm | 3.861 ± 2.598 | 6.342 ± 1.882 | Left forearm | 5.103 ± 2.724 | 6.101 ± 2.843 | |
| Right hand | 2.927 ± 2.534 | 5.373 ± 0.708 | Left hand | 2.692 ± 2.177 | 5.238 ± 2.99 | |
|
| ||||||
| f_post_acc | Right upper arm | 7.263 ± 3.065 | 8.476 ± 1.338 | Left upper arm | 7.210 ± 3.962 | 9.109 ± 2.638 |
| Right forearm | 4.642 ± 3.149 | 6.960 ± 1.711 | Left forearm | 6.883 ± 5.155 | 5.987 ± 2.281 | |
| Right hand | 2.881 ± 2.2821 | 6.463 ± 1.884 | Left hand | 2.189 ± 1.5860 | 4.716 ± 1.281 | |
|
| ||||||
| RMS_kin_gyr | Right upper arm | 37.44 ± 21.235 | 38.85 ± 22.193 | Left upper arm | 33.69 ± 13.926 | 29.344 ± 22.912 |
| Right forearm | 45.37 ± 16.075 | 38.445 ± 13.822 | Left forearm | 48.706 ± 15.478 | 34.746 ± 15.483 | |
| Right hand | 94.38 ± 50.830 | 75.52 ± 27.201 | Left hand | 102.949 ± 41.806 | 53.629 ± 23.809 | |
|
| ||||||
| RMS_kin_acc | Right upper arm | 1.5377 ± 0.684 | 2.237 ± 1.755 | Left upper arm | 1.741 ± 0.981 | 1.301 ± 1.100 |
| Right forearm | 1.8329 ± 0.628 | 1.912 ± 1.500 | Left forearm | 1.641 ± 0.803 | 1.024 ± 0.677 | |
| Right hand | 2.6642 ± 1.335 | 3.395 ± 2.262 | Left hand | 2.729 ± 1.107 | 2.017 ± 1.382 | |
|
| ||||||
| RMS_post_gyr | Right upper arm | 4.8751 ± 3.650 | 5.218 ± 3.298 | Left upper arm | 3.974 ± 2.542 | 4.452 ± 2.172 |
| Right forearm | 5.1201 ± 3.841 | 5.870 ± 1.942 | Left forearm | 3.983 ± 2.160 | 4.518 ± 1.867 | |
| Right hand | 8.261 ± 7.465 | 6.589 ± 1.707 | Left hand | 8.774 ± 7.580 | 7.808 ± 6.445 | |
|
| ||||||
| RMS_post_acc | Right upper arm | 0.238 ± 0.087 | 0.389 ± 0.303 | Left upper arm | 0.296 ± 0.209 | 0.411 ± 0.546 |
| Right forearm | 0.292 ± 0.178 | 0.259 ± 0.073 | Left forearm | 0.249 ± 0.110 | 0.203 ± 0.078 | |
| Right hand | 0.423 ± 0.212 | 0.351 ± 0.210 | Left hand | 0.504 ± 0.436 | 0.438 ± 0.376 | |
|
| ||||||
| ApEn_kin_gyr | Right upper arm | 0.381 ± 0.134 | 0.514 ± 0.291 | Left upper arm | 0.443 ± 0.108 | 0.585 ± 0.116 |
| Right forearm | 0.364 ± 0.097 | 0.407 ± 0.123 | Left forearm | 0.351 ± 0.114 | 0.434 ± 0.041 | |
| Right hand | 0.307 ± 0.144 | 0.283 ± 0.130 | Left hand | 0.305 ± 0.109 | 0.375 ± 0.087 | |
|
| ||||||
| ApEn_kin_acc | Right upper arm | 0.556 ± 0.196 | 0.561 ± 0.210 | Left upper arm | 0.513 ± 0.167 | 0.600 ± 0.252 |
| Right forearm | 0.333 ± 0.152 | 0.462 ± 0.190 | Left forearm | 0.445 ± 0.183 | 0.593 ± 0.352 | |
| Right hand | 0.389 ± 0.181 | 0.353 ± 0.133 | Left hand | 0.405 ± 0.116 | 0.522 ± 0.207 | |
|
| ||||||
| ApEn_post_gyr | Right upper arm | 0.564 ± 0.152 | 0.542 ± 0.056 | Left upper arm | 0.579 ± 0.187 | 0.579 ± 0.138 |
| Right forearm | 0.570 ± 0.186 | 0.645 ± 0.233 | Left forearm | 0.549 ± 0.201 | 0.678 ± 0.216 | |
| Right hand | 0.476 ± 0.179 | 0.532 ± 0.210 | Left hand | 0.445 ± 0.166 | 0.595 ± 0.162 | |
|
| ||||||
| ApEn_post_acc | Right upper arm | 0.970 ± 0.129 | 0.845 ± 0.227 | Left upper arm | 0.879 ± 0.177 | 0.803 ± 0.232 |
| Right forearm | 0.898 ± 0.201 | 0.698 ± 0.309 | Left forearm | 0.867 ± 0.273 | 0.678 ± 0.386 | |
| Right hand | 0.738 ± 0.199 | 0.792 ± 0.273 | Left hand | 0.750 ± 0.144 | 0.745 ± 0.364 | |
4. Discussion
Application of inertial measurement units for clinical research of patients and PD tremor evaluation allows providing quantitative information for diagnostic purposes, during screening in a clinical setting that differentiates between PD patients and controls. Three basic parameters (frequency, RMS, and approximation entropy) can be used to separate two different groups and for quantitative tremor assessment according to the UPDRS score.
As can be seen from the results obtained (Tables 2–4) to find statistically significant differences between the calculated parameters between PD and CO groups, ApEn is the best way to separate the groups from each other. The result obtained for ApEn values is higher in the PD group, which indicates that the movement is more unpredictable and more incidental. Higher values of ApEn between the subjects and the different sides indicate which side and segment are more severe in the PD group. RMS values show tremor intensity. The result shows that the intensity of the postural tremor is larger on the left side of the angular velocity signal. The dominant frequency is one of the main characteristics for estimating PD tremor, and the obtained result indicates that postural tremor detection is a more appropriate angular velocity signal than the acceleration signal.
Divided PD patients according UDPRS clinical assessment showed a statistically difference. The higher values of the calculated parameter indicate that the values set by the medical doctor correspond to the difference between the calculated values, and their values are higher among the estimates.
Acknowledgments
Special thanks are due to the Clinics of Neurology and Neurosurgery of Vilnius University Hospital Santaros Klinikos medical doctors Rūta Kaladytė–Lokominienė, Dalius Jatužis, and Ramunė Bunevičiūtė.
Data Availability
The data used to support the findings of this study are available from the corresponding author upon request.
Conflicts of Interest
The authors have no conflicts of interest to report.
References
- 1.Rigas G., Tzallas A. T., Tsalikakis D. G., Konitsiotis S., Fotiadis D. I. Real-time quantification of resting tremor in the Parkinson’s disease. Proceedings of the 31st Annual International Conference of the IEEE Engineering in Medicine and Biology Society. IEEE Engineering in Medicine and Biology Society. Annual Conference. 2009;2009:1306–1309. doi: 10.1109/IEMBS.2009.5332580. [DOI] [PubMed] [Google Scholar]
- 2.El-Gohary M., McNames J., Chung K., Aboy M., Salarian A., Horak F. Continuous at-home monitoring of tremor in patients with Parkinson’s disease. Proceedings of Biosignal 2010: Analysis of Biomedical Signals and Images; 2010; pp. 420–424. [Google Scholar]
- 3.Heida T., Wentink E., Marani E. Power spectral density analysis of physiological, rest and action tremor in Parkinson’s disease patients treated with deep brain stimulation. Journal of NeuroEngineering and Rehabilitation. 2013;10(1):p. 70. doi: 10.1186/1743-0003-10-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dai H., Zhang P., Lueth T. C. Quantitative assessment of Parkinsonian tremor based on an inertial measurement unit. Sensors. 2015;15(10):25055–25071. doi: 10.3390/s151025055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ruonala V., Meigal A., Rissanen S. M., Airaksinen O., Kankaanp M., Karjalainen P. A. EMG signal morphology and kinematic parameters in essential tremor and Parkinson’s disease patients. Journal of Electromyography and Kinesiology. 2014;24(2):300–306. doi: 10.1016/j.jelekin.2013.12.007. [DOI] [PubMed] [Google Scholar]
- 6.Grimaldi G., Manto M. Neurological tremor: sensors, signal processing and emerging applications. Sensors. 2010;10(2):1399–1422. doi: 10.3390/s100201399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Duval C. Rest and postural tremors in patients with Parkinson’s disease. Brain Research Bulletin. 2006;70(1):44–48. doi: 10.1016/j.brainresbull.2005.11.010. [DOI] [PubMed] [Google Scholar]
- 8.Mostile G., Giuffrida J. P., Adam O. R., Davidson A., Jankovic J. Correlation between kinesia system assessments and clinical tremor scores in patients with essential tremor. Movement Disorders. 2010;25(12):1938–1943. doi: 10.1002/mds.23201. [DOI] [PubMed] [Google Scholar]
- 9.Thanawattano C., Pongthornseri R., Anan C., Dumnin S., Bhidayasiri R. Temporal fluctuations of tremor signals from inertial sensor: a preliminary study in differentiating Parkinson’s disease from essential tremor. BioMedical Engineering OnLine. 2015;14(1):p. 101. doi: 10.1186/s12938-015-0098-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sternberg E. J., Alcalay R. N., Levy O. A., Louis E. D. Postural and intention tremors: a detailed clinical study of essential tremor vs. Parkinson’s disease. Frontiers in Neurology. 2013;4:1–8. doi: 10.3389/fneur.2013.00051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Surangsrirat D., Thanawattano C., Pongthornseri R., Dumnin S., Anan C., Bhidayasiri R. Support vector machine classification of Parkinson’s disease and essential tremor subjects based on temporal fluctuation. Proceedings of the 38th Annual International Conference of the IEEE Engineering in Medicine and Biology Society. IEEE Engineering in Medicine and Biology Society. Annual Conference. 2016;2016:6389–6392. doi: 10.1109/EMBC.2016.7592190. [DOI] [PubMed] [Google Scholar]
- 12.Ramani R. G., Sivagami G. Parkinson’s Disease classification using data mining algorithms. Int. J. Comput. Appl. 2011;32:17–22. [Google Scholar]
- 13.Arvind R., Karthik B., Sriraam N., Kamala-Kannan J. Automated detection of PD resting tremor using PSD with recurrent neural network classifier. Proceedings of the 2nd International Conference in Advances in Recent Technologies in Communication and Computing (ARTCom) 2010;2010:414–417. [Google Scholar]
- 14.Salarian A., Russmann H., Wider C., Burkhard P. R., Vingerhoets F. J. G., Vingerhoets K. Quantification of tremor and bradykinesia in Parkinson’s disease using a novel ambulatory monitoring system. IEEE Transactions on Biomedical Engineering. 2007;54(2):313–322. doi: 10.1109/tbme.2006.886670. [DOI] [PubMed] [Google Scholar]
- 15.Florian Amtage J. K. Spectral and higher-order spectral analysis of tremor time series. Clinical and Experimental Pharmacology and Physiology. 2014;4 [Google Scholar]
- 16.Surangsrirat D., Intarapanich A., Thanawattano C., Bhidayasiri R., Petchrutchatachart S., Anan C. Tremor assessment using spiral analysis in time-frequency domain. Proceedings of IEEE Southeastcon. 2013;1:1–6. [Google Scholar]
- 17.Gil L. M., Nunes T. P., Faria A. C. D., Melo P. L. Analysis of human tremor in patients with Parkinson disease using entropy measures of signal complexity. Annual International Conference of the IEEE Engineering in Medicine and Biology. 2010;1:2786–2789. doi: 10.1109/IEMBS.2010.5626365. [DOI] [PubMed] [Google Scholar]
- 18.Wilk B. Assessment of a hand tremor based on analysis of the accelerometer signal. Przegląd Elektrotechniczny. 2016;1(11):146–149. doi: 10.15199/48.2016.11.36. [DOI] [Google Scholar]
- 19.Sanchez-Ramos J., Reimer D., Zesiewicz T., Sullivan K., Nausieda P. A. Quantitative analysis of tremors in welders. International Journal of Environmental Research and Public Health. 2011;8(5):1478–1490. doi: 10.3390/ijerph8051478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Abhinaya B., Charanya D. Feature extraction and selection of a combination of entropy features for real-time epilepsy detection. International Journal Of Engineering And Computer Science. 2016;5:16073–16078. [Google Scholar]
- 21.Chon K., Scully C., Lu S. Approximate entropy for all signals. IEEE Engineering in Medicine and Biology Magazine. 2009;28:18–23. doi: 10.1109/MEMB.2009.934629. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used to support the findings of this study are available from the corresponding author upon request.