Abstract
Polypoidal choroidal vasculopathy (PCV) is increasingly recognized as an important cause of exudative maculopathy in Asians as against Wet age-related macular degeneration in Caucasians. A panel of retinal experts methodically evaluated pertinent updated literature on PCV with thorough PubMed/MEDLINE search. Based on this, the panel agreed upon and proposed the current consensus recommendations in the diagnosis (clinical and imaging), management and follow-up schedule of PCV. Diagnosis of PCV should be based on the gold standard indocyanine green angiography which demonstrates early nodular hyperfluorescence signifying the polyp with additional features such as abnormal vascular network (AVN). Optical coherence tomography is an excellent adjuvant for diagnosing PCV, monitoring disease activity, and decision-making regarding the treatment. Current treatment modalities for PCV include photodynamic therapy, anti-vascular endothelial growth factor agents, and thermal laser. Choice of specific treatment modality and prognosis depends on multiple factors such as the location and size of PCV lesion, presence or absence of polyp with residual AVN, amount of submacular hemorrhage, presence or absence of leakage on fundus fluorescein angiography, visual acuity, and so on. Current recommendations would be invaluable for the treating physician in diagnosing PCV and in formulating the best possible individualized treatment strategy for optimal outcomes in PCV management.
Keywords: Abnormal vascular network, indocyanine green angiography, optical coherence tomography, photodynamic therapy, polypoidal choroidal vasculopathy, thermal laser
Polypoidal choroidal vasculopathy (PCV) was first described by Yannuzzi et al. in 1982,[1] as a clinical entity distinctive from neovascular age-related macular degeneration (AMD), consisting of subretinal polypoidal vascular lesions associated with serous and hemorrhagic pigment epithelial detachments (PED). Following this, various reports from other parts of the world were published revealing differences in presentation among different populations and ethnicities.
Initially, PCV was thought to be a rare condition, seen mainly in middle-aged negroid females. However, in the present day, it has been described in all races. PCV is seen more commonly in pigmented races, that is, Asians and African-Americans compared to Caucasians. The prevalence of PCV among patients diagnosed with neovascular AMD is as high as 24.5%[2] to 54.7%[3] in Chinese and Japanese population, respectively, 49% in the Taiwanese[4] and 24.6% in the Korean populations[5] compared to 4% to 9.8% in Caucasians.[6,7,8]
The mean age at presentation noted in various studies ranges between 60 and 72 years, although PCV has been noted from the age of 20 years to 80 years.[9] The age of presentation of PCV is earlier than that for AMD.[10] In a study by Anantharaman et al.,[11] the mean age noted in Indian population was 61.06 years (41–80), which is comparable to the previously published reports.[9] Interestingly, PCV is seen more commonly in males in Asian population, unlike the Caucasians where it is more common in females (75%).[9] PCV is seen bilaterally in 21%–55% Caucasian population, whereas <20% Asians have bilateral disease.[9] The study on Indian population also revealed a male predilection with M:F ratio of 1.4:1 and bilateral involvement in 17.8% patients.[11] Similarly, the locations of polyps also vary among the Asians and Caucasians. The polyps are seen in the macular region in 92% Asians, while there is an even distribution of polyps in the macular and peripapillary location among the Europeans.[9] These variations among different ethnicities could be because of some genetic susceptibility among the pigmented races.
Treatment modalities for PCV include verteporfin photodynamic therapy (PDT), anti-vascular endothelial growth factor (anti-VEGF) therapy, and thermal laser (TL) photocoagulation. Several studies have described variable results with these therapeutic modalities, especially in the long-term. Although international guidelines exist for the management of PCV, they are based on literature present up to March 2012.[12] In addition, over the past 3 years, there has been significant advancement in imaging of PCV, especially on spectral domain optical coherence tomography (SD-OCT). This has notable implications, especially where facilities for performing an indocyanine green angiography (ICGA), considered the gold standard in diagnosing PCV, may be unavailable. To overcome this constraint, a panel of retinal experts met in India on November 7 and 8, 2015 to systematically evaluate pertinent updated literature existing up to November 3, 2015. The purpose was to provide an updated recommendation in the diagnosis (clinical and imaging), management, and follow-up schedule of PCV. Results from the yet to be published PLANET study and recently published EVEREST II study have been incorporated to provide up-to-date management protocol.[13,14] The ultimate objective is to recommend the best possible diagnostic and therapeutic strategies for optimal outcomes in the PCV management.
Methods
We methodically searched PubMed using the following search terminologies: PCV, PCV and clinical features, PCV and classification, PCV and diagnosis or imaging or ICGA or fundus fluorescein angiography (FFA) or OCT, PCV and PDT, PCV and TL, and PCV and bevacizumab or ranibizumab or aflibercept or anti-VEGF. All articles up to November 3, 2015 were manually and meticulously screened by the panel and relevant literature was selected to formulate the guidelines. Review articles and case reports with ≤5 patients were excluded.
Consensus Evidence-Based Guidelines
When to suspect the presence of PCV on clinical evaluation?
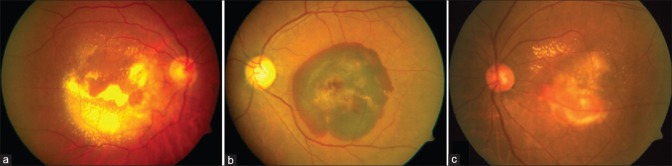
The classical clinical finding of PCV is the presence of reddish-orange subretinal nodules.[15] They can be small, medium, or large in size. The large nodules are easily seen clinically, especially when the overlying retinal pigment epithelium (RPE) is thinned. Apart from polyps, the clinical features more commonly seen include varying degree of serous or serosanguinous PEDs, subretinal hemorrhage, lipid deposition as well as neurosensory retinal detachment in the peripapillary or macular retina[12,16] [Fig. 1].
Figure 1.
Color fundus photograph showing clinical types of polypoidal choroidal vasculopathy: (a) Exudative; (b) Hemorrhagic; (c) Mixed
Clinical classification of polypoidal choroidal vasculopathy
Quiescent: Presence of polyp in the absence of any intraretinal or subretinal fluid or hemorrhage
Active
Exudative: Absence of hemorrhage; presence of exudation in the form of either serous macular detachment/intraretinal fluid/serous PED/lipid exudation
Hemorrhagic: Subretinal or sub-RPE hemorrhage/hemorrhagic PED
Mixed: Presence of features of both exudative and hemorrhagic variety.
The study by Anantharaman et al.[11] reported exudative pattern in 34 out of 47 eyes (72%) and the remaining 13 eyes had a predominantly hemorrhagic pattern. In a study by Kwok et al.,[17] the most common clinical feature noted was subretinal hemorrhage (63.6%) followed by retinal exudation (59.1%) and hemorrhagic PED (59.1%). In another study by Sho et al.,[10] clinical features in 110 eyes of 100 patients were evaluated and serous macular detachment was noted in 52% cases, submacular hemorrhage in 30% cases, and RPE degeneration in 10% cases. Few cases with subretinal fibrovascular proliferations (7%) were also noted. Occasionally, PCV can be located outside the posterior vascular arcades and may cause peripheral exudative hemorrhagic chorioretinopathy.[18] At times, PCV can also present with breakthrough vitreous hemorrhage.
Patients with PCV most commonly present with diminution of vision. Other symptoms include metamorphopsia, floaters, and central scotoma.[17] Typically, a patient who has symptoms for <3 months may have extensive subretinal exudation and hemorrhage but minimal intraretinal cystic changes and a good visual acuity.[9] A significant difference in the visual acuity has been noted between patients with neovascular AMD and PCV, the visual acuity being unexpectedly better in the latter group.[19] The better visual acuity has been speculated to be because of minimal intraretinal changes and the possible extrafoveal location in PCV. However, late presentations may have considerable lipid depositions due to protein leakage from the polypoidal vascular abnormalities.[9] In long-standing cases, there may be signs of subretinal fibrosis, pigment epithelial hyperplasia, or atrophic retinal degeneration.[9]
Recommendation 1
Suspect polypoidal choroidal vasculopathy in the presence of one of the following classical clinical features
Reddish-orange subretinal nodules
Serosanguineous maculopathy
Disproportionate amount of exudation as compared to size of lesion
Hemorrhagic PED/Spontaneous submacular hemorrhage
Nonresponsiveness to anti-VEGF therapy.
Imaging in Polypoidal Choroidal Vasculopathy
Indocyanine green angiography
Is Indocyanine green mandatory for diagnosis of PCV?
PCV, by virtue of primarily being an abnormality of the choroidal circulation, is imaged and characterized better by ICGA than FFA. While the RPE and choroid absorb 59% to 75% of the blue-green light in FFA, only 21% to 38% of the near-infrared light employed in ICGA is absorbed.[20] In addition, ICG being largely protein-bound (98%), tends to remain within the lumen of the fenestrated choroidal vasculature. This permits greater delineation of the choroidal anatomy, unlike fluorescein which extravasates into the interstitium to obfuscate the choroidal details.
Recommendation 2
ICGA is considered to be the current gold standard for detection and evaluation of PCV.
When should we perform ICGA?
While polyps in PCV remain its most recognizable feature, considerable ambiguity in its definition and description exist in literature. They have been variably referred to as “focal vascular dilations,” “polypoidal lesions,” or “polypoidal choroidal vascular dilations.”[1] The EVEREST study used 3 specific criteria to define the polyps of PCV – nodular hyperfluorescence on stereoscopic ICGA (91.8%), hypofluorescent halo around the nodule (68.9%), and pulsation during dynamic ICGA (6.6%).[21] The study also underscored the value of stereo-paired ICGA images as they help highlight the nodularity and depth of the lesion, both vital traits in differentiating polyps of PCV from similar appearing vascular lesions such as seen in retinal macroaneurysms. The EVEREST criteria was tested over a large number (241 eyes) of exudative maculopathy cases, of which 131 were PCV cases and 110 typical Wet AMD cases with fundus camera based ICGA. The single criteria of focal subretinal hyperfluorescence on ICGA for a diagnosis of PCV had a sensitivity of 85.3% and a specificity of 80.9% while applying the EVEREST definition of combining criteria, sensitivity reduced to 78.4% but specificity improved to 87.1% supporting use of the latter in fundus camera-based ICGA. Stereo photographic nodular polyps were the best of the additional criteria.[22]
Recommendation 3
Classic clinical features of PCV described above with or without characteristic notched/peaked PED on OCT is an indication to perform an ICGA.
How to define “Polyp” and “Abnormal Vascular Network” on ICGA? Which phases of ICGA are critical for diagnosing PCV?
Typically, the early phase of the ICG angiogram (First 1 min) reveals a distinct network of vessels within the choroid, called as abnormal vascular network (AVN). Miniscule hyperfluorescent polyps, isolated or in clusters, become visible soon after the PCV network is discernible on the ICG angiogram. These polyps are the angiographic equivalents and correspond to the reddish-orange subretinal nodules seen on the clinical examination. The polyps seem to leak slowly as the surrounding hitherto hypofluorescent area becomes increasingly hyperfluorescent.[1,23,24] Midphase choroidal hyperfluorescence, usually which is multifocal patchy may be seen suggestive of choroidal hyperpermeability [Fig. 2].[23,25]
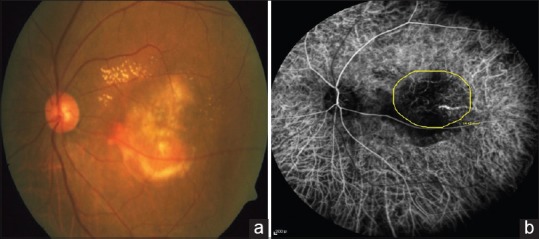
Figure 2.
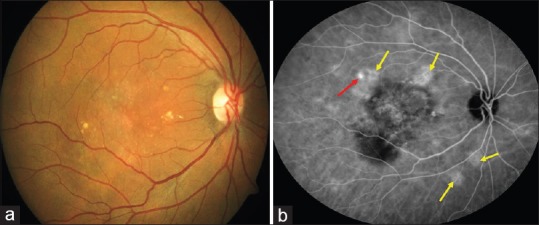
Color fundus photograph (a) of a patient with polypoidal choroidal vasculopathy. Midphase indocyanine green angiography (b) showing the presence of polyp (Red arrow) and multifocal areas of hyperfluorescence (Yellow arrows)
Late-onset focal hyperfluorescence (after 6 min) are more likely to be staining of unhealthy RPE or window defects.[19] Some studies have described late geographic hyperfluorescence (LGH) – defined as a hyperfluorescent lesion with clearly demarcated geographic margin, which become apparent approximately 10 min after the injection of ICG dye with a rosette-pattern and these strongly support the diagnosis of PCV[25] [Fig. 3].
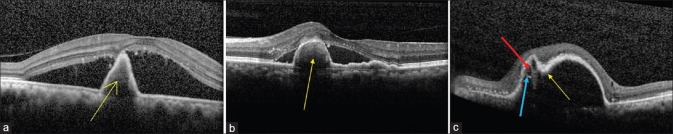
Figure 3.
Spectral domain optical coherence tomography images showing characteristic features of polypoidal choroidal vasculopathy: (a) Sharp-peaked pigment epithelial detachments (Yellow arrow); (b) Thumb-like pigment epithelial detachments, also called thumb-like polyp (thumb-like polyp; Yellow arrow); (c) Notch present at nasal portion of pigment epithelial detachments (Notched PED; Yellow arrow), along with hyporeflective lumen (Red arrow) surrounded by hyperreflective ring (Blue arrow) attached to undersurface of retinal pigment epithelium
When polypoidal lesions are not found due to blockage by hemorrhage or insufficient image quality, these cases may be termed as “PCV suspects” or “suspected of PCV.”[26]
Recommendation 4
Importance of phases of indocyanine green angiography
First 1 min: Recognition of AVN, especially feeder vessel in branch vascular network (BVN) which appears very early (Within first 30 s). Dynamic ICGA should be performed as far as possible within the 1st minute to identify pulsatile polyps in addition to defining the extent of AVN.
Characterization of Abnormal Vascular Network:
Interconnecting channels (IC): AVN appearing within 1 min of dye injection in the absence of feeder vessel [Fig. 4]
BVN: AVN appearing within 1 min of dye injection in the presence of feeder vessel [Fig. 5].
Figure 4.
Color fundus photograph (a) of a patient with serosanguinous polypoidal choroidal vasculopathy. Early phase indocyanine green angiography (b) showing the presence of abnormal vascular network (Yellow circle) in the absence of feeder vessel suggestive of interconnecting channels
Figure 5.
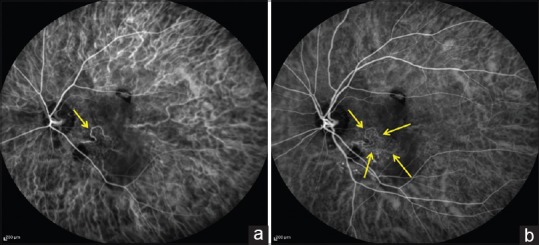
Early-phase indocyanine green angiography showing the presence of a feeder vessel (Yellow arrow in a) with filling of the entire abnormal vascular network (Yellow arrows in b) suggestive of branch vascular network
First 6 min: Characterization of polyp: Early nodular hyperfluorescence arising from choroidal circulation noted within the first 6 min of dye injection.[23,27]
They may be either solitary or arranged in strings or clusters.
Additional ICGA features include:
Hypofluorescent halo around the hyperfluorescent nodule
Abnormal vascular channels terminating in the polyps
Pulsatile filling of polyps (Video ICGA).
Indocyanine green angiography-based classification of polypoidal choroidal vasculopathy based on location
Based on ICGA, PCV is classified in following subtypes with relation to the location of polyp/AVN [Fig. 6].
Figure 6.
Indocyanine green angiography images showing various topographic locations of polyps (Yellow arrow): (a) Subfoveal; (b) Juxtafoveal; (c) Extrafoveal; (d) Peripapillary; (e) Peripheral
-
Macular
- Subfoveal: Below the fovea
- Juxtafoveal: Located within 1–199 μ from center of fovea
- Extrafoveal: Location 200 μ or more from center of fovea
Peripapillary: Located with one disc diameter from the margins of the disc
Peripheral: Located outside the arcade
Following 10 min: “LGH” can be appreciated well [Fig. 7].
Figure 7.
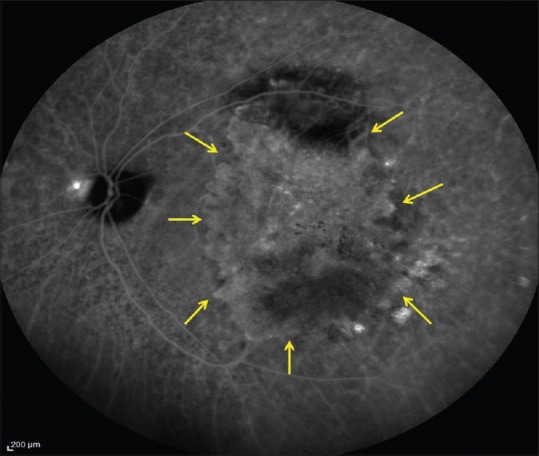
Indocyanine green angiography image showing the presence of hyperfluorescent lesion with clearly demarcated geographic margin (Yellow arrows) suggestive of late geographic hyperfluorescence
Recommendation 5
Based on ICGA, the location of polyp and AVN should be clearly defined which will help in selecting the best treatment strategy.
How to decide on extent of the lesion on ICGA?
The spot size for PDT was originally determined by the greatest linear diameter of the lesion based on fluorescein angiography. Recently, clinicians have used the greatest linear diameter measured by ICGA and obtained good results.[28,29,30] In the EVEREST study,[21,27] the drawing tools in the Heidelberg Eye Explorer software were used to obtain the PCV lesion area. A best-fit circle can be plotted around each polyp. The area of each polyp may be calculated using the diameter of each circle. The freehand drawing tool of the software can be used to outline the total lesion, encompassing the polyps and the abnormal vascular channels and the automation provides the net area. An outline encompassing all polyps identified and the area of the abnormal vascular channels (recognized using dynamic ICGA) may be charted, and the provided automation computes the total area. A best-fit circle around the total lesion area is next drawn using the circle drawing tool, and the diameter of this is taken as the greatest linear dimension[21] [Fig. 8]. An alteration in the lesion size was recognized when there was a size change of >10% at the corresponding area on each angiogram on successive visits.[31] The maximal lesion size is best estimated in the early-phase ICGA in the majority (about 90%) of cases.
Figure 8.

Indocyanine green angiography showing the presence of multiple polyps with network of vessels in the foveal region. Yellow circle represents the total area (Polyp + abnormal vascular network) of polypoidal choroidal vasculopathy to be treated
Recommendation 6:
The total lesion area of PCV is the total area including all polyps and AVN on ICGA.
Fluorescein angiography
Is Fundus Fluorescein Angiography necessary in PCV?
In a study by Gomi et al., aimed at investigating the comparative value of fluorescein angiography, confocal scanning laser ophthalmoscopy (CSLO)-based ICGA, and fundus camera-based ICG in diagnosing PCV, the authors assessed 37 eyes, in which all the angiographies were performed on the same day.[31] The lesion sizes on FFA using confocal SLO and the fundus camera were consistent in all eyes. When a PED was present at the margin of the lesion, FFA shows a larger lesion size than on ICGA. This was because the PED is hyperfluorescent on FFA and hypofluorescent on ICGA and on the angiogram all hyperfluorescent areas were included. Hence, FFA may prove to be useful in cases with several or large PEDs at the edge of the lesion. Even in patients who did not have PEDs at the edges, in about 90% of them, FFA showed the largest lesion size. The maximal lesion size of PCV is best made out by a combination of CSLO-ICGA in the early phase coupled with FFA.
Tan et al.[32] performed ICGA + digital fluorescein angiography (DFA) on 107 patients with PCV and followed these patients over 5 years. They categorized their patients into: Type A (Polyp + IC), Type B (Polyp + BVN without leakage on DFA), and Type C (Polyp + BVN with leakage on DFA). They found the best visual prognosis in Type A followed by Type B and worst with Type C. Hence, performing a combination of ICGA and DFA at baseline may help us to prognosticate the visual outcomes in PCV. Whereas, ICGA delineates the extent of lesion FFA is necessary to identify leakage from BVN, which is a sign of activity.
Indocyanine green + fundus fluorescein angiography-based classification of polypoidal choroidal vasculopathy based on prognosis
Polyp + IC
Polyp + BVN without leakage on FFA
Polyp + BVN with leakage on FFA.
Recommendation 7
FFA should be performed in all patient of PCV at the initial examination to identify the presence or absence of leakage from the AVN which plays a role in prognosticating the disease outcome.
Optical coherence tomography
What are the characteristic features of PCV on OCT?
OCT shows certain distinctive features which aids the clinician to suspect the presence of PCV. It may especially be useful at centers where ICGA is unavailable. Although not diagnostic in isolation, it is a useful adjuvant to ICGA. It is an indispensable tool for monitoring disease activity and response to therapy by recognition features such as subretinal and/or intraretinal fluid.
Recommendation 8
Based on OCT,[33,34,35] PCV can be suspected if there is the presence of any one of the following features [Fig. 3]:
Thumb-like polyp (TLP)/Sharp-peaked PED: Denotes polyp
Tomographic notch in PED: Signifies the polypoidal lesion at margin of PED
Hyporeflective lumen surrounded by hyperreflective ring attached to undersurface of RPE
Double-layer sign (DLS): Presence of two hyperreflective lines on SD-OCT representing shallow irregular RPE elevation and Bruch's membrane, signifying AVN [Fig. 9].
Figure 9.
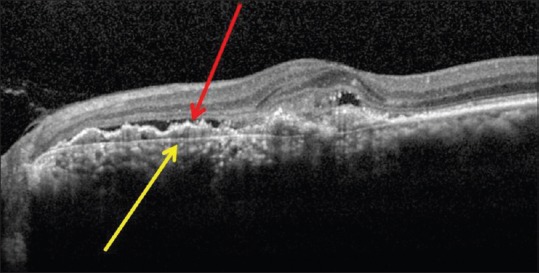
Spectral domain optical coherence tomography showing the presence of double-layer sign, represented by two hyperreflective lines, inner signifying shallow retinal pigment epithelium elevation (Red arrow), and outer signifying Bruch's membrane (Yellow arrow) indicative of abnormal vascular network
The presence of normal/increased choroidal thickness (pachychoroid) on enhanced-depth imaging OCT (EDI-OCT) provides supportive evidence of PCV and can be used to differentiate it from AMD, in which the choroid is usually thin.[36,37]
Is it possible to differentiate between PCV and Wet AMD on basis of OCT?
Liu et al.[35] compared the use of SD-OCT to distinguish between PCV and AMD in 188 eyes, based on the presence of two of the following three features: PED, DLS, and TLP. They found a sensitivity of 89.4% and specificity of 85.3% in detecting PCV. Similarly, another study by De Salvo et al.[34] using SD-OCT to differentiate between PCV and occult CNVM showed a sensitivity of 94.6%, specificity of 92.9%, positive predictive value of 97.2%, and negative predictive value of 86.7% to identify PCV. However, in this study, the diagnostic criteria on SD-OCT used were (Any 3 out of 4): Sharp PED peak, notched PED, multiple PEDs, and hyporeflective lumen within hyperreflectivity lesion adherent to RPE.
Recommendation 9
By identifying classical features of PCV on OCT such as tall-peaked PED, notched PED, DLS, and TLP, it may be possible to suspect PCV and differentiate it from Wet AMD to a large extent. Nonetheless, ICGA remains the gold standard in diagnosing PCV and should be performed if available.
Treatment
How to decide whether to treat/observe PCV? If treatment is essential, how do we decide on the area of treatment?
The treatment of PCV is primarily based on its location, and whether it is active or inactive. The entire PCV lesion including the polyp and AVN should be treated.[21,27,31]
How do we define disease activity?
Recommendation 10
PCV can be considered active[12] in the presence of any one of the following features:
Intraretinal/subretinal fluid
Sub-RPE/subretinal hemorrhage
Vision loss ≥5 ETDRS letters
Leakage on FFA can be considered as a corroborative feature in defining the disease activity
When to treat PCV?
The panel recommended that inactive PCV could be safely observed and monitored. In situations when the PCV is active but asymptomatic, such as in cases of peripapillary or peripheral PCV, whether to initiate therapy or consider close monitoring is based on discretion of the treating physician. This approach is advocated based on collective evidence in literature and on consensus of the panel.[16,38,39] In addition, if there are multiple polyps present on ICGA scattered throughout the posterior pole, but the evidence of activity is limited to only one particular polyp, the panel recommends only the active polyps be treated based on its location. The inactive polyps need close follow-up.
Recommendation 11
Active symptomatic PCV: Treat
Active asymptomatic PCV: Can consider treatment based on discretion
Inactive PCV: Observe.
Treatment of subfoveal and juxtafoveal polypoidal choroidal vasculopathy
When is PDT indicated in PCV? Is a combination therapy with anti-VEGF agent essential?
PDT is indicated in cases where there is subfoveal or juxtafoveal polyp and extension of the branching vascular network subfoveally. Isolated extrafoveal polyps may be treated with TL.
There is still no clarity regarding management of polyp + AVN in extrafoveal location. TL is associated with the risk of hemorrhage and scotomas. Hence, it is safer to consider such lesions for a combination treatment with PDT + Anti-VEGF therapy. TL for extrafoveal lesions should be limited to smaller lesions which are primarily polyps without much network. In addition, in majority of cases of PCV, the polyp + AVN can usually be covered by the largest PDT spot size that is available. Very rarely, we encounter larger networks. In such situation, the current recommendation would be to treat with the largest spot size with three loading doses of anti-VEGF agents. Subsequently, ICGA should be repeated at 3 months and further treatment should be based on the residual lesion size and activity. If the lesion is still active but responding to the treatment without any complications, we should consider one more cycle of combination therapy for the residual network.
The EVEREST study was the first randomized controlled trial comparing standard fluence (SF) PDT with or without three loading doses of ranibizumab 0.5 mg and ranibizumab monotherapy in PCV.[27] The primary endpoint was the proportion of patients with complete regression of polyps at 6 months, as determined by ICGA. The study reported a higher polyp closure rate of PDT with or without ranibizumab compared to ranibizumab alone (77.8% and 71.4% vs. 28.6%). This study established the efficacy of PDT in the closure of polyps. One limitation of EVEREST study was the short follow-up period. To overcome this limitation, EVEREST II study was designed to assess 24-month outcome of ranibizumab 0.5 mg monotherapy and ranibizumab in combination PDT for macular PCV.[14] The 12-month data reported better visual acuity gains in combined group (8.3 lines) versus ranibizumab monotherapy group (5.1 lines). In addition, the polyp regression rate was 69.3% in combination arm, whereas 34.7% in ranibizumab monotherapy arm. To assess the effect of PDT versus anti-VEGF in terms of visual outcome, the LAPTOP study, a multicenter randomized controlled trial was conducted.[40] Ninety-three patients were randomized to 2 arms: SF PDT monotherapy arm and a ranibizumab monotherapy arm where patients received 3 monthly injections of 0.5 mg ranibizumab. Additional treatment was performed as needed in each arm. At 12 months, the study found a higher proportion of patients gaining >0.2 logMAR units in the ranibizumab arm (30.4% vs. 17.0%). In addition, the mean gain in logMAR visual acuity was also greater in the ranibizumab arm at 12 and 24 months. These 2 trials showed that although PDT may be more effective at polyp closure than anti-VEGF, anti-VEGF therapy seemed to be better for improving or preventing visual loss in patients with PCV.
The FUJISAN study has shown that both early and deferred PDT showed similar functional and anatomical results at 12 months. However, the number of intravitreal ranibizumab injections is reduced in early PDT cases.[41]
Primary endpoint of treatment being polyp closure and improvement in visual acuity, these three landmark trials for PCV established the role of combination therapy of full-fluence PDT (greater polyp closure rate) with anti-VEGF agents (better visual outcomes) in initiating therapy for this disease entity.
In all of the reports of PDT in PCV with a follow-up of at least 1 year, preservation and improvement of VA were achieved in >80% of patients.[28,29,30,42,43,44,45,46,47,48,49,50,51,52,53,54]
PDT may be more effective for PCV than for neovascular AMD. In 2008, Gomi et al.[43] reported on the differences between outcomes in the treatment of PCV and neovascular AMD. Using ICGA, 36 eyes (39%) were diagnosed with PCV and 54 eyes (58%) with choroidal neovascularization secondary to AMD. The VA improved (15 letters) in AMD and PCV by 6% and 25%, respectively, and decreased (15 letters) by 31% and 8%, respectively. Fluorescein leakage stopped at 1 year in 86% of PCV and 61% of AMD eyes.
The one major concern regarding the efficacy of PDT for PCV is the recurrence or the development of new polypoidal lesions with longer follow-up.[55] Retinal function, as assessed by multifocal electroretinography, can be altered by PDT.[56] However, retinal sensitivity in the macular area of eyes with subfoveal PCV improved shortly after PDT.[57] Subretinal hemorrhage can occur after PDT. This is occasionally massive and can lead to vitreous hemorrhage and a poor visual prognosis. Recurrent bullous detachment and chorioretinal anastomosis after PDT have also been reported.[44,45,46,47,48]
Recent reports of aflibercept suggest that the success rate may be much higher than that reported with ranibizumab, although prospective randomized trials similar to EVEREST are lacking.[58] Off-label use of ziv-aflibercept has also been reported in PCV.[59] The PLANET study was a noninferiority trial comparing the effect of intravitreal aflibercept with rescue active PDT/rescue sham PDT in 333 eyes with PCV.[13] At 52 weeks, there was no significant difference in visual outcomes in aflibercept monotherapy arm (10.7 letters) and when combined with PDT (10.8 letters). No active polyp was detected in 81.7% of monotherapy arm and 88.9% of combination arm. In addition, polyp regression occurred in 38.9% of monotherapy patients and 44.8% of combination therapy patients, respectively, which was not significant. Given the excellent visual and anatomical outcomes, the PLANET study concluded that aflibercept monotherapy was noninferior to combination therapy with PDT.
Recommendation 12
Active subfoveal and juxtafoveal PCV should be treated with full-fluence PDT with three loading doses of anti-VEGF injections [Fig. 10].
Figure 10.
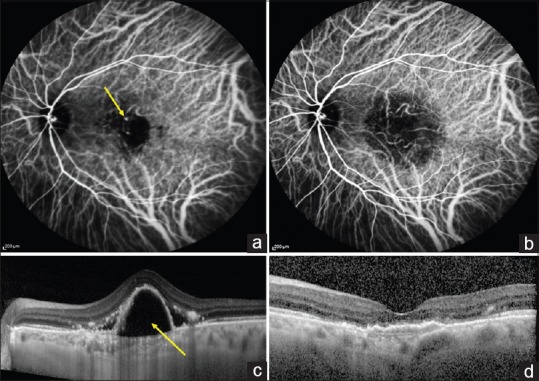
Pretreatment image of a patient with nodular hyperfluorescence on indocyanine green angiography (a; Yellow arrow) and thumb-like pigment epithelial detachments on spectral domain optical coherence tomography (c; Yellow arrow). After 3 months of treatment with full-fluence photodynamic therapy and three doses of intravitreal ranibizumab, there was complete resolution of polypoidal choroidal vasculopathy on indocyanine green angiography (b; absence of nodular hyperfluorescence) and spectral domain optical coherence tomography (d; resolution of pigment epithelial detachments and fluid)
Is there any role for Reduced-Fluence PDT in the management of PCV?
There are very few reports on RF PDT compared to SF PDT. While prospective randomized studies are lacking comparing the two, uncontrolled studies on RFPDT with or without anti-VEGF therapy suggest that the visual outcomes may be comparable to SF PDT.[60] The major advantage seems to be a lesser incidence of subretinal hemorrhage after PDT. Subretinal hemorrhage is known to be a characteristic adverse event after conventional PDT for the treatment of PCV. A risk of subretinal hemorrhage has been reported in 4.7% to 30.8% of patients with PCV.[28,43,61,62] In a prospective series of reduced fluence (RF) PDT for PCV, Yamashita et al., reported only minimal subretinal hemorrhage in 10% of patients with no case of severe subretinal hemorrhage over 1 optic disc diameter.[63] Studies of combined therapy with standard-fluence PDT and either intravitreal bevacizumab or intravitreal ranibizumab have reported reduced risk of subretinal hemorrhage, compared to PDT monotherapy.[64,65,66] It is thought that the decreased vascular permeability and the vasoconstrictive effect of intravitreal bevacizumab may result in suppression of hemorrhage and that a reduced light dose of PDT itself may reduce its risk as well.
Michels et al.,[67] reported that ICGA at 3 months after treatment demonstrated at least moderate perfusion changes of the choriocapillaris in 80% of the standard-fluence PDT (light dose, 50 J/cm2) group, while no choriocapillary perfusion changes of moderate or worse severity were present at 3 months in the reduced-fluence PDT group.
Recommendation 13
RF PDT should be performed in the following situations:
BCVA ≥20/40
Lesion size >3 DD (Higher chances of bleeding with SF PDT)
What is the role of anti-VEGF agents in management of PCV, both as a primary modality of treatment and in management of residual/recurrent PCV?
Recommendation 14
If initially the extent of lesion is not clearly defined on ICG due to the presence of blocked fluorescence secondary to hemorrhage, it is advisable to initiate anti-VEGF monotherapy alone. Once the hemorrhage clears, ICG + FFA should be performed and if PCV is confirmed, combination therapy with PDT and anti-VEGF agent should be done. Anti-VEGF monotherapy can also be considered in peripapillary PCV. Exceptional situations, such as lack of access to PDT and in resource-constrained countries, there may be an unavoidable situation of treating with anti-VEGF monotherapy [Fig. 11]. However, there is a strong possibility that there may be incomplete resolution of polyps, and the number of injections required would be more than what may be required when PDT is combined with anti-VEGF therapy.
Figure 11.
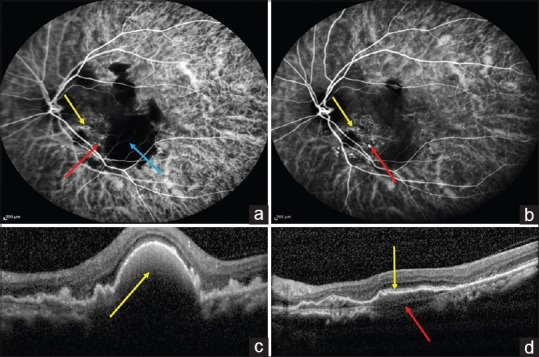
Pretreatment indocyanine green angiography (a) image of a patient with nodular hyperfluorescence (a; red arrow), abnormal vascular network (AVN; Yellow arrow), and large area of blocked hyperfluorescence due to hemorrhage (a; Blue arrow) and corresponding spectral domain optical coherence tomography (c) showing thumb-like pigment epithelial detachments with dense hyperreflectivity with backshadowing suggestive of hemorrhagic pigment epithelial detachments (Yellow arrow). After treatment with four doses of monthly intravitreal ranibizumab, indocyanine green angiography (b) showed residual polyps (b; Red arrow) and abnormal vascular network (b; Yellow arrow) while the blocked fluorescence resolved completely and corresponding spectral domain optical coherence tomography (d) demonstrated resolution of pigment epithelial detachments but persistence of double-layer sign represented by irregular retinal pigment epithelium elevation (d; Yellow line) and Bruch's membrane (d; Red arrow)
Recommendation 15
Indications for initiation with anti-VEGF monotherapy:
Small submacular hemorrhage associated with PCV (<4DD)
Thin submacular hemorrhage associated with PCV (< 500 μm)
Polyp extent not clearly defined by ICG
Peripapillary PCV
Of all the anti-VEGF agents available today, which one should be the agent of choice?
All the landmark trials including the EVEREST, LAPTOP, and FUJISAN have evaluated the role of ranibizumab as monotherapy or in combination therapy.[27,40,41] They have shown polyp regression rate ranging from 25% to 33% with significantly better visual acuity outcomes. Bevacizumab monotherapy has shown similar results in polyp regression rates, BCVA improvement, and central macular thickness reduction in comparison with ranibizumab monotherapy by Cho et al. at 6 months.[68] However, not many other studies have evaluated the role of bevacizumab therapy.
Aflibercept is a recombinant soluble fusion protein with enhanced binding affinity to VEGF-A, VEGF-B, and placental growth factor as compared to ranibizumab and bevacizumab.[58] This facilitates increased response to sub-RPE lesions such as PCV. Inoue et al.[69] has shown a polyp regression rate of 75% at the end of 6 months in 16 eyes. Yamamoto et al.[70] evaluated 1 year outcomes of 90 eyes treated with monthly aflibercept for first 3 months followed by 2 monthly doses. They demonstrated statistically significant improvement in BCVA and reduction in the central retinal thickness at 12 months from baseline (P < 0.001; P < 0.001). About 71.1% eyes had dry macula and polyp regression was complete in 55.4% and partial in 32.5% of eyes. Saito et al.[71] exhibited additional polyp regression (50%), improved BCVA and reduction in central retinal thickness after switching to aflibercept in patients’ refractory to ranibizumab. However, in the landmark PLANET study, the polyp regression rate was 38.9% with aflibercept which is much lower than other studies in literature.[13] However, direct comparison between EVEREST and PLANET studies is limited due to differences in the study design. While in EVEREST study, PDT was given as baseline, and in the PLANET study, it was given as a rescue therapy. Thus, the polyp regression rate with aflibercept (38.9%–75%) is comparatively higher as compared to ranibizumab (25%–33%).[27,71]
Recommendation 16
Ranibizumab is considered as the preferred anti-VEGF agent based on level I evidence. Although no level I evidence exists for aflibercept use till now, it can also be considered as a primary anti-VEGF agent or in patients refractory to ranibizumab based on physician's discretion.
What should be our follow-up protocol of patients who receive PDT + Anti-VEGF combination therapy? When should ICGA + FFA be repeated after initiating therapy?
After initiation of treatment, the patient should be followed up monthly for 3 months with evaluation of BCVA, fundus examination, OCT, and loading dose of anti-VEGF agent. At the end of 3 months, ICG + FFA should be performed to evaluate the disease activity in addition to OCT. In cases with complete regression of polyp (defined as no intraretinal and subretinal fluid on OCT, resolution on ICG, and no leakage on FFA), the patient should be followed up monthly up to 6 months and every 3 monthly thereafter. This is defined as the “Wait and Observe” regimen. BCVA and OCT should be performed at all visits and ICG + FFA at 6 months and 12 months, respectively. OCT features may be a useful guidance to decide on repeating ICG angiography. If there is incomplete regression of polyps, repeat treatment with SF PDT with anti-VEGF agents should be performed with monthly BCVA and OCT follow-up. In scenarios where the polyps have regressed completely but leaking AVN persists, anti-VEGF monotherapy should be executed.
Recommendation 17
ICGA + FFA should be repeated after 3 months to analyze disease activity. If quiescent, ICGA + FFA should be repeated again after 6 months and 12 months, respectively. BCVA and OCT should be performed at all follow-up visits. For incomplete regression of polyps, retreatment with full-fluence PDT with intravitreal injection of anti-VEGF should be performed. Half-fluence PDT may also be considered if the BCVA is ≥ 20/40. If FFA/ICGA shows no polyp, but persistence of leaking AVN, monotherapy with anti-VEGF should be performed.
How do we recognize and manage recurrent PCV?
OCT is indicated at every visit to look for subretinal or intraretinal fluid and PED. On enhanced SD-OCT images, AVNs are marked by undulation of the RPE line associated with a clearly delineated Bruch's membrane (DLS).[72] Recurrence of subretinal fluid, PED, or fresh subretinal hemorrhage could be useful OCT-based indicators to repeat ICG angiography.[12,73]
In typical fresh cases, the DLS is lost when the fine vascular network regresses or increases when the network enlarges.[74] However, in majority of the cases, the fine vascular network seems to be present within or above Bruch's membrane, and may permit fluid leakage into the subpigment epithelial space.[74,75,76]
Recommendation 18
At any of the follow-up visits, if there is a drop in BCVA or appearance of hemorrhage or exudation seen clinically or presence of fluid (subretinal/intraretinal) on OCT, ICG + FFA should be repeated. For recurrence of polyps seen on FFA/ICG, retreatment with full-fluence PDT with intravitreal injection of anti-VEGF should be performed. Reduced-fluence PDT may also be considered if the BCVA is ≥20/40. If FFA/ICGA shows no polyp but the persistence of leaking AVN, monotherapy with anti-VEGF should be executed.
Nonresponsiveness either due to tachyphylaxis or due to tolerance is known. Switch over to another anti-VEGF or increase in the dose of anti-VEGF injections has been tried by a few. Moon et al.[77] in a retrospective analysis of 32 cases reported efficacy of aflibercept for improvement and maintenance of BCVA for PCV refractory to ranibizumab. Marcus et al.[78] reported the efficacy of 2.0 mg/0.05 ml of ranibizumab in PCV without any increase in adverse effects. However, the evidence regarding effectiveness of these therapies remains limited. Further large-scale prospective studies will be required before definite guidelines can be established in this regard.
Treatment of extrafoveal, peripapillary, and peripheral polypoidal choroidal vasculopathy
What is the role of thermal laser in management of PCV? What should be the laser parameters in treating PCV?
TL has a significant role in the management of PCV since a significant proportion of PCV lesions arise in extrafoveal, peripapillary, and peripheral regions [Fig. 12]. It is an effective treatment modality and relatively inexpensive as compared to PDT.[79,80]
Figure 12.
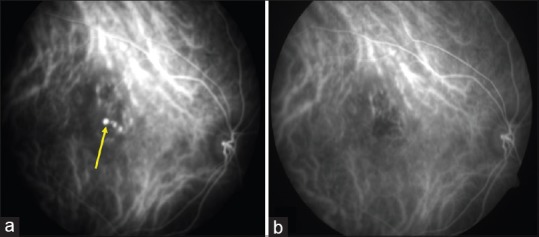
Pretreatment indocyanine green angiography (a) demonstrating nodular hyperfluorescence (Yellow arrow) suggestive of extrafoveal polypoidal choroidal vasculopathy. After treatment with thermal laser and three loading doses of intravitreal ranibizumab, there was complete resolution of polyps on indocyanine green angiography (b)
Recommendation 19
Guidelines for the management of extrafoveal PCV:
Between 200 μ-≤500 μ from fovea = PDT + 3 loading doses of anti-VEGF agents
-
500 μ-≤1000 μ from fovea =
- Lesion size >1000 μ: PDT + 3 loading doses of anti-VEGF agents
- Lesion size ≤1000 μ: TL + Anti-VEGF
Beyond 1000 μ from fovea = TL + Anti-VEGF
While determining the management of extrafoveal PCV based on the location from the fovea, it is important to note that determination of the center of fovea may be difficult and needs due consideration. In addition, the 500–1000 μ limit refers to the macular edge of the lesion and not the center of the lesion.
One major concern with the use of TL is chorioretinal scarring, scotoma, and CNVM formation.[80,81] Hence, it is preferable to give TL to lesions beyond 1000 μ from the center of fovea. For lesions between 500 μ and 1000 μ from the center of fovea, TL can be considered if the lesion size is <1000 μ. This reduces chances of foveal damage due to scar expansion. TL is normally done with 532-green argon laser with a spot size of 100 μ–200 μ and duration 200–300 ms.[11] The target is to achieve a grayish or moderately white lesion, and these should be titrated according to the blanching starting with low energy.
Recommendation 20
Guidelines for the management of peripapillary and peripheral PCV:
Active symptomatic PCV: TL + Anti-VEGF agent
Active asymptomatic PCV: Consider treatment
Quiescent PCV: Observe
The outcome of TL is variable. Lafaut et al.[6] has demonstrated 100% polyp regression in peripapillary region, whereas only 55.5% in case of macular polyps. In another study, Kwok et al.[17] demonstrated that 56% of TL-treated eyes had stable visual acuity as compared to 31% of nonlaser group. Lee et al.[78] found at 12 months after TL to PCV, 75% of eyes had stable or improved vision and 64.3% of eyes showed clinical or angiographic resolution of maculopathy. Despite receiving TL, 14.3% of eyes still had persistent leakage causing neurosensory detachment, and 10.7% of treated eyes developed subfoveal recurrence of polyps. Moreover, another 10.7% of eyes developed secondary CNVM subsequently.
Thermal laser for abnormal vascular network
With the use of high-speed videoangiography, feeder vessel can be visualized in up to 70% of PCV cases. Multiple studies have shown favorable results with regard to feeder vessel ablation. In a retrospective study by Nishijima et al.,[82] the use of ICGA-guided feeder vessel laser photocoagulation resulted in complete resolution of serous macular detachment in 66% of eyes after the mean follow-up of 13.6 months. Moreover, 53% of eyes had improvement in BCVA by 2 lines or more, and only 13% of eyes had vision loss after treatment. However, 60% of eyes required 2 or more laser treatment sessions due to persistent or recurrent polypoidal lesions. In a retrospective study comparing TL to polyp alone (Group 1) versus TL to polyp and AVN (Group 2), Yuzawa et al.[81] showed stabilization or improvement in BCVA in 46% of eyes in Group 2 as compared to 90% of eyes in group 1. While comparing the role of TL alone or in combination with anti-VEGF agent for extrafoveal PCV, Cheung et al.[79] have demonstrated no significant difference in visual outcomes between the two groups. Treatment of the entire AVN lesion is more controversial since AVN usually involves a large area requiring excessive laser photocoagulation and subsequently higher likelihood of complications.
Recommendation 21
Photocoagulation to the feeder vessel should be certainly considered in cases where it is visible on ICG and it is >500 μ from the center of fovea. Treatment of the whole lesion is controversial and is based on discretion.
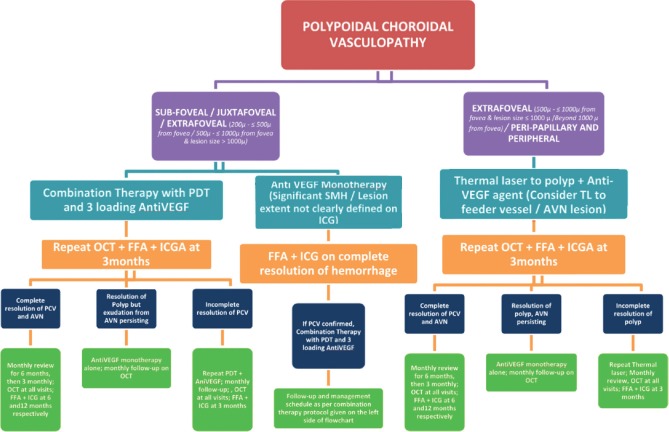
Conclusions
A concise table regarding the updated guidelines for the management of PCV based on evidence in literature and collective experience of panel of experts is depicted in Fig. 13. Our panel endorses the need for randomized long-term trials in evaluating the role of evolving treatment modalities such as RF PDT and newer anti-VEGF agents such as aflibercept and conbercept in addition to traditional modalities such as PDT, anti-VEGF agents such as ranibizumab, TL photocoagulation, and pneumatic displacement ± tPA. Furthermore, research into the pathogenesis, genetic and racial risk factors, and relatively less response to anti-VEGF agents in PCV as compared to Wet AMD are warranted.
Figure 13.
Flowchart for management of PCV based on the updated guidelines
One of the limitations of the current recommendations includes that they are based on the current body of literature on the management of PCV and their interpretation by the authors. In current clinical practice, many of the patients with PCV are managed with anti-VEGF monotherapy for various reasons which also include poor accessibility to PDT. It is imperative for the treating specialist to appropriately recognize the eyes which are poor/nonresponders to anti-VEGF therapy and shift them to combination therapy with PDT. Although initial experience with intravitreal aflibercept based on current literature is more promising than other anti-VEGF agents, we still do not have long-term data and results with aflibercept.
In summary, the modified evidence-based guidelines for the management of PCV emphasizes the need for ICGA + FFA + OCT for diagnosis and monitoring of disease activity and recommends PDT with three loading doses of anti-VEGF for treating subfoveal and juxtafoveal PCV, whereas TL photocoagulation ± anti-VEGF for extrafoveal, peripapillary, and peripheral PCV. These recommendations would be advantageous to the treating physician in diagnosing PCV and in formulating the best possible individualized treatment strategy for optimal outcomes in PCV management.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Yannuzzi LA. Miami, FL: 1982. Idiopathic polypoidal choroidal vasculopathy. Macula Society Meeting. [Google Scholar]
- 2.Liu Y, Wen F, Huang S, Luo G, Yan H, Sun Z, et al. Subtype lesions of neovascular age-related macular degeneration in chinese patients. Graefes Arch Clin Exp Ophthalmol. 2007;245:1441–5. doi: 10.1007/s00417-007-0575-8. [DOI] [PubMed] [Google Scholar]
- 3.Maruko I, Iida T, Saito M, Nagayama D, Saito K. Clinical characteristics of exudative age-related macular degeneration in Japanese patients. Am J Ophthalmol. 2007;144:15–22. doi: 10.1016/j.ajo.2007.03.047. [DOI] [PubMed] [Google Scholar]
- 4.Chang YC, Wu WC. Polypoidal choroidal vasculopathy in Taiwanese patients. Ophthalmic Surg Lasers Imaging. 2009;40:576–81. doi: 10.3928/15428877-20091030-07. [DOI] [PubMed] [Google Scholar]
- 5.Byeon SH, Lee SC, Oh HS, Kim SS, Koh HJ, Kwon OW, et al. Incidence and clinical patterns of polypoidal choroidal vasculopathy in Korean patients. Jpn J Ophthalmol. 2008;52:57–62. doi: 10.1007/s10384-007-0498-2. [DOI] [PubMed] [Google Scholar]
- 6.Lafaut BA, Leys AM, Snyers B, Rasquin F, De Laey JJ. Polypoidal choroidal vasculopathy in caucasians. Graefes Arch Clin Exp Ophthalmol. 2000;238:752–9. doi: 10.1007/s004170000180. [DOI] [PubMed] [Google Scholar]
- 7.Ladas ID, Rouvas AA, Moschos MM, Synodinos EE, Karagiannis DA, Koutsandrea CN, et al. Polypoidal choroidal vasculopathy and exudative age-related macular degeneration in Greek population. Eye (Lond) 2004;18:455–9. doi: 10.1038/sj.eye.6700706. [DOI] [PubMed] [Google Scholar]
- 8.Scassellati-Sforzolini B, Mariotti C, Bryan R, Yannuzzi LA, Giuliani M, Giovannini A, et al. Polypoidal choroidal vasculopathy in Italy. Retina. 2001;21:121–5. doi: 10.1097/00006982-200104000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Imamura Y, Engelbert M, Iida T, Freund KB, Yannuzzi LA. Polypoidal choroidal vasculopathy: A review. Surv Ophthalmol. 2010;55:501–15. doi: 10.1016/j.survophthal.2010.03.004. [DOI] [PubMed] [Google Scholar]
- 10.Sho K, Takahashi K, Yamada H, Wada M, Nagai Y, Otsuji T, et al. Polypoidal choroidal vasculopathy: Incidence, demographic features, and clinical characteristics. Arch Ophthalmol. 2003;121:1392–6. doi: 10.1001/archopht.121.10.1392. [DOI] [PubMed] [Google Scholar]
- 11.Anantharaman G, Ramkumar G, Gopalakrishnan M, Rajput A. Clinical features, management and visual outcome of polypoidal choroidal vasculopathy in Indian patients. Indian J Ophthalmol. 2010;58:399–405. doi: 10.4103/0301-4738.67052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Koh AH; Expert PCV Panel, Chen LJ, Chen SJ, Chen Y, Giridhar A, Iida T, et al. Polypoidal choroidal vasculopathy: Evidence-based guidelines for clinical diagnosis and treatment. Retina. 2013;33:686–716. doi: 10.1097/IAE.0b013e3182852446. [DOI] [PubMed] [Google Scholar]
- 13.Cheung G. Intravitreal Aflibercept in the Treatment of Polypoidal Choroidal Vasculopathy: The Planet Study. Presented at the 10th APVRS Annual Meeting, Bangkok. 2016 [Google Scholar]
- 14.Koh A, Lai TYY, Takahashi K, Wong TY, Chen LJ, Ruamviboonsuk P, et al. Efficacy and safety of ranibizumab with or without verteporfin photodynamic therapy for polypoidal choroidal vasculopathy: A Randomized clinical trial. JAMA Ophthalmol. 2017;135:1206–13. doi: 10.1001/jamaophthalmol.2017.4030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ampornpruet A, Ruamviboonsuk P, Kokekhuntod S. The fundoscopic features for differentiation between polypoidal choroidal vasculopathy and choroidal neovascularization from age-related macular degeneration. J Med Assoc Thai. 2005;88(Suppl 9):S51–6. [PubMed] [Google Scholar]
- 16.Uyama M, Wada M, Nagai Y, Matsubara T, Matsunaga H, Fukushima I, et al. Polypoidal choroidal vasculopathy: Natural history. Am J Ophthalmol. 2002;133:639–48. doi: 10.1016/s0002-9394(02)01404-6. [DOI] [PubMed] [Google Scholar]
- 17.Kwok AK, Lai TY, Chan CW, Neoh EL, Lam DS. Polypoidal choroidal vasculopathy in Chinese patients. Br J Ophthalmol. 2002;86:892–7. doi: 10.1136/bjo.86.8.892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mantel I, Schalenbourg A, Zografos L. Peripheral exudative hemorrhagic chorioretinopathy: Polypoidal choroidal vasculopathy and hemodynamic modifications. Am J Ophthalmol. 2012;153:910–2200. doi: 10.1016/j.ajo.2011.10.017. [DOI] [PubMed] [Google Scholar]
- 19.Coscas G, Lupidi M, Coscas F, Benjelloun F, Zerbib J, Dirani A, et al. Toward a specific classification of polypoidal choroidal vasculopathy: Idiopathic disease or subtype of age-related macular degeneration. Invest Ophthalmol Vis Sci. 2015;56:3187–95. doi: 10.1167/iovs.14-16236. [DOI] [PubMed] [Google Scholar]
- 20.Desmettre T, Devoisselle JM, Mordon S. Fluorescence properties and metabolic features of indocyanine green (ICG) as related to angiography. Surv Ophthalmol. 2000;45:15–27. doi: 10.1016/s0039-6257(00)00123-5. [DOI] [PubMed] [Google Scholar]
- 21.Tan CS, Ngo WK, Chen JP, Tan NW, Lim TH; EVEREST Study Group. EVEREST study report 2: Imaging and grading protocol, and baseline characteristics of a randomised controlled trial of polypoidal choroidal vasculopathy. Br J Ophthalmol. 2015;99:624–8. doi: 10.1136/bjophthalmol-2014-305674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cheung CM, Laude A, Wong W, Mathur R, Chan CM, Wong E, et al. Improved specificity of polypoidal choroidal vasculopathy diagnosis using a modified Everest criteria. Retina. 2015;35:1375–80. doi: 10.1097/IAE.0000000000000482. [DOI] [PubMed] [Google Scholar]
- 23.Japanese Study Group of Polypoidal Choroidal Vasculopathy. Criteria for diagnosis of polypoidal choroidal vasculopathy. Nippon Ganka Gakkai Zasshi. 2005;109:417–27. [PubMed] [Google Scholar]
- 24.Guyer DR, Yannuzzi LA, Slakter JS, Sorenson JA, Hope-Ross M, Orlock DR, et al. Digital indocyanine-green videoangiography of occult choroidal neovascularization. Ophthalmology. 1994;101:1727–35. doi: 10.1016/s0161-6420(13)31433-x. [DOI] [PubMed] [Google Scholar]
- 25.Kang SW, Chung SE, Shin WJ, Lee JH. Polypoidal choroidal vasculopathy and late geographic hyperfluorescence on indocyanine green angiography. Br J Ophthalmol. 2009;93:759–64. doi: 10.1136/bjo.2008.145862. [DOI] [PubMed] [Google Scholar]
- 26.Honda S, Matsumiya W, Negi A. Polypoidal choroidal vasculopathy: Clinical features and genetic predisposition. Ophthalmologica. 2014;231:59–74. doi: 10.1159/000355488. [DOI] [PubMed] [Google Scholar]
- 27.Koh A, Lee WK, Chen LJ, Chen SJ, Hashad Y, Kim H, et al. EVEREST study: Efficacy and safety of verteporfin photodynamic therapy in combination with ranibizumab or alone versus ranibizumab monotherapy in patients with symptomatic macular polypoidal choroidal vasculopathy. Retina. 2012;32:1453–64. doi: 10.1097/IAE.0b013e31824f91e8. [DOI] [PubMed] [Google Scholar]
- 28.Chan WM, Lam DS, Lai TY, Liu DT, Li KK, Yao Y, et al. Photodynamic therapy with verteporfin for symptomatic polypoidal choroidal vasculopathy: One-year results of a prospective case series. Ophthalmology. 2004;111:1576–84. doi: 10.1016/j.ophtha.2003.12.056. [DOI] [PubMed] [Google Scholar]
- 29.Eandi CM, Ober MD, Freund KB, Slakter JS, Yannuzzi LA. Selective photodynamic therapy for neovascular age-related macular degeneration with polypoidal choroidal neovascularization. Retina. 2007;27:825–31. doi: 10.1097/IAE.0b013e31804b3f70. [DOI] [PubMed] [Google Scholar]
- 30.Otani A, Sasahara M, Yodoi Y, Aikawa H, Tamura H, Tsujikawa A, et al. Indocyanine green angiography: Guided photodynamic therapy for polypoidal choroidal vasculopathy. Am J Ophthalmol. 2007;144:7–14. doi: 10.1016/j.ajo.2007.03.014. [DOI] [PubMed] [Google Scholar]
- 31.Gomi F, Sawa M, Mitarai K, Tsujikawa M, Tano Y. Angiographic lesion of polypoidal choroidal vasculopathy on indocyanine green and fluorescein angiography. Graefes Arch Clin Exp Ophthalmol. 2007;245:1421–7. doi: 10.1007/s00417-007-0564-y. [DOI] [PubMed] [Google Scholar]
- 32.Tan CS, Ngo WK, Lim LW, Lim TH. A novel classification of the vascular patterns of polypoidal choroidal vasculopathy and its relation to clinical outcomes. Br J Ophthalmol. 2014;98:1528–33. doi: 10.1136/bjophthalmol-2014-305059. [DOI] [PubMed] [Google Scholar]
- 33.Alshahrani ST, Al Shamsi HN, Kahtani ES, Ghazi NG. Spectral-domain optical coherence tomography findings in polypoidal choroidal vasculopathy suggest a type 1 neovascular growth pattern. Clin Ophthalmol. 2014;8:1689–95. doi: 10.2147/OPTH.S68471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.De Salvo G, Vaz-Pereira S, Keane PA, Tufail A, Liew G. Sensitivity and specificity of spectral-domain optical coherence tomography in detecting idiopathic polypoidal choroidal vasculopathy. Am J Ophthalmol. 2014;158:1228–380. doi: 10.1016/j.ajo.2014.08.025. [DOI] [PubMed] [Google Scholar]
- 35.Liu R, Li J, Li Z, Yu S, Yang Y, Yan H, et al. Distinguishing polypoidal choroidal vasculopathy from typical neovascular age-related macular degeneration based on spectral domain optical coherence tomography. Retina. 2016;36:778–86. doi: 10.1097/IAE.0000000000000794. [DOI] [PubMed] [Google Scholar]
- 36.Chung SE, Kang SW, Lee JH, Kim YT. Choroidal thickness in polypoidal choroidal vasculopathy and exudative age-related macular degeneration. Ophthalmology. 2011;118:840–5. doi: 10.1016/j.ophtha.2010.09.012. [DOI] [PubMed] [Google Scholar]
- 37.Jirarattanasopa P, Ooto S, Nakata I, Tsujikawa A, Yamashiro K, Oishi A, et al. Choroidal thickness, vascular hyperpermeability, and complement factor H in age-related macular degeneration and polypoidal choroidal vasculopathy. Invest Ophthalmol Vis Sci. 2012;53:3663–72. doi: 10.1167/iovs.12-9619. [DOI] [PubMed] [Google Scholar]
- 38.Yamaoka S, Okada AA, Sugahara M, Hida T. Clinical features of polypoidal choroidal vasculopathy and visual outcomes in the absence of classic choroidal neovascularization. Ophthalmologica. 2010;224:147–52. doi: 10.1159/000236040. [DOI] [PubMed] [Google Scholar]
- 39.Laude A, Cackett PD, Vithana EN, Yeo IY, Wong D, Koh AH, et al. Polypoidal choroidal vasculopathy and neovascular age-related macular degeneration: Same or different disease? Prog Retin Eye Res. 2010;29:19–29. doi: 10.1016/j.preteyeres.2009.10.001. [DOI] [PubMed] [Google Scholar]
- 40.Oishi A, Miyamoto N, Mandai M, Honda S, Matsuoka T, Oh H, et al. LAPTOP study: A 24-month trial of verteporfin versus ranibizumab for polypoidal choroidal vasculopathy. Ophthalmology. 2014;121:1151–2. doi: 10.1016/j.ophtha.2013.12.037. [DOI] [PubMed] [Google Scholar]
- 41.Gomi F, Oshima Y, Mori R, Kano M, Saito M, Yamashita A, et al. Initial versus delayed photodynamic therapy in combination with ranibizumab for treatment of polypoidal choroidal vasculopathy: The Fujisan Study. Retina. 2015;35:1569–76. doi: 10.1097/IAE.0000000000000526. [DOI] [PubMed] [Google Scholar]
- 42.Akaza E, Mori R, Yuzawa M. Long-term results of photodynamic therapy of polypoidal choroidal vasculopathy. Retina. 2008;28:717–22. doi: 10.1097/IAE.0b013e31816577cb. [DOI] [PubMed] [Google Scholar]
- 43.Gomi F, Ohji M, Sayanagi K, Sawa M, Sakaguchi H, Oshima Y, et al. One-year outcomes of photodynamic therapy in age-related macular degeneration and polypoidal choroidal vasculopathy in Japanese patients. Ophthalmology. 2008;115:141–6. doi: 10.1016/j.ophtha.2007.02.031. [DOI] [PubMed] [Google Scholar]
- 44.Honda S, Imai H, Yamashiro K, Kurimoto Y, Kanamori-Matsui N, Kagotani Y, et al. Comparative assessment of photodynamic therapy for typical age-related macular degeneration and polypoidal choroidal vasculopathy: A multicenter study in Hyogo prefecture, Japan. Ophthalmologica. 2009;223:333–8. doi: 10.1159/000221837. [DOI] [PubMed] [Google Scholar]
- 45.Kurashige Y, Otani A, Sasahara M, Yodoi Y, Tamura H, Tsujikawa A, et al. Two-year results of photodynamic therapy for polypoidal choroidal vasculopathy. Am J Ophthalmol. 2008;146:513–9. doi: 10.1016/j.ajo.2008.05.025. [DOI] [PubMed] [Google Scholar]
- 46.Lee WK, Lee PY, Lee SK. Photodynamic therapy for polypoidal choroidal vasculopathy: Vaso-occlusive effect on the branching vascular network and origin of recurrence. Jpn J Ophthalmol. 2008;52:108–15. doi: 10.1007/s10384-007-0501-y. [DOI] [PubMed] [Google Scholar]
- 47.Mauget-Faÿsse M, Quaranta-El Maftouhi M, De La Marnièrre E, Leys A. Photodynamic therapy with verteporfin in the treatment of exudative idiopathic polypoidal choroidal vasculopathy. Eur J Ophthalmol. 2006;16:695–704. doi: 10.1177/112067210601600506. [DOI] [PubMed] [Google Scholar]
- 48.Ogino T, Takeda M, Imaizumi H, Okushiba U. Photodynamic therapy for age-related macular degeneration in japanese patients: Results after one year. Jpn J Ophthalmol. 2007;51:210–5. doi: 10.1007/s10384-007-0436-3. [DOI] [PubMed] [Google Scholar]
- 49.Quaranta M, Mauget-Faÿsse M, Coscas G. Exudative idiopathic polypoidal choroidal vasculopathy and photodynamic therapy with verteporfin. Am J Ophthalmol. 2002;134:277–80. doi: 10.1016/s0002-9394(02)01516-7. [DOI] [PubMed] [Google Scholar]
- 50.Rogers AH, Greenberg PB, Martidis A, Puliafito CA. Photodynamic therapy of polypoidal choroidal vasculopathy. Ophthalmic Surg Lasers Imaging. 2003;34:60–3. [PubMed] [Google Scholar]
- 51.Saito M, Iida T, Nagayama D. Photodynamic therapy with verteporfin for age-related macular degeneration or polypoidal choroidal vasculopathy: Comparison of the presence of serous retinal pigment epithelial detachment. Br J Ophthalmol. 2008;92:1642–7. doi: 10.1136/bjo.2007.137075. [DOI] [PubMed] [Google Scholar]
- 52.Sayanagi K, Gomi F, Sawa M, Ohji M, Tano Y. Long-term follow-up of polypoidal choroidal vasculopathy after photodynamic therapy with verteporfin. Graefes Arch Clin Exp Ophthalmol. 2007;245:1569–71. doi: 10.1007/s00417-007-0582-9. [DOI] [PubMed] [Google Scholar]
- 53.Silva RM, Figueira J, Cachulo ML, Duarte L, Faria de Abreu JR, Cunha-Vaz JG, et al. Polypoidal choroidal vasculopathy and photodynamic therapy with verteporfin. Graefes Arch Clin Exp Ophthalmol. 2005;243:973–9. doi: 10.1007/s00417-005-1139-4. [DOI] [PubMed] [Google Scholar]
- 54.Spaide RF, Donsoff I, Lam DL, Yannuzzi LA, Jampol LM, Slakter J, et al. Treatment of polypoidal choroidal vasculopathy with photodynamic therapy. Retina. 2002;22:529–35. doi: 10.1097/00006982-200210000-00001. [DOI] [PubMed] [Google Scholar]
- 55.Gomi F, Sawa M, Sakaguchi H, Tsujikawa M, Oshima Y, Kamei M, et al. Efficacy of intravitreal bevacizumab for polypoidal choroidal vasculopathy. Br J Ophthalmol. 2008;92:70–3. doi: 10.1136/bjo.2007.122283. [DOI] [PubMed] [Google Scholar]
- 56.Imai H, Honda S, Nakanishi Y, Yamamoto H, Tsukahara Y, Negi A, et al. Different transitions of multifocal electroretinogram recordings between patients with age-related macular degeneration and polypoidal choroidal vasculopathy after photodynamic therapy. Br J Ophthalmol. 2006;90:1524–30. doi: 10.1136/bjo.2006.092783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Yodoi Y, Tsujikawa A, Kameda T, Otani A, Tamura H, Mandai M, et al. Central retinal sensitivity measured with the micro perimeter 1 after photodynamic therapy for polypoidal choroidal vasculopathy. Am J Ophthalmol. 2007;143:984–94. doi: 10.1016/j.ajo.2007.01.026. [DOI] [PubMed] [Google Scholar]
- 58.Hara C, Sawa M, Sayanagi K, Nishida K. One-year results of intravitreal aflibercept for polypoidal choroidal vasculopathy. Retina. 2016;36:37–45. doi: 10.1097/IAE.0000000000000767. [DOI] [PubMed] [Google Scholar]
- 59.Videkar C, Kapoor A, Chhablani J, Narayanan R. Ziv-aflibercept: A novel option for the treatment of polypoidal choroidal vasculopathy. BMJ Case Rep 2015. 2015 doi: 10.1136/bcr-2015-212988. pii: bcr2015212988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Fan NW, Lau LI, Chen SJ, Yang CS, Lee FL. Comparison of the effect of reduced-fluence photodynamic therapy with intravitreal bevacizumab and standard-fluence alone for polypoidal choroidal vasculopathy. J Chin Med Assoc. 2014;77:101–7. doi: 10.1016/j.jcma.2013.10.012. [DOI] [PubMed] [Google Scholar]
- 61.Akaza E, Yuzawa M, Matsumoto Y, Kashiwakura S, Fujita K, Mori R, et al. Role of photodynamic therapy in polypoidal choroidal vasculopathy. Jpn J Ophthalmol. 2007;51:270–7. doi: 10.1007/s10384-007-0452-3. [DOI] [PubMed] [Google Scholar]
- 62.Hirami Y, Tsujikawa A, Otani A, Yodoi Y, Aikawa H, Mandai M, et al. Hemorrhagic complications after photodynamic therapy for polypoidal choroidal vasculopathy. Retina. 2007;27:335–41. doi: 10.1097/01.iae.0000233647.78726.46. [DOI] [PubMed] [Google Scholar]
- 63.Yamashita A, Shiraga F, Shiragami C, Shirakata Y, Fujiwara A. Two-year results of reduced-fluence photodynamic therapy for polypoidal choroidal vasculopathy. Am J Ophthalmol. 2013;155:96–1020. doi: 10.1016/j.ajo.2012.06.027. [DOI] [PubMed] [Google Scholar]
- 64.Sato T, Kishi S, Matsumoto H, Mukai R. Combined photodynamic therapy with verteporfin and intravitreal bevacizumab for polypoidal choroidal vasculopathy. Am J Ophthalmol. 2010;149:947–540. doi: 10.1016/j.ajo.2009.12.038. [DOI] [PubMed] [Google Scholar]
- 65.Gomi F, Sawa M, Wakabayashi T, Sasamoto Y, Suzuki M, Tsujikawa M, et al. Efficacy of intravitreal bevacizumab combined with photodynamic therapy for polypoidal choroidal vasculopathy. Am J Ophthalmol. 2010;150:48–540. doi: 10.1016/j.ajo.2010.02.008. [DOI] [PubMed] [Google Scholar]
- 66.Ruamviboonsuk P, Tadarati M, Vanichvaranont S, Hanutsaha P, Pokawattana N. Photodynamic therapy combined with ranibizumab for polypoidal choroidal vasculopathy: Results of a 1-year preliminary study. Br J Ophthalmol. 2010;94:1045–51. doi: 10.1136/bjo.2009.173120. [DOI] [PubMed] [Google Scholar]
- 67.Michels S, Hansmann F, Geitzenauer W, Schmidt-Erfurth U. Influence of treatment parameters on selectivity of verteporfin therapy. Invest Ophthalmol Vis Sci. 2006;47:371–6. doi: 10.1167/iovs.05-0354. [DOI] [PubMed] [Google Scholar]
- 68.Cho HJ, Baek JS, Lee DW, Kim CG, Kim JW. Short-term effectiveness of intravitreal bevacizumab vs. ranibizumab injections for patients with polypoidal choroidal vasculopathy. Korean J Ophthalmol. 2012;26:157–62. doi: 10.3341/kjo.2012.26.3.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Inoue M, Arakawa A, Yamane S, Kadonosono K. Short-term efficacy of intravitreal aflibercept in treatment-naive patients with polypoidal choroidal vasculopathy. Retina. 2014;34:2178–84. doi: 10.1097/IAE.0000000000000229. [DOI] [PubMed] [Google Scholar]
- 70.Yamamoto A, Okada AA, Kano M, Koizumi H, Saito M, Maruko I, et al. One-year results of intravitreal aflibercept for polypoidal choroidal vasculopathy. Ophthalmology. 2015;122:1866–72. doi: 10.1016/j.ophtha.2015.05.024. [DOI] [PubMed] [Google Scholar]
- 71.Saito M, Kano M, Itagaki K, Oguchi Y, Sekiryu T. Switching to intravitreal aflibercept injection for polypoidal choroidal vasculopathy refractory to ranibizumab. Retina. 2014;34:2192–201. doi: 10.1097/IAE.0000000000000236. [DOI] [PubMed] [Google Scholar]
- 72.Sato T, Kishi S, Watanabe G, Matsumoto H, Mukai R. Tomographic features of branching vascular networks in polypoidal choroidal vasculopathy. Retina. 2007;27:589–94. doi: 10.1097/01.iae.0000249386.63482.05. [DOI] [PubMed] [Google Scholar]
- 73.Yamashita A, Shiraga F, Shiragami C, Ono A, Tenkumo K. One-year results of reduced-fluence photodynamic therapy for polypoidal choroidal vasculopathy. Am J Ophthalmol. 2010;149:465–710. doi: 10.1016/j.ajo.2009.09.020. [DOI] [PubMed] [Google Scholar]
- 74.Oishi A, Mandai M, Kimakura M, Nishida A, Kurimoto Y. Characteristics of fine vascular network pattern associated with recurrence of polypoidal choroidal vasculopathy. Eye (Lond) 2011;25:1020–6. doi: 10.1038/eye.2011.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wakabayashi T, Gomi F, Sawa M, Tsujikawa M, Tano Y. Marked vascular changes of polypoidal choroidal vasculopathy after photodynamic therapy. Br J Ophthalmol. 2008;92:936–40. doi: 10.1136/bjo.2007.132357. [DOI] [PubMed] [Google Scholar]
- 76.Hikichi T, Ohtsuka H, Higuchi M, Matsushita T, Ariga H, Kosaka S, et al. Improvement of angiographic findings of polypoidal choroidal vasculopathy after intravitreal injection of ranibizumab monthly for 3 months. Am J Ophthalmol. 2010;150:674–820. doi: 10.1016/j.ajo.2010.05.026. [DOI] [PubMed] [Google Scholar]
- 77.Moon DRC, Lee DK, Kim SH, You YS, Kwon OW. Aflibercept treatment for neovascular age-related macular degeneration and polypoidal choroidal vasculopathy refractory to anti-vascular endothelial growth factor. Korean J Ophthalmol. 2015;29:226–32. doi: 10.3341/kjo.2015.29.4.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Marcus DM, Singh H, Fechter CM, Chamberlain DP. High-dose ranibizumab monotherapy for neovascular polypoidal choroidal vasculopathy in a predominantly non-asian population. Eye (Lond) 2015;29:1427–37. doi: 10.1038/eye.2015.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Gemmy Cheung CM, Yeo I, Li X, Mathur R, Lee SY, Chan CM, et al. Argon laser with and without anti-vascular endothelial growth factor therapy for extrafoveal polypoidal choroidal vasculopathy. Am J Ophthalmol. 2013;155:295–3040. doi: 10.1016/j.ajo.2012.08.002. [DOI] [PubMed] [Google Scholar]
- 80.Lee MW, Yeo I, Wong D, Ang CL. Argon laser photocoagulationfor the treatment of polypoidal choroidal vasculopathy. Eye (Lond) 2009;23:145–8. doi: 10.1038/sj.eye.6702955. [DOI] [PubMed] [Google Scholar]
- 81.Yuzawa M, Mori R, Haruyama M. A study of laser photocoagulation for polypoidal choroidal vasculopathy. Jpn J Ophthalmol. 2003;47:379–84. doi: 10.1016/s0021-5155(03)00042-x. [DOI] [PubMed] [Google Scholar]
- 82.Nishijima K, Takahashi M, Akita J, Katsuta H, Tanemura M, Aikawa H, et al. Laser photocoagulation of indocyanine green angiographically identified feeder vessels to idiopathic polypoidal choroidal vasculopathy. Am J Ophthalmol. 2004;137:770–3. doi: 10.1016/j.ajo.2003.09.059. [DOI] [PubMed] [Google Scholar]