Abstract
Purpose:
The aim of this study was to establish the prevalence and association of age-related macular degeneration (AMD) and obesity which was not studied extensively in Indian population over 60 years of age.
Methods:
This was a cross-sectional, population-based study. A total of 4791 patients with gradable fundus photography were included. All patients underwent detailed ophthalmic examination and AMD was graded with retinal photographs. Grading of AMD was done according to the International ARM Epidemiological Study Group and staged based on grading in worse eye. The association of AMD severity and obesity (based on body mass index, waist–hip ratio, waist circumference, isolated abdominal obesity, isolated generalized obesity, and combined obesity) was assessed. The main outcome variable was an association between the presence and severity of AMD with different grades of obesity.
Results:
No direct significant association was noted between the presence and severity of AMD and any obesity indices. Subgroup analyses based on lifestyle patterns and common systemic pathologies in AMD population were done. Late AMD was significantly associated with tobacco consumption in population with combined obesity (P = 0.033 and odds ratio = 2.998).
Conclusion:
No direct association was noted between the presence or severity of AMD and obesity in South Indian population. However, indirect associations between the severity of AMD and combined obesity were found.
Keywords: Age-related macular degeneration, age-related macular degeneration and obesity, age-related macular degeneration in South Indian population, obesity, obesity in South Indian population
Age-related macular degeneration (AMD) is a complex disease with genetic and environmental etiology and is the leading cause of irreversible blindness in developed countries and in a few developing countries in the elderly age group.[1] It is a progressive neurodegenerative ocular disease which affects the central portion of retina and choroid.[2] Although few treatments are available for AMD, including specific nutritional intake and dietary supplements for dry AMD and anti-vascular endothelial growth factor (VEGF) therapies for neovascular form, without new treatments or preventive strategies, the rates of vision loss are expected to rise in the future. For this reason, a better understanding of the pathogenesis is essential to develop preventive measures to reduce the burden of the disease.
Chronic low-grade inflammation state was found to be involved in the complex pathogenesis of AMD. Obesity being a pro-inflammatory state contributes to the disease process.[3] Previous studies have shown an association of both generalized and abdominal obesities with AMD.[4,5]
Studies had reported that waist-to-hip ratio (WHR), which is a measure of abdominal obesity, had a stronger relationship with AMD than body mass index (BMI), which is a measure of generalized obesity.[4,5] Evidence shows that the prevalence of obesity, abdominal, general, and combined, differs in various populations and ethnic groups.
It has been postulated that Asians are prone to visceral fat accumulation, which might be the reason for the greatest prosperity to develop diseases such as diabetes at relatively low BMI values.[6] To the best of our knowledge, no population-based studies had been done which show the association of various types of obesity and AMD in India. The aim of this study is to establish the association of both abdominal and generalized obesities with AMD in Indian population.
Methods
A population-based, cross-sectional study of 5495 persons from Indian population, above the age of 60 years, was done between 2009 and 2011. The study design and research methodology were described in detail elsewhere.[7] This study was approved by the institutional review board, a written consent was obtained from the participants following the Declaration of Helsinki.
Of the 5495 patients, 4791 patients with gradable retinal photographs were included in the study. A detailed questionnaire enumerating the medical history, general physical examination, educational status, occupation, history of smoking, and consumption of tobacco and alcohol was admitted. The medical history data included the duration and treatment of diabetes mellitus, hypertension, and coronary artery disease. The ocular history included details of ocular complaints and past ocular treatment or surgery.
All the patients underwent a detailed ophthalmic evaluation, which includes assessment of visual acuity using modified Early Treatment Diabetic Retinopathy Study chart (Light House Low Vision Products, NY, USA), refraction, anterior-segment examination using a slit-lamp (Zeiss SL 130, Carl Zeiss, Jena, Germany), measurement of intraocular pressure (Zeiss AT 030 Applanation Tonometer; Carl Zeiss), and fundus examination using binocular indirect ophthalmoscope (Keeler Instruments Inc., Broomall, PA, USA).
Grading of lens opacification was done using the Lens Opacities Classification System III (LOCS Chart III; Leo T Chylack, Harvard Medical School, Boston, MA, USA) by experienced ophthalmologists. A slit-lamp photography of the crystalline lens after dilatation was obtained in all patients for comparing it with LOCS chart III and grading was done accordingly. Retinal photographs were obtained after pupillary dilatation (Carl Zeiss fundus camera; FF-450, Germany). The grading of AMD was done by a single experienced (more than 5 years) vitreoretinal surgeon in accordance with the International ARM Epidemiological Study Group and staged based on the grading in the worst eye.[8]
Anthropometric measurements such as weight (to the nearest 0.5 kg), height, waist, and hip measurements using a nonstretchable measuring tape (to the nearest centimeter) were obtained using standardized techniques. Based on BMI, waist circumference (WC), and WHR, the type of obesities were classified.
Definitions
Early AMD: It is defined as the presence of drusen as discrete whitish-yellow spots located external to the neuroretina or retinal pigmented epithelium (RPE) or the presence of drusen with RPE abnormalities seen as areas of hyperpigmentation or hypopigmentation[8]
Late AMD: (a) Dry AMD: It is defined as the presence of geographic atrophy of the RPE in the absence of neovascularization. (b) Wet AMD: It is defined as the presence of RPE detachments, which may be associated with neurosensory retinal detachment, sub-RPE or subretinal neovascular membranes, and subpigment epithelial, subretinal, or intraretinal scar or glial tissue. Fibrin-like deposits and subretinal hemorrhages might be present which will not be related to other retinal vascular diseases[8]
BMI: It is calculated using the following formula: weight (in kg)/height (in m2)
WC and hip circumference: The WC is the measurement of smallest horizontal circumference between the costal margins and the iliac crests at minimal respiration. And the greatest circumference, widest protrusion of the hip, was measured as hip girth
WHR: It is calculated by dividing the WC (in cm) by the hip circumference (in cm)
Obesity: According to the World Health Organization Expert Consultation guidelines, obesity is defined based on BMI alone (BMI ≥23 kg/m2), WC alone (men ≥90 cm and women ≥80 cm), and WHR alone (men ≥0.90 and women ≥0.85)[9,10]
Isolated generalized obesity: It is defined as increased BMI with normal WC (BMI ≥23 kg/m2 and WC in men <90 cm and women <80 cm)
Isolated abdominal obesity: It is defined as increased WC with normal BMI (WC in men ≥90 cm and women ≥80 cm and BMI ≤23 kg/m2)
Combined obesity: It is defined as both increased WC and BMI (BMI ≥23 kg/m2 and WC in men ≥90 cm and women ≥80 cm).
Statistical analysis
Statistical analyses were carried out using SPSS statistical software for Windows, Version 21.0 (IBM Corp, Released 2013, Armonk, NY, USA) and Microsoft Excel 2013 (Microsoft Corp, Redmond, WA, USA). For the categorical variables, Chi-square test and logistic regression analysis with step-wise forward method were used to find the association between AMD and obesity. For continuous variables, to compare difference between independent groups, Student's t-test for parametric data and Mann–Whitney U-test for nonparametric data were done. P < 0.05 was considered statistically significant.
Results
Table 1a and b shows the demographic and baseline characteristics of both AMD and normal population. In Table 1a, the overall parameters of AMD population and normal population were compared. Statistically significant difference was noted between AMD and normal populations in parameters such as age, BMI in kg/m2, hip and WC in centimeter, proportion of smoking, tobacco and alcohol consumption, diabetes, hypertension, and obesity indices such as obesity based on BMI, WC, and combined obesity. In Table 1b, the parameters of both the groups were compared between males and females. Statistically significant difference between males and females was noted in characteristics such as age, BMI in kg/m2, hip circumference in centimeter, WHR, the proportion of smoking, alcohol consumption, hypertension, and all obesity indices with P < 0.05 in both the groups. The proportion of obesity indices was comparable between AMD and normal population.
Table 1a.
Baseline characteristics of the study population (overall)
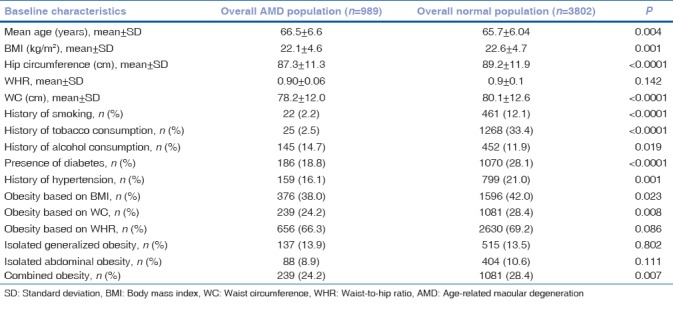
Table 1b.
Baseline characteristics of the study population (male vs. female)
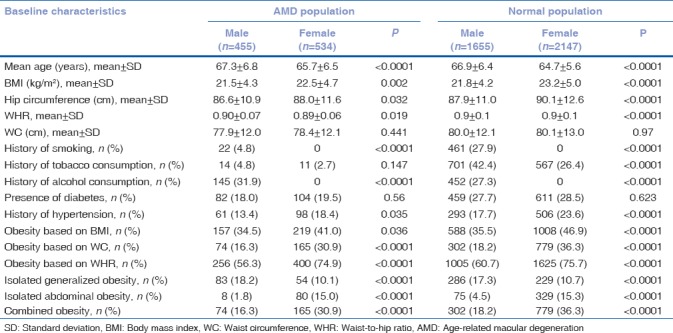
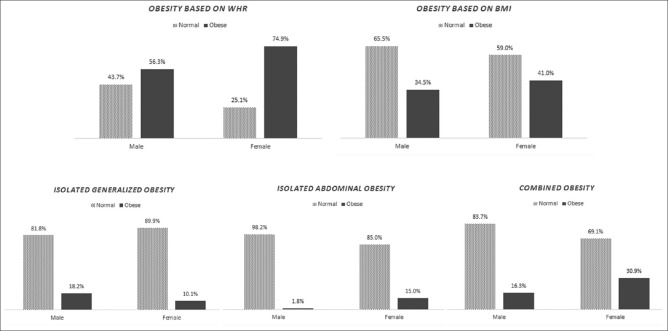
Fig. 1 shows the graphical representation of prevalence of various obesity indices in AMD population. In our study population, the prevalence of obesity based on WHR was more compared to normal, whereas the prevalence of obesity based on BMI, isolated generalized obesity, isolated abdominal obesity, and combined obesity was less compared to normal proportion in each group.
Figure 1.
Prevalence of obesity indices in age-related macular degeneration and normal populations (over 60 years of age)
Binary logistic regression analysis was done to obtain the odds ratio (OR) and P value and to find any association of obesity with various types of obesity. The results are summarized in Table 2a. A total of 4791 patients for whom AMD was gradable were included in this analysis. Out of 4791, 3802 patients had no AMD and 989 patients had either early or late stage of AMD. No statistically significant association was noted between the presence of AMD and any obesity indices. A subanalysis was done to find if the stage of AMD was associated with either of the obesity indices, in overall population and in each gender. Table 2b shows the proportions of patients in each obesity index and their comparison between early AMD and late AMD. No significant associations were noted. The ORs were adjusted for age, diabetes status, smoking status, socioeconomic score, systolic blood pressure, and diastolic blood pressure.
Table 2a.
Association of age-related macular degeneration and various types of obesity
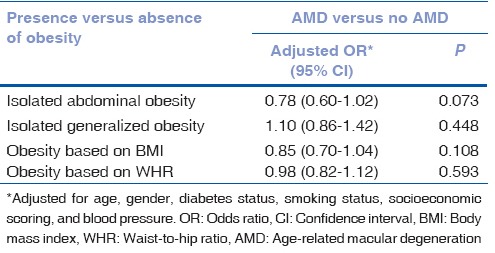
Table 2b.
Subanalysis of association between stages of age-related macular degeneration and obesity indices in men and women
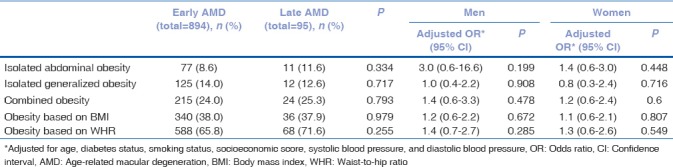
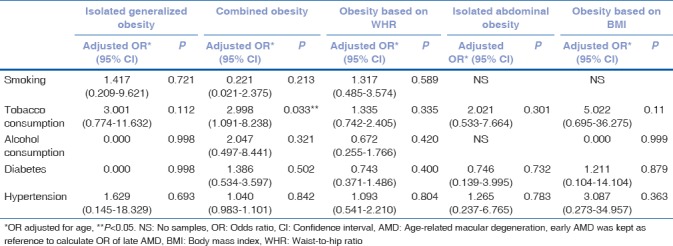
Table 3 shows the combined association of stage of AMD with various obesity indices and risk factors, adjusting for age. The risk factors such as smoking, alcohol and tobacco consumption, diabetes, and hypertension were compared with the stage of AMD (early and late) in the population with each obesity indices. Consumption of tobacco was significantly associated with late AMD in the population with combined obesity, with P = 0.033 and OR being 2.998 (1.091–8.238). No significant association was noted for other risk factors.
Table 3.
Association between obesity indices, risk factors, and age-related macular degeneration
Discussion
This study estimates the prevalence of various obesity indices in AMD patients and its association with severity and risk factors of AMD. The prevalence of obesity was more in women when compared to men, which was statistically significant. No significant association was noted between any obesity indices and presence or severity of AMD.
Association of AMD with obesity indices such as obesity based on BMI, WC, WHR, isolated generalized obesity, isolated abdominal obesity, and combined obesity was evaluated in our study. Previous studies had shown that the correlation of various obesity indices does not have a linear relationship. It was found that the correlation of BMI and central obesity varies from one individual to another. Age and gender have an influence on various obesity indices. Hence, we studied the association of AMD with possible obesity indices.
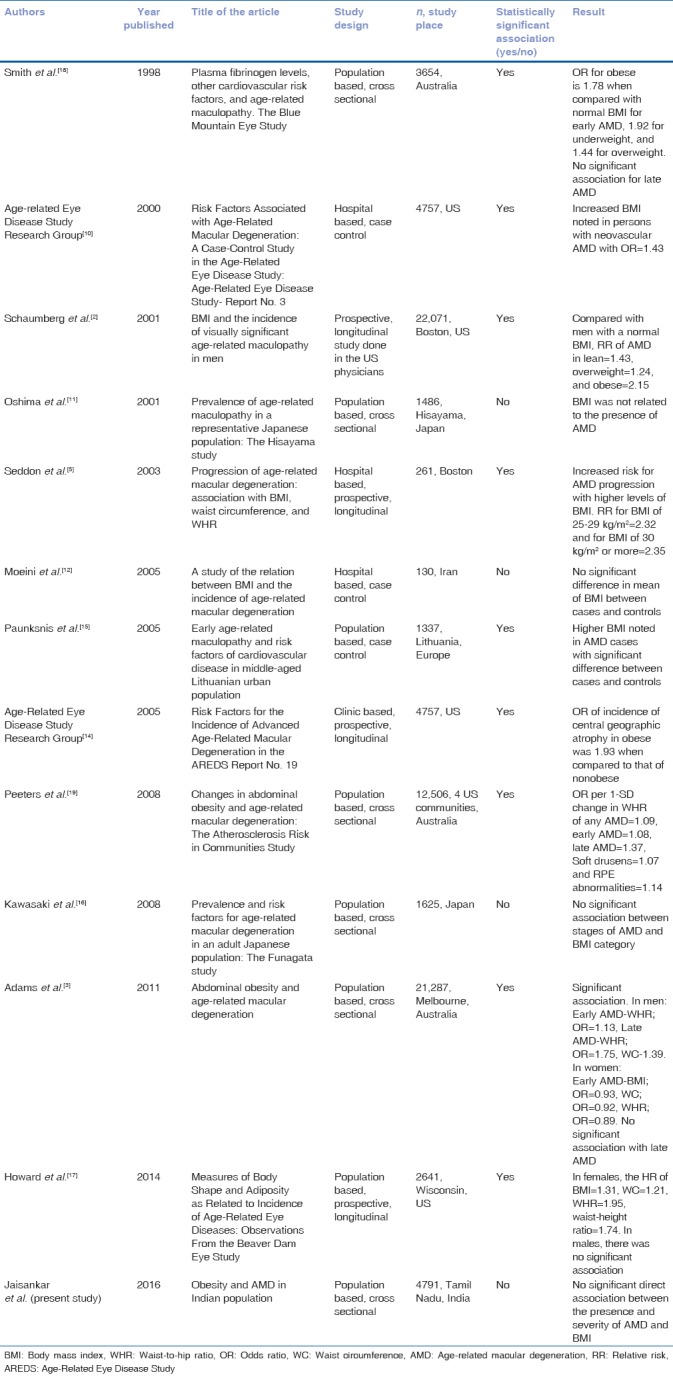
In our study, we adjusted for age, gender, smoking status, socioeconomic scoring, diabetes status, and blood pressure to find an association between the presence of various obesity indices and presence and severity of AMD. No statistically significant direct association was noted. Similar to our study, few case–control and cross-sectional studies had reported that there was no significant association between obesity and AMD.[11,12,13] However, many case–control or longitudinal studies[2,5,14,15,16,17] and few cross-sectional studies[3,13,18] had shown a significant association between AMD and either one of the obesity indices. Table 4 shows the summary of previous studies done to determine the association between AMD and obesity.
Table 4.
Summary on studies on association of obesity indices and age-related macular degeneration
Zhang et al.[1] did a meta-analysis of prospective studies on the association of obesity and AMD. They concluded that excess body weight may act as a potential risk factor for AMD incidence. They postulated from the previous studies that the secretion of pro-inflammatory messengers, such as monocyte chemoattractant protein-1 and tumor necrosis factor-α, was significantly elevated in obese individuals. The migration and infiltration of monocyte could be regulated by these pro-inflammatory factors, causing a disturbance in the function of the RPE which might contribute to retinal changes encountered in AMD.[19,20] They had also described that increased adiposity on the distribution of macular carotenoids may partly be related to increased risk of AMD in obese individuals.[21]
We did not find any association with risk factors such as smoking and alcohol consumption. Previous studies[22,23,24,25,26] had shown smoking to be a well-known risk factor for AMD progression. Smoking is known to affect the circulation of antioxidants. This leads to decrease in the levels of compounds with antioxidant capabilities in the body, thereby the protection of retina against oxidative damage is perturbed.[14] Severity of AMD was significantly associated with consumption of tobacco in the population with combined obesity. This infers that combined obesity is indirectly associated with AMD in addition to tobacco consumption. However, this study being a cross-sectional study, we could not find the relative risk of smoking and alcohol, which could be established well with a longitudinal study by assessing the progression of AMD in groups with and without risk factors.
We did not find any significant association of AMD with systemic diseases such as diabetes mellitus and hypertension. Increase in the risk of AMD progression with the presence of diabetes mellitus and hypertension in obesity category was reported in previous studies.[5,19,27]
The novelty of the study is its design being population based which included both urban and rural populations of India over 60 years of age with large sample size. However, there are few limitations: (1) This being a cross-sectional study, the relative risk of AMD progression with the presence of obesity and other risk factors could not be assessed. This study restricted to measuring the occurrence rather than incidence of AMD. (2) Patients in early stage are usually asymptomatic and it is not easy to distinguish them only by routine ophthalmic examination. Thus, the true association of early AMD is more likely to be underestimated; however, to overcome this, we have highlighted both early and late AMD. (3) A higher level of BMI tends to be associated with other unhealthy behaviors, such as lower levels of physical activity, lower vegetable consumption, and higher alcohol consumption. Hence, it could be a confounding factor. However, these confounders could not be tested due to nonavailability of the data.
Conclusion
In the Indian population, presence or severity of AMD did not seem to directly relate to any of the obesity indices. However, there is an association between severity of AMD and consumption of tobacco in population with combined obesity. AMD, being a multifactorial etiology, should be more carefully studied with a longitudinal study with a similar design for prevention of its progression by altering the lifestyle-related risk factors.
Financial support and sponsorship
This work was funded by Jamshetji Tata trust, Mumbai.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Zhang QY, Tie LJ, Wu SS, Lv PL, Huang HW, Wang WQ, et al. Overweight, obesity, and risk of age-related macular degeneration. Invest Ophthalmol Vis Sci. 2016;57:1276–83. doi: 10.1167/iovs.15-18637. [DOI] [PubMed] [Google Scholar]
- 2.Schaumberg DA, Christen WG, Hankinson SE, Glynn RJ. Body mass index and the incidence of visually significant age-related maculopathy in men. Arch Ophthalmol. 2001;119:1259–65. doi: 10.1001/archopht.119.9.1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Adams MK, Simpson JA, Aung KZ, Makeyeva GA, Giles GG, English DR, et al. Abdominal obesity and age-related macular degeneration. Am J Epidemiol. 2011;173:1246–55. doi: 10.1093/aje/kwr005. [DOI] [PubMed] [Google Scholar]
- 4.Klein BE, Klein R, Lee KE, Jensen SC. Measures of obesity and age-related eye diseases. Ophthalmic Epidemiol. 2001;8:251–62. doi: 10.1076/opep.8.4.251.1612. [DOI] [PubMed] [Google Scholar]
- 5.Seddon JM, Cote J, Davis N, Rosner B. Progression of age-related macular degeneration: Association with body mass index, waist circumference, and waist-hip ratio. Arch Ophthalmol. 2003;121:785–92. doi: 10.1001/archopht.121.6.785. [DOI] [PubMed] [Google Scholar]
- 6.Després JP, Lemieux I. Abdominal obesity and metabolic syndrome. Nature. 2006;444:881–7. doi: 10.1038/nature05488. [DOI] [PubMed] [Google Scholar]
- 7.Raman R, Pal SS, Ganesan S, Gella L, Vaitheeswaran K, Sharma T, et al. The prevalence and risk factors for age-related macular degeneration in rural-urban India, Sankara Nethralaya rural-urban age-related macular degeneration study, report no 1. Eye (Lond) 2016;30:688–97. doi: 10.1038/eye.2016.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bird AC, Bressler NM, Bressler SB, Chisholm IH, Coscas G, Davis MD, et al. An international classification and grading system for age-related maculopathy and age-related macular degeneration. The International ARM Epidemiological Study Group. Surv Ophthalmol. 1995;39:367–74. doi: 10.1016/s0039-6257(05)80092-x. [DOI] [PubMed] [Google Scholar]
- 9.WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 10.World Health Organization. Melbourne: International Diabetes Institute; 2000. The Asia Pacific Perspective, Redefining Obesity and its Treatment: International Association for the Study of Obesity and International Obesity Task Force. [Google Scholar]
- 11.Oshima Y, Ishibashi T, Murata T, Tahara Y, Kiyohara Y, Kubota T, et al. Prevalence of age related maculopathy in a representative Japanese population: The Hisayama study. Br J Ophthalmol. 2001;85:1153–7. doi: 10.1136/bjo.85.10.1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moeini HA, Masoudpour H, Ghanbari H. A study of the relation between body mass index and the incidence of age related macular degeneration. Br J Ophthalmol. 2005;89:964–6. doi: 10.1136/bjo.2005.066241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kawasaki R, Wang JJ, Ji GJ, Taylor B, Oizumi T, Daimon M, et al. Prevalence and risk factors for age-related macular degeneration in an adult Japanese population: The Funagata study. Ophthalmology. 2008;115:1376–81. doi: 10.1016/j.ophtha.2007.11.015. 1381.e1-2. [DOI] [PubMed] [Google Scholar]
- 14.Age-Related Eye Disease Study Research Group. Risk factors associated with age-related macular degeneration. A case-control study in the age-related eye disease study: Age-related eye disease study report number 3. Ophthalmology. 2000;107:2224–32. doi: 10.1016/s0161-6420(00)00409-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Paunksnis A, Cimbalas A, Cerniauskiene LR, Luksiene DI, Margeviciene L, Domarkiene S, et al. Early age-related maculopathy and risk factors of cardiovascular disease in middle-aged Lithuanian urban population. Eur J Ophthalmol. 2005;15:255–62. doi: 10.1177/112067210501500213. [DOI] [PubMed] [Google Scholar]
- 16.Clemons TE, Milton RC, Klein R, Seddon JM, Ferris FL, 3rd Age-Related Eye Disease Study Research Group. Risk factors for the incidence of advanced age-related macular degeneration in the age-related eye disease study (AREDS) AREDS report no 19. Ophthalmology. 2005;112:533–9. doi: 10.1016/j.ophtha.2004.10.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Howard KP, Klein BE, Lee KE, Klein R. Measures of body shape and adiposity as related to incidence of age-related eye diseases: Observations from the beaver dam eye study. Invest Ophthalmol Vis Sci. 2014;55:2592–8. doi: 10.1167/iovs.13-13763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smith W, Mitchell P, Leeder SR, Wang JJ. Plasma fibrinogen levels, other cardiovascular risk factors, and age-related maculopathy: The Blue Mountains Eye Study. Arch Ophthalmol. 1998;116:583–7. doi: 10.1001/archopht.116.5.583. [DOI] [PubMed] [Google Scholar]
- 19.Peeters A, Magliano DJ, Stevens J, Duncan BB, Klein R, Wong TY, et al. Changes in abdominal obesity and age-related macular degeneration: The atherosclerosis risk in communities study. Arch Ophthalmol. 2008;126:1554–60. doi: 10.1001/archopht.126.11.1554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Charo IF, Taubman MB. Chemokines in the pathogenesis of vascular disease. Circ Res. 2004;95:858–66. doi: 10.1161/01.RES.0000146672.10582.17. [DOI] [PubMed] [Google Scholar]
- 21.Age-Related Eye Disease Study 2 Research Group. Lutein+zeaxanthin and omega-3 fatty acids for age-related macular degeneration: The age-related eye disease study 2 (AREDS2) randomized clinical trial. JAMA. 2013;309:2005–15. doi: 10.1001/jama.2013.4997. [DOI] [PubMed] [Google Scholar]
- 22.Smith W, Assink J, Klein R, Mitchell P, Klaver CC, Klein BE, et al. Risk factors for age-related macular degeneration: Pooled findings from three continents. Ophthalmology. 2001;108:697–704. doi: 10.1016/s0161-6420(00)00580-7. [DOI] [PubMed] [Google Scholar]
- 23.Klein R, Cruickshanks KJ, Nash SD, Krantz EM, Nieto FJ, Huang GH, et al. The prevalence of age-related macular degeneration and associated risk factors. Arch Ophthalmol. 2010;128:750–8. doi: 10.1001/archophthalmol.2010.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Connell PP, Keane PA, O’Neill EC, Altaie RW, Loane E, Neelam K, et al. Risk factors for age-related maculopathy. J Ophthalmol 2009. 2009;360764 doi: 10.1155/2009/360764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Christen WG, Glynn RJ, Manson JE, Ajani UA, Buring JE. A prospective study of cigarette smoking and risk of age-related macular degeneration in men. JAMA. 1996;276:1147–51. [PubMed] [Google Scholar]
- 26.Seddon JM, Willett WC, Speizer FE, Hankinson SE. A prospective study of cigarette smoking and age-related macular degeneration in women. JAMA. 1996;276:1141–6. [PubMed] [Google Scholar]
- 27.Hogg RE, Woodside JV, Gilchrist SE, Graydon R, Fletcher AE, Chan W, et al. Cardiovascular disease and hypertension are strong risk factors for choroidal neovascularization. Ophthalmology. 2008;115:1046–52. doi: 10.1016/j.ophtha.2007.07.031. [DOI] [PubMed] [Google Scholar]