Abstract
Background
Trait and automatic approach‐avoidance (AA) tendencies are central concepts in research on affective disorders. We longitudinally examined the associations of trait and automatic AA tendencies with the risk of onset and chronicity of anxiety and depressive disorders.
Methods
Participants were subdivided into those with (n = 766) versus without (n = 1,636) a current anxiety or depression diagnosis at baseline. Clinical diagnoses were reassessed after 2‐year follow‐up. Automatic AA tendencies in reaction to facial expressions were assessed using the Approach‐Avoidance Task, whereas self‐reported trait AA tendencies were assessed using the Behavioral Inhibition System and the Behavioral Activation System scales. Analyses were adjusted for socio‐demographics (basic adjustment) and for severity and history of psychopathology (full adjustment).
Results
Stronger trait avoidance tendencies predicted both increased risk of onset and increased risk of a chronic course of anxiety disorders after full adjustment (Odds ratioonset = 1.55, P < .001, and Odds ratiochronicity = 1.31, P = .03). The associations between stronger trait avoidance tendencies and increased risk of onset and chronicity of depressive disorders were no longer significant after full adjustment. In contrast, trait approach tendencies and automatic AA tendencies were not related to onset or chronicity of disorders.
Conclusions
Increased trait avoidance tendencies are a risk factor for affective disorders in general, with possibly a slightly more pronounced role in anxiety than depressive disorders. This underlines the importance of addressing trait avoidance tendencies in both the treatment and aftercare of affective disorders.
Keywords: AAT, activation, behavior, BIS/BAS, inhibition, motivation
1. INTRODUCTION
Affective disorders cause a major burden for societies worldwide and this is projected to worsen over time (World Health Organization, 2008). Global scientific efforts directed at alleviating some of this burden are influenced by current classification schemes of mental disorders that are largely related to historical propositions (Cuthbert & Insel, 2013). This is the main reason for the National Institute of Mental Health to develop and maintain the Research Domain Criteria initiative (RDoC), which strives to incorporate genetics, imaging, cognitive science, and other levels of information to lay the foundation for a new mental disorders classification system. Two of the five core dimensions that form the centerpiece of the RDoC are negative valence systems (systems primarily responsible for responses to aversive situations or contexts, such as fear, anxiety, and loss) and positive valence systems (systems primarily responsible for responses to positive motivational situations or contexts, such as reward seeking, consummatory behavior, and reward/habit learning). These dimensions can be measured on a trait behavioral level (e.g., by means of the Behavioral Inhibition System and the Behavioral Activation System (BIS/BAS) questionnaire) and on an automatic behavioral level (e.g., by means of the Approach‐Avoidance Task (AAT)).
The BIS/BAS questionnaires are constructed to measure two broadband motivational systems, the Behavioral Inhibition System and the Behavioral Activation System (BIS/BAS), which play a central role in several neuropsychological models of emotion and emotional disorders (Carver & White, 1994). An overly sensitive BIS causes increased attention to threat, increased negative affect, and behavioral inhibition, whereas an unresponsive BAS leads to a lack of positive experiences and positive affect through decreased behavioral activation, both of which are possible pathways for the development of psychopathology. Studies using a cross‐sectional research design most often find a positive association between BIS scores and depression, as well as between BIS scores and anxiety, and a negative association between BAS scores and depression (Beevers & Meyer, 2002; Campbell‐Sills, Liverant, & Brown, 2004; Fullana et al., 2004; Hundt, Nelson‐Gray, Kimbrel, Mitchell, & Kwapil, 2007; Johnson, Turner, & Iwata, 2003; Jones & Day, 2008; Jorm et al., 1999; Kimbrel, Mitchell, & Nelson‐Gray, 2010; Kimbrel, Nelson‐Gray, & Mitchell, 2007; Pinto‐Meza et al., 2006; Segarra et al., 2007). Longitudinal studies exploring these associations are sparse and found that low BAS scores are related to worse outcomes in depressed patients (Kasch, Rottenberg, Arnow, & Gotlib, 2002; McFarland, Shankman, Tenke, Bruder, & Klein, 2006) and that high BIS scores are related to less improvement in patients with affective disorders (Brown, 2007).
In recent years, new tasks have been developed to assess people's approach‐avoidance (AA) tendencies directly without the need for self‐report. For example, the AAT was designed as a measure of automatic AA tendencies in reaction to disorder‐relevant stimuli such as spiders, alcoholic beverages, or emotional faces (Rinck & Becker, 2007). The AAT is a computerized task in which participants respond to pictures presented on a screen by either pulling or pushing a joystick, often by responding to an irrelevant feature of the picture, such as the color of the picture filter (i.e., implicit AAT). Cross‐sectional associations of AAT outcomes and affective disorders in previous research provide mixed results and a recent study showed no relation between automatic AA tendencies and affective disorders in a large naturalistic sample encompassing healthy as well as depressed and anxious individuals (Struijs et al., 2017). To date, there are no longitudinal studies examining the associations between AAT outcomes and affective disorders.
Previous studies of motivational behavior in relation to affective disorders are limited by methodological shortcomings. Many used small, non‐clinical samples without a control group, focused on either depression or anxiety, used either trait or automatic measures as predictive variables, were mostly cross‐sectional in nature, and did not take into account the possible difference between the onset and the course of psychopathology. In order to address these shortcomings, the current study sought to examine prospectively whether trait and automatic AA tendencies can predict the onset and chronicity of affective disorders in a large group of participants with and without a current affective disorder, using a 2‐year longitudinal design.
2. METHODS
2.1. Study design and sample
Data were derived from the 4‐year and 6‐year follow‐up assessment of the Netherlands Study of Depression and Anxiety (NESDA), an ongoing longitudinal cohort study designed to study the long‐term antecedents, course, and consequences of depression and anxiety. Subjects with current or remitted depressive or anxiety disorders as well as healthy controls were included in the study at the first assessment (N = 2981). Participants were recruited from three different settings: the community, primary care, and mental health care in order to reflect the entire, wide range of psychopathology. A detailed description of the NESDA design and sampling procedure is provided elsewhere (Penninx et al., 2008).
Recruitment used the following inclusion and exclusion criteria: an age of 18 through 65 years, proficiency in the Dutch language, and no diagnosis of a psychotic disorder, obsessive compulsive disorder, bipolar disorder, or severe addiction disorder. The study protocol was approved by the ethical review board of each participating center. All participants signed written informed consent before participating in the study. The 4‐year assessment started in September 2008 and ended in February 2011. The 6‐year assessment started in September 2010 and ended in February 2013. For the sake of simplicity, the 4‐year and 6‐year assessments will be referred to as “baseline” and “follow‐up” respectively throughout the rest of the paper.
Baseline assessment was completed by 2,402 participants. Two thousand and one hundred sixty‐seven participants completed both assessments, which means that 235 (9.7%) were lost to follow‐up. Due to various reasons (for specification see the AAT sections below), information on 295 additional participants was missing on the AAT. Since missing data results in loss of power and often introduces bias because of selective response, multiple imputation (MI) was performed. With the SPSS MI option, 100 imputed data sets were generated, using the fully conditional specification method. The imputation model included all variables included in the analyses and variables associated with attrition (ancestry and sampling location; Lamers et al., 2012). Results from the analyses of the 100 imputed datasets were pooled, correcting the standard errors of the regression coefficients for within‐imputation variability and between‐imputation variability (Rubin, 1987). Using this method, the full baseline sample of 2402 participants could be retained.
3. MEASURES
3.1. Psychopathology
Depressive (major depressive disorder (MDD) or dysthymia (Dys)) and anxiety disorders (panic disorder (PD), social anxiety disorder (SAD), generalized anxiety disorder (GAD), agoraphobia (Ago)) were assessed by means of the lifetime Composite International Diagnostic Interview (Wittchen, 1994) at baseline and follow‐up. Participants who met the requirements for a diagnosis in the past 6 months at baseline were classified “current” and divided into “current anxiety” and “current depression.” Participants who met the requirements for both a depressive disorder and an anxiety disorder were included in both groups. Earlier history of a depressive or anxiety disorder was determined, and considered a covariate for analyses. Depressive symptom severity was measured via the 30‐item Inventory of Depressive Symptomatology (IDS) (Rush, Gullion, Basco, & Jarrett, 1996) and anxiety symptom severity was measured via the 21‐item Beck's Anxiety Inventory (BAI) (Beck, Brown, Epstein, & Steer, 1988).
3.2. Trait approach‐avoidance tendencies
Trait AA tendencies were measured by two subscales of the BIS/BAS (Carver & White, 1994). The questionnaire consists of 11 questions that measure two different traits. The BIS subscale consists of seven questions using a four‐point scale (1 = strongly agree to 4 = strongly disagree), which measures responsiveness to punishment cues (i.e., behavioral inhibition sensitivity). The BAS‐drive subscale consists of four questions using a four‐point scale (1 = strongly agree to 4 = strongly disagree), which measures motivation to engage in approach behavior in the context of potential reward (i.e., behavioral activation sensitivity). The BIS and BAS measures were reverse coded so that a higher score reflects stronger trait avoidance and trait approach tendencies, respectively. Both the BIS and BAS‐drive scales were found to have good reliability and validity ratings (Caseras, Avila, & Torrubia, 2003).
3.3. Automatic approach‐avoidance tendencies
At the baseline assessment, the AAT was used as an automatic measure of AA behavior (for details about the AAT that was used in the current study also see: Struijs et al., 2017). The AAT is a computerized speeded reaction time (RT) task (Heuer, Rinck, & Becker, 2007), in which participants were instructed to respond as quickly as possible to pictures of faces which are presented in a random order. The behavioral responses on the AAT are sufficiently reliable and valid to be used in the assessment of group differences (Reinecke, Becker, & Rinck, 2010). We earlier demonstrated reasonable internal consistency of the AAT in the current sample with Cronbach's alpha values ranging between .79 (pushing happy faces) and .82 (pushing neutral faces) separately for each condition (Struijs et al., 2017). Face stimuli were selected from the Karolinska Directed Emotional Faces database (Lundqvist, Flykt, & Öhman, 1998). For this study we focused on facial stimuli that are most often used in previous clinical AAT studies. Angry, happy, and neutral facial expressions were taken from the same model. The pictures can be pushed away or pulled closer by means of a joystick. They respectively enlarge or shrink to create the experience of either approaching or avoiding the face in the picture (zooming effect). This measure is preferred as outcome measure because the zooming effect can be taken into account, which increases the likelihood of assessing an automatic effect of emotional valence on AA behavior (Phaf, Mohr, Rotteveel, & Wicherts, 2014). Participants were asked to respond to a task‐relevant stimulus, in this case the color of the picture filter (yellow or gray), by either pushing or pulling the joystick as quickly as possible. Participants were presented with 20 practice trials before the actual test of 60 trials. The RTs from onset of the picture (after participants push the fire button of the joystick) to picture disappearance (when the joystick is moved at a 30 degree angle from the upright position) were measured. Not all participants were able or willing to visit the research center, so their interviews were conducted at home or by telephone, which did not include the AAT. One thousand nine hundred and seventy‐one participants completed the AAT at baseline.
4. DATA ANALYSIS
4.1. Data preparation AAT
The RTs from picture appearance to first movement of the joystick were filtered using a <150 and a >1,500 ms cut‐off, as used by others before (Enter, Colzato, & Roelofs, 2012). For each participant, the median of the remaining RTs (95%) for the correct responses was calculated per condition. Seventy‐six participants were excluded with a high error rate of >20% test trials in any condition. A cut‐off of three standard deviations from the mean in any condition was used for defining outliers in the remaining median RTs, which excluded another 23 participants. This yielded 1,872 participants who had complete AAT data at baseline. Assumptions of ANCOVA were met since all variables were normally distributed and showed equality of (co)variance. AAT‐effect scores were calculated by subtracting the median pull RT from the corresponding median push RT for each participant and facial expression. As a result, negative scores reflect avoidance behavior, whereas positive scores reflect approach behavior.
4.2. Predicting onset of new depression and anxiety
Within the group of participants without current depression or anxiety at baseline, logistic regression models were performed with new onset of a depressive and/or anxiety disorder, new onset of a depressive disorder, or new onset of an anxiety disorder as outcome measures. New onset was defined as the occurrence of a clinical diagnosis during the 2‐year follow‐up period between baseline and 2‐year assessment. The models were first adjusted for age, gender, and education (basic adjustment), and then additionally adjusted for history of psychopathology and severity of psychopathology at baseline (IDS and BAI; fully adjusted). Age, gender, and education were included in the regression models as covariates because this allows for a better generalizability of our results to the population. Furthermore, severity and history of psychopathology are predictors of a worse course of psychopathology (Penninx et al., 2011) and are correlated with approach and avoidance tendencies. Consequently they could confound our associations and therefore we included them as covariates in the fully adjusted models. Predictor variables of automatic and trait AA tendencies were separately included in the analyses (i.e., one analysis per predicting variable). The same method was used for predicting chronicity of depression and anxiety and also for the dimensional analyses described below.
4.3. Predicting chronicity of depression and anxiety
Analyses were computed in participants who were depressed and/or anxious at baseline (n = 766). Additionally, consistency of results across depression and anxiety was checked by also separately analyzing participants with a depressive disorder at baseline (n = 467) and participants with an anxiety disorder at baseline (n = 545). For these three samples, logistic regression models were constructed with chronicity of depression, chronicity of anxiety, and chronicity of depression and/or anxiety as outcome measures, respectively. Chronicity was defined as the presence of a clinical diagnosis (6‐month recency) at the 2‐year follow‐up assessment. The models were initially adjusted for age, gender, and education, and in addition for severity of psychopathology at baseline.
4.4. Dimensional analyses
In order to assess dose‐response relationships of automatic and trait AA tendencies with baseline to 2‐year follow‐up changes in symptoms of psychopathology in all study participants we used a residualized change approach. First, we regressed the 2‐year follow‐up up IDS and BAI severity scores on their corresponding baseline scores while saving the standardized residuals. Second, two multiple regression models were used with these standardized residuals as outcome variables; sex, age, education, and baseline psychopathology severity as covariates; and BIS/BAS and AAT scores as predicting variables.
5. STATISTICS
Results are based on the multiple imputed dataset (see study design and sample for details). We report odds‐ratios (OR) with corresponding P‐values of all tests. Parameter estimates are reported as betas. All analyses were carried out with SPSS (version 20), and the significance level was set at P < .05.
6. RESULTS
The 2,402 subjects were on average 46 years old, and 66.2% were female. Overall, the participants with a disorder at baseline were more often female and less educated as compared to participants without a disorder at baseline. Also, they displayed more symptoms of depression and anxiety at baseline and follow‐up. Of all participants without a diagnosis at baseline, 304 (18.6%) developed a diagnosis. Of all participants who were depressed or anxious, 476 (62.2%) were still depressed or anxious at follow‐up (Table 1).
Table 1.
Sample characteristics of participants at baseline and 2‐year follow up outcomes as a function of group (n = 2,402)
| Depressed and/or anxious (n = 766) | Not depressed or anxious (n = 1,636) | ||||
|---|---|---|---|---|---|
| Mean | (SD) | Mean | (SD) | P | |
| Age | 46.4 | (12.4) | 45.8 | (13.5) | .30 |
| Female (%) | 69.8 | 64.7 | .01 | ||
| Years of education | 12.2 | (3.4) | 13.1 | (3.2) | <.001 |
| Current depressive disorder (%) | 61.0 | 0 | |||
| Current anxiety disorder (%) | 71.1 | 0 | |||
| Remitted earlier diagnosis (%) | − | 70.9 | |||
| IDS baseline | 26.0 | (12.5) | 10.7 | (8.2) | <.001 |
| BAI baseline | 14.7 | (9.9) | 5.2 | (5.5) | <.001 |
| Neutral AAT | −23.2 | (81.6) | −20.6 | (75.7) | .51 |
| Happy AAT | −16.3 | (84.2) | −11.8 | (81.3) | .29 |
| Angry AAT | −15.7 | (82.3) | −7.9 | (78.3) | .05 |
| BIS | 22.7 | (3.6) | 19.6 | (4.0) | <.001 |
| BAS | 9.3 | (2.8) | 9.6 | (2.8) | .02 |
| Follow‐up outcomes | |||||
| IDS 2‐year follow‐up | 24.3 | (12.7) | 11.7 | (9.3) | <.001 |
| BAI 2‐year follow‐up | 14.3 | (9.8) | 6.4 | (6.5) | <.001 |
| Onset of depression and/or anxiety (%) | − | 18.6 | − | ||
| Chronicity of depression and/or anxiety (%) | 62.2 | − | − | ||
Note. SD, Standard deviation; AAT, Approach‐Avoidance Task; BIS, Behavioral Inhibition Scale; BAS, Behavioral Activation Scale; IDS, Inventory of Depressive Symptomatology; BAI, Beck Anxiety Inventory.
6.1. Onset of depression and anxiety
Logistic regression models predicting new onset of psychopathology indicated that stronger trait avoidance tendencies at baseline predicted an increased risk of developing a diagnosis at follow‐up (Table 2). This effect was consistently noticeable for both depression and anxiety (Depression: OR = 1.73, 95% CI (1.45–2.06), P < .001; Anxiety: OR = 2.13, 95% CI (1.72–2.64), P < .001). The association between trait avoidance tendencies at baseline and depression at follow‐up was no longer significant after full adjustment for possible confounds and symptom severity at baseline (Depression: OR = 1.20, 95% CI (.98–1.47), P = .07). Post‐hoc analyses revealed that the risk of disorder onset increased with higher BIS scores (left panel Figure 1; adjusted OR = 5.97, 95% CI (3.66–9.73), P < .001 for the highest BIS quintile). Also, there was no significant interaction between BIS and a history of diagnosis, indicating that the predictive power of BIS does not vary whether participants had a previous diagnosis or not. Trait approach tendencies and automatic AA tendencies were not related to the onset of disorders.
Table 2.
Associations between automatic and trait approach‐avoidance tendencies at baseline and 2‐year onset of new depressive and/or anxiety disorder episodes among participants without initial diagnosis at baseline
| Basic adjusted analysesa | Fully adjusted analysesb | |||
|---|---|---|---|---|
| OR (95% CI) | P | OR (95% CI) | P | |
| New onset of depression and/or anxiety (n = 1,636, incidence = 304) | ||||
| AAT neutral | .99 (.86–1.14) | .89 | 1.02 (.86–1.22) | .81 |
| AAT angry | 1.00 (.87–1.15) | .97 | 1.01 (.86–1.19) | .89 |
| AAT happy | 1.06 (.92–1.24) | .39 | 1.05 (.86–1.28) | .64 |
| BAS | .98 (.85–1.12) | .73 | 1.05 (.90–1.21) | .55 |
| BIS | 1.88 (1.60–2.20) | <.001 | 1.30 (1.09–1.56) | .004 |
| New onset of depression (n = 1,636, incidence = 216) | ||||
| AAT neutral | .98 (.83–1.15) | .81 | .99 (.84–1.17) | .92 |
| AAT angry | .97 (.82–1.15) | .76 | .97 (.82–1.16) | .74 |
| AAT happy | 1.07 (.88–1.29) | .50 | 1.04 (.86–1.27) | .68 |
| BAS | .99 (.85–1.16) | .88 | 1.05 (.89–1.25) | .56 |
| BIS | 1.73 (1.45–2.06) | <.001 | 1.20 (.98–.1.47) | .07 |
| New onset of anxiety (n = 1,636, incidence = 164) | ||||
| AAT neutral | 1.04 (.87–1.25) | .67 | 1.07 (.89–1.30) | .48 |
| AAT angry | 1.06 (.88–1.26) | .56 | 1.06 (.88–1.28) | .52 |
| AAT happy | 1.16 (.93–1.44) | .18 | 1.15 (.92–1.44) | .23 |
| BAS | .97 (.81–1.16) | .97 | 1.03 (.85–1.24) | .77 |
| BIS | 2.13 (1.72–2.64) | <.001 | 1.55 (1.23–1.96) | <.001 |
Note. Predictors are standardized units of measurement. There is one analysis per row. The total sample size is based on all participants having at least one predicting measure (e.g., BIS, BAS, or AAT‐effect score). AAT, Approach‐Avoidance Task; BAS, Behavioral Activation Scale; BIS, Behavioral Inhibition Scale.
Logistic regression analyses, adjusted for age, gender, and education.
Logistic regression analyses, adjusted for age, gender, education, and severity of psychopathology at baseline.
Figure 1.
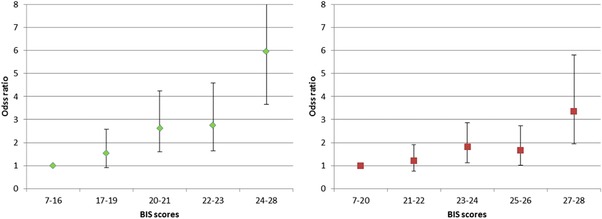
Odds ratios of depression and/or anxiety diagnosis at the 2‐year follow‐up assessment as a function of Behavioral Inhibition Scale scores at baseline
Note. Quintiles of behavioral inhibition at baseline were formed by categorizing Behavioral Inhibition Scale scores. The first quintile is the reference category, with a relative risk of 1. The odds ratios are corrected for age, sex, and education. Left panel depicts depression and/or anxiety onset, n = 607. The right panel depicts depression and/or anxiety chronicity, n = 1,460.
Because of comorbidity (Kessler et al., 2005, Lamers et al., 2011), diagnostic instability within affective disorders (Hovenkamp‐Hermelink et al., 2016; Scholten et al., 2016) and low statistical power when analyzing small subgroups, we decided to group the new onsets of disorders together in our main analysis. However, since a breakdown of this group into the onset of specific disorders might still be informative, we provide the numbers and explorative post‐hoc analyses here. Of all participants without a disorder at baseline, 202 participants developed an MDD, 38 Dys, 55 GAD, 48 SAD, 50 PD, and 33 Ago. BIS significantly predicted the onset of several specific disorders after adjustment for socio‐demographics, severity, and history of psychopathology: Dys (OR = 2.17, P = .002), GAD (OR = 2.06, P < .001), and SAD (OR = 1.96, P = .002). BIS did not significantly predict the onset of MDD (OR = 1.16, P = .16), PD (OR = 1.20, P = .37), and Ago (OR = 1.02, P = .91).
6.2. Chronicity of psychopathology
Logistic regression models predicting the chronicity of psychopathology indicated that stronger trait avoidance tendencies predicted an increased risk of still having a disorder after 2 years, thus, having a chronic course of psychopathology (Table 3). This association was consistently noticeable for both depression and anxiety (Depression: OR = 1.44, 95% CI (1.17–1.77), P = .001; Anxiety: OR = 1.38, 95% CI (1.13–1.67), P = .001). The association between trait avoidance tendencies at baseline and depression at follow‐up was no longer significant after full adjustment for possible confounds and symptom severity at baseline (Depression: OR = 1.23, 95% CI (.99–1.54), P = .09). The odds of chronicity increased with higher BIS scores (right panel Figure 1; adjusted OR = 3.36, 95% CI (1.95–5.80), P < .001 for the highest BIS quintile). Automatic AA tendencies were not related to a chronic course of disorders (Table 3).
Table 3.
Associations between automatic and trait approach‐avoidance tendencies at baseline and 2‐year chronicity of new depressive and/or anxiety disorder episodes among participants with an initial diagnosis at baseline
| Basic adjusted analysesa | Fully adjusted analysesb | |||
|---|---|---|---|---|
| OR (95% CI) | P | OR (95% CI) | P | |
| Chronicity of depression and/or anxiety (n = 766, chronic psychopathology = 476) | ||||
| AAT neutral | .98 (.82–1.17) | .83 | .99 (.82–1.21) | .99 |
| AAT angry | 1.00 (.83–1.19) | .96 | 1.05 (.87–1.26) | .64 |
| AAT happy | 1.01 (.84–1.21) | .91 | 1.01 (.84–1.22) | .90 |
| BAS | 1.00 (.86–1.17) | .97 | 1.01 (.86–1.20) | .88 |
| BIS | 1.44 (1.23–1.69) | <.001 | 1.29 (1.08–1.54) | .005 |
| Chronicity of depression (n = 467, chronic disorder = 236) c | ||||
| AAT neutral | 1.08 (.86–1.35) | .54 | 1.08 (.85–1.37) | .55 |
| AAT angry | 1.07 (.86–1.34) | .54 | 1.09 (.86–1.39) | .49 |
| AAT happy | 1.07 (.86–1.33) | .57 | 1.05 (.84–1.32) | .67 |
| BAS | .83 (.68–1.01) | .07 | .83 (.67–1.03) | .10 |
| BIS | 1.44 (1.17–1.77) | .001 | 1.23 (.99–1.54) | .09 |
| Chronicity of anxiety (n = 545, chronic disorder = 311) d | ||||
| AAT neutral | .93 (.76–1.15) | .52 | .95 (.76–1.17) | .61 |
| AAT angry | .94 (.77–1.16) | .56 | .98 (.79–1.22) | .85 |
| AAT happy | .92 (.74–1.14) | .42 | .92 (.73–1.15) | .45 |
| BAS | 1.10 (.91–1.33) | .32 | 1.11 (.91–1.34) | .31 |
| BIS | 1.38 (1.13–1.67) | .001 | 1.31 (1.07–1.62) | .03 |
Note. Predictors are standardized units of measurement. There is one analysis per row. The total sample size is based on all participants having at least one predicting measure (e.g., BIS, BAS, or AAT‐effect score). AAT, Approach‐Avoidance Task; BAS, Behavioral Activation Scale; BIS, Behavioral Inhibition Scale.
Logistic regression analyses, adjusted for age, gender, and education.
Logistic regression analyses, adjusted for age, gender, education, and severity of psychopathology at baseline.
The continued presence of depression at follow‐up in participants with a depressive disorder at baseline.
The continued presence of anxiety at follow‐up in participants with an anxiety disorder at baseline.
6.3. Dimensional analysis
Stronger trait avoidance tendencies at baseline predicted more symptoms of depression and anxiety at follow‐up (Table 4; β = .05, 95% CI (.01–.09), P = .03, and β = .08, 95% CI (.04–.12), P < .001, respectively). Approach tendencies as well as automatic AA behavior at baseline were not related to changes in symptom severity of depression and anxiety at follow‐up (Table 4).
Table 4.
Multiple regression analyses predicting 2‐year residualized change in IDS scores (left panel) and BAI scores (right panel) (n = 2,402)
| Inventory of Depressive Symptomatology | Beck Anxiety Inventory | |||||
|---|---|---|---|---|---|---|
| β | CI | P | β | CI | P | |
| AAT neutral | −.02 | −.06–.03 | .53 | −.01 | −.06–.04 | .60 |
| AAT angry | −.03 | −.07–.03 | .44 | .01 | −.04–.06 | .71 |
| AAT happy | .03 | −.02–.08 | .25 | .03 | −.02–.08 | .26 |
| BAS | −.03 | −.01–.08 | .10 | −.00 | −.05–.05 | .93 |
| BIS | .05 | .01–.09 | .03 | .08 | .04–.12 | <.001 |
Note. Predictors are standardized units of measurement. There is one analysis per row. AAT, Approach‐Avoidance Task; BAS, Behavioral Activation Scale; BIS, Behavioral Inhibition Scale.
The estimates of the multiple regression analyses are standardized and are corrected for sex, age, and education.
7. DISCUSSION
The current study provides a first examination of longitudinal associations of trait and automatic AA tendencies with onset and course of affective disorders in a large group of participants without or with a current depressive disorder and/or anxiety disorder at baseline, respectively. Stronger trait avoidance tendencies predicted both increased risk of onset and increased risk of a chronic course of anxiety disorders after full adjustment. The associations between stronger trait avoidance tendencies and increased risk of onset and chronicity of depressive disorders were no longer significant after full adjustment. We found no predictive power of trait approach and automatic AA tendencies for the onset and course of psychopathology.
7.1. Motivation and onset of depression and anxiety
For healthy persons at baseline, increased trait avoidance tendencies predicted the onset of an affective disorder during the following 2 years. This effect was no longer significant for depressive disorders after full adjustment. Also, stronger trait avoidance tendencies predicted more severe symptoms of depression and anxiety over time. Previous research regarding motivation and affective disorders is mostly cross‐sectional in nature, and most often report on self‐reported symptoms that may not necessarily extend to psychiatric disorders. The majority of those studies conclude that increased trait avoidance tendencies are associated with more symptoms of depression (Hundt et al., 2007; Jones & Day, 2008; Pinto‐Meza et al., 2006), anxiety (Fullana et al., 2004; Kimbrel et al., 2010), or both (Beevers & Meyer, 2002; Campbell‐Sills et al., 2004; Coplan, Wilson, Frohlick, & Zelenski, 2006; Johnson, Turner, & Iwata, 2003; Jorm et al., 1999; Kimbrel, Nelson‐Gray, & Mitchell, 2007; Muris, Meesters, de Kanter, & Timmerman, 2005; Segarra et al., 2007; Van Meter & Youngstrom, 2015). There are some studies that examined the relationship of trait approach and avoidance tendencies with the development of depression and anxiety symptoms in undiagnosed students and school children (Li, Xu, & Chen, 2015; Sportel, Nauta, de Hullu, & de Jong, 2013; Takahashi, Roberts, Yamagata, & Kijima, 2015). In these samples, increased trait avoidance tendencies predicted general symptoms of distress, and decreased trait approach tendencies predicted symptoms of depression (Takahashi et al., 2015). However, these associations were diminished in two studies when controlling for baseline severity of symptoms (Li et al., 2015; Sportel et al., 2013). Whether trait avoidance tendencies are predictive of affective disorders in adults that are not currently diagnosed has not been examined before. Our findings emphasize the importance of raising awareness of these tendencies in both depression and anxiety aftercare as well as during preventive healthcare. It will be beneficial for persons at risk to enlist strategies that continuously counter their overall tendency to avoid possible negative outcomes.
In previous cross‐sectional research, decreased trait approach tendencies were associated mostly with more severe symptoms of depression (Beevers & Meyer, 2002; Campbell‐Sills et al., 2004; Hundt et al., 2007; Pinto‐Meza et al., 2006), but also with more severe symptoms of anxiety (Kimbrel et al., 2010) or both (Coplan et al., 2006). Whether trait approach tendencies are predictive of onset of affective disorders has not been examined before. We found that trait approach tendencies were not associated with the risk of developing a new disorder during the following 2 years. Trait approach tendencies were not associated with the development of symptoms of depression and anxiety either. This could imply that the previous positive cross‐sectional findings are (at least in part) due to state effects of depression and/or anxiety. However, trait approach tendencies can be seen as a stable construct (Brown, 2007), which contradicts this hypothesis.
7.2. Motivation and chronicity of depression and anxiety
For participants with a diagnosis at baseline, trait avoidance tendencies predicted the chronicity of an affective disorder diagnosis 2 years later. This result resembles that of Brown (Brown, 2007), who showed that increased trait avoidance tendencies were predictive of a worse outcome in affective disorder psychopathology over the course of 2 years. This implies that overall threat‐avoidance might indeed be an important feature in affective disorders, predicting disorder chronicity. As such, clinicians should address not only specific sets of avoidance behavior, but also the general tendency to avoid negative outcomes, in their treatment of affective disorders.
7.3. Automatic approach‐avoidance behavior and the course of depression and anxiety
We found no predictive value of automatic AA tendencies for the onset and course of psychopathology. Cross‐sectional associations of AAT outcomes and affective disorders in previous research provide mixed results. In our recent study, we could not show a cross‐sectional relation between automatic AA tendencies and affective disorders in our large naturalistic sample encompassing healthy as well as depressed and anxious individuals either (Struijs et al., 2017). The current findings corroborate the notion that, as of yet, the predictive value of the AAT using emotional facial expressions is not established. However, note that in addictions, the AAT does have predictive value (Cousijn, Goudriaan, & Wiers, 2011).
8. STRENGTHS AND LIMITATIONS
The present study has several strengths and limitations. Strengths include the large sample, with longitudinal design and measuring both depressive and anxiety symptoms as well as disorders using psychiatric criteria. Also, dispositional and automatic AA tendencies were assessed using different methodologies. The BIS/BAS questionnaire measures trait like tendencies by means of self‐report, whereas the AAT is a state measure using RTs of behavioral responses. It is important to note that because of these different characteristics the AAT is inherently a less stable measure and therefore a less reliable predictor. Limitations include the compilation of participants with different anxiety disorders into one group. This was necessary because, partly due to high comorbidity across anxiety disorders (Lamers et al., 2011; Scholten et al., 2016), there were not enough patients per single anxiety disorder diagnosis (e.g., pure GAD) to allow for separate analyses. Also, the study sample used in the onset analyses is over‐inclusive of participants with a remitted diagnosis, which can hamper generalizability of the study results to the general population. It must be noted, however, that the predictive value of trait avoidance tendencies was not significantly different in participants with versus without a history of previous diagnoses. Lastly, multiple hypothesis‐testing could be an issue for some of our findings that are relatively weak (P > .01), and thus require replication. However, since the significant associations are all related to BIS, which is significantly associated across multiple outcomes, we are fairly confident that the findings are not due to chance.
9. CONCLUSION
Trait measures of AA tendencies provide evidence that threat‐avoidance is an important feature in affective disorders, predicting disorder onset and chronicity even after controlling for socio‐demographic variables. It underlines the importance of addressing trait avoidance tendencies in the treatment of affective disorders.
CONFLICT OF INTEREST
All authors declare that they have nothing to disclose.
ACKNOWLEDGMENTS
We thank Dr. Sarah Hiles for proofreading the article. The infrastructure for the NESDA study (http://www.nesda.nl) is funded through the Geestkracht program of the Netherlands Organisation for Health Research and Development (Zon‐Mw, grant number 10‐000‐1002) and is supported by participating universities and mental health care organizations (VU University Medical Center, GGZ inGeest, Arkin, Leiden University Medical Center, GGZ Rivierduinen, University Medical Center Groningen, Lentis, GGZ Friesland, GGZ Drenthe, Scientific Institute for Quality of Healthcare (IQ healthcare), Netherlands Institute for Health Services Research (NIVEL), and Netherlands Institute of Mental Health and Addiction (Trimbos Institute)). BP has received funding—not related to this work—from Jansen Research and Boehringer Ingelheim. FL has received funding from the European Union Seventh Framework Programme (FP7/2007‐2013) under grant agreement n° PCIG12‐GA‐2012‐334065.
CONTRIBUTORS
Author BP designed the study and wrote the protocol. Author MR created the AAT. Authors SS and FL managed the literature searches and analyses. Author SS undertook the statistical analysis and wrote the first draft of the manuscript. Authors BP, FL, MR, KR, and PS revised the paper critically for important intellectual content. All authors contributed to and have approved the final manuscript. All authors declare that they have no conflict of interest.
Struijs SY, Lamers F, Rinck M, Roelofs K, Spinhoven P, Penninx BWJH. The predictive value of Approach and Avoidance tendencies on the onset and course of depression and anxiety disorders. Depress Anxiety. 2018;35:551–559. https://doi.org/10.1002/da.22760
Funding information Grant sponsor: Geestkracht program of the Netherlands Organisation for Health Research and Development; Contract grant number: 10‐000‐1002; Grant sponsor: European Union Seventh Framework Programme (FP7/2007–2013); Grant number: PCIG12‐GA2012‐334065.
REFERENCES
- Beck, A. , Brown, G. , Epstein, N. , & Steer, R. (1988). An inventory for measuring clinical anxiety: Psychometric properties. Journal of Consulting and Clinical Psychology, 56(6), 893–897. https://doi.org/10.1037/0022-006X.56.6.893 [DOI] [PubMed] [Google Scholar]
- Beevers, C. , & Meyer, B. (2002). Lack of positive experiences and positive expectancies mediate the relationship between BAS responsiveness and depression. Cognition & Emotion, 16(4), 549–564. https://doi.org/10.1080/02699930143000365 [Google Scholar]
- Brown, T. A. (2007). Temporal course and structural relationships among dimensions of temperament and DSM‐IV anxiety and mood disorder constructs. Journal of Abnormal Psychology, 116(2), 313–328. https://doi.org/10.1037/0021-843X.116.2.313 [DOI] [PubMed] [Google Scholar]
- Campbell‐Sills, L. , Liverant, G. , & Brown, T. (2004). Psychometric evaluation of the behavioral inhibition/behavioral activation scales in a large sample of outpatients with anxiety and mood disorders. Psychological Assessment, 16(3), 244–254. https://doi.org/10.1037/1040-3590.16.3.244 [DOI] [PubMed] [Google Scholar]
- Carver, C. , & White, T. (1994). Behavioral‐inhibition, behavioral activation, and affective responses to impending reward and punishment: The BIS/BAS scales. Journal of Personality and Social Psychology, 67(2), 319–333. https://doi.org/10.1037/0022-3514.67.2.319 [Google Scholar]
- Caseras, X. , Avila, C. , & Torrubia, R. (2003). The measurement of individual differences in Behavioural Inhibition and Behavioural Activation Systems: A comparison of personality scales. Personality and Individual Differences, 34(6), 999–1013. https://doi.org/10.1016/S0191-8869(02)00084-3 [Google Scholar]
- Coplan, R. J. , Wilson, J. , Frohlick, S. L. , & Zelenski, J. (2006). A person‐oriented analysis of behavioral inhibition and behavioral activation in children. Personality and Individual Differences, 41(5), 917–927. https://doi.org/10.1016/j.paid.2006.02.019 [Google Scholar]
- Cousijn, J. , Goudriaan, A. E. , & Wiers, R. W. (2011). Reaching out towards cannabis: Approach‐bias in heavy cannabis users predicts changes in cannabis use. Addiction, 106(9), 1667–1674. https://doi.org/10.1111/j.1360-0443.2011.03475.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuthbert, B. N. , & Insel, T. R. (2013). Toward the future of psychiatric diagnosis: The seven pillars of RDoC. BMC Medicine, 11, 126 https://doi.org/10.1186/1741-7015-11-126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enter, D. , Colzato, L. S. , & Roelofs, K. (2012). Dopamine transporter polymorphisms affect social approach‐avoidance tendencies. Genes Brain and Behavior, 11(6), 671–676. https://doi.org/10.1111/j.1601-183X.2012.00791.x [DOI] [PubMed] [Google Scholar]
- Fullana, M. , Mataix‐Cols, D. , Trujillo, J. , Caseras, X. , Serrano, F. , Alonso, P. , … Torrubia, R. (2004). Personality characteristics in obsessive‐compulsive disorder and individuals with subclinical obsessive‐compulsive problems. British Journal of Clinical Psychology, 43, 387–398. https://doi.org/10.1348/0144665042388937 [DOI] [PubMed] [Google Scholar]
- Heuer, K. , Rinck, M. , & Becker, E. S. (2007). Avoidance of emotional facial expressions in social anxiety: The Approach‐Avoidance Task. Behaviour Research and Therapy, 45(12), 2990–3001. https://doi.org/10.1016/j.brat.2007.08.010 [DOI] [PubMed] [Google Scholar]
- Hovenkamp‐Hermelink, J. H. M. , Riese, H. , van der Veen, D. C. , Batelaan, N. M. , Penninx, B. W. J. H. , & Schoevers, R. A. (2016). Low stability of diagnostic classifications of anxiety disorders over time: A six‐year follow‐up of the NESDA study. Journal of Affective Disorders, 190, 310–315. https://doi.org/10.1016/j.jad.2015.10.035 [DOI] [PubMed] [Google Scholar]
- Hundt, N. E. , Nelson‐Gray, R. O. , Kimbrel, N. A. , Mitchell, J. T. , & Kwapil, T. R. (2007). The interaction of reinforcement sensitivity and life events in the prediction of anhedonic depression and mixed anxiety‐depression symptoms. Personality and Individual Differences, 43(5), 1001–1012. https://doi.org/10.1016/j.paid.2007.02.021 [Google Scholar]
- Johnson, S. , Turner, R. , & Iwata, N. (2003). BIS/BAS levels and psychiatric disorder: An epidemiological study. Journal of Psychopathology and Behavioral Assessment, 25(1), 25–36. https://doi.org/10.1023/A:1022247919288 [Google Scholar]
- Jones, S. , & Day, C. (2008). Self appraisal and behavioural activation in the prediction of hypomanic personality and depressive symptoms. Personality and Individual Differences, 45(7), 643–648. https://doi.org/10.1016/j.paid.2008.07.008 [Google Scholar]
- Jorm, A. , Christensen, H. , Henderson, A. , Jacomb, P. , Korten, A. , & Rodgers, B. (1999). Using the BIS/BAS scales to measure behavioural inhibition and behavioural activation: Factor structure, validity and norms in a large community sample. Personality and Individual Differences, 26(1), 49–58. [Google Scholar]
- Kasch, K. , Rottenberg, J. , Arnow, B. , & Gotlib, I. (2002). Behavioral activation and inhibition systems and the severity and course of depression. Journal of Abnormal Psychology, 111(4), 589–597. https://doi.org/10.1037//0021-843X.111.4.589 [DOI] [PubMed] [Google Scholar]
- Kessler, R. , Chiu, W. , Demler, O. , & Walters, E. (2005). Prevalence, severity, and comorbidity of 12‐month DSM‐IV disorders in the national comorbidity survey replication. Archives of General Psychiatry, 62(6), 617–627. https://doi.org/10.1001/archpsyc.62.6.617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimbrel, N. A. , Mitchell, J. T. , & Nelson‐Gray, R. O. (2010). An examination of the relationship between behavioral approach system (BAS) sensitivity and social interaction anxiety. Journal of Anxiety Disorders, 24(3), 372–378. https://doi.org/10.1016/j.janxdis.2010.02.002 [DOI] [PubMed] [Google Scholar]
- Kimbrel, N. A. , Nelson‐Gray, R. O. , & Mitchell, J. T. (2007). Reinforcement sensitivity and maternal style as predictors of psychopathology. Personality and Individual Differences, 42(6), 1139–1149. https://doi.org/10.1016/j.paid.2006.06.028 [Google Scholar]
- Lamers, F. , van Oppen, P. , Comijs, H. C. , Smit, J. H. , Spinhoven, P. , van Balkom, A. J. , … Penninx, B. W. (2011). Comorbidity patterns of anxiety and depressive disorders in a large cohort study: The Netherlands Study of Depression and Anxiety (NESDA). Journal of Clinical Psychiatry, 72(3), 341–348. https://doi.org/10.4088/JCP.10m06176blu [DOI] [PubMed] [Google Scholar]
- Lamers, F. , Hoogendoorn, A. W. , Smit, J. H. , van Dyck, R. , Zitman, F. G. , Nolen, W. A. , & Penninx, B. W. (2012). Sociodemographic and psychiatric determinants of attrition in the netherlands study of depression and anxiety (NESDA). Comprehensive Psychiatry, 53(1), 63–70. https://doi.org/10.1016/j.comppsych.2011.01.011 [DOI] [PubMed] [Google Scholar]
- Li, Y. , Xu, Y. , & Chen, Z. (2015). Effects of the behavioral inhibition system (BIS), behavioral activation system (BAS), and emotion regulation on depression: A one‐year follow‐up study in Chinese adolescents. Psychiatry Research, 230(2), 287–293. https://doi.org/10.1016/j.psychres.2015.09.007 [DOI] [PubMed] [Google Scholar]
- Lundqvist, D. , Flykt, A. , Öhman, A. . (1998). The Karolinska directed emotional faces ‐ KDEF, CD ROM from Department of Clinical Neuroscience [Video/DVD], Psychology section Karolinska Institutet. https://doi.org/ISBN 91-630-7164-9
- McFarland, B. , Shankman, S. , Tenke, C. , Bruder, G. , & Klein, D. (2006). Behavioral activation system deficits predict the six‐month course of depression. Journal of Affective Disorders, 91(2‐3), 229–234. https://doi.org/10.1016/j.jad.2006.01.012 [DOI] [PubMed] [Google Scholar]
- Muris, P. , Meesters, C. , de Kanter, E. , & Timmerman, P. (2005). Behavioural inhibition and behavioural activation system scales for children: relationships with Eysenck's personality traits and psychopathological symptoms. Personality and Individual Differences, 38(4), 831–841. https://doi.org/10.1016/j.paid.2003.06.007 [Google Scholar]
- Penninx, B. W. , Beekman, A. T. , Smit, J. H. , Zitman, F. G. , Nolen, W. A. , Spinhoven, P. , … van Dyck, R. (2008). The Netherlands Study of Depression and Anxiety (NESDA): Rationale, objectives and methods. International Journal of Methods in Psychiatric Research, 17(3), 121–140. https://doi.org/10.1002/mpr.256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penninx, B. W. J. H. , Nolen, W. A. , Lamers, F. , Zitman, F. G. , Smit, J. H. , Spinhoven, P. , … Beekman, A. T. F. (2011). Two‐year course of depressive and anxiety disorders: Results from the netherlands study of depression and anxiety (NESDA). Journal of Affective Disorders, 133(1–2), 76–85. https://doi.org/10.1016/j.jad.2011.03.027 [DOI] [PubMed] [Google Scholar]
- Phaf, R. H. , Mohr, S. E. , Rotteveel, M. , & Wicherts, J. M. (2014). Approach, avoidance, and affect: A meta‐analysis of approach‐avoidance tendencies in manual reaction time tasks. Frontiers in Psychology, 5, 378 https://doi.org/10.3389/fpsyg.2014.00378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinto‐Meza, A. , Caseras, X. , Soler, J. , Puigdemont, D. , Perez, V. , & Torrubia, R. (2006). Behavioural Inhibition and Behavioural Activation Systems in current and recovered major depression participants. Personality and Individual Differences, 40(2), 215–226. https://doi.org/10.1016/j.paid.2005.06.021 [Google Scholar]
- Reinecke, A. , Becker, E. S. , & Rinck, M. (2010). Three indirect tasks assessing implicit threat associations and behavioral response tendencies test‐retest reliability and validity. Zeitschrift Fur Psychologie‐Journal of Psychology, 218(1), 4–11. https://doi.org/10.1027/0044-3409/a000002 [Google Scholar]
- Rinck, M. , & Becker, E. S. (2007). Approach and avoidance in fear of spiders. Journal of Behavior Therapy and Experimental Psychiatry, 38(2), 105–120. https://doi.org/10.1016/j.jbtep.2006.10.001 [DOI] [PubMed] [Google Scholar]
- Rubin, D. B. (1987). Multiple imputation for nonresponse in surveys. New York: John Wiley & Sons. [Google Scholar]
- Rush, A. J. , Gullion, C. M. , Basco, M. R. , & Jarrett, R. B. (1996). The Inventory of Depressive Symptomatology (IDS): Psychometric properties. Psychological Medicine: A Journal of Research in Psychiatry and the Allied Sciences, 26(3), 477–486. https://doi.org/10.1017/S0033291700035558 [DOI] [PubMed] [Google Scholar]
- Scholten, W. D. , Batelaan, N. M. , Penninx, B. W. J. H. , van Balkom, A. J. L. M. , Smit, J. H. , Schoevers, R. A. , & van Oppen, P. (2016). Diagnostic instability of recurrence and the impact on recurrence rates in depressive and anxiety disorders. Journal of Affective Disorders, 195, 185–190. https://doi.org/10.1016/j.jad.2016.02.025 [DOI] [PubMed] [Google Scholar]
- Segarra, P. , Ross, S. R. , Pastor, M. C. , Montanes, S. , Poy, R. , & Molto, J. (2007). MMPI‐2 predictors of Gray's two‐factor reinforcement sensitivity theory. Personality and Individual Differences, 43(3), 437–448. https://doi.org/10.1016/j.paid.2006.12.013 [Google Scholar]
- Sportel, B. E. , Nauta, M. H. , de Hullu, E. , & de Jong, P. J. (2013). Predicting internalizing symptoms over a two year period by BIS, FFFS and attentional control. Personality and Individual Differences, 54(2), 236–240. https://doi.org/10.1016/j.paid.2012.08.043<bib> [Google Scholar]
- Struijs, S. Y. , Lamers, F. , Vroling, M. S. , Roelofs, K. , Spinhoven, P. , & Penninx, B. W. J. H. (2017). Approach and avoidance tendencies in depression and anxiety disorders. Psychiatry Research, 256, 475–481. https://doi.org/S0165-1781(16)30900-3 [pii] [DOI] [PubMed] [Google Scholar]
- Takahashi, Y. , Roberts, B. W. , Yamagata, S. , & Kijima, N. (2015). Personality traits show differential relations with anxiety and depression in a nonclinical sample. Psychologia, 58(1), 15–26. [Google Scholar]
- Van Meter, A. R. , & Youngstrom, E. A. (2015). A tale of two diatheses: Temperament, BIS, and BAS as risk factors for mood disorder. Journal of Affective Disorders, 180, 170–178. https://doi.org/10.1016/j.jad.2015.03.053 [DOI] [PubMed] [Google Scholar]
- Wittchen, H. (1994). Reliability and validity studies of the WHO‐Composite International Diagnostic Interview (CIDI): A critical review. Journal of Psychiatric Research, 28(1), 57–84. https://doi.org/10.1016/0022-3956(94)90036-1 [DOI] [PubMed] [Google Scholar]
- World Health Organization . (2008). The global burden of disease: 2004 Update. Geneva, Switzerland: Author. [Google Scholar]


