Abstract
Hypertension is a serious world-wide health problem as it increases cardiovascular atherosclerotic risk, stroke and attending morbidity and mortality. Both systolic and diastolic blood pressures and particularly systolic pressure increase with aging. The downsides from pharmacological therapy have led to consideration of additional treatments, including acupuncture, which evokes endogenous neural-hormonal systems to lower blood pressure. Using basic science studies to guide clinical approaches to research, it is apparent that low frequency, low intensity electroacupuncture reduces sympathetic outflow in approximately 70% of patients with mild to moderate hypertension who are off antihypertensive drugs. Systolic and, to a lesser extent, diastolic arterial blood pressures can be lowered over two to four weeks for prolonged periods, lasting as long as one month, after cessation of an eight weeks of once weekly stimulation. Many questions about long-term therapy, treatment of resistant patients and efficacy in patients on medication remain to be studied. Current data, however, suggest that there may be a role of acupuncture in treatment of hypertension.
Keywords: sympathetic, transcriptional regulation, renin, norepinephrine, hypertension
1 Introduction
Hypertension is a serious world-wide health problem. In the United States the prevalence was 29% between 2011 and 2014[1]. It is slightly more common in men than women (30% vs 28%) and increases with age[1]. China likewise has a high prevalence of hypertension as noted in a cross-sectional study between 2007–2008 (27%, 29% vs 24% males vs females) [2]. The importance of uncontrolled hypertension is evident by its role as a major risk factor for cardiovascular disease (CVD), including deaths from myocardial infarction, stroke and heart failure[1, 3, 4]. The burden of hypertension and its associated cardiovascular mortality in China increases from 12.6% between ages 35–39 years to 58.4% between 70–74 years and varies substantially by region[5]. Furthermore, only 29.6% of these patients had their hypertension controlled[6]. Uncontrolled hypertension in China is associated with a relative risk for CVD mortality ranging from 4.1 to 1.9[6]. Hypertension accounts for one third of all deaths due to CVD[5]. These facts indicate that diagnosis, awareness and control of hypertension need to be improved in both China and western countries[7]. While awareness and treatment of hypertension have been improved, control has not[8]. A recent Center for Disease Control (CDC) grand rounds in the US highlighted the cost of hypertension of $49 billion dollars for the 35 million US residents with uncontrolled hypertension[9]. Many patients do not recognize their hypertension since it often presents with no symptoms and because providers miss opportunities to diagnose it and to offer strategies that can lead to effective blood pressure control. The Million Hearts Initiative (Million Hearts) from the US Department of Health and Human Services has been developed to reduce one million heart attacks and strokes by 2017 and to increase by 10 million the number of patients in the US whose elevated blood pressure is controlled[10]. More accurate blood pressure measurement and monitoring, improved treatment and increased awareness of hypertension are central to the success of this initiative. In this regard, we know that reducing the prevalence of hypertension and lowering blood pressure in oriental populations lead to a decline in stroke mortality[11]. Hence there is a sound rationale for improving treatment and awareness.
Treatment and awareness depend on setting appropriate blood pressure goals. The consensus for many years following recommendations from the Joint National Commission (JNC) 7 was a goal of less than 140/90 mmHg for most patients with hypertension, irrespective of age, and 130/80 mmHg for patients with diabetes, chronic renal disease and certain cardiovascular conditions[12]. More recent modifications by JNC 8[13, 14], have raised the systolic blood pressure goal to 150 mmHg for patients aged 60 years or older. New clinical studies, ACCORD and SPRINT[15–17], have led to the conclusion that 120/80 mmHg for adults below 50 years and 130 mmHg systolic in patients with CVD, chronic renal disease or diabetes should be the goal based on a wealth of epidemiological data[18]. Individuals between 50 and 74 years should have a systolic blood pressure goal of <130 mmHg, although sometimes the first target should be <140 mmHg[18]. Finally, systolic blood pressure in patients aged 75 years and above should be reduced to <140 mmHg[18]. Thus, in addition to healthy life-styles it has been recognized that blood pressure for population in general should be lowered to levels below 120/80 mmHg, or the lowest levels possible consistent with maintaining good renal function and cognition because of the almost linear increased risk of CVD above this level[18].
Healthy life-style includes not smoking, maintaining optimal weight, a diet in which salt is lowered and reducing stress. This advice is first line of therapy in any patient with hypertension. Because blood pressure frequently remains elevated, drug therapy often is initiated. Drugs, however, pose problems both because compliance often is suboptimal and the side effects that accompany almost all drugs. Hence, there is a rationale for consideration of additional therapies. One such possibility is acupuncture.
2 Early studies
In 1997 during studies on the influence of acupuncture on demand-induced myocardial ischemia, we noted that ischemia was relieved through acupuncture’s lowering of oxygen demand[19]. This experimental model included partial ligation of a coronary artery to simulate coronary atherosclerosis. Stress was created by transiently elevating blood pressure through stimulation of a visceral sympathoexcitatory reflex. This maneuver led to a disparity between oxygen supply, which was limited by the partial coronary occlusion, and demand created by the increased blood pressure and the attendant elevation in the rate-pressure product. Acupuncture did not improve supply (i.e., coronary blood flow) but lessened demand since it blunted the reflex elevation in blood pressure. This observation led us to conclude that acupuncture might lower sympathetic outflow and hence decrease the magnitude of the cardiovascular reflex sympathetically mediated vasoconstriction. Subsequent studies largely targeted acupuncture’s blood pressure actions and underlying mechanisms. For example, a follow-up study[20] showed that the opioid system played a prominent role in the blood pressure and ischemia reducing effects of acupuncture (Fig. 1).
Fig. 1.
Reflex increases in arterial blood pressure (AP) and myocardial wall thickening (Wth) are reduced with electroacupuncture (EA) in cats. At time points indicated by arrows, bradykinin (BK) was applied to surface of the gallbladder: a, baseline control measurement; b, a small branch of left anterior descending coronary artery (LAD) was ligated and the response to BK was examined; c, EA (0.5 ms, 4 Hz) was applied at P5-P6 on forelegs for 30 min and BK response was evaluated; d, opioid antagonist, naloxone, was administered intravenously and response to BK was measured. The fall in normalized wall thickening (%Wth) associated with reflexly increased sympathetic stimulation in presence of LAD ligation (b) was reversed by EA (c). A decline in AP response also was apparent (c). Intravenous administration of naloxone blocked the effects of EA; wall thickening declined, and AP response returned to normal (d). Sympathoinhibitory effects of EA at P5-P6 persist for at least 1 h in this model. Therefore, naloxone was administered at a time when sympathoinhibition by EA was expected to maintain improved %Wth and diminished AP response to BK stimulation[20].
3 Mechanisms
It is clear that acupuncture exerts its systemic actions through the peripheral and central nervous systems. Meridians, a long-held belief in Traditional Chinese Medicine, have never been identified anatomically[21]. However, substantial evidence indicates that both finely myelinated Group III and unmyelinated Group IV sensory nerves are stimulated during low frequency, low intensity electroacupuncture[19]. Interruption of these systems for example by lidocaine[22] or by administering capsaicin to neonatal rats to eliminate Group IV fibers, reverses the anti-nociceptive and sympathoinhibitory actions of acupuncture[23, 24]. Furthermore, selective blockade of the actions or release of neurotransmitters in the hypothalamus, including the paraventricular and arcuate nuclei[25–27], midbrain ventrolateral periaqueductal gray[28–30] and brain stem unclei raphé pallidus and rostral ventrolateral medulla[31–34] likewise blocks the action of electroacupuncture on reflex elevations in blood pressure. In addition to opioids, including enkephalins and endorphins, in the medulla and hypothalamus[27, 35], gamma aminobutyric acid and nociceptin in the medulla[33], glutamate in the medulla[34], midbrain[28] and hypothalamus[28], serotonin in the medulla[36, 37], endocannabinoids in the midbrain[29, 38] and acetylcholine in the hypothalamus[26] underlie acupuncture’s antihypertensive actions (Fig. 2).
Fig. 2.
Neuronal pathways, circuitry and synaptic transmission involved in electroacupuncture (EA)’s cardiovascular responses at acupoints P5-P6 and ST36-ST37 on sympathoexcitatory reflex responses elicited by activation of visceral afferents in cats and rats. Spinal visceral afferent pathways (orange arrows) ascending to medulla, midbrain and hypothalamus activate (+) cardiovascular neurons, which can be modified by 30 min EA at P5-P6 (activating median nerves, MN) and ST36-ST37 (activating deep peroneal nerves, DPN) to reduce (−) sympathetic outflow (blue arrows) that in turn influences cardiovascular function. Acupuncture influences neurons that regulate cardiovascular function in the paraventricular nucleus (PVN), arcuate nucleus (ARC), ventrolateral periaqueductal gray (vlPAG), nucleus raphe-pallidus (NR-P), rostral ventrolateral medullar (rVLM), and neurotransmitters beta-endorphin (β-End), acetylcholine (ACh), L-glutamate (L-Glu), gamma-butyric acid (GABA), enkephalin (Enk), serotonin 1A receptor (5-HT1A) that participate in the central neural processing during EA. Dyn = dynorphin, DH = dorsal horn, IML = intermediolateral column.
4 Preclinical studies
Experimental studies laid groundwork for clinical investigation. Both manual acupuncture and electroacupuncture exert similar reductions in blood pressure transiently elevated during reflex abdominal visceral organ stimulation to evoke sympathoexcitation[39]. Low frequency, as opposed to high frequency electroacupuncture is optimal for lowering elevated blood pressure[40]. Electroacupuncture is employed as a consistent repetitive 2–4 Hz form of stimulation over a 30 minute period. Points overlying the median nerve (Pericardial 5 and 6) on the wrist and the deep peroneal nerve (Stomach 36 and 37) just below the knee more effectively lower elevated blood pressure than points overlying the superficial radial nerve (Large Intestine 7 and Lung 6) on the forearm and superficial peroneal nerve (Gallbladder 37 and 38) on the lower leg[41]. These point specific cardiovascular actions of acupuncture define locations on peripheral nerves that exert the largest blood pressure lowering responses as well as control points that have little or no effect on cardiovascular function. When blood pressure is elevated, stimulation of either the median or deep peroneal nerves innervating deep somatic structures leads to blood pressure decreases because they provide substantial modulatory input to the rostral ventrolateral medulla, a brain stem region containing premotor sympathetic neurons that during acupuncture downregulates sympathetic outflow, compared to more superficial radial and peroneal sensory nerves that ultimately project less to this autonomic nucleus[41]. Finally, although acupuncture can lower repeated short-term reflex elevations in blood pressure for one to two hours, recent studies have focused on experimental hypertension, to demonstrate that repeated sequential application every second or third day can produce blood pressure depression lasting for several days[42]. Through transcriptional regulation repetitive electroacupuncture stimulates production of preproenkephalin, the mRNA precursor to the peptide neurotransmitter enkephalin[42, 43] (Fig. 3).
Fig. 3.
Repetitive electroacupuncture (EA) treatment (twice weekly) reduces blood pressure in cold-induced hypertension (CIH), an environmental model of sustained high blood pressure in rats[46]. Cold exposure increased systolic blood pressure (SBP; Panel A), diastolic blood pressure (DBP; Panel B) and heart rate (HR; Panel C) after four weeks and induced sustained hypertension by six weeks. BPs and HRs of rats in the hypertension and sham-EA groups remained elevated at 11 weeks. In contrast, elevated SBP and DBP but not HR in the EA group was reduced after six sessions of EA and remained low throughout EA treatment. BPs and HRs of normotensive rats remained stable throughout the study. SBP and DBP of EA-treated CIH rats, although beginning to return to pre-treatment levels were still significantly reduced for three days following termination of EA compared to sham-EA and CIH-rats. Values represent means ± SEM. ^, * and # indicate P < 0.05 compared with sham-EA, CIH and normotensive controls, respectively. Preproenkephalin (PPE) was measured by real-time polymerase chain reaction in EA-CIH, sham-EA-CIH, CIH and normotensive rats respectively in 9, 6, 6, and 6 rats at 72 h after termination of treatment. Group data (Panel D) show that PPE mRNA, 72 h after termination of EA treatment, was increased relative to controls. ^, * and # indicate significant differences (P < 0.05) compared respectively with CIH treated with sham-EA-CIH, CIH and the normotensive controls[42]. w, week(s).
5 Clinical studies
Previous studies of acupuncture treatment of hypertension produced mixed results, success depending on whether acupuncture was used as a standalone or adjunctive therapy[44]. Some trials used pattern diagnosis while others used a standardized protocol. Some measured cuff sphygmomanometer blood pressure, relying on observer measurement, while others used automated 24 h ambulatory monitoring. Most used manual acupuncture.
Based on previous experimental observations to guide therapy, we selected patients with mild to moderate systolic and/or diastolic hypertension (Table 1) off all antihypertensive medications to eliminate confounding effects of potentially inconsistent medication usage[45]. Low intensity, low frequency electroacupuncture was applied once weekly for eight weeks to active points with demonstrated cardiovascular actions and compared either longitudinally or in a cross-over design to points that had little or no cardiovascular action in experimental studies. Ambulatory blood pressure was measured over a 24 h period (every 30 min diurnally, every hour nocturnally) once weekly. Systolic, and to a lesser extent, diastolic blood pressures were reduced by stimulation of active points after 2–4 weeks, whereas they were little changed in patients receiving control stimulation (Figs. 4 & 5). Classifying responders as those manifesting ≥6 mmHg decrease in systolic blood pressure, ~70% of patients in the active group showed −9 mmHg average systolic and −17 mmHg peak (highest 24 h) systolic blood pressure (Fig. 6). Systolic pressure in a subset of responsive patients followed for two months remained low for as long as one month after termination of the procedure (Fig. 7). In a pilot protocol, a very small number of patients (n = 6) on monthly reinforcement (once each month) maintained lower systolic pressures compared to baseline and after an initial eight-week course of therapy (Fig. 8). Serum catecholamines and plasma renin activity in the responsive group (−6 mmHg or more) were decreased (Fig. 9). These data strongly suggest that if acupuncture is applied in a standardized manner to stimulate sensory pathways shown to be effective experimentally, systolic and, to a lesser extent, diastolic blood pressure are lowered slowly and for a prolonged period and that monthly reapplication may be able to maintain lower blood pressures. The later observation, however, needs confirmation since only few patients were studied for prolonged periods, over several months. Hypertensive patients with high baseline catecholamines (presumably a marker of high sympathetic outflow) and renin appear to be most responsive[45].
Table 1.
Patient characteristics in acupuncture hypertension study
| Treatment group | PC 5-6 + ST 36-37 (active) | LI 6-7 + GB 37-39 (control) | Total | P value |
|---|---|---|---|---|
| Mean age (range) (years) | 58 ± 2 (38–75) | 54 ± 2 (38–71) | >0.05 | |
| Sex (n) | ||||
| Male | 16 | 14 | 30 | |
| Female | 17 | 18 | 35 | |
| Total | 33 | 32 | 65 | |
| Body mass index (kg/m2) | 26 ± 1 (22–42) | 25 ± 1 (22–30) | >0.05 | |
| Baseline mean arterial pressure (mmHg) | ||||
| 24-h peak | 130 ± 2 | 126 ± 3 | >0.05 | |
| 48-h peak | 107 ± 2 | 105 ± 4 | >0.05 | |
Values expressed with ± sign are the mean ± standard error of the mean. Values expressed in parentheses are ranges[45].
Fig. 4.
Systolic (panel A, SBP), diastolic (panel B, DBP) and mean (panel C, MBP) blood pressures averaged over 24 h were reduced in 33 hypertensive patients treated with electroacupuncture (EA) bilaterally at PC5-6 + ST36-37 active acupoints for eight weeks. EA did not alter heart rate (panel D, HR). Significant BP reductions were observed by four weeks of treatment. *, indicates significant decrease in BP compared to BP prior to treatment[45]. w, week(s).
Fig. 5.
Group comparison of the changes in SBP and DBP at 2, 4, 6, 8 weeks with electroacupuncture (EA) treatment at active and control acupoints (see text for definitions[45]). The changes in SBP were different at week eight in the two groups of patients with treatment at PC5-6 + ST36-37 and LI6-7 + GB37-39 (panel A). Acupuncture treatment at PC5-6 + ST36-37 acupoints for eight weeks decreased average DBP compared to control treatment (panel B). *, indicates significant difference bettween the groups[45]. w, week(s).
Fig. 6.

Effect of EA on SBP was evaluated during eight weeks of EA (PC5-6 + ST36-37) in 22 patients. Average SBP was reduced from week two to eight during treatment. Onset of decreased peak SBP was at four weeks and remained reduced throughout treatment. *, displays significantly lowered SBP. w, week(s).
Fig. 7.
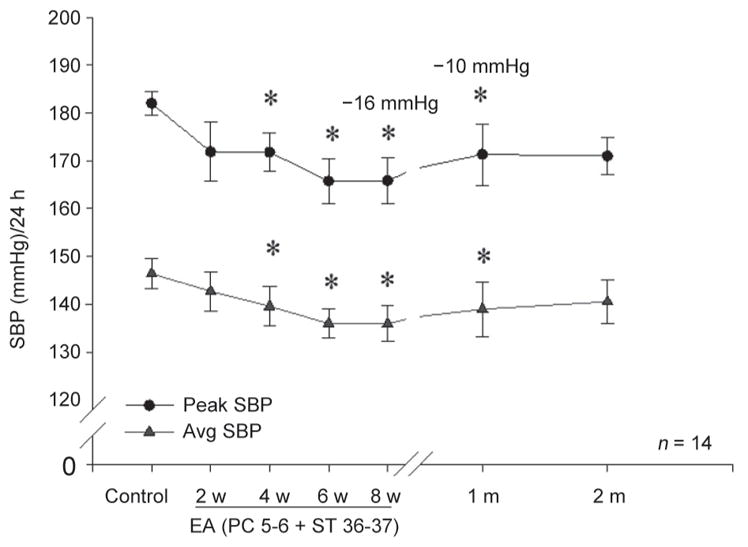
Effect of EA on SBP was evaluated for two months during the follow-up study in 14 patients. Peak and average SBPs were reduced for one-month following the EA (PC5-6 + ST36-37) therapy. Peak and average SBPs were reduced at weeks six and eight during EA treatment. Significant decrease in SBP is indicated with (*)[45]. w, week(s).
Fig. 8.

Pilot data showing action of EA over a six-month period assessed during monthly reinforcement therapy in subgroup of six hypertensive subjects. Following a course of eight weeks of weekly acupuncture therapy, continued monthly EA treatment maintained a low systolic blood pressure relative to pre-EA control (Significant decrease in SBP is indicated with *)[45]. w, week(s); m, month(s).
Fig. 9.
EA modulation of plasma norepinephrine and renin activity. Norepinephrine in 25 hypertensive patients was measured before and after eight weeks of treatment with EA at PC5-6 + ST36-37. Baseline norepinephrine was higher before EA (**P < 0.05) and decreased by 164 ng/mL in subjects responsive to EA (*P < 0.05). Norepinephrine was not altered by eight weeks of EA treatment in twelve patients unresponsive to EA. Renin activity in all 13 of 22 hypertensive patients responsive to EA at PC5-6+ST36-37 was decreased significantly after eight weeks of treatment (*P < 0.05). Nine low-responders to EA with lower renin activities before EA were unchanged by eight weeks of EA therapy[45]. w, week(s).
6 Conclusions
Hypertension is a world-wide health problem leading to CVD with significant morbidity and mortality. Stroke, vascular disease, myocardial infarction, heart and renal failure are all consequences of uncontrolled hypertension. While great strides are being made to reduce hypertension by focusing on improved recognition, education and treatment, it remains a serious epidemiological problem in the US and China. Current therapy is effective but often suboptimal, providing a rationale for development of new therapeutic strategies. Healthy life-styles are commonly recognized as first line therapy. The ancient Chinese therapy of acupuncture may be considered to be a form of natural therapy that activates the brain’s chemistry to reduce elevated blood pressure. Although previous studies have shown mixed outcomes, there is reason to believe that their study design could have been improved. In this regard, a recent randomized prospective single blinded clinical trial using information from mechanistic experimental studies to guide its design suggests that electroacupuncture in patients with mild to moderate hypertension off all antihypertensive drugs may be beneficial. This study was designed to be translatable to clinical practice, incorporating once weekly application of low frequency, low intensity 30 min electroacupuncture for eight weeks and stimulating a set of points that influence cardiovascular function. Both peak and average systolic and, to a lesser extent, diastolic blood pressure were lowered by 4–8 mmHg. If patients fell into the group showing 6 mmHg or more decrease, comprising ~70% of all patients, they demonstrated a decline after 2–4 weeks and a prolonged response, often lasting for a month after cessation of therapy[45]. Pilot data suggest that it may be possible to reinforce these prolonged decreases in elevated blood pressure, but clearly more study is necessary. This information suggests that, in the future, acupuncture may be a viable adjunct to help our societies more effectively reduce the burden of hypertension.
Acknowledgments
The authors thank Dr. Peng Li for his significant contribution to the conceptualization and completion of many of the cited studies and Drs. Zhi-Ling Guo and Liang-Wu Fu for their scientific contributions.
Research from the corresponding author’s laboratory was supported by grants from the U.S. National Institutes of Health (NIH) (No. HL-63313, HL-72125, AT-9347-01A1), Adolph Coors and Dana Foundations.
References
- 1.Yoon SS, Carroll MD, Fryar CD. Hypertension Prevalence and Control Among Adults: United States, 2011–2014. NCHS Data Brief. 2015;(220):1–8. [PubMed] [Google Scholar]
- 2.Gao Y, Chen G, Tian H, Lin L, Lu J, Weng J, Jia W, Ji L, Xiao J, Zhou Z, Ran X, Ren Y, Chen T, Yang W. Prevalence of hypertension in china: a cross-sectional study. PLoS One. 2013;8:e65938. doi: 10.1371/journal.pone.0065938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fryar CD, Chen TC, Li X. Prevalence of uncontrolled risk factors for cardiovascular disease: United States, 1999–2010. 2012;(103):1–8. [PubMed] [Google Scholar]
- 4.Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Makuc DM, Marcus GM, Marelli A, Matchar DB, Moy CS, Mozaffarian D, Mussolino ME, Nichol G, Paynter NP, Soliman EZ, Sorlie PD, Sotoodehnia N, Turan TN, Virani SS, Wong ND, Woo D, Turner MB. Heart disease and stroke statistics--2012 update: a report from the American Heart Association. Circulation. 2012;125:e2–e220. doi: 10.1161/CIR.0b013e31823ac046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lewington S, Lacey B, Clarke R, Guo Y, Kong XL, Yang L, Chen Y, Bian Z, Chen J, Meng J, Xiong Y, He T, Pang Z, Zhang S, Collins R, Peto R, Li L, Chen Z. The burden of hypertension and associated risk for cardiovascular mortality in China. JAMA Intern Med. 2016;176:524–532. doi: 10.1001/jamainternmed.2016.0190. [DOI] [PubMed] [Google Scholar]
- 6.Lewington S, Lacey B, Clarke R. Uncontrolled hypertension and risk of cardiovascular mortality in China-reply. JAMA Intern Med. 2016;176:1234. doi: 10.1001/jamainternmed.2016.3825. [DOI] [PubMed] [Google Scholar]
- 7.Wong ND, Franklin SS. Reducing the burden of hypertension: China’s long march ahead. JAMA Intern Med. 2016;176:532–533. doi: 10.1001/jamainternmed.2016.0213. [DOI] [PubMed] [Google Scholar]
- 8.Bundy JD, He J. Hypertension and related cardiovascular disease burden in China. Ann Glob Health. 2016;82:227–233. doi: 10.1016/j.aogh.2016.02.002. [DOI] [PubMed] [Google Scholar]
- 9.Merai R, Siegel C, Rakotz M, Basch P, Wright J, Wong B, Thorpe P. CDC grand rounds: A public health approach to detect and control hypertension. MMWR Morb Mortal Wkly Rep. 2016;65:1261–1264. doi: 10.15585/mmwr.mm6545a3. [DOI] [PubMed] [Google Scholar]
- 10.Frieden TR, Berwick DM. The “Million Hearts” initiative--preventing heart attacks and strokes. N Engl J Med. 2011;365:e27. doi: 10.1056/NEJMp1110421. [DOI] [PubMed] [Google Scholar]
- 11.Ueshima H, Zhang XH, Choudhury SR. Epidemiology of hypertension in China and Japan. J Hum Hypertens. 2000;14:765–769. doi: 10.1038/sj.jhh.1001054. [DOI] [PubMed] [Google Scholar]
- 12.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, Jones DW, Materson BJ, Oparil S, Wright JT, Jr, Roccella EJ National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 13.James PA, Oparil S, Carter BL, Cushman WC, nison-Himmelfarb C, Handler J, Lackland DT, LeFevre ML, MacKenzie TD, Ogedegbe O, Smith SC, Jr, Svetkey LP, Taler SJ, Townsend RR, Wright JT, Jr, Narva AS, Ortiz E. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8) JAMA. 2014;311:507–520. doi: 10.1001/jama.2013.284427. [DOI] [PubMed] [Google Scholar]
- 14.Weber MA, Schiffrin EL, White WB, Mann S, Lindholm LH, Kenerson JG, Flack JM, Carter BL, Materson BJ, Ram CV, Cohen DL, Cadet JC, Jean-Charles RR, Taler S, Kountz D, Townsend R, Chalmers J, Ramirez AJ, Bakris GL, Wang J, Schutte AE, Bisognano JD, Touyz RM, Sica D, Harrap SB. Clinical practice guidelines for the management of hypertension in the community a statement by the American Society of Hypertension and the International Society of Hypertension. J Hypertens. 2014;32:3–15. doi: 10.1097/HJH.0000000000000065. [DOI] [PubMed] [Google Scholar]
- 15.Cushman WC, Evans GW, Byington RP, Goff DC, Jr, Grimm RH, Jr, Cutler JA, Simons-Morton DG, Basile JN, Corson MA, Probstfield JL, Katz L, Peterson KA, Friedewald WT, Buse JB, Bigger JT, Gerstein HC, Ismail-Beigi F. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med. 2010;362:1575–1585. doi: 10.1056/NEJMoa1001286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wright JT, Jr, Williamson JD, Whelton PK, Snyder JK, Sink KM, Rocco MV, Reboussin DM, Rahman M, Oparil S, Lewis CE, Kimmel PL, Johnson KC, Goff DC, Jr, Fine LJ, Cutler JA, Cushman WC, Cheung AK, Ambrosius WT. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373:2103–2116. doi: 10.1056/NEJMoa1511939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Williamson JD, Supiano MA, Applegate WB, Berlowitz DR, Campbell RC, Chertow GM, Fine LJ, Haley WE, Hawfield AT, Ix JH, Kitzman DW, Kostis JB, Krousel-Wood MA, Launer LJ, Oparil S, Rodriguez CJ, Roumie CL, Shorr RI, Sink KM, Wadley VG, Whelton PK, Whittle J, Woolard NF, Wright JT, Jr, Pajewski NM. Intensive vs standard blood pressure control and cardiovascular disease outcomes in adults aged ≥75 years: a randomized clinical trial. JAMA. 2016;315:2673–2682. doi: 10.1001/jama.2016.7050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chobanian AV. Hypertension in 2017-What Is the Right Target? JAMA. 2017;317(6):579–580. doi: 10.1001/jama.2017.0105. [DOI] [PubMed] [Google Scholar]
- 19.Li P, Pitsillides KF, Rendig SV, Pan HL, Longhurst JC. Reversal of reflex-induced myocardial ischemia by median nerve stimulation: a feline model of electroacupuncture. Circulation. 1998;97:1186–1194. doi: 10.1161/01.cir.97.12.1186. [DOI] [PubMed] [Google Scholar]
- 20.Chao DM, Shen LL, Tjen-A-Looi SC, Pitsillides KF, Li P, Longhurst JC. Naloxone reverses inhibitory effect of electroacupuncture on sympathetic cardiovascular reflex responses. Am J Physiol. 1999;276:H2127–H2134. doi: 10.1152/ajpheart.1999.276.6.H2127. [DOI] [PubMed] [Google Scholar]
- 21.Longhurst JC. Defining meridians: a modern basis of understanding. J Acupunct Meridian Stud. 2010;3:67–74. doi: 10.1016/S2005-2901(10)60014-3. [DOI] [PubMed] [Google Scholar]
- 22.Shen E(沈锷), Wu WY, Du HJ, Wei JY, Zhu DX. Electromyographic activity produced locally by acupuncture manipulation. Chin Med J (中华医学杂志) 1973;53:532–535. (in Chinese) [Google Scholar]
- 23.Tjen-A-Looi SC, Fu LW, Zhou W, Longhurst JC. Role of unmyelinated fibers in electroacupuncture cardiovascular responses. Auton Neurosci. 2005;118:43–50. doi: 10.1016/j.autneu.2004.12.006. [DOI] [PubMed] [Google Scholar]
- 24.Tobaldini G, Aisengart B, Lima MM, Tambeli CH, Fischer L. Ascending nociceptive control contributes to the antinociceptive effect of acupuncture in a rat model of acute pain. J Pain. 2014;15:422–434. doi: 10.1016/j.jpain.2013.12.008. [DOI] [PubMed] [Google Scholar]
- 25.Tjen-A-looi SC, Guo ZL, Fu LW, Longhurst JC. Paraventricular nucleus modulates excitatory cardiovascular reflexes during electroacupuncture. Sci Rep. 2016;6:25910. doi: 10.1038/srep25910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li P, Tjen-A-Looi SC, Longhurst JC. Excitatory projections from arcuate nucleus to ventrolateral periaqueductal gray in electroacupuncture inhibition of cardiovascular reflexes. Am J Physiol. 2006;209:H2535–H2542. doi: 10.1152/ajpheart.00972.2005. [DOI] [PubMed] [Google Scholar]
- 27.Li P, Tjen-A-Looi SC, Guo ZL, Fu LW, Longhurst JC. Long-loop pathways in cardiovascular electroacupuncture responses. J Appl Physiol. 2009;106:620–630. doi: 10.1152/japplphysiol.91277.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Li P, Tjen-A-Looi SC, Guo ZL, Longhurst JC. An arcuate-ventrolateral periaqueductal gray reciprocal circuit participates in electroacupuncture cardiovascular inhibition. Auton Neurosci. 2010;158:13–23. doi: 10.1016/j.autneu.2010.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tjen-A-Looi SC, Li P, Longhurst JC. Processing cardiovascular information in the vlPAG during electroacupuncture in rats: Roles of endocannabinoids and GABA. J Appl Physiol. 2009;106:1793–1799. doi: 10.1152/japplphysiol.00142.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tjen-A-Looi SC, Li P, Longhurst JC. Midbrain vIPAG inhibits rVLM cardiovascular sympathoexcitatory responses during acupuncture. Am J Physiol. 2006;290:H2543–H2553. doi: 10.1152/ajpheart.01329.2005. [DOI] [PubMed] [Google Scholar]
- 31.Li P, Tjen-A-Looi SC, Longhurst JC. Nucleus raphé pallidus in EA inhibition of rostral ventrolateral medulla and cardiovascular excitatory responses. FASEB J. 2010;24(1 Supplement) 1052.5. [Google Scholar]
- 32.Li P, Tjen-A-Looi SC, Longhurst JC. Rostral ventrolateral medullary opioid receptor subtypes in the inhibitory effect of electroacupuncture on reflex autonomic response in cats. Auton Neurosci. 2001;89:38–47. doi: 10.1016/S1566-0702(01)00247-8. [DOI] [PubMed] [Google Scholar]
- 33.Tjen-A-Looi SC, Li P, Longhurst JC. Role of medullary GABA, opioids, and nociceptin in prolonged inhibition of cardiovascular sympathoexcitatory reflexes during electroacupuncture in cats. Am J Physiol. 2007;293:H3627–H3635. doi: 10.1152/ajpheart.00842.2007. [DOI] [PubMed] [Google Scholar]
- 34.Zhou W, Fu LW, Tjen-A-Looi SC, Guo ZL, Longhurst JC. Role of glutamate in a visceral sympathoexcitatory reflex in rostral ventrolateral medulla of cats. Am J Physiol. 2006;291:H1309–H1318. doi: 10.1152/ajpheart.00202.2006. [DOI] [PubMed] [Google Scholar]
- 35.Tjen-A-Looi SC, Li P, Longhurst J. Rostral VLM opioid receptor subtypes in electroacupuncture inhibition of reflex autonomic response. Clin Auton Res. 1999;9:247–248. doi: 10.1016/S1566-0702(01)00247-8. [DOI] [PubMed] [Google Scholar]
- 36.Moazzami A, Tjen-A-Looi SC, Guo ZL, Longhurst JC. Serotonergic projection from nucleus raphe pallidus to rostral ventrolateral medulla modulates cardiovascular reflex responses during acupuncture. J Appl Physiol. 2010;108:1336–1346. doi: 10.1152/japplphysiol.00477.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Guo Z-L, Moazzami A, Tjen-A-Looi S, Longhurst J. Responses of opioid and serotonin containing medullary raphe neurons to electroacupuncture. Brain Res. 2008;1229:125–136. doi: 10.1016/j.brainres.2008.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fu LW, Longhurst C. Electroacupuncture modulates vlPAG release of GABA through presynaptic cannabinoid CB1 receptor. J Appl Physiol. 2009;106:1800–1809. doi: 10.1152/japplphysiol.91648.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhou W, Tjen-A-Looi S, Longhurst JC. Brain stem mechanisms underlying acupuncture modality-related modulation of cardiovascular responses in rats. J Appl Physiol. 2005;99:851–860. doi: 10.1152/japplphysiol.01365.2004. [DOI] [PubMed] [Google Scholar]
- 40.Zhou W, Fu LW, Tjen-A-Looi SC, Li P, Longhurst JC. Afferent mechanisms underlying stimulation modality-related modulation of acupuncture-related cardiovascular responses. J Appl Physiol. 2005;98:872–880. doi: 10.1152/japplphysiol.01079.2004. [DOI] [PubMed] [Google Scholar]
- 41.Tjen-A-Looi SC, Li P, Longhurst JC. Medullary substrate and differential cardiovascular response during stimulation of specific acupoints. Am J Physiol. 2004;287:R852–R862. doi: 10.1152/ajpregu.00262.2004. [DOI] [PubMed] [Google Scholar]
- 42.Li M, Tjen-A-Looi SC, Guo ZL, Longhurst JC. Repetitive electroacupuncture attenuates cold-induced hypertension through enkephalin in the rostral ventral lateral medulla. Sci Rep. 2016;6:35791. doi: 10.1038/srep35791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Li M, Tjen-A-Looi SC, Guo ZL, Longhurst JC. Repetitive electroacupuncture causes prolonged increased met-enkephalin expression in the rVLM of conscious rats. Auton Neurosci. 2012;170:30–35. doi: 10.1016/j.autneu.2012.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Li DZ, Zhou Y, Yang YN, Ma YT, Li XM, Yu J, Zhao Y, Zhai H, Lao L. Acupuncture for essential hypertension: a meta-analysis of randomized sham-controlled clinical trials. Evid Based Complement Alternat Med. 2014;2014:279478. doi: 10.1155/2014/279478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Li P, Tjen-A-Looi SC, Cheng L, Lui D, Painovich J, Vinjanury S, Longhurst JC. Long-lasting reduction of blood pressure by electroacupuncture in patients with hypertension: randomized controlled trial. Med Acupunct. 2015;27:253–266. doi: 10.1089/acu.2015.1106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Papanek PE, Wood CE, Fregly MJ. Role of the sympathetic nervous system in cold-induced hypertension in rats. J Appl Physiol. 1991;71:300–306. doi: 10.1152/jappl.1991.71.1.300. [DOI] [PubMed] [Google Scholar]








