Summary
European countries have enhanced the scope of private provision within their health care systems. Privatizing services have been suggested as a means to improve access, quality, and efficiency in health care. This raises questions about the relative performance of private hospitals compared with public hospitals. Most systematic reviews that scrutinize the performance of the private hospitals originate from the United States. A systematic overview for Europe is nonexisting. We fill this gap with a systematic realist review comparing the performance of public hospitals to private hospitals on efficiency, accessibility, and quality of care in the European Union. This review synthesizes evidence from Italy, Germany, the United Kingdom, France, Greece, Austria, Spain, and Portugal. Most evidence suggests that public hospitals are at least as efficient as or are more efficient than private hospitals. Accessibility to broader populations is often a matter of concern in private provision: Patients with higher social‐economic backgrounds hold better access to private hospital provision, especially in private parallel systems such as the United Kingdom and Greece. The existing evidence on quality of care is often too diverse to make a conclusive statement. In conclusion, the growth in private hospital provision seems not related to improvements in performance in Europe. Our evidence further suggests that the private (for‐profit) hospital sector seems to react more strongly to (financial) incentives than other provider types. In such cases, policymakers either should very carefully develop adequate incentive structures or be hesitant to accommodate the growth of the private hospital sector.
Keywords: efficiency, health care quality, health services accessibility, literature review, private sector
1. INTRODUCTION
It is an ongoing debate what the role of the private sector in the health care system should be. In theory, under competitive forces and the right preconditions, private hospitals might outperform public providers. However, empirical evidence, mostly originating from the United States, does not confirm such hypothesis.1, 2, 3 For example, Schlesinger and Gray3 find that although the evidence is mixed, it seems to favor nonprofit hospitals. Eggleston et al4 analyzing differences in quality of care also find mixed evidence. Herrera et al5 provide an overview of systematic reviews focusing on quality of for‐profit (FP), not‐for‐profit (NFP), and public providers. Among other things, they concluded that FP providers have higher mortality rates. The US studies illustrate that NFP hospitals seem to mimic FP hospitals on more competitive markets, which might blur the distinctions between both ownership types.6
Most European health markets are both less competitive and more inclusive than the United States, which may provide private providers with different incentives. During the past decades, a high amount of public provision spurred discussions about possible inefficiencies, and a movement towards privatization could be observed across Europe.7, 8 Nowadays, practically all European Union (EU) health systems “contract” both public and private providers. However, EU countries do differ regarding the scale and scope of private hospitals. In most Bismarck‐type systems, private hospitals may be on par with public hospitals: Public and private providers provide comparable services and are reimbursed in a similar way. However, in most Beveridge systems, the private sector runs parallel to the public sector as an alternative provision.8 The private sector then also is paid through a parallel private funding scheme (ie, out‐of‐pocket payments or private insurance). Such systematic differences may influence the composition and performance of private hospitals. Furthermore, countries differ on the extent of privatization. In some countries, such as the Nordic countries, hospital ownership is predominantly public, while in other countries, such as the Netherlands, public ownership is nonexistent.
It is currently unknown whether private hospitals outperform public hospitals in the different European health systems. Reviews on this topic are to the best of our knowledge nonexistent. The main aim of this review is to compare the private sector with the public sector on efficiency, quality, and accessibility of services within the EU. We are well aware that the profit status of private hospitals is most likely an important theoretical confounder in explaining differences in performance ever since Arrow9 pointed to the fact that private nonprofit status might function as a way to limit market imperfections in situations of unobservable performance of information asymmetries.9 However, distinctions between public and private provisions are often at least as important as institutional demarcations, as the distinction between FP and NFP hospitals. That is the reason that we focus on the distinction between public and private. However, if indicated in the included studies, we also differentiate our results between FP and NFP private hospitals.
Our review contributes in 3 ways: (1) to map available literature and to highlight knowledge voids, (2) to identify differences between private and public provisions, and, finally, (3) to find institutional and health care system related drivers for differences in efficiency, accessibility, and quality of care.
2. METHODS
2.1. Definitions
Public hospitals can be either state owned or fully run by public entities; private ownership can be mission driven (NFP) or return driven (FP).10 The term “private” hospitals will be used as an encompassing term throughout this paper, making no distinction between NPF and FP. To compare public and private hospitals, this review will investigate 3 umbrella outcomes: (1) efficiency, (2) accessibility, and (3) quality of care. Efficiency holds the notion as the extent to which objectives are achieved in relation to the resources consumed.11 This includes both productivity measures on the basis of frontier analysis or other regression‐based approached, efficiency ratios (eg, employment ratios), and other efficiency outcomes such as length of stay (LOS) or responsiveness to demand. The most applied productivity methods are the stochastic frontier analysis (SFA) and the data envelopment analysis (DEA).1, 12 Efficiency measures are reflected in multiple indicators such as technical efficiency (maximum output from a given set of inputs or a minimum set of inputs with a given set of outputs), cost efficiency (technical efficiency accounting for the input price), scale efficiency (when the size of the unit is at its optimum), and/or allocative/profit efficiency (cost minimization or profit maximization).13 Accessibility is categorized into financial affordability, physical access, informed access, and timely access (eg, waiting times).14 Quality of care is structured along the lines of the Donabedian model of structure, process, and outcomes.15 Some studied indicators, such as LOS, can be classified under different domains within the Donabedian framework. On the basis of consultations during 2 expert meetings, such indicators were classified towards the most suitable domain. Another difficulty arises with practice variation. To illustrate, does a high rate of surgical interventions indicate better or poor quality of care? To avoid the complex discussion on practice variation and the ambiguous relationship with quality of care, this review does not look into variation in practices.
2.2. Realist review
Our study follows a realist review approach. A realistic review is suited to review interventions that are embedded in complex systems, whereby outcomes are dependent and influenced by their contexts.16 Rationales and drivers behind the implementation or growth of the private sector are diverse. Because of the peculiar nature of our “intervention,” minor deviations from the realist review protocol were necessary (ie, no explicit distinction is made between intervention, context, and mechanism). This review limits its territory to the EU (28 countries), because the EU countries are, to a certain extent, comparable but have various health care systems. The variety of health care systems can be used to explore how private hospitals perform within various settings. We strive towards a review that “delivers illumination rather than generalizable truths and contextual fine‐tuning rather than standardization.”16 (p24) Hence, the empirical findings are embedded within descriptive context.
2.3. Search strategy
The review was conducted from August to October 2015 and updated in June 2017. Data management was done by using Mendeley and Excel. Four databases were searched: Scopus, SocINDEX, Web of Science, and EconLit. Grey literature was excluded. The searches in the relevant databases were updated in June 2017. Different search terms were tested before the actual selection of the articles, to reassure the quality and relevance of the included hits. Table 1 shows the search terms in a simplified manner; in Table A1, the complete search string is given.
Table 1.
Search terms in abstract, keywords, and title (simplified)
| Intervention: private hospital OR privatization OR public‐private hospital, OR hospital ownership OR for‐profit hospital |
| Outcome: efficiency OR health care quality OR health care accessibility OR hospital admission OR patient admission OR health care delivery OR affordability OR health care utilization OR health care availability |
| AND NOT: job satisfaction OR Medicare in keywords (for <2008, United States in Keywords) |
| Limitations: Journal articles in English after 2000 |
2.4. Selection process
Figure 1 shows the flow chart of the review process. Only research after 2000, conducted in the EU and articles written in English, were included. Papers were included by matching them with the 5 Population, Intervention, Comparison, Outcome and Study Design (PICOS) criteria (Table 2). To safeguard quality and limit selection bias, the full‐text and appraisal stage was performed by 2 reviewers.
Figure 1.
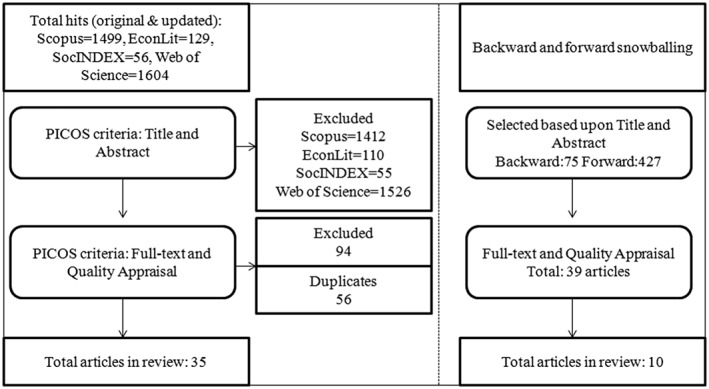
Flow chart of selection process
Table 2.
Inclusion criteria for the second phase
| Population | Private hospitals; this could be a nonprofit or for‐profit hospital. Papers that include private hospitals as a control variable are also considered to be eligible. |
| Intervention/exposure | Patients are exposed to the service delivery of private hospitals. |
| Comparison | A comparison should be made with public hospitals. |
| Outcome | One of the following 3 elements should be covered: efficiency, quality of care, and accessibility. Articles that only include employment conditions are not taken into consideration. |
| Study design | Empirical research, no descriptive papers or economic modeling are included. |
Articles were assessed using a standard format to appraise the quality of the studies (see Table A2). The main criteria for exclusion were as follows: (1) research designs were considered to be (extremely) weak and (2) poor reporting on the dataset and methodology, or no possibility of a critical appraisal. The 2 reviewers only included evidence, whereby the quality assessment demonstrated that the findings contributed to our research objective (in Table A3 the excluded references in quality appraisal phase). In total, 35 articles could be included.
A snowballing procedure was performed in December 2015 and January 2016. Forward snowballing identifies articles that refer to the selected articles in the review. Backward snowballing means that the reference list of the articles was included into the review process. Additionally, the literature selected in other systematic reviews covering the EU was included.1, 2, 12, 17, 18 Such a snowballing methodology has been assessed as a successful addition to the systematic review by advocates of realist reviews.16 Articles conceived to be useful upon the PICOS criteria went through the same inclusion process. In total, another 10 articles could be included, bringing the total number of studies to 45.
3. RESULTS
The selected articles are shown in summary tables in Table A4. Thirteen articles originated from Italy, 8 from Germany, 7 from the United Kingdom, 6 from France, 5 from Greece, 3 from Austria, 2 from Spain, and 1 from Portugal. While in Germany, Italy, France, and Austria most private hospitals act as a substitute for public hospitals, in the UK, Portugal, Spain, and Greece, most private hospitals do complement the public system.
3.1. Efficiency
We found 12 articles using productivity functions assessing primarily technical efficiency. 3 studies analyzing profit and/or cost efficiency, and 10 articles reflecting other efficiency measures (eg, LOS). The evidence on technical efficiency shows no unambiguous conclusion can be made that FP and NFP hospitals are more (cost and/or technical) efficient than public hospitals, although public hospitals seem to be just as efficient as or more efficient than private hospitals. The findings on the other efficiency measures indicate that private hospitals seem to be more responsive to (financial) incentives.
3.1.1. Productivity functions
The studies that estimated technical and/or cost efficiency use a DEA19, 20, 21, 22 or an SFA model.23, 24, 25, 26, 27 Other studies contrast multiple approaches, SFA versus DEA.28, 29, 30 The (adjusted) discharged patients23, 29 and the number of inpatient (weighted) cases were most often used as output parameters.20, 21, 24, 25, 30 Diagnosis‐related groups (DRGs),19, 22 outpatient visits,19 and differentiation of specific procedures (eg, number of complex surgery and emergency room treatments)27, 29 were used less frequently. Regarding input factors, most studies used the number of beds as a proxy for capital investments; one study used the amount spent on supplies as measurement of the capital used.20 To identify labor inputs, all studies incorporate the number of full‐time equivalents of physicians, nurses, and other staff members (eg, administrative, nonclinicians, and teaching staff); one study could not include full‐time equivalents, but only the number of staff members because of data limitations.27
Only the results on technical efficiency are grouped in Table 3, since this was the dominant outcome and enhances comparability. The findings show mixed results (Table 3), but do indicate more favorable results for public hospitals. Four German studies found that public hospitals were more efficient than FP hospitals.21, 28, 30 One possible explanation is that local governments sell the inefficient hospitals to the private sector.28 Also, German FP hospitals with over a thousand beds were found to operate more efficiently.21 In Italy, one study found that FP hospitals (Lazio Regio) were less technical efficient than public hospitals.27 Whereas when comparing NFP hospitals and public hospitals, the different methodologies and years covered caused divergent results.27 Three studies also concluded that NFP hospitals were less efficient in Germany.21, 24, 30 Berta et al23 reveal that Italian FP hospitals are less efficient than their public/nonprofit counterparts, but over time have converged towards the same efficiency level as other types. Similar converging results were found in Germany.25 NFP hospitals in Germany and Italy also show convergent efficiency scores according to a total of 4 studies.20, 22, 23, 29 Two studies, from Austria and Germany, reasoned that private providers are more efficient than public hospitals.19, 20 The German study analyzed the process of privatization, whereby hospitals that converted to FP status also increased their efficiency. This indicates that a longitudinal design might show different results than cross‐sectional designs. Hospitals that converted to NFP status initially also show increases in efficiency; however, these diminish over time.20 In the case of Portugal, one study concludes that private hospitals were more cost‐efficient than their public counterparts.26 Using a different methodology—nonoriented super efficiency and different sample selections—no difference in efficiency was found.22
Table 3.
Overview technical efficiency of private hospitals compared with public hospitals
| Less Efficient | No Difference | More Efficient | |
|---|---|---|---|
| FP | 5 studies from Germany and Italy find private FP hospitals less efficient than public hospitals21, 24, 27, 28, 30 | 2 studies from Germany and Italy find no difference between private FP and public hospitals23, 25 | 1 study from Germany finds private FP hospitals to be more efficient than public hospitals20 |
| NFP | 3 studies from Germany find private NFP hospitals to be less efficient than public21, 24, 30 | 4 studies from Germany and Italy find no difference between private NFP and public hospitals20, 22, 23, 29 | 1 study from Austria finds private NFP hospitals to be more efficient than public hospitals19 |
Abbreviations: FP, for‐profit; NFP, not‐for‐profit.
The overarching message in most studies might actually be the fact that reimbursement schemes are of importance. In Italy, FP hospitals were found to be less efficient because they use resources less efficiently. This might be due to the fact that private FP hospitals are confronted with specific regulations that set a limit to the number of funded admissions; since such limits fluctuate over time and are quite volatile, FP hospitals might face problems to adjust fixed input resources accordingly.27 Another indication of the importance of funding schemes might be the fact that after a DRG‐based payment system had been introduced in Italy, NFP hospitals converged to the same levels of technical efficiency as public hospitals.29 In Germany, Herr et al25 also found no statistically significant differences in technical efficiency between FP and public hospitals after a DRG‐based payment system had been introduced in 2004. Earlier, Herr24 showed that private hospitals were on average less cost and technical efficient, maybe because of the fact that in that timeframe, there existed an incentive to increase LOS to raise revenues. Nonetheless, FP hospitals were found to be more profit efficient than public hospitals, meaning that hospitals have certain output prices and input prices, and FP hospitals choose the best combination of both input and output factors.25 However, another study discovered that under the DRG payment system, efficiency gains among FP‐privatized hospitals were significantly lower compared with before the DRG payment system.20 The Austrian DRG system only covers up to 50% of hospital costs, and additional funds come from states and operational‐deficit coverage, determined ex post by the local authorities. Such funds disproportionally accrue to public providers placing the private sector at bay, but possibly also increasing their incentives to operate more cost conscious.19
3.1.2. Other efficiency outcomes
A subset of studies do use other outcomes to assess the efficiency of hospital providers. Multiple studies analyze the relationship between ownership and LOS (Table 4). A short case‐mixed LOS is seen as an indicator of superior efficiency. French private hospitals have longer LOS for knee procedures, but shorter LOS for hip procedures.31 For most diagnostic groups, there exists no difference in LOS between UK public hospitals and private independent sector treatment centers (ISTCs), although for some treatments, particularly hip and knee procedures, a longer LOS was found for National Health Service (NHS) hospitals.32 Another study using the same dataset as the former study supports the latter findings, whereby LOS in ISTCs is shorter than in public hospitals for hip replacements.33 Evidence from Italy reports shorter LOS in private hospitals for aortic valve substitution.34 However, LOS was found to be longer in Italian private psychiatric hospitals.35 The authors explain this by private psychiatric hospitals being funded on a per diem basis, creating incentives to increase LOS. Indeed, in Greece, LOS was also higher in private mental health clinics.36 This alludes to the assumption that FP providers seem to apply more revenue‐maximizing strategies. Overall, per diem funding structures—as in mental health—seem to increase LOS among private providers, while prospective structures as in acute care seem to create an opposing effect. Both underline the idea that the private providers respond more intensely to incentives than public hospitals. This is tested in a more head‐to‐head approach by Schwierz.37 The author identifies that the introduction of a new payment system in 2014 pushed for economic discipline and penalized high‐cost hospitals, creating incentives for German private hospitals to take over public hospitals.37 In general, FP hospitals were also found to respond faster to increasing demand than other ownership types. Public hospitals were more likely to default; therefore, privatization became an appealing option.37 Another study, also conducted in Germany, analyzes changes in hospital staff after privatization. This study discovers that FP privatization reduced staff per inpatient case (especially nurses, other nonphysician clinical staff, and other nonclinical staff). Such findings were not found when NFP hospitals were the acquiring party.38 Similar finding was found in Greece; FP hospitals seem to have lower nursing staff rates for nurses compared with the public hospitals.36
Table 4.
Other efficiency measures
| Outcome/Indicator | Number of Studies | Type (Private) | Countries | Impact |
|---|---|---|---|---|
| LOS | 3 | Aortic valve substitution, hip and knee procedures in private hospitals or ISTCs | Italy, United Kingdom, France | Private hospitals have shorter LOS |
| 3 | Private (ie, psychiatric hospitals, mental health clinics) hospitals and specifically for knee procedures | Italy, Greece, France | Private hospitals have longer LOS | |
| 1 | ISTCs (for most diagnostic groups) | United Kingdom | No difference | |
| Responsiveness to demand | 1 | FP | Germany | Public hospitals are less responsive |
| Employment | 1 | NFP | Germany | No difference |
| 2 | FP | Germany, Greece | Lower staff rate | |
| Upcoding | 1 | NFP + FP | Italy | Public hospitals have less “upcoding” |
| 1 | NFP + FP | Italy | No difference |
Abbreviations: ISTCs, independent sector treatment centers; FP, for‐profit; LOS, length of stay; NFP, not‐for‐profit.
Finally, 2 studies addressed upcoding. In Italy, Vittadini et al39 looked at registering patients with nonexisting complications to increase reimbursement. There was evidence that both NFP and FP hospitals were to some extent engaged in “upcoding” before a specific law against upcoding in 2007 was institutionalized. No such evidence was found for public hospitals.39 Berta et al23 also found that during 2003 to 2005, FP hospitals had more intense upcoding practices than other hospital types. However, no ownership differences were found after 2005, probably because of more severe checks implemented after 2003.23
3.2. Accessibility
Included articles examine 11 different indicators of accessibility (Table 5). Most included studies do raise concerns about accessibility to private hospitals; most of them flag this issue by analyzing the complexity of the cases and various patients' characteristics. In many countries, private providers do target higher socioeconomic classes, often through parallel private insurance. High‐income patients hold better access to private hospitals and that waiting times in the private sector are lower.
Table 5.
Accessibility indicators overview
| Concept | Number of Studies | Outcome/Indicator | Type (Private) | Countries | Impact |
|---|---|---|---|---|---|
| Affordable | 8 | SES of patients (eg, employment status, residents from deprived versus affluent region) | Private (ie, maternity, psychiatric), ISTCs | Italy, United Kingdom, Greece, Spain | Public hospitals perform better |
| 2 | Method of payment (ie, private health insurance and pay out‐of‐pocket) | Private | Greece | ||
| 1 | Payment per discharge | FP | Greece | ||
| Physical | 3 | Case‐mix differences (eg, cream skimming) | FP, ISTCs | Italy, UK | |
| 1 | Access to specialty care (ie, adjusted rates of revascularization) | Private | France | ||
| 1 | Admission pattern | Private psychiatric | Italy | ||
| 1 | Access to preemptive registration | FP | France | ||
| 1 | Regional physical mobility (number of nonresident patients in the region admitted) | Private | Italy |
| Physical | 1 | Mean expenditure and usage of drugs | FP | France | No difference |
|---|---|---|---|---|---|
| Affordable | 1 | Access to specialty care (ie, ambulatory care services) | Private | France | Private hospitals perform better |
| 1 | Method of payment (ie, informal payment) | Private | Greece | ||
| Physical | 1 | Chance op follow‐up treatment | Private psychiatric | Italy | |
| Timely | 1 | Waiting times | ISTCs | UK |
Abbreviations: ISTCs, independent sector treatment centers; FP, for‐profit; SES, socioeconomic status.
3.2.1. Affordable access
In the United Kingdom, patients of private ISTCs are less likely to coming from deprived residential areas.32, 40 One other study concludes that patients in private hospitals diagnosed with prostate cancer come from the more affluent regions.41 In Greece, monthly family income is positively related to private hospital admissions.42, 43, 44 In addition, both patients with private health insurance and rural residents are more likely to use private care services.44 Under comparable circumstances, FP hospitals generally charge more for admitted patients falling under the Greek Social Health Insurance fund.36 In Greece, more private patients had to pay out‐of‐pocket payments than in public hospitals. On the other hand, and maybe remarkably, “under‐the‐table” payments were lower in private hospitals.45
In Spain, private maternity units/hospitals proportionally treat more patients from higher socioeconomic backgrounds.46, 47 In private hospitals, the prevalence of cesarean sections was also higher among immigrants in comparison with natives; no such distinctions were found within public hospitals.47 In Italy, patient characteristics differ between private and public (psychiatric) hospitals. Older patients are less likely to be unemployed and make more use of private services.48
3.2.2. Physical access
Private hospitals are often accused of cream skimming and selecting more profitable patients. We found some illustrations to that suspicion. One Italian study argues that FP hospitals were more involved in cream skimming than both public or NFP hospitals.23 In the United Kingdom, ISTCs treat less complex NHS patients.32, 40 In France, a higher percentage of patients with ambulatory care sensitive conditions visit public hospitals in comparison with private hospitals, while the opposite appears for revascularization. The explanation is that in France, public and NFP hospitals account for most acute inpatient stays and FP hospitals provide half the total revascularizations procedures.49 Regarding a specific case from Italy, Preti et al50 detected that private psychiatric facilities were less likely to admit patients who attempted suicide prior to admission; this might serve as an indicator that high‐risk mental health patients are less able to access private services. Patients in private acute psychiatric inpatient clinics were also more likely to receive a follow‐up treatment (ie, rehabilitation and psychotherapy).48 Bonastre et al51 identified that in France, no significant differences exist between public and private hospitals in relation to the use of expensive drugs (anticancer drugs), after controlling for case mix. One French study investigated if hospital types differed in terms of access to renal (kidney) transplantation. The authors observe that FP hospitals were less likely to have patients on the preemptive registration list than (public) academic hospitals, corrected for case‐mix differences.52 Preemptive transplantation is associated with longer patient survival. Hence, patients in FP hospitals might be disadvantaged in access to such treatments. Regarding regional mobility, a study from Italy found that nonresident patients are more likely to be admitted to private hospitals compared with public hospitals when they could not gain access to care in their own region.34 The authors point out that this is of concern, since patients with financial resources can afford to be more mobile.34
3.2.3. Timely access
In the United Kingdom, shorter inpatient waiting times are associated with higher rates of private hospital beds.53
3.3. Quality of care
Quality of care encompasses many different aspects of health care. This is also reflected in the variety of outcome variables found in this review (Table 6). The quality of care studies are structured according to the Donabedian model of structure, process, and outcomes15 and show mixed results.
Table 6.
Quality of care indicators overview
| Concept | Number of Studies | Outcome/Indicator | Type (Private) | Country | Impact |
|---|---|---|---|---|---|
| Structure | 1 | Discontinuity of care | Private psychiatric | Italy | Public hospitals perform better |
| 1 | Qualification staff | FP | Greece | ||
| Process | 2 | Adherence guideline and screening | Private | Austria and Italy | |
| 1 | Appropriate admission | Private | Italy | ||
| Outcome | 2 | Mortality rate (avoidable mortality) | FP, private | France, Italy | |
| 1 | Rehospitalization rates | Private | France |
| Outcome | 1 | Patient's experiences | ISTCs | United Kingdom | No difference |
|---|---|---|---|---|---|
| Outcome | 3 | Mortality (risk of dying) | Private hospitals, NFP and FP | Germany, Italy | Private hospitals perform better |
| 1 | Readmission (likely to be readmitted in 30 days) | Private hospitals | Italy | ||
| 1 | Patients experience (regarding amenities) | ISTCs | United Kingdom |
Abbreviations: ISTCs, independent sector treatment centers; FP, for‐profit; NFP, not‐for‐profit.
3.3.1. Structure
Kondilis et al36 find that FP hospitals in Greece seem to have less qualified compared with the public hospitals. One of the possible explanations given by the authors is that FP hospitals might maximize profits and therefore minimize expenses on nursing staff. Another possible explanation is that FP hospitals use nursing staff more efficiently than public facilities. In Italy, private psychiatric clinics collaborated less intensely with the community system as public psychiatric departments do.48
3.3.2. Process
From discharge data extracted from Emilia‐Romagna hospitals, the appropriateness of admission was evaluated. Although the number of inappropriate admissions decreased between 2001 and 2005, private hospitals exhibit in all years more inappropriate admissions than public hospitals.54 Private hospitals are also showing less adherence to antenatal screening among pregnant women in 6 Italian regions.55 A study on Austrian hospitals shows that adherence to the guidelines for colorectal cancer screening was worse among private hospitals. After the implementation of a guideline for colorectal screening, only 3.8% of private hospitals changed their routine practice versus 14.2% of public hospitals.56
3.3.3. Outcomes
In Germany, Tiemann and Schreyögg21 analyzed hospital mortality rates. They found that, controlling for case‐mix differences, FP and NFP hospitals showed better mortality figures than the public sector. One of the potential explanations for this finding might be that publicly enforced transparency on quality indicators seems to have stimulated FP hospitals to put comparatively more emphasis on such issues.
France was the country were the 2 included studies on quality outcomes indicated a consistently worse performance for the private sector. Mortality rates for patients aged over 35 and admitted for heart attacks were found to differ among hospital types. Public (nonteaching) hospitals have a lower mortality rates compared with FP hospitals.57 Rehospitalization rates, a possible indicator for worse quality, differ as well between French hospitals. Private hospitals have higher rates of 30‐day all‐cause rehospitalizations of older patients compared with public providers.58
In Italy, regional degrees of privatization (1993‐2003) are used as a quasinatural experimental design to investigate the association between public and private hospitals spending on (the reduction of) avoidable mortality. Spending increases on public delivery of health care services was associated with increased reduction in avoidable mortality. However, no such positive effects were found with respect to spending increases on private health care services. This implies that increases of spending on private health care services might hamper the possible reduction in avoidable mortality by investments in the public sector.59 Contrary results indicate that patients in private hospitals are less likely to be readmitted and less likely to die within 30 days after discharge, although the impact of the latter was found to be much lower.60 This corresponds to the results of a multilevel analysis, also from Italy, which assessed that the risk of dying was significantly less in private hospitals.61
Both Pérotin et al62 and Owusu‐Frimpong et al63 examine UK patient experiences. The latter study finds that users of ISTCs have higher satisfaction rates than the users of public facilities for amenities, for instance, obtaining attention from doctors.63 However, Pérotin did not find a significant difference on the reported overall patient experiences between public and private clinics. Differences that were found seemed to relate to other variables such as patient characteristics.62
4. DISCUSSION AND CONCLUSION
This review points to various messages. Findings on efficiency show mixed results, but do suggest that the public sector is at least as or more efficient as the private sector. Many papers mention that the institutional context might be an important constraint for the efficiency for the private sector. For example, Austrian NFP hospitals seem to be “induced” to operate with high levels of operational efficiency. There exists quite some evidence that the private sector seems more sensitive to incentives than the public sector. This was shown for a range of indicators such as responding to changes in demand, upcoding, or adjusting LOS. Differences in LOS seem to depend on type of treatment, whereby consistent evidence shows the private sector has shorter LOS for hip procedures compared with the public sector and type of payment: Per diem funding increases LOS in private settings more than in public surroundings, especially for mental health. As expected, in South European countries and also in the United Kingdom where a parallel and partly duplicate system exists between private and public provisions, the private sector is used by the more affluent population, who may experience, for example, lower waiting times and better amenities. This suggests that universal access and a broader inclusion of private providers in the mainstream health system might be an important option to reduce such disparities in access. The same goes for cream‐skimming, which, although higher in private hospitals, might be prevented by sophisticated case‐mix corrections in the payment structures. Private hospitals may perform better on observable quality outcomes such as for example exist in Germany and Italy for mortality and readmissions. In France, private hospitals specialize in certain (elective) procedures. One might expect better outcomes for private hospitals as a result of such specializations, but in France, the findings predominantly seem to favor public hospitals. This casts doubt on the advantages of private hospital specialization.
This realist review analyzes a complex and context‐dependent issue and thus is subject to various limitations. Included studies used a wide range of indicators; research designs vary substantially. This makes it somewhat problematic to extrapolate or generalize these findings. Many findings relate to specific diseases and/or indicators implying they do not necessarily hold for a broader spectrum of diseases. Studies covering efficiency showed more consistency among their use of parameters and methodology. We also were able to only include studies from a limited number of EU countries. Most evidence compromises a few countries: Italy, Germany, France, the United Kingdom, and Greece. However, these 5 countries do cover for a substantial part of the total EU population and—more importantly—cover for most health care system types (tax‐funded or social insurance, multiple payer and single payer, and decentralized and more centralized). Including articles not written in English could broaden the scope of this research. Furthermore, transferability of our results from one country to another is a difficult and complex task.64 The performance of different types of hospital ownership may be highly dependent on their embeddedness in health system ecosystems. Indeed, private hospitals may compete, specialize, or complement public providers, which could partly explain conflicting outcomes. A more thorough understanding of the position of the private sector in the wider health system could aid policy makers in designing sound and evidence‐based policies in this area.
We provide policymakers with several take‐away messages. Firstly, the private hospital sector consists of many complex layers. Both a polarizing political debate and traditional economist reasoning towards the superiority of a regulated market also in health care do not suit the complexity of the issue. Secondly, our evidence shows that one should take a careful note to the incentives built into the health care systems, because they seem to be an important driver for either the divergence or convergence of the private and public sector. For‐profit providers seem to respond more intensely to incentives. Fine tuning such structure, eg, hospital payment systems, becomes even more important if the role of the private sector increases. Thirdly, despite popular opinion that enhancing the role of the private sector increases efficiency, we do not find a lot of evidence that supports this claim. Most evidence shows that public hospitals are as efficient as or more efficient than private counterparts. For Beveridge countries, we found that access to private hospitals is substantially worse for patients with either low incomes or a more complex case mix. Finally, this review highlights that policy “shopping” among research results is dangerous. The evidence on private sector performance should be critically assessed; research designs (ie, indicator specification, methodology, and sample selection) do cause divergent results between studies. Our assessment is that the supposed superior performance of the private sector—and especially the private nonprofit hospital sector—for Beveridge countries depends on full inclusion in the health system to guarantee broader access to the private sector.
Overall, this review could contribute to the discussion on the role of the private sector in providing hospital services in the EU and how different systems, institutions, and incentive structures might affect the public and private hospital sectors.
ETHICS STATEMENT
No ethical approval was required for this research, since this research is based on review of published literature.
ACKNOWLEDGEMENTS
This research was supported in part by a traineeship at the European Foundation for the Improvement of Living and Working Conditions during 2015 to 2016. The corresponding author participated in the project Delivering hospital services: A greater role for the private sector?, of which the final report has been published in January 2017, available from the Eurofound website at: http://www.eurofound.europa.eu/publications. The author would like to thank colleagues from Eurofound, especially Daniel Molinuevo and Jan Vandamme. Furthermore, my sincere gratitude to Prof Jonathan Skinner for his advice and to the participants in the expert workshops—organized by the European Foundation—held on November 4, 2015, in Brussels and on September 22, 2016, in Dublin by providing useful input.
All authors declare no conflict of interest.
APPENDIX A.
A.1.
Table A1.
Search string
| Scopus | |
|---|---|
| Before 2008 | |
|
Search in title, abstract, and key
Block 1: (private ‐within 2 words‐ hospital) AND efficiency OR “health care quality” OR “quality of health care” OR (health care ‐within 3 words‐ access*) OR “hospital admission” OR “patient admission” OR afford* OR “health care ‐within 3 words‐ delivery” OR “health care utilization” OR “health care availability” AND NOT “job satisfaction” OR Block 2: hospital AND privatization AND efficiency OR “health care quality” OR “quality of health care” OR (health care ‐within 3 words‐ access*) OR “hospital admission” OR “patient admission” OR afford* OR “health care ‐within 3 words‐ delivery” OR “health care utilization” OR “health care availability” AND NOT “job satisfaction” OR Block 3: (“public private*” ‐within 3 words‐ hospital) AND efficiency OR “health care quality” OR “quality of health care” OR (health care ‐within 3 words‐ access*) OR “hospital admission” OR “patient admission” OR afford* OR “health care ‐within 3 words‐ delivery” OR “health care utilization” OR “health care availability” AND NOT “job satisfaction” OR Block 4 “hospital ownership” AND efficiency OR “health care quality” OR “quality of health care” OR (health care ‐within 3 words‐ access*) OR “hospital admission” OR “patient admission” OR afford* OR “health care ‐within 3 words‐ delivery” OR “health care utilization” OR “health care availability” AND NOT “job satisfaction” Block 5 “for profit hospital” AND efficiency OR “health care quality” OR “quality of health care” OR (health care ‐within 3 words‐ access*) OR “hospital admission” OR “patient admission” OR afford* OR “health care ‐within 3 words‐ delivery” OR “health care utilization” OR “health care availability” AND NOT “job satisfaction” And no keywords “Medicare” OR “US” OR “United States” Limit to Journal, Article, English | |
| After 2008 | |
|
Search in title, abstract, and key
Block 1: (private ‐within 2 words‐ hospital) AND efficiency OR “health care quality” OR “quality of health care” OR (health care ‐within 3 words‐ access*) OR “hospital admission” OR “patient admission” OR afford* OR “health care ‐within 3 words‐ delivery” OR “health care utilization” OR “health care availability” AND NOT “job satisfaction” OR Block 2: hospital AND privatization AND efficiency OR “health care quality” OR “quality of health care” OR (health care ‐within 3 words‐ access*) OR “hospital admission” OR “patient admission” OR afford* OR “health care ‐within 3 words‐ delivery” OR “health care utilization” OR “health care availability” AND NOT “job satisfaction” OR Block 3: “public private*” ‐within 3 words‐ hospital) AND efficiency OR “health care quality” OR “quality of health care” OR (health care ‐within 3 words‐ access*) OR “hospital admission” OR “patient admission” OR afford* OR “health care ‐within 3 words‐ delivery” OR “health care utilization” OR “health care availability” AND NOT “job satisfaction” OR Block 4 “hospital ownership” AND efficiency OR “health care quality” OR “quality of health care” OR (health care ‐within 3 words access*) OR “hospital admission” OR “patient admission” OR afford* OR “health care ‐within 3 words‐ delivery” OR “health care utilization” OR “health care availability” AND NOT “job satisfaction” Block 5 “for profit hospital” AND efficiency OR “health care quality” OR “quality of health care” OR (health care ‐within 3 words‐ access*) OR “hospital admission” OR “patient admission” OR afford* OR “health care ‐within 3 words‐ delivery” OR “health care utilization” OR “health care availability” AND NOT “job satisfaction” | |
| And no keywords “Medicare” | |
| Limit to Journal, Article, English | |
| Search string: EconLit & SocINDEX | |
|
Search terms (AB “private w/2 hospital” OR AB (privatization AND hospital) OR AB “hospital ownership” OR AB “for profit hospitals” OR AB “public private w/3 hospital” OR AB “PPP w/3 hospital”) OR (SU (“private w/2 hospital” OR (privatization AND hospital) OR “hospital ownership” OR “for profit hospitals” OR “public private w/3 hospital” OR AB “PPP w/3 hospital”) |
Search Options Published Date: 20000101‐20151231 Source types Academic Journals and English |
| Search string: Web of Science | |
|
TS = “private hospital” OR TS = (privatization AND hospital) OR TS = “hospital ownership” OR TS = “for profit hospital” OR TS = “non profit hospital” OR TS = (“public private” AND hospital) OR TS = (PPP AND hospital) AND LANGUAGE: (English) AND DOCUMENT TYPES: (Article) |
Indexes = SCI‐EXPANDED, SSCI, A&HCI, ESCI Timespan = 2000‐2017 |
Table A2.
Quality appraisal form
| Component Ratings of Study: | Score | Justification/Comments |
|---|---|---|
| Strong = 3/Modest = 2/Weak = 1 | ||
| A) Design | ||
| Outcome of interest as main (3) or control variable (2/1)? | ||
| Cross‐sectional (2/1) or longitudinal (3) | ||
| Prospective (3) or retrospective (2/1) | ||
| Is the method of analysis appropriate? (strong, modest, weak) | ||
| Is the method of analysis sufficiently rigorous? (strong, modest, weak) | ||
| B) Quality of reporting | ||
| Enough data have been presented to show how the authors arrived at their findings (Strong, Modest, Weak) | ||
| Enough information is given what the methodological design is? (Strong, Modest, Weak) | ||
| Enough information is given where the data comes from and what the characteristics are of the sample (ie, summary statistics and sample sizes). (Strong, Modest, Weak) | ||
| C) Selection bias | ||
| Strong: The selected individuals/hospitals are very likely to be representative of the target population | ||
| Moderate: The selected individuals/hospitals are at least somewhat likely to be representative of the target population | ||
| Weak: The selected individuals/hospitals are not likely to be representative of the target population | ||
| D) Confounders (ie, region, demographics) | ||
| Strong: will be assigned to those articles that controlled for most relevant confounders | ||
| Moderate: will be given to those studies that controlled for relevant confounders, but explicitly mentions that it missed some relevant confounders | ||
| Weak: will be assigned when the relevant confounders were not controlled for | ||
| E) Data collection methods | ||
| Strong: The data collection tools have been shown to be valid; and the data collection tools have been shown to be reliable | ||
| Moderate: The data collection tools have been shown to be valid; and the data collection tools have not been shown to be reliable or reliability is not described. | ||
| Weak: The data collection tools have not been shown to be valid or both reliability and validity are not described. | ||
| F) Outcome variable | ||
| The choice of measurement of the outcome variable (accessibility, quality of care efficiency) is valid? | ||
| Strong: Clear connection with 1 of the 3 concepts, and/or is generally accepted by scholars | ||
| Moderate: A couple of validity issues arise. The connection between the outcome variable and the concepts of interest is moderate (eg, only one disease is analyzed) | ||
| Weak: Serious concerns about how the outcome variable (1 of the 3 concepts) is measured | ||
| G) Number of hospitals | ||
| Strong: More than 10 hospitals are included in the analysis | ||
| Moderate: Between 3 and 10 hospitals are included in the analysis | ||
| Weak: Only 2 hospitals are compared | ||
| H) Context | ||
| Strong: Includes many different contexts/regions, high complexity in demographic characteristics | ||
| Moderate: Combines 2 or 3 different regions | ||
| Weak: One very specific region with specific characteristics | ||
| J) Independence | ||
| Is this an independent study? Yes (3) Debatable (2) No (1) | ||
| K) Drop‐outs—only if applicable | ||
| Strong: (If applicable: will be assigned when the follow‐up rate is 80% or greater). | ||
| Moderate (If applicable: will be assigned when the follow‐up rate is 60%‐79%). | ||
| Weak: (If applicable: will be assigned when a follow‐up rate is less than 60% or if the withdrawals and drop‐outs were not described). | ||
| Total score | ||
| Additional comments | Answers to comments | |
| Do the results seem to be valid? | ||
| Do the results seem to be reliable? | ||
| Are the results relevant? Does it fall within the scope of our research question? | ||
| Can the results be generalized? | ||
| In or out | If needed: justification | |
| Final judgment made based on the score and the additional comments | ||
Table A3.
Excluded references in quality appraisal
|
Browne, J., L. Jamieson, J. Lewsey, J. van der Meulen, L. Copley and N. Black (2008). “Case‐mix & patients' reports of outcome in Independent Sector Treatment Centres: comparison with NHS providers.” BMC health services research
8: 78. Caballer‐Tarazona, M., A. Clemente‐Collado and D. Vivas‐Consuelo (2016). “A cost and performance comparison of public private partnership and public hospitals in Spain.” Health Economics Review 6(1): 1‐7. Colais, P., L. Pinnarelli, D. Fusco, M. Davoli, M. Braga and C. A. Perucci (2013). “The impact of a pay‐for‐performance system on timing to hip fracture surgery: experience from the Lazio Region (Italy).” BMC health services research 13: 393. De Girolamo, G., A. Barbato, R. Bracco, A. Gaddini, R. Miglio, P. Morosini, B. Norcio, A. Picardi, E. Rossi and P. Rucci (2007). “Characteristics and activities of acute psychiatric in‐patient facilities: national survey in Italy.” The British Journal of Psychiatry 191(2): 170‐177. Grilli, R., P. Guastaroba and F. Taroni (2007). “Effect of hospital ownership status and payment structure on the adoption and use of drug‐eluting stents for percutaneous coronary interventions.” Canadian Medical Association Journal 176(2): 185‐190. Keong, N., D. Ricketts, N. Alakeson and P. Rust (2004). “Pressure sores following elective total hip arthroplasty: pitfalls of misinterpretation.” Annals of the Royal College of Surgeons of England 86: 174‐176. Kontodimopoulos, N., P. Nanos and D. Niakas (2006). “Balancing efficiency of health services and equity of access in remote areas in Greece.” Health policy (Amsterdam, Netherlands) 76: 49‐57. Mathoulin‐Pélissier, S., Y. Bécouarn, G. Belleannée, E. Pinon, A. Jaffré, G. Coureau, D. Auby, J.‐L. Renaud‐Salis and E. Rullier (2012). “Quality indicators for colorectal cancer surgery and care according to patient‐, tumor‐, and hospital‐related factors.” BMC cancer 12: 297. Mossialos, E., S. Allin, K. Karras and K. Davaki (2005). “An investigation of caesarean sections in three Greek hospitals: the impact of financial incentives and convenience.” European journal of public health 15: 288‐295. Nemec, J., B. Meričková and J. Štrangfeldová (2010). “The ownership form of hospitals from the viewpoints of economic theory and slovak practice.” E a M: Ekonomie a Management 13: 19‐31. O' Herlihy, A., P. Lelliott, D. Bannister, A. Cotgrove, H. Farr and S. Tulloch (2007). Provision of child and adolescent mental health in‐patient services in England between 1999 and 2006. Psychiatric Bulletin. Papadaki, S. and P. Stankova (2016). “Comparison of horizontally integrated hospitals in private and public sectors of Czech Republic.” Economics and Sociology 9(3): 180‐194. Sellbrant, I., C. Pedroletti and J. G. Jakobsson (2017). “Pelvic organ prolapse surgery: changes in perioperative management improving hospital pathway.” Minerva Ginecologica 69(1): 18‐22. van Rompaey, B., M. M. Elseviers, M. J. Schuurmans, L. M. Shortridge‐Baggett, S. Truijen and L. Bossaert (2009). “Risk factors for delirium in intensive care patients: a prospective cohort study.” Critical Care 13(3). Vanhegan, I., A. Hakmi, N. De Roeck and A. Rumian (2015). “Effect of an independent‐sector treatment centre on provision of elective orthopaedic surgery in East and North Hertfordshire.” Annals of the Royal College of Surgeons of England 97(7): 519‐525. Wood, G. C. a. and C. Howie (2011). “Do waiting list initiatives discriminate in favour of those in a higher socioeconomic group?” Scottish Medical Journal 56: 76‐79. |
Table A4.
Summary of findings table (alphabetic order)
| Indicator | Methodology | Reliability Results | Generalizability Results | Year(s) Covered | Type (Private) | Country | |
|---|---|---|---|---|---|---|---|
| Efficiency | |||||||
| Barbetta et al29 | Technical | COLS, SFA, and DEA | Strong | Strong | 1995‐2000 | NFP | Italy |
| Barros et al26 | Cost | SFA | Moderate | Moderate | 1997‐2008 | NS | Portugal |
| Czypionka et al19 | Technical | Two‐stage DEA | Strong | Strong | 2010 | NFP | Austria |
| Daidone and D'Amico27 | Technical | SFA | Strong | Moderate | 2000‐2005 | FP + NFP | Italy |
| Gigantesco et al35 | LOS | Logistic regression | Weak | Strong | 2002‐2003 | Psych. | Italy |
| Tiemann and Schreyogg20 | Technical | Two‐stage DEA and Diff‐in‐Diff | Strong | Strong | 1996‐2008 | FP + NFP | Germany |
| Heimeshoff, Schreyögg, and Tiemann38 | Employment reduction | Diff‐in‐Diff and FE | Strong | Strong | 1996‐2008 | FP + NFP | Germany |
| Herr24 | Technical and cost | SFA | Strong | Strong | 2000‐2003 | FP + NFP | Germany |
| Herr, Schmitz, and Augurzky25 | Technical, cost and profit | SFA | Strong | Strong | 2002‐2006 | FP | Germany |
| Herwartz and Strumann28 | Technical | Two‐stage DEA + SFA | Strong | Strong | 1995‐2008 | FP + NFP | Germany |
| Lindlbauer and Schreyögg30 | Technical | Two‐stage DEA and SFA | Strong | Strong | 2000‐2010 | FP + NFP | Germany |
| Maravic and Landais31 | LOS | Linear multiple regression | Weak | Weak | 2001 | NS | France |
| Schwierz37 | Responsiveness to demand changes | IVs + FE | Strong | Strong | 1996‐2006 | FP + NFP | Germany |
| Siciliani et al33 | LOS | Quantile regression | Moderate | Weak | 2006‐2007 | NS | United Kingdom |
| Sommersguter‐Reichmann and Stepan22 | Technical | Super efficiency DEA | Strong | Strong | 2009‐2012 | NFP | Austria |
| Vittadini et al39 | Upcoding (by the LOS) | Diff‐in‐Diff and FE | Strong | Moderate | 2007‐2008 | FP + NFP | Italy |
| Accessibility | |||||||
| Barbiere et al41 | Utilization by socioeconomic status | Multivariate logistic regression | Moderate | Weak | 1998‐2006 | ISTC | United Kingdom |
| Biro and Hellowell53 | Waiting times | Region fixed effects | Moderate | Strong | 2000‐2001 & 2008‐2009 | ISTC | United Kingdom |
| Bonastre et al51 | Mean expenditure and usage chemotherapy | Multilevel analysis | Strong | Strong | 2008 | FP | France |
| Gusmano et al58 | Avoidable hospitalization | Multilevel analysis | Strong | Strong | 2004‐2008 | NS | France |
| Mason et al40 | Patient complexity | Mean difference by HRG | Moderate | Low | 2005‐2006 & 2006‐2007 | ISTC | United Kingdom |
| Pappa et al42 | Utilization by socio economic status | Multivariate logistic | Moderate | Low | 2003 | NS | Greece |
| Preti et al50 | Admission after suicide | Multivariate logistic | Moderate | Low | 2004 | Psych. | Italy |
| Riffaut et al52 | Access to preemptive registration on the waiting list | Multilevel analysis | Strong | Low | 2008‐2012 | FP | France |
| Río et al46 | Utilization by socioeconomic status | Logistic regression | Low | Moderate | 2005‐2006 | NS | Spain |
| Salvador et al (2009) | Utilization by socioeconomic status | Logistic regression | Low | Low | 1993‐2003 | NS | Spain |
| Siskou et al43 | Utilization by socioeconomic status and rural versus urban citizens | Stratified survey‐logistic regression | Low | Moderate | 2005 | NS | Greece |
| Souliotis et al45 | Utilization by socioeconomic and out‐of‐pocket payment | Descriptive statistics based upon a stratified sample | Weak | Moderate | 2011‐2012 | NS | Greece |
| Tountas et al44 | Utilization by socioeconomic status | Multivariate logistic analysis | Weak | Moderate | 2006 | NS | Greece |
| Quality of care | |||||||
| Berta et al61 | Mortality rate | Multilevel | Strong | Weak | 2009 | NFP | Italy |
| Britto‐Arias et al56 | Adherence guideline in colorectal cancer screening | Cohort study, relative frequencies with confidence intervals | Weak | Moderate | 2007‐2013 | NS | Austria |
| Gobillon and Milcent57 | Mortality rate | Survival analysis: cox model | Strong | Moderate | 1998‐2003 | FP | France |
| Gusmano et al58 | Rehospitalization rates | Step by step regression models | Moderate | Moderate | 2010 | NS | France |
| Louis et al54 | Inappropriate medical admissions | Descriptive statistics | Weak | Weak | 2001‐2005 | NS | Italy |
| Moscone et al60 | Readmission and death within 30 days | Multivariate OLS regression | Moderate | Weak | 2005‐2007 | NS | Italy |
| Owusu‐Frimponget al63 | Patient satisfaction on accessibility | Mixed method: semistructured interviews + cross‐sectional survey using ANOVA | Weak | Weak | X | NS | United Kingdom |
| Pérotin et al62 | Patients experience | Two‐stage switching regression model (incl. fixed effects) | Strong | Moderate | 2007‐2008 | ISTC | United Kingdom |
| Quercioli, Messina, Basu, McKee, Nante, and Stuckler59 | Avoidable mortality | Region‐specific fixed effects | Strong | Strong | 1993‐2003 | NS | Italy |
| Stroffolini et al55 | Compliance to the antenatal hepatitis B screening program | Multivariate logistic regression based upon a survey | Weak | Weak | 2001 | NS | Italy |
| Multiple dimensions: accessibility, quality of care, and/or efficiency | |||||||
| Preti et al48 | Characteristics of patients, patterns of care, and discharges | Chi‐square or Fischer exact test | Weak | Weak | Data collection 2001‐2005 | Psych. | Italy |
| Berta et al23 | Cream skimming, readmission technical efficiency | SFA | Moderate | Strong | 1998‐2007 | FP + NFP | Italy |
| Fattore et al34 | Regional physical mobility, LOS | Logistic regression + multilevel | Strong | Strong | 2009 | NS | Italy |
| Kondilis et al36 | Bed capacity, occupancy rate, nursing staff rate, LOS, and payment per discharge | Confidence interval analysis | Weak | Moderate | 2001‐2003 | FP | Spain |
| Street et al32 | Patients from deprived versus affluent regions, LOS | Within‐HRG differences with t test | Weak | Weak | 2006/2007 | ISTC | United Kingdom |
| Tiemann and Schreyogg21 | Technical and controlled for mortality | Two‐stage DEA | Strong | Strong | 2002‐2006 | FP + NFP | Germany |
Abbreviations: ANOVA, analysis of variance; COLS, corrected ordinary least squares; DEA, data envelopment analysis; Diff‐in‐Diff, difference‐in‐difference; FE, fixed effect; FP, for‐profit; HRG, Healthcare Resource Groups; ISTC, independent sector treatment centers; IVs, instrumental variables; LOS, length of stay; NFP, not‐for‐profit; NS, not specified; OLS, ordinary least squares; Psych., (private) psychiatric hospitals; SFA, stochastic frontier analysis.
Kruse FM, Stadhouders NW, Adang EM, Groenewoud S, Jeurissen PPT. Do private hospitals outperform public hospitals regarding efficiency, accessibility, and quality of care in the European Union? A literature review. Int J Health Plann Mgmt. 2018;33:e434–e453. https://doi.org/10.1002/hpm.2502
Florien Kruse and Niek Stadhouders should be considered joint first author.
REFERENCES
- 1. Hollingsworth B. Non‐parametric and parametric applications measuring efficiency in health care. Health Care Manag Sci. 2003;6(4):203‐218. [DOI] [PubMed] [Google Scholar]
- 2. Sibbel R, Nagarajah B. Sind die privaten Krankenhausträger effizienter?–Ergebnisse aus der internationalen Literatur. Das Gesundheitswesen. 2012;74(06):379‐386. https://doi.org/10.1055/s-0031-1280844 [DOI] [PubMed] [Google Scholar]
- 3. Schlesinger M, Gray BH. How nonprofits matter in American medicine, and what to do about it. Health Aff. 2006;25(4):W287‐W303. https://doi.org/10.1377/hlthaff.25.w287 [DOI] [PubMed] [Google Scholar]
- 4. Eggleston K, Shen YC, Lau J, Schmid CH, Chan J. Hospital ownership and quality of care: what explains the different results in the literature? Health Econ. 2008;17(12):1345‐1362. https://doi.org/10.1002/hec.1333 [DOI] [PubMed] [Google Scholar]
- 5. Herrera CA, Rada G, Kuhn‐Barrientos L, Barrios X. Does ownership matter? An overview of systematic reviews of the performance of private for‐profit, private not‐for‐profit and public healthcare providers. PLoS One. 2014;9(12):1‐18. https://doi.org/10.1371/journal.pone.0093456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Horwitz JR, Nichols A. Hospital ownership and medical services: market mix, spillover effects, and nonprofit objectives. J Health Econ. 2009;28(5):924‐937. [DOI] [PubMed] [Google Scholar]
- 7. Jeurissen P, Duran A, Saltman RB. Uncomfortable realities: the challenge of creating real change in Europe's consolidating hospital sector. BMC Health Serv Res. 2016;16(2):15 https://doi.org/10.1186/s12913-016-1389-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Maarse H. The privatization of health care in Europe: an eight‐country analysis. J Health Polit Policy Law. 2006;31(5):981‐1014. https://doi.org/10.1215/03616878-2006-014 [DOI] [PubMed] [Google Scholar]
- 9. Arrow KJ. Uncertainty and the welfare economics of medical care. Am Econ Rev. 1963;53(5):941‐973. https://doi.org/10.1016/b978-0-12-214850-7.50028-0 [Google Scholar]
- 10. Saltman RB. Melting public‐private boundaries in European health systems. Eur J Public Health. 2003;13(1):24‐29. https://doi.org/10.1093/eurpub/13.1.24 [DOI] [PubMed] [Google Scholar]
- 11. Jacobs R, Smith PC, Street A. Measuring efficiency in health care: analytic techniques and health policy. Cambridge: Cambridge University Press; 2006. [Google Scholar]
- 12. Tiemann O, Schreyögg J, Busse R. Hospital ownership and efficiency: a review of studies with particular focus on Germany. Health Policy. 2012;104(2):163‐171. https://doi.org/10.1016/j.healthpol.2011.11.010 [DOI] [PubMed] [Google Scholar]
- 13. Coelli TJ, Rao DSP, O'Donnell CJ, Battese GE. An Introduction to Efficiency and Productivity Analysis. New York: Springer; 2005. [Google Scholar]
- 14. Dubois H, Anderson R. Impacts of the Crisis on Access to Healthcare Services in the EU. 2013. [Google Scholar]
- 15. Donabedian A. The quality of care: how can it be assessed? JAMA. 1988;260(12):1743‐1748. https://doi.org/10.1001/jama.1988.03410120089033 [DOI] [PubMed] [Google Scholar]
- 16. Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist review—a new method of systematic review designed for complex policy interventions. J Health Serv Res Policy. 2005;10(suppl 1):21‐34. https://doi.org/10.1258/1355819054308530 [DOI] [PubMed] [Google Scholar]
- 17. Hanratty B, Zhang T, Whitehead M. How close have universal health systems come to achieving equity in use of curative services? A systematic review. Int J Health Serv. 2007;37(1):89‐109. https://doi.org/10.2190/TTX2-3572-UL81-62W7 [DOI] [PubMed] [Google Scholar]
- 18. Torchia M, Calabrò A, Morner M. Public‐private partnerships in the health care sector: a systematic review of the literature. Publ Manag Rev. 2015;17(2):236‐261. https://doi.org/10.1080/14719037.2013.792380 [Google Scholar]
- 19. Czypionka T, Kraus M, Mayer S, Röhrling G. Efficiency, ownership, and financing of hospitals: the case of Austria. Health Care Manag Sci. 2014;17(4):331‐347. https://doi.org/10.1007/s10729-013-9256-9 [DOI] [PubMed] [Google Scholar]
- 20. Tiemann O, Schreyögg J. Changes in hospital efficiency after privatization. Health Care Manag Sci. 2012;15(4):310‐326. https://doi.org/10.1007/s10729-012-9193-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Tiemann O, Schreyögg J. Effects of ownership on hospital efficiency in Germany. BUR‐Bus Res. 2009;2(2):115‐145. https://doi.org/10.1007/BF03342707 [Google Scholar]
- 22. Sommersguter‐Reichmann M, Stepan A. The interplay between regulation and efficiency: evidence from the Austrian hospital inpatient sector. Socioecon Plann Sci. 2015;52:10‐21. https://doi.org/10.1016/j.seps.2015.09.001 [Google Scholar]
- 23. Berta P, Callea G, Martini G, Vittadini G. The effects of upcoding, cream skimming and readmissions on the Italian hospitals efficiency: a population‐based investigation. Econ Modell. 2010;27(4):812‐821. https://doi.org/10.1016/j.econmod.2009.11.001 [Google Scholar]
- 24. Herr A. Cost and technical efficiency of German hospitals: does ownership matter? Health Econ. 2008;17(9):1057‐1071. https://doi.org/10.1002/hec.1388 [DOI] [PubMed] [Google Scholar]
- 25. Herr A, Schmitz H, Augurzky B. Profit efficiency and ownership of German hospitals. Health Econ. 2011;20(6):660‐674. https://doi.org/10.1002/hec.1622 [DOI] [PubMed] [Google Scholar]
- 26. Barros CP, de Menezes AG, Vieira JC. Measurement of hospital efficiency, using a latent class stochastic frontier model. Appl Econ. 2013;45(1):47‐54. https://doi.org/10.1080/00036846.2011.579061 [Google Scholar]
- 27. Daidone S, D'Amico F. Technical efficiency, specialization and ownership form: evidences from a pooling of Italian hospitals. J Prod Anal. 2009;32(3):203‐216. https://doi.org/10.1007/s11123-009-0137-7 [Google Scholar]
- 28. Herwartz H, Strumann C. On the effect of prospective payment on local hospital competition in Germany. Health Care Manag Sci. 2012;15(1):48‐62. https://doi.org/10.1007/s10729-011-9180-9 [DOI] [PubMed] [Google Scholar]
- 29. Barbetta GP, Turati G, Zago AM. Behavioral differences between public and private not‐for‐profit hospitals in the Italian National Health Service. Health Econ. 2007;16(1):75‐96. https://doi.org/10.1002/hec.1143 [DOI] [PubMed] [Google Scholar]
- 30. Lindlbauer I, Schreyögg J. The relationship between hospital specialization and hospital efficiency: do different measures of specialization lead to different results? Health Care Manag Sci. 2014;17(4):365‐378. https://doi.org/10.1007/s10729-014-9275-1 [DOI] [PubMed] [Google Scholar]
- 31. Maravic M, Landais P. Usefulness of a national hospital database to evaluate the burden of primary joint replacement for coxarthrosis and gonarthrosis in patients aged over 40 years. Osteoarthritis Cartilage. 2006;14(6):612‐615. https://doi.org/10.1016/j.joca.2005.12.009 [DOI] [PubMed] [Google Scholar]
- 32. Street A, Sivey P, Mason A, Miraldo M, Siciliani L. Are English treatment centres treating less complex patients? Health Policy (Amsterdam, Netherlands). 2010;94(2):150‐157. https://doi.org/10.1016/j.healthpol.2009.09.013 [DOI] [PubMed] [Google Scholar]
- 33. Siciliani L, Sivey P, Street A. Differences in length of stay for hip replacement between public hospitals, specialised treatment centres and private providers: selection or efficiency? Health Econ. 2013;22(2):234‐242. https://doi.org/10.1002/hec.1826 [DOI] [PubMed] [Google Scholar]
- 34. Fattore G, Petrarca G, Torbica A. Traveling for care: inter‐regional mobility for aortic valve substitution in Italy. Health Policy. 2014;117(1):90‐97. https://doi.org/10.1016/j.healthpol.2014.03.002 [DOI] [PubMed] [Google Scholar]
- 35. Gigantesco A, de Girolamo G, Santone G, Miglio R, Picardi A. Long‐stay in short‐stay inpatient facilities: risk factors and barriers to discharge. BMC Public Health. 2009;9(1):1 https://doi.org/10.1186/1471-2458-9-306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Kondilis E, Gavana M, Giannakopoulos S, Smyrnakis E, Dombros N, Benos A. Payments and quality of care in private for‐profit and public hospitals in Greece. BMC Health Serv Res. 2011;11(1):1 https://doi.org/10.1186/1472-6963-11-234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Schwierz C. Expansion in markets with decreasing demand‐for‐profits in the German hospital industry. Health Econ. 2011;20(6):675‐687. https://doi.org/10.1002/hec.1624 [DOI] [PubMed] [Google Scholar]
- 38. Heimeshoff M, Schreyögg J, Tiemann O. Employment effects of hospital privatization in Germany. The European journal of health economics: HEPAC: health economics in prevention and care. 2014;15(7):747‐757. https://doi.org/10.1007/s10198-013-0520-1 [DOI] [PubMed] [Google Scholar]
- 39. Vittadini G, Berta P, Martini G, Callea G. The effect of a law limiting upcoding on hospital admissions: evidence from Italy. Empirical economics. 2012;42(2):563‐582. https://doi.org/10.1007/s00181-012-0548-6 [Google Scholar]
- 40. Mason A, Street A, Verzulli R. Private sector treatment centres are treating less complex patients than the NHS. J R Soc Med. 2010;103(8):322‐331. https://doi.org/10.1258/jrsm.2010.100044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Barbiere JM, Greenberg DC, Wright KA, et al. The association of diagnosis in the private or NHS sector on prostate cancer stage and treatment. J Public Health. 2012;34(1):108‐114. [DOI] [PubMed] [Google Scholar]
- 42. Pappa E, Niakas D. Assessment of health care needs and utilization in a mixed public‐private system: the case of the Athens area. BMC Health Serv Res. 2006;6(1):1 https://doi.org/10.1186/1472-6963-6-146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Siskou O, Kaitelidou D, Papakonstantinou V, Liaropoulos L. Private health expenditure in the Greek health care system: where truth ends and the myth begins. Health Policy. 2008;88(2–3):282‐293. https://doi.org/10.1016/j.healthpol.2008.03.016. Accessed Dec. [DOI] [PubMed] [Google Scholar]
- 44. Tountas Y, Oikonomou N, Pallikarona G, et al. Sociodemographic and socioeconomic determinants of health services utilization in Greece: the Hellas Health I study. Health Serv Manage Res. 2011;24(1):8‐18. https://doi.org/10.1258/hsmr.2010.010009 [DOI] [PubMed] [Google Scholar]
- 45. Souliotis K, Golna C, Tountas Y, Siskou O, Kaitelidou D, Liaropoulos L. Informal payments in the Greek health sector amid the financial crisis: old habits die last. Eur J Health Econ. 2016;17(2):159‐170. https://doi.org/10.1007/s10198-015-0666-0 [DOI] [PubMed] [Google Scholar]
- 46. Río I, Castelló A, Barona C, et al. Caesarean section rates in immigrant and native women in Spain: the importance of geographical origin and type of hospital for delivery. Eur J Public Health. 2010;20(5):524‐529. https://doi.org/10.1093/eurpub/ckq067 [DOI] [PubMed] [Google Scholar]
- 47. Salvador J, Cano‐Serral G, Rodriguez‐Sanz M, Lladonosa A, Borrell C. Inequalities in caesarean section: influence of the type of maternity care and social class in an area with a national health system. J Epidemiol Community Health. 2009;63(3):259‐261. https://doi.org/10.1136/jech.2007.071977 [DOI] [PubMed] [Google Scholar]
- 48. Preti A, Rucci P, Gigantesco A, et al. Patterns of care in patients discharged from acute psychiatric inpatient facilities. Soc Psychiatry Psychiatr Epidemiol. 2009;44(9):767‐776. [DOI] [PubMed] [Google Scholar]
- 49. Gusmano MK, Weisz D, Rodwin VG, et al. Disparities in access to health care in three French regions. Health Policy. 2013;114(1):31‐40. https://doi.org/10.1016/j.healthpol.2013.07.011 [DOI] [PubMed] [Google Scholar]
- 50. Preti A, Tondo L, Sisti D, Rocchi MB, De Girolamo G. Correlates and antecedents of hospital admission for attempted suicide: a nationwide survey in Italy. Eur Arch Psychiatry Clin Neurosci. 2010;260(3):181‐190. [DOI] [PubMed] [Google Scholar]
- 51. Bonastre J, Chevalier J, Van der Laan C, Delibes M, De Pouvourville G. Access to innovation: is there a difference in the use of expensive anticancer drugs between French hospitals? Health Policy. 2014;116(2):162‐169. https://doi.org/10.1016/j.healthpol.2013.11.006 [DOI] [PubMed] [Google Scholar]
- 52. Riffaut N, Lobbedez T, Hazzan M, et al. Access to preemptive registration on the waiting list for renal transplantation: a hierarchical modeling approach. Transpl Int. 2015;28(9):1066‐1073. https://doi.org/10.1111/tri.12592 [DOI] [PubMed] [Google Scholar]
- 53. Biro A, Hellowell M. Public‐private sector interactions and the demand for supplementary health insurance in the United Kingdom. Health Policy. 2016;120(7):840‐847. [DOI] [PubMed] [Google Scholar]
- 54. Louis D, Taroni F, Melotti R, et al. Increasing appropriateness of hospital admissions in the Emilia‐Romagna region of Italy. J Health Serv Res Policy. 2008;13(4):202‐208. https://doi.org/10.1258/jhsrp.2008.007157 [DOI] [PubMed] [Google Scholar]
- 55. Stroffolini T, Bianco E, Szklo A, et al. Factors affecting the compliance of the antenatal hepatitis B screening programme in Italy. Vaccine. 2003;21(11–12):1246‐1249. https://doi.org/10.1016/s0264-410x(02)00439-5. Accessed Mar [DOI] [PubMed] [Google Scholar]
- 56. Britto‐Arias M, Waldmann E, Jeschek P, et al. Forceps versus snare polypectomies in colorectal cancer screening: are we adhering to the guidelines? Endoscopy. 2015;47(10):898‐902. https://doi.org/10.1055/s-0034-1392328 [DOI] [PubMed] [Google Scholar]
- 57. Gobillon L, Milcent C. Evaluating the effect of ownership status on hospital quality: The key role of innovative procedures. Ann Econ Stat/Annales d'Economie et de Statistique. 2016;(121–122):161‐186. [Google Scholar]
- 58. Gusmano M, Rodwin V, Weisz D, Cottenet J, Quantin C. Comparison of rehospitalization rates in France and the United States. J Health Serv Res Policy. 2014:1355819614551849. doi:https://doi.org/10.1177/1355819614551849;(1):18‐25. [DOI] [PubMed] [Google Scholar]
- 59. Quercioli C, Messina G, Basu S, McKee M, Nante N, Stuckler D. The effect of healthcare delivery privatisation on avoidable mortality: longitudinal cross‐regional results from Italy, 1993–2003. J Epidemiol Community Health. 2013;67(2):132‐138. [DOI] [PubMed] [Google Scholar]
- 60. Moscone F, Tosetti E, Vittadini G. Social interaction in patients' hospital choice: evidence from Italy. J R Stat Soc A Stat Soc. 2012;175(2):453‐472. https://doi.org/10.1111/j.1467-985X.2011.01008.x [Google Scholar]
- 61. Berta P, Seghieri C, Vittadini G. Comparing health outcomes among hospitals: the experience of the Lombardy region. Health Care Manag Sci. 2013;16(3):245‐257. https://doi.org/10.1007/s10729-013-9227-1 [DOI] [PubMed] [Google Scholar]
- 62. Pérotin V, Zamora B, Reeves R, Bartlett W, Allen P. Does hospital ownership affect patient experience? An investigation into public‐private sector differences in England. J Health Econ. 2013;32(3):633‐646. https://doi.org/10.1016/j.jhealeco.2013.03.003 [DOI] [PubMed] [Google Scholar]
- 63. Owusu‐Frimpong N, Nwankwo S, Dason B. Measuring service quality and patient satisfaction with access to public and private healthcare delivery. Int J Pub Sect Manage. 2010;23(3):203‐220. [Google Scholar]
- 64. Goeree R, Burke N, O'Reilly D, Manca A, Blackhouse G, Tarride J‐E. Transferability of economic evaluations: approaches and factors to consider when using results from one geographic area for another. Curr Med Res Opin. 2007;23(4):671‐682. https://doi.org/10.1185/030079906X167327 [DOI] [PubMed] [Google Scholar]


