Abstract
Introduction
Comprehensive Behavioral Intervention for Tics (CBIT) has been shown to be efficacious for Chronic Tic Disorders (CTDs), but utilization is limited by a lack of treatment providers and perceived financial and time burden of commuting to treatment. A promising alternative to in-person delivery is Voice over Internet Protocol (VoIP), allowing for remote, real-time treatment delivery to patients’ homes. However, little is known about the effectiveness of VoIP for CTDs. Therefore, the present study examined the preliminary efficacy, feasibility, and acceptability of VoIP-delivered CBIT (CBIT-VoIP).
Methods
Twenty youth (8–17) with CTDs participated in a randomized, waitlist-controlled pilot trial of CBIT-VoIP. The main outcome was pre- to post-treatment change in clinician-rated tic severity (Yale Global Tic Severity Scale). The secondary outcome was clinical responder rate (Clinical Global Impressions – Improvement Scale), assessed using ratings of ‘very much improved’ or ‘much improved’ indicating positive treatment response.
Results
Intention-to-treat analyses with the last observation carried forward were performed. At post-treatment (10-weeks), significantly greater reductions in clinician-rated, [F (1, 18) = 3.05, p < 0.05, partial η2 = 0.15], and parent-reported tic severity, [F (1, 18) = 6.37, p < 0.05, partial η2 = .26] were found in CBIT-VoIP relative to waitlist. One-third (N = 4) of those in CBIT-VoIP were considered treatment responders. Treatment satisfaction and therapeutic alliance were high. Discussion: CBIT can be delivered via VoIP with high patient satisfaction, using accessible, low-cost equipment. CBIT-VoIP was generally feasible to implement, with some audio and visual challenges. Modifications to enhance treatment delivery are suggested.
Keywords: Tourette’s Disorder, Chronic Tic Disorders, Voice over Internet Protocol, web-based videoconferencing, web camera
Introduction
Chronic Tic Disorders (CTDs), including Tourette’s Disorder (TD) are associated with impairment in physical, psychological, social, and family functioning.1, 2 Medications can be effective, but bothersome side effects (e.g., weight gain, drowsiness, cognitive dulling) limit their use for many individuals, especially children.3 Habit reversal training (HRT), consisting of awareness training, competing response training, and social support is a viable non-pharmacological alternative treatment option for those who prefer a non-pharmacological approach or who cannot tolerate medication.4 Recently, HRT was combined with psychoeducation, function-based assessment and intervention, self-monitoring, relaxation training, and behavioral rewards into a treatment package known as Comprehensive Behavioral Intervention for Tics.5 The efficacy of CBIT was demonstrated in large, randomized-controlled trials with both children6 and adults7. Both CBIT and HRT are considered evidence-based treatments for tic disorders.8–10
Despite its efficacy, access to CBIT remains limited due to a lack of trained treatment providers and perceived financial and time burdens associated with travelling long distances to treatment visits.11 Videoconferencing (VC) is a possible method for overcoming these barriers. Traditional VC involves connecting patients with health professionals located in a hospital or clinic via specialty VC equipment and an internet connection.12 Himle and colleagues13 compared VC-delivered and face-to-face CBIT in a randomized trial of 20 children with CTDs. Results showed significant pre- to post-treatment reductions in clinician-rated tic severity for both VC and in-person modalities, with no significant outcome differences between the two. Likewise, treatment response rates were 80% and 75% in the VC and in-person groups, respectively, and both modalities were rated as highly acceptable to parents and children. Furthermore, parent and child-reported satisfaction and therapeutic alliance were high and undifferentiated between groups.13
Despite positive results, traditional VC has its own accessibility and utilization challenges. For example, VC requires specialized equipment and technological support that may not be readily available to many consumers, thus requiring patients to travel to a regional hospital or university setting.12 To overcome these barriers, some have begun to utilize VoIP, which allows providers at clinics to connect with patients in their homes using a personal computer, internet connection, web camera, and user-friendly software that can be downloaded from the internet.14, 15
Research evaluating psychological interventions delivered via VoIP has shown positive results for delivering therapy for a wide range of psychiatric disorders,16–20 but can be associated with some complications; including difficulties with (a) audio and video feed,17, 18, 20, 21–23 (b) interpretation of nonverbal cues,18,19 (c) ensuring patient and clinician treatment adherence,22 (d) homework nonadherence,18 (e) the therapeutic relationship,19 and (f) disruptions from family members.21 Still, VoIP has several potential benefits over VC, including the potential for greater treatment flexibility,22 generalizability of treatment gains,19 convenience,17, 20, 22 novelty,17, 21 and the ability to incorporate family members in treatment when needed.22
In the current controlled trial, the preliminary efficacy, acceptability, and feasibility of CBIT delivered via VoIP were examined by comparing CBIT-VoIP to waitlist (WL) in 20 children with CTDs.
Method
Participants
Participants (see Table 1) ranged from 8 to 16 years (M = 12.16, SD = 2.34) and were predominantly male (58%). Most (85%) participants had a diagnosis of TD, and 25% had at least one additional psychiatric diagnosis. Thirty-five percent of participants were on anti-tic medication. Participants resided an average of 87 miles away from the study site, a Tic Disorders Specialty Clinic.
Table 1.
Baseline Characteristics
| Characteristic | CBIT-VoIP (N = 12) |
Waitlist (N = 8) |
||
|---|---|---|---|---|
| Demographics | ||||
| Age (mean, SD) | 12.3 | 2.39 | 11.96 | 2.41 |
| WASI-Vocab T-score (mean, SD) | 60.0 | 9.32 | 59.13 | 9.42 |
| Male Gender (N, %) | 7 | 58.3% | 6 | 75% |
|
| ||||
| Ethnicity (N, %) | ||||
| Non-Hispanic | 12 | 100% | 8 | 100% |
|
| ||||
| Race (N, %) | ||||
| Caucasian | 11 | 91.7% | 8 | 100% |
| Biracial (African-American and Caucasian) | 1 | 8.3% | ||
|
| ||||
| On Tic Meds at Entry (N, %) | 4 | 25% | 3 | 37.5% |
| No medication | 8 | 75% | 5 | 62.5% |
| Alpha-agonist | 3 | 25% | 1 | 12.5% |
| Alpha-agonist + Antipsychotic | 1 | 12.5% | ||
| 2 Alpha-agonists + Antipsychotic | 1 | 8.3% | ||
| Antipsychotic + Anticonvulsant | 1 | 12.5% | ||
|
| ||||
| Two Parent Family Home (N, %) | 10 | 83.3% | 7 | 87.5% |
|
| ||||
| Highest Parent Education (N, %) | ||||
| High School Diploma | 1 | 12.5% | ||
| Technical School/Some College | 3 | 25% | 1 | 12.5% |
| College Graduate | 5 | 41.7% | 3 | 37.5% |
| Professional Degree | 4 | 33.3% | 2 | 25.0% |
|
| ||||
| Household Income (N, %) | ||||
| 40,001–60,000 | 3 | 25% | 2 | 25% |
| 60,001–80,000 | 2 | 16.7% | 1 | 12.5% |
| 80,001–100,000 | 2 | 16.7% | 3 | 37.5% |
| 100,000+ | 3 | 25% | 2 | 25% |
|
| ||||
| Diagnoses (N, %) | ||||
| Tourette’s Disorder | 9 | 75% | 8 | 100% |
| Chronic Motor Tic Disorder | 3 | 25% | ||
| Attention Deficit Hyperactivity Disorder | 2 | 16.7% | 2 | 25% |
| Oppositional Defiant Disorder | 1 | 12.5% | ||
| Obsessive-compulsive Disorder | 1 | 8.3% | ||
| Generalized Anxiety Disorder | 1 | 12.5% | ||
| Social Phobia | 1 | 8.3% | ||
| Separation Anxiety Disorder | 1 | 8.3% | ||
| Specific Phobia | 1 | 8.3% | ||
|
| ||||
| Special Education Services During Lifetime (N, %) | 3 | 25% | 2 | 25% |
|
| ||||
| Yale Global Tic Severity Scale (mean, SD) | ||||
| Total Score | 25.75 | 8.51 | 22 | 5.71 |
| Motor Subscale | 16.33 | 3.31 | 14.13 | 2.00 |
| Phonic Subscale | 9.42 | 6.13 | 7.88 | 5.33 |
| Impairment Scale | 31.25 | 9.16 | 31.75 | 6.27 |
Materials
Skype©, a peer-to-peer VoIP software application providing free web-based videoconferencing, and utilizing security features, including standard encryption algorithms and digital user authentication certificates, was used to deliver treatment24, 25 from a private clinic room, using a Dell© Optiplex GX 980 desktop computer with a 21.5 inch screen, Logitech© c270 web camera, and a high speed (54.0 megabytes per second) university-based local area network internet connection. The Skype© picture-in-picture feature was used in all sessions, so therapists and the independent evaluator (IE) could monitor their body positioning. In most cases, participants used their own home computer, high speed internet connection, and a web camera to connect with the therapist. For five families who did not previously own a web camera, a Logitech© c110 web camera ($20) was provided by the investigators. One web camera was loaned to a family that was excluded following the screening assessment, and there were no between-group differences in the number of families who borrowed one.
Measures
The Mini International Neuropsychiatric Interview – Kid (MINI-Kid)
The MINI-Kid26 is a brief structured diagnostic clinician-administered interview assessing psychiatric disorders and suicidality in children ages 6 to 17. It has high interrater and test-retest reliability; and convergent validity ranging from good to excellent.26
Wechsler Abbreviated Scale of Intelligence (WASI)
The WASI27 is a clinician-administered measure assessing intellectual functioning of individuals between the ages 6 and 89. It has good validity,28 good interrater and test-retest reliability,27 high internal consistency,29 and good concurrent validity.30 The vocabulary subtest was used in the present study.
Yale Global Tic Severity Scale (YGTSS)
The YGTSS31 is a clinician-rated tic severity scale assessing number, frequency, intensity, complexity, and interference. The measure yields independent 0–25 point subscores for motor and vocal tics, which are summed to a 0–50 point total tic severity scale. The scale also includes a 0–50 point tic-related impairment scale. The YGTSS has demonstrated acceptable psychometric properties; with good internal consistency and inter-rater reliability, as well as adequate convergent and divergent validity.31, 32 YGTSS ratings obtained via in-person and VoIP-administered interviews display high cross-modality agreement.33
Clinical Global Impression-Improvement Scale (CGI-I)
The CGI-I is a clinician-rated scale,34 adapted for use with patients with tic disorders.35 The CGI-I requires a clinician to provide a rating of improvement since baseline. Clinicians assess improvement using a 1 (very much improved) to 8 (very much worse) scale. By convention,6 a score of 1 or 2 (much improved) was used to identify treatment responders.
Parent Tic Questionnaire (PTQ)
The PTQ36 is a parent-report measure of child tic severity. The measure yields tic severity scores for motor tics, vocal tics, and a combined severity score for all tics. The PTQ has test-retest reliability in the good to excellent range, and superior internal consistency and convergent validity.36
Children’s Perception of Therapeutic Relationship (CPTR)
This 10-item, 5-point scale measures child perceptions of the therapeutic relationship.37 Total scores range from 10 to 50, with higher scores reflecting stronger therapeutic alliances. The measure shows satisfactory internal consistency and reliability.38
Client Satisfaction Questionnaire (CSQ)
This 8-item measure39 assesses client satisfaction with health services and programs. Total scores range from 8 to 32, with higher ratings indicating greater satisfaction. The CSQ has high internal consistency39, 40 and excellent concurrent validity.39, 41
Treatment Acceptability Questionnaire (TAQ)
The TAQ is a 6-item parent-report measure, modified from a questionnaire by Hunsley.42 It assesses treatment acceptability, ethics, and effectiveness; acceptability of treatment side effects, and therapist knowledge and trustworthiness. Total scores range from 6 to 42, with higher ratings indicating increased acceptance. The TAQ has good test-retest reliability, internal consistency and concurrent validity.42
Videoconferencing Satisfaction Questionnaire (VSQ)
This 14-item questionnaire, adapted from a Telemedicine Satisfaction Questionnaire,43 assesses patient satisfaction with the VC modality. Total scores range from 14 to 70.
Design
Patients were randomized to CBIT or WL using Random Allocation Software, Version 1.0.44 Groups were stratified with respect to medication status and gender. Families were informed of group assignment via phone after baseline. The IE was blinded to assignment. To maintain the blind, assessment and treatment staff were separated, and children and parents were instructed to avoid disclosing treatment assignment to the IE.
Procedure
Participants were recruited from December 2012 to August 2013 through solicitations mailed to health care professionals and newspaper advertisements posted in several major cities within the state. Families seeking standard services from the clinic were also invited to participate.
After obtaining verbal consent, a phone screening was conducted with 35 families to assess whether the patient met eligibility criteria. Inclusion criteria included (a) residence within the State (b) ages 8–17; (c) a DSM-IV-TR45 diagnosis of CTD or TD) (d) YGTSS Total Score > 14 and < 30 for TD or > 10 and < 20 for CTD; (e) unmedicated or on stable medication treatment for tics, Obsessive-Compulsive Disorder, Attention Deficit/Hyperactivity Disorder, anxiety, and/or depressive disorder for at least 6 weeks, with no planned changes for the duration of study participation; and (f) fluency in English. Exclusion criteria included (a) YGTSS Total Tic Severity Score > 30 for consistency with the original trial;6 for any score exceeding 30 on the YGTSS, the research team determined the appropriateness of the patient’s participation in the study); (b) WASI-Vocabulary subtest T-Score < 37; (c) DSM-IV-TR45 substance abuse or dependence or Conduct Disorder diagnosis within the past 3 months; (d) Lifetime DSM-IV-TR45 diagnosis of pervasive developmental disorder, mania, or psychotic disorder; (e) a serious psychiatric, psychosocial, or neurological condition requiring immediate treatment; (f) previous HRT for tics; (g) lack of a functional, and accessible home computer, and high speed (i.e., cable/DSL) internet connection; and (h) refusal to sign a release of information form for the child’s local primary care physician, mental health professional, or neurologist.
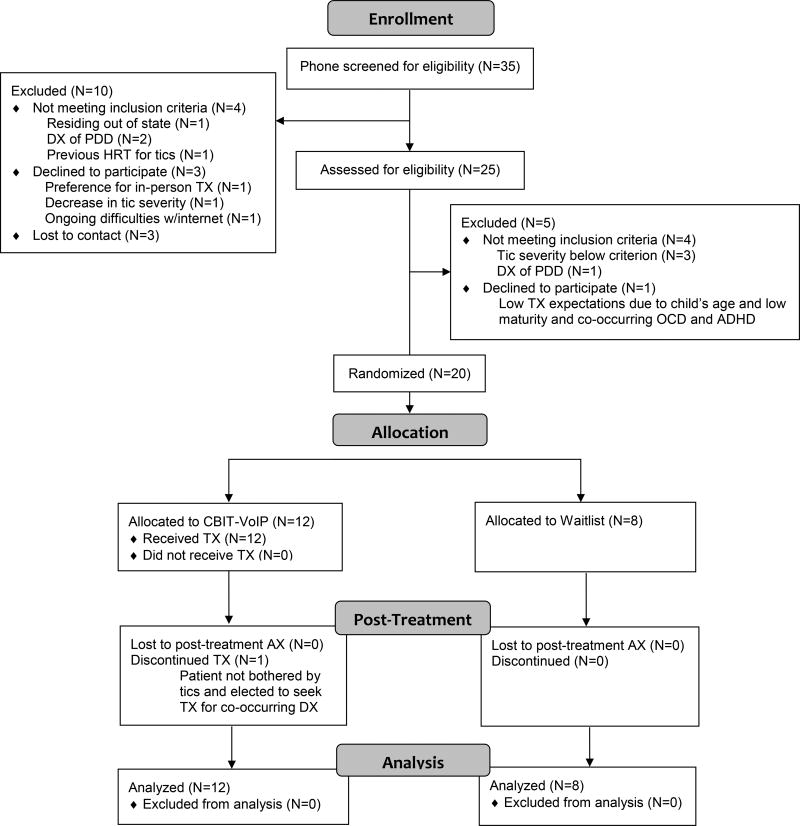
Of the 35 families phone screened, four were ineligible and six declined participation. See Figure 1 for a CONSORT flow diagram.46
Figure 1.
CONSORT diagram of participant flow through the trial. Diagram is based on template from Schulz, Altman, Moher, for the CONSORT group (2010).
Note. DX=diagnosis; PDD=Pervasive Developmental Delay; TX=Treatment; AX=Assessment
Assessment
Participants eligible following the phone screen (N = 25), underwent a 2-step screening process. A study staff member drove to the family’s home to obtain informed child assent and parental consent using Institutional Review Board-approved forms. Additionally, standard clinic consent and privacy paperwork were completed. The parent was also asked to provide demographic data, and their child’s treatment and medical history, and to rate their child’s tic severity using the PTQ. Participants then received on-site technical support for downloading and installing Skype© along with written instructions. Prior to departing, the study staff member tested the equipment to ensure the sound and video feed was functioning properly, and participants received a handout featuring guidelines on maintaining privacy, the limits of privacy, and the possibility of miscommunication due to technological difficulties during VoIP sessions. On the second day of screening, an assessment was conducted by the IE via Skype© from inside a private room in the clinic. During the screening assessment, the IE administered the MINI-Kid, YGTSS, and WASI-Vocabulary subtest.
Of the 25 who were screened via VoIP, 4 were ineligible and 1 was eligible but declined further participation (See CONSORT diagram; Figure 1). Eligible participants (N = 20) received a baseline assessment approximately 7 to 10 days later via Skype©, during which the IE re-administered the YGTSS, and the parent re-rated their child’s tic severity using an internet-based version of the PTQ through Qualtrics.47
Participants assigned to CBIT-VoIP completed the CPTR after their third treatment session. During the post-assessment, the IE re-administered the YGTSS and rated treatment response using the CGI-I. All parents completed the PTQ. Parents in the CBIT-VoIP group completed the TAQ, CSQ, and VSQ. Patients in the CBIT-VoIP group completed the CSQ and VSQ. Assessment sessions were digitally recorded for quality assurance purposes using Evaer© video recorder48 for Skype©. Participants were paid $25 for completion of the baseline assessment and $75 for completion of the post-assessment.
Training of Study Personnel
Treatment was delivered by four Master’s level therapists who were trained using the CBIT manual outlined by Woods and colleagues.5 Therapists were supervised weekly by the first author of the CBIT manual (DWW).
Prior to conducting assessments, the IE, a Master’s level doctoral student, was trained to established criteria by an off-site TD expert (i.e., MBH). The IE received weekly supervision from the lead author (EJR), an upper level doctoral student with 6 years’ experience in the administration of the main outcome measures.
Study Groups
CBIT-VoIP
CBIT-VoIP was delivered by a therapist located in a University-based Tic Disorders Specialty Clinic. Per the manual,5 both child and parent were required to be present for sessions, but this requirement was waived for mature older adolescents (i.e., 16 and older) at the therapist’s discretion (n=1). Treatment consisted of two 1.5-hour sessions followed by six 1-hour sessions occurring over a 10-week period. CBIT-VoIP incorporated HRT, psychoeducation about CTDs, self-monitoring of tics, function-based assessment and intervention, and diaphragmatic breathing and progressive muscle relaxation. Behavioral rewards (e.g., gift card to a toy store, trip to an amusement park), funded by the parent, were used to motivate treatment engagement.5
WL
Participants randomized to the WL group were placed on a waiting list to receive CBIT-VoIP following the end of the study period. Participants in this group met with the IE for baseline and post-treatment assessments as described above.
Results
Baseline Characteristics
Group differences in key baseline characteristics were examined using independent samples t-tests. No significant between-group differences were found for age [t (18) = −0.31, p = 0.76, two-tailed], WASI-Vocabulary T-score [t (18) = −0.21, p = 0.84, two-tailed], or YGTSS total severity score [t (18) = −1.10, p = 0.29, two-tailed]. Using chi-square tests for independence (with Yates Continuity Correction), no significant between-group differences were found in proportion of males and females, χ2 (1, n = 20) = 0.08, p = 0.77, phi = −0.17, Caucasian participants, χ2 (1, n = 20) = 0.00, p = 1.00, phi = −0.19, participants on tic meds, χ2 (1, n = 20) = 0.00, p = 1.00, phi = −0.04, diagnosis of TD, χ2 (1, n = 20) = 0.80, p = 0.37, phi = −0.34, or any comorbid condition, χ2 (1, n = 20) = 0.00, p = 1.00, phi = −0.04.
Of the 20 participants enrolled in the trial, 12 were randomized to CBIT-VoIP, and 8 were randomized to WL (see Figure 1). Ten participants in the CBIT-VoIP group (83.3%) received all 8 treatment sessions, and 1 participant (8.3%) completed treatment in 7 sessions. One participant (assigned to CBIT-VoIP) withdrew from the study after the first session due to a loss of interest in receiving treatment, yielding a 5% attrition rate across both groups.
Primary Outcomes
Results were analyzed using SPSS 21.0. To address missing data, intention to treat analyses with the last observation carried forward were performed for pre-post data. Missing values within scales were imputed using the scale or subscale item means. A series of 2×2 mixed analyses of variance were performed to determine whether there were significantly greater decreases in YGTSS total scores from baseline to post-treatment among participants in CBIT-VoIP relative to WL. Based on a priori hypotheses, significance was determined using one-tailed p-values. Effect sizes were estimated using partial eta squared, with benchmarks suggested by Cohen49 to define small, medium, and large effects, set at 0.01, 0.06, and 0.14, respectively.
For the YGTSS total scores, a significant main effect was found for time, F (1, 18) = 8.16, p < 0.01, partial η2 = 0.31. The main effect comparing CBIT-VoIP and WL groups was not significant, F (1, 18) = 0.11, p = 0.37, partial η2 = 0.01. A significant group × time interaction was found, F (1, 18) = 3.05, p < 0.05, partial η2 = 0.15. Paired samples t-tests were conducted on pre-post YGTSS total scores for both groups (see Table 2). Effect sizes were estimated using Cohen’s d with small, medium, and large effects set at 0.20, 0.50, and 0.80, respectively.49 In CBIT-VoIP there was a statistically significant decrease of 7.25 points in YGTSS total scores from baseline to post-assessment, t (11) = 3.11, p < .01, d = .90. In the WL group, the 1.75 point decrease on the YGTSS total scores from baseline to post-assessment, t (7) = 1.11, p = 0.15, d = 0.39 was not significant. Pre- and post-intervention means and standard deviations across all outcome variables are presented in Table 2. As can be seen in Table 2, differences in the total YGTSS scores were primarily driven by changes in motor tics.
Table 2.
Pre- and Post-treatment Means, Standard Deviations, and Effect Sizes
| CBIT-VoIP | Waitlist | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Pre (N = 12) | Post (N = 12) | d | Pre (N = 8) | Post (N = 8) | d | Partial η2 | ||||||
|
|
||||||||||||
| Measure | M | SD | M | SD | M | SD | M | SD | ||||
| YGTSS | ||||||||||||
| Total | 25.75 | 8.51 | 18.50 | 7.75 | .90** | 22.00 | 5.71 | 20.25 | 6.21 | .39 | .15* | |
| Motor | 16.33 | 3.31 | 12.08 | 3.48 | 1.07** | 14.13 | 1.96 | 13.13 | 2.90 | .42 | .19* | |
| Phonic | 9.42 | 6.13 | 6.42 | 5.89 | .57* | 7.88 | 5.33 | 7.13 | 4.79 | .15 | .18 | |
| Impairment | 31.25 | 9.16 | 20.83 | 8.08 | .94** | 31.75 | 6.27 | 28.00 | 7.11 | .67 | .12 | |
| PTQ | 40.17 | 19.94 | 21.75 | 20.07 | 1.38*** | 34.38 | 17.24 | 29.63 | 23.15 | .53 | .26* | |
Note:
p < .05;
p < .01;
p < .001
For YGTSS impairment scores, a significant main effect was found for time, F (1, 18) = 11.04, p < 0.01, partial η2 = 0.38. No significant main effect was found for the between group comparison, F (1, 18) = 1.71, p = 0.11, partial η2 = 0.09, nor for the group × time interaction, F (1, 18) = 2.45, p = 0.07, partial η2 = 0.12. Nevertheless, because the interaction trended toward significance, follow-up comparisons were conducted. Scores among the CBIT-VoIP group significantly decreased 10.42 points from baseline to post-assessment, t (11) = 3.26, p < 0.01, d = 0.94, whereas the 3.75 point decrease in YGTSS impairment scores found in the WL group was not significant, t (7) = 1.87, p = 0.05, d = 0.67.
For PTQ total scores, there was a significant main effect for time, F (1, 18) = 18.30, p < 0.001, partial η2 = 0.50, but not group, F (1, 18) = 0.01, p = 0.45, partial η2 = 0.001. The interaction between time and group was significant, F (1, 18) = 6.37, p < 0.05, partial η2 = 0.26. In the CBIT-VoIP group, PTQ total scores decreased 18.42 points from baseline to post-assessment, t (11) = 4.76, p < 0.001, d = 1.38, but the PTQ total score drop of 4.75 points from baseline to post-assessment, t (7) = 1.50, p = 0.09, d = 0.53, was not statistically significant.
A Chi-square test for independence was performed to determine if there was a significant difference between groups in the proportion of CGI-I-classified treatment responders. Results indicated a significantly higher proportion of treatment responders in CBIT-VoIP (33.3%) relative to waitlist (0%), χ2 (1, n = 20) = 0.33, p < 0.05, phi = 0.41 (one-tailed).
Treatment Acceptability
Parent-reported treatment acceptability questionnaire ratings (scale range = 6–42) were high (M = 39.27, SD = 3.85). Parent (M = 29.64, SD = 3.01) and patient (M = 29.64, SD = 3.07) ratings on the Client Satisfaction Questionnaire (scale range = 8–32) were also high. VC satisfaction (scale range = 14–70) was also high, with mean parent and patient ratings of 67.18 (SD = 3.63), and 65.27 (SD = 5.76), respectively. Satisfaction measures were completed only by those in the CBIT-VoIP group. Those in WL did not complete this measure after receiving treatment. The therapeutic alliance, as measured by the CPTR (scale range = 10–50) questionnaire, was moderately strong (M = 37.45, SD = 7.61).
VoIP Call Quality
The type and severity of VoIP technological difficulties were assessed by the therapist after each treatment session using the following qualitative ratings:50 ‘none’, ‘insignificant’ (difficulties present, but session quality not affected), ‘minimal’, ‘moderate’, ‘major’, and ‘severe’ (could not complete the session). Therapists also rated the type of technical difficulty (i.e., sound or video). Technological difficulties occurred in 37.6% of all therapy sessions, of which, more than half (56.3%) were coded50 as insignificant, 34.4% as minimal, and 12.5% as moderate. Of the sessions with technological difficulties, video quality issues (e.g., freezing, delays, blurriness, dropped calls) occurred in 68.8%, sound quality difficulties (e.g., echoing, delays, choppiness, difficulty hearing) occurred in 53.1%, and video was unable to be seen during part of 6.3% of sessions.
Therapist and Independent Evaluator Adherence
Twenty percent (N = 19) of treatment sessions were randomly selected for co-rating by an off-site expert (i.e., MBH) for adherence on a 1 to 4 scale, with higher ratings indicating greater adherence to the protocol. Two session recordings each were rated for 7 participants, with 1 viewed for each of the remaining 5 participants. The mean adherence rating was 3.26 (SD = 0.73). The off-site expert also co-rated 25% (N = 5) of videotaped IE assessment sessions for reliability. On average, the percent difference between the IE and expert rating was 7.86% (SD = 7.54%) – within the pre-set standard of 15% of the expert’s rating.
Discussion
The primary aim of the study was to examine the preliminary efficacy, acceptability, and feasibility of CBIT delivered via VoIP relative to a WL-control condition. Significantly greater pre-post reductions in clinician-rated tic severity were found in CBIT-VoIP relative to WL. Participants receiving CBIT-VoIP demonstrated a mean reduction in clinician-rated total tic severity (28.2%) similar to that observed in a previously conducted, large scale pediatric trial of face-to-face CBIT (30.8%).6 Results were also positive for parent-reported tic severity with greater pre-post reductions found in the treatment group relative to WL. Inconsistent with results of the original trial, between-group differences in clinician-rated tic-related impairment did not reach statistical significance. This may be attributable to a lack of statistical power or delayed effect of treatment on functioning.
Despite similarities between the present and previous studies on YGTSS and PTQ outcomes, the overall treatment response rate in the present study was lower. Although the proportion of treatment responders (33%) was found to be significantly greater in CBIT-VoIP compared to WL (0%), the response rate is considerably lower than what has been reported in trials incorporating in-person delivery (52.5%)6 and delivery via traditional VC (80%).13 The reason for this discrepancy is unclear, but the lower response rate may be attributed to the small sample size, differential outcomes between therapists, or technological difficulties with respect to audio and visual quality. Additionally, there may be some aspect of the VoIP modality (i.e., reduced time and travel efforts for families) that negatively influenced treatment adherence for some.
Treatment satisfaction, VC satisfaction, and therapeutic alliance ratings were high. Mean ratings on the TAQ (parent) were high and consistent with those found in CBIT delivered via traditional VC (35.5).13 Additionally, parents and children endorsed high general treatment satisfaction (CSQ) and VC satisfaction (VSQ). The therapeutic alliance (CPTR) was relatively strong.
Despite positive results, several concerns emerged with respect to the feasibility of VoIP-delivery of CBIT. Specifically, therapists experienced challenges performing specific treatment components due to limited web camera viewing range, and audio or visual difficulties. Additionally, difficulty viewing homework, homework nonadherence, and fluctuating parent and child focus (i.e., shifting parental attendance due to home-related disruptions; inattentiveness, and difficulty remaining seated for a few child patients) were also noted.
To counter these concerns, the following modifications are suggested. To improve visual range, both the patient and therapist may need to step or sit back from the computer screen to perform specific treatment components. To improve homework viewing, families could complete forms on the internet for direct viewing by the therapist. It is unclear whether homework adherence is a greater problem in VoIP relative to face-to-face CBIT; however, one way to address the issue is to use a website hosting web-based versions of homework forms, and set-up automated email reminders to complete assignments.
To address fluctuating parent and child focus, it will be important to preface future VoIP treatment with very clear expectations for patient and parent attendance and participation, including an emphasis on minimizing disruptions by family members not directly involved in treatment. Parents should be encouraged to create a formal session environment, preferably in a private room within the home. With regard to maintaining child focus, increased parental management of inattention and hyperactivity may need to be emphasized, as it’s possible the therapist is a less salient stimulus relative to face-to-face sessions.
The study has several limitations. First, the sample size was rather small, limiting statistical power. Also, use of a WL-control group instead of a face-to-face CBIT group makes it difficult to draw definitive conclusions regarding acceptability of VoIP-delivered CBIT relative to face-to-face sessions. Also, longer-term follow-up assessment was not included, so maintenance of gains cannot be assessed or compared to previous trials. Additionally, a selection bias may have inflated the acceptability ratings, as many participants who were uninterested in the VoIP delivery method may have been less likely to inquire about participating in the study. Furthermore, although not necessarily a limitation, it is worth noting that patient adherence and satisfaction may have been influenced by the initial home visit, as it may have functioned to establish initial rapport with families.
Use of VoIP also raises some questions regarding maintenance of patient privacy and management of potential psychiatric crises. To address privacy concerns, families were informed of the limits of privacy (over the internet and within the home) during VoIP sessions in both the informed consent and assent, and in a separate handout featuring videoconferencing guidelines. With respect to potential psychiatric emergencies, none were reported, but families were required to provide contact information at screening for their child’s local health professional as a cautionary measure.
Conclusion
Overall, results of the present trial show CBIT can be implemented via VoIP with good treatment adherence, using low-cost equipment or products already owned by families. Despite never entering the clinic and experiencing some technological difficulties during treatment sessions, satisfaction and therapeutic alliance ratings among families were high. Furthermore, as it may be argued that VoIP treatments are biased towards higher socioeconomic status portions of the population due to technological requirements, it is important to note that no families who underwent phone screening were excluded for lacking a high speed (i.e., Cable/DSL) internet connection; and only one family who seemed eligible for the study during phone screening was unable to participate in the full 2-step screening process due to technological difficulties with their internet connection. Additionally, the majority of families enrolled already owned a web camera prior to the study.
In the future, a randomized-controlled trial with a larger sample size is needed to assess VoIP-delivery of CBIT relative to in-person treatment. Also, inclusion of both short- and long-term follow-up assessments is needed to assess maintenance of gains. It would also be informative to explore relationships between computer and internet technology variables (e.g., computer processor speed, internet speed, etc.) and therapeutic outcomes, as these indices may influence rate and severity of technological difficulties, in turn affecting VoIP administration. Furthermore, it may be helpful to pilot CBIT on personal tablets or smart phones, as VoIP programs are available for download on these devices, and several families expressed interest in performing VoIP sessions on their personal tablets at the outset of study participation.
Acknowledgments
The research reported in this publication was supported by the National Institute of Mental Health of the National Institutes of Health under Award Number F31MH096375. The content is the responsibility of the authors and is not necessarily representative of the views of the National Institutes of Health.
DWW receives royalties from the Guilford Press, Oxford University Press, and Springer Press, and honoraria for presentations sponsored by the Tourette Syndrome Association through their collaborative partnership with the Centers for Disease Control and Prevention.
Footnotes
ClinicalTrials.gov Identifier: NCT02247206
Declaration of Conflicting Interests
All other authors declare no conflicts of interest.
Guarantor and Statement of Contributorship
EJR contributed to study conception and design, assessment and data collection, supervision, analysis and interpretation of data, and manuscript drafting and editing. ARG contributed to assessment, and data collection and interpretation. MRC contributed to treatment delivery, and data collection and interpretation. CRB, NGB contributed to treatment delivery, and data acquisition. MBH contributed to study conception and design, supervision, and data interpretation. FME contributed to supervision and data collection. Additionally, all authors made substantial contributions to critical revisions of the manuscript, gave final approval, and agree to be accountable for all aspects of the work. IS contributed to data collection, and data analysis and interpretation. DR contributed to data collection, and data interpretation. DWW is the corresponding author, and contributed to study concept and design, acquiring funding, supervision, manuscript drafting and revision, and interpretation of findings.
Research Ethics
This research protocol was reviewed and approved by the Institutional Review Board (#12.085) of the University of Wisconsin-Milwaukee Human Research Protection Program.
References
- 1.Cavanna AE, David K, Bandera V, et al. Health-related quality of life in Gilles de la Tourette Syndrome: A decade of research. Behav Neurol. 2013;27:83–93. doi: 10.3233/BEN-120296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Conelea CA, Woods DW, Zinner SH, et al. Exploring the impact of Chronic Tic Disorders on youth: Results from the Tourette Syndrome impact survey. Child Psychiatry Hum Dev. 2011;42:219–242. doi: 10.1007/s10578-010-0211-4. [DOI] [PubMed] [Google Scholar]
- 3.Scahill L, Erenberg G, Berlin CM, Jr, et al. Contemporary assessment and pharmacotherapy of Tourette syndrome. NeuroRx. 2006;3:192–206. doi: 10.1016/j.nurx.2006.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Himle MB, Woods DW, Piacentini J, et al. A brief review of habit reversal training for Tourette syndrome. J Child Neurol. 2006;21:719–725. doi: 10.1177/08830738060210080101. [DOI] [PubMed] [Google Scholar]
- 5.Woods DW, Piacentini J, Chang SW, et al. Managing Tourette Syndrome: A Behavioral Intervention for Children and Adults. New York, NY: Oxford University Press Inc; 2008. [Google Scholar]
- 6.Piacentini J, Woods DW, Scahill L, et al. Behavior therapy for children with Tourette Disorder: A randomized controlled trial. JAMA. 2010;303:1929–1937. doi: 10.1001/jama.2010.607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wilhelm S, Peterson AL, Piacentini J, et al. Randomized trial of behavior therapy for adults with Tourette Syndrome. Arch Gen Psychiatry. 2012;69:795–803. doi: 10.1001/archgenpsychiatry.2011.1528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Murphy TK, Lewin AB, Storch EA, et al. Practice parameter for the assessment and treatment of children and adolescents with tic disorder. J Am Acad Child Adolesc Psychiatry. 2013;52:1341–1359. doi: 10.1016/j.jaac.2013.09.015. [DOI] [PubMed] [Google Scholar]
- 9.Steeves T, McKinlay BD, Gorman D, et al. Canadian guidelines for the evidence-based treatment of tic disorders: behavioural therapy, deep brain stimulation, and transcranial magnetic stimulation. Can J Psychiatry. 2012;57:144–151. doi: 10.1177/070674371205700303. [DOI] [PubMed] [Google Scholar]
- 10.Verdellen C, Van De Griendt J, Hartmann A, et al. European clinical guidelines for Tourette Syndrome and other tic disorders. Part III: Behavioural and psychosocial interventions. Eur Child Adolesc Psychiatry. 2011;20:197–207. doi: 10.1007/s00787-011-0167-3. [DOI] [PubMed] [Google Scholar]
- 11.Woods DW, Conelea CA, Himle MB. Behavior therapy for Tourette’s disorder: Utilization in a community sample and an emerging area of practice for psychologists. Prof Psychol Res Pr. 2010;41:518–525. [Google Scholar]
- 12.Hilty DM, Luo JS, Morache C, et al. Telepsychiatry: An overview for psychiatrists. CNS Drugs. 2006;16:527–548. doi: 10.2165/00023210-200216080-00003. [DOI] [PubMed] [Google Scholar]
- 13.Himle MB, Freitag M, Walther M, et al. A randomized pilot trial comparing videoconference versus face-to-face delivery of behavior therapy for childhood tic disorders. Behav Res Ther. 2012;50:565–570. doi: 10.1016/j.brat.2012.05.009. [DOI] [PubMed] [Google Scholar]
- 14.Martin S, Sutcliffe P, Griffiths F, et al. Effectiveness and impact of networked communication interventions in young people with mental health conditions: A systematic review. Patient Educ Couns. 2011;85:e108–e119. doi: 10.1016/j.pec.2010.11.014. [DOI] [PubMed] [Google Scholar]
- 15.Tantam D. Computers, the internet and the World Wide Web: An introduction for the e-therapist. Adv Psychiatr Treat. 2006;12:359–367. [Google Scholar]
- 16.Choi NG, Hegel MT, Marti CM, et al. Telehealth problem-solving therapy for depressed low-income homebound older adults: Acceptance and preliminary efficacy. Am J Geriatr Psychiatry. 2014a;22:263–271. doi: 10.1097/JGP.0b013e318266b356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.King VL, Brooner RK, Peirce JM, et al. A randomized trial of web-based videoconferencing for substance abuse counseling. J Subst Abuse Treat. 2014;46:36–42. doi: 10.1016/j.jsat.2013.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lichstein KL, Scogin F, Thomas J, et al. Telehealth cognitive behavior therapy for co-occurring insomnia and depression symptoms in older adults. J Clin Psychol. 2013;69:1056–1065. doi: 10.1002/jclp.22030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Storch EA, Caporino NE, Morgan JR, et al. Preliminary investigation of web-camera delivered cognitive-behavioral therapy for youth with obsessive-compulsive disorder. Psychiatry Res. 2011;189:407–412. doi: 10.1016/j.psychres.2011.05.047. [DOI] [PubMed] [Google Scholar]
- 20.Yuen EK, Herbert JD, Forman EM, et al. Acceptance based behavior therapy for social anxiety disorder through videoconferencing. Journal Anxiety Disord. 2013;27:389–397. doi: 10.1016/j.janxdis.2013.03.002. [DOI] [PubMed] [Google Scholar]
- 21.Choi NG, Wilson NL, Sirrianni L, et al. Acceptance of home-based telehealth problem-solving therapy for depressed, low-income homebound older adults: Qualitative interviews with the participants and aging-service case managers. Gerontologist. 2014b;54:704–713. doi: 10.1093/geront/gnt083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Goetter EM, Herbert JD, Forman EM, et al. Delivering exposure and ritual prevention for obsessive-compulsive disorder via videoconference: Clinical considerations and recommendations. J Obsessive Compuls and Relat Disord. 2013;2:137–143. [Google Scholar]
- 23.Khatri N, Marzali E, Tchernikov I, et al. Comparing telehealth-based and clinic-based group cognitive behavioral therapy for adults with depression and anxiety: A pilot study. Clin Interv Aging. 2014;9:765–770. doi: 10.2147/CIA.S57832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Armfield NR, Gray LC, Smith AC. Clinical use of Skype: A review of the evidence base. J Telemed Telecare. 2012;18:125–127. doi: 10.1258/jtt.2012.SFT101. [DOI] [PubMed] [Google Scholar]
- 25. [accessed 5 October 2013];Skype and Microsoft. What is Skype? http://about.skype.com/
- 26.Sheehan DV, Sheehan KH, Shytle RD, et al. Reliability and validity of the Mini International Neuropsychiatric Interview for Children and Adolescents (MINI-Kid) J Clin Psychiatry. 2010;71:313–326. doi: 10.4088/JCP.09m05305whi. [DOI] [PubMed] [Google Scholar]
- 27.Wechsler D. Wechsler Abbreviated Scale of Intelligence (WASI) London: The Psychological Corporation; 1999. [Google Scholar]
- 28.Canivez GL, Konold TR, Collins JM, et al. 2009. Construct validity of the Wechsler Abbreviated Scale of Intelligence and Wide Range Intellligence Test: Convergent and structural validity. Sch Psychol Q. 2009;24:252–265. [Google Scholar]
- 29.AXELROD BN. Validity of the Wechsler Abbreviated Scale of Intelligence and other very short forms of estimating intellectual functioning. Assessment. 2002;9:17–23. doi: 10.1177/1073191102009001003. [DOI] [PubMed] [Google Scholar]
- 30.Saklofske DH, Caravan G, Schwartz C. Concurrent validity of the Wechsler Abbreviated Scale of Intelligence (WASI) with a sample of Canadian children. Can J Psychol. 2000;16:87–94. [Google Scholar]
- 31.Leckman JF, Riddle MA, Hardin MT, et al. The Yale Global Tic Severity Scale: Initial testing of a clinician-rated scale of tic severity. J Am Acad Child Adolesc Psychiatry. 1989;28:566–573. doi: 10.1097/00004583-198907000-00015. [DOI] [PubMed] [Google Scholar]
- 32.Storch EA, Murphy TK, Geffken GR, et al. Reliability and validity of the Yale Global Tic Severity Scale. Psychol Assess. 2005;17:486–491. doi: 10.1037/1040-3590.17.4.486. [DOI] [PubMed] [Google Scholar]
- 33.Ricketts EJ, Bauer CC, Ran D, et al. Pilot open case series of Voice over Internet Protocol-delivered behavior therapy for tic disorders. Cogn Behav Pract. doi: 10.1016/j.cbpra.2014.09.003. Epub ahead of print 16 October 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Guy W. ECDEU assessment manual for psychopharmacology. Rev. Rockville, MD: National Institute of Mental Health; 1976. (DHEW publication no. (ADM) 76-338) [Google Scholar]
- 35.Scahill L, Chappell PB, Kim YS, et al. A placebo-controlled trial of Guanfacine in the treatment of children with tic disorders and attention deficit hyperactivity disorder. Am J Psychiatry. 2001;158:1067–1074. doi: 10.1176/appi.ajp.158.7.1067. [DOI] [PubMed] [Google Scholar]
- 36.Chang S, Himle MB, Tucker BTP, et al. Initial psychometric properties of a brief parent-report instrument for assessing tic severity in children with Chronic Tic Disorder. Child Fam Behav Ther. 2009;31:181–191. [Google Scholar]
- 37.Kendall PC, Flannery-Schroeder E, Panichelli-Mindel SM, Southam-Gerow M, Henin A, Warman M. Therapy for youths with anxiety disorders: A second randomized clinical trial. J Consult Clin Psychol. 1997;65:366–380. doi: 10.1037//0022-006x.65.3.366. (1997) [DOI] [PubMed] [Google Scholar]
- 38.Elvins R, Green J. The conceptualization and measurement of therapeutic alliance: An empirical review. Clin Psychol Rev. 2008;28:1167–1187. doi: 10.1016/j.cpr.2008.04.002. [DOI] [PubMed] [Google Scholar]
- 39.Larsen DL, Attkisson C, Hargreaves WA, et al. Assessment of client/patient satisfaction: Development of a general scale. Eval Program Plann. 1997;2:197–207. doi: 10.1016/0149-7189(79)90094-6. [DOI] [PubMed] [Google Scholar]
- 40.Roberts RE, Attkisson CC. Assessing client satisfaction among Hispanics. Evaluation and Program Planning. 6:401–413. doi: 10.1016/0149-7189(83)90019-8. [DOI] [PubMed] [Google Scholar]
- 41.Nguyen TD, Attkisson CC, Stegner BL. Assessment of patient satisfaction: Development and refinement of a Service Evaluation Questionnaire. Eval Program Plann. 1983;6:299–314. doi: 10.1016/0149-7189(83)90010-1. [DOI] [PubMed] [Google Scholar]
- 42.Hunsley J. Development of the Treatment Acceptability Questionnaire. J Psychopathol Behav Assess. 1992;14:55–64. [Google Scholar]
- 43.Yip MP, Chang AM, Chan J, et al. Development of the Telemedicine Satisfaction Questionnaire to evaluate patient satisfaction with telemedicine: A preliminary study. J Telemed Telecare. 2003;9:46–50. doi: 10.1258/135763303321159693. [DOI] [PubMed] [Google Scholar]
- 44.Saghaei M. Random Allocation Software. Version 1.0. Isfahan, Iran: Saghaei M; 2004. (2004) [Google Scholar]
- 45.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 2000. [Google Scholar]
- 46.Schulz KF, Altman DG, Moher D, et al. CONSORT 2010 Statement: Updated guidelines for reporting parallel group randomized trials. BMJ. 2010;340:698–702. doi: 10.1097/AOG.0b013e3181d9d421. [DOI] [PubMed] [Google Scholar]
- 47.Qualtrics Labs Inc. Qualtrics Research Suite. Version 21269. Provo, UT: Qualtrics Labs, Inc; 2011. [Google Scholar]
- 48.Evaer Technology. Evaer video recorder for Skype. Version 1.3.9.29. Evaer Technology. 2013 [Google Scholar]
- 49.Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. (1988) [Google Scholar]
- 50.Yuen EK. PhD Thesis. Drexel; Philadelphia, PA, US: 2010. Acceptance-based behavior therapy for social anxiety disorder using videoconferencing. [DOI] [PubMed] [Google Scholar]