Abstract
Hospitalization in the intensive care unit can be a stressful time for patients and their family members. Patients’ family members often have difficulty processing all of the information that is given to them. Therefore,an intensive care unit diary can serve as a conduit for synthesizing information, maintaining connection with patients, and maintaining a connection with family members outside the intensive care unit. Paper intensive care unit diaries have been used outside the United States for many years. This article explores the development of an electronic intensive care unit diary using a rapid prototyping model to accelerate the process. Initial results of design testing demonstrate that it is feasible, useful, and desirable to consider the implementation of electronic intensive care unit diaries for patients at risk for post–intensive care syndrome.
Keywords: ICU diaries, post–intensive care syndrome, electronic diary
Critical illness and intensive care can disrupt both short- and long-term health among intensive care unit (ICU) survivors. Neurocognitive and functional abilities can be profoundly disturbed, decreasing quality of life.1,2 Acknowledged in the literature as post-intensive care syndrome (PICS), debilitation including posttraumatic stress disorder (PTSD) after intensive care can continue for years.1–5 This condition, when associated with ICU hospitalization and critical illness, is often unrecognized and therefore untreated.5 ICU-related PTSD appears to have a unique clinical profile, likely requiring comprehensive assessment and treatment upon discharge.5 Prevalence of PICS is as high as 50% among ICU survivors.1–3,6 This percentage will increase as the population ages and the corresponding use of critical care units goes up.1,2
Family members of ICU survivors may also experience psychological symptoms including, but not limited to, depression, generalized anxiety, symptoms of posttraumatic stress, and sleep disorders. This syndrome is known as post-intensive care syndrome-family (PICS-F).6
Cognitive impairment is experienced by as many as 1 in 4 ICU survivors for as long as 12 months after discharge, and the symptoms can have the same severity as mild Alzheimer disease.3 ICU diaries have been used to reduce the neuropsychiatric impact of critical illness7 and can help patients and their families recall daily events both outside and inside the ICU as well as emotions, thoughts, and well wishes from friends, family members, and clinicians. In a randomized controlled trial reported by Jones et al,7 ICU diaries resulted in a significant reduction in PICS 3 months after ICU discharge.8
Studies have reported that ICU diaries are used outside the United States, but their use has not been fully explored in the United States.7-11 Some experts suggest that diaries be considered for implementation in ICUs to reduce anxiety, depression, and posttraumatic stress in family members of ICU patients.12 In this article, we describe the process of preparing a prototype electronic diary for ICU patients and families.
Current State of ICU Diaries
Successful strategies used in previous ICU diary programs were identified using a literature review. The literature search used MEDLINE, PubMed-NCBI, Cochrane CENTRAL, and Google databases and included the following search terms: intensive care diaries, intensive care recovery, post-intensive care syndrome, intensive care journals, posttraumatic stress disorder, intensive care patients, post-traumatic stress symptoms, and rehabilitation after mechanical ventilation. References from each article were used to identify additional relevant articles. Studies and publications were excluded if they were not in English, were not published between January 1990 and December 2014, were not relevant to the ICU, or were not original research or literature reviews.
Of 56 abstracts identified, 25 eligible studies were included in the review. The search results revealed that most ICU diaries were used in Europe and primarily involved ICU patients, although a few diaries focused on the ICU staff. Diaries were implemented in adult medical, surgical, and mixed ICUs among patients whose ICU lengths of stay were at least 48 hours and who were mechanically ventilated.13 In many studies, ICU diaries were viewed as a physical journal of entries and a common outlet for physicians and ICU staff to connect with the patient and the patient’s family members.
Across the studies, several common elements emerged: use of photos, standardized headings, daily entries by staff and family members, use of nonmedical language, and keeping the diary with patients throughout their ICU hospitalization.13 Differences among studies included time of diary return and the method in which it was returned. With regards to diary return, the differeces included returning the diary at discharge from the ICU, at 1 month after hospital discharge, or up to 3 months after discharge. Most study protocols followed up with the patient a minimum of 6 months after discharge.13 In one exception, a study explored patients’ lived experiences of being followed in a program that used patient diaries, post-ICU conversations, and return visits to the ICU for 18 months after discharge.14
The literature review did not contain studies describing the exact mechanisms by which ICU diaries improve outcomes—this has implications for future uses of ICU diaries. Without this knowledge, best practices in prototype development cannot be assumed. Acknowledging the limitations of existing research and the need to conduct further research about ICU diaries is important when considering the use of technology as an alternative medium to paper diaries. All of the studies we reviewed used a paper format that was kept at the patient’s bedside, thereby limiting entries to caregivers and family members who physically entered the room.13 With paper diaries there is the risk of misplacement of the diary (by the patient at home or in the hospital by staff) and the inability to link the diary to an electronic medical record for use by the patient’s primary physician at follow-up appointments or by patients for accessing their own record. An electronic version facilitates easier reading compared to diaries that are hand written. After conducting the literature review, we decided to develop an electronic ICU diary application that could address some of the drawbacks identified in the use of a paper ICU diary.
Innovation and Technology
Problem Statement
We approached the Innovation Department within our organization to obtain grant funding to develop an electronic ICU diary pilot project that could be used in a 21-hospital health system in northern California. The team consisted of an intensivist physician-researcher, a clinical nurse specialist and consultant, a project manager, an Innovation Fund for Technology team leader, and a designer with expertise in user experience.
Our initial problem statement was as follows: “Critical illness and intensive care can have a traumatic impact on a patient including nightmares and posttraumatic stress disorder. Studies have shown that an ICU patient ‘diary’ or journal in which family and providers can record daily ICU events and procedures can serve as a powerful tool in patient recovery. Paper-based diaries are widely used in Europe but not as frequently in the United States.” At the recommendation of the Innovation Fund for Technology committee, we revised the statement to address specific factors that make the ICU experience stressful and added information on how an ICU diary could serve as a conduit to alleviate stressors (Table 1).
Table 1:
Stressors for Family Members of Intensive Care Unit Patients Addressed by an Electronic Diary
| Family members do not understand or are unfamiliar with ICU technology. |
| Multiple unfamiliar ICU caregivers make it difficult for family to communicate with hospital staff. (Whom do I talk to? About which aspects of care?) |
| Caregivers’ schedules are unpredictable. (When will the doctor come by the room?) |
| Family members do not know what they can do to help. (How can I be involved in daily care?) |
| Family members are overwhelmed by information on external websites. (What is relevant to our family or loved one?) |
| Family members have trouble understanding technical information given by clinicians. (What was meant by “weaning from the ventilator”?) |
| Lack of follow-up and long-term side effects occur after the episode of care is over. (Whom should I speak to about memory problems?) |
Abbreviations: ICU, intensive care unit.
Functional Requirements
The next step in our project was to determine the relevant functional requirements for an electronic ICU diary. We divided the functional requirements into 3 parts: (1) components essential to building a prototype, (2) nonessential components, and (3) components that could be built into the application with unlimited and unrestricted grant funding (Table 2).
Table 2:
Proposed Content for An intensive care Unit Electronic diary
| Guided | Space for health updates including medical conditions, organized by organ system (brain, heart, lung, gastrointestinal, kidney) Space for care team goals including mobility, breathing, medications, devices, procedures, general information Space to record how to help ICU patients with muscle strength, confusion, nutrition, emotional support, pain, infection Input by user structured by the application for majority of pages including health updates, care team goals, how to help |
| Not guided | Space for nonmedical updates about events, thoughts, visitors—the user inputting the information uses free text Space for questions—the user inputting the information uses free text |
| Other | Devices and procedures My care team (ICU staff) Information button (not on main screen) that contains information “About This ICU” Application menu choices continually apparent to user Minimal clicks needed to navigate the application, minimal drill down menus Information on what families can do to align with “Rethinking Critical Care” aims (ie, our own institution's goals for ICU patients) Space for input from users about future updates and/or additions requested for improvement of the application |
Abbreviations: ICU, intensive care unit.
Our aim was to develop an electronic ICU diary that could be exported directly into patients’ medical records and accessed through an electronic portal by patients and by the primary physician with patient permission. As the technology for electronic medical records evolves, we imagine that in the future this application could become a standard method for storing and viewing electronic ICU diaries.
Summary of Existing Technology
In accordance with the funding proposal requirements, we assessed current technology platforms that could be used for an ICU diary. A review of the existing technology revealed web applications used primarily to manage family members’ medical care; these applications included simple journal function and potentially customizable educational components and organizational tools (eg, calendars, to-do lists, reminder emails). A simple journal format does not allow for sub-menus, additional linking to events, explanations of ICU equipment unique to an individual’s ICU care, or explanations of medications used. Examples of existing technology included Care Zone,15 Caring Bridge,16 and Care Pages.17
During our comparative analysis of existing technology, we focused on the need for a patient-oriented tool to mitigate or prevent PICS by providing an accurate narrative of the ICU stay that could “fill in the gaps” when the patient was not cognitively intact. This analysis led to the conclusion that we needed to develop our own electronic ICU diary application. The application needed to be specifically tailored to assist ICU patients in their recovery process after discharge. The information provided in the application needed to be specific to this organization’s ICUs. This diary could then be shared with the patient’s primary health care provider upon discharge to explain possible health and cognitive issues arising from a prolonged ICU admission.
Obtaining Stakeholder Approval
Feedback from key stakeholders was obtained as part of the iterative software development. Stakeholders included senior medical and nursing leaders of northern California ICUs in addition to senior leaders of the Innovation Department. The grant was funded through the organization’s Innovation Fund for Technology to be used primarily for the development of the application using a rapid prototyping approach, with the understanding that any pilot phase of the application would require further financial consideration.
The platform was presented at key stakeholder meetings, including those of the regional Northern California (NCAL) ICU Medical Chiefs, Clinical Adult Service Directors, and ICU Nurse Managers, to garner buy-in for the development and subsequent assessment of the application. Legal concerns were addressed through our legal department.We decided to have family members and nurses make entries during the prototype assessment and to discuss further entries during the pilot phase. Entries from nursing staff were not to discuss diagnoses, burden of illness, or trajectory of disease process.
Leveraging Technology to Build an ICU Diary
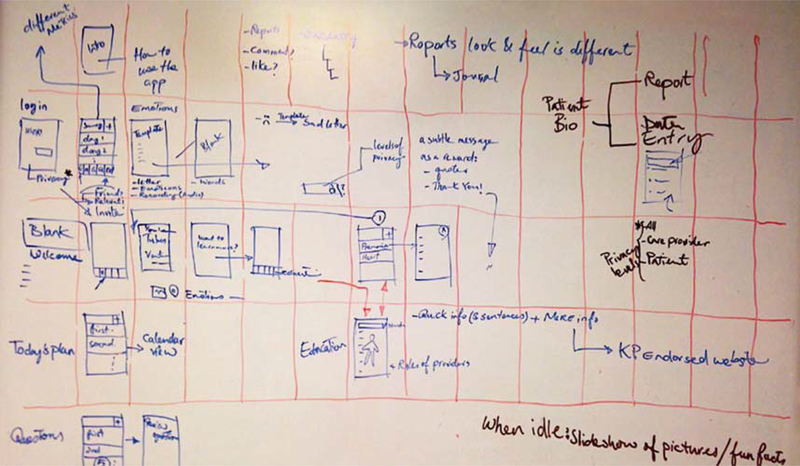
After receiving a grant from the Innovation Fund for Technology to develop the electronic application prototype, the team was formed and regular meetings began. Using a storyboard approach to provide visualization of the navigation process and content sequencing, we developed a hypothetical story to determine how we would format the prototype for testing with patients and families and to provide a simulation of “reality” for our stakeholders to view (Figure 1).
Figure 1:
Storyboard for the electronic diary.
Hypothetical Story Used for the Storyboard
Sonia is a 73-year-old woman who was admitted for extensive cardiac surgery. She experienced postoperative complications in the operating room and spent 4 hours on bypass in the operating room. After her surgery, Sonia went to the ICU, where she spent 4 days unconscious. During this time, her 3 children and her husband were continuously at her bedside. During the ICU stay, Sonia was intubated for 4 days and received intravenous sedation during some of that time. She was transferred out of the ICU to the general ward on day 8 of her hospitalization and was discharged to her home the following day. Sonia’s oldest son Kevin, who is 37 years old, took primary responsibility for completing her ICU diary. We created some hypothetical sample diary entries for him and another family member. These sample entries are organized into the 4 functional categories we envisioned for the application: (1) emotional updates, (2) health updates, (3) goals of care, and (4) questions for clinicians.
Emotional Update:
Hi Mom, Well I have to say I did not expect to see you with so many tubes and machines on you. It was a bit of a shock to see you like this, even though the surgeon explained to us what we would see. It’s different when you first walk into the room. They told us that you would be out of it from the drugs, and I guess you are because you do not respond to us in any way. Sarah is coming down with the kids, but I am not sure if I want them to see you like this. They have told us you should be waking up in the next day or so. Everyone says hello and to hang in there. We love you Mom—love Kevin.
Health Update.
Mom is asleep and is not waking up after the surgery. She is currently receiving minimal sedative medication and is hooked up to a central line, pacemaker, 2 chest tubes, and a ventilator. She looks gray and feels cold when I touch her. (Entry from family member after medical rounds and from looking at the menus on the application that explain all the equipment and medications.)
Goals of Care.
When the doctor and the other people came into the room today, they said the goals of care for my mom were (1) reduce sedation, (2) spontaneous breathing trial, and (3) assess for delirium. (Goals of care discussed daily on multidisciplinary rounds.)
Questions for Clinicians.
When will my Mom wake up? Why didn’t my Mom wake up right after surgery? Does she hear us? What will she remember about this? When will Mom be able to get out of bed? What are all the tubes that are attached to my Mom and what do they do for her?
Building the Prototype
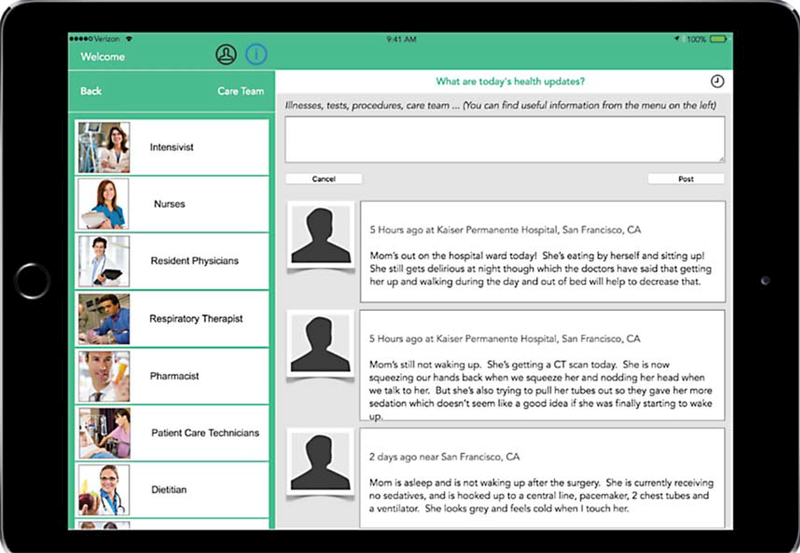
Prototype version 1 was developed and demonstrated to senior leadership as an application loaded onto an electronic tablet. With input from leadership, the intensivist leading the innovation decided that a continually visible, left-hand menu structure would be easier to navigate. The stakeholders decided that the application should be aligned with the current organizational ICU quality-improvement initiatives to optimize possibilities for future integration into the ICU workflow. Since 2010, all 21 hospitals in northern California had been engaged in a “Rethinking Critical Care” initiative to reduce mortality and improve outcomes in the ICUs, and it was appropriate to align the design of the prototype with the workflow in the ICU.18 After receiving leadership feedback, the team redesigned the application and developed prototype version 2 of the ICU diary (Figure 2). Version 2 included menus that provided information about sedation in the ICU and why it was important to use less sedation to reduce the incidence of delirium and for the patient to be more alert. Mobility was highlighted as being an essential part of daily activity in the ICU. The menu also included information about equipment and personnel in the ICU and why it was important to assess daily the ability of the patient to be liberated from the ventilator. These components of the application all aligned with the “Rethinking Critical Care” initiative.18
Figure 2:
Version 2 prototype of the electronic diary using simulated patient data.
Involving Patient and Families
Confidential feedback from family members and patients is always included in the organization’s innovation projects. Version 2 of the prototype was finalized and we had families assess the application in 2 ICUs in one of the larger medical centers in the health system. At the ICU in our San Francisco hospital, 4 family members were interviewed. The users were female and aged between 52 and 68 years; each had a family member in the ICU at the time of the assessment. The interview included a demonstration of the application, and the end user was asked to accomplish specific tasks while being observed. We used the following questions in our assessment: (1) What value is possible to obtain through this product—Is it useful? (2) How much effort is required to extract value from the product—Is it useable? (3) Is extracting value from the product satisfying or enjoy able—Is it desirable?
User Feedback
What Value Is Possible to Obtain Through This Product—Is It Useful?
One user, a nurse with a family member in the ICU, believed that the application could be useful at patient care conferences to enable family members to recollect their thoughts and questions and to document outcomes from the conference. Two of the other users thought it would be a great tool for communication among family members. In general, the common elements extrapolated from the feedback were that the application could be useful (1) for long-term patients who cannot remember their stay in the ICU, (2) for communicating the patient’s status to friends and family members who visit so they can look at the entries, (3) for providing a reference for family members in patient care conferences, and (4) for giving the family a sense of control by not having to constantly ask doctors and nurses questions. They also thought the application was easy to use.
How Much Effort Is Required to Extract the Value From the Product—Is It Usable?
The 4 users who evaluated the diary application at this stage did not report any significant issues with the interface. After watching a brief demonstration, 3 users accomplished the assigned tasks easily. All feedback comments were positive, and 3 of the 4 users remarked how easy it was to see the menus and to navigate the tabs and submenus due to the large font and bright screen.
Is Extracting Value From The Product Satisfying or Enjoyable—Is It Desirable?
Although 3 of the users loved the concept, 1 user did not. She did not touch the application, even though she was keeping a paper journal to track her husband’s progress in the ICU. Another user wanted to download the application for immediate use, and she stated that the technology was very similar to social media applications she already used daily. It became clear that the electronic diary might be helpful for most families but not for all.
Concerns From the Users
The issue of security of the tablet device containing the application was raised by the staff of the ICU. Both families and the staff expressed concern about the safety and security of data on an electronic device with multiple users. Nurses were concerned about how the ICU diary would be integrated into their workflow in relation to the time needed to enter information and to assist family members in understanding how to use the application. Observations and suggestions from the application assessment with the family members and staff were compiled (Table 3).
Table 3:
Issues Observed From Feedback and Proposed Improvements
| Issue | Potential Improvements |
|---|---|
| Difficulties returning to main menu from submenus and tabs | When the user is on various tabs or submenus, the main menu tab should not change position. All the tabs and submenus remain in the same place on the screen of the electronic tablet. |
| Unclear how to upload an image onto the electronic tablet where it could be easily accessed and stored | Make the application downloadable onto a personal device so that it can be used anywhere and photos can be downloaded directly from the application. Email capability to enable photos to be sent to the device. |
| Multiple requests for “sharing” updates with other family members and friends who could not visit or who lived in a different state or part of the world | Create a button in updates to enable users to “share” a status with whomever they wish. Allow remote access to the updates with a secure password. |
| Need a medium for enabling family members to journal their thoughts. Users wanted to learn about other possible applications | Adapting the application so that it could serve as a pregnancy electronic journal. |
| Distinguishing different update topics was not clear for the users (eg, “Goals” vs “Questions” vs “Health”) | Provide clear classifications for each title so that users can choose the best update category easily. |
| Difficulty locating the patient profile icon | Use a more communicative icon and/or text for patient profile. |
| Trouble searching for specific information related to their family member's health issue at the ICU | Provide ability to filter and customize the data and information on the education section of the application, based on different health issues. |
| Most users thought it should be used as a social application | Create a social network rather than a single-user application. Like any other application, the users should have freedom to set up their preference on privacy settings. |
| Goals of care may be forgotten or confusing for users | Develop a pull system rather than a push system (ie, where the user enters the data). The pull system can incorporate the goals of care from the electronic medical record. Include the capability to take a picture of an image or document from the tablet. |
Abbreviations: ICU, intensive care unit.
Putting It All Together
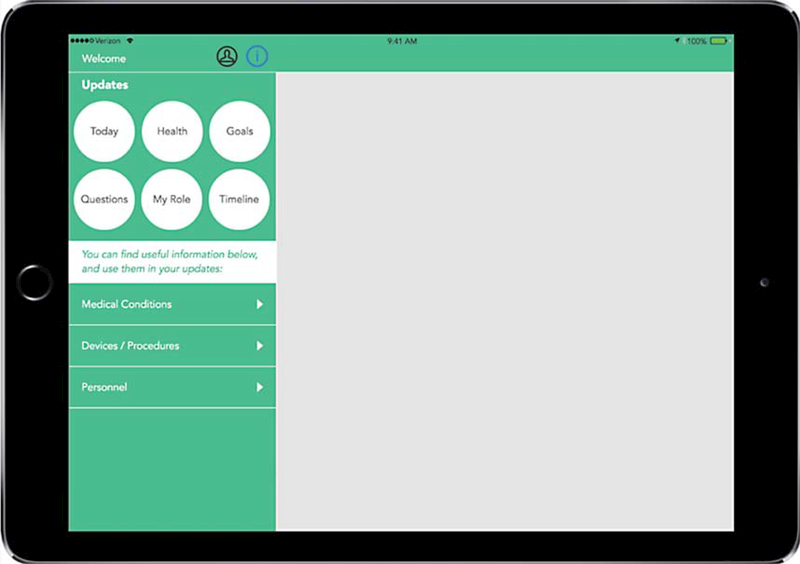
When we started this project to provide an electronic ICU diary for staff, patients, and families, we wanted to ensure that the design priority was focused on the patient and family members. After testing and assessing the prototype and soliciting feedback from the potential end users of the product, the design team incorporated as many of the suggestions as possible, given the time and financial restraints. The final application was designed for use on a tablet device and it was shared with internal stakeholders and potential external vendors at a showcase celebration highlighting the concept of storyboarding and rapid prototyping (Figure 3).
Figure 3:
Final version of the electronic diary for use in the intensive care unit.
Next Steps and Future Development
The cost of developing an application like this one is substantial and should be taken into consideration. The design team and innovators spent many months in the development phase, and the final product reflected expertise in application development, nursing delivery of ICU care, and family desires regarding support and communication in the ICU. Rather than delay the implementation of diaries due to development concerns, we decided to commence a pilot project using a paper version of the ICU diary. Not only was this a reasonable strategy to introduce the concept and process to staff, patients, and families, but also it allowed us to explore the feasibility and some of the legal concerns around patient privacy before launching an electronic diary. Subsequent concerns will be reviewed after this phase of the project to determine next steps. In the meantime, we continue to report the project findings to key stakeholders and are seeking sponsorship and interest from other ICUs.
Conclusion
Developing and assessing the electronic ICU diary with patients, family members, and ICU staff produced both successes and challenges. The successes included the ease of use for staff and family members; many users were already familiar with navigating menus because they interacted with social media applications in their daily lives. The ICU diary concept gained acceptance from key stakeholders and ICU medical chiefs and nurse managers, and the potential issues these stakeholders put forward directed necessary research. Family members of ICU patients who assessed the ICU diary application were open to the idea of an electronic conduit for their thoughts and medical questions. Challenges stemmed from potential patient privacy violations and securing the tablet at the patient’s bedside so it would not be misplaced or stolen. Concern about potential liability when making an entry into the ICU diary by medical and nursing staff surfaced regularly during discussions. Discussion of legal implications continues regarding the development and subsequent implementation of the diaries to ensure that all regulatory and issues are addressed.
Patient and family member engagement are increasingly recognized as important components of hospital care, especially in the ICU environment. However, strategies for standardizing that care are limited. Familiar electronic tools (eg, social media websites, tablets) are used widely for daily activities and could offer a seamless opportunity to improve the experiences of patients and family members, in particular through patient-driven journals. Understanding how ICU journals promote improved patient recovery will be essential for designing tools that can improve outcomes.
ACKNOWLEDGMENTS
The authors thank Innovation Fund team leader Suzanne Furuya for her assistance with rapid prototyping.
Footnotes
This project was funded by Kaiser Permanente's Innovation Fund for Technology.
REFERENCES
- 1.Needham DM, Davidson JE, Cohen H, et al. Improving long-term outcomes after discharge from intensive care unit: report from a stakeholders' conference. Crit Care Med. 2012;40:502–509. [DOI] [PubMed] [Google Scholar]
- 2.Elliot D, Davidson JE, Harvey MA, et al. Exploring the scope of post-intensive care syndrome therapy and care: engagement of non-critical care providers and survivors in a second stakeholders meeting. Crit Care Med. 2012;42(12):2519–2526. [DOI] [PubMed] [Google Scholar]
- 3.Pandharipande PP, Girard TD, Jackson JC, et al. Long-term cognitive impairment after critical illness. BRAIN-ICU study investigators. N Engl J Med. 2013; 369(14):1306–1316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.de Miranda S, Pochard F, Chaize M, et al. Post intensive care unit psychological burden in patients with chronic obstructive pulmonary disease and informal caregivers: a multicenter study. Crit Care Med. 2011; 39:112–118. [DOI] [PubMed] [Google Scholar]
- 5.Jackson JC, Jutte JE, Huddelston Hunter C, et al. Post- traumatic stress disorder (PTSD) after critical illness: a conceptual review of distinct clinical issues and their implications. Rehab Psych. 2016;61(2):132–140. [DOI] [PubMed] [Google Scholar]
- 6.Davidson JE, Jones C, Bienvenu OJ. Family response to critical illness: post-intensive care syndrome-family. Crit Care Med. 2012;40:618–624. [DOI] [PubMed] [Google Scholar]
- 7.Jones C, Backman C, Capuzzo M, et al. RACHEL group. Intensive care diaries reduce new onset posttraumatic stress disorder following critical illness: a randomized controlled trial. Crit Care. 2010;14(5):R168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jones C, Backman C, Griffiths DR. Intensive care diaries reduce PTSD-related symptom levels in relatives following critical illness: a pilot study. Am J Crit Care. 2011; 21(3):172–176. [DOI] [PubMed] [Google Scholar]
- 9.Combe D The use of patient diaries in an intensive care unit. Nurs Crit Care. 2005;10(1):31–34. [DOI] [PubMed] [Google Scholar]
- 10.Egerod I, Schwartz-Nielsen KH, Hansen GM, Laerkner E. The extent and application of patient diaries in Danish ICUs in 2006. Nurs Crit Care. 2007;12(3):159–167. [DOI] [PubMed] [Google Scholar]
- 11.Akerman E, Granberg-Axell A, Ersson A, et al. Use and practice of patient diaries in Swedish intensive care units: a national survey. Nurs Crit Care. 2010; 15(1): 26–33. [DOI] [PubMed] [Google Scholar]
- 12.Davidson J, Aslakson RA, Long AC, et al. Guidelines for family-centered care in the neonatal, pediatric and adult ICU. Crit Care Med. 2017;45(1):103–128. [DOI] [PubMed] [Google Scholar]
- 13.Beg M, Scruth E, Liu V. Developing a framework for implementing intensive care unit diaries: a focused review of the literature. Aust Crit Care. 2016;(4):224–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Storli SL, Lind R. The meaning of follow-up in intensive care: patients' perspective. Scan J Caring Sci. 2009; 23(1):45–56. [DOI] [PubMed] [Google Scholar]
- 15.Care Zone website. https://carezone.com/home. Accessed March 29, 2017.
- 16.Caring Bridge organization website. https://www.car-ingbridge.org/. Accessed March 29, 2017.
- 17.Care Pages website. https://www.carepages.com/. Accessed March 29, 2017.
- 18.Liu V, Herbert D, Foss-Durant A, et al. Evaluation following staggered implementation of the “Rethinking Critical Care” ICU care bundle in a multicenter community setting. Crit Care Med. 2016;44(3):460–467. [DOI] [PMC free article] [PubMed] [Google Scholar]