Abstract
Mothers who have experienced childhood maltreatment are more likely to have children also exposed to maltreatment, a phenomenon known as intergenerational transmission. Factors in the perinatal period may contribute uniquely to this transmission but timing effects have not been ascertained. Using structural equation modeling with 1,016 mothers and their 2,032 children in the Environmental Risk (E-Risk) Longitudinal Twin Study, we tested the mediating role of postpartum depression between maternal childhood maltreatment and a cascade of negative child outcomes, specifically child exposure to maltreatment, internalizing symptoms, and externalizing symptoms: (1) adjusting for later maternal depression, (2) comparing across sex differences, and (3) examining the relative role of maltreatment subtypes. Mothers who had been maltreated as children were at increased risk for postpartum depression, especially those who had experienced emotional or sexual abuse. In turn, postpartum depression predicted children’s exposure to maltreatment, followed by emotional and behavioral problems. Indirect effects from maternal childhood maltreatment to child outcomes were robust across child sex and supported significant mediation through postpartum depression; however, this appeared to be carried by mothers’ depression beyond the postpartum period. Identifying and treating postpartum depression—and preventing its recurrence—may help interrupt the intergenerational transmission of maltreatment and its sequelae.
Keywords: Intergenerational transmission, child maltreatment, postpartum depression, perinatal mental health, childhood trauma
Introduction
Childhood maltreatment is a potent and common form of early trauma (Cicchetti & Toth, 2005; Stoltenborgh et al., 2015). Exposure to childhood maltreatment has been shown to compromise healthy development across critical domains (Cicchetti, 2016), with detrimental effects persisting into adulthood (Norman et al., 2012). Adding to this concerning picture, research suggests that childhood maltreatment not only produces negative outcomes for individuals during their own lifetime, but also has consequences extending to the next generation (Roberts et al., 2004). Studies have long observed that parents who have experienced childhood maltreatment are more likely to have children likewise exposed to maltreatment (Egeland et al., 1988; Pears & Capaldi, 2001), a phenomenon referred to as intergenerational transmission of maltreatment (Thornberry et al., 2012).
Although a wide range of transmission rates has been documented (Oliver, 1993), literature suggests that roughly one third of individuals maltreated as children go on to perpetuate maltreatment in the next generation, an estimate about six times higher than for the general population (Kaufman & Zigler, 1987). Parents maltreated as children have also been found to demonstrate heightened maltreatment potential (DiLillo et al., 2000; Rodriguez & Tucker, 2011) as well as disrupted parenting behaviors more broadly (Bert et al., 2009), which can contribute to maladjustment and psychopathology in the next generation—thereby transmitting to children negative sequelae of maltreatment in addition to maltreatment itself. Together, a better understanding of what facilitates intergenerational transmission of maltreatment and its sequelae is needed to inform critical efforts to interrupt such transmission.
Since the phenomenon of intergenerational transmission was proposed, studies have sought to explore relevant mechanisms. Classic explanatory frameworks have included (1) social learning theory (Bandura, 1973), through direct modeling of abusive behavior, and (2) attachment theory (Ainsworth, 1979; Bowlby, 1978), through disrupted working models of relationships that influence subsequent relationships, including with one’s children (Zeanah & Zeanah, 1989). Caregiver mental health may represent another key pathway. Maternal depression has been associated with maltreating behaviors in early childhood (Windham et al., 2004), potentially by reducing emotional resources to respond to caregiving demands. Furthermore, maternal depression is relatively easy to detect by self-report or clinical interview and also amenable to intervention, making it a tractable risk factor from a public health perspective. In this study, it is proposed that maternal depression in the perinatal period, occurring at the earliest intersection between generations, may fundamentally contribute to maltreatment and its sequelae in the next generation. Emerging findings from a separate stream of literature—perinatal mental health—may be relevant for this hypothesis.
Perinatal mental health research is concerned with the study of prevalence, risk factors, and consequences of mental disorders during the perinatal period, common of which is postpartum depression (Wisner et al., 2002). Of relevance, women who have experienced maltreatment as children are found at greater risk for postpartum depression (Alvarez-Segura et al., 2014; Choi & Sikkema, 2016). While maltreatment history is a risk factor for psychopathology across the life course (Widom et al., 2007), it may particularly kindle depression in the postpartum period, a time fraught with hormonal shifts (Hendrick et al., 1998), physical recovery from childbirth (Brown & Lumley, 2000), and heightened demands of caregiving (Campbell et al., 1992) which may also reactivate own early memories of caregiving. In turn, postpartum depression is recognized for its short- and long-term impacts on child outcomes (Choi et al., 2017; Murray & Cooper, 1996), even beyond later maternal depression in the child’s life (Hay et al., 2003; Murray et al., 2010). This may be due to disturbances in maternal caregiving behavior and exposure to depressed maternal affect during a critical time for child development (Field, 2010), which could set a long-term foundation for negative interactions and increased vulnerability to emotional/behavioral problems. Thus, while there is likely no single factor underlying intergenerational transmission of maltreatment (Dixon et al., 2005), maternal depression is expected to be an important conduit for transmitting negative outcomes to children, particularly during sensitive developmental windows such as the postpartum period.
Prior work with longitudinal cohorts has examined how the timing of maternal depression affects child outcomes (Barker, 2013). To date, research has not disentangled timing effects of maternal depression in relation to intergenerational transmission of maltreatment—for instance, whether postpartum depression contributes critically to this transmission pathway, or whether this is better explained by maternal depression across development broadly. A better understanding of timing effects would inform when interventions should best be targeted. According to a sensitive window hypothesis, maternal depression during the first year of life is expected to be uniquely impactful above and beyond later exposure(s) (Bagner et al., 2010; Bureau et al., 2009). This may be why treating maternal depression in early childhood has been suggested to reduce later maltreatment (McCann et al., 1992). However, no studies have formally examined postpartum and ensuing depression in the pathway between maternal childhood maltreatment and long-term child outcomes, including child victimization and later psychopathology. Alternatively, since early depressive episodes are known to kindle or increase risk for further episodes (Monroe & Harkness, 2005), it could be that cumulative exposure to maternal depression is most noxious.
Furthermore, how intergenerational pathways vary across sex differences and maltreatment types has not been well examined. Growing literature suggests boys may be more sensitive to early environmental adversity (Rutter et al., 2003), including maternal psychopathology in the perinatal period (Choe et al., 2013; McGinnis et al., 2015). In addition, literature on intergenerational transmission has tended to examine maltreatment exposure aggregated as a whole (Berzenski et al., 2014), whereas certain forms of maltreatment may be more likely than others to be transmitted via postpartum depression to the next generation. Comparative analyses would highlight forms of childhood maltreatment most likely to be carried forward into the next generation and thus most relevant for perinatal intervention.
To address these gaps in literature, this study drew on a large British longitudinal cohort of mothers and their twin children in which intergenerational continuity of maltreatment has been previously reported (Jaffee et al., 2013). The current aim was to test the mediating role of postpartum depression between maternal childhood maltreatment and a cascade of negative child outcomes, specifically child exposure to maltreatment, internalizing symptoms, and externalizing symptoms: (1) before and after adjusting for effects of later maternal depression, (2) comparing across sex differences, and (3) examining the relative role of maltreatment subtypes. Postpartum depression was expected to significantly mediate the relationship between maternal childhood maltreatment and child outcomes, above and beyond later maternal depression; to differentially affect female and male children; and to be particularly influenced by particular maltreatment subtypes such as emotional abuse (Minnes et al., 2008).
Methods
Sample
Participants were mothers and children involved in the Environmental Risk (E-Risk) Longitudinal Twin Study, which tracks the development of a birth cohort of British children. This cohort sample was drawn from a larger birth register of twins born in England and Wales in 1994-1995. Full details about the sample are reported elsewhere (Moffitt, 2002). Briefly, the E-Risk sample was constructed in 1999-2000, when 1,116 families (93% of those eligible) with same-sex 5-year-old twins participated in home visit assessments. Families were recruited to represent the UK population of families with newborns in the 1990’s, based on (a) residential location throughout England and Wales and (b) maternal age, with over-selection of teenaged mothers and under-selection of older mothers having twins via assisted reproduction. Higher-risk households were deliberately oversampled to compensate for their selective loss from the register due to non-response and likely attrition over time.
At follow-up, the resulting sample of households represented the full range of socioeconomic conditions in the UK, as captured by a neighborhood-level index (ACORN; A Classification of Residential Neighborhoods, developed by CACI Inc. for commercial use in the UK). ACORN utilizes census and other survey-based geodemographic data to classify neighborhoods across the UK into five categories ranging from “wealthy achievers” (Category 1; 26% E-risk families vs. 26% UK), “urban prosperity” (Category 2; 5% vs 12%) and “comfortably off” (Category 3; 30% vs 27%) to “moderate means” (Category 4; 13% vs. 14%) and “hard-pressed” neighborhoods (Category 5; 26% vs. 21%). The ACORN distribution of households participating in the E-Risk study closely matched the nationwide distribution across all categories (Odgers et al., 2012), though underrepresented the “urban prosperity” category (e.g., young professionals) because such households are likely to be childless.
Procedures
Home visit assessments began in 1999-2000 when children were 5 years old, and follow-up assessments reported in this article were conducted when children were 7 (98% participation), 10 (96% participation), and 12 (96% participation). An overview of procedures at each assessment is publicly available (Medical Research Council, 2017). Informed consent was initially obtained from mothers and assent given by the children through their 12-year assessment. At all phases, procedures were approved by the Joint South London and Maudsley and the Institute of Psychiatry NHS Research Ethics Committee.
Measures
Maternal childhood maltreatment
Mothers were administered the Childhood Trauma Questionnaire (CTQ) as part of a structured face-to-face interview. The CTQ (Bernstein & Fink, 1998) is a widely used 28-item scale that retrospectively measures exposure to maltreatment before the age of 18, including physical abuse, sexual abuse, emotional abuse, emotional neglect, and physical neglect. An overall maltreatment score was available as a continuous variable (with possible scores between 25-125), as were continuous scores for each of the five maltreatment subtypes (with possible scores between 5-25). Continuous scores were used for all main analyses. As in previous E-Risk research (Jaffee et al., 2013) and for descriptive purposes, dichotomous variables were created to reflect moderate-to-severe exposure to each of the childhood maltreatment subtypes, as per CTQ manual cut-offs (Bernstein & Fink, 1998), and substantial exposure to any childhood maltreatment was determined by moderate-to-severe exposure to at least one or more maltreatment subtypes.
Maternal postpartum depression
At the first assessment, mothers were interviewed by a trained clinician regarding their lifetime depressive symptoms up to when the twins were 5 years old, using the standardized Diagnostic Interview Schedule based on DSM-IV criteria (American Psychiatric Association, 2000). Mothers who met criteria for lifetime major depressive disorder were then asked to refer to the Life History Calendar (LHC) in order to specify the timing of their depressive episodes. If mothers did not meet criteria for lifetime major depressive disorder, their score on all reference periods was entered as zero. The LHC is a reliable visual method for recalling the occurrence, timing, and duration of life events, including psychopathology (Caspi et al., 1996). Specifically, the reliability of recalling depressive episodes using the LHC method was separately evaluated using a one-month test-retest and determined to be high at 93% (Kim-Cohen et al., 2005). Mothers were asked to indicate whether they had experienced depression during various reference periods, including the first year following the twins’ birth (i.e., postpartum year). For postpartum depression, maternal reports of depression specifically during the postpartum year were extracted into a dichotomous variable.
Later maternal depression
Later maternal depression was assessed in study mothers using the Diagnostic Interview Schedule and Life History Calendar together across subsequent assessments. A variable was created to reflect the cumulative number of periods in which the mother was depressed between 1 and 10 years of the twins’ lives (1 to 4 years, 5, 6, 7, 8, 9, 10 years), with cumulative periods modeled categorically (ordinally) in all main analyses. This variable did not include maternal depression at 12 years to minimize conflation with reported child outcomes at 12 years. For descriptive purposes, a dichotomous variable reflecting any later maternal depression between 1 to 10 years was also derived.
Child exposure to maltreatment
Child exposure to physical and sexual maltreatment by an adult was assessed using a validated structured interview protocol (Dodge et al., 1990) administered to mothers at each phase of assessment (5 years, 7 years, 10 years, 12 years of twins’ lives). Details of this measure have been previously reported (Arseneault et al., 2011; Jaffee et al., 2013; Polanczyk et al., 2009). Briefly, standardized questions were designed to sensitively and validly elicit information about potential maltreatment (e.g., “Do you remember any time when your child was disciplined severely enough that he or she may have been hurt?” or “Next, I want to ask specifically about harm to your child of a sexual nature.”). At each phase, any positive reports were probed by the interviewer for further details about the incident and to rule out accidental harm or harm from peers. This narrative information was documented in a dossier along with maternal narratives and any referrals made. Each dossier was maintained over phases of assessment and then independently reviewed at 12 years by two clinical psychologists to reach consensus about likelihood of maltreatment occurrence between birth to 12 years of age. Initial inter-rater agreement between coders exceeded 90% and discrepancies were resolved through consensus review. Child exposure to harm was indexed in a three-level categorical variable: none, probable, and definite. Examples of probable harm included instances in which a mother reported spanking her child and leaving marks or bruises, where sexually inappropriate behavior from an adult was suspected and resulted in preventive action, or where social services had been contacted due to concerns about child maltreatment. Examples of definite harm included instances where children sustained serious injuries from neglectful or abusive care, were discovered to be subject to inappropriate sexual contact from an adult, or were already registered on a child protective registry. A dichotomous variable was created to reflect likely maltreatment exposure (probable or definite) versus no such exposure, as in previous research (Jaffee et al., 2004).
Child internalizing and externalizing symptoms
Child internalizing and externalizing symptoms were measured at 12 years using the Child Behavior Checklist (CBCL) (Achenbach, 1991b; Achenbach & Rescorla, 2001) for mothers and the Teacher Report Form (TRF) (Achenbach, 1991a) for schoolteachers. Mother and teacher ratings were summed to provide an overall measure of child symptomatology across settings (Cairns et al., 2005) and in order to incorporate multiple sources of variance, since children may behave or express emotions differently across settings. Continuous scores on withdrawn and anxious/depressed subscales were combined to form the overall internalizing problems scale, while continuous scores on aggressive and delinquent behavior subscales were combined to form the overall externalizing problems scale. Given combined mother-teacher ratings and use of a UK-based sample, overall raw scores were used and reported for all analyses.
Covariates
Maternal age in years reflected the mother’s age when twins were born. Maternal socioeconomic status was indexed using a standardized composite of family income, education, and social class indicators measured at the first assessment. These correlated indicators were found to load significantly onto a single latent factor (Trzesniewski et al., 2006). Based on cohort-wide distribution of scores on this latent factor, mothers were divided into three tiers reflecting overall socioeconomic standing. This three-level categorical variable was coded in this study to reflect increasing levels of socioeconomic disadvantage. Regarding descriptive child characteristics, categorical information on child sex (male versus female) and twin zygosity status (monozygotic versus dizygotic) was also obtained at the first assessment.
Analytic Strategy
Main analyses
Descriptive analyses were initially conducted in SPSS (SPSS IBM v.23, Armonk, NY) to understand patterns of childhood maltreatment and depression as experienced by study mothers, and to characterize outcomes experienced by study children. Then, structural equation modeling (SEM) was conducted using Mplus v.7.3 (Muthén & Muthén, 1998-2014) to test the hypothesized interrelationships between maternal childhood maltreatment, maternal postpartum depression, and child outcomes. SEM allows for associations to be simultaneously evaluated rather than estimating multiple independent regressions, and also permits estimation of both direct and indirect effects (Bollen, 1987). Data from both twins were included in the SEM analyses. To account for nesting within mothers, the dataset was structured at the family level so that each twin’s data were included as variables within the same family case, with elder versus younger twin variables distinguished accordingly. Twin outcomes on a same variable (e.g., externalizing symptoms) were mapped as indicators with equal factor loadings onto one latent outcome variable, as consistent with the common fate model for dyadic data (Ledermann & Kenny, 2012; Peugh et al., 2013), with factor mean and variance set to zero and one, respectively. As a sensitivity analysis for this twin-based approach, a similar structural model was initially tested where only one child from each pair was randomly selected for a singleton analysis without latent twin variables.
To test continuity of maltreatment and related sequelae across generations, preliminary path analyses were conducted using maximum likelihood estimation to examine maternal childhood maltreatment scores as a predictor of each individual latent child outcome. Next, an overall structural model was used to test the extent to which postpartum depression mediates the association between maternal history of childhood maltreatment and child exposure to maltreatment and subsequent child internalizing and externalizing symptoms. Given the inclusion of categorical variables (e.g., postpartum depression) in the overall model, all subsequent analyses used WLSMV (weighted least squares means and variance adjusted) estimation. Specifically, maternal childhood maltreatment was predicted to influence postpartum depression; postpartum depression was predicted to influence child harm exposure between birth and 12 years; and child harm exposure was predicted to subsequently influence child internalizing and externalizing symptoms at 12 years. Direct paths were also estimated between maternal childhood maltreatment and child outcomes, and between postpartum depression and child internalizing and externalizing symptoms, to explore any influences above and beyond the hypothesized pathway. Child internalizing and externalizing symptom residuals were allowed to covary. Within each twin pair, children were expected to be interchangeable—i.e., meaningfully different on outcome variables based on order of birth (elder versus younger). This assumption was explicitly tested using a chi-square difference test, which revealed no significant worsening of model fit for a nested model when outcome means and variances were specified as equal across elder and younger twins, so this specification was preserved throughout model testing. All possible indirect effects of maternal childhood maltreatment on child outcomes were queried.
SEM results were evaluated sequentially. First, to assess overall model fit, comparative fit indices (CFI/TLI, with acceptable values >.90) and the root mean square error of approximation (RMSEA, with acceptable values <.08 and associated 90% CIs) were examined as statistical tests of the goodness of fit of the overall model (Schreiber et al., 2006). Second, the direct effects of maternal childhood maltreatment on child outcomes were examined. Third, the mediating effect of postpartum depression was evaluated. After this initial evaluation, maternal age and socioeconomic disadvantage were entered as covariates for all endogenous variables in the model. Finally, paths were added structurally to test the extent to which later maternal depression might carry the mediating effect of postpartum depression on child outcomes. This final model was again evaluated for overall fit as well as its direct and indirect effects. All effects were interpreted using standardized coefficients depending on the scale (continuous or categorical) of the independent variable.
Testing for moderation by child sex
To probe for potential differences in susceptibility to maternal risk across child sex, multiple-group testing was performed with the final model to determine whether structural pathways differed across male and female children. Chi-square difference tests were conducted to compare a model in which all structural paths leading to child outcomes were constrained across male and female groups, against a model in which these parameters were free to vary. In each model, pathways between maternal variables (e.g., maternal trauma to postpartum depression) were fixed as equal across groups, as they were not theoretically suspected to differ across male and female children. All other parameters were free to vary. If the chi-square difference statistic was non-significant, the more restricted sex-neutral model was considered acceptable given no substantial worsening in fit; conversely, a significant result would suggest that imposing parameter restrictions led to significantly worsened model fit, such that the sexes should be considered separately.
Examining role of maltreatment subtypes
To evaluate the relative impact of specific forms of maternal childhood maltreatment on child outcomes, both directly and indirectly through postpartum depression, a structural model based on the adjusted final model was tested to account for maltreatment subtypes using five predictor variables decomposed from the overall maltreatment variable (physical abuse; sexual abuse; emotional abuse; emotional neglect; physical neglect). Inter-correlations between maltreatment subtypes were automatically factored into the model given their specification as exogenous variables.
Results
Missing Data
Among the 1,116 E-Risk families, a small subset had CTQ data completed by an individual other than the mother (e.g., father, grandparent). These cases were excluded from the present study because the CTQ data would not reflect maternal trauma, leaving 1,038 families with CTQ data completed by the mother herself. Of these, 22 cases had missing maternal data (eight on postpartum depression and 14 on CTQ) and were excluded from analysis as WLSMV would handle this data using pairwise deletion, resulting in a final sample of 1,016 mothers and their children. The subsample with missing data did not differ significantly from the final analytic sample on socioeconomic categories, child sex, twin zygosity, or maternal age.
Descriptive Findings
Sample characteristics are summarized in Table 1 for mothers and Table 2 for children. Of note, 18% (N=180) of mothers endorsed clinical depression in the postpartum year, and the majority of these women (83%, N=150) reported at least some depression in later years, while 17% of mothers (N=30) reported depression only in the postpartum year. Almost one in four mothers (24%, N=248) experienced at least one type of childhood maltreatment at the moderate/severe level. The most common maltreatment subtype was emotional neglect (16%), followed by emotional abuse and sexual abuse (both 11%); physical abuse was reported by 8% of mothers and 6% reported physical neglect. Among the children, there was a relatively even balance across gender as well as across identical versus fraternal twins. One in five children was determined to have experienced likely harm before 12 years of age.
Table 1. Maternal sample characteristics.
| Maternal variables | N = 1,016 |
|---|---|
| Age; mean (s.d.) | 28.0 (5.9) |
| Socioeconomic risk | |
| High | 33% (330) |
| Moderate | 33% (336) |
| Low | 34% (350) |
| Childhood maltreatment (yes/no) | |
| Any | 24% (248) |
| Physical abuse | 8% (79) |
| Sexual abuse | 10% (105) |
| Emotional abuse | 11% (107) |
| Physical neglect | 6% (59) |
| Emotional neglect | 16% (161) |
| Postpartum depression | 18% (180) |
| Any later depression | 39% (396) |
Table 2. Child sample characteristics.
| Child variables | N = 2,032 |
|---|---|
| Gender | |
| Female | 51% (1044) |
| Male | 49% (988) |
| Twin zygosity | |
| Identical | 54% (1102) |
| Fraternal | 46% (930) |
| Harm exposure between 0-12 years | 21% (422) |
| Internalizing symptoms at 12 years; mean (s.d.) | 4.7 (3.8) |
| Externalizing symptoms at 12 years; mean (s.d.) | 6.9 (6.9) |
Among mothers who reported postpartum depression, 40% (N=72/180) had at least one child who was later exposed to maltreatment, compared to 22% (N=188/836) among mothers without postpartum depression. Even in cases of discordant maltreatment exposure where only one twin was exposed to maltreatment, independent sample t-tests indicated the twin who was exposed to maltreatment had slightly higher but not significantly different internalizing or externalizing scores than the non-exposed twin, suggesting that a shared context where at least one child is being maltreated has consequences for both twins.
Structural Model Findings
Continuity of maltreatment and related sequelae across generations
In individual path analyses, maternal childhood maltreatment significantly predicted children’s harm exposure (B=.32, p<.001), internalizing symptoms (B=.33, p<.001) and externalizing symptoms (B=.35, p<.001), supporting continuity of maltreatment and related sequelae in the next generation. These significant paths persisted even when adjusted for maternal age and socioeconomic disadvantage, which would be later added to the full structural model.
Mediating effect of postpartum depression on child outcomes
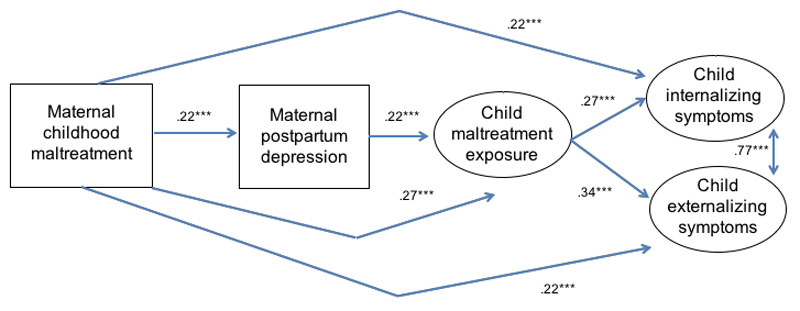
The main structural model with postpartum depression (Figure 1; significant paths shown, with standardized coefficients) fit the data well, X2(20)=60.06, p<.001, RMSEA=.04 [.032-.058], CFI/TLI=.99/.98, explaining 15% of variance in child harm exposure, 20% of variance in child internalizing symptoms, and 24% of variance in child externalizing symptoms (all p<.001). With regards to direct effects, maternal childhood maltreatment significantly predicted postpartum depression (B=.22, p<.001). In turn, postpartum depression significantly predicted child exposure to harm (B=.22, p<.001), which in turn predicted child internalizing (B=.27, p<.001) and externalizing symptoms (B=.34, p<.001). Maternal childhood maltreatment also had significant direct paths to each child outcome (p<.001, see Figure 1 for standardized coefficients).
Figure 1. Main structural model with postpartum depression as mediator.
Rectangles represent observed variables; ovals represent latent variables on which younger and elder twin scores have been regressed (paths not shown to improve readability). Solid lines represent paths with coefficients significant at p<.05* or p<.001***, with only significant paths shown in the model.
In terms of mediating effects, there was a significant indirect effect of maternal childhood maltreatment on child harm exposure through postpartum depression (B= .05, p=.002). For child internalizing symptoms, total indirect effects of maternal childhood maltreatment through the hypothesized model were also significant (B=.11, p<.001). Decomposition of specific indirect effects showed significant mediating pathways through the combined pathway of postpartum depression → subsequent child harm (B=.01, p=.011) and through child harm exposure alone (B=.07, p<.001). The indirect pathway through postpartum depression without child harm exposure was non-significant. For child externalizing symptoms, total indirect effects were similarly significant (B=.12, p<.001) and decomposition of specific indirect effects again showed significant mediating pathways through postpartum depression → subsequent child harm (B=.02, p=.004) and through child harm exposure alone (B=.09, p<.001). The indirect pathway through postpartum depression without child harm exposure was non-significant.
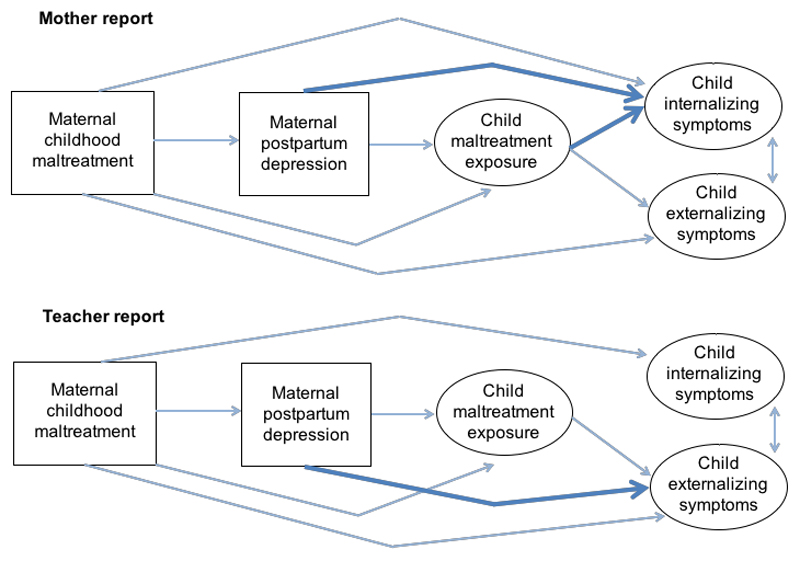
Sensitivity analyses
First, an analysis using only one randomly selected child from each twin pair revealed the same pattern of significant direct and indirect effects (not shown) as in the twin-based model, thus the more comprehensive twin-based approach was conserved in subsequent analyses. Second, the comprehensive model was examined separately based on mother- versus teacher-only reports of child symptoms, as opposed to combined reports. Each model continued to fit well, though minor pathway differences were found by informant (as shown in Figure 2). Specifically, when mothers reported on child symptoms, all model pathways were significant as before, but postpartum depression also predicted child internalizing symptoms directly, and thus significantly mediated between maternal childhood maltreatment and child internalizing symptoms above and beyond child harm exposure. When teachers reported on child symptoms, the pathway from child harm exposure to internalizing symptoms was not significant; however, postpartum depression predicted child externalizing symptoms directly, and thus significantly mediated between maternal childhood maltreatment and child externalizing symptoms above and beyond child harm exposure. While these results were used to contextualize main findings (see Discussion), combined reports across mothers and teachers were used in subsequent analyses since a comprehensive measure of child symptoms across settings was desired and different reporters are able to provide complementary evidence about children’s emotional/behavioral problems (Cairns et al., 2005).
Figure 2. Sensitivity analyses of mother- versus teacher-only informant reports.
Rectangles represent observed variables; ovals represent latent variables on which younger and elder twin scores have been regressed (paths not shown to improve readability). Solid lines represent significant paths. Of note, bolded lines represent significant paths that were different across child outcomes as measured by mother- versus teacher-only reports.
Adjusting for sociodemographic factors
The model retained good fit even when maternal age and socioeconomic disadvantage were added as covariates, X2(26)=64.76, p<.001, RMSEA=.038 [.027-.050], CFI/TLI=.99/.98, and the overall pattern of significant direct and indirect effects remained the same. In addition, socioeconomic disadvantage significantly predicted each of the child outcomes (B=.11, p=.010 for harm exposure; B=.16, p=.002 for internalizing symptoms; B=.26, p<.001 for externalizing symptoms), while maternal age was a significant predictor of child harm exposure (B=-.12, p=.004) such that younger mothers had a higher risk of later child harm. This adjusted model explained 19% of variance in child harm exposure, 22% of variance in child internalizing symptoms, and 30% of variance in child externalizing symptoms (all p<.001).
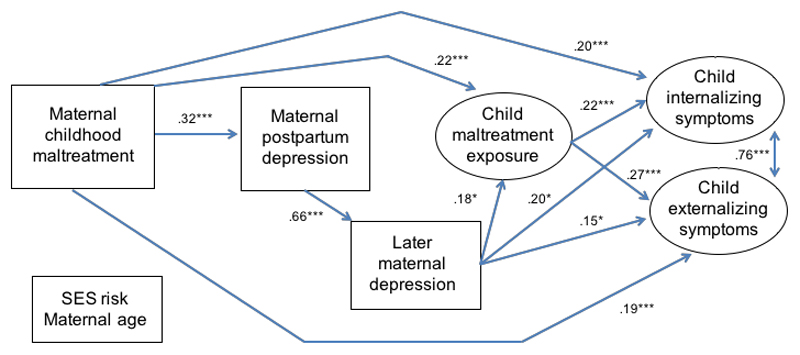
Exploring the potential role of later maternal depression
When later maternal depression was included structurally in the adjusted model so it followed postpartum depression and was also allowed to predict each of the child outcomes (see Figure 3; significant paths shown, with standardized coefficients), the resulting model continued to fit the data well, X2(30)=96.35, p<.001, RMSEA=.047 [.036-.057], CFI/TLI=.98/.97. In this model, maternal childhood maltreatment significantly predicted postpartum depression (B=.32, p<.001). Postpartum depression then significantly predicted later maternal depression (B=.66, p<.001) which in turn predicted child harm exposure (B=.18, p=.027), internalizing symptoms (B=.20, p=.016) and externalizing symptoms (B=.15, p=.033); however, postpartum depression was no longer a significant direct predictor of child outcomes. Maternal childhood maltreatment continued to have significant direct paths to each of the child outcomes (p<.001, see Figure 3 for coefficients). Socioeconomic disadvantage predicted later maternal depression (B=.13, p=.004), though not postpartum depression.
Figure 3. Adjusted structural model including later maternal depression.
Rectangles represent observed variables; ovals represent latent variables on which younger and elder twin scores have been regressed (paths not shown to improve readability). Solid lines represent paths with coefficients significant at p<.05* or p<.001***, with only significant paths shown in the model.
In terms of mediating effects, there was a significant total indirect effect of maternal childhood maltreatment for child harm exposure (B=.07, p<.001), specifically through the pathway that included both postpartum depression and later maternal depression (B=.04, p=.032). For child internalizing symptoms, there was a significant total indirect effect of maternal childhood maltreatment (B=.10, p<.001), through the specific pathways of postpartum depression → later maternal depression (B=.05, p=.021) and through child harm exposure only (B=.05, p=.004), but not solely through postpartum depression. The indirect pathway through postpartum depression → later maternal depression → child harm exposure was also marginally insignificant (B=.008, p=.080) after adjusting for covariates. For child externalizing symptoms, there was a significant total indirect effect of maternal childhood maltreatment (B=.11, p<.001), with specific pathways through postpartum depression → later maternal depression (B=.03, p=.039), postpartum depression → later maternal depression → child harm exposure (B=.01, p=.046), and through child harm exposure only (B=.06, p<.001), but not solely through postpartum depression. With the inclusion of later maternal depression, the model explained 20% of variance in child harm exposure, 24% of variance in child internalizing symptoms, and 34% of variance in child externalizing symptoms (all p<.001).
Testing the moderating effects of child sex
Means and variances were allowed to vary across male and female children; as expected, boys on average had higher externalizing symptoms than girls. When the moderating effect of child sex on structural paths was tested, chi-square difference tests revealed a significant worsening in model fit from the freed model (in which all structural paths to child outcomes were allowed to vary across males and females) to the more constrained model (in which these paths were set as equal), X2∆(17)=29.41, p=.031. However, follow-up difference tests that constrained paths either from (1) maternal childhood maltreatment to child outcomes (direct effects) or (2) postpartum or later maternal depression to child outcomes (mediator effects) were non-significant, suggesting these paths were comparable across male and female children, at least when adjusting for all paths considered. Significant worsening in fit was found only when (3) paths from maternal demographic covariates to child outcomes were constrained across male and female children, X2∆(6)=18.43, p=.005. Inspection of unconstrained path coefficients between groups revealed that in this model, maternal socioeconomic disadvantage predicted child harm exposure among males (p=.005) but not females (p=.993); internalizing symptoms for females (p=.005) but not males (p=.282); and externalizing symptoms for both sexes (p<.001). Younger maternal age at birth significantly predicted child harm exposure only for females (p<.001). These findings suggest some differential susceptibility of male versus female children to contextual risks but not to the overall intergenerational transmission of maltreatment through maternal depression.
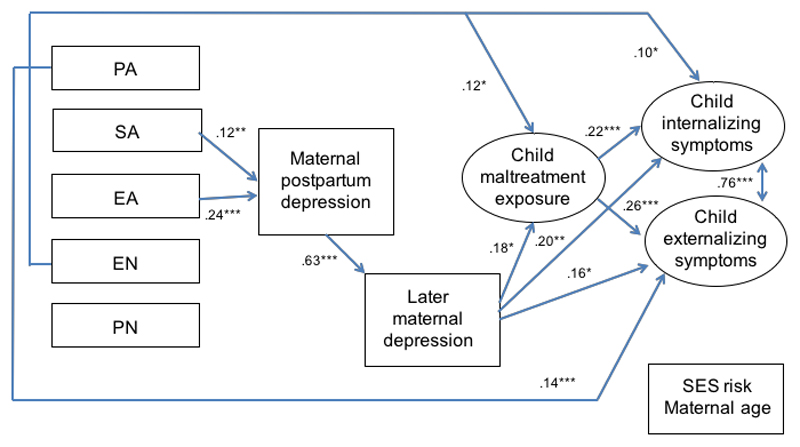
Examining maltreatment subtypes
When all maltreatment subtypes were entered instead of overall maltreatment in the final structural model with covariates (Figure 4), the resulting model fit the data well, X2(46)=104.94, p<.001, RMSEA=.036 [.027-.045], CFI/TLI=.98/.96, and explained comparable variance in child outcomes as the overall maltreatment model, with similar pathways. Among subtypes, maternal histories of emotional abuse and sexual abuse were significant predictors of postpartum depression (B=.24, p<.001 for emotional abuse; B=.12, p=.005 for sexual abuse) above and beyond the other subtypes. Additionally, maternal history of emotional neglect had significant direct paths to child harm exposure (B=.12, p=.017), child internalizing symptoms (B=.10, p=.042), and marginally externalizing symptoms (B=.07, p=.060). Maternal history of physical abuse had a significant direct relationship with child externalizing symptoms (B=.14, p<.001).
Figure 4. Examining the relative contribution of maltreatment subtypes.
Rectangles represent observed variables; ovals represent latent variables on which younger and elder twin scores have been regressed (paths not shown to improve readability). Solid lines represent paths with coefficients significant at p<.05* or p<.001***, with only significant paths shown in the model.
Discussion
Summary and Integration
This study examined the mediating role of postpartum and subsequent depression in the intergenerational transmission of maltreatment and its psychological sequelae. It drew on a large birth cohort that was nationally representative of household conditions across the UK, in which mothers were not selected for their trauma histories or depression risk. The fact that almost one in five of mothers endorsed clinically significant depression in the postpartum year and nearly one in four had been exposed to at least one substantial form of childhood abuse or neglect supports the prevalence of these exposures at a population level and a need to understand how such exposures might affect outcomes in the next generation.
As expected, maternal childhood maltreatment was associated with greater risk for postpartum depression. Mothers who reported postpartum depression had nearly twice the prevalence (40% vs. 22%) of having a child exposed to later maltreatment. In SEM analyses, postpartum depression significantly mediated the relationship between maternal childhood maltreatment and child harm exposure, with subsequent influences on child internalizing and externalizing symptoms at 12 years. This mediating effect persisted even when accounting for socioeconomic disadvantage, suggesting that structural links observed between maternal childhood maltreatment, postpartum depression, and child outcomes were not simply explained by underlying levels of environmental adversity. These core results integrate findings from two separate streams of literature towards a more nuanced framework of intergenerational transmission, where (1) history of childhood maltreatment has been associated with increased risk for postpartum depression (Alvarez-Segura et al., 2014; Choi & Sikkema, 2016), and (2) postpartum depression has been associated with a range of long-term child psychological outcomes (Hay et al., 2003; Murray et al., 2010). In this study, postpartum depression was linked to child outcomes mainly through risk of child harm, a cascade consistent with literature on maternal depression in the perinatal period (Pawlby et al., 2011; Plant et al., 2017).
Contrary to the sensitive window hypothesis, results indicated the mediating effect of postpartum depression from maternal childhood maltreatment on child harm and subsequent outcomes was carried by later maternal depression, consistent with recent literature (Agnafors et al., 2012; Sanger et al., 2015). Most women with postpartum depression experienced at least some depression in later years, highlighting the persistent nature of maternal depression beyond the postpartum period. Some mothers who continue to be depressed may directly engage in abusive behavior, perhaps due to limited emotional resources in response to child misbehavior (Shay & Knutson, 2008); however, an alternative is they may be less able to actively monitor child safety or effectively protect the child from a violent partner or abusive acquaintance. The stronger effects of later maternal depression relative to postpartum depression might be explained in various ways. First, its occurrence is more proximal to child symptoms being assessed; developmental plasticity may have allowed intervening events to continue shaping outcomes beyond the postpartum period (Champagne, 2010). Second, it could be that cumulative exposure, as indexed by later maternal depression following postpartum depression, is particularly harmful (Halligan et al., 2007; Hay et al., 2008). Third, an interaction effect may exist where early exposure to postpartum depression may sensitize children with genetic vulnerabilities to develop psychopathology but only when encountering later stressors such as continued maternal depression (Starr et al., 2014), representing a G x E x E interaction.
Moreover, findings suggested the overall intergenerational transmission pathway was robust to sex differences. Differential susceptibility of boys to maternal depression or history of childhood maltreatment was not supported in the current data, despite prior evidence of potential sex differences (Choe et al., 2013; McGinnis et al., 2015). Lack of findings could reflect timing of child outcomes assessed. Another British longitudinal cohort (Quarini et al., 2016) also revealed no sex differences related to maternal postpartum depression for child depression outcomes at 12 years; rather, potentially latent differences emerged at 18 years, with male children showing greater vulnerability following maternal postpartum depression.
When different maternal childhood maltreatment subtypes were considered together, emotional abuse emerged above and beyond other subtypes as a significant predictor of postpartum depression. While consistent with prior literature (Minnes et al., 2008), the present study extended this finding by examining its implications for child outcomes. Literature increasingly recognizes the uniquely harmful effects of emotional maltreatment (Hibbard et al., 2012; Spinazzola et al., 2014). Given that maltreatment subtypes often co-occur rather than occur in isolation, a history of emotional abuse may also indicate the early maltreating environment was particularly noxious, containing a strong psychological component in addition to external harm. For clinicians, inquiring about childhood emotional abuse and neglect in addition to reports of past physical or sexual abuse may yield nuanced insights about mothers and children at greatest risk. Studying additional dimensions of maltreatment exposure—including the timing, severity, duration, and multiplicity of these experiences (Teicher & Parigger, 2015)—and how they uniquely perturb neurodevelopmental systems that may affect later psychopathology and/or parenting may illuminate further opportunities for prevention.
It must be noted that maternal childhood maltreatment continued to predict child outcomes above and beyond the maternal depression pathway, suggesting only partial mediation. This confirms how intergenerational transmission is a multifactorial phenomenon. Other mediators of this transmission could include hostile or controlling parenting styles, maternal substance abuse, or mental health disorders such as PTSD. Broader contextual factors such as domestic violence, household food insecurity, and neighborhood environments previously investigated in the E-Risk cohort (Belsky et al., 2010; Jaffee et al., 2007; Jaffee et al., 2002) may also be relevant, though our goal was to specifically ascertain timing effects of maternal depression. Algorithms of combined risk developed using computational learning methods (Mair et al., 2000) may be a promising direction for comprehensive prevention efforts, in which maternal depression and other contextual factors should be included as key indicators.
Furthermore, while not the focus of this study, it must be acknowledged that even in the presence of maternal risks, there was still substantial discontinuity in the transmission of maltreatment and related child outcomes. Mechanisms for resilience have been previously described in the literature (Cicchetti, 2013). Of relevance to the postpartum period, resilient child outcomes may be more likely when depressed mothers with maltreatment histories draw upon memories from early positive interactions with caregivers as they interact with their infants (Lieberman, Padrón, Van Horn, & Harris, 2005) and when they continue displaying positive affect towards their infants despite some negative parenting behavior (Martinez-Torteya et al., 2014). Understanding how to promote these relational capacities in the presence of depressive symptoms may yield novel directions for intervening with mothers at risk.
Limitations and Future Directions
Several limitations of this study should be noted. First of all, study assessments did not index severity of postpartum depression beyond threshold for diagnosis, which would capture a range of symptomatology and potentially be more informative in predicting later outcomes (Fihrer et al., 2009). Given the study’s initial focus on specific maternal risk factors such as depression, comprehensive psychiatric evaluation was not undertaken; thus, other mental health morbidities such as PTSD or anxiety that could also influence risk transmission were not measured from the outset. Maternal childhood maltreatment was also measured retrospectively with the CTQ, which may be subject to underreporting (Brewin et al., 1993) though has been found to correspond well to other sources of maltreatment information (Bernstein et al., 1997) and should be considered a reasonable index of actual exposure. Similarly, mothers reported on postpartum depressive episodes as part of a retrospective clinical interview. Though this validated measure has been shown to increase accuracy of recall (Caspi et al., 1996), recollection of prior depressive episodes may be biased by current mood and functioning at time of assessment. Findings would benefit from replication and extension using cohort studies with prospective data on maternal risk factors starting before birth. Indeed, our results converge with a recent study examining antenatal and postpartum depression in the transmission of negative outcomes in a prospective cohort (Plant et al., 2017).
Second, as the E-Risk study was conducted in the UK, results and policy implications may not be generalizable to other settings. For example, maternal and child health care systems in the UK are nationally managed, such that average British mothers may have greater access than mothers in the US to supports and services throughout the course of their children’s development, potentially mitigating intergenerational risks. Additionally, the use of a twin-based sample could also limit generalizability to singleton families, despite sensitivity analyses using only one randomly selected twin from each pair. For instance, mothers of twins may experience higher levels of depression (Thorpe et al., 1991). However, findings from this study resonate with others that have observed intergenerational links between maternal childhood maltreatment, maternal mental health, and child psychological outcomes in non-twin families (Plant et al., 2017; Roberts et al., 2015).
Third, there was potential for informant bias since mothers reported on their own maltreatment history and depression as well as children’s outcomes, albeit at different time points. We attempted to mitigate this by separately testing the model using only mother or teacher reports of child symptoms. Results suggested that the proposed intergenerational pathway to child externalizing symptoms was robust across informants and particularly salient when teachers reported these symptoms, while the pathway to child internalizing symptoms was only significant when mothers reported these symptoms. Differential pathway results may reflect how externalizing symptoms are more obvious across settings, while mothers may be more likely than teachers to observe subtle internalizing symptoms within home contexts. Drawing on multiple informants and/or objective child assessments in future studies will clarify whether current findings for child internalizing symptoms are better explained by informant bias or actual contextual variation. In addition, child harm exposure over time was documented carefully by trained clinicians but did rely on caregiver self-report, which may result in biased estimates, though formal child registries may also underestimate actual cases compared to sensitively elicited personal reports (Gilbert et al., 2009).
This study did not explicitly rule out genetic mediation of intergenerational transmission, in which genetic factors shared between mothers and their children predispose them similarly to elicit maltreatment from their environment and/or demonstrate overall psychological vulnerability. For example, difficult temperament—a putatively heritable characteristic—may elicit both negative parenting behavior and parental depression (Dix & Yan, 2014). To examine genetic versus environmental mediation, studies could draw upon adoptive mother-child cohorts (McAdams et al., 2015) or recruit egg donor in vitro fertilization (IVF) samples where the mother carries the pregnancy without being genetically related to the child (Thapar et al., 2009), to examine whether evidence converges across these types of studies. Finally, while postpartum depression appeared to partially link maternal trauma and child outcomes, it could reflect causal effects of maternal depression prior to birth (e.g., during pregnancy), though we were not able to explicitly test this in our study. Future research should factor in the previously observed role of antenatal depression in intergenerational transmission (Plant et al., 2013; Plant et al., 2017) and test relative contributions of antenatal, postpartum, and later maternal depression to refine timing of interventions, as well as potentially synergistic effects of combined maternal depression and maltreatment histories.
Implications
For treatment and prevention, this study has highlighted the predictive utility of postpartum depression for the intergenerational transmission of maltreatment and its sequelae. Elevated maternal depressive symptoms at any point after birth appear to increase risk of intergenerational transmission, and these symptoms may appear as early as the postpartum period. Postpartum depression could serve as a useful early marker—that is, part of a clinical endophenotype—for intergenerational risk, one amenable to detection and intervention. This aligns with national recommendations (Siu & the U.S. Preventive Services Task Force, 2016) to screen for postpartum depression when follow-up options are available. Postpartum interventions may be strategic since mothers may be open to treatment and support during this time (Leis et al., 2009). For example, efforts have been made to incorporate depression treatment into home visiting programs (Ammerman et al., 2013) but notably program effects appear to be attenuated by maternal histories of maltreatment (Ammerman et al., 2016), suggesting that depressed new mothers with trauma histories may require specialized attention and integrated interventions that simultaneously address trauma and mental health. Among psychotherapeutic options, one example is mindfulness-based cognitive therapy (MBCT), which was developed to prevent depression relapse (Morgan, 2003) and may be especially effective for individuals with childhood trauma (Williams et al., 2014). MBCT has demonstrated promise for preventing perinatal relapse in women with prior depressive episodes (Dimidjian et al., 2016). Mothers with trauma histories could benefit from such intervention but it is unknown whether effects would extend beyond the postpartum period into later years.
Identifying and treating maternal depression in the earliest years may be an important way to interrupt cycles of trauma and improve maternal and child outcomes: an efficient strategy from a public health standpoint. However, postpartum depression may be most predictive of poor child outcomes within a course of maternal depression that is ongoing or recurrent, often including depressive episodes that onset before and/or during pregnancy. Research increasingly suggests that postpartum depression is not a homogeneous condition (Kettunen et al., 2014; Vliegen et al., 2014). For a subset of women—such as those with maltreatment histories (Nanni et al., 2012)—postpartum depression may reflect more chronic lifelong vulnerability for depression. These mothers should be clinically distinguished from those experiencing a more “classic” state of postpartum depression associated with hormonal shifts and acute life transition. While both groups require support and intervention, this study suggests there is a two-generation impetus for targeting mothers with chronic trajectories. Given the likelihood of recurrent depression, mothers with maltreatment histories should be monitored for depressive symptoms beginning in pregnancy and at later points in their child’s life, and treated accordingly when symptoms elevate. Ob/gyn and pediatric settings offer a prime opportunity to detect ongoing maternal depression and related risk factors that could affect child development (Earls, 2010).
Conclusion
This study found that postpartum depression, especially when followed by recurrent maternal depression, plays a mediating role in the intergenerational transmission of maltreatment. Mothers who have experienced childhood maltreatment are at increased risk for postpartum depression and their postpartum depression may also be more persistent and difficult to resolve, with downstream consequences for children’s wellbeing. Notably, this study contributes to a growing body of evidence that children’s risk for exposure to maltreatment and subsequent mental health problems can be predicted as early as the perinatal period, offering a promising window of opportunity for prevention. Some gaps in knowledge remain, including whether and how targeting early maternal depression can yield enduring effects for children, or require maintenance throughout childhood. Nonetheless, interventions that address both depression and trauma in the context of caregiving are critically needed for mothers in the perinatal period (Ammerman et al., 2016; Muzik et al., 2015) and may assist ongoing efforts to interrupt intergenerational cycles of maltreatment.
Acknowledgements
The E-Risk Study is funded by the Medical Research Council (UK MRC grants G9806489 and 61002190) and the NICHD (HD077482). We are grateful to Study mothers, twins, and twins' teachers for their participation. Additional thanks to Avshalom Caspi, Michael Rutter, and Robert Plomin, to Thomas Achenbach for kind permission to adapt the Child Behavior Checklist, and to the E-Risk team for their dedication, hard work, and insights. KWC was supported by a Doris Duke Fellowship for the Promotion of Child Well-Being from Chapin Hall and Global Health Doctoral Scholar Dissertation Grant from Duke University.
Bibliography
- Achenbach TM. Manual for Teacher’s Report Form and 1991 Profile. Burlington, VT: Department of Psychiatry, University of Vermont; 1991a. [Google Scholar]
- Achenbach TM. Manual for the Child Behavior Checklist/4-18 and 1991 profile. Burlington, VT: Department of Psychiatry, University of Vermont; 1991b. [Google Scholar]
- Achenbach TM, Rescorla L. ASEBA School-Age Forms & Profiles. Burlington, VT: Department of Psychiatry, University of Vermont; 2001. [Google Scholar]
- Agnafors S, Sydsjö G, deKeyser L, Svedin CG. Symptoms of depression postpartum and 12 years later-associations to child mental health at 12 years of age. Maternal and Child Health Journal. 2012;17(3):405–414. doi: 10.1007/s10995-012-0985-z. [DOI] [PubMed] [Google Scholar]
- Ainsworth MS. Infant–mother attachment. American Psychologist. 1979;34(10):932–937. doi: 10.1037//0003-066x.34.10.932. [DOI] [PubMed] [Google Scholar]
- Alvarez-Segura M, Garcia-Esteve L, Torres A, Plaza A, Imaz ML, Hermida-Barros L, San L, Burtchen N. Are women with a history of abuse more vulnerable to perinatal depressive symptoms? A systematic review. Archives of Women's Mental Health. 2014;17(5):343–357. doi: 10.1007/s00737-014-0440-9. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. (4th ed.) Washington, DC: 2000. [Google Scholar]
- Ammerman RT, Peugh JL, Teeters AR, Putnam FW, Van Ginkel JB. Child maltreatment history and response to CBT treatment in depressed mothers participating in home visiting. Journal of Interpersonal Violence. 2016;31(5):774–791. doi: 10.1177/0886260514556769. [DOI] [PubMed] [Google Scholar]
- Ammerman RT, Putnam FW, Altaye M, Stevens J, Teeters AR, Van Ginkel JB. A clinical trial of in-home CBT for depressed mothers in home visitation. Behavior Therapy. 2013;44(3):359–372. doi: 10.1016/j.beth.2013.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arseneault L, Cannon M, Fisher HL, Polanczyk G, Moffitt TE, Caspi A. Childhood trauma and children's emerging psychotic symptoms: A genetically sensitive longitudinal cohort study. American Journal of Psychiatry. 2011;168(1):65–72. doi: 10.1176/appi.ajp.2010.10040567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagner DM, Pettit JW, Lewinsohn PM, Seeley JR. Effect of maternal depression on child behavior: A sensitive period? Journal of the American Academy of Child & Adolescent Psychiatry. 2010;49(7):699–707. doi: 10.1016/j.jaac.2010.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandura A. Aggression: A Social Learning Analysis. Englewood Cliffs, NJ: Prentice-Hall; 1973. [Google Scholar]
- Barker ED. The duration and timing of maternal depression as a moderator of the relationship between dependent interpersonal stress, contextual risk and early child dysregulation. Psychological Medicine. 2013;43(08):1587–1596. doi: 10.1017/S0033291712002450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belsky DW, Moffitt TE, Arseneault L, Melchior M, Caspi A. Context and Sequelae of Food Insecurity in Children's Development. American Journal of Epidemiology. 2010;172(7):809–818. doi: 10.1093/aje/kwq201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein DP, Ahluvalia T, Pogge D, Handelsman L. Validity of the Childhood Trauma Questionnaire in an adolescent psychiatric population. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36(3):340–348. doi: 10.1097/00004583-199703000-00012. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Fink L. Childhood Trauma Questionnaire: A retrospective self-report manual. San Antonio, TX: The Psychological Corporation; 1998. [Google Scholar]
- Bert SC, Guner BM, Lanzi RG. The influence of maternal history of abuse on parenting knowledge and behavior. Family Relations. 2009;58(2):176–187. doi: 10.1111/j.1741-3729.2008.00545.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berzenski SR, Yates TM, Egeland B. A multidimensional view of continuity in intergenerational transmission of child maltreatment. In: Korbin JE, Krugman RD, editors. Handbook of Child Maltreatment. Vol. 2. Netherlands: Springer; 2014. [Google Scholar]
- Bollen KA. Total, direct, and indirect effects in structural equation models. Sociological Methodology. 1987;17(1):37–69. [Google Scholar]
- Bowlby J. Attachment theory and its therapeutic implications. Adolescent Psychiatry. 1978;6:5–33. [PubMed] [Google Scholar]
- Brewin CR, Andrews B, Gotlib IH. Psychopathology and early experience: a reappraisal of retrospective reports. Psychological Bulletin. 1993;113(1):82–98. doi: 10.1037/0033-2909.113.1.82. [DOI] [PubMed] [Google Scholar]
- Brown S, Lumley J. Physical health problems after childbirth and maternal depression at six to seven months postpartum. BJOG: An International Journal of Obstetrics & Gynaecology. 2000;107(10):1194–1201. doi: 10.1111/j.1471-0528.2000.tb11607.x. [DOI] [PubMed] [Google Scholar]
- Bureau JF, Easterbrooks MA, Lyons-Ruth K. Maternal depressive symptoms in infancy: unique contribution to children's depressive symptoms in childhood and adolescence? Dev Psychopathol. 2009;21(2):519–537. doi: 10.1017/S0954579409000285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cairns AM, Mok JYQ, Welbury RR. Injuries to the head, face, mouth and neck in physically abused children in a community setting. International Journal of Paediatric Dentistry. 2005;15(5):310–318. doi: 10.1111/j.1365-263X.2005.00661.x. [DOI] [PubMed] [Google Scholar]
- Campbell SB, Cohn JF, Flanagan C, Popper S, Meyers T. Course and correlates of postpartum depression during the transition to parenthood. Development and Psychopathology. 1992;4(01):29–47. [Google Scholar]
- Caspi A, Moffitt TE, Thornton A, Freedman D, Amell JW, Harrington H, Smeijers J, Silva PA. The life history calendar: A research and clinical assessment method for collecting retrospective event-history data. International Journal of Methods in Psychiatric Research. 1996;6(2):101–114. [Google Scholar]
- Choe DE, Sameroff AJ, McDonough SC. Infant functional regulatory problems and gender moderate bidirectional effects between externalizing behavior and maternal depressive symptoms. Infant Behavior and Development. 2013;36(3):307–318. doi: 10.1016/j.infbeh.2013.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi KW, Sikkema KJ. Childhood maltreatment and perinatal mood and anxiety disorders: A systematic review. Trauma Violence Abuse. 2016;17(5):427–453. doi: 10.1177/1524838015584369. [DOI] [PubMed] [Google Scholar]
- Choi KW, Sikkema KJ, Vythilingum B, Geerts L, Faure SC, Watt MH, Roos A, Stein DJ. Maternal childhood trauma, postpartum depression, and infant outcomes: Avoidant affective processing as a potential mechanism. Journal of Affective Disorders. 2017;211:107–115. doi: 10.1016/j.jad.2017.01.004. [DOI] [PubMed] [Google Scholar]
- Cicchetti D. Annual research review: Resilient functioning in maltreated children–past, present, and future perspectives. Journal of Child Psychology and Psychiatry. 2013;54(4):402–422. doi: 10.1111/j.1469-7610.2012.02608.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti D. Socioemotional, personality, and biological development: Illustrations from a multilevel developmental psychopathology perspective on child maltreatment. Annual Reviews of Psychology. 2016;67:187–211. doi: 10.1146/annurev-psych-122414-033259. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Toth SL. Child maltreatment. Annual Review of Clinical Psychology. 2005;1:409–438. doi: 10.1146/annurev.clinpsy.1.102803.144029. [DOI] [PubMed] [Google Scholar]
- DiLillo D, Tremblay GC, Peterson L. Linking childhood sexual abuse and abusive parenting: The mediating role of maternal anger. Child Abuse & Neglect. 2000;24(6):767–779. doi: 10.1016/s0145-2134(00)00138-1. [DOI] [PubMed] [Google Scholar]
- Dimidjian S, Goodman SH, Felder JN, Gallop R, Brown AP, Beck A. Staying well during pregnancy and the postpartum: A pilot randomized trial of mindfulness-based cognitive therapy for the prevention of depressive relapse/recurrence. Journal of Consulting and Clinical Psychology. 2016;84(2):134–145. doi: 10.1037/ccp0000068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dix T, Yan N. Mothers' depressive symptoms and infant negative emotionality in the prediction of child adjustment at age 3: Testing the maternal reactivity and child vulnerability hypotheses. Development and Psychopathology. 2014;26(01):111–124. doi: 10.1017/S0954579413000898. [DOI] [PubMed] [Google Scholar]
- Dixon L, Browne K, Hamilton-Giachritsis C. Risk factors of parents abused as children: a mediational analysis of the intergenerational continuity of child maltreatment (Part I) Journal of Child Psychology and Psychiatry. 2005;46(1):47–57. doi: 10.1111/j.1469-7610.2004.00339.x. [DOI] [PubMed] [Google Scholar]
- Dodge KA, Bates JE, Pettit GS. Mechanisms in the cycle of violence. Science. 1990;250(4988):1678–1683. doi: 10.1126/science.2270481. [DOI] [PubMed] [Google Scholar]
- Earls MF. Incorporating recognition and management of perinatal and postpartum depression into pediatric practice. Pediatrics. 2010;126(5):1032–1039. doi: 10.1542/peds.2010-2348. [DOI] [PubMed] [Google Scholar]
- Egeland B, Jacobvitz D, Sroufe LA. Breaking the cycle of abuse. Child Development. 1988;59(4):1080–1088. doi: 10.1111/j.1467-8624.1988.tb03260.x. [DOI] [PubMed] [Google Scholar]
- Field T. Postpartum depression effects on early interactions, parenting, and safety practices: A review. Infant Behavior and Development. 2010;33(1):1–6. doi: 10.1016/j.infbeh.2009.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fihrer I, McMahon CA, Taylor AJ. The impact of postnatal and concurrent maternal depression on child behaviour during the early school years. Journal of Affective Disorders. 2009;119(1–3):116–123. doi: 10.1016/j.jad.2009.03.001. [DOI] [PubMed] [Google Scholar]
- Gilbert R, Kemp A, Thoburn J, Sidebotham P, Radford L, Glaser D, MacMillan HL. Recognising and responding to child maltreatment. The Lancet. 2009;373(9658):167–180. doi: 10.1016/S0140-6736(08)61707-9. [DOI] [PubMed] [Google Scholar]
- Halligan SL, Murray L, Martins C, Cooper PJ. Maternal depression and psychiatric outcomes in adolescent offspring: a 13-year longitudinal study. Journal of Affective Disorders. 2007;97(1–3):145–154. doi: 10.1016/j.jad.2006.06.010. [DOI] [PubMed] [Google Scholar]
- Hay DF, Pawlby S, Angold A, Harold GT, Sharp D. Pathways to violence in the children of mothers who were depressed postpartum. Developmental Psychology. 2003;39(6):1083–1094. doi: 10.1037/0012-1649.39.6.1083. [DOI] [PubMed] [Google Scholar]
- Hay DF, Pawlby S, Waters CS, Sharp D. Antepartum and postpartum exposure to maternal depression: Different effects on different adolescent outcomes. Journal of Child Psychology and Psychiatry. 2008;49(10):1079–1088. doi: 10.1111/j.1469-7610.2008.01959.x. [DOI] [PubMed] [Google Scholar]
- Hendrick V, Altshuler LL, Suri R. Hormonal changes in the postpartum and implications for postpartum depression. Psychosomatics. 1998;39(2):93–101. doi: 10.1016/S0033-3182(98)71355-6. [DOI] [PubMed] [Google Scholar]
- Hibbard R, Barlow J, MacMillan H, Abuse TCoC, Neglect, American Academic of Child & Adolescent Psychiatry, & Child Maltreatment and Violence Committee Psychological maltreatment. Pediatrics. 2012;130(2):372–378. doi: 10.1542/peds.2012-1552. [DOI] [PubMed] [Google Scholar]
- Jaffee SR, Bowes L, Ouellet-Morin I, Fisher HL, Moffitt TE, Merrick MT, Arseneault L. Safe, stable, nurturing relationships break the intergenerational cycle of abuse: A prospective nationally representative cohort of children in the United Kingdom. Journal of Adolescent Health. 2013;53(4):S4–S10. doi: 10.1016/j.jadohealth.2013.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaffee SR, Caspi A, Moffitt TE, Polo-Tomás M, Taylor A. Individual, family, and neighborhood factors distinguish resilient from non-resilient maltreated children: A cumulative stressors model. Child Abuse & Neglect. 2007;31(3):231–253. doi: 10.1016/j.chiabu.2006.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaffee SR, Caspi A, Moffitt TE, Taylor A. Physical maltreatment victim to antisocial child: Evidence of an environmentally mediated process. Journal of Abnormal Psychology. 2004;113(1):44–55. doi: 10.1037/0021-843X.113.1.44. [DOI] [PubMed] [Google Scholar]
- Jaffee SR, Moffitt TE, Caspi A, Taylor A, Arseneault L. Influence of adult domestic violence on children's internalizing and externalizing problems: an environmentally informative twin study. J Am Acad Child Adolesc Psychiatry. 2002;41(9):1095–1103. doi: 10.1097/00004583-200209000-00010. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Zigler E. Do abused children become abusive parents? Am J Orthopsychiatry. 1987;57(2):186–192. doi: 10.1111/j.1939-0025.1987.tb03528.x. [DOI] [PubMed] [Google Scholar]
- Kettunen P, Koistinen E, Hintikka J. Is postpartum depression a homogenous disorder: time of onset, severity, symptoms and hopelessness in relation to the course of depression. BMC Pregnancy and Childbirth. 2014;14:402. doi: 10.1186/s12884-014-0402-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim-Cohen J, Moffitt TE, Taylor A, Pawlby SJ, Caspi A. Maternal depression and children's antisocial behavior: Nature and nurture effects. Archives of General Psychiatry. 2005;62(2):173–181. doi: 10.1001/archpsyc.62.2.173. [DOI] [PubMed] [Google Scholar]
- Ledermann T, Kenny DA. The common fate model for dyadic data: variations of a theoretically important but underutilized model. Journal of Family Psychology. 2012;26(1):140–148. doi: 10.1037/a0026624. [DOI] [PubMed] [Google Scholar]
- Leis JA, Mendelson T, Tandon SD, Perry DF. A systematic review of home-based interventions to prevent and treat postpartum depression. Archives of Women's Mental Health. 2009;12(1):3–13. doi: 10.1007/s00737-008-0039-0. [DOI] [PubMed] [Google Scholar]
- Mair C, Kadoda G, Lefley M, Phalp K, Schofield C, Shepperd M, Webster S. An investigation of machine learning based prediction systems. Journal of Systems and Software. 2000;53(1):23–29. [Google Scholar]
- McAdams TA, Rijsdijk FV, Neiderhiser JM, Narusyte J, Shaw DS, Natsuaki MN, Spotts EL, Ganiban JM, Reiss D, Leve LD, Lichtenstein P, et al. The relationship between parental depressive symptoms and offspring psychopathology: evidence from a children-of-twins study and an adoption study. Psychological Medicine. 2015;45(12):2583–2594. doi: 10.1017/S0033291715000501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCann J, Voris J, Simon M. Genital injuries resulting from sexual abuse: A longitudinal study. Pediatrics. 1992;89(2):307–317. [PubMed] [Google Scholar]
- McGinnis E, Bocknek E, Beeghly M, Rosenblum KL, Muzik M. Does child sex moderate vulnerability to postpartum risk among infants of mothers at risk for psychopathology? Infancy. 2015;20(1):42–69. [Google Scholar]
- Medical Research Council. Environmental Risk (E-Risk) Longitudinal Twin Study: About the cohort. 2017, 2016 from https://www.mrc.ac.uk/research/facilities-and-resources-for-researchers/cohort-directory/environmental-risk-e-risk-longitudinal-twin-study/
- Minnes S, Singer LT, Kirchner HL, Satayathum S, Short EJ, Min M, Eisengart S, Mack JP. The association of prenatal cocaine use and childhood trauma with psychological symptoms over 6 years. Archives of Women's Mental Health. 2008;11(3):181–192. doi: 10.1007/s00737-008-0011-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moffitt TE. Teen-aged mothers in contemporary Britain. Journal of Child Psychology & Psychiatry. 2002;43(6):727–742. doi: 10.1111/1469-7610.00082. [DOI] [PubMed] [Google Scholar]
- Monroe SM, Harkness KL. Life stress, the “kindling” hypothesis, and the recurrence of depression: considerations from a life stress perspective. Psychol Rev. 2005;112(2):417–445. doi: 10.1037/0033-295X.112.2.417. [DOI] [PubMed] [Google Scholar]
- Morgan D. Mindfulness-based cognitive therapy for depression: A new approach to preventing relapse. Psychotherapy Research. 2003;13(1):123–125. doi: 10.1080/713869628. [DOI] [PubMed] [Google Scholar]
- Murray L, Arteche A, Fearon P, Halligan S, Croudace T, Cooper P. The effects of maternal postnatal depression and child sex on academic performance at age 16 years: a developmental approach. Journal of Child Psychology & Psychiatry. 2010;51(10):1150–1159. doi: 10.1111/j.1469-7610.2010.02259.x. [DOI] [PubMed] [Google Scholar]
- Murray L, Cooper PJ. The impact of postpartum depression on child development. International Review of Psychiatry. 1996;8(1):55–63. [Google Scholar]
- Muzik M, Rosenblum KL, Alfafara EA, Schuster MM, Miller NM, Waddell RM, Stanton Kohler E. Mom Power: preliminary outcomes of a group intervention to improve mental health and parenting among high-risk mothers. Archives of Women's Mental Health. 2015;18(3):507–521. doi: 10.1007/s00737-014-0490-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nanni V, Uher R, Danese A. Childhood maltreatment predicts unfavorable course of illness and treatment outcome in depression: A meta-analysis. American Journal of Psychiatry. 2012;169(2):141–151. doi: 10.1176/appi.ajp.2011.11020335. [DOI] [PubMed] [Google Scholar]
- Norman RE, Byambaa M, De R, Butchart A, Scott J, Vos T. The long-term health consequences of child physical abuse, emotional abuse, and neglect: a systematic review and meta-analysis. PLoS medicine. 2012;9(11):e1001349. doi: 10.1371/journal.pmed.1001349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Odgers CL, Caspi A, Russell MA, Sampson RJ, Arseneault L, Moffitt TE. Supportive parenting mediates neighborhood socioeconomic disparities in children's antisocial behavior from ages 5 to 12. Development and Psychopathology. 2012;24(3):705–721. doi: 10.1017/S0954579412000326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliver JE. Intergenerational transmission of child abuse: Rates, research, and clinical implications. The American Journal of Psychiatry. 1993;150(9):1315–1324. doi: 10.1176/ajp.150.9.1315. [DOI] [PubMed] [Google Scholar]
- Pawlby S, Hay D, Sharp D, Waters CS, Pariante CM. Antenatal depression and offspring psychopathology: The influence of childhood maltreatment. British Journal of Psychiatry. 2011;199(2):106–112. doi: 10.1192/bjp.bp.110.087734. [DOI] [PubMed] [Google Scholar]
- Pears KC, Capaldi DM. Intergenerational transmission of abuse: A two-generational prospective study of an at-risk sample. Child Abuse and Neglect. 2001;25(11):1439–1461. doi: 10.1016/s0145-2134(01)00286-1. [DOI] [PubMed] [Google Scholar]
- Peugh JL, DiLillo D, Panuzio J. Analyzing mixed-dyadic data using structural equation models. Structural Equation Modeling: A Multidisciplinary Journal. 2013;20(2):314–337. [Google Scholar]
- Plant DT, Barker ED, Waters CS, Pawlby S, Pariante CM. Intergenerational transmission of maltreatment and psychopathology: the role of antenatal depression. Psychological Medicine. 2013;43(3):519–528. doi: 10.1017/S0033291712001298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plant DT, Jones FW, Pariante CM, Pawlby S. Association between maternal childhood trauma and offspring childhood psychopathology: mediation analysis from the ALSPAC cohort. The British Journal of Psychiatry. 2017 doi: 10.1192/bjp.bp.117.198721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polanczyk G, Caspi A, Williams B, Price TS, Danese A, Sugden K, Uher R, Poulton R, Moffitt TE. Protective effect of CRHR1 gene variants on the development of adult depression following childhood maltreatment: replication and extension. Archives of General Psychiatry. 2009;66(9):978–985. doi: 10.1001/archgenpsychiatry.2009.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quarini C, Pearson RM, Stein A, Ramchandani PG, Lewis G, Evans J. Are female children more vulnerable to the long-term effects of maternal depression during pregnancy? Journal of Affective Disorders. 2016;189:329–335. doi: 10.1016/j.jad.2015.09.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts AL, Chen Y, Slopen N, McLaughlin KA, Koenen KC, Austin SB. Maternal experiences of abuse in childhood and depressive symptoms in adolescent and adult offspring: A 21-year longitudinal study. Depression and Anxiety. 2015;32(10):709–719. doi: 10.1002/da.22395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts R, O’Connor T, Dunn J, Golding J. The effects of child sexual abuse in later family life; mental health, parenting and adjustment of offspring. Child Abuse & Neglect. 2004;28(5):525–545. doi: 10.1016/j.chiabu.2003.07.006. [DOI] [PubMed] [Google Scholar]
- Rodriguez CM, Tucker MC. Behind the cycle of violence, beyond abuse history: A brief report on the association of parental attachment to physical child abuse potential. Violence and Victims. 2011;26(2):246–256. doi: 10.1891/0886-6708.26.2.246. [DOI] [PubMed] [Google Scholar]
- Rutter M, Caspi A, Moffitt TE. Using sex differences in psychopathology to study causal mechanisms: unifying issues and research strategies. Journal of Child Psychology and Psychiatry. 2003;44(8):1092–1115. doi: 10.1111/1469-7610.00194. [DOI] [PubMed] [Google Scholar]
- Sanger C, Iles JE, Andrew CS, Ramchandani PG. Associations between postnatal maternal depression and psychological outcomes in adolescent offspring: a systematic review. Archives of Women's Mental Health. 2015;18(2):147–162. doi: 10.1007/s00737-014-0463-2. [DOI] [PubMed] [Google Scholar]
- Schreiber JB, Nora A, Stage FK, Barlow EA, King J. Reporting structural equation modeling and confirmatory factor analysis results: A review. The Journal of Educational Research. 2006;99(6):323–338. [Google Scholar]
- Shay NL, Knutson JF. Maternal depression and trait anger as risk factors for escalated physical discipline. Child Maltreatment. 2008;13(1):39–49. doi: 10.1177/1077559507310611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siu AL, the U.S. Preventive Services Task Force Screening for depression in adults: Us preventive services task force recommendation statement. JAMA. 2016;315(4):380–387. doi: 10.1001/jama.2015.18392. [DOI] [PubMed] [Google Scholar]
- Spinazzola J, Hodgdon H, Liang L-J, Ford JD, Layne CM, Pynoos R, Briggs EC, Stolbach B, Kisiel C. Unseen wounds: The contribution of psychological maltreatment to child and adolescent mental health and risk outcomes. Psychological Trauma: Theory, Research, Practice, and Policy. 2014;6(S1):S18. [Google Scholar]
- Spinhoven P, Elzinga BM, Hovens JGFM, Roelofs K, Zitman FG, van Oppen P, Penninx BWJH. The specificity of childhood adversities and negative life events across the life span to anxiety and depressive disorders. Journal of Affective Disorders. 2010;126(1–2):103–112. doi: 10.1016/j.jad.2010.02.132. [DOI] [PubMed] [Google Scholar]
- Starr LR, Hammen C, Conway CC, Raposa E, Brennan PA. Sensitizing effect of early adversity on depressive reactions to later proximal stress: Moderation by polymorphisms in serotonin transporter and corticotropin releasing hormone receptor genes in a 20-year longitudinal study. Development and Psychopathology. 2014;26(Special Issue 4, part 2):1241–1254. doi: 10.1017/S0954579414000996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoltenborgh M, Bakermans-Kranenburg MJ, Alink LRA, van Ijzendoorn MH. The prevalence of child maltreatment across the globe: Review of a series of meta-analyses. Child Abuse Review. 2015;24(1):37–50. [Google Scholar]
- Teicher MH, Parigger A. The 'Maltreatment and Abuse Chronology of Exposure' (MACE) scale for the retrospective assessment of abuse and neglect during development. PLoS One. 2015;10(2):e0117423. doi: 10.1371/journal.pone.0117423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thapar A, Rice F, Hay D, Boivin J, Langley K, van den Bree M, Rutter M, Harold G. Prenatal smoking might not cause attention-deficit/hyperactivity disorder: evidence from a novel design. Biological Psychiatry. 2009;66(8):722–727. doi: 10.1016/j.biopsych.2009.05.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thornberry TP, Knight KE, Lovegrove PJ. Does maltreatment beget maltreatment? A systematic review of the intergenerational literature. Trauma, Violence, & Abuse. 2012;13(3):135–152. doi: 10.1177/1524838012447697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorpe K, Golding J, MacGillivray I, Greenwood R. Comparison of prevalence of depression in mothers of twins and mothers of singletons. British Medical Journal. 1991;302(6781):875–878. doi: 10.1136/bmj.302.6781.875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trzesniewski KH, Moffitt TE, Caspi A, Taylor A, Maughan B. Revisiting the association between reading achievement and antisocial behavior: New evidence of an environmental explanation from a twin study. Child Development. 2006;77(1):72–88. doi: 10.1111/j.1467-8624.2006.00857.x. [DOI] [PubMed] [Google Scholar]
- Vliegen N, Casalin S, Luyten P. The course of postpartum depression: a review of longitudinal studies. Harvard Review of Psychiatry. 2014;22(1):1–22. doi: 10.1097/HRP.0000000000000013. [DOI] [PubMed] [Google Scholar]
- Widom CS, DuMont K, Czaja SJ. A prospective investigation of major depressive disorder and comorbidity in abused and neglected children grown up. Archives of General Psychiatry. 2007;64(1):49–56. doi: 10.1001/archpsyc.64.1.49. [DOI] [PubMed] [Google Scholar]
- Williams JMG, Crane C, Barnhofer T, Brennan K, Duggan DS, Fennell MJV, Hackmann A, Krusche A, Muse K, Von Rohr IR, Shah D, et al. Mindfulness-Based Cognitive Therapy for preventing relapse in recurrent depression: A randomized dismantling trial. Journal of Consulting and Clinical Psychology. 2014;82(2):275–286. doi: 10.1037/a0035036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Windham AM, Rosenberg L, Fuddy L, McFarlane E, Sia C, Duggan AK. Risk of mother-reported child abuse in the first 3 years of life. Child Abuse Negl. 2004;28(6):645–667. doi: 10.1016/j.chiabu.2004.01.003. [DOI] [PubMed] [Google Scholar]
- Wisner KL, Parry BL, Piontek CM. Postpartum depression. New England Journal of Medicine. 2002;347(3):194–199. doi: 10.1056/NEJMcp011542. [DOI] [PubMed] [Google Scholar]
- Zeanah CH, Zeanah PD. Intergenerational transmission of maltreatment: Insights from attachment theory and research. Psychiatry: Interpersonal and Biological Processes. 1989;52(2):177–196. doi: 10.1080/00332747.1989.11024442. [DOI] [PubMed] [Google Scholar]