Summary
Burn injuries are often seen among the paediatric population. Mortality from burn injuries is high in developing countries. Poor facilities and poverty contribute to this. A look at the epidemiology of burn injuries among children from this part of the world will therefore serve as a means for developing programs for burn injury prevention. A retrospective review of burn injuries among the paediatric population was conducted. The aim was to outline common aetiologies, sex predisposition and sites of injury with a view to recommending possible ways of preventing these injuries. A total of 148 children sustained burn injuries during the period under study. There were 85 (57.4%) boys and 63 (42.6%) girls. Scald was the most common cause of injury, observed in 127 (85.8%) children, followed by flame burn in 18 (12.2%), chemical burn in 2 (1.4%), and friction burn in 1 (0.68%). Almost all of the injuries (144, 98%) occurred at home. Sources of heat were hot water, which caused injury in 109 (73.6%) children, and hot oil, hot soup and hot soya milk which were responsible for 7 (4.7%), 7 (4.7%) and 3 (2.0%) cases, respectively. Other sources were kerosene explosion (7, 4.7%), burning firewood (1, 0.6%) petrol explosion (5, 3.4%), candlelight (3, 2.0%), hot ashes (1, 0.6%), soot (1, 0.6%), burned house, chemicals and friction (1, 0.6%). Preventive methods are suggested based on aetiologies, and include education and certain precautions in the home environment. These will reduce burn injuries and associated morbidity and mortality in developing countries.
Keywords: paediatric, burn, morbidity, epidemiology, prevention program
Abstract
Les enfants sont une population particulièrement à risque de brûlure, grevées d’une mortalité élevée dans les pays en développement, à laquelle contribuent la pauvreté et des infrastructures défaillantes. L’étude de l’épidémiologie des brûlures dans ces pays a pour but de cibler les campagnes de prévention. Cette étude a été réalisée rétrospectivement, en recueillant les étiologies les plus fréquentes, le sexe et le site de l’accident chez 148 victimes. On comptait 85 garçons (57,4%) et 63 filles (42,6%). Un ébouillantement était observé 127 fois (85,8%), une brûlure par flamme 18 fois (12,2%), une brûlure chimique 2 fois (1,4%) et une dermabrasion 1 fois (0,68%). Presque toutes les brûlures étaient survenues au domicile (114, 98%). De l’eau chaude était en cause 109 fois (73,6%), d’autres liquides (huile 7/ 4,7%, soupe 7/ 4,7%, lait de soja 3/ 2%) 17 fois. On observait par ailleurs des explosions de kérosène (7,4%) ou de pétrole (3,4%), un feu de bois (0,6%), des bougies (2%), des braises (0,6%), de la suie, un incendie de maison (0,6% à chaque fois). Les mesures préventives suggérées comprennent l’éducation et l’adaptation de l’environnement domestique.
Introduction
Burn injuries constitute a major cause of morbidity and mortality worldwide. Children are at risk for burn injuries because of their curiosity, their mode of reaction, their compulsiveness and their lack of experience in the calculation of risk. Paediatric burn injuries are second only to motor vehicle accidents as the leading cause of death in children aged 1 to 4 years, and the most frequent cause of injury and death among all children from birth up to the age of 19.
Morbidity and mortality from paediatric burn injuries is high in developing countries, partly because of ignorance, poverty and non-availability of appropriate burn facilities to take care of these children. A prevention program is therefore necessary in the developing world to reduce the current spate of morbidity and mortality. Epidemiological surveys provide objective information on hazardous agents and on the settings in which burns are most likely to occur. They are essential for the development of appropriate preventive strategies. This is highly necessary in the developing world.
Materials and methods
A retrospective review of all burn injuries observed in children under the age of 12 years at the National Orthopaedic Hospital, Enugu was conducted. The children’s case notes were reviewed. Information obtained included age, sex, site and type of burn, source and method of sustaining burn injury, associated morbidity etc. The results were collated and analysed using SPSS Version 17 with tables, frequencies and percentages. These were used as guidelines for the prevention of burn injuries in children in the developing world.
Results
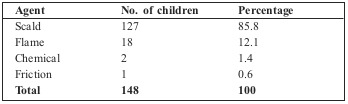
A total of 148 children sustained burn injuries during the period under study. There were 85 (57.4%) boys and 63 (42.6%) girls. Scald was the most common cause of burn injury and was observed in 127 (85.8%) children, followed by flame in 18 (12.2%), chemical burn in 2 (1.4%) and friction burn in 1 (0.68%) (Table I).
Table I. Aetiology of burn injuries.
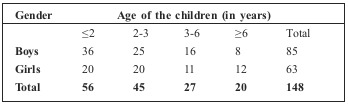
Almost all of the injuries (144, 98%) occurred at home. The age of the children ranged from one month to twelve years, with a peak age of 2 years (37.8%). The age group with the highest number of injured children was the <2 group (56, 37.8%), followed by the 2-3 years group (45, 30.4%), then the 3-6 years group (27, 18.2%). Twenty children (13.5%) were over 6 years old (Table II).
Table II. Age group of the children who sustained burns.
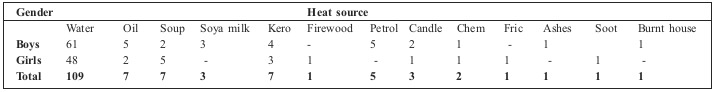
The sources of heat that caused burn in the children are shown in Table III, with hot water responsible for the highest number (109, 73.6%), and hot oil, hot soup and hot soya milk the cause of 7 (4.7%), 7 (4.7%) and 3 (2.0%), respectively. Other sources were kerosene explosion (7, 4.7%), burning firewood (1, 0.6%), petrol explosion (5, 3.4%), candlelight (3, 2.0%), hot ashes (1, 0.6%), soot (1, 0.6%), burned house, chemicals and friction (1, 0.6%).
Table III. Distribution of heat source by gender.
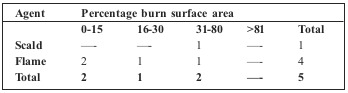
Five of the children died from their injuries, bringing mortality to 3.4%, with 4 (80%) of them injured by flame and only one (20%) by scald (Table IV). Mortality among the scald injured was 0.8% and among the flame injured 22.2%.
Table IV. Burn mortality in relation to the agent and percentage of burn.
Discussion
The burden of severe injury is an important health statistic.1 Most burn injuries in this environment, as in most parts of the world, have been found to be preventable. The frequency of burns in the under 1-year-old population highlights a need for greater emphasis on burn prevention directed at this group. Prevention of burn injuries, based on the epidemiology of burns in developing countries, remains a major way of reducing the current spate of morbidity and mortality in our patients. 2 Special attention should be focused on the specific aetiology of these burns with a view to developing a prevention program. Causes of childhood burns are largely preventable, thus require active social/medical education and public enlightenment campaigns on the various methods of prevention.3 The current status of burn care, the lack of infrastructure and traditional methods of treatment further contribute to the unsatisfactory status of overall burn management and prevention, and the rehabilitation of burn survivors. Therefore, there have been a number of suggestions made in the past regarding a strategy for improving burn care in Africa.4
As observed, the most common cause of burn injuries in these children is scald. Starting points for prevention should address the number of burns caused by hot drinks and bottle warming practices in the case of scalds, and the dangers of household radiators and hot water pipes in the case of contact burns.5 Children sustain these injuries either in the kitchen or dining room, where these substances are in places that are accessible to toddlers. The most common age group for burns has been observed to be 1-2 years, while the most common type of burn is scald.6 The current study also confirms this. Preventive efforts should therefore address this age group in particular.
As the world economy worsens and the number of career women rises, children are increasingly being looked after by grandmothers and underage housemaids, and this may be partly responsible for paediatric burns. The establishment of day-care centres and crèches in the work place will ensure that welltrained caregivers keep the children safe while their mother is at work.
A scald prevention program will therefore reduce the incidence of burn injuries among this age group. With increased education and facilities in Britain, it has been noted that the number of scalds from teapots has fallen from 20.8% to 2.7%, in contrast to scalds from cups of hot liquid which have increased from 8.9% to 42.5% over the 35-year period.7
Educating people on the need to avoid toddlers being allowed in the kitchen, using placemats rather than tablecloths on the dining table and ensuring the temperature of hot water meant for the bath is suitably reduced before carrying it out of the kitchen are important measures to take. Since in developing countries most domestic chores are carried out by mothers, educating mothers and would-be mothers is vital. This can take place during the antenatal period at maternity centres or at other religious or social gatherings. The introduction of burn prevention and especially paediatric burn prevention should form part of the school curriculum. Hence older children would be educated on what to do when in the kitchen, and on how to handle hot liquids and foods to prevent contact with children.
Parents should be educated on the need to prevent underage children from cooking, and older children should only be allowed to cook while under supervision.
In this study, domestic accidents constitute the greatest risk for burn injuries, like in many other studies. The home should be made safer for children, and attention must therefore be paid to the home environment in order to prevent paediatric burns. The most dangerous location in the house is the living room, followed by the bathroom, kitchen then bedroom, and the majority of burns are related to hot drinks, followed by hot food and then bathing.6 While the kitchen was the most common site of accident in the current study, hot foods - water, soup, oil, tea - were the agents that caused the most injuries. Lowering the temperature of domestic hot water is necessary, and statutory control is likely to offer the best solution to the problem of domestic hot tap water scalds in childhood.8 Cooking at floor level is a common practice in most villages and towns in developing countries. The danger this poses to a child who wants to explore everything should be made clear to mothers, and cooking at floor level discouraged. Keeping soup or water at floor level should also be avoided. The need to keep soup in a safe cupboard or locker should be stressed.
A population-based study on the epidemiology of burns in Sweden demonstrated the importance of developing a program for the prevention of paediatric scalds by educating family members to be aware of the dangers.9 It has also been suggested that in order to reduce mortality and disability from paediatric trauma in the rural developing world, prevention strategies targeting domestic burns in younger children, increased attention to the care of extremity injuries and burns, and increased use of non-medical health care providers in more remote areas should be observed.10 It has been noted that boys are more affected by domestic burn accidents than girls.6 We observed a slight preponderance of boys (57.4%) in the current study.
Although burn injury from flame was not significantly high among these children (18, 12.2%), their injuries were preventable. Causes included pouring kerosene into lit lanterns/stoves, and carrying a naked flame where there were inflammable liquids like gasoline.
Educating household members on ways to prevent injury from these substances could have prevented most of those injuries. Proper regulation of the design and production of industrial products such as alcohol and domestic stoves, coupled with adequate social support and health education programs are ways to lower the incidence of severe burn injuries.11 Teaching children and adults that they need to extinguish the flame before pouring kerosene into hurricane lamps and kerosene stoves is important.
Conclusion
Mortality from burn injuries is high in Nigeria and in other developing countries.12 Prevention of burn injuries should therefore be assiduously worked towards. The management of childhood burns will only be successful if educational, social, fiscal and infrastructure standards are improved. Traditional beliefs and methods cannot be discarded as they play an important role in the management of these children.4 Scald prevention, high-risk environments (home and recreational), high-risk populations (male and female children) and unsafe practices with flammable liquids (petrol in particular) should be emphasized in paediatric burn prevention programmes.13
References
- 1.Creamer GL, Civil I, Koelmeyer T, Adams D, Cacala S. Populationbased study of age, gender and causes of severe injury in Auckland, 2004. ANZ J Surg. 2008;78(11):995–998. doi: 10.1111/j.1445-2197.2008.04719.x. [DOI] [PubMed] [Google Scholar]
- 2.Olaitan PB, Olaitan JO. Burns and scalds - epidemiology and prevention in a developing country. Niger J Med. 2005;2005:9–16. doi: 10.4314/njm.v14i1.37128. [DOI] [PubMed] [Google Scholar]
- 3.Archibong AE, Antia UE, Udosen J. Childhood burns in south eastern Nigeria. East Afr Med J. 1997;74(6):382–384. [PubMed] [Google Scholar]
- 4.Albertyn R, Bickler SWXX, Rode H. Paediatric burn injuries in Sub Saharan Africa - an overview. Burns. 2006;32(5):605–612. doi: 10.1016/j.burns.2005.12.004. [DOI] [PubMed] [Google Scholar]
- 5.Nguyen DQ, Tobin S, Dickson WA, Potokar TS. Infants under 1 year of age have a significant risk of burn injury. Burns. 2008;34(6):863–867. doi: 10.1016/j.burns.2007.11.011. [DOI] [PubMed] [Google Scholar]
- 6.Tse T, Poon CH, Tse KH, Tsui TK, Ayyappan T, Burd A. Paediatric burn prevention: an epidemiological approach. Burns. 2006;32(2):229–234. doi: 10.1016/j.burns.2005.08.025. [DOI] [PubMed] [Google Scholar]
- 7.Eadie PA, Williams R, Dickson WA. Thirty-five years of paediatric scalds: are lessons being learned? Br J Plast Surg. 1995;4882):103–105. doi: 10.1016/0007-1226(95)90105-1. [DOI] [PubMed] [Google Scholar]
- 8.Tennant WG, Davison PM. Bath scalds in children in the south-east of Scotland. J R Coll Surg Edinb. 1991;36(5):319–322. [PubMed] [Google Scholar]
- 9.Carlsson A, Udén G, Håkansson A, Karlsson ED. Burn injuries in small children, a population-based study in Sweden. J Clin Nurs. 2006;15(2):129–134. doi: 10.1111/j.1365-2702.2006.01259.x. [DOI] [PubMed] [Google Scholar]
- 10.Mock CN, Denno D, Adzotor ES. Paediatric trauma in the rural developing world: low cost measures to improve outcome. Injury. 1993;24(5):291–296. doi: 10.1016/0020-1383(93)90047-a. [DOI] [PubMed] [Google Scholar]
- 11.Werneck GL, Reichenheim ME. Paediatric burns and associated risk factors in Rio de Janeiro, Brazil. Burns. 1997;2386):478–483. doi: 10.1016/s0305-4179(97)00046-6. [DOI] [PubMed] [Google Scholar]
- 12.Olaitan PB, Dairo MD, Uduezue AO, Ogbonnaya IS. Paediatric mortality in a burn unit. African Journal of Paediatrics. 2007;1(1):82–85. [Google Scholar]
- 13.Ryan CA, Shankowsky HA, Tredget EE. Profile of the paediatric burn patient in a Canadian burn centre. Burns. 1992;18(4):267–272. doi: 10.1016/0305-4179(92)90146-l. [DOI] [PubMed] [Google Scholar]


