Abstract
Introduction A pneumatized turbinate, also called concha bullosa, is a normal anatomical variant of the paranasal sinus region. Depending on the site of pneumatization, the concha is classified into extensive, bulbous or lamellar type. The middle turbinate concha bullosa has been implicated as a possible etiological factor in chronic sinusitis.
Objectives The aim of this study was to investigate the anatomical variations of the concha bullosa, based on paranasal sinus imaging, and its possible association with sinusitis.
Methods This prospective descriptive study was performed at the Department of ENT and Head Neck Surgery over a period of one year, from 2016 to 2017. We studied the computed tomography scans of the nose and paranasal sinuses— in axial, coronal and sagittal planes—of patients who had symptoms of nasal obstruction, or headache and features of chronic sinusitis.
Results Out of the 202 scans studied, the prevalence of concha bullosa was 31.7%. The concha was bilateral in 35 (54.7%) patients and unilateral in 29 (45.3%) patients. Out of 99 conchae, 54 were on the right side and 45 were on left side. Ipsilateral sinusitis was found in 40.4% of the sides in the scans of subjects with concha. There was no statistically significant association between any type of middle turbinate concha with sinusitis, but sinusitis was more predominant with the extensive type of concha ( p > 0.05).
Conclusion Multiple air cells, mucocele, pyocele and inflammatory mucosal thickenings in the concha are relatively rare. Detailed knowledge of anatomic variations of the concha bullosa is imperative for the radiologists and the operating surgeons.
Keywords: sinusitis, turbinates, mucocele
Introduction
A concha bullosa (CB) represents the presence of air cell in the turbinates, and the middle turbinate (MT) concha bullosa is a common nasal cavity anatomical variation. Pneumatization of the MT happens due to variation in the ethmoidal air cell system development. The incidence rates for pneumatization of the MT is between 13 and 53.6%. 1 2 3 4 Concha bullosa is generally asymptomatic and diagnosed incidentally by computed tomography. Sometimes, an over-pneumatized MT can lead to nasal obstruction, contact headache, deviated nasal septum and chronic sinusitis. Concha bullosa can be unilateral or bilateral and can be classified into three types according to the site of pneumatization. They are lamellar-type (vertical lamella of MT pneumatization), bulbous-type (inferior portion of MT pneumatization) and extensive/large type (vertical lamella and inferior portion of the MT pneumatization). A disease process of the paranasal sinuses can affect the CB, resulting in mucosal thickening, retention of mucous secretion, mucocele and pyocele within the CB. The CB itself can cause mechanical obstruction, affecting the drainage pathway and leading to sinusitis. Understanding the anatomical variations of the CB make it possible to plan for appropriate management. In this article, we described some of the rare anatomical variations of MT CB, such as extensive mucosal thickening within the CB, air cells in the CB, and mucopyocele of the CB, which can cause orbital complications. All these conditions and their clinical importance are discussed. The role of the MT CB in predisposition to chronic sinusitis is in question, and there is dissensus on the relationship between the CB and sinus pathology. Very few research works have investigated the pneumatization and anatomical variation of the CB and its possible association to chronic sinusitis.
Objectives
The objectives of this study were to investigate the anatomical variation of the MT concha bullosa based on paranasal sinus imaging, and its possible association with rhinosinusitis.
Methods
A prospective descriptive study was performed at the Department of ENT and Head Neck Surgery over a period of 1 year, from 1st May 2016 to 30th April 2017, to determine the prevalence of CB in the paranasal sinus imaging of patients who had symptoms of nasal obstruction or headache and features of chronic sinusitis. Demographic data, clinical presentation, computed tomography (CT) of nose and paranasal sinuses 5-mm-thick imaging scans in the axial, coronal and sagittal planes were recorded. The inclusion criterion was the presence of any type of pneumatization of the MT in CTs of the nose and paranasal sinuses. Any mucosal thickening of 4 mm or more in the sinus cavity wall was taken as positive for sinusitis. 5 Informed consent forms signed by the patients as well as the institute ethical committee's clearance were obtained prior to this study.
In this study, CT scans of the nose and paranasal sinus of 202 patients were studied, out of which 64 patients (37 males, 27 females; mean age 30.3 years; range 16 to 60 years) had concha bullosa in their imaging study. The CB was classified as lamellar, bulbous or extensive type, according to the classification developed by Bolger et al. 6
Patients who underwent any nasal surgery, had any congenital abnormalities of the nose or had been in accidents involving the faciomaxillary region before taking the CT scan were excluded from this study. A total of 42 patients (65.6%) underwent surgery to treat symptomatic CB.
Results
Out of the CT scans studied of the nose and paranasal sinus of 202 patients, the prevalence of CB was 31.7%. Concha bullosa was bilateral in 35 (54.7%) patients, and unilateral in 29 (45.3%) patients. Out of 99 cases of CB, 54 (54.5%) were on right side and 45 (45.5%) were on left side. Two patients had mucopyocele of the CB, in its lamellar part, and four patients had extensive mucosal thickening within the CB ( Fig. 1a and 1b ). The distribution of anatomical variation of CB is shown in Table 1 . Computed tomography of mucocele or pyocele within a CB shows a prominent well circumscribed soft tissue density with a thin bony framework at the margin ( Fig. 2a and 2b ). Migrating ethmoidal air cells within the CB is a rare finding ( Fig. 3a and 3b ) seen in one patient, bilaterally.
Fig. 1.
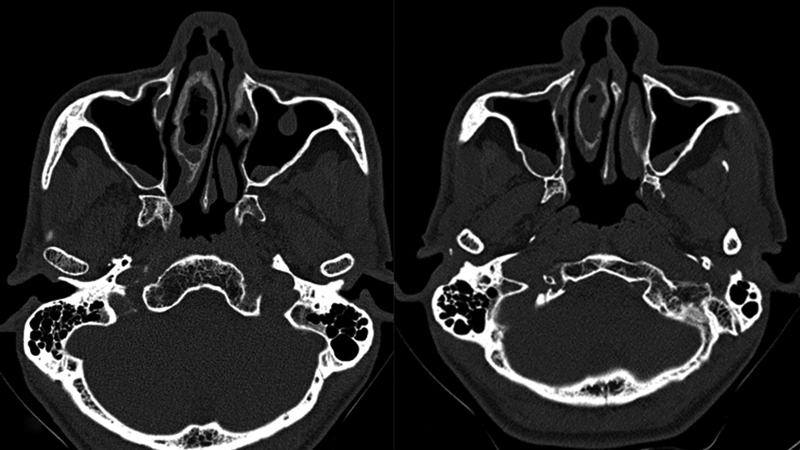
(a and b) Axial sections of computed tomography of the paranasal sinuses showing mucosal thickening within the right concha bullosa, and thickening of the surrounding bony walls. Also noted are areas of mild mucosal thickening in both maxillary sinuses and a mucosal polyp in the anterior wall of left maxillary sinus.
Table 1. Anatomical variations of middle turbinate concha bullosa.
| S.No | Anatomical variation of concha bullosa | Number (%) | Total number (%) |
|---|---|---|---|
| 1. | Pure extensive type | 44 (44.5%) | 49 (49.5%) |
| 2. | Mucosal thickening within the extensive type | 4 (4%) | |
| 3. | Polyp within extensive type | 1 (1%) | |
| 4. | Pure bulbous type | 26 (26.3%) | 28 (28.3%) |
| 5. | Air cells within bulbous type | 2 (4%) | |
| 6. | Pure lamellar type | 20 (20.2%) | 22 (22.2%) |
| 7. | Mucopyocele within lamellar type | 2 (2%) |
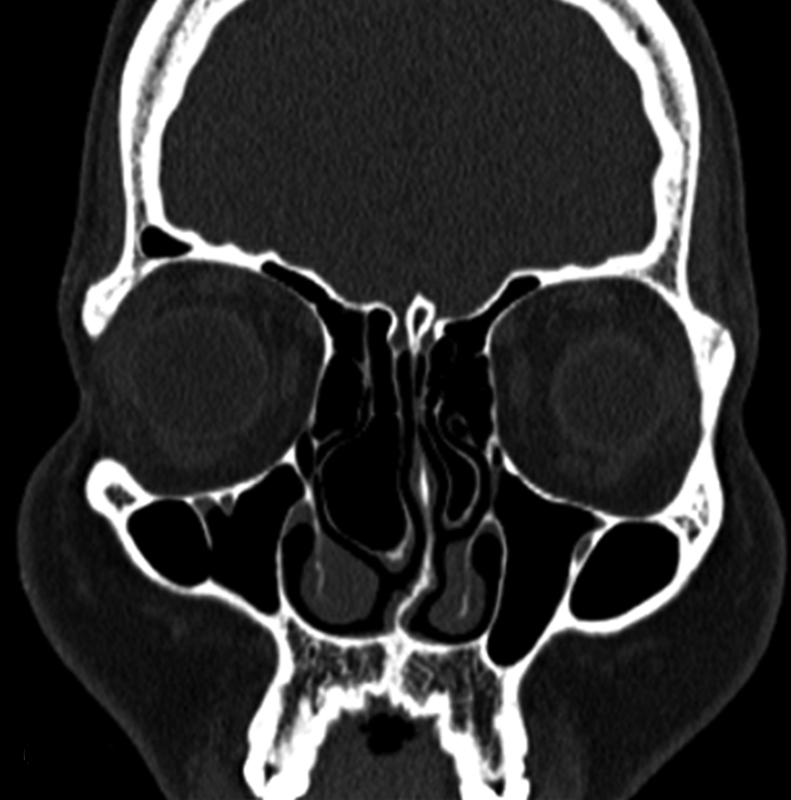
Fig. 2.
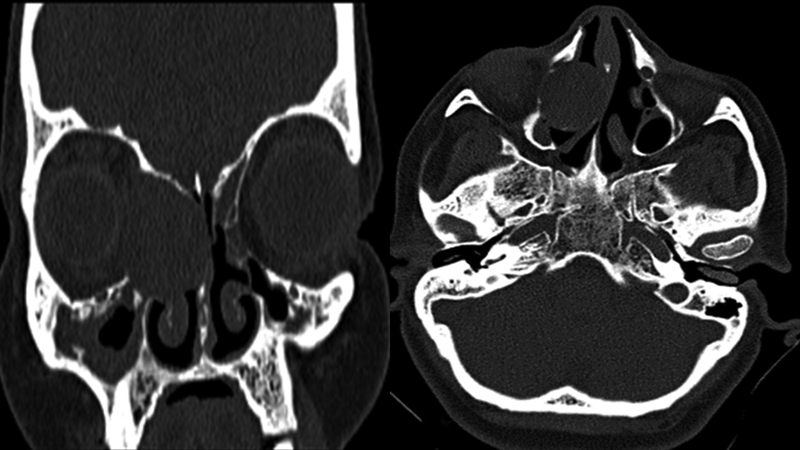
(a) Coronal and (b) axial sections of non-contrast computed tomography of paranasal sinuses show expansile soft tissue density within the concha bullosa causing extreme thinning of the bony walls and mass effect on and thinning of the medial wall of right orbit and the nasal septum, suggestive of a mucopyocele of the concha bullosa. Fig 2a also shows obstruction of the right maxillary sinus drainage pathway with resultant chronic sinusitis.
Fig. 3.
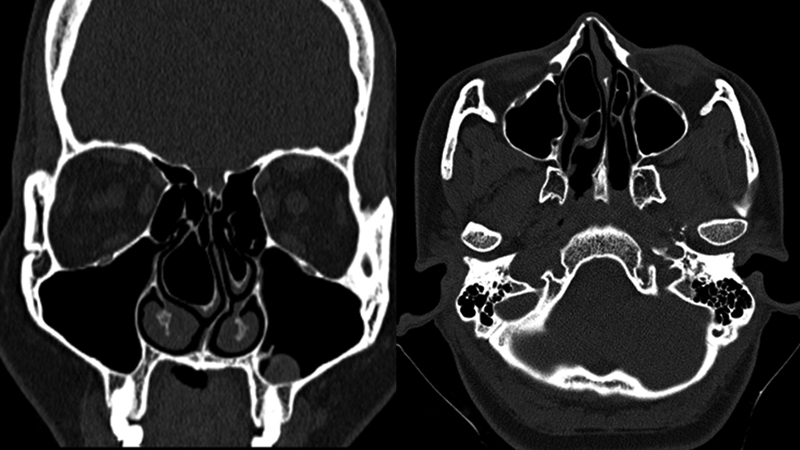
(a) Coronal and (b) axial sections of computed tomography of the paranasal sinuses show the presence of multiple air cells within the bilateral concha bullosae. Deviation of the nasal septum to the left side is noted. Also seen is a small mucosal polyp in the inferior wall of the left maxillary sinus.
The most common incidental pathology accompanying CB was nasal septal deviation ( n = 49) ( Fig. 4a ). Ipsilateral sinusitis was found in only 40 (40.4%) of the sides in scans of subjects with CB. Out of the 49 extensive conchae, 11 were on the right side (22.4%), which had associated ipsilateral osteomeatal complex blockage and mucosal thickening within the sinuses, and 16 (32.6%) had free ipsilateral osteomeatal complex without mucosal thickening of the sinuses ( Fig. 5 ). In our study, the maxillary sinus was the most commonly involved sinus, followed by the ethmoid and frontal sinuses. Two proportion tests were used for the statistical analysis using STATA version 12.0 (Stata Corp, College Station, TX, USA). A p value < 0.05 was taken as statistically significant. There was no statistically significant association between any type of CB with sinusitis, but sinusitis was more predominant with the extensive type than with any other type of CB ( Table 2 ).
Fig. 4.
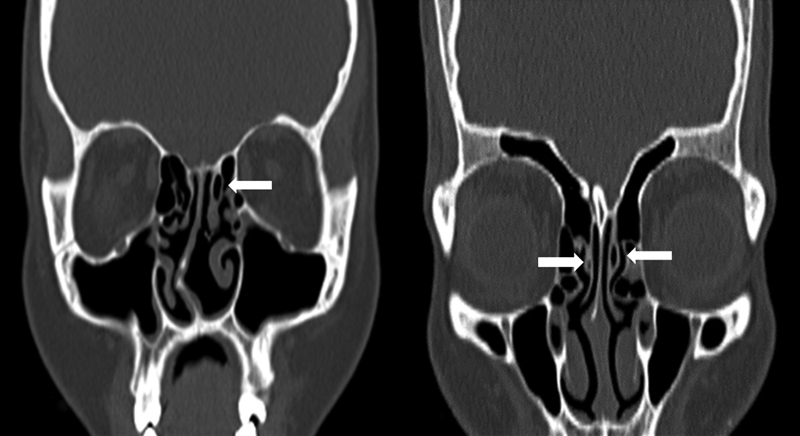
(a and b) Coronal sections of non-contrast computed tomography scan of the paranasal sinuses showing pneumatized vertical lamella of left middle turbinate (lamellar type of concha shown with arrow). Incidental deviation of the nasal septum to the right side is noted.
Fig. 5.
Coronal section of computed tomography of the paranasal sinuses shows extensive pneumatisation of the inferior portion and vertical lamella of the bilateral middle turbinates, more on the right side, suggestive of extensive/large type of concha bullosa.
Table 2. Association of different types of middle turbinate concha bullosa with sinusitis.
| S. No | Concha bullosa type and laterality | Associated with sinusitis | Not associated with sinusitis | P value |
|---|---|---|---|---|
| 1. | Right extensive | 11 | 16 | 0.965 |
| 2. | Left extensive | 10 | 12 | 0.5834 |
| 3. | Right bulbous | 4 | 10 | 0.332 |
| 4. | Left bulbous | 6 | 8 | 0.839 |
| 5. | Right lamellar | 5 | 8 | 0.8793 |
| 6. | Left lamellar | 4 | 5 | 0.7956 |
Discussion
The ethmoturbinal and maxilloturbinal are the embryological precursors of the nasal turbinates, which appear between the eighth and tenth weeks of gestation. The ethmoturbinal gives rise to the uncinate process, the MT and the superior turbinate. The MT is formed by the medial part of the ethmoid bone. The ethmoidal air cells extending into the frontal, maxillary, and the sphenoid paranasal sinus bones retain their ostia at the site of initial evagination. 7 The ostia remain as their drainage pathway. Anterior ethmoidal cells originating from the middle meatus pneumatize the MT in ∼ 55% of cases, which usually drain into the frontal recess. 8 Posterior ethmoid cells originated from the superior meatus pneumatize in ∼ 45% of the cases, and they usually drain into the retrobulbar recess. Most commonly, the drainage occurs through the conchal ostium present near the frontal recess region into which the frontal sinus drains. The CB becomes apparent after 7– 8 years of age and continues its development even after the period of adolescence. 9 The degree of pneumatization and the inflammatory changes that occur within the CB may correlate with the presentation and the severity of symptoms. The mean age (30.3 years) of this study's participants with CB was consistent with other studies on the same topic. 10 11 The proportion of males was higher than that of females in our study, in contrast with other studies. 4 10 12 13 The prevalence of CB was 31.7% in our study. Aramani et al and Koo SK et al reported a prevalence rate of 53.7% in their studies. 11 14 In our study, the MT CB prevalences of extensive, bulbous and lamellar types were 49 (49.5%), 28 (28.3%) and 22 (22.2%), respectively, which are the same as noted in a study by Tonai et al. 15 Various other studies report different incidences, which could be due to the differences in the target population and racial variation. 4 5 16
The CB, rarely when filled with fluid and pus results in mucopyocele. Concha bullosa mucopyocele happens due to chronic obstruction of the CB ostium, which prevents the optimal air current flow between the CB cavity and the surrounding structures, such as the frontal recess, ethmoidal cells or middle meatus. 17 18 19 For this reason, the epithelial lining in a CB mucocele/pyocele remains intact, lacking an epithelial covering in other types of mucocele. 18 19 It is important to differentiate between CB mucocele/pyocele and ethmoidal pyocele. Concha bullosa pyocele shows an enlarged tip or body of the MT that touches the nasal septum medially and bulges into the lateral wall of the nose laterally or into the medial wall of the orbit. Mucocele of the ethmoid sinus usually displaces the MT inferiorly, against the septum. The MT is seen distinctly as an intact structure, but compressed. Any secretions within a CB will have a mucoid attenuation of 10–18 HU in the CT scan. The presence of a bony shell around the CB on a CT scan evaluation allows a conchal mucocele to be differentiated from other nasal masses, but the bony rim may sometimes be absent or extremely thinned out due to bone remodeling in the pathogenesis of mucocele ( Fig. 2 ). Concha bullosa mucocele/pyocele can masquerade as an intranasal tumor, and it is very important to consider CB mucocele/pyocele in the differential diagnosis.
Mucosal thickening and polyp formation within a CB is also uncommon. The inner surface of the CB is lined with mucous membrane and any inflammatory process will incite mucosal hypertrophy and polyp formation. 20 Usually, the CB contains only a single air cell. Multiple air cells are relatively rare. Ceylan S et al described a giant complex CB, in which the ethmoid bulla invaginated into the MT CB. 21 In our study, we found ethmoidal air cells in the CB; however, the clinical importance of such discovery is still unclear. Extensive pneumatization of the turbinates with mucosal contact can lead to headache, even in the absence sinonasal inflammation. 22
In our study, there was no significant association between any type of CB with ipsilateral rhinosinusitis, but, clinically, we found that sinusitis was more predominant in the extensive type of CB, compared with other types; however, this finding was not statistically significant. We also found that patients with mucopyocele of the CB always associated with ipsilateral sinusitis. Lee et al, Yasan et al, and Armengot et al also reported similar findings in their case studies that CB mucocele/pyocele cause ipsilateral sinusitis. 3 18 23 Aktas D et al studied the CT paranasal scans of 54 patients with CB and found no relationship between unilateral and bilateral CB with sinusitis. 24
Conclusion
Radiologists and surgeons should be aware of anatomical variants of the CB present in the paranasal sinus imaging. Our findings show that the CB does not appear to give rise to chronic sinusitis, but the extensive type was more symptomatic than the bulbous or lamellar types. Certain anatomical variations, like air cells in a MT CB and extensive mucosal thickening within a MT CB, are herein defined for the first time in the literature.
References
- 1.Joe J K, Ho S Y, Yanagisawa E.Documentation of variations in sinonasal anatomy by intraoperative nasal endoscopy Laryngoscope 2000110(2 Pt 1):229–235. [DOI] [PubMed] [Google Scholar]
- 2.Al-Sebeih K H, Bu-Abbas M H. Concha bullosa mucocele and mucopyocele: a series of 4 cases. Ear Nose Throat J. 2014;93(01):28–31. [PubMed] [Google Scholar]
- 3.Lee J H, Hong S L, Roh H J, Cho K S. Concha bullosa mucocele with orbital invasion and secondary frontal sinusitis: a case report. BMC Res Notes. 2013;6(06):501. doi: 10.1186/1756-0500-6-501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Unlü H H, Akyar S, Caylan R, Nalça Y. Concha bullosa. J Otolaryngol. 1994;23(01):23–27. [PubMed] [Google Scholar]
- 5.Rak K M, Newell J D, II, Yakes W F, Damiano M A, Luethke J M. Paranasal sinuses on MR images of the brain: significance of mucosal thickening. AJR Am J Roentgenol. 1991;156(02):381–384. doi: 10.2214/ajr.156.2.1898819. [DOI] [PubMed] [Google Scholar]
- 6.Bolger W E, Butzin C A, Parsons D S.Paranasal sinus bony anatomic variations and mucosal abnormalities: CT analysis for endoscopic sinus surgery Laryngoscope 1991101(1 Pt 1):56–64. [DOI] [PubMed] [Google Scholar]
- 7.Zinreich S J, Mattox D E, Kennedy D W, Chisholm H L, Diffley D M, Rosenbaum A E. Concha bullosa: CT evaluation. J Comput Assist Tomogr. 1988;12(05):778–784. doi: 10.1097/00004728-198809010-00012. [DOI] [PubMed] [Google Scholar]
- 8.Van Alyea O E. Baltimore: Williams and Wilkins; 1951. Nasal sinuses: an anatomic and clinical consideration. [Google Scholar]
- 9.Cohen S D, Matthews B L. Large concha bullosa mucopyocele replacing the anterior ethmoid sinuses and contiguous with the frontal sinus. Ann Otol Rhinol Laryngol. 2008;117(01):15–17. doi: 10.1177/000348940811700104. [DOI] [PubMed] [Google Scholar]
- 10.Stallman J S, Lobo J N, Som P M. The incidence of concha bullosa and its relationship to nasal septal deviation and paranasal sinus disease. AJNR Am J Neuroradiol. 2004;25(09):1613–1618. [PMC free article] [PubMed] [Google Scholar]
- 11.Aramani A, Karadi R N, Kumar S. A study of anatomical variations of osteomeatal complex in chronic rhinosinusitis patients—CT findings. J Clin Diagn Res. 2014;8(10):KC01–KC04. doi: 10.7860/JCDR/2014/9323.4923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nadas S, Duvoisin B, Landry M, Schnyder P. Concha bullosa: frequency and appearances on CT and correlations with sinus disease in 308 patients with chronic sinusitis. Neuroradiology. 1995;37(03):234–237. doi: 10.1007/BF01578264. [DOI] [PubMed] [Google Scholar]
- 13.Lam W WM, Liang E Y, Woo J K, Van Hasselt A, Metreweli C. The etiological role of concha bullosa in chronic sinusitis. Eur Radiol. 1996;6(04):550–552. doi: 10.1007/BF00182491. [DOI] [PubMed] [Google Scholar]
- 14.Koo S K, Kim J D, Moon J S, Jung S H, Lee S H. The incidence of concha bullosa, unusual anatomic variation and its relationship to nasal septal deviation: A retrospective radiologic study. Auris Nasus Larynx. 2017;44(05):561–570. doi: 10.1016/j.anl.2017.01.003. [DOI] [PubMed] [Google Scholar]
- 15.Tonai A, Baba S. Anatomic variations of the bone in sinonasal CT. Acta Otolaryngol Suppl. 1996;525:9–13. [PubMed] [Google Scholar]
- 16.Uygur K, Tüz M, Doğru H. The correlation between septal deviation and concha bullosa. Otolaryngol Head Neck Surg. 2003;129(01):33–36. doi: 10.1016/S0194-59980300479-0. [DOI] [PubMed] [Google Scholar]
- 17.Lee J S, Ko I J, Kang H D, Lee H S. Massive concha bullosa with secondary maxillary sinusitis. Clin Exp Otorhinolaryngol. 2008;1(04):221–223. doi: 10.3342/ceo.2008.1.4.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yasan H, Doğru H, Tüz M, Yeşildağ A, Karahan N. Polypoid degeneration of the middle turbinate mucocele mimicking intranasal neoplasia. J Otolaryngol. 2005;34(03):207–209. doi: 10.2310/7070.2005.03108. [DOI] [PubMed] [Google Scholar]
- 19.Pinto J A, Cintra P P, de Marqui A C, Perfeito D J, Ferreira R D, da Silva R H. [Mucopyocele of the middle turbinate: a case report] Rev Bras Otorrinolaringol (Engl Ed) 2005;71(03):378–381. doi: 10.1016/S1808-8694(15)31340-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Erkan A N, Canbolat T, Ozer C, Yilmaz I, Ozluoglu L N. Polyp in concha bullosa: a case report and review of the literature. Head Face Med. 2006;2(02):11. doi: 10.1186/1746-160X-2-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ceylan S, Bora F, Batmaz T, Atalay B. Complex Concha Bullosa. Otolaryngol (Sunnyvale) 2012;2:109. [Google Scholar]
- 22.Kantarci M, Karasen R M, Alper F, Onbas O, Okur A, Karaman A. Remarkable anatomic variations in paranasal sinus region and their clinical importance. Eur J Radiol. 2004;50(03):296–302. doi: 10.1016/j.ejrad.2003.08.012. [DOI] [PubMed] [Google Scholar]
- 23.Armengot M, Ruiz N, Carda C, Hostalet P, Basterra J. Concha bullosa mucocele with invasion of the orbit. Otolaryngol Head Neck Surg. 1999;121(05):650–652. doi: 10.1016/S0194-5998(99)70075-6. [DOI] [PubMed] [Google Scholar]
- 24.Aktas D, Kalcioglu M T, Kutlu R, Ozturan O, Oncel S. The relationship between the concha bullosa, nasal septal deviation and sinusitis. Rhinology. 2003;41(02):103–106. [PubMed] [Google Scholar]


