Abstract
Hepatic ischemia-reperfusion injury (IRI) represents a major risk factor of early graft dysfunction and acute/chronic rejection as well as a key obstacle to expanding the donor pool in orthotopic liver transplantation (OLT). Although glucocorticoid receptor (GR) signaling may enhance cytoprotective programs, clinical use of glucocorticoid is limited due to adverse effects, while clinical relevance of GR-facilitated cytoprotection in OLT remains unknown. We aimed to evaluate the significance of hepatic GR in clinical OLT and verify the impact of recombinant human relaxin (rhRLX), which may function as GR agonist in tissue/disease-specific manner. Fifty-one liver transplant patients were recruited under IRB protocol. Liver biopsies were collected after cold storage (prior to the surgery) and 2h post-reperfusion (prior to the abdominal closure), followed by Western blot-assisted hepatic analyses. Forty-three percent of OLTs failed to increase GR peri-operatively under surgical stress. Post-/pre-GR ratios at post-operative day 1 correlated negatively with serum AST/cleaved caspase-3 and positively with Bcl-xL/Bcl-2 levels. In a murine OLT model with extended (18h) cold storage, treatment with rhRLX ameliorated IR-damage and improved survival while upregulating hepatocyte GR and Bcl-xL/Bcl-2 expression in OLT. rhRLX-induced GR suppressed hepatocyte HMGB1 translocation/release, accompanied by decreased TLR4/RAGE, suppressed IL1β, CCL2, CXCL10, TNFα, CXCL1 and CXCL2 levels and attenuated neutrophil/macrophage accumulation in OLT. Inhibition of GR in hepatocyte culture and in OLT diminished rhRLX-mediated cytoprotection. Conclusion: This translational study underscores the role of rhRLX – GR signaling as a novel regulator of hepatocellular protection against IR-stress in OLT. In the context of a recent phase III clinical trial demonstrating positive outcomes of rhRLX in patients with acute heart failure, studies on rhRLX for the management of IRI in liver transplant recipients are warranted.
Keywords: liver transplantation, liver biopsy, innate immunity, apoptosis, high-mobility group box 1
Although orthotopic liver transplantation (OLT) has become the standard of care for patients with end-stage liver disease and those with hepatic malignancies, shortage of available organs remains important clinical challenge (1). Ischemia-reperfusion injury (IRI), a leading cause of early graft dysfunction and failure, represents a major risk factor in the development of acute and chronic rejection (2). However, despite obvious clinical importance, the mechanisms that account for liver IRI are not well understood, and novel strategies to improve outcomes and expand donor pool are warranted.
Liver IRI is characterized by innate immune-driven sterile inflammation in which reoxygenation of hypoxic cells promotes reactive oxygen species formation, including hydrogen peroxide and superoxide, followed by hepatocyte death (2). The cellular insult leads to secretion of danger-associated molecular patterns, including high-mobility group box 1 (HMGB1), ATP and histone/DNA (3), which then trigger a cascade of inflammatory cytokine/chemokine programs, further contributing to target cell death. As hepatocyte damage is the initiating event in innate immune activation and ultimate graft dysfunction, preventing hepatocyte death is one of the obvious therapeutic strategies against organ IRI. Indeed Ad-mediated gene transfer of antiapoptotic Bcl-2 attenuated liver IRI in mice (4), while by upregulating antiapoptotic Bcl-xL, recombinant erythropoietin improved the hepatocellular function in rat livers exposed to IR-insult (5).
Glucocorticoid receptor (GR), a ubiquitously expressed ligand-dependent nuclear hormone receptor, functions as a transcription factor regulating the expression of glucocorticoid-responsive genes (6). While GR signaling induces apoptosis in a wide range of cells, other cell types may exert anti-apoptotic response (7). Ligand-stimulated GR binds and activates Bcl-xL promoter sequences in vitro and in vivo, and suppresses apoptosis in fibrosarcoma cells (8) whereas dexamethasone was shown to increase Bcl-2/Bcl-xL and inhibit apoptosis in primary hepatocyte cultures (9). In line with these findings, the efficacy of glucocorticoid to mitigate hepatic IRI was recorded in cholestatic rat liver model (10) and in patients undergoing liver resection (11). However, steroid-related metabolic disorders and well-known adverse effects, such as recurrence of hepatitis C, delayed wound healing or infections, severely limit their use, while clinical relevance of GR hepatoprotection has not been examined to-date.
Relaxin, a group of low-molecular weight peptides of the insulin-growth factor family, consists of seven members, with relaxin-2 (RLX-2) accounting for most of the abundant physiological actions (12). Isolated mainly from ovaries, RLX-2 is essential in hemodynamic adaptation by decreasing systemic vascular resistance, increasing cardiac output and improving global arterial compliance (13). Besides its function at the maternal-fetal interface in pregnancy, studies on cytoprotective (14), anti-inflammatory (15) and anti-fibrotic (16) effects, underpin the increasing interest in RLX-2 as a therapeutic agent. Indeed, a recent phase III randomized clinical trial demonstrated the efficacy, safety and tolerability of recombinant human RLX-2 (rhRLX) in patients with acute heart failure (17). RLX-2 binds with high affinity to cognate relaxin family peptide receptor-1 (RXFP1) (18) expressed in reproductive tissues, heart, kidney, lung and brain (19). Others reported on protective effects of RLX-2 in cardiac (12), renal (20) and lung (21) IRI models. Although RLX-2 seemed to reduce cell damage in an isolated rat liver perfusion system (22), the mechanism and putative clinical relevance of the finding remain unknown. Interestingly, recent studies have identified RLX-2 as a potential GR agonist that may function independently of RXFP1 in a tissue and disease-specific manner (23).
Here, we have identified a novel rhRLX – GR cytoprotection pathway in mouse and human OLT settings. We demonstrated that peri-operative enhancement of hepatocyte GR expression triggers local anti-apoptotic programs and hepatocellular protection in liver graft recipients. In the context of a recent clinical trial in acute heart failure patients (24), our translational study validates the use of rhRLX in the management of IRI in liver transplant recipients.
Experimental Procedures
Clinical liver transplantation study
Fifty-one adult OLT recipients recruited between May 2013 and August 2015 received routine standard of care and immunosuppressive therapy, as specified by UCLA liver transplant protocols. Study data were managed using REDCap electronic data capture tools. Recipient blood was collected prior to the transplant and at post-operative day 1–14 (POD 1–14). Liver function was evaluated by serum alanine aminotransferase (sALT) and aspartate aminotransferase (sAST). Protocol Tru-Cut needle biopsies (Bx) were obtained from the left liver lobe and snap-frozen. Pre-transplant Bx were obtained after liver cold storage on the back table (prior to the surgery), while post-transplant Bx were collected 2h after portal reperfusion (prior to the abdominal closure). Early allograft dysfunction was defined by the presence of one or more of the following: total bilirubin ≥10 mg/dL (171 μmol/L) at POD 7, INR ≥1.6 at POD 7, and ALT/AST >2,000 IU/L within the first 7 POD.
Animals
C57BL/6 mice at 6–8 weeks of age were used (Jackson Laboratory, Bar Harbor, ME). Animals were housed in UCLA animal facility under specific pathogen-free conditions, received humane care according to the criteria outlined in the “Guide for the Care and Use of Laboratory Animals” (NIH publication 86-23 revised 1985).
Reagents
Recombinant form of human relaxin-2 (rhRLX; RLX030) was provided by Novartis International AG (East Hanover, NJ). Gene-specific small interfering RNA (siRNA) against GR (or scrambled siRNA) were purchased from Santa Cruz Biochemistry (Santa Cruz, CA); GR antagonist (RU-486) was obtained from Sigma Aldrich (St. Louis, MO).
Mouse liver transplantation
We used a well-established mouse model of ex-vivo hepatic cold storage followed by orthotopic liver transplantation (OLT), as described by our group (25). To mimic “marginal” human OLT setting, donor livers were stored in UW solution at 4°C for 18h prior to transplantation into syngeneic mice. Animals were treated with rhRLX (5μg/kg i.v.) or lactate ringer solution (control) at the time of reperfusion. In some experiments, donor livers were pre-incubated with GR antagonist (RU-486, 500nM) for 18h during the cold storage. OLT and serum samples were collected at 6h of reperfusion, the peak of hepatocellular damage in this model. Separate groups of OLT recipients were monitored for survival. The sham group underwent the same procedures except for OLT.
Hepatocellular function assay
Serum ALT and AST levels were measured with Infinity™ ALT and AST Liquid Stable Reagent (Thermo Scientific, Rockford, IL) and validated with Validate®GC3 (Maine Standards Company, LLC, ME).
Liver histology and IRI grading
Formalin-fixed paraffin-embedded liver sections (5μm) were stained with hematoxylin and eosin. The severity of IRI was graded using Suzuki’s criteria (26).
Immunohistochemistry
The expression of RXFP1 and GR (liver, heart, kidney, lung, esophagus) was examined using rabbit anti-RXFP1 Ab (Santa Cruz) and rabbit anti-GR mAb (Cell Signaling Technology, Danvers, MA). Immunostaining signals were visualized with a labeled polymer in the EnVision+ system horseradish-peroxidase kit (Dako, Carpinteria, CA). Liver infiltrating macrophages and neutrophils were detected with rat anti-CD11b Ab (BD Biosciences, San Jose, CA) and rat anti-Ly6G Ab (Bio-Rad, Hercules, CA), respectively. Signals were visualized with secondary Alexa Fluor 488 anti-rat IgG. Results were scored semi-quantitatively by blindly counting the number of positive cells in 10 HPF/section (x400).
Cell isolation and cultures
Primary mouse hepatocytes were isolated by a two-stage collagenase perfusion method (27). To trigger oxidative stress, hydrogen peroxide (H2O2; Sigma Aldrich) was added (2mM for 5h) into the culture with or without rhRLX pretreatment (1μg/ml for 24h). In some experiments, hepatocytes were transfected with GR-siRNA (or scrambled siRNA) using Lipofectamine reagent (Invitrogen, Waltham, MA) in advance to rhRLX treatment. Culture medium was analyzed for LDH cytotoxicity and ALT/AST levels.
TdT-mediated dUTP nick end labeling (TUNEL) assay
Cell death in formalin-fixed paraffin-embedded liver sections (5μm) was detected by Apop Tag Plus Peroxidase in Situ Apoptosis Kit (Millipore, Temecula, CA). Results were scored semi-quantitatively by blindly counting the number of positive cells in 10 HPF/section. Cell death in cultured hepatocytes was assessed by TUNEL Kit (Sigma Aldrich) and TUNEL-positive cells were counted in 4 HPF/group (x400).
Western blot assay
Proteins were extracted from liver tissues/hepatocyte cultures and their concentration was measured (BCA Protein Assay Kit, Thermo Scientific). Equal amount of protein was electrophoresed, blotted, and incubated with primary Ab, secondary HRP-conjugated Ab, and developed. Primary Ab detecting GR, Bcl-xL, Bcl-2, cleaved caspase 3, β-actin (Cell Signaling), HMGB1 (Abcam, Cambridge, MA) and RXFP1 (R&D Systems, Minneapolis, MN) were used. To compare protein expression in human OLT samples, densitometry quantification was conducted, as follows. In a preliminary study, one of Bx samples expressing all target proteins was assigned as a “reference” sample. Equal amount of protein lysate from each sample was applied to each well/gel, and target band intensity was normalized by reference sample, followed by normalization with β-actin.
Quantitative RT-PCR analysis
RNA was extracted from liver tissue samples using RNAse Mini Kit (Qiagen, Germantown, MD). A total of 5.0μg of RNA was reverse-transcribed into cDNA. Quantitative PCR was performed using DNA Engine with Chromo 4 Detector (MJ Research, Waltham, MA). The primers sequences are listed (Table S1). The expression of the target gene was normalized to the housekeeping HPRT.
ELISA
Serum HMGB1 concentration was measured by ELISA (MyBioSource, Inc., San Diego, CA) according to the manufacturer’s protocol.
Statistical analysis
In mouse studies, group comparisons were performed using a Student t-test. For human data, continuous values were analyzed by Mann-Whitney U test and categorical variables by Fisher’s exact test. Spearman’s correlation coefficient (r) was used to evaluate the strength of linear relationship between variables. The cumulative survival rate was analyzed by Kaplan-Meier method, and differences were compared using a log-rank test. EZR (Saitama Medical Center, Jichi Medical University), a graphical user interface for R (The R Foundation for Statistical Computing, version 3.2.2) and GraphPad Prism 5 for Mac (GraphPad Software, Inc., La Jolla, CA) were used for Fisher’s exact test and for the other analyses, respectively. A p-value of <0.05 was considered statistically significant.
Study approval
All studies were approved by the UCLA Institutional Research Board (IRB #13-000143) and Animal Research Committee.
Results
Hepatic GR expression correlates with hepatocellular function and anti-apoptotic phenotype in human OLT
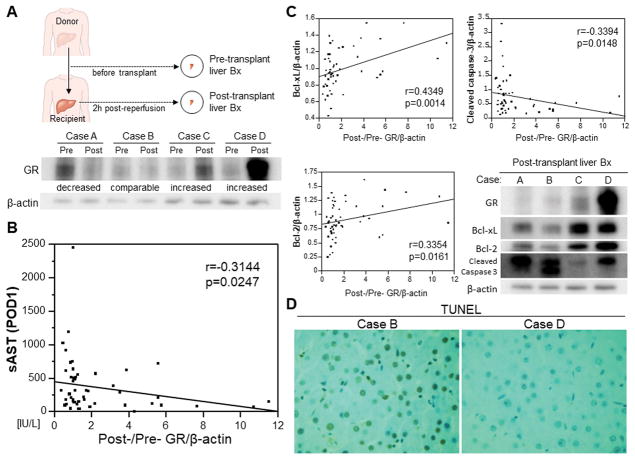
We aimed to evaluate retrospectively the peri-operative graft GR enhancement and its correlation with liver function in our human OLT cohort (n=51). Donor liver biopsies (Bx) were collected after cold storage at the back table (prior to the transplant surgery) while post-transplant liver Bx were obtained 2h after portal reperfusion (prior to the abdominal closure) (Fig. 1A). The Bx samples were analyzed by Western blots and post-/pre-transplant expression levels were calculated to determine peri-operative GR profile (representative 4 cases are shown in Fig. 1A). Interestingly, 43% of OLT recipients failed to increase graft GR peri-operatively (22/51; Post-/Pre-GR: median, 1.09; range, 0.29–11.5, Fig. S1). There was no significant correlation between GR increase and cold ischemia time or intraoperative blood loss (factors of surgical stress) (Fig. S2). Post-/pre-GR ratios negatively correlated with sAST levels at POD1 (r=-0.3144, p=0.0247, Fig. 1B), indicating peri-operative GR increase was accompanied by improved OLT function. Moreover, post-/pre-GR ratios correlated positively with Bcl-xL/Bcl-2 profile, and negatively with cleaved caspase 3 levels (Fig. 1C). Western blots (Fig. 1C) and TUNEL staining (Fig. 1D) from representative Bx samples (Fig. 1A) are shown.
Figure 1. Increased peri-transplant GR levels correlate with improved hepatocellular function and cytoprotection in human OLT.
(A) Pre-transplant (post cold storage) and post-transplant (2h after reperfusion) liver biopsies (Bx) were collected from fifty-one OLTs. Bx samples were analyzed by Western blots with β-actin normalization for post-/pre-transplant GR ratios. Four representative peri-operative GR profiles are shown (Case A: decreased, B: comparable, C/D: increased). (B) Relationship between post-/pre-GR ratio and sAST level at postoperative day 1 (POD1). (C) Relationship between post-/pre-GR ratio and post-transplant Bcl-xL, Bcl-2, cleaved caspase 3 levels. Representative Western blots (lower right). (D) Representative TUNEL staining (original magnification, x400). r: Spearman’s correlation coefficient.
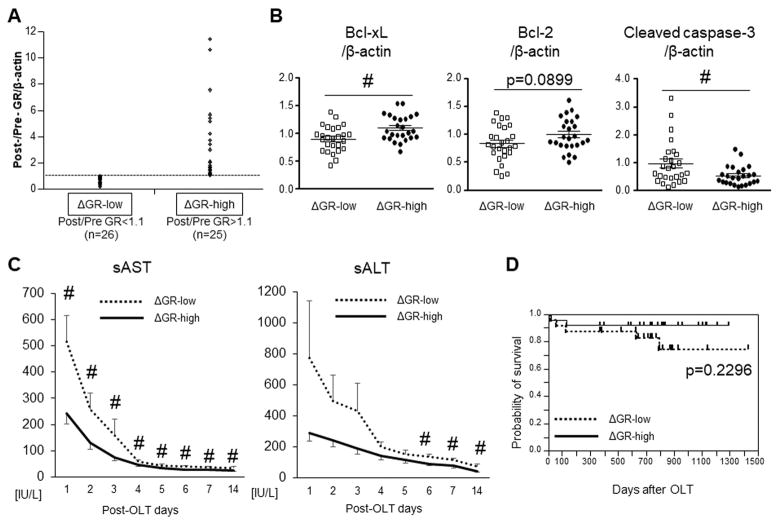
To evaluate the impact of intra-graft GR levels for clinical outcomes, fifty-one human OLTs were classified into ΔGR-low (post-/pre-GR<1.1, n=26) and ΔGR-high (post-/pre-GR>1.1, n=25) expression groups (Fig. 2A). The patients’ demographic data and clinical parameters are shown (Table S2). There was no correlation between ΔGR classification and donor/recipient background, including cold ischemia time, MELD score, age, gender or BMI. Consistent with Fig. 1C data, ΔGR-high cases showed suppressed cleaved caspase 3 (p<0.05) and enhanced Bcl-xL (p<0.05) expression. Despite similar trends, Bcl-2 variables did not reach statistically significant difference (p=0.0899) between ΔGR-low vs. ΔGR-high groups (Fig. 2B). OLT recipients characterized by ΔGR-high exhibited lower levels of sAST at POD1–14 (p<0.05) and of sALT at POD6–14 (p<0.05) as compared with ΔGR-low group (Fig. 2C). ΔGR-high recipients experienced shorter post-transplant ICU stay (14.4±1.8 vs 20.0±5.5 days, p=0.1930) and lower incidence of early allograft dysfunction (0.0 vs 11.5%, p=0.1248). To examine whether GR levels may predict long-term clinical outcomes, we analyzed cumulative post-transplant survival, with the median follow-up of 740 days (range, 4–1432). None of patients underwent secondary transplantation. Despite obvious trends, the improved survival in ΔGR-high group failed to reach statistical significance when compared with ΔGR-low group (p=0.2296, Fig. 2D).
Figure 2. Peri-transplant GR levels are associated with clinical OLT outcomes.
(A) Bx samples collected from fifty-one OLTs were divided into ΔGR-low (post-/pre-GR<1.1, n=26) and ΔGR-high (post-/pre-GR>1.1, n=25) groups. (B) Western blot-assisted expression of Bcl-xL, Bcl-2 and cleaved caspase 3. Data shown in dot plots and bars indicate mean±SEM. # p<0.05 (Mann-Whitney U test). (C) Serum AST and ALT levels at POD1–14. Dotted line indicates ΔGR-low, while solid line ΔGR-high. # p<0.05 (Mann-Whitney U test). (D) The cumulative probability of OLT survival (Kaplan-Meier method). Dotted line indicates ΔGR-low, while solid line ΔGR-high (log-rank test).
rhRLX ameliorates hepatocellular IR-damage and improves survival in mouse OLT
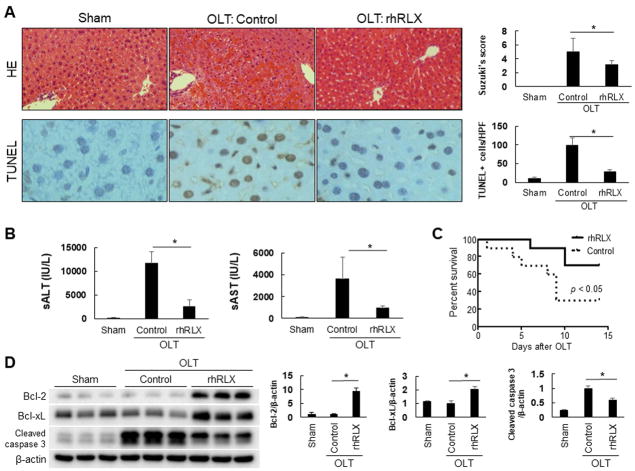
To determine the impact of pharmacological GR enhancement in the liver, we used rhRLX, a putative GR agonist, in a mouse model of extended (18h) ex vivo hepatic cold storage followed by OLT, which mimics marginal human liver transplant setting (25). After the optimal rhRLX dose and route of administration were determined (Fig. S3A/B), recipient mice were infused with a single dose of rhRLX (5μg/kg i.v.) or lactate ringer (control) immediately prior to reperfusion at the completion of surgery. At 6h of reperfusion, rhRLX treated OLTs showed attenuated sinusoidal congestion, vacuolization and hepatocellular necrosis as compared with controls (Fig. 3A). These correlated with diminished Suzuki’s histological grading of hepatocellular damage (p<0.05; Fig. 3A); decreased frequency of TUNEL+ cells (p<0.0005; Fig. 3A); depressed sALT (p<0.01) / sAST (p<0.05) levels (Fig. 3B); and improved OLT survival as compared with controls (70% vs. 30%; p<0.05; n=10/grp, Fig. 3C). In addition, rhRLX markedly increased Western blot-assisted expression of anti-apoptotic Bcl-2/Bcl-xL, while depressing pro-apoptotic cleaved caspase 3 (Fig. 3D). Thus, by enhancing anti-apoptotic programs, rhRLX attenuated hepatocellular damage and markedly improved survival of OLTs subjected to prolonged cold storage.
Figure 3. rhRLX alleviates hepatocellular damage and improves post-transplant survival in IR-stressed mouse OLT.
Mouse (C57/Bl6) livers subjected to 18h of cold storage were transplanted orthotopically to syngeneic mice. OLT recipients were treated with recombinant human relaxin (rhRLX; 5μg/kg i.v.) or equivalent amount of lactate ringer solution (control) at reperfusion. Liver grafts and serum samples were analyzed at 6h post-OLT. (A) Representative hematoxylin and eosin staining (upper left, original magnification, x100) and Suzuki’s histological grading of liver IRI (upper right, n=5–6/group). Representative TUNEL staining (lower left, original magnification, x400) and quantification of TUNEL-positive cells/HPF (n=5/group). (B) Serum ALT and AST levels (IU/L, n=5–6/group). (C) rhRLX treated or control recipients were monitored for 14 days and cumultive survival was analyzed by Kaplan-Meier method. Solid line indicates rhRLX-treated while dotted line control mice (n=10/group, p<0.05, log-rank test). (D) Western blot-asisted detection and relative intensity ratio of Bcl-2, Bcl-xL and cleaved caspase 3. β-actin expression served as an internal control and used for normalization (n=3/group). Data are shown as mean±SD (*p<0.05, Student t-test).
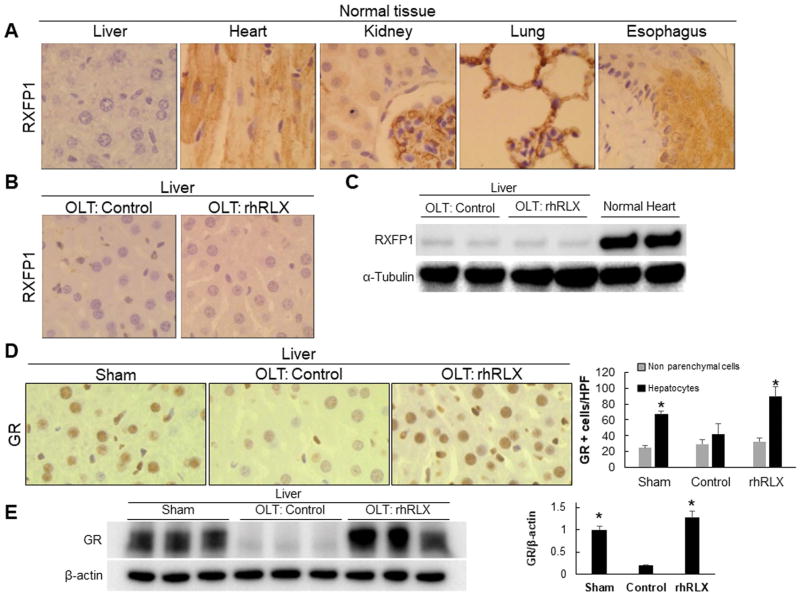
rhRLX interacts with hepatic GR rather than RXFP1 cognate receptor
We used immunohistochemistry and Western blots to analyze hepatic levels of two major rhRLX binding partners, i.e., RXFP1 (RLX family peptide receptor 1, cognate receptor) and GR. In contrast to murine heart, kidney, lung, or esophagus, RXFP1 expression was barely detectable in normal mouse liver (Fig. 4A), and neither affected by IR-stress nor rhRLX treatment (Fig. 4B). Moreover, marginal induction of RXFP1 was found in IR-stressed OLTs with or without adjunctive rhRLX (Fig. 4C), suggesting that hepatic RXFP1 signaling is not essential in rhRLX-mediated in vivo effects.
Figure 4. rhRLX triggers GR but not RXFP1 expression in IR-stressed mouse OLT.
(A) Representative RXFP1 staining in mouse liver, heart, kidney, lung and esophagus under basal condition (original magnification, x400; n=3). (B) Representative RXFP1 staining in control and rhRLX treated OLT (original magnification, x400; n=3). (C) Representative Western blot-asisted detection of RXFP1 in control OLT, rhRLX-treated OLT and normal heart (n=4/group). (D) Representative GR staining in sham-operated liver, control OLT and rhRLX-treated OLT, and quantification of GR-positive cells in non-parenchymal cells (gray) vs. hepatocytes (black) (n=5/group). (E) Western blot-assisted detection and relative intensity ratio of GR. β-actin expression served as an internal control and used for normalization (n=3/group). Data shown as mean±SD. *p<0.05 vs. OLT: Control (Student t-test).
Immunohistochemistry confirmed predominantly hepatocyte GR expression (Fig. 4D). Although rhRLX treatment recreated otherwise blunted GR levels in mouse liver grafts (Fig. 4D/E), relatively low GR expression in OLT-infiltrating non-parenchymal cells was only marginally affected by rhRLX (Fig. 4D). Thus, rhRLX – hepatocyte GR crosstalk is essential for OLT protection against IR-stress.
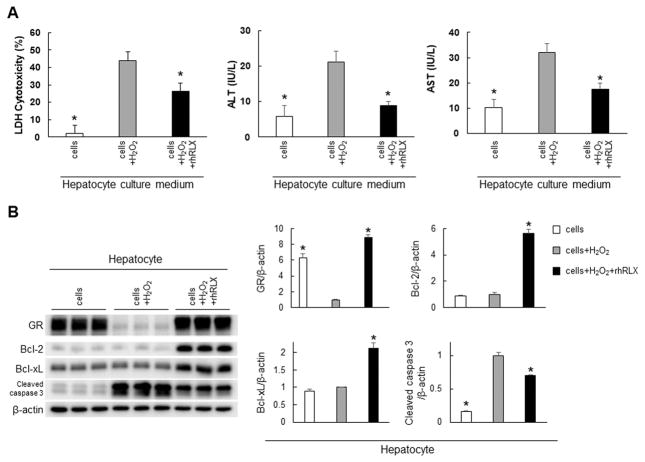
rhRLX attenuates reactive oxygen species-induced hepatocyte death and increases GR/Bcl-2/Bcl-xL expression in vitro
To focus on hepatocyte rhRLX – GR function, we investigated primary mouse hepatocyte cultures exposed to H2O2-induced oxidative stress. As shown in Fig. 5A, pretreatment with rhRLX (1μg/ml) mitigated hepatocellular death, evidenced by depressed LDH cytotoxicity as well as ALT/AST release into the culture supernatants. Consistent with our in vivo findings (Fig. 4D/E), adjunctive rhRLX suppressed otherwise elevated cleaved caspase 3 while increasing GR/Bcl-2/Bcl-xL expression profile (Fig. 5B).
Figure 5. rhRLX protects hepatocytes from H2O2-induced cell death while upregulating GR/Bcl-2/Bcl-xL in vitro.
Primary mouse hepatocytes exposed to H2O2-induced oxidative stress (2mM; 5h) were pretreated with or without rhRLX (1μg/ml; 24h). (A) Cell damage was assessed by LDH, ALT and AST levels in the culture medium (n=4/group) (B) Western blot-assisted detection and relative intensity ratio of GR, Bcl-2, Bcl-xL, cleaved caspase 3. β-actin expression served as an internal control and used for normalization (n=3/group). Data shown as mean±SD. *p<0.05 vs. cells+H2O2 (Student t-test).
rhRLX attenuates H2O2-stressed hepatocyte death in GR-dependent manner
Having shown GR induction and cytoprotection by exogenous rhRLX in vivo and in vitro, we focused on the functional significance of GR signaling in rhRLX-conditioned primary hepatocyte cultures. Unlike in scrambled siRNA-treated group, adjunctive GR-siRNA knockdown recreated cellular damage in rhRLX treated hepatocytes, evidenced by increased LDH and ALT/AST levels in otherwise H2O2-stress resistant rhRLX-treated cells (Fig. 6A). Neither rhRLX nor adjunctive GR knockdown by siRNA affected anti-oxidant heme oxygenase-1 (hsp 32) expression in hepatocyte cultures (Fig. S4). In addition, GR silencing suppressed Bcl-2/Bcl-xL while augmenting cleaved caspase 3 (Fig. 6B) and restoring TUNEL+ (Fig. 6C) hepatocyte expression. These data indicate that rhRLX mitigates hepatocyte death via GR – Bcl-2/Bcl-xL signaling axis.
Figure 6. Hepatocyte protection by rhRLX against reactive oxygen species-stress is GR-dependent.
H2O2-stressed (2mM; 5h) primary mouse hepatocytes were pretreated with or without rhRLX (1μg/ml; 24h) and siRNA against GR. (A) Culture medium was screened for LDH, ALT and AST levels (n=4/group). (B) Western blot-assisted detection and relative intensity ratio of GR, Bcl-2, Bcl-xL, cleaved caspase 3. β-actin expression served as an internal control and used for normalization (n=3/group). (C) Representative TUNEL-assisted detection of hepatocyte death (Actin: green, DAPI: blue, TUNEL: red) and quantification of TUNEL-positive cells (four randomly chosen HPF/group). Data shown as mean±SD. *p<0.05 vs. cells+H2O2+rhRLX+siRNA (scrambled) (Student t-test).
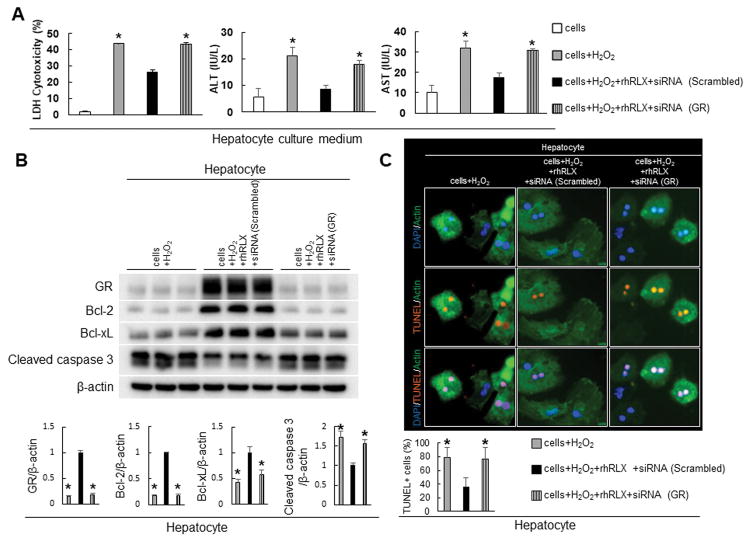
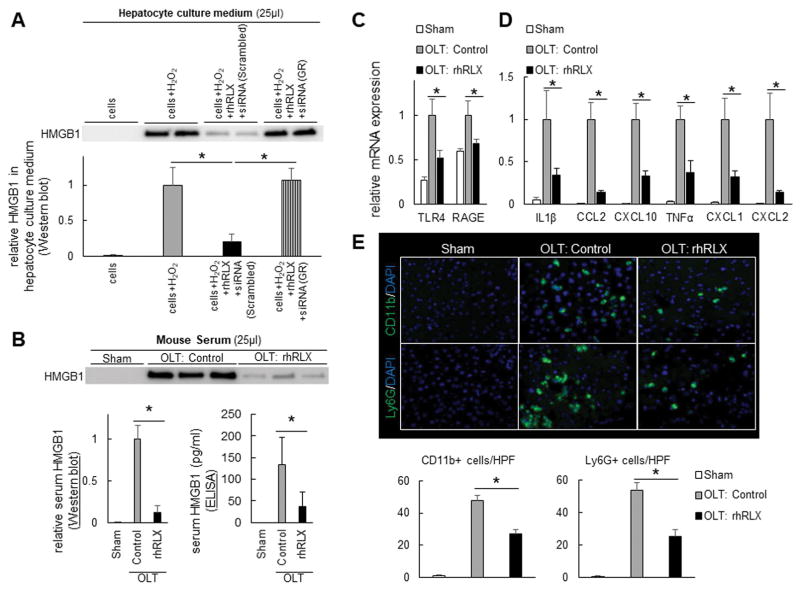
rhRLX prevents HMGB1 translocation and release from H2O2-stressed hepatocytes
As the release of damage-associated molecular patterns from injured cells is the key event in early phase of innate immune activation, we next examined HMGB1 levels in H2O2-stressed mouse hepatocyte cultures. As shown in Fig. 7A, the efficacy of rhRLX to inhibit translocation of cellular HMGB1 into the culture medium was blocked after adjunctive GR silencing (siRNA) as compared with scrambled siRNA-treated cells. Thus, rhRLX – GR signaling prevented cell death (Fig. 6A–C) and suppressed HMGB1 release from stressed hepatocytes (Fig. 7A).
Figure 7. rhRLX mitigates HMGB1 translocation and suppresses TLR4/RAGE as well as pro-inflammatory phenotype in IR-stressed OLT.
(A) H2O2-stressed (2mM; 5h) primary mouse hepatocytes were pretreated with or without rhRLX (1μg/ml; 24h) and siRNA against GR. Representative Western blot-assisted detection of HMGB1 in culture medium and quantitation of relative expression values (n=3–4/group, *p<0.05) (B–E) Mouse livers stored for 18h in 4C were transplanted orthotopically followed by 6h of reperfusion. rhRLX (5μg/kg i.v.) or lactate ringer (control) was administered at the time of reperfusion. (B) Representative Western blot-assisted HMGB1 detection in serum and quantitation of relative expression values (n=3–4/group, *p<0.05), and serum HMGB1 levels measured by ELISA (pg/ml, n=4–5/each, *p<0.05) (C/D) qRT-PCR-assisted detection of mRNA coding for TLR4, RAGE, IL1β, CCL2, CXCL10, TNFα, CXCL1 and CXCL2. Data were normalized to HPRT gene expression (n=4/group, *p<0.05) (E) Representative immunohistochemical staining and quantification of OLT-infiltrating CD11b+ and Ly6G+ cells (positive cells/HPF; original magnification, x400; n=5/group, *p<0.05). Data shown as mean±SD (Student t-test).
rhRLX suppresses cellular HMGB1 release to mitigate IRI in mouse OLT
To confirm the impact of rhRLX on HMGB1 translocation and release in vivo, we profiled HMGB1 and inflammatory markers in IR-stressed mouse OLTs. Consistently, rhRLX treatment reduced serum HMGB1 levels (Western blots & ELISA, Fig. 7B) as well as hepatic TLR4 and RAGE, i.e., major extracellular HMGB1-activated immune receptors (Fig. 7C). Consistent with proinflammatory pathway blockade, rhRLX mitigated mRNA levels coding for IL1β, CCL2, CXCL10, TNFα, CXCL1 and CXCL2 (Fig. 7D) while decreasing macrophage (CD11b) and neutrophil (Ly6G) infiltration (Fig. 7E). Thus, rhRLX attenuated local inflammation in vivo, at least in part, by suppressing translocation of cellular HMGB1 in IR-stressed OLTs.
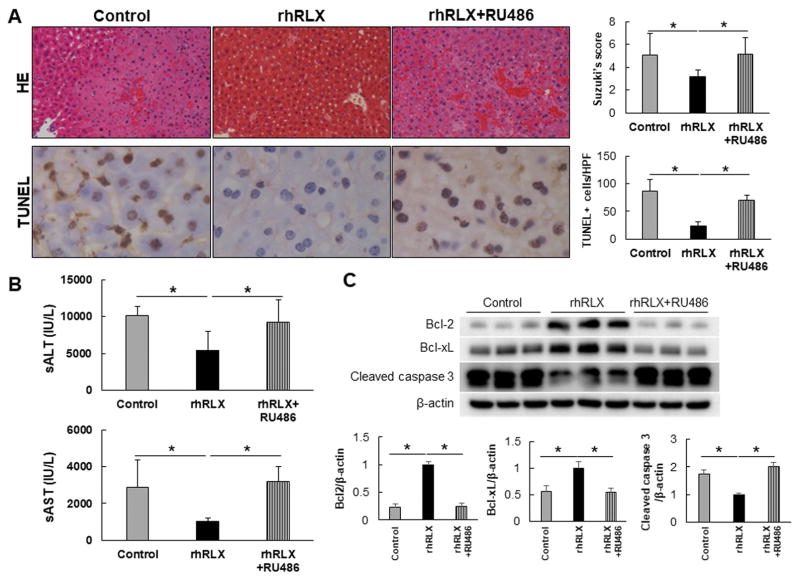
rhRLX hepatoprotection in IR-stressed mouse OLT is GR-dependent
Having shown rhRLX facilitated GR-dependent hepatoprotection in vitro (Fig. 6), accompanied by HMGB1-mediated immune regulation (Fig. 7), we aimed to determine the significance of GR signaling in vivo model. Indeed, rhRLX-induced hepatoprotection was abolished after adjunctive treatment with RU486 (GR antagonist), as evidenced by hematoxylin and eosin staining, Suzuki’s scores, TUNEL staining (Fig. 8A), and sAST/sALT levels (Fig. 8B). In parallel, RU486 adjunct diminished Bcl-2/Bcl-xL while enhancing cleaved caspase 3 expression in rhRLX-treated OLT (Fig. 8C). RU486 treatment alone did not increase liver damage (sAST/sALT level and Suzuki’s score) as compared to control OLT (Fig. S5). Thus, hepatocyte GR functions as an essential regulator in rhRLX-mediated protection against IRI.
Figure 8. GR antagonist (RU-486) abrogates rhRLX-induced hepatoprotection in IR-stressed mouse OLT.
Mouse livers subjected to 18h of cold storage were transplanted to syngeneic recipients treated with rhRLX or lactate ringer (control) at the time of reperfusion. Separate donor livers were pre-incubated with UW containing GR antagonist (RU-486, 500nM) for 18h during cold storage. (A) Representative hematoxylin and eosin staining (upper left, original magnification, x100) and Suzuki’s histological IRI grading (upper right, n=3–5/group). Representative TUNEL staining (lower left, original magnification, x400) and quantification of TUNEL-positive cells/HPF (n=3–4/group) (B) Serum ALT and AST levels (IU/L, n=3–5/group). (C) Western blot-assisted detection and relative intensity ratio of Bcl-2, Bcl-xL and cleaved caspase 3. β-actin expression served as an internal control and used for normalization (n=3/group). Data shown as mean±SD (Student t-test).
Discussion
This is the first study, to the best of our knowledge, demonstrating the key regulatory role of hepatic GR signaling in inflammatory injury in a human liver. Indeed, increased peri-operative GR expression correlated with enhanced anti-apoptotic programs and preservation of hepatocellular function in OLT recipients (Fig. 1–2). Our parallel studies in a clinically relevant mouse model of hepatic cold storage and liver transplantation have revealed cytoprotective function and putative mechanisms of hepatocyte rhRLX – GR crosstalk in vivo and in vitro. A single i.v. infusion of rhRLX, a GR agonist, conferred OLT protection against IR-insult, evidenced by decreased release of liver enzymes, suppression of histopathological tissue injury scores, and modulation of apoptosis. These findings were confirmed in primary mouse hepatocyte cultures where addition of rhRLX attenuated cell death by increasing GR/Bcl-2/Bcl-xL expression and preventing HMGB1 translocation from H2O2-stressed cells. GR-dependent cytoprotection after rhRLX treatment was confirmed in TNFα-stressed hepatocyte cultures (data not shown). Hence, this translational study highlights previously unrecognized function of hepatocyte GR and rhRLX therapy in IR-stressed livers.
A recent phase III randomized clinical trial in a cohort of 1,161 patients with acute heart failure, demonstrated positive outcomes after rhRLX treatment, only with controllable hypotension (19). Of note, up to 48h continuous intravenous rhRLX administration did not increase the incidence of adverse infections. In addition, a single infusion of rhRLX at reperfusion in our murine IRI-OLT model was well tolerated and markedly improved post-transplant liver function and survival (Fig. 3C). Thus, by documenting hepatocyte-protective rhRLX – GR signaling, our findings complement published data in patients with acute heart failure and validate future rhRLX clinical trials. Failure to find significant differences in post-OLT survival between ΔGR-high vs. ΔGR-low groups, despite obvious trends, may be due to limited patient cohort. Further studies are required as the correlation between IRI severity and post-OLT graft/patient survival remains controversial (28, 29).
In the clinical arm of our study, 43% of human OLTs failed to increase GR expression (Fig. S1) despite a routine hydrocortisone bolus given at reperfusion. High ΔGR was associated with a trend toward more severe recipient status (higher MELD, longer pre-transplant hospital/ICU stay) while favoring lower donor pre-transplant transaminase levels (Table S2). However, these differences failed to reach statistical significance and studies in larger patient cohorts are needed to further explore these clinical factors. Unable to elucidate the causality of such a GR decrease, we may envision the following scenarios. First, the cellular stress may alter GR expression profile as hypoxia did reduce GR function and its ligand binding ability in a fetal heart (30). Moreover, NLRP3/caspase-1 axis, which is essential in liver IRI pathogenesis, cleaves cellular GR and diminishes cell sensitivity to glucocorticoid (31). In our study, cold storage (18h) alone did not decrease GR expression in the liver graft (data not shown). However, 6h of reperfusion depressed hepatic GR in vivo (Fig. 4D/E); and H2O2–induced stress depressed hepatocyte GR in vitro (Fig. 5B) while increasing cleaved caspase-1 (data not shown). Second, despite hypothalamic-pituitary-adrenal axis secreting glucocorticoid in stress response to a trauma (32), major surgery may increase glucocorticoid demand throughout the body, with actual demand sometimes exceeding physiological/pharmacological supply, and resulting in the adrenal failure. In this case, GR suppression may result in insufficient ligand binding, implying the 43% of GR-depressed OLTs might potentially be rescued by the adequate ligand supply. We are aware of putative differences between human and rodent glucocorticoid biological functions. While corticosterone is the major circulating glucocorticoid in rodents due to the absence of a cortisol synthesis enzyme, in humans the corticosterone level is 10–20-fold lower than of cortisol, with the latter exhibiting far more powerful activity than corticosterone (33). Thus, although rhRLX treatment markedly increased GR expression in murine OLT (Fig. 4D–E), it remains unknown whether rhRLX can equally enhance hepatic GR in coritisol-dominated human OLT. Despite these shortcomings, however, our findings validate future studies on rhRLX – GR crosstalk in human liver graft GR expression/function.
RXFP1 expression was barely detectable in a mouse liver, and neither OLT nor rhRLX treatment made any difference (Fig. 4A–C). Indeed, although Fallowfield reported undetectable RXPF1 protein levels in normal human or rat livers, hepatic stellate cells, myofibroblasts and sinusoidal endothelial cells became RXFP1+ in fibrotic livers (34). However, despite marginal RXFP1 expression in OLTs, we cannot exclude a possibility of RXFP1 signaling functioning as a part of a complex rhRLX cytoprotection axis. Indeed, one of the distinct relaxin actions is mediated by endothelial RXFP1-PI3K-Akt-eNOS signaling (35), while relaxin dilated sinusoid in un-stressed rat liver via NO-dependent manner (36). Further studies using RXFP1 knockout mice or “RXFP1-inactive relaxin (chemically modified porcine relaxin biologically inactive at RXFP1)” (37) are warranted to verify the involvement of RXFP1 in rhRLX cytoprotection. On the other hand, GR knockdown by siRNA abolished hepatocyte protection by rhRLX in vitro (Fig. 6); while adjunctive GR antagonist (RU486) diminished graft protection seen otherwise following rhRLX monotherapy in vivo. However, as GR is expressed ubiquitously, we cannot exclude the possibility that RU486 might influence other cell types in IRI pathogenesis (e.g., macrophage, lymphocyte, endothelial cells). Hepatocyte-specific GR knockout mice (38) are indispensable to confirm the significance of hepatocyte-specific GR signaling.
HMGB1, a multifunctional danger molecule (alarmin) orchestrating the inflammatory and immune cascades in organ IRI (3), is a ubiquitously expressed protein that binds to the minor groove of nuclear DNA to control the activity of transcription factors by structurally modifying the DNA double helix. Once translocated and released passively or secreted actively from injured or dying cells into extracellular space, it acts as a key damage-associated molecular patterns that alerts innate immune system to activate macrophages via downstream TLR4 and neutrophils by RAGE signaling (39). Indeed, Ilmakunnas et al. reported that HMGB1 may represent a useful biomarker of hepatocellular damage in human liver transplantation (40). The efficacy of pharmacological HMGB1 deactivation in warm hepatic rat and mouse (41) IRI models has been recently reported. Thus, HMGB1 secretion from injured hepatocytes is not only an indicator of liver function, but it may also serve as a regulator of sterile inflammatory tissue injury. Consistent with the latter, suppression of HMGB1 mobilization and translocation from hepatocytes was accompanied by decreased TLR4/RAGE expression and IR-inflammation, suggesting anti-inflammatory phenotype in mouse OLT after treatment with rhRLX could be attributed, at least in part, to suppressed HMGB1 secretion. We are aware rhRLX – GR signaling may directly regulate macrophage activation. Indeed, porcine relaxin or RXFP1-inactive relaxin suppressed TNFα/IL6 production from THP-1 cells while adjunctive RU486 reversed that effect (37). We found rhRLX suppressed pro-inflammatory while enhancing anti-inflammatory gene expression programs in mouse bone marrow-derived macrophage (BMDM) cultures (data not shown). On the other hand, RLX-2 stimulated THP-1 cell adhesion and migration through RXFP1-depending mechanism (42). Although relaxin may promote inflammation via RXFP1 in decidual macrophage (43), addition of rhRLX failed to alter total GR or RXFP1 protein expression in BMDM cultures (Nakamura, unpublished). The precise rhRLX macrophage regulatory mechanism requires further in-depth studies.
Gujral et al. reported the majority of cell death in rat livers subjected to warm ischemia occurred by necrosis and only a minority of damaged hepatocytes displaying features of apoptosis (44). Indeed, pan-caspase inhibitors Z-Asp-cmk (44) and Z-VD-fmk (45) failed to protect livers against IRI. However, necrosis and apoptosis represent interdependent phenomena resulting from activation of shared pathways and apoptosis precedes necrosis in the pathogenesis of liver IRI (44, 45). In addition, although some pan-caspase inhibitors paradoxically reported increased necrosis (46), necroptosis (47) or autophagic cell death (48), it is noteworthy that a caspase inhibitor IDN-6556, which reduced liver IRI in a murine model was also tested in a phase II clinical liver transplant trial (49). We recently reported that hepatoprotection after treatment with Nec-1s (a necrosis inhibitor) was abolished in Kupffer cell-deficient mice, indicating Nec-1s’s direct hepatocyte effect failed to mitigate liver cell death in the mechanism of IRI (50). Consistent with the anti-apoptotic program critically important in liver IR-resistance, in our clinical arm screen of fifty-one OLT patients, post-transplant Bcl-xL expression negatively correlated with AST levels at POD1 (r=-0.3148, p=0.0245); and rhRLX treatment attenuated hepatocellular damage while increasing Bcl-xL/Bcl-2 and depressing cleaved caspase-3 in IR-stressed mouse OLT.
In conclusion, our results underscore the role of GR signaling as a novel regulator of hepatocellular protection in IR-stressed OLT. As a promising candidate to mitigate innate activation and sterile inflammatory tissue injury, future studies on rhRLX, a GR ligand and agonist, in the management of liver transplant recipients are warranted.
Supplementary Material
Acknowledgments
Financial support: Novartis International AG; NIH grants PO1 AI120944; RO1 DK062357, DK107533, DK102110 (to JWKW); and The Dumont Research Foundation.
We thank Ko Takanashi (UCLA-TPCL) and Damla Oncel (undergrad UCLA student) for immunohistochemical assistance; and Dr. Takahiro Ito for helping to collect clinical data.
List of abbreviations
- Bx
biopsy
- GR
glucocorticoid receptor
- H2O2
hydrogen peroxide
- HMGB1
high-mobility group box 1
- IRI
ischemia-reperfusion injury
- OLT
orthotopic liver transplantation
- POD
post-operative day
- RLX-2
relaxin-2
- rhRLX
recombinant human RLX-2
- RXFP1
relaxin family peptide receptor-1
- sALT
serum alanine aminotransferase
- sAST
serum aspartate aminotransferase
References
- 1.Dutkowski P, Linecker M, DeOliveira ML, Mullhaupt B, Clavien PA. Challenges to liver transplantation and strategies to improve outcomes. Gastroenterology. 2015;148:307–323. doi: 10.1053/j.gastro.2014.08.045. [DOI] [PubMed] [Google Scholar]
- 2.Zhai Y, Petrowsky H, Hong JC, Busuttil RW, Kupiec-Weglinski JW. Ischaemia-reperfusion injury in liver transplantation--from bench to bedside. Nat Rev Gastroenterol Hepatol. 2013;10:79–89. doi: 10.1038/nrgastro.2012.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tsung A, Tohme S, Billiar TR. High-mobility group box-1 in sterile inflammation. J Intern Med. 2014;276:425–443. doi: 10.1111/joim.12276. [DOI] [PubMed] [Google Scholar]
- 4.Bilbao G, Contreras JL, Eckhoff DE, Mikheeva G, Krasnykh V, Douglas JT, Thomas FT, et al. Reduction of ischemia-reperfusion injury of the liver by in vivo adenovirus-mediated gene transfer of the antiapoptotic Bcl-2 gene. Ann Surg. 1999;230:185–193. doi: 10.1097/00000658-199908000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shawky HM, Younan SM, Rashed LA, Shoukry H. Effect of recombinant erythropoietin on ischemia-reperfusion-induced apoptosis in rat liver. J Physiol Biochem. 2012;68:19–28. doi: 10.1007/s13105-011-0114-2. [DOI] [PubMed] [Google Scholar]
- 6.Nicolaides NC, Galata Z, Kino T, Chrousos GP, Charmandari E. The human glucocorticoid receptor: molecular basis of biologic function. Steroids. 2010;75:1–12. doi: 10.1016/j.steroids.2009.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gruver-Yates AL, Cidlowski JA. Tissue-specific actions of glucocorticoids on apoptosis: a double-edged sword. Cells. 2013;2:202–223. doi: 10.3390/cells2020202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gascoyne DM, Kypta RM, Vivanco M. Glucocorticoids inhibit apoptosis during fibrosarcoma development by transcriptionally activating Bcl-xL. J Biol Chem. 2003;278:18022–18029. doi: 10.1074/jbc.M301812200. [DOI] [PubMed] [Google Scholar]
- 9.Bailly-Maitre B, de Sousa G, Zucchini N, Gugenheim J, Boulukos KE, Rahmani R. Spontaneous apoptosis in primary cultures of human and rat hepatocytes: molecular mechanisms and regulation by dexamethasone. Cell Death Differ. 2002;9:945–955. doi: 10.1038/sj.cdd.4401043. [DOI] [PubMed] [Google Scholar]
- 10.Subhas G, Gupta A, Bakston D, Silberberg B, Lobocki C, Andrus L, Decker M, et al. Protective effect of methylprednisolone on warm ischemia-reperfusion injury in a cholestatic rat liver. Am J Surg. 2010;199:377–380. doi: 10.1016/j.amjsurg.2009.09.012. discussion 380–371. [DOI] [PubMed] [Google Scholar]
- 11.Orci LA, Toso C, Mentha G, Morel P, Majno PE. Systematic review and meta-analysis of the effect of perioperative steroids on ischaemia-reperfusion injury and surgical stress response in patients undergoing liver resection. Br J Surg. 2013;100:600–609. doi: 10.1002/bjs.9035. [DOI] [PubMed] [Google Scholar]
- 12.Di Lascio G, Harmelin G, Targetti M, Nanni C, Bianchi G, Gasbarri T, Gelsomino S, et al. Cellular retrograde cardiomyoplasty and relaxin therapy for postischemic myocardial repair in a rat model. Tex Heart Inst J. 2012;39:488–499. [PMC free article] [PubMed] [Google Scholar]
- 13.Teichman SL, Unemori E, Teerlink JR, Cotter G, Metra M. Relaxin: review of biology and potential role in treating heart failure. Curr Heart Fail Rep. 2010;7:75–82. doi: 10.1007/s11897-010-0010-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lodhi RS, Nakabayashi K, Suzuki K, Yamada AY, Hazama R, Ebina Y, Yamada H. Relaxin has anti-apoptotic effects on human trophoblast-derived HTR-8/SV neo cells. Gynecol Endocrinol. 2013;29:1051–1054. doi: 10.3109/09513590.2013.829444. [DOI] [PubMed] [Google Scholar]
- 15.Nistri S, Chiappini L, Sassoli C, Bani D. Relaxin inhibits lipopolysaccharide-induced adhesion of neutrophils to coronary endothelial cells by a nitric oxide-mediated mechanism. Faseb j. 2003;17:2109–2111. doi: 10.1096/fj.03-0216fje. [DOI] [PubMed] [Google Scholar]
- 16.Lekgabe ED, Kiriazis H, Zhao C, Xu Q, Moore XL, Su Y, Bathgate RA, et al. Relaxin reverses cardiac and renal fibrosis in spontaneously hypertensive rats. Hypertension. 2005;46:412–418. doi: 10.1161/01.HYP.0000171930.00697.2f. [DOI] [PubMed] [Google Scholar]
- 17.Teerlink JR, Cotter G, Davison BA, Felker GM, Filippatos G, Greenberg BH, Ponikowski P, et al. Serelaxin, recombinant human relaxin-2, for treatment of acute heart failure (RELAX-AHF): a randomised, placebo-controlled trial. Lancet. 2013;381:29–39. doi: 10.1016/S0140-6736(12)61855-8. [DOI] [PubMed] [Google Scholar]
- 18.Halls ML, Bathgate RA, Summers RJ. Relaxin family peptide receptors RXFP1 and RXFP2 modulate cAMP signaling by distinct mechanisms. Mol Pharmacol. 2006;70:214–226. doi: 10.1124/mol.105.021691. [DOI] [PubMed] [Google Scholar]
- 19.Bathgate RA, Halls ML, van der Westhuizen ET, Callander GE, Kocan M, Summers RJ. Relaxin family peptides and their receptors. Physiol Rev. 2013;93:405–480. doi: 10.1152/physrev.00001.2012. [DOI] [PubMed] [Google Scholar]
- 20.Collino M, Rogazzo M, Pini A, Benetti E, Rosa AC, Chiazza F, Fantozzi R, et al. Acute treatment with relaxin protects the kidney against ischaemia/reperfusion injury. J Cell Mol Med. 2013;17:1494–1505. doi: 10.1111/jcmm.12120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Alexiou K, Matschke K, Westphal A, Stangl K, Dschietzig T. Relaxin is a candidate drug for lung preservation: relaxin-induced protection of rat lungs from ischemia-reperfusion injury. J Heart Lung Transplant. 2010;29:454–460. doi: 10.1016/j.healun.2009.09.012. [DOI] [PubMed] [Google Scholar]
- 22.Boehnert MU, Hilbig H, Armbruster FP. Relaxin as an additional protective substance in preserving and reperfusion solution for liver transplantation, shown in a model of isolated perfused rat liver. Ann N Y Acad Sci. 2005;1041:434–440. doi: 10.1196/annals.1282.065. [DOI] [PubMed] [Google Scholar]
- 23.Dschietzig T, Bartsch C, Stangl V, Baumann G, Stangl K. Identification of the pregnancy hormone relaxin as glucocorticoid receptor agonist. Faseb j. 2004;18:1536–1538. doi: 10.1096/fj.03-1120fje. [DOI] [PubMed] [Google Scholar]
- 24.Teerlink JR, Cotter G, Davison BA, Felker GM, Filippatos G, Greenberg BH, Ponikowski P, et al. Serelaxin, recombinant human relaxin-2, for treatment of acute heart failure (RELAX-AHF): a randomised, placebo-controlled trial. Lancet. 2013;381:29–39. doi: 10.1016/S0140-6736(12)61855-8. [DOI] [PubMed] [Google Scholar]
- 25.Shen XD, Gao F, Ke B, Zhai Y, Lassman CR, Tsuchihashi S, Farmer DG, et al. Inflammatory responses in a new mouse model of prolonged hepatic cold ischemia followed by arterialized orthotopic liver transplantation. Liver Transpl. 2005;11:1273–1281. doi: 10.1002/lt.20489. [DOI] [PubMed] [Google Scholar]
- 26.Suzuki S, Toledo-Pereyra LH, Rodriguez FJ, Cejalvo D. Neutrophil infiltration as an important factor in liver ischemia and reperfusion injury. Modulating effects of FK506 and cyclosporine. Transplantation. 1993;55:1265–1272. doi: 10.1097/00007890-199306000-00011. [DOI] [PubMed] [Google Scholar]
- 27.Tamaki N, Hatano E, Taura K, Tada M, Kodama Y, Nitta T, Iwaisako K, et al. CHOP deficiency attenuates cholestasis-induced liver fibrosis by reduction of hepatocyte injury. Am J Physiol Gastrointest Liver Physiol. 2008;294:G498–505. doi: 10.1152/ajpgi.00482.2007. [DOI] [PubMed] [Google Scholar]
- 28.Berberat PO, Friess H, Schmied B, Kremer M, Gragert S, Flechtenmacher C, Schemmer P, et al. Differentially expressed genes in postperfusion biopsies predict early graft dysfunction after liver transplantation. Transplantation. 2006;82:699–704. doi: 10.1097/01.tp.0000233377.14174.93. [DOI] [PubMed] [Google Scholar]
- 29.Ali JM, Davies SE, Brais RJ, Randle LV, Klinck JR, Allison ME, Chen Y, et al. Analysis of ischemia/reperfusion injury in time-zero biopsies predicts liver allograft outcomes. Liver Transpl. 2015;21:487–499. doi: 10.1002/lt.24072. [DOI] [PubMed] [Google Scholar]
- 30.Xue Q, Dasgupta C, Chen M, Zhang L. Foetal hypoxia increases cardiac AT(2)R expression and subsequent vulnerability to adult ischaemic injury. Cardiovasc Res. 2011;89:300–308. doi: 10.1093/cvr/cvq303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yue S, Zhu J, Zhang M, Li C, Zhou X, Zhou M, Ke M, et al. The myeloid heat shock transcription factor 1/beta-catenin axis regulates NLR family, pyrin domain-containing 3 inflammasome activation in mouse liver ischemia/reperfusion injury. Hepatology. 2016;64:1683–1698. doi: 10.1002/hep.28739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Desborough JP. The stress response to trauma and surgery. Br J Anaesth. 2000;85:109–117. doi: 10.1093/bja/85.1.109. [DOI] [PubMed] [Google Scholar]
- 33.Raubenheimer PJ, Young EA, Andrew R, Seckl JR. The role of corticosterone in human hypothalamic-pituitary-adrenal axis feedback. Clin Endocrinol (Oxf) 2006;65:22–26. doi: 10.1111/j.1365-2265.2006.02540.x. [DOI] [PubMed] [Google Scholar]
- 34.Fallowfield JA, Hayden AL, Snowdon VK, Aucott RL, Stutchfield BM, Mole DJ, Pellicoro A, et al. Relaxin modulates human and rat hepatic myofibroblast function and ameliorates portal hypertension in vivo. Hepatology. 2014;59:1492–1504. doi: 10.1002/hep.26627. [DOI] [PubMed] [Google Scholar]
- 35.McGuane JT, Debrah JE, Sautina L, Jarajapu YP, Novak J, Rubin JP, Grant MB, et al. Relaxin induces rapid dilation of rodent small renal and human subcutaneous arteries via PI3 kinase and nitric oxide. Endocrinology. 2011;152:2786–2796. doi: 10.1210/en.2010-1126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bani D, Nistri S, Quattrone S, Bigazzi M, Bani Sacchi T. The vasorelaxant hormone relaxin induces changes in liver sinusoid microcirculation: a morphologic study in the rat. J Endocrinol. 2001;171:541–549. doi: 10.1677/joe.0.1710541. [DOI] [PubMed] [Google Scholar]
- 37.Dschietzig T, Bartsch C, Baumann G, Stangl K. RXFP1-inactive relaxin activates human glucocorticoid receptor: further investigations into the relaxin-GR pathway. Regul Pept. 2009;154:77–84. doi: 10.1016/j.regpep.2008.11.010. [DOI] [PubMed] [Google Scholar]
- 38.Mueller KM, Kornfeld JW, Friedbichler K, Blaas L, Egger G, Esterbauer H, Hasselblatt P, et al. Impairment of hepatic growth hormone and glucocorticoid receptor signaling causes steatosis and hepatocellular carcinoma in mice. Hepatology. 2011;54:1398–1409. doi: 10.1002/hep.24509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tsung A, Klune JR, Zhang X, Jeyabalan G, Cao Z, Peng X, Stolz DB, et al. HMGB1 release induced by liver ischemia involves Toll-like receptor 4 dependent reactive oxygen species production and calcium-mediated signaling. J Exp Med. 2007;204:2913–2923. doi: 10.1084/jem.20070247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ilmakunnas M, Tukiainen EM, Rouhiainen A, Rauvala H, Arola J, Nordin A, Makisalo H, et al. High mobility group box 1 protein as a marker of hepatocellular injury in human liver transplantation. Liver Transpl. 2008;14:1517–1525. doi: 10.1002/lt.21573. [DOI] [PubMed] [Google Scholar]
- 41.Kadono K, Uchida Y, Hirao H, Miyauchi T, Watanabe T, Iida T, Ueda S, et al. Thrombomodulin Attenuates Inflammatory Damage Due to Liver Ischemia and Reperfusion Injury in Mice in Toll-Like Receptor 4-Dependent Manner. Am J Transplant. 2017;17:69–80. doi: 10.1111/ajt.13991. [DOI] [PubMed] [Google Scholar]
- 42.Figueiredo KA, Mui AL, Nelson CC, Cox ME. Relaxin stimulates leukocyte adhesion and migration through a relaxin receptor LGR7-dependent mechanism. J Biol Chem. 2006;281:3030–3039. doi: 10.1074/jbc.M506665200. [DOI] [PubMed] [Google Scholar]
- 43.Horton JS, Yamamoto SY, Bryant-Greenwood GD. Relaxin modulates proinflammatory cytokine secretion from human decidual macrophages. Biol Reprod. 2011;85:788–797. doi: 10.1095/biolreprod.110.089201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gujral JS, Bucci TJ, Farhood A, Jaeschke H. Mechanism of cell death during warm hepatic ischemia-reperfusion in rats: apoptosis or necrosis? Hepatology. 2001;33:397–405. doi: 10.1053/jhep.2001.22002. [DOI] [PubMed] [Google Scholar]
- 45.Yang M, Antoine DJ, Weemhoff JL, Jenkins RE, Farhood A, Park BK, Jaeschke H. Biomarkers distinguish apoptotic and necrotic cell death during hepatic ischemia/reperfusion injury in mice. Liver Transpl. 2014;20:1372–1382. doi: 10.1002/lt.23958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lemaire C, Andreau K, Souvannavong V, Adam A. Inhibition of caspase activity induces a switch from apoptosis to necrosis. FEBS Lett. 1998;425:266–270. doi: 10.1016/s0014-5793(98)00252-x. [DOI] [PubMed] [Google Scholar]
- 47.Galluzzi L, Kroemer G. Necroptosis: a specialized pathway of programmed necrosis. Cell. 2008;135:1161–1163. doi: 10.1016/j.cell.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 48.Vandenabeele P, Vanden Berghe T, Festjens N. Caspase inhibitors promote alternative cell death pathways. Sci STKE. 2006;2006:pe44. doi: 10.1126/stke.3582006pe44. [DOI] [PubMed] [Google Scholar]
- 49.Baskin-Bey ES, Washburn K, Feng S, Oltersdorf T, Shapiro D, Huyghe M, Burgart L, et al. Clinical Trial of the Pan-Caspase Inhibitor, IDN-6556, in Human Liver Preservation Injury. Am J Transplant. 2007;7:218–225. doi: 10.1111/j.1600-6143.2006.01595.x. [DOI] [PubMed] [Google Scholar]
- 50.Yue S, Zhou H, Wang X, Busuttil RW, Kupiec-Weglinski JW, Zhai Y. Prolonged Ischemia Triggers Necrotic Depletion of Tissue-Resident Macrophages To Facilitate Inflammatory Immune Activation in Liver Ischemia Reperfusion Injury. J Immunol. 2017;198:3588–3595. doi: 10.4049/jimmunol.1601428. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.