Abstract
Little is known about the co-sleeping behaviors of school-aged children, particularly among anxious youth who commonly present for the treatment of sleep problems. The current study examined the occurrence of co-sleeping in both healthy and clinically anxious children and its associated sleep patterns. A total of 113 children (ages 6–12), 75 with primary generalized anxiety disorder and 38 healthy controls, participated along with their primary caregiver. Families completed structured diagnostic assessments, and parents reported on their child’s co-sleeping behaviors and anxiety severity. Children provided reports of anxiety severity and completed one week of wrist-based actigraphy to assess objective sleep patterns. A significantly greater proportion of anxious youth compared to healthy children co-slept, and greater anxiety severity was related to more frequent co-sleeping. Co-sleeping in anxious youth was associated with a delay in sleep timing and with greater sleep variability (i.e., more variable nightly sleep duration). All analyses controlled for child age, race/ethnicity, family income, and parental marital status. Co-sleeping is highly common in anxious school-aged children, with more than 1 in 3 found to co-sleep at least sometimes (2–4 times a week). Co-sleeping was even more common for youth with greater anxiety severity. Increased dependence on others to initiate and maintain sleep may contribute to poorer sleep in this population via shifted schedules and more variable sleep patterns.
Keywords: anxiety disorders, co-sleeping, sleep dependence, sleep variability
The term ‘co-sleeping’ is broadly used to refer to children who sleep in close proximity to parents and often includes bed sharing (sharing a sleeping surface with a family member for all or a portion of the sleep period; Goldberg and Keller 2007; McKenna and Volpe 2007). Co-sleeping/bed sharing is a controversial topic in the pediatric sleep literature, with no general consensus regarding its potential benefits or consequences (Thoman 2006). To a large extent, co-sleeping is a cultural phenomenon, widely accepted in Eastern societies that prioritize collectiveness and dependency, and less practiced in Western societies where autonomy is emphasized (Latz et al. 1999; Mileva-Seitz et al. 2017). Across nearly all cultures however, co-sleeping is most common in infancy and early childhood and declines as children enter school (BaHammam et al. 2008; Cortesi et al. 2004; Jenni et al. 2005; Li et al. 2009). Still, reported rates of co-sleeping among children in the United States vary greatly (anywhere from 5–88%), with very little understanding of the factors that influence or sleep patterns that result from this practice, particularly in school-aged children (Cortesi et al., 2004; Jenni et al., 2005; Latz et al. 1999; Mileva-Seitz et al. 2017; Welles-Nystrom, 2005).
A need to more closely examine co-sleeping behaviors in school-aged children is derived from evidence linking co-sleeping in middle to late childhood with greater levels of sleep-related difficulties and anxiety/fear (Blader et al. 1997; Cortesi et al. 2004; Liu et al. 2003; Mindell et al. 2009). For example, co-sleeping during the school-aged years has been associated with problems initiating sleep, less nighttime sleep, more daytime sleepiness, more bedtime resistance, increased nighttime awakenings, and greater levels of sleep anxiety (Blader et al. 1997; Cortesi et al. 2008; Jiang et al. 2016). Investigations of co-sleeping are especially needed among anxious children, who often experience heightened fear/arousal surrounding sleep as well as problems initiating sleep, which can prompt requests to co-sleep with parents or siblings (Alfano et al. 2007; Alfano et al. 2010; Forbes et al. 2006; Hansen et al. 2011). Children with anxiety disorders are commonly referred for problems sleeping independently (Beidel and Alfano 2011; Cowie et al. 2014) and capitulation to co-sleeping requests (i.e., as a means of preventing or reducing child distress) ranks among the most common and most interfering forms of parental accommodation among school-aged children with anxiety disorders (Thompson-Hollands et al. 2014). Paradoxically, however, investigations on the occurrence and associated outcomes of co-sleeping in clinically-anxious youth are virtually nonexistent in the literature. The aim of the current study was to fill this research gap by examining rates of co-sleeping and relationships between co-sleeping and objective sleep patterns in a sample of clinically-anxious and non-anxious school-aged children.
Co-Sleeping and Anxiety in School-Aged Children
Children’s requests to co-sleep are often reactive or occur in response to previous sleep difficulties or anxieties (Cortesi et al. 2004; Cortesi et al. 2008; Jain et al. 2011; Rath and Okum 1995; Smedje et al. 2001). For example, children who struggle to self-soothe at night have more difficulty falling asleep independently and often ‘signal’ their distress to parents (Sadeh and Anders 1993). The period leading up to sleep is particularly stressful for clinically-anxious children, who experience higher subjective levels of cognitive and physiological arousal (Alfano et al. 2010), higher cortisol levels (Forbes et al. 2006), and greater anxiety and fear (Hansen et al. 2011) during the pre-sleep period than age-matched peers. Together with difficulties regulating distress more broadly (Carthy et al. 2010; Suveg and Zeman 2004), anxious youth might be more likely to signal this distress to parents, giving rise to parental accommodation in the form of co-sleeping (Thompson-Hollands et al. 2014).
Preliminary evidence suggests co-sleeping is prevalent among school-aged children with anxiety disorders (Alfano et al. 2007; Storch et al. 2007). Among one study investigating 6–11 year-old children with various anxiety disorders, 61% of parents reported that their child commonly resisted or refused to sleep alone (Alfano et al. 2007). However, in addition to the lack of a healthy comparison group of children, the actual occurrence of co-sleeping was not the focus of this investigation, and it remains unknown whether co-sleeping in school-aged children with anxiety disorders relates to both anxiety severity and/or problematic sleep patterns.
Co-Sleeping and Child Sleep Patterns
Having a parent present during sleep onset is one of the strongest predictors of poor sleep patterns throughout childhood (Mindell et al. 2009). Although typically limited to only subjective parent-reported sleep disturbances, numerous cross-sectional studies in school-aged children find co-sleeping to be a risk factor for sleep problems. For example, co-sleeping has been related to greater night awakenings (Cortesi et al. 2004; Keller and Goldberg 2004; Mindell et al. 2009), shorter sleep duration (Cortesi et al. 2008), more bedtime resistance (Cortesi et al. 2008; Jiang et al. 2016), poor sleep quality (Jiang et al. 2016) and more daytime sleepiness (Jiang et al. 2016; Liu et al. 2003).
Conceivably, relationships between co-sleeping and sleep problems result from alterations or inconsistency in sleeping arrangements and schedules (Lozoff et al. 1984; Peterman et al. 2015). Because co-sleeping/bed sharing inherently introduces greater variability into the sleep routine and creates a dependence on the schedule of other family members, both bedtimes and awakening times may shift (Li et al. 2009). Cross-sectional research has indeed found children who share a bedroom experience greater intraindividual variability in sleep onset and offset times (Buckhalt et al. 2007), and co-sleeping children are more likely to go to bed later (Cortesi et al. 2008) and have less regular bedtimes (Hayes et al. 2001).
A host of research emphasizes organization of the sleep-wake system in healthy developmental outcomes, including the timing and regularity of sleep patterns. A greater degree of instability and irregularity has been found to predict worse behavioral and health problems (Thelen 1993; Thoman 1990). Independent of sleep quantity, inconsistent sleep schedules in children are associated with poor mental health, daytime functioning, and school performance (Becker et al. in press). Further, a shifted sleep-wake cycle (e.g., a later bedtime) in youth is related to greater emotional distress or poorer health outcomes both concurrently and later in adulthood (McGlinchey and Harvey 2015), including greater depressive symptoms (Emens et al. 2009; Short et al. 2013).
Sleep Timing and Variability among Anxious Children
Subjective reports of sleep problems among anxious youth are highly common (Alfano et al. 2007; Alfano et al. 2010). However, consistency and/or timing of sleep and their impact on daytime functioning have received far less attention among children with anxiety disorders (Alfano et al. 2007; Cowie et al. 2014; Hansen et al. 2011; Peterman et al. 2015). One study found clinically-anxious youth to go to bed significantly later than healthy controls on school nights (based on sleep diary reports; Hudson et al. 2009). The same study found significant variability in bedtimes on weekdays and weekends among both clinically-anxious and healthy youth (Hudson et al. 2009). The fact that only subjective sleep reports were used, which do not always correspond with objective measurement of sleep, particularly for clinically anxious youth, to some extent limit these findings (Alfano et al. 2015). However, variability in sleep timing is also concurrently associated with increased anxiety symptoms in healthy school-aged children (Fletcher et al. in press) and research in adolescents has linked anxiety symptoms and variability in sleep time (Fuligni and Hardway 2006) independent of mean sleep duration. Notably, none of these studies considered the potential role of co-sleeping behavior.
Current Study
The current study sought to investigate the occurrence of co-sleeping and its correlates in a school-aged sample (6–12 years old) of clinically-anxious and non-anxious children. Our first aim was to document and compare the frequency of parent-reported co-sleeping in these two groups of children, and to examine associations with anxiety severity within the clinical sample (based on parent, child, and clinician ratings). We hypothesized that anxious youth would co-sleep significantly more often than non-anxious youth, and that more frequent co-sleeping would be related to greater levels of anxiety.
Based on previous research suggesting that both increased anxiety and co-sleeping relate to greater sleep problems (Mindell et al. 2009) and to later shifts and greater variability in sleep patterns (Buckhalt et al. 2007; Doane et al. 2015; Fuligni and Hardway 2006; Hudson et al. 2009; Li et al. 2009), the second aim of our study was to examine relationships among co-sleeping and sleep patterns within a clinically-anxious sample. Building on some of the limitations of previous studies, we examined these associations using an objective sleep measure (actigraphy). Specifically, we examined relationships between co-sleeping and mean total sleep duration, night wakings (number of awakenings, time spent awake after the onset of sleep), and sleep timing (sleep onset and offset times). Additionally, we examined relationships among co-sleeping and intraindividual variability in sleep (i.e., day-to-day variability in sleep duration and sleep timing). Consistent with prior findings, we hypothesized a greater frequency of co-sleeping to be associated with more problematic sleep patterns.
Importantly, because decisions to co-sleep may be pragmatic or cultural in nature (Owens 2004), and because co-sleeping tends to decline with age (Mindell et al. 2009), all analyses controlled for age, race/ethnicity, income, and parent marital status.
Method
Participants
Participants included 113 youth ages 6–12 and a primary caregiver. Demographic characteristics are reported in Table 1. Children were diagnosed with primary generalized anxiety disorder (GAD; n = 75) or were healthy controls (n = 38). Three additional families participated, but did not complete the co-sleeping measure. These participants were not included in the current study. Children were required to be fluent in English, live with their parent/caregiver for minimum of one year prior to assessment, and be enrolled in regular education classes. Any children with a current or lifetime history of psychotic, pervasive developmental, bipolar, eating, or substance use disorder, or suicidal ideation/self-harm were excluded from participation. Other exclusion criteria included the child’s use of psychiatric medications or medications known to impact sleep, any chronic illness that could impact sleep, or current use of treatment services for anxiety or sleep problems.
Table 1.
Group Differences in Demographics and Variables of Interest
| Anxious | Control | Total Sample | Comparison Statistics | |||
|---|---|---|---|---|---|---|
|
|
||||||
| M (SD) / % (n) | M (SD) / % (n) | M (SD) / % (n) | t or X2 (df) | p | ||
| Age | 9.01 (1.70) | 8.92 (1.26) | 8.98 (1.56) | −.33 (95.77) | .75 | |
| Gender (Female) | 50.7% (38) | 52.6% (20) | 51.3% (58) | .04 (1) | .84 | |
| Race/Ethnicity | 3.00 (4) | .56 | ||||
| Caucasian | 54.7% (41) | 60.5% (23) | 56.6% (64) | |||
| African-American | 4% (3) | 5.3% (2) | 4.4% (5) | |||
| Asian | 1.3% (1) | 2.6% (1) | 1.8% (2) | |||
| Hispanic | 13.3% (10) | 18.4% (7) | 15% (17) | |||
| Other/Biracial | 26.7% (20) | 13.2% (5) | 22.1% (25) | |||
| Income | −1.58 (109) | .12 | ||||
| < $10K | N/A | 5.4% (2) | 1.8% (2) | |||
| $10–20K | 2.7% (2) | 2.6% (1) | 2.7% (3) | |||
| $20–40K | 8.1% (6) | 10.8% (4) | 9% (10) | |||
| $40–60K | 8.1% (6) | 5.4% (2) | 7.2% (8) | |||
| $60–80K | 10.8% (8) | 16.2% (6) | 12.6% (14) | |||
| $80–100K | 10.8% (8) | 16.2% (6) | 12.6% (14) | |||
| >$100K | 59.5% (44) | 43.2% (16) | 54.1% (60) | |||
| Maternal Education | −1.38 (110) | .17 | ||||
| Some grade school | 1.4% (1) | 2.6% (1) | 1.8% (2) | |||
| Completed high school | 1.4% (1) | 10.5% (4) | 4.5% (5) | |||
| Some College | 17.6% (13) | 10.5% (4) | 15.2% (17) | |||
| Completed College | 40.5% (30) | 47.4% (18) | 42.9% (48) | |||
| Advanced Degree | 39.2% (29) | 28.9% (11) | 35.7% (40) | |||
| Paternal Education | −.69 (4) | .50 | ||||
| Some grade school | 1.4% (1) | N/A | .9% (1) | |||
| Completed high school | 11% (8) | 5.6% (2) | 9.2% (10) | |||
| Some College | 17.8% (13) | 36.1% (13) | 23.9% (26) | |||
| Completed College | 34.2% (25) | 33.3% (12) | 33.9% (37) | |||
| Advanced Degree | 35.6% (26) | 25% (9) | 32% (35) | |||
| Parent Marital Status | 1.25 (1) | .26 | ||||
| Married | 81.3% (61) | 89.5% (34) | 84.1% (95) | |||
| Other (e.g., Single, Divorced) | 18.7% (14) | 10.5% (4) | 15.9% (18) | |||
| CGAS | 57.27 (6.01) | - | - | - | - | |
| SCARED-P | 31.22 (12.10) | 4.65 (3.80) | 22.70 (16.09) | −16.95 (94.82) | <.001 | |
| SCARED-C | 30.75 (14.07) | 15.19 (9.51) | 25.61 (14.67) | −6.81 (96.60) | <.001 | |
| Co-Sleeping | 8.35 (2) | .02 | ||||
| Usually | 22.7% (17) | 5.3% (2) | 16.8% (19) | |||
| Sometimes | 13.3% (10) | 5.3% (2) | 10.6% (12) | |||
| Rarely | 64% (48) | 89.5% (34) | 72.6% (82) | |||
| WEP | 17.12 (7.71) | 14.24 (8.24) | 16. 11 (7.98) | −1.81 (107) | .07 | |
| WASO (minutes) | 51.14 (26.95) | 44.38 (24.18) | 48.78 (26.11) | −1.29 (107) | .19 | |
| TST (minutes) | 499.92 (39.14) | 504.41 (44.28) | 501.49 (40.86) | .55 (107) | .59 | |
| Sleep Onset | 22:09 (1:04) | 22:02 (0:47) | 22:06 (0:59) | −.62 (107) | .54 | |
| Sleep Offset | 7:19 (0:50) | 7:10 (0:41) | 07:16 (0:47) | −.95 (107) | .35 | |
| TST SD (minutes) | 53.17 (25.98) | 45.15 (17.56) | 50.37 (23.62) | −1.69 (107) | .09 | |
| Sleep Onset SD (minutes) | 39.01 (24.65) | 38.72 (19.39) | 38.91 (22.86) | −.06 (107) | .95 | |
| Sleep Offset SD (minutes) | 42.46 (25.64) | 45.68 (19.13) | 43.58 (23.53) | .68 (107) | .50 | |
Notes. CGAS = Children's Global Assessment Scale. SCARED-P = Screen for Child Anxiety Related Disorders, Parent Report. SCARED-C = Screen for Child Anxiety Related Disorders, Child Report. WEP = Wake Episodes. WASO = Wake After Sleep Onset. TST = Total Sleep Time. TST SD = Standard Deviation of Total Sleep Time (Intraindividual Variability in Sleep Duration). Sleep Onset SD = Standard Deviation of Sleep Onset. Sleep Offset SD = Standard Deviation of Sleep Offset.
Procedures
Participants were recruited via flyers, local publications, mailings to school counselors/nurses and pediatrician offices, and at local community events from both the Washington, D.C. (n = 42) and Houston, TX (n = 71) metropolitan regions. Each child and their parent participated in one of two studies conducted by the authors: 1) a research study on “behavior and emotion” which included a group of children with generalized anxiety disorder (n = 44) and the healthy control group (n = 38); and 2) a study offering behavioral treatment for anxious children (n = 31).1 Advertisements for the former research study targeted both healthy children and children who “worry too much.” Advertisements for the latter treatment study targeted families who were “looking for help with their anxious child.” The protocols were approved by an Institutional Review Board at both locations. Parents and children were first consented/assented and were given the opportunity to ask any questions prior to participation. All participants underwent an initial assessment that included a set of child and parent questionnaires and a structured clinical interview. Parents reported on demographic information, their child’s sleep habits, and their child’s anxiety severity. Children also reported on their anxiety severity. Following this initial appointment, children completed one week of sleep monitoring using a wrist actigraph (and completion of a sleep diary). During this week, children were instructed to follow their normal sleep routines. Participants from the research study about “behavior and emotion” were paid $160. Participants from the treatment study were offered 16 weeks of free behavioral treatment after the initial assessment period.
Measurement
Clinical Interview
Parents and children participated in separate clinical interviews to determine diagnostic status using the Anxiety Disorders Interview Schedule for the DSM-IV for Children and Parents (ADIS-C/P; Silverman and Albano 1996), which is considered the gold standard for diagnosing child anxiety disorders (Lyneham et al. 2007; Silverman et al. 2001) and assesses symptoms across a range of anxiety, mood, and externalizing disorders. All interviews followed procedures outlined in the ADIS-C/P Clinician Manual (Albano and Silverman 1996). Children and parents were interviewed separately and clinical information and severity ratings were derived from both reporters. As is often the case among anxious youth, children and parents were often discrepant in their severity ratings for a GAD diagnosis (ICC = .02), which were reconciled using established procedural guidelines in the ADIS-C/P manual (pp. 11–14). Clinician severity ratings (range = 0–8), which integrate information provided by children and parents, were used to determine severity of each disorder, with ratings of 4 or above signifying clinically-significant impairment. Mean clinician severity ratings for children with GAD ranged from 4–8 (M = 6.15, SD = 1.14). All interviews were conducted by trained doctoral graduate students and post-doctoral fellows and were reviewed with a licensed clinical psychologist prior to assigning final diagnoses. Interviews were video-recorded and 25% were randomly selected for independent ratings by a Ph.D. level student in clinical psychology to determine reliability. Interrater reliability for the presence or absence of a GAD diagnosis was excellent for both the research study and the treatment study (kappas = 1.0 and .81, respectively). ADIS-C/P interviews were also used to extract a rating of global functioning for each child using the Children’s Global Assessment Scale (CGAS), ranging from 0–100 (extremely impaired to doing very well). Some anxious children also met criteria for comorbid diagnoses, including separation anxiety disorder (n = 13), social anxiety disorder (n = 26), ADHD (n = 7), ODD (n = 2), specific phobia (n = 10), panic disorder (n = 1), depressive disorder NOS (n = 3), and tic disorder (n = 1).
Demographics
Parents completed demographic questions regarding their marital status, income, and education, along with their child’s race/ethnicity, age, and gender.
Co-Sleeping
Parents completed the Children’s Sleep Habits Questionnaire (CSHQ; Owens et al. 2000). Parents reported on how often their child experienced a range of different sleep problems. Reliability for overall reports of sleep disturbances in the current study (a total score including all sleep problems assessed) was good (α = .84). Co-sleeping was assessed by the question, “How often does your child fall asleep in a parent’s or sibling’s bed?” Parents responded by answering on a 3-point scale indicating whether their child co-sleeps: 1 (rarely; 0–1 time a week), 2 (sometimes; 2–4 times a week), or 3 (usually; 5 or more times a week).
Anxiety Severity
Parents reported on their child’s anxiety severity using the Screen for Child Anxiety Related Disorders: Parent Version (SCARED-P; Birmaher et al. 1999). Children reported on their anxiety severity using the child version of this measure (SCARED-C) which mirrors the items on the SCARED-P. The SCARED consists of 41 questions assessing symptoms of panic, GAD, separation anxiety, social phobia, and school phobia based on DSM-IV classifications. Participants report how true each item has been over the past 3 months. Items are measured on a 3-point Likert scale from 0 (not true or hardly every true) to 2 (very true or often true). Ratings were summed to create a SCARED-P total score (α = .95) and a SCARED-C total score (α = .93), with higher scores indicating greater anxiety.
Objective Sleep Patterns
Sleep variables were measured using Micro MotionLogger Actigraph Sleep Watches (Ambulatory Monitoring, Inc., Ardsley, NY), an accelerometer-based wrist-worn device that monitors sleep via activity and movement over the course of one week. Data was collected and stored in one minute epochs, and was visually inspected to omit epochs where the watch was not worn. Data was scored using the zero crossing mode and the Sadeh algorithm (Sadeh et al. 1994), which is commonly used in pediatric sleep research (Meltzer et al. 2012). Participants were instructed to push an event marking button on the watch to indicate when they got into bed at night and when they got out of bed in the morning, which was used to calculate the time spent in bed. Families also completed a sleep diary which provided a validation check for actigraphy and is considered necessary to accurately confirm sleep-wake times, identify artifacts, and to clarify any irregularities in the objective data (Meltzer et al. 2012).
Sleep duration was calculated as the mean number of minutes spent asleep each night during the actigraphy week. Number of awakenings was calculated as the average number of blocks of contiguous wake epochs each night, and wake after sleep onset was calculated as the average number of minutes spent awake after the onset of sleep each night. Averages were also calculated for the sleep onset time and sleep offset time across the actigraphy week. Finally, variability in sleep duration was calculated as the standard deviation of total sleep time across the week in minutes for each participant, and variability in sleep timing was calculated using the standard deviation of sleep onset times and the standard deviation of sleep offset times across the week for each participant. The standard deviation is commonly used for quantifying intraindividual variability in sleep-wake patterns in children and adolescents (Becker et al. in press). Three children did not complete the actigraphy week, and one child was missing 4 nights of data. Based on recommendations that a minimum of five nights of actigraphy are necessary to obtain reliable measures of sleep in children and adolescents (Acebo et al. 1999), these participants were excluded from all analyses using actigraphy.
Analysis Plan
All analyses were conducted using SPSS version 24. Preliminary analyses were conducted to examine bivariate relationships among variables and to test for group differences in demographic, sleep, and anxiety variables. To examine rates of co-sleeping among both groups, a chi-square analysis of reported co-sleeping (i.e., rarely, sometimes, or usually) was conducted, followed by an ANCOVA to determine whether group was related to co-sleeping frequency while controlling for covariates. To examine how anxiety severity was related to co-sleeping, we ran a regression model with co-sleeping as the dependent variable, and parent-reported anxiety symptoms, child-reported anxiety symptoms, and clinician-rated global functioning as independent predictors. To examine the role of co-sleeping in predicting sleep patterns among clinically-anxious youth, we ran a series of regression analyses with co-sleeping as an independent variable, and each sleep outcome as the dependent variable while controlling for covariates.
Results
Preliminary Analyses
Descriptive statistics for each group for are reported in Table 1 and bivariate correlations are reported in Table 2. Anxious children experienced greater parent- and child-reported anxiety, and marginally greater wake episodes and intraindividual variability in sleep duration. There were no other differences between groups in terms of demographic characteristics or variables of interest. Older children had lower CGAS scores, and greater self-reported anxiety. Older children also had a shorter sleep duration and a later sleep onset time. Caucasian children experienced more wake episodes, and earlier and less variable sleep onset and offset times. Parents with higher income and who were married reported lower rates of co-sleeping and less intraindividual variability in sleep offset time. Higher income was also related to less intraindividual variability in total sleep duration and greater wake episodes. Greater parent-reported anxiety was related to later sleep offset times and greater variability in total sleep duration, and child-reported anxiety was related with greater variability in sleep duration.
Table 2.
Bivariate Correlations among Variables of Interest for all Participants
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age | |||||||||||||||
| 2. Race/Ethnicity | .03 | ||||||||||||||
| 3. Income | .02 | .33*** | |||||||||||||
| 4. Marital Status | −.05 | .21* | .36*** | ||||||||||||
| 5. Co-Sleeping | .06 | −.10 | −.21* | −.25** | |||||||||||
| 6. CGAS | −.28* | .11 | .12 | .10 | −.13 | ||||||||||
| 7. SCARED-P | .05 | −.07 | .02 | −.16 | .47*** | −.43*** | |||||||||
| 8. SCARED-C | .20* | −.03 | −.04 | −.07 | .28** | −.36** | .41*** | ||||||||
| 9. WEP | −.08 | .23* | .28* | .09 | −.09 | .05 | .10 | −.06 | |||||||
| 10. WASO | −.11 | .15 | .16 | .10 | −.07 | .08 | .08 | −.13 | .86** | ||||||
| 11. TST | −.34*** | .11 | .05 | −.05 | −.09 | .06 | −.06 | −.05 | −.06 | −.18 | |||||
| 12. Sleep Onset | .31** | −.19* | −.15 | −.01 | .33*** | −.17 | .17 | .16 | −.29** | −.31** | −.48*** | ||||
| 13. Sleep Offset | .02 | −.05 | −.07 | .01 | .30** | −.13 | .21* | .07 | .08 | .02 | .15 | .68*** | |||
| 14. TST SD | −.04 | −.11 | −.21* | −.14 | .35*** | −.08 | .28* | .26** | −.05 | −.09 | −.05 | .22* | .18 | ||
| 15. Sleep Onset SD | .17 | −.25** | −.18 | −.12 | .09 | −.16 | −.01 | .10 | −.18 | −.11 | −.17 | .37*** | −.08 | −.08 | |
| 16. Sleep Offset SD | .10 | −.28** | −.27** | −.24* | .23* | −.04 | .04 | .09 | −.21* | −.19 | −.19* | .53*** | .14 | .14 | .49*** |
Notes.
p < .001,
p < .01,
p < .05.
CGAS = Children’s Global Assessment Scale (reported for the anxious group only). SCARED-P = Screen for Child Anxiety Related Disorders, Parent Report. SCARED-C = Screen for Child Anxiety Related Disorders, Child Report. WEP = Wake Episodes. WASO = Wake After Sleep Onset. TST = Total Sleep Time. TST SD = Standard Deviation of Total Sleep Time (Intraindividual Variability in Sleep Duration). Sleep Onset SD = Standard Deviation of Sleep Onset. Sleep Offset SD = Standard Deviation of Sleep Offset. Co-Sleeping is coded as 1 = usually, 0 = rarely or sometimes. Race/ethnicity is dummy coded as 1 = white/Caucasian, 0 = other. Marital status is dummy coded as 1 = married, 0 = other. All CGAS correlations are presented for the anxious group only.
Aim 1: Co-Sleeping in Clinically-Anxious and Healthy Children
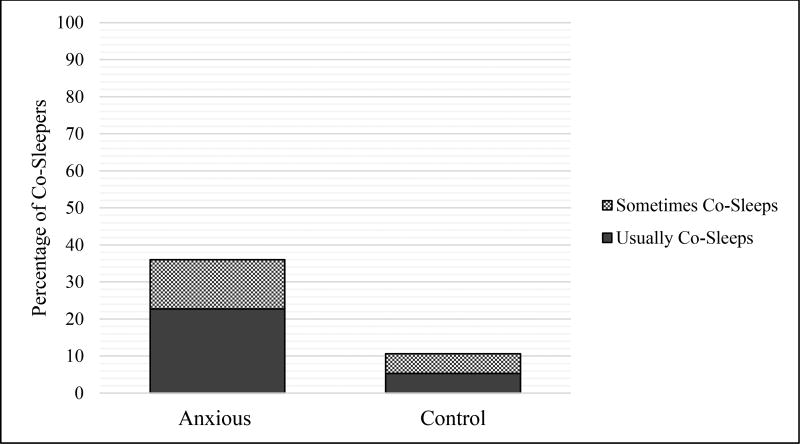
A chi-square analysis indicated that anxious children co-slept more often than healthy controls (Cramer’s V = .27). Parents of anxious children were significantly more likely to report that their child usually or sometimes co-slept compared to healthy controls. These results are displayed in Table 1 and Figure 1. After controlling for age, income, child race/ethnicity, and parent marital status, findings were similar, with anxious children co-sleeping more often than healthy controls, F(1, 105) = 9.26, p = .003, 95% CI [−.76, −.16], partial η2 = .08.
Figure 1.
Frequency of co-sleeping in anxious and healthy school-aged children.
To examine whether severity of anxiety pathology (assessed via parent-reported anxiety symptoms, child-reported anxiety symptoms, and clinician-rated global functioning ratings) predicted co-sleeping in the anxious group specifically, we ran a series of hierarchical regression analyses using age, income, child race/ethnicity, and parent marital status as covariates. Greater frequency of co-sleeping was significantly predicted by parent-reported anxiety severity and by child-reported anxiety severity, but not by clinician-rated global functioning. See Table 3.
Table 3.
Anxiety Severity Predicting Co-Sleeping in Anxious Children
| Co-Sleeping | |||||
|---|---|---|---|---|---|
|
|
|||||
| Adj. R2 | β | b | SE | 95% CI | |
| .14* | |||||
| Age | −.02 | −.01 | .06 | −.13, .11 | |
| Race/Ethnicity | .01 | .01 | .21 | −.40, .42 | |
| Income | −.17 | −10 | .07 | −.24, .05 | |
| Parent Marital Status | −.08 | −.18 | .26 | −.70, .35 | |
| SCARED-P | .37** | .03 | .01 | .01, .04 | |
| SCARED-C | .21+ | .01 | .01 | −.002, .03 | |
| CGAS | .09 | .01 | .02 | −.03, .06 | |
Notes.
p < .01,
p < .05,
p < .10.
Standardized and unstandardized and standardized estimates are reported.
CGAS = Children’s Global Assessment Scale. SCARED-P = Screen for Child Anxiety Related Disorders, Parent Report. SCARED-C = Screen for Child Anxiety Related Disorders, Child Report. Race/ethnicity is dummy coded as 1 = white/Caucasian, 0 = other. Marital status is dummy coded as 1 = married, 0 = other.
Aim 2: Co-Sleeping and Objective Sleep Patterns in Anxious Youth
To examine relationships between co-sleeping and objective sleep parameters, a series of hierarchical regression models were conducted with co-sleeping as the independent variable (and age, income, child race/ethnicity, and parent marital status as covariates). Only clinically-anxious children were included in the models given the low overall incidence of co-sleeping behavior among controls. Clock time variables (i.e., sleep onset and offset times) were converted to minutes and centered around the sample mean to aid in the interpretability of regression coefficients. When examining mean levels of sleep disturbances during the actigraphy week, co-sleeping was not related to the number of awakenings, wake after sleep onset, or to total sleep time (see Table 3). However, greater co-sleeping was related to mean levels of sleep timing, including later sleep onset times and later sleep offset times (see Table 4). When examining intraindividual variability across the week, co-sleeping was associated with greater variability in the total sleep time, but not to variability in sleep timing. These results are displayed in Table 5.
Table 4.
Co-Sleeping Predicting Average Objective Sleep Parameters in Anxious Children
| WEP | WASO | TST | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||||
| β | b | SE | 95% CI | β | b | SE | 95% CI | β | b | SE | 95% CI | |
| Age | −.19 | −.89 | .53 | −1.95, .18 | −.24* | −3.94 | 1.89 | −7.70, −.17 | −.36** | −8.52 | 2.66 | −13.82, −3.31 |
| Race/Ethnicity | .06 | .86 | 1.83 | −2.81, 4.53 | .01 | .67 | 6.45 | −12.29, 13.64 | .20 | 15.46 | 9.14 | −2.80, 33.72 |
| Income | .26 | 1.36 | .74 | −.12, 2.83 | .09 | 1.57 | 2.61 | −3.64, 6.78 | .09 | 2.38 | 3.68 | −4.97, 9.72 |
| Parent Marital Status | .11 | 2.17 | 2.54 | −2.90, 7.25 | .17 | 11.71 | 8.97 | −6.20, 29.62 | −.30* | −30.58 | 12.63 | −55.81, −5.35 |
| Co-Sleeping | −.08 | −.73 | 1.13 | −2.99, 1.54 | −.15 | −4.70 | 4.00 | −12.70, 3.29 | −.01 | −.32 | 5.67 | −11.58, 10.93 |
| Adj. R2 | .12* | .10* | .16** | |||||||||
Notes.
p < .01,
p < .05.
Standardized and unstandardized estimates are reported.
WEP = Wake Episodes. WASO = Wake After Sleep Onset. TST = Total Sleep Time. Race/ethnicity is dummy coded as 1 = white/Caucasian, 0 = other. Marital status is dummy coded as 1 = married, 0 = other.
Table 5.
Co-Sleeping Predicting Average Objective Sleep Timing in Anxious Children
| Sleep Onset Time | Sleep Offset Time | |||||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| β | b | SE | 95% CI | β | b | SE | 95% CI | |
| Age | .27* | 10.64 | 4.14 | 2.37, 19.90 | −.08 | −2.34 | 3.53 | −9.38, 4.70 |
| Race/Ethnicity | −.17 | −21.35 | 14.24 | −49.80, 7.10 | −.05 | −5.33 | 12.13 | −29.56, 18.91 |
| Income | −.28* | −12.34 | 5.73 | −23.78, −.91 | −.24 | −8.37 | 4.88 | −18.11, 1.37 |
| Parent Marital Status | .25* | 41.21 | 19.68 | 1.90, 80.52 | .19 | 24.44 | 16.76 | −9.04, 57.92 |
| Co-Sleeping | .28* | 21.64 | 8.78 | 4.10, 39.18 | .30* | 17.89 | 7.48 | 2.95, 32.83 |
| Adj. R2 | .25*** | .12* | ||||||
Notes.
p < .001,
p < .05.
Standardized and unstandardized estimates are reported.
Race/ethnicity is dummy coded as 1 = white/Caucasian, 0 = other. Marital status is dummy coded as 1 = married, 0 = other.
Discussion
The current study fills gaps in the limited body of research examining the presence and associated sleep patterns of co-sleeping in anxious school-aged children. Building on research showing anxious youth often struggle with sleep problems, we investigated the frequency of co-sleeping in both healthy and clinically anxious school-aged children and relationships between co-sleeping and anxiety severity using multiple reporters. We also examined sleep-related correlates of co-sleeping in this anxious sample using objective (i.e., actigraphy-based) sleep assessments. As expected, we found anxious children to co-sleep significantly more than healthy children, with more than 1 in 3 anxious children co-sleeping usually or sometimes. Importantly, co-sleeping was even more common among youth with greater anxiety severity. The high rates reported in this sample are remarkable given the relative lack of co-sleeping research in this population. Importantly, co-sleeping was also related to more problematic sleep patterns in anxious youth (i.e., greater intraindividual variability in sleep duration and shifted bed and wake times). Overall, this study provides novel information regarding the occurrence of co-sleeping in school-aged anxious youth, and suggests that frequent co-sleeping may be one factor associated with sleep problems in this population. Problematic sleep-onset associations may be a malleable treatment target for school-aged children (Paine and Gradisar 2011), and thus these findings might be used to inform intervention and prevention efforts.
Our finding that over one third of anxious children sleep in a parent or sibling’s bed (at least a couple of times a week) is in line with high rates of bedtime resistance and refusal to sleep alone found in other studies (Alfano et al. 2007). Further, among anxious youth, co-sleeping was linked with more severe forms of anxiety (based on both parent and child reports), fitting the view that co-sleeping is reactionary in response to heightened fear and arousal surrounding sleep (Alfano et al. 2010; Forbes et al. 2006; Hansen et al. 2011). Although we did not directly assess family preferences for sleeping arrangements, overall rates of sleep complaints among anxious youth and their parents (Alfano et al. 2007; Alfano et al. 2010) along with the frequency with which co-sleeping is identified by parents as a specific goal of treatment (Paine and Gradisar 2011), suggests that co-sleeping is often reactive in this population. Generally, co-sleeping declines as children enter the school-aged years (BaHammam et al. 2008; Cortesi et al. 2004; Jenni et al. 2005; Li et al. 2009). In school-aged children with anxiety disorders however, persistent nighttime fears and problems initiating sleep may give rise to parental accommodation in the form of co-sleeping (Thompson-Hollands et al. 2014).
Precise mechanisms of sleep disturbances among anxious individuals are largely unknown; however, our study identified co-sleeping as a potentially important yet unexplored correlate of sleep problems among clinically-anxious youth. It is important to note, however, that we did not find significant differences in actigraphy-measured sleep indicators between healthy and anxious children (with the exception of a marginal difference in wake episodes and variability in total sleep duration). This is in line with many studies investigating sleep in anxious youth, which often find high rates of subjectively reported sleep problems, but fail to find differences compared to healthy youth using objective methodology (McMakin and Alfano 2016). However, our findings suggest that objectively measured sleep disruptions may be greatest among the subset of anxious youth who frequently co-sleep. These findings are not surprising given prior research linking co-sleeping in healthy school-aged youth to a range of sleep difficulties.
In particular, we found that anxious youth who co-slept more often were also more likely to experience a greater shift in their sleep timing (i.e., later sleep onset and offset times). Children with anxiety often resist going to bed (Alfano et al. 2010), which can create stress for both parents and children, prolong bedtime routines (Meltzer 2010), and culminate in parents allowing children to co-sleep. Paradoxically, children who avoid nighttime anxiety by co-sleeping may disrupt their sleep even more via shifting their bedtime later in order to coincide with parents’ bedtime. A shift in sleep timing during the school-aged years may contribute to and potentially exacerbate the reliable, biologically-based circadian delay that occurs with the onset of puberty (Burgess and Eastman 2004; Carskadon et al. 1993). As a later circadian phase in adolescence is associated with greater emotional distress and depressive symptoms (McGlinchey and Harvey 2015; Short et al. 2013), identifying these problematic patterns early, when they may be more malleable (Takeuchi et al. 2001), seems critical.
In addition, although we did not find relationships with overall sleep duration, we did find that co-sleeping was related to greater intraindividual variability in sleep duration among anxious children. Few studies have considered the impact of co-sleeping on the consistency of children’s sleep. It is possible that the later bedtimes that we observed among our co-sleeping anxious youth resulted in less sleep throughout the week, necessitating longer “catch up” sleep periods on weekends and greater variability in sleep duration from weekdays to weekends. Across ages, less consistency of sleep-wake patterns corresponds with more behavioral, academic, and health-related problems (Becker et al. in press; Thoman 1990; Wolfson and Carskadon 1998), which can in turn maintain anxiety symptoms over time. Children with attention deficit/hyperactivity disorder (ADHD), for example, exhibit more variable sleep-wake patterns than healthy children (Gruber et al. 2000). As both ADHD and anxiety can be viewed as disorders of arousal regulation (Brown and McMullen 2001), greater night-to-night sleep variability could be an antecedent as much as a consequence of these conditions. Indeed, sleep rhythmicity (i.e., regularity of sleep schedules) in early childhood has been shown to precede the onset of anxiety disorders in adolescence (Ong et al. 2006). Thus, a focus on sleep variability, in addition to total sleep duration, should be a focus of behavioral sleep interventions for children, particularly those with elevated levels of anxiety.
Limitations and Future Directions
Despite their important clinical implications, our findings are not without limitations. First, although we used an objective measure of sleep and multiple reporters of anxiety severity, our co-sleeping assessment only captured bed sharing with a parent or sibling. Further, we only assessed parental retrospective report of co-sleeping, which may not have accurately reflected how often children co-slept during the actigraphy week. Future research should therefore more comprehensively assess co-sleeping. Importantly, a subset of our anxious participants were treatment-seeking, and prior research suggests that anxious youth receiving treatment are more impaired than anxious youths who participate in non-treatment-related research (De Los Reyes et al. 2017). Thus, findings require replication in a clinic-based sample of anxious youth, especially considering some of our main variables of interest (e.g., reports of anxiety severity, sleep variability) differed between the two samples.1 Varying compensation across our two samples should also be noted (i.e., research-seeking families were provided with monetary compensation while treatment-seeking families received free treatment). Finally, although our models examined anxiety as a predictor of co-sleeping and co-sleeping as a predictor of sleep-wake patterns, the cross-sectional nature of these data preclude our ability to determine directionality. Given bidirectional relationships between sleep problems and anxiety symptoms (McMakin and Alfano 2016), as well as co-sleeping and sleep-related difficulties (Mileva-Seitz et al. 2017), it is possible that the sleep problems in our anxious youth may have preceded their co-sleeping. Longitudinal research can provide more information on the directional nature of these relationships.
Conclusions
In sum, the current research provides evidence that co-sleeping is common in clinically-anxious school-aged youth and corresponds with more severe forms of anxiety. Building on research revealing a majority of children with anxiety disorders experience sleep-related problems, these findings suggest that frequent co-sleeping in this population may be one factor that disrupts healthy sleep patterns. At the same time, we urge clinicians as well as researchers to broaden conceptualizations of problematic sleep to include the timing of when sleep occurs and the night-to-night inconsistency of sleep schedules. The use of a one-time report of a child’s bed/wake times and/or total sleep duration ignores the wealth of evidence linking inconsistent sleep patterns with deleterious child outcomes. Moreover, based on the reciprocal relationship shared by anxiety and sleep, frequent co-sleeping might serve as a risk and/or maintaining factor of anxiety pathology vis-à-vis disrupted sleep practices. In such cases, co-sleeping should be considered a target for intervention.
Table 6.
Co-Sleeping Predicting Objective Intraindividual Variability in Sleep Duration and Timing in Anxious Children
| TST SD | Sleep Onset SD | Sleep Offset SD | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||||
| β | b | SE | 95% CI | β | b | SE | 95% CI | β | b | SE | 95% CI | |
| Age | −.04 | −.55 | 1.70 | −3.94, 2.84 | .22 | 3.31 | 1.79 | −.28, 6.89 | .03 | .51 | 1.78 | −3.04, 4.07 |
| Race/Ethnicity | −.04 | −2.11 | 6.04 | −14.18, 9.96 | −.19 | −9.15 | 6.17 | −21.48, 3.17 | −.14 | −7.18 | 6.12 | −19.42, 5.05 |
| Income | −.35** | −6.05 | 2.28 | −10.61, −1.48 | −.13 | −2.24 | 2.48 | 7.20, 2.72 | −.16 | −2.67 | 2.46 | −7.59, 2.25 |
| Parent Marital Status | .07 | 4.76 | 8.19 | −11.59, 21.12 | .02 | 1.15 | 8.52 | −15.88, 18.19 | −.14 | −9.19 | 8.46 | −26.10, 7.72 |
| Co-Sleeping | .29* | 8.91 | 3.56 | 1.76, 16.05 | −.04 | 1.22 | 3.81 | −8.82, 6.38 | .14 | 4.31 | 3.78 | −3.23, 11.86 |
| Adj. R2 | .19** | .03 | .09* | |||||||||
Notes.
p < .01,
p < .05.
TST SD = Standard Deviation of Total Sleep Time (Intraindividual Variability in Sleep Duration). Sleep Onset SD = Standard Deviation of Sleep Onset. Sleep Offset SD = Standard Deviation of Sleep Offset. Race/ethnicity is dummy coded as 1 = white/Caucasian, 0 = other. Marital status is dummy coded as 1 = married, 0 = other.
Acknowledgments
This project was funded by grant K23MH081188 from the National Institute of Mental Health (PI: C. Alfano), University of Houston Small Grants Program (Co-PIs: C. Alfano & M. Clementi), and Texas Psychological Foundation Graduate Research Proposal Grant (PI: M. Clementi).
Footnotes
There were several significant differences between the research-seeking and treatment-seeking samples on variables of interest. The research-seeking sample had greater CGAS scores compared to the treatment-seeking sample [t(73) = 3.34, p = .001; Mresearch = 59.09, SDresearch = 5.93, Mtreatment = 54.68, SDtreatment = 5.18]. The treatment-seeking sample had greater parent-reported SCARED scores [t(70) = −2.29, p = .025; Mresearch = 28.46, SDresearch = 12.37, Mtreatment = 34.87, SDtreatment = 10.87], child-reported SCARED scores [t(71) = −2.45, p = .017; Mresearch = 27.40, SDresearch = 13.37, Mtreatment = 35.29, SDtreatment = 13.91], and variability in total sleep duration [t(33.37) = −4.36, p < .001; Mresearch = 42.75, SDresearch = 16.07, Mtreatment = 70.85, SDtreatment = 30.48]. Participants in the treatment-seeking sample also had a later average sleep onset time [t(34.52) = −2.13, p = .041; Mresearch = 21:55, SDresearch = 0:43, Mtreatment = 22:32, SDtreatment = 1:25]. Importantly, the significance and direction of all findings generally remained the same when accounting for the study as a covariate, with the exception of the relationship between co-sleeping and variability in total sleep duration, which dropped to marginal in the regression model (p = .06). Although the small sample of anxious children in each study limit our ability to draw firm conclusions based on these findings, these results generally suggest that the treatment-seeking sample presented with more severe symptoms than the research-seeking sample.
References
- Acebo C, Sadeh A, Seifer R, Tzischinsky O, Wolfson AR, Hafer A, Carskadon M. Estimating sleep patterns with activity monitoring in children and adolescents: How many nights are necessary for reliable measures? Sleep. 1999;22:95–103. doi: 10.1093/sleep/22.1.95. [DOI] [PubMed] [Google Scholar]
- Albano AM, Silverman WK. The Anxiety Disorders Interview Schedule for Children for DSM-IV: Clinician Manual (Child and Parent Versions) Psychological Corporation; San Antonio, TX: 1996. [Google Scholar]
- Alfano CA, Ginsburg GS, Kingery JN. Sleep-related problems among children and adolescents with anxiety disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46:224–232. doi: 10.1097/01.chi.0000242233.06011.8e. [DOI] [PubMed] [Google Scholar]
- Alfano CA, Patriquin MA, De Los Reyes A. Subjective – objective sleep comparisons and discrepancies among clinically-anxious and healthy children. Journal of Abnormal Child Psychology. 2015;43:1343–1353. doi: 10.1007/s10802-015-0018-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alfano CA, Pina AA, Zerr AA, Villalta IK. Pre-sleep arousal and sleep problems of anxiety-disordered youth. Child Psychiatry and Human Development. 2010;41:156–167. doi: 10.1007/s10578-009-0158-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BaHammam A, Alameri H, Hersi A. Cosleeping and its correlates in Saudi school-aged children. International Journal of Behavioral Medicine. 2008;15:336–340. doi: 10.1080/10705500802365623. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Brent DA, Chiappetta L, Bridge J, Monga S, Baugher M. Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED): A replication study. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38:1230–1236. doi: 10.1097/00004583-199910000-00011. [DOI] [PubMed] [Google Scholar]
- Becker SP, Sidol CA, Van Dyk TR, Epstein JN, Beebe DW. Intraindividual variability of sleep/wake patterns in relation to child and adolescent functioning: A systematic review. Sleep Medicine Reviews. doi: 10.1016/j.smrv.2016.07.004. (in press). Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beidel DC, Alfano CA. Childhood Anxiety Disorders: A Guide to Research and Treatment. 2. New York, NY: Taylor & Francis/Routledge Mental Health; 2011. [Google Scholar]
- Blader JC, Koplewicz HS, Abikoff H, Foley C. Sleep problems of elementary school children. A community survey. Archives of Pediatrics and Adolescent Medicine. 1997;151:473–480. doi: 10.1001/archpedi.1997.02170420043007. [DOI] [PubMed] [Google Scholar]
- Brown TE, McMullen WJ., Jr Attention deficit disorders and sleep/arousal disturbance. Annals of the New York Academy of Sciences. 2001;931:271–286. doi: 10.1111/j.1749-6632.2001.tb05784.x. [DOI] [PubMed] [Google Scholar]
- Buckhalt JA, El-Sheikh M, Keller P. Children’s sleep and cognitive functioning: race and socioeconomic status as moderators of effects. Child Development. 2007;78:213–231. doi: 10.1111/j.1467-8624.2007.00993.x. [DOI] [PubMed] [Google Scholar]
- Burgess HJ, Eastman CI. Early versus late betimes phase shift the human dim light melatonin rhythm despite a fixed morning lights on time. Neuroscience Letters. 2004;356:115–118. doi: 10.1016/j.neulet.2003.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carskadon MA, Viera C, Acebo C. Association between puberty and delayed phase preference. Sleep. 1993;16:258–262. doi: 10.1093/sleep/16.3.258. [DOI] [PubMed] [Google Scholar]
- Carthy T, Horesh N, Apter A, Edge MD, Gross JJ. Emotional reactivity and cognitive regulation in anxious children. Behaviour Research and Therapy. 2010;48:384–393. doi: 10.1016/j.brat.2009.12.013. [DOI] [PubMed] [Google Scholar]
- Cortesi F, Giannotti F, Sebastiani T, Vagnoni C. Cosleeping and sleep behavior in Italian school-aged children. Journal of Developmental and Behavioral Pediatrics. 2004;25:28–33. doi: 10.1097/00004703-200402000-00005. [DOI] [PubMed] [Google Scholar]
- Cortesi F, Giannotti F, Sebastiani T, Vagnoni C, Marioni P. Cosleeping versus solitary sleeping in children with bedtime problems: Child emotional problems and parental distress. Behavioral Sleep Medicine. 2008;2:89–105. doi: 10.1080/15402000801952922. [DOI] [PubMed] [Google Scholar]
- Cowie J, Alfano CA, Patriquin MA, Reynolds KC, Talavera D, Clementi MA. Addressing sleep in children with anxiety disorders. Sleep Medicine Clinics. 2014;9:137–148. [Google Scholar]
- De Los Reyes A, Alfano CA, Clementi MA, Viana A. Are the clinical characteristics of anxious youths participating in non-treatment-related research comparable to those of youths receiving treatment? Child Youth Car Forum. 2017;46:1–17. [Google Scholar]
- Doane LD, Gress-Smith JL, Breitenstein RS. Multi-method assessments of sleep over the transition to college and the associations with depression and anxiety symptoms. Journal of Youth and Adolescence. 2015;44:389–404. doi: 10.1007/s10964-014-0150-7. [DOI] [PubMed] [Google Scholar]
- Emens J, Lewy A, Kinzie JM, Arntz D, Rough J. Circadian misalignment in major depressive disorder. Psychiatry Research. 2009;168:259–261. doi: 10.1016/j.psychres.2009.04.009. [DOI] [PubMed] [Google Scholar]
- Fletcher FE, Conduit R, Foster-Owens MD, Rinehart NJ, Rajaratnam SMW, Cornish KM. The association between anxiety symptoms and sleep in school-aged children: a combined insight from the Children’s Sleep Habits Questionnaire and actigraphy. Behavioral Sleep Medicine. doi: 10.1080/15402002.2016.1180522. (in press). Online ahead of print. [DOI] [PubMed] [Google Scholar]
- Forbes EE, Williamson DE, Ryan ND, Birmaher B, Axelson DA, Dahl RE. Peri-sleep-onset cortisol levels in children and adolescents with affective disorders. Biological Psychiatry. 2006;59:24–30. doi: 10.1016/j.biopsych.2005.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuligni AJ, Hardway C. Daily variation in adolescents’ sleep, activities, and psychological well-being. Journal of Research on Adolescence. 2006;16:353–378. [Google Scholar]
- Gruber R, Sadeh A, Rviv A. Instability of sleep patterns in children with attention-deficit/hyperactivity disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;38:495–501. doi: 10.1097/00004583-200004000-00019. [DOI] [PubMed] [Google Scholar]
- Goldberg WA, Keller MA. Parent-infant co-sleeping: why the interest and concern? Infant and Child Development. 2007;16:331–339. [Google Scholar]
- Hansen BH, Skirbekk B, Oerbeck B, Richter J, Kristensen H. Comparison of sleep problems in children with anxiety and attention deficit/hyperactivity disorders. European Child and Adolescent Psychiatry. 2011;20:321–330. doi: 10.1007/s00787-011-0179-z. [DOI] [PubMed] [Google Scholar]
- Hayes MJ, Parker KG, Sallinen B, Davare AA. Bed sharing, temperament, and sleep disturbance in early childhood. Sleep. 2001;24:657–662. doi: 10.1093/sleep/24.6.657. [DOI] [PubMed] [Google Scholar]
- Hudson JL, Gradisar M, Gamble A, Schniering CA, Rebelo I. The sleep patterns and problems of clinically anxious children. Behaviour Research and Therapy. 2009;47:339–344. doi: 10.1016/j.brat.2009.01.006. [DOI] [PubMed] [Google Scholar]
- Jain S, Romack R, Jain R. Bed sharing in school-age children-clinical and social implications. Journal of Child and Adolescent Psychiatric Nursing. 2011;24:185–189. doi: 10.1111/j.1744-6171.2011.00293.x. [DOI] [PubMed] [Google Scholar]
- Jenni OG, Fuhrer HZ, Iglowstein I, Molinari L, Largo RH. A longitudinal study of bed sharing and sleep problems among Swiss children in the first 10 years of life. Pediatrics. 2005;115:233–240. doi: 10.1542/peds.2004-0815E. [DOI] [PubMed] [Google Scholar]
- Jiang Y, Chen W, Spruyt K, Sun W, Wang Y, Li S, Shen X, Wang G, Jiang F. Bed-sharing and related factors in early adolescents. Sleep Medicine. 2016;17:75–80. doi: 10.1016/j.sleep.2015.08.022. [DOI] [PubMed] [Google Scholar]
- Keller MA, Goldberg WA. Co-sleeping: Help or hindrance for young children’s independence? Infant and Child Development. 2004;13:369–388. [Google Scholar]
- Latz S, Wolf AW, Lozoff B. Cosleeping in context: Sleep practices and problems in young children in Japan and the United States. Archives of Pediatrics and Adolescent Medicine. 1999;153:339–346. doi: 10.1001/archpedi.153.4.339. [DOI] [PubMed] [Google Scholar]
- Liu X, Liu L, Wang R. Bed sharing, sleep habits, and sleep problems among Chinese school-aged children. Pediatrics. 2003;26:839–844. doi: 10.1093/sleep/26.7.839. [DOI] [PubMed] [Google Scholar]
- Lozoff B, Wolf AW, Davis NS. Cosleeping in urban families with young children in the United States. Pediatrics. 1984;74:171–182. [PubMed] [Google Scholar]
- Lyneham HJ, Abbott MJ, Rapee RM. Interrater reliability of the Anxiety Disorders Interview Schedule for DSM-IV: Child and parent versions. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46:731–736. doi: 10.1097/chi.0b013e3180465a09. [DOI] [PubMed] [Google Scholar]
- McGlinchey EL, Harvey AG. Risk behaviors and negative health outcomes for adolescents with late bedtimes. Journal of Youth and Adolescence. 2015;44:478–488. doi: 10.1007/s10964-014-0110-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKenna JJ, Volpe LE. Sleeping with baby: An internet-based sampling of parental experiences, choices, perceptions, and interpretations in a Western industrialized context. Infant and Child Development. 2007;16:359–385. [Google Scholar]
- McMakin DL, Alfano CA. Sleep and anxiety in late childhood and early adolescence. Current Opinion in Psychaitry. 2016;28:483–489. doi: 10.1097/YCO.0000000000000204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meltzer LJ. Clinical management of behavioral insomnia of childhood: Treatment of bedtime problems and night wakings in young children. Behavioral Sleep Medicine. 2010;8:172–189. doi: 10.1080/15402002.2010.487464. [DOI] [PubMed] [Google Scholar]
- Meltzer LJ, Montgomery-Downs HE, Insana SP, Walsh CM. Use of actigraphy for assessment in pediatric sleep research. Sleep Medicine Reviews. 2012;16:463–475. doi: 10.1016/j.smrv.2011.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mileva-Setiz VR, Bakermans-Kranenburg MJ, Battaini C, Luijk MPCM. Parent-child bed-sharing: The good, the bad, and the burden of evidence. Sleep Medicine Reviews. 2017;32:4–27. doi: 10.1016/j.smrv.2016.03.003. [DOI] [PubMed] [Google Scholar]
- Mindell JA, Meltzer LJ, Carskadon MA, Chervin RD. Developmental aspects of sleep hygiene: Findings from the 2004 National Sleep Foundation Sleep in America Poll. Sleep Medicine. 2009;10:771–779. doi: 10.1016/j.sleep.2008.07.016. [DOI] [PubMed] [Google Scholar]
- Ong SH, Wickramaratne P, Tang M, Weissman MM. Early childhood sleep and eating problems as predictors of adolescent and adult mood and anxiety disorders. Journal of Affective Disorders. 2006;96:1–8. doi: 10.1016/j.jad.2006.05.025. [DOI] [PubMed] [Google Scholar]
- Owens JA. Sleep in children: Cross-cultural perspectives. Sleep and Biological Rhythms. 2004;2:165–173. [Google Scholar]
- Owens JA, Spirito A, McGuinn M. The Children’s Sleep Habits Questionnaire (CSHQ): Psychometric properties of a survey instrument for school-aged children. Sleep. 2000;23:1–9. [PubMed] [Google Scholar]
- Paine S, Gradisar M. A randomised controlled trial of cognitive-behaviour therapy for behavioural insomnia of childhood in school-aged children. Behavior Research and Therapy. 2011;49:379–388. doi: 10.1016/j.brat.2011.03.008. [DOI] [PubMed] [Google Scholar]
- Peterman JS, Carper MM, Kendall PC. Anxiety disorders and comorbid sleep problems in school-aged youth: A review and future research directions. Child Psychiatry and Human Development. 2015;46:376–392. doi: 10.1007/s10578-014-0478-y. [DOI] [PubMed] [Google Scholar]
- Rath FH, Jr, Okum ME. Parents and children sleeping together: Co-sleeping prevalence and concerns. American Journal of Orthopsychiatry. 1995;65:411–418. doi: 10.1037/h0079654. [DOI] [PubMed] [Google Scholar]
- Sadeh A, Anders TF. Infant sleep problems: Origins, assessment, interventions. Infant Mental Health Journal. 1993;14:17–34. [Google Scholar]
- Sadeh A, Sharkey KM, Carskadon MA. Activity-based sleep—wake identification: an empirical test of methodological issues. Sleep. 1994;17:201–207. doi: 10.1093/sleep/17.3.201. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Albano A. The Anxiety Disorders Interview Schedule for Children-IV (Child and parent versions) San Antonio: Psychological Corporation; 1996. [Google Scholar]
- Silverman WK, Saaverdra LM, Pina AA. Test-retest reliability of anxiety symptoms and diagnoses with the Anxiety Disorders Interview Schedule for DSM-IV: Child and parent versons. Adolescent Psychiatry. 2001;40:937–944. doi: 10.1097/00004583-200108000-00016. [DOI] [PubMed] [Google Scholar]
- Short MA, Gradisar M, Lack LC, Wright HR. The impact of sleep on adolescent depressed mood, alertness and academic performance. Journal of Adolescence. 2013;36:1025–1033. doi: 10.1016/j.adolescence.2013.08.007. [DOI] [PubMed] [Google Scholar]
- Smedje H, Broman JE, Hetta J. Short-term prospective study of sleep disturbances in 5–8-year-old children. Acta Paediatr. 2001;90:1456–1463. doi: 10.1080/08035250152708897. [DOI] [PubMed] [Google Scholar]
- Storch EA, Geffken GR, Merlo LJ, Jacob ML, Murphy TK, Goodman WK, Larson MJ, Fernandez M, Grabill K. Family accommodation in pediatric obsessive-compulsive disorder. Journal of Clinical Child and Adolescent Psycholology. 2007;36:207–216. doi: 10.1080/15374410701277929. [DOI] [PubMed] [Google Scholar]
- Suveg C, Zeman J. Emotion regulation in children with anxiety disorders. Journal of Clinical Child and Adolescent Psychology. 2004;33:750–759. doi: 10.1207/s15374424jccp3304_10. [DOI] [PubMed] [Google Scholar]
- Takeuchi H, Inoue M, Watanabe N, Yamashita Y, Hamada M, Kadota G, Harada T. Parental enforcement of bedtime during childhood modulates preference of Japanese junior high school students for eveningness chronotype. Chronobiology International. 2001;18:823–829. doi: 10.1081/cbi-100107517. [DOI] [PubMed] [Google Scholar]
- Thelen E. Self-organization in developmental processes: Can systems approaches work? In: Johnson MH, editor. Brain development and cognition. Oxford, England: Blackwell; 1993. pp. 555–592. [Google Scholar]
- Thoman EB. Sleeping and waking states in infants: A functional perspective. Neuroscience and Biobehavioral Reviews. 1990;14:93–107. doi: 10.1016/s0149-7634(05)80165-4. [DOI] [PubMed] [Google Scholar]
- Thoman EB. Co-sleeping, an ancient practice: Issues of the past and present, and possibilities for the future. Sleep Medicine Reviews. 2006;10:407–417. doi: 10.1016/j.smrv.2005.12.001. [DOI] [PubMed] [Google Scholar]
- Thompson-Hollands J, Kerns CE, Pincus DB, Comer JS. Parental accomodation of child anxiety and related symptoms: Range, impact, and correlates. Journal of Anxiety Disorders. 2014;28:765–773. doi: 10.1016/j.janxdis.2014.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfson AR, Carskadon MA. Sleep schedules and daytime functioning in adolescents. Child Development. 1998;69:875–887. [PubMed] [Google Scholar]