Abstract
We are reporting a novel “off-label” use of lumen apposing metal stent (LAMS) for management of refractory gastro-jejunal (GJ) anastomotic stricture after Roux-en-y gastric bypass (RYGB). With increasing prevalence of obesity, bariatric surgery is performed more frequently than ever. RYGB is one of the most commonly performed bariatric procedures. GJ anastomotic stricture is a late complication of this procedure. Our patient, seven years after RYGB developed GJ anastomotic ulcer and subsequently a stricture not amendable to repeated pneumatic dilations. Instead of using the conventional fully covered self-expanding metal stent (fcSEMS) we deployed the relatively new LAMS keeping in mind its novel dumbbell shaped design. Our patient’s symptoms were controlled successfully and she remained asymptomatic on follow-up. Despite initial approval for pancreatic pseudocyst drainage, LAMS has been used with increased frequency at various locations within gastrointestinal tract including GJ anastomotic strictures. Future randomized control trials are warranted to compare the efficacy of fcSEMS to LAMS.
Keywords: Gastro-jejunal anastomotic stricture, Lumen apposing metal stent, Dysphagia, Roux-en-Y gastric bypass
Core tip: Gastro-jejunal (GJ) anastomotic stricture is a common late complication of Roux-en-y gastric bypass. Pneumatic dilation is the first line treatment for these strictures and fully covered self-expanding metal stent (fcSEMS) can be used as an alternative. In this case report we represent the successful off-label placement of lumen apposing metal stent instead of fcSEMS for GJ anastomotic stricture.
INTRODUCTION
Worldwide obesity has tripled since 1975. The number of bariatric surgeries performed each year in united states has been increasing steadily with approximately 196000 surgeries performed in the year 2015[1]. Roux-en-y gastric bypass (RYGB) is the second most common bariatric surgery performed after sleeve gastrectomy. One of the late complications of this procedure is gastro-jejunal (GJ) anastomotic stricture[2]. Initially this is typically managed safely with pneumatic dilation[3]. Alternatives to dilation include needle-knife incisional therapy, local steroid injection and fully covered self-expanding metal stent (fcSEMS). The fcSEMS has a high rate of adverse events including stent migration and recurrence of strictures after removal of stent[4]. Lumen apposing metal stent (LAMS) was initially used for draining pancreatic fluid collections/cystogastrostomy though recently has been used in various locations throughout the gastrointestinal tract due to its novel dumbbell shaped design. In this case report we present a case of GJ anastomotic stricture successfully managed with LAMS after failure of serial balloon dilations and steroid injections. LAMS was preferred over fcSEMS to avoid the high rate of complications.
CASE REPORT
A 42-year-old female with history of RYGB performed seven years ago, complicated by GJ anastomotic ulcer three years ago was seen in follow-up for symptomatic GJ anastomotic stricture. She reported weakness, fatigue and a 50-pound weight loss over the past year due to her inability to tolerate both solids and liquids orally. Her BMI was 18.79 and she did not have any medical comorbidities including no obstructive sleep apnea or hypertension. Patient’s GJ anastomotic ulcer healed two years ago after starting a hydrogen-potassium ATPase inhibitor and she reduced her smoking from one pack per day to three cigarettes per day. For her persistent GJ anastomotic stricture she underwent through-the-scope (TTS) dilation twice this year and twice in the year before with triamcinolone injected in the stricture on her second dilation. These measures provided only temporary relief of her symptoms. On her last esophagogastroduodenoscopy (EGD), she had persistent GJ stricture and no gastro-gastric fistula. Her Helicobacter pylori status was negative on multiple occasions on stool antigen testing and on microscopic examination of obtained tissue samples during EGD. We performed a repeat EGD on which the GJ anastomosis was characterized by severe stenosis (2 mm opening) (Figure 1). A LAMS (Axios stent 15 mm x 10 mm; Boston Scientific, Marlborough, MA, United States) was placed into the anastomotic stricture (Figures 2-4). A wire-guided TTS balloon dilator (CRE; Boston Scientific, Marlborough, MA, United States) was passed over a guidewire (Hydra Jagwire 0.035 cm x 260 cm; Boston Scientific, Marlborough, MA, United States) through the LAMS. Dilation with 10 mm-11 mm-12 mm anastomotic balloon dilators was performed and held inflated for 2 min under fluoroscopic guidance. Our patient did not develop any immediate or delayed stent-related adverse events. Patient’s symptoms improved remarkably after the procedure, she had gained 5 pounds and was asymptomatic on three-month follow-up. We aim to remove the stent after a total of six months for maximum effect.
Figure 1.
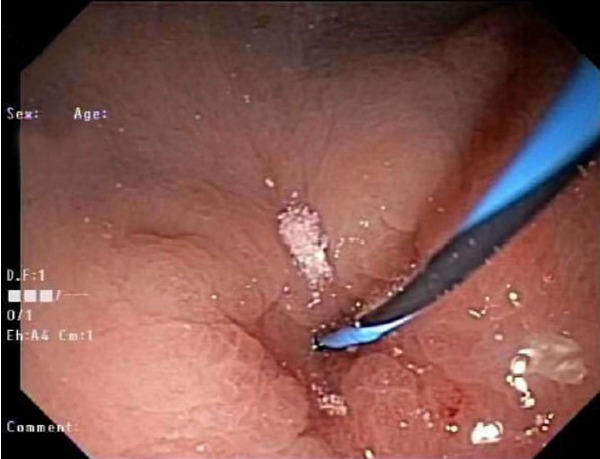
Gastro-jejunal anastomotic stricture with 2 mm opening.
Figure 2.
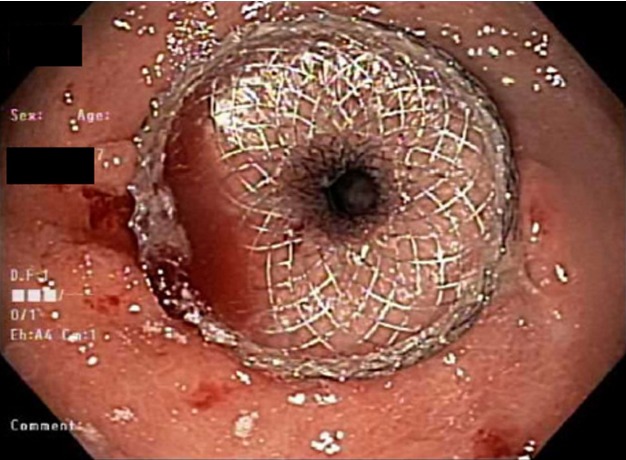
Axios stent placed in gastro-jejunal anastomotic stricture.
Figure 4.
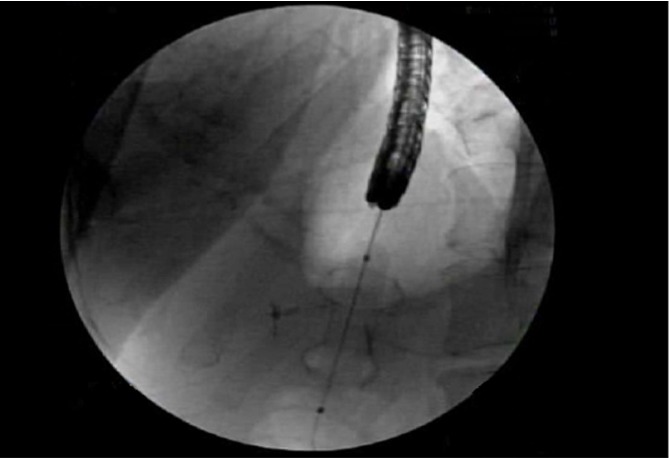
Confirmation of lumen apposing metal stent with fluoroscopic guidance.
Figure 3.
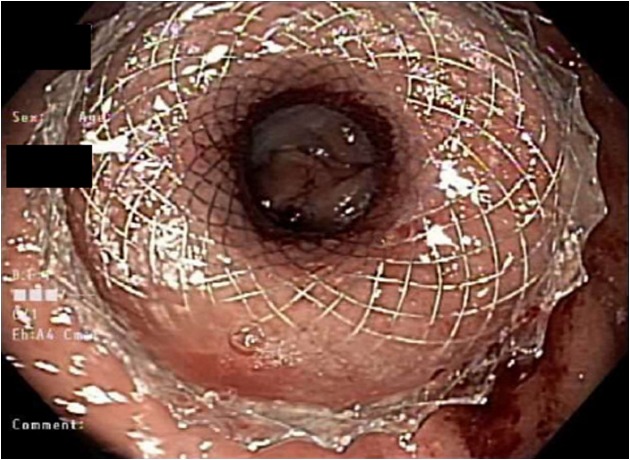
Dilated gastro-jejunal anastomotic stricture with visible jejunal lumen.
DISCUSSION
RYGB is associated with both early and late adverse events. The early adverse events include staple/suture leak, postoperative hemorrhage and bowel obstruction. Late adverse events include but are not limited to marginal ulceration, fistula formation, nutritional deficiencies, difficulty performing endoscopic retrograde cholangiopancreatography (ERCP) and anastomotic stricture. The rate of GJ anastomotic stricture ranges between 2.9% to 23% after RYGB[5-7]. Factors that are implicated in development of this adverse events include anastomotic dehiscence, local ischemia, tension at anastomosis, healing capacity of patient, non-adherence to recommended nutrition and the technique used to create the anastomosis[4,8,9]. This condition is more common in patients with laparoscopic RYGB compared to an open approach[6]. Patients can present anywhere from a couple of weeks to months post-operatively with progressively worsening dysphagia, nausea, vomiting, gastroesophageal reflux and epigastric pain[8]. GJ anastomotic stricture can be identified through various radiographic studies though EGD should be performed if suspected.
Pneumatic dilation is the first line therapy for GJ anastomotic strictures and has shown good results though in some cases serial dilations may be required[6,9-11]. Carrodeguas et al[12] reported a mean of two dilatory sessions required to achieve an anastomotic diameter of 10 mm to 16.5 mm for 94 patients with GJ anastomotic stricture identified through retrospective analysis. Rate of perforation in this study was reported as 2.1%. Alternatives to pneumatic dilation include needle-knife incisional therapy[13] and fcSEMS. The fcSEMS are not ideal due to the high rate of adverse events including intolerance, stent migration and recurrence of symptoms after stent removal[14]. LAMS were originally FDA approved for draining pancreatic fluid collections[15] but case reports/series of off-label use have been recently published with promising results. Gastrointestinal strictures/stenosis where LAMS has been successfully used include benign esophageal stricture, benign gastric outlet obstruction[16], malignant duodenal stricture, colorectal anastomotic stricture[17] and GJ anastomotic stricture[18]. Bazerbachi et al[19] published a multi-center retrospective analysis of 49 patients who underwent 56 LAMS placement procedures for benign gastrointestinal luminal strictures, 77.6% of these patients had anastomotic strictures with 34.7% (17/49) being gastro-jejunal. 36.4% LAMS placed at anastomotic strictures required re-intervention and rate of migration for upper gastrointestinal strictures was 11.1%.
In our case we describe an off-label use of LAMS for GJ anastomotic stricture as a result of RYGB. LAMS was utilized here due to stricture caused by ulceration induced stenosis and not purely “anastomotic stricture”, there was fibrosis from multiple prior dilation attempts. In contrast to conventional fcSEMS, the LAMS is shorter, smaller and its novel dumbbell shape design prevents leakage and migration due to 24 mm anchoring flanges. The stent is deployed with or without fluoroscopic guidance and this is a TTS device. Using conventional stents such as fcSEMS have a higher chance of migration despite using clip fasteners with higher rate of adverse events including ulceration and perforation. The inflation of CRE balloon inside Axios stent causes shortening as with fcSEMS, however due to novel dumbbell design the risk of migration while dilating the stricture through LAMS is very low. The manufacturer recommendation on LAMS duration for cystogastrostomy is four weeks. For off-label use commonly chosen duration is three months[16,17], we intend to keep it in for six months for maximal effect and to prevent stricture recurrence/stent replacement.
Recently published literature has suggested safety and efficacy of LAMS for management of GJ anastomotic strictures and this stent provides us with an alternative to fcSEMS. In our case LAMS was successful in controlling patient’s symptoms without any adverse events. Future randomized controlled trials are warranted to compare the safety, efficacy and cost effectiveness of more expensive LAMS to conventional fcSEMS.
ARTICLE HIGHLIGHTS
Case characteristics
Our patient’s main reported symptoms were weakness, fatigue and a 50-pound weight loss.
Clinical diagnosis
On esophagogastroduodenoscopy (EGD) patient was found to have a gastro-jejunal (GJ) anastomotic stricture.
Differential diagnosis
A careful endoscopic evaluation is necessary to exclude alternative diagnosis such as marginal ulcer and gastro-gastric fistula which can present with similar symptoms.
Laboratory diagnosis
Main laboratory testing for GJ anastomotic stricture involves checking for Helicobacter Pylori through hydrogen breath test, serology, stool antigen test or microscopic examination of obtained tissue during EGD.
Imaging diagnosis
No imaging techniques were used in diagnosis and management of this case though an upper gastrointestinal series can be performed to diagnosis GJ anastomotic stricture/stenosis.
Pathological diagnosis
No Helicobacter pylori organisms were found on microscopic examination of specimens obtained during EGD.
Treatment
Lumen apposing metal stent (LAMS) was deployed in GJ anastomotic stricture during EGD while patient was continued on daily proton pump inhibitor orally.
Term explanation
The term “Hydrogen-potassium ATPase inhibitor” mentioned in this case report is more commonly known as “proton pump inhibitor”.
Experiences and lessons
The newer LAMS is a safe and effective option for management of GJ anastomotic stricture and provides us with an alternative to fully covered self-expanding metal stent.
Footnotes
Informed consent statement: The patient involved in this study gave informed consent authorizing use and disclosure of her protected health information.
Conflict-of-interest statement: All authors have no conflicts of interest to report.
CARE Checklist (2013) statement: The authors have read the CARE Checklist (2013), and the manuscript was prepared and revised according to the CARE Checklist (2013).
Manuscript source: Unsolicited manuscript
Peer-review started: January 12, 2018
First decision: March 7, 2018
Article in press: April 19, 2018
Specialty type: Gastroenterology and hepatology
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Koch TR S- Editor: Cui LJ L- Editor: A E- Editor: Tan WW
Contributor Information
Muhammad Sohail Mansoor, Department of Gastroenterology, Albany Medical Center, Albany, NY 12047, United States. mansoom@amc.edu.
Juan Tejada, Department of Gastroenterology, Albany Medical Center, Albany, NY 12047, United States.
Nour A Parsa, Department of Gastroenterology, Albany Medical Center, Albany, NY 12047, United States.
Eric Yoon, Department of Gastroenterology, Albany Medical Center, Albany, NY 12047, United States.
Sven Hida, Department of Gastroenterology, Albany Medical Center, Albany, NY 12047, United States.
References
- 1.Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012;62:10–29. doi: 10.3322/caac.20138. [DOI] [PubMed] [Google Scholar]
- 2.Fringeli Y, Worreth M, Langer I. Gastrojejunal Anastomosis Complications and Their Management after Laparoscopic Roux-en-Y Gastric Bypass. J Obes. 2015;2015:698425. doi: 10.1155/2015/698425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gill RS, Whitlock KA, Mohamed R, Birch DW, Karmali S. Endoscopic Treatment Options in Patients With Gastrojejunal Anastomosis Stricture Following Roux-en-Y Gastric Bypass. Gastroenterology Res. 2012;5:1–5. doi: 10.4021/gr385w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Freedman J, Jonas E, Näslund E, Nilsson H, Marsk R, Stockeld D. Treatment of leaking gastrojejunostomy after gastric bypass surgery with special emphasis on stenting. Surg Obes Relat Dis. 2013;9:554–558. doi: 10.1016/j.soard.2012.03.002. [DOI] [PubMed] [Google Scholar]
- 5.Alasfar F, Sabnis AA, Liu RC, Chand B. Stricture rate after laparoscopic Roux-en-Y Gastric bypass with a 21-mm circular stapler: the Cleveland Clinic experience. Med Princ Pract. 2009;18:364–367. doi: 10.1159/000226289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mathew A, Veliuona MA, DePalma FJ, Cooney RN. Gastrojejunal stricture after gastric bypass and efficacy of endoscopic intervention. Dig Dis Sci. 2009;54:1971–1978. doi: 10.1007/s10620-008-0581-7. [DOI] [PubMed] [Google Scholar]
- 7.Takata MC, Ciovica R, Cello JP, Posselt AM, Rogers SJ, Campos GM. Predictors, treatment, and outcomes of gastrojejunostomy stricture after gastric bypass for morbid obesity. Obes Surg. 2007;17:878–884. doi: 10.1007/s11695-007-9163-6. [DOI] [PubMed] [Google Scholar]
- 8.Goitein D, Papasavas PK, Gagné D, Ahmad S, Caushaj PF. Gastrojejunal strictures following laparoscopic Roux-en-Y gastric bypass for morbid obesity. Surg Endosc. 2005;19:628–632. doi: 10.1007/s00464-004-9135-z. [DOI] [PubMed] [Google Scholar]
- 9.Nguyen NT, Stevens CM, Wolfe BM. Incidence and outcome of anastomotic stricture after laparoscopic gastric bypass. J Gastrointest Surg. 2003;7:997–1003; discussion 1003. doi: 10.1016/j.gassur.2003.09.016. [DOI] [PubMed] [Google Scholar]
- 10.Csendes A, Burgos AM, Burdiles P. Incidence of anastomotic strictures after gastric bypass: a prospective consecutive routine endoscopic study 1 month and 17 months after surgery in 441 patients with morbid obesity. Obes Surg. 2009;19:269–273. doi: 10.1007/s11695-008-9625-5. [DOI] [PubMed] [Google Scholar]
- 11.Lee JK, Van Dam J, Morton JM, Curet M, Banerjee S. Endoscopy is accurate, safe, and effective in the assessment and management of complications following gastric bypass surgery. Am J Gastroenterol. 2009;104:575–582; quiz 583. doi: 10.1038/ajg.2008.102. [DOI] [PubMed] [Google Scholar]
- 12.Carrodeguas L, Szomstein S, Zundel N, Lo Menzo E, Rosenthal R. Gastrojejunal anastomotic strictures following laparoscopic Roux-en-Y gastric bypass surgery: analysis of 1291 patients. Surg Obes Relat Dis. 2006;2:92–97. doi: 10.1016/j.soard.2005.10.014. [DOI] [PubMed] [Google Scholar]
- 13.Samanta J, Dhaka N, Sinha SK, Kochhar R. Endoscopic incisional therapy for benign esophageal strictures: Technique and results. World J Gastrointest Endosc. 2015;7:1318–1326. doi: 10.4253/wjge.v7.i19.1318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Choi WJ, Park JJ, Park J, Lim EH, Joo MK, Yun JW, Noh H, Kim SH, Choi WS, Lee BJ, et al. Effects of the temporary placement of a self-expandable metallic stent in benign pyloric stenosis. Gut Liver. 2013;7:417–422. doi: 10.5009/gnl.2013.7.4.417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Walter D, Will U, Sanchez-Yague A, Brenke D, Hampe J, Wollny H, López-Jamar JM, Jechart G, Vilmann P, Gornals JB, et al. A novel lumen-apposing metal stent for endoscopic ultrasound-guided drainage of pancreatic fluid collections: a prospective cohort study. Endoscopy. 2015;47:63–67. doi: 10.1055/s-0034-1378113. [DOI] [PubMed] [Google Scholar]
- 16.Pinson R, Pathirana I, Magulick J, Domanski J, Okoh E, Womeldorph C. Novel Use of a Uniquely Designed, Lumen-Apposing, Metal Stent in Benign Gastric Outlet Obstruction in Two Patients. ACG Case Rep J. 2017;4:e20. doi: 10.14309/crj.2017.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Majumder S, Buttar NS, Gostout C, Levy MJ, Martin J, Petersen B, Topazian M, Wong Kee Song LM, Abu Dayyeh BK. Lumen-apposing covered self-expanding metal stent for management of benign gastrointestinal strictures. Endosc Int Open. 2016;4:E96–E101. doi: 10.1055/s-0041-108195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Uchima H, Abu-Suboh M, Mata A, Cruz M, Espinos J. Lumen-apposing metal stent for the treatment of refractory gastrojejunal anastomotic stricture after laparoscopic gastric bypass. Gastrointest Endosc. 2016;83:251. doi: 10.1016/j.gie.2015.07.008. [DOI] [PubMed] [Google Scholar]
- 19.Bazerbachi F, Heffley JD, Abu Dayyeh BK, Nieto J, Vargas EJ, Sawas T, Zaghlol R, Buttar NS, Topazian MD, Wong Kee Song LM, et al. Safety and efficacy of coaxial lumen-apposing metal stents in the management of refractory gastrointestinal luminal strictures: a multicenter study. Endosc Int Open. 2017;5:E861–E867. doi: 10.1055/s-0043-114665. [DOI] [PMC free article] [PubMed] [Google Scholar]


