Abstract
Purpose
Posttraumatic arthritis (PTA) may develop years after acetabular fracture, hindering joint function and causing significant chronic musculoskeletal pain. Given the delayed onset of PTA, few studies have assessed outcomes of delayed total hip arthroplasty (THA) in acetabular fracture patients. This study systematically reviewed the literature for outcomes of THA in patients with PTA and prior acetabular fracture.
Methods
Pubmed, EMBASE, SCOPUS, and Cochrane library were searched for articles containing the keywords “acetabular”, “fracture”, “arthroplasty”, and “post traumatic arthritis” published between 1995 and August 2017. Studies with less than 10 patients, less than 2 years of follow-up, conference abstracts, and non-English language articles were excluded. Data on patient demographics, surgical characteristics, and outcomes of delayed THA, including implant survival, complications, need for revision, and functional scores, was collected from eligible studies.
Results
With 1830 studies were screened and data from 10 studies with 448 patients were included in this review. The median patient age on date of THA was 51.5 years, ranging from 19 to 90 years. The median time from fracture to THA was 37 months, with a range of 27–74 months. Mean follow-up times ranged from 4 to 20 years. The mean Harris hip scores (HHS) improved from 41.5 pre-operatively, to 87.6 post-operatively. The most prevalent postoperative complications were heterotopic ossification (28%–63%), implant loosening (1%–24%), and infection (0%–16%). The minimum 5-year survival of implants ranged from 70% to 100%. Revision rates ranged from 2% to 32%.
Conclusion
Despite the difficulties associated with performing THA in patients with PTA from previous acetabular fracture (including soft tissue scarring, existing hardware, and acetabular bone loss) and the relatively high complication rates, THA in patients with PTA following prior acetabular fracture leads to significant improvement in pain and function at 10-year follow-up. Further high quality randomized controlled studies are needed to confirm the outcomes after delayed THA in these patients.
Keywords: Total hip arthroplasty, Posttraumatic arthritis, Acetabular fractures, Post-operative complications, Heterotopic ossification, Delayed total hip arthroplasty
Introduction
Complications following surgical fixation of acetabular fractures (AFs) are common and defined by the occurrence of posttraumatic arthritis (PTA), chondrolysis, osteonecrosis of the femoral head, and iatrogenic nerve palsies.1 In 2005, Giannoudis et al2 performed a meta-analysis of 3670 AFs treated with open reduction and internal fixation (ORIF) and found that 13%–44% of patients developed PTA. PTA may be a crippling sequelae after AF, and total hip arthroplasty (THA) is often necessary to correct the clinical progression of symptoms.3 In review of Giannoudis et al2, 9% of the AF patients required conversion to THA at an average of two years after the initial procedure. Local tissue changes, including the development of scar tissue, bone density changes, and infection can make this conversion a challenging task for surgeons and may ultimately warrant subsequent THA revisions. Sermon et al4 found a 22% THA conversion rate for AF patients after failing an initial treatment course. Regardless of when THA is performed, patients with prior AFs are at risk for several complications. Heterotopic ossification (HO), surgical site infection, and implant loosening are among the leading reasons why AF patients with THA may require a surgical revision.5 Several studies have suggested that THA in the setting of AF underperforms THA for nontraumatic primary osteoarthritis (OA) on various metrics including survivorship and complication rates.6 However, many studies involve small sample sizes, and there is minimal continuity in terms of the complications that are described from study to study. Overall, reliable epidemiological data on AFs is scarce, yet the orthopedic community is looking for more evidence to help improve long-term outcomes and lessen complications associated with AFs.7, 8
The purpose of this study was to perform a comprehensive review of the 1995–2017 literature concerning the surgical management of acetabular injuries with delayed THA, and subjected the data to a meta-analysis to assess the incidence of various postoperative complications, including the need for surgical revision. We intend for the updated results to help guide the surgical decision-making process moving forward, while serving as an evidence-based instrument which surgeons can utilize when discussing long-term prognoses with their patients.
Methods
Eligibility criteria
We included all study types with n > 10 patients for analysis in this review. We considered only full-text manuscripts available in English, published in peer-reviewed journals the year 1995 or later, with follow-up data available for at least two years. This criteria was selected in an effort to capture two decades of THA procedures, along with an additional two years permitted for adequate patient follow-up. Two-year windows are frequently cited in the literature when discussing post-operative orthopaedic complications, and therefore this interval was built into our search. The patient number requirement was chosen arbitrarily, in an effort to reduce study-to-study variation and permit our paper's authors to adequately examine the methods and results of each included study.
We included study participants of all ages who had undergone delayed THA for the treatment of post-traumatic arthritis following ORIF or non-operative management for traumatic acetabular fractures. Patients with pathologic fractures, stress fractures, peri-prosthetic fractures, or co-existing femur fractures were excluded from review. Participants with developmental dysplasia of the hip were also excluded. We excluded articles with high risk of attrition bias, defined as greater than 30% of patients lost to follow-up.9 We excluded any articles that failed to meet all inclusion criteria or omitted information related to inclusion criteria. We excluded conference and meeting abstracts.
Our outcomes of interest were: patient demographics, time from AF to THA, operative characteristics, and various outcomes following conversion arthroplasty. These outcomes included: implant survival, need for revision, readmissions, pooled complication rate, functional scores, and predictors of poor outcomes. The secondary aims of this study were to compare outcomes of delayed THA following AFs to outcomes of AFs treated with primary THA and non-traumatic primary THA.
Search strategy
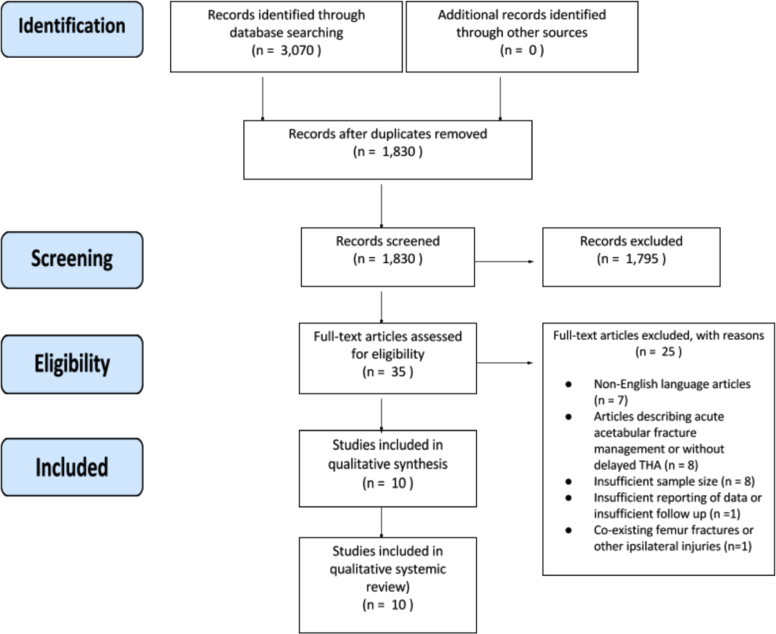
We searched Pubmed, EMBASE, SCOPUS, and Cochrane library from 1995 to 08/30/2017 for articles containing the keywords “acetabular”, “fracture”, “arthroplasty”, and “post traumatic arthritis”. Our database search on 8/30/2017 yielded a total of 3070 results. We identified and excluded duplicate reports and combined multiple reports on the same study, so that each study, rather than each report, was the unit of interest in this review. De-duplication reduced our search to 1830 unique studies. We identified additional studies from the references of full-text articles.
Study selection
The titles and abstracts of 1830 studies were screened independently by two review authors (EL, HP) for relevance and potential inclusion in this systematic review. We obtained the full-text of all potentially relevant reports and two review authors (EL, HP) independently screened all full-text reports for inclusion and exclusion criteria. Twenty-five articles were excluded after full text review for the following reasons: seven non-English language articles,10, 11, 12, 13, 14, 15, 16 eight articles describing acute fracture management or lacking delayed THA,17, 18, 19, 20, 21, 22, 23, 24 eight articles with insufficient sample size (case reports and review articles),5, 6, 25, 26, 27, 28, 29, 30 one article with insufficient outcome data or follow-up duration,31 and one article with co-occurring femur fractures and other ipsilateral injuries.32 Cases of disagreement were resolved by discussion, and if no consensus was reached a third review author (SN) was consulted to make the decision. We recorded the selection process in a PRISMA flow diagram.33 Fig. 1 shows an illustration of the overall search, exclusion, and inclusion methods performed in this paper. We identified 10 unique studies that fit our criteria for further qualitative review.
Fig. 1.
PRISMA flow diagram.
Data extraction
Two review authors (HP, SH) conducted data extraction. In cases where more than one follow-up data point was reported for an outcome of interest, we chose the data point closest to the time point of interest.
Discrepancies in data extraction results were resolved by a third independent review author (SN). We measured the standard means for various outcomes. Initially, we intended to perform a meta-analysis, but we were not able to perform this study due to the amount of missing data and the heterogeneity of the outcomes included in the reviewed studies.
Results
Demographic and injury data
A total of ten studies were included in this review. Six of the studies were retrospective and four were prospective. The median patient age (based on date of initial procedure) across all studies was 51.5 years, ranging from 19 to 90 years of age. In total, 448 patients were included our review, with the smallest study involving 21 patients and the largest study involving 79 patients. The study durations spanned from 53 months to 12 years. Three of the ten studies were comparative studies that assessed delayed THA for PTA versus THA for primary OA of the hip; the other seven studies consisted of a case series with no control group. Table 1 illustrates the main features of the included studies.
Table 1.
Overview of included studiesa.
| Study (year) | Journal | Evidence level | Study years | Control group | Number of hips | Mean follow-up (months) |
|---|---|---|---|---|---|---|
| Chiu34 2015 | Orthopedics | IV | 1996–2010 | No | 56 | 120 |
| Khurana35 2015b | Am J Orthop | III | 2005–2013 | Yes [Primary OA] |
22 | 53 |
| Morison36 2016 | Clin Orthop Relate Res | III | 1987–2011 | Yes [Primary OA] |
74 | 96 |
| Lizaur-Utrilla37 2012 | J Trauma Acute Care Surg | III | 1992–2005 | Yes [Primary OA] |
24 | 101 |
| Zhang38 2011 | J Arthoplasty | IV | 1998–2007 | No | 55 | 64 |
| Ranawat39 2009 | J Arthoplasty | IV | 1995–2003 | No | 32 | 56 |
| Berry40 2002 | Clin Orthop Relate Res | IV | 1984–1990 | No | 34 | 143 |
| Bellabarba41 2001 | J Bone Joint Surg | IV | 1984–1995 | No | 30 | 63 |
| Huo42 1999 | J Arthoplasty | IV | 1985–1993 | No | 21 | 65 |
| Weber43 1998 | J Bone Joint Surg | IV | 1970–1993 | No | 66 | 115 |
OA: osteoarthritis.
The majority of studies reported both mean postoperative Harris hip score and overall revision rate.
Khurana study included data for femoral neck fractures; we examined only data involving fractures of the acetabulum, which totaled 22 hips.
Perioperative variables
The patient age on the initial date of fracture was reported in five studies, garnering a median age of 47 years and a range from 19 years to 90 years. In four studies, the treatment of fracture (i.e., open-reduction, internal fixation versus nonsurgical management) was reported, with the proportion of patients undergoing surgery ranging from 44% to 100%. Preoperative Harris hip score (HHS) was reported in six studies, with a median score of 39.5 (Table 2). Six studies reported the time between fracture and THA, which varied from 27 months to 74 months with a median time of 37 months. Patients' height and weight information was reported in four studies, with a median BMI of 26.4.
Table 2.
Preoperative and postoperative HHS after delayed total hip arthroplasty.
| Study name | Total number of hips | Pre-operative HHS | Post-operative HHS | Follow-up time (months) | Score improvement |
|---|---|---|---|---|---|
| Lizaur-Utrilla37 | 34 | 35 | 77 | 101 | 42 |
| Bellabarba41 | 30 | 41 | 88 | 63 | 47 |
| Zhang38 | 55 | 49 | 90 | 64 | 41 |
| Ranawat39 | 32 | 28 | 82 | 56 | 54 |
| Huo42 | 21 | 30 | 90 | 65 | 60 |
| Weber43 | 66 | 49 | 93 | 115 | 44 |
| Overall | 238 | 41.5a | 87.6a | 82a | 46.2 |
HHS: Harris hip score.
Denotes the average across studies weighted per hip.
Four studies reported operative times, which ranged from 97 min to 240 min. Only two studies reported average blood loss (898 mL and 1000 mL). Three studies reported the average number of units of blood transfusions required per procedure, which ranged from 0.65 units to 3.50 units. Khurana et al35 included PTA patients with both acetabular and femoral head fractures. Given that this was one of the latest studies featuring newer implants, we extracted data involving PTA patients who presented with AFs only, and included only these patients in our analysis.
Postoperative outcomes
Both preoperative and postoperative HHS were included in six of the studies. Postoperative scores were measured at an average follow-up time of 82 months (range 53–115 months). Postoperative hip scores improved by an average of 46.2 points (range 41–60), constituting an overall mean improvement of 111% from baseline in these six data sets consisting of 238 hip THA surgeries. These findings are summarized in Table 2. Break down of HHS data for studies that assessed both preoperative and postoperative scores.
Postoperative complications
Overall complication rates were reported in three studies, with a median complication rate of 10.2%. The most common clinically significant complication was implant loosening, which ranged from 2% to 24% across five studies. Rates of HO were also reported in five studies, ranging from 28% to 63% with additional stratifications made based on Brooker HO classification.44 Ten-year survival was reported in five studies, with a median of 84% and a range of 70%–97%. Revision rates were variable: revision surgery was reported in eight of the ten studies, ranging from 2% to 32%. Iatrogenic nerve injury was the least frequently reported complication at 3%. Table 3 breaks down the reported postoperative complications.
Table 3.
Outcome variables after delayed total hip arthroplasty for posttraumatic arthritisa.
| Outcome of interest | Number of studies | Total number of hips | Total outcome number | Mean occurrence (%) |
|---|---|---|---|---|
| Revision surgery | 8 | 362 | 67 | 18.50 |
| Sciatic nerve injury (Iatrogenic) | 4 | 216 | 6 | 2.77 |
| Heterotopic ossification (Brooker class I-IV) | 5 | 212 | 81 | 38.20 |
| Dislocation | 6 | 270 | 17 | 6.20 |
| Infection | 3 | 136 | 14 | 10.20 |
| Loosening (acetabular + femur) | 5 | 246 | 50 | 20.32 |
| 10 year implant survival | 5 | 250 | N/A | 83.74 |
Summary of common reported outcome variables following delayed THA for posttraumatic arthritis. Of note, Zhang et al.38 also reported asymptomatic heterotopic ossification; we excluded those cases since they were not categorized into the Brooker criteria.
Discussion
The management of AFs has evolved rapidly since Letournel et al45 pioneered ORIF techniques over three decades ago. Recent studies have suggested that PTA is very common following these fractures, regardless of how the anatomy is reconstructed.46 Since this form of arthritis leads to chronic pain, poor function, and a decreased quality of life, the orthopaedic community is actively looking for evidence-based solutions that will guide future management strategies. The pathomechanics underlying PTA is likely multifactorial; Morison et al36 previously suggested that the disease may not only be a result of articular incongruities following reduction, but also stem from the articular cartilage damage that occurs from the initial trauma. Regardless of the mechanism, the associated pain often necessitates THA, and more pooled studies are needed to evaluate THA outcomes in this population.
There was a wide variation in revision rates between the studies included in our analysis, from 2% to 32%. Morison et al36 and Berry et al40 reported the highest revision rates of 30% and 32%, respectively, during their long-term follow-up. They concluded that (1) younger patient age, (2) the presence of sclerotic bone, (3) abnormal anatomy after trauma, (4) loss of acetabular bone stock, and (5) development of hardware complications, all lead to higher revision rates. In both of these high-revision studies, the overwhelming majority (96%) of patients received cementless acetabular components during the THA procedure. These cementless components have shown improved survival compared to cemented components, which have previously demonstrated a higher incidence of aseptic loosening and subsequent need for more frequent revision.43 Both Morison et al36 and Berry et al40 suggested that the high (relative) revision rates were likely attributed to peri-prosthetic osteolysis, polyethylene wear, and loosening. The occurrence of polyethylene liner wear is particularly relevant in younger patient populations with monoarticular injuries who are generally more active after surgery, and Morison et al36 attributed lower rates of revision in prior studies to the use of elevated liners. Berry et al40 found that use of first and second-generation cementless acetabular cups resulted in more polyethylene wear, leading to higher revision rates. In contrast, data from the studies of Chiu et al34 and Zhang et al,38 which reported revision rates of 5% and 2%, respectively, suggests that cup material and liner selection may affect the durability of THA following PTA. The study of Chiu et al34 included 8 hips treated with trabecular metal (TM) cups, with none of the TM patients experiencing mechanical failure on follow-up. In addition, the case series of Zhang et al38 included the use of ceramic bearing surfaces in over 50% of the THAs, further supporting the idea that the use of these materials at the joint interface may combat periacetabular osteolysis and lessen the revision requirement. The use of newer generation TM acetabular cups, polyethylene liner, and interface may be among the reasons for lower revision rate seen in the studies of Chiu et al34 and Zhang et al.38 After performing our analysis, we hypothesize that the materials used at the acetabular joint interface play an integral role in reducing the burden of revision. Given recent advancements in the bearing surface materials utilized for THA, it is plausible that the rate of failure in THA for PTA will decline secondary to decreased surface wear. This material surface hypothesis is limited by the short and variable follow-up times, small sample sizes, and lack of control group included in the study designs of Chiu et al34 and Zhang et al38 study designs. For this reason, new patient data is needed to establish revision rates and determine if arthroplasties for PTA are becoming more durable than previously reported.
HO was one of the most common reported complications of delayed THA. Morison et al36 reported the highest occurrence of clinically significant HO at 43%, nearly 40% of which met Brooker Class II criteria. Overall, we found that HO ranged from 28% to 40% across our review. Bellabarba et al41 cited that only 20% (2/8) patients who received HO prophylaxis developed the complication, compared to 50% (11/22) who did not receive prophylactic treatment for HO prevention. This suggests that indomethacin may play an important role in reducing the occurrence of HO following THA. Anterior approaches and pre-operative prophylactic radiation were also associated with a reduced likelihood of developing HO, specifically in cases of delayed THA where extensive dissection was required prior to the conversion.47, 48 More data on the efficacy of preoperative radiation for HO prophylaxis is necessary to determine if this confers benefit in THA patients.
When THA patients with PTA are compared to THA patients with primary OA, it appears that the post-trauma cases present more operative challenges and postoperative complications.35 Khurana et al35 found that post-trauma patients lost a mean of 360 mL more blood compared to THA for primary OA, requiring more blood transfusions (1.59 units vs. 0.85 units). This is likely attributable to the increased operative times witnessed in post-trauma THA cases, and the inherent challenges surgeons face when encountering tissues that have been considerably altered by the inciting trauma. Several operative metrics (e.g., operative times, blood loss, transfusion requirements) reported by Bellabarba et al41 revealed a similar trend. Despite these increased surgical challenges, the HHS of patients improved dramatically after undergoing delayed THA. Low preoperative HHS suggests that these patients experienced significant impairment in daily functioning prior to seeking THA. Thus, the risks of suboptimal outcomes and complications associated with delayed THA should be weighed against the potential for significant improvements in pain, range of motion, and daily functioning during patient counseling and surgical decision making in patients with prior AF.
Our study has several limitations. Of the ten studies included in this review, only three papers incorporated a control group; further research involving randomized control studies is necessary to reduce the potential for unidentified confounding relationships. There was considerable variation across the ten studies incorporated in this review, and therefore the clinical significance of our study is curtailed by the limited availability of high quality original data reported for this unique patient population. In addition, although the HHS is an excellent endpoint for assessing THA outcomes, it was not utilized across all of the studies, limiting our ability to compare surgical outcomes across different treatment modalities and draw more robust conclusions. For future case series and prospective studies on THA for PTA, we hope that investigators will continue to utilize this validated measurement tool.
Higher level of evidence is needed in this area in the form of prospective, comparative clinical trials. Furthermore, there is a need for large, well-designed studies comparing early and delayed THA with adequate follow-up to compare long-term outcomes.
Footnotes
Peer review under responsibility of Daping Hospital and the Research Institute of Surgery of the Third Military Medical University.
Supplementary data related to this article can be found at https://doi.org/10.1016/j.cjtee.2018.02.004.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Matta J.M., Mehne D.K., Roffi R. Fractures of the acetabulum. Early results of a prospective study. Clin Orthop Relat Res. 1986;205:241–250. [PubMed] [Google Scholar]
- 2.Giannoudis P.V., Grotz M.R., Papakostidis C. Operative treatment of displaced fractures of the acetabulum. A meta-analysis. J Bone Jt Surg Br. 2005;87:2–9. [PubMed] [Google Scholar]
- 3.Romness D.W., Lewallen D.G. Total hip arthroplasty after fracture of the acetabulum. Long-term results. J Bone Jt Surg Br. 1990;72:761–764. doi: 10.1302/0301-620X.72B5.2211750. [DOI] [PubMed] [Google Scholar]
- 4.Sermon A., Broos P., Vanderschot P. Total hip replacement for acetabular fractures. Results in 121 patients operated between 1983 and 2003. Injury. 2008;39:914–921. doi: 10.1016/j.injury.2007.12.004. [DOI] [PubMed] [Google Scholar]
- 5.Sierra R.J., Mabry T.M., Sems S.A. Acetabular fractures: the role of total hip replacement. Bone Joint J. 2013;95-B(11 Suppl A):11–16. doi: 10.1302/0301-620X.95B11.32897. [DOI] [PubMed] [Google Scholar]
- 6.Jimenez M.L., Tile M., Schenk R.S. Total hip replacement after acetabular fracture. Orthop Clin N Am. 1997;28:435–446. doi: 10.1016/s0030-5898(05)70300-x. [DOI] [PubMed] [Google Scholar]
- 7.Tonetti J., Jouffroy P., Pelvis-Acetabulum Club Recent progress in the diagnosis and treatment of pelvic ring and acetabular fracture. Orthop Traumatol Surg Res. 2017;103:631–632. doi: 10.1016/j.otsr.2017.06.002. [DOI] [PubMed] [Google Scholar]
- 8.Firoozabadi R., Cross W.W., Krieg J.C. Acetabular fractures in the senior population- epidemiology, mortality and treatments. Arch Bone Jt Surg. 2017;5:96–102. [PMC free article] [PubMed] [Google Scholar]
- 9.Amico K.R. Percent total attrition: a poor metric for study rigor in hosted intervention designs. Am J Publ Health. 2009;99:1567–1575. doi: 10.2105/AJPH.2008.134767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Macedo C.A., Galia C.R., Cejas F.A. Use of Spotorno expansive acetabulum in sequel of acetabular fracture. Rev Fac Cien Med Univ Nac Cordoba. 2000;57:81–88. [PubMed] [Google Scholar]
- 11.Chu X.B., Tong P.J., Zhang J.H. Total hip arthroplasty for the post-traumatic osteoarthritis after open reduction and internal fixation of acetabular fracture. Zhonghua Wai Ke Za Zhi. 2010;48:1097–1100. [PubMed] [Google Scholar]
- 12.Delgado Serrano P.J., López-Oliva Muñoz F., Forriol Campos F. Clinical and laboral results of total hip arthroplasty in postraumatic osteoarthritis. Patol del Apar Locomot. 2007;5:83–92. [Google Scholar]
- 13.Zhang J., Ling J., Liu H. Short-term effectiveness of total hip arthroplasty for post-traumatic osteoarthritis secondary to acetabular fracture. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2013;27:990–993. [PubMed] [Google Scholar]
- 14.Yu L., Zhang C., Guo T. Middle and long-term results of total hip arthroplasties for secondary post-traumatic arthritis and femoral head necrosis after acetabular fractures. Zhong Guo Gu Shang. 2016;29:109–113. [PubMed] [Google Scholar]
- 15.D'Imporzano M., Pierannunzii L., Fadigati P. Total hip arthroplasty after acetabular fracture. Minerva Ortop Traumatol. 2003;54:111–118. [Google Scholar]
- 16.Pavelka T., Linhart M., Houček P. Hip joint arthroplasty following surgical treatment of acetabular fracture. Acta Chir Orthop Traumatol Cech. 2006;73:268–274. [PubMed] [Google Scholar]
- 17.Boudissa M., Ruatti S., Kerschbaumer G. Part 2: outcome of acetabular fractures and associated prognostic factors—a ten-year retrospective study of one hundred and fifty six operated cases with open reduction and internal fixation. Int Orthop. 2016;40:2151–2156. doi: 10.1007/s00264-015-3070-6. [DOI] [PubMed] [Google Scholar]
- 18.Enocson A., Blomfeldt R. Acetabular fractures in the elderly treated with a primary burch-schneider reinforcement ring, autologous bone graft, and a total hip arthroplasty: a prospective study with a 4-year follow-up. J Orthop Trauma. 2014;28:330–337. doi: 10.1097/BOT.0000000000000016. [DOI] [PubMed] [Google Scholar]
- 19.Gupta R.K., Jindal N., Pruthi M. Acetabular fractures labelled poor surgical choices: analysis of operative outcome. J Clin Orthop Trauma. 2015;6:94–100. doi: 10.1016/j.jcot.2015.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lin C., Caron J., Schmidt A.H. Functional outcomes after total hip arthroplasty for the acute management of acetabular fractures: 1- to 14-year follow-up. J Orthop Trauma. 2015;29:151–159. doi: 10.1097/BOT.0000000000000164. [DOI] [PubMed] [Google Scholar]
- 21.Ortega-Briones A., Smith S., Rickman M. Acetabular fractures in the elderly: midterm outcomes of column stabilisation and primary arthroplasty. BioMed Res Int. 2017;2017:4651518. doi: 10.1155/2017/4651518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rickman M., Young J., Trompeter A. Managing acetabular fractures in the elderly with fixation and primary arthroplasty: aiming for early weightbearing. Clin Orthop Relat Res. 2014;472:3375–3382. doi: 10.1007/s11999-014-3467-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Salama W., Mousa S., Khalefa A. Simultaneous open reduction and internal fixation and total hip arthroplasty for the treatment of osteoporotic acetabular fractures. Int Orthop. 2017;41:181–189. doi: 10.1007/s00264-016-3175-6. [DOI] [PubMed] [Google Scholar]
- 24.Salar N., Bilgen M.S., Bilgen Ö F. Total hip arthroplasty for acetabular fractures: “early application”. Ulus Travma Acil Cerrahi Derg. 2017;23:337–342. doi: 10.5505/tjtes.2016.55675. [DOI] [PubMed] [Google Scholar]
- 25.Cuckler J.M. Dealing with post-traumatic arthrosis of the hip. Orthopedics. 2001;24:867–868. doi: 10.3928/0147-7447-20010901-18. [DOI] [PubMed] [Google Scholar]
- 26.Swanson M.A., Huo M.H. Total hip arthroplasty for post-traumatic arthritis after previous acetabular fractures. Semin Arthroplasty. 2008;19:303–306. [Google Scholar]
- 27.Swanson M.A., Knight J.R., Huo M.H. Total hip arthroplasty following previous acetabular fracture. Operat Tech Orthop. 2009;19:150–154. [Google Scholar]
- 28.Wu E.S., Jauregui J.J., Banerjee S. Outcomes of delayed total hip arthroplasty in patients with a previous ipsilateral acetabular fracture. Expert Rev Med Dev. 2015;12:297–306. doi: 10.1586/17434440.2015.1026327. [DOI] [PubMed] [Google Scholar]
- 29.Butterwick D., Papp S., Gofton W. Acetabular fractures in the elderly: evaluation and management. J Bone Jt Surg Am. 2015;97:758–768. doi: 10.2106/JBJS.N.01037. [DOI] [PubMed] [Google Scholar]
- 30.Veerappa L.A., Tripathy S.K., Sen R.K. Management of neglected acetabular fractures. Eur J Trauma Emerg Surg. 2015;41:343–348. doi: 10.1007/s00068-014-0462-z. [DOI] [PubMed] [Google Scholar]
- 31.O'Toole R.V., Hui E., Chandra A. How often does open reduction and internal fixation of geriatric acetabular fractures lead to hip arthroplasty? J Orthop Trauma. 2014;28:148–153. doi: 10.1097/BOT.0b013e31829c739a. [DOI] [PubMed] [Google Scholar]
- 32.Woon R.P., Johnson A.J., Amstutz H.C. Results of conserve plus® metal-on-metal hip resurfacing for post-traumatic arthritis and osteonecrosis. Hip Int. 2012;22:195–202. doi: 10.5301/HIP.2012.9226. [DOI] [PubMed] [Google Scholar]
- 33.Moher D., Liberati A., Tetzlaff J. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62:1006–1012. doi: 10.1016/j.jclinepi.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 34.Chiu F.Y., Lin Y.P., Hung S.H. Cementless acetabular reconstruction for arthropathy in old acetabular fractures. Orthopedics. 2015;38:e934–e939. doi: 10.3928/01477447-20151002-63. [DOI] [PubMed] [Google Scholar]
- 35.Khurana S., Nobel T.B., Merkow J.S. Total hip arthroplasty for posttraumatic osteoarthritis of the hip fares worse than THA for primary osteoarthritis. Am J Orthop. 2015;44:321–325. [PubMed] [Google Scholar]
- 36.Morison Z., Moojen D.J., Nauth A. Total hip arthroplasty after acetabular fracture is associated with lower survivorship and more complications. Clin Orthop Relat Res. 2016;474:392–398. doi: 10.1007/s11999-015-4509-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lizaur-Utrilla A., Sanz-Reig J., Serna-Berna R. Cementless acetabular reconstruction after acetabular fracture: a prospective, matched-cohort study. J Trauma Acute Care Surg. 2012;73:232–238. doi: 10.1097/TA.0b013e31824cf39e. [DOI] [PubMed] [Google Scholar]
- 38.Zhang L., Zhou Y., Li Y. Total hip arthroplasty for failed treatment of acetabular fractures: a 5-year follow-up study. J Arthroplasty. 2011;26:1189–1193. doi: 10.1016/j.arth.2011.02.024. [DOI] [PubMed] [Google Scholar]
- 39.Ranawat A., Zelken J., Helfet D. Total hip arthroplasty for posttraumatic arthritis after acetabular fracture. J Arthroplasty. 2009;24:759–767. doi: 10.1016/j.arth.2008.04.004. [DOI] [PubMed] [Google Scholar]
- 40.Berry D.J., Halasy M. Uncemented acetabular components for arthritis after acetabular fracture. Clin Orthop Relat Res. 2002;405:164–167. doi: 10.1097/00003086-200212000-00020. [DOI] [PubMed] [Google Scholar]
- 41.Bellabarba C., Berger R.A., Bentley C.D. Cementless acetabular reconstruction after acetabular fracture. J Bone Jt Surg Am. 2001;83-A:868–876. doi: 10.2106/00004623-200106000-00008. [DOI] [PubMed] [Google Scholar]
- 42.Huo M.H., Solberg B.D., Zatorski L.E. Total hip replacements done without cement after acetabular fractures: a 4- to 8-year follow-up study. J Arthroplasty. 1999;14:827–831. doi: 10.1016/s0883-5403(99)90033-5. [DOI] [PubMed] [Google Scholar]
- 43.Weber M., Berry D.J., Harmsen W.S. Total hip arthroplasty after operative treatment of an acetabular fracture. J Bone Jt Surg Am. 1998;80:1295–1305. doi: 10.2106/00004623-199809000-00008. [DOI] [PubMed] [Google Scholar]
- 44.Brooker A.F., Bowerman J.W., Robinson R.A. Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Jt Surg Am. 1973;55:1629–1632. [PubMed] [Google Scholar]
- 45.Letournel E. Acetabulum fractures: classification and management. Clin Orthop Relat Res. 1980;151:81–106. [PubMed] [Google Scholar]
- 46.Makridis K.G., Obakponovwe O., Bobak P. Total hip arthroplasty after acetabular fracture: incidence of complications, reoperation rates and functional outcomes: evidence today. J Arthroplasty. 2014;29:1983–1990. doi: 10.1016/j.arth.2014.06.001. [DOI] [PubMed] [Google Scholar]
- 47.Newman E.A., Holst D.C., Bracey D.N. Incidence of heterotopic ossification in direct anterior vs posterior approach to total hip arthroplasty: a retrospective radiographic review. Int Orthop. 2016;40:1967–1973. doi: 10.1007/s00264-015-3048-4. [DOI] [PubMed] [Google Scholar]
- 48.Archdeacon M.T., d'Heurle A., Nemeth N. Is preoperative radiation therapy as effective as postoperative radiation therapy for heterotopic ossification prevention in acetabular fractures? Clin Orthop Relat Res. 2014;472:3389–3394. doi: 10.1007/s11999-014-3670-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.