Abstract
Purpose
“Polytrauma” patients are of a higher risk of complications and death than the summation of expected mortality and morbidity of their individual injuries. The ideal goal in trauma resuscitation care is to identify and treat all injuries. With clinical and technological advanced imaging available for diagnosis and treatment of traumatic patients, point of care–rapid ultrasound in shock and hypotension (RUSH) significantly affects modern trauma services and patient outcomes. This study aims to evaluate the accuracy of RUSH and patient outcomes by early detection of the causes of unstable polytrauma.
Methods
This cross-sectional, prospective study included 100 unstable polytrauma patients admitted in Suez Canal University Hospital. Clinical exam, RUSH and pan-computed tomography (pan-CT) were conducted. The result of CT was taken as the standard. Patients were managed according to the advanced trauma life support (ATLS) guidelines and treated of life threatening conditions if present. Patients were followed up for 28 days for a short outcome.
Results
The most diagnostic causes of unstability in polytrauma patients by RUSH are hypovolemic shock (64%), followed by obstructive shock (14%), distributive shock (12%) and cardiogenic shock (10%) respectively. RUSH had 94.2% sensitivity in the diagnosis of unstable polytrauma patients; the accuracy of RUSH in shock patients was 95.2%.
Conclusion
RUSH is accurate in the diagnosis of unstable polytrauma patients; and 4% of patients were diagnosed during follow-up after admission by RUSH and pan-CT.
Keywords: Polytrauma, Shock, Rapid ultrasound in shock and hypotension
Introduction
The exam rapid ultrasound in shock and hypotension (RUSH) is described as a thorough ultrasound evaluation which can be separated into 3 categories: the pump (focused echocardiogram for pericardial effusion, global left ventricular contractility, and right ventricular: left ventricular ratio as a surrogate marker for massive pulmonary embolism); the tank (inferior vena cava for volume status, peritoneal and pleural cavities for free fluid); and the pipes (thoracic aorta for evidence of dissection, abdominal aorta for abdominal aortic aneurysm, and the lower extremity veins for deep venous thrombosis).1
Trauma is the commonest cause of death in the first four decades of life, and it still a major health problem in all countries, regardless of the urban or rural area.2 The term “polytrauma” has been used for long to describe blunt trauma patients with injuries affecting multiple body areas or cavities, compromising the physiology of patients and inducing dysfunction of uninjured organs.
Polytrauma patients have a higher risk of complications and death than the summation of expected mortality and morbidity of their individual injuries.3 In this study, polytrauma is defined as a clinical state following injuries to body leading to profound physio-metabolic changes involving any of the following combination of injuries: (1) two major system injury + one major limb injury; (2) one major system injury + two major limb injury; (3) one major system injury + one grade 3 open skeletal injury; and (4) unstable pelvic fracture with associated visceral injury.4 Here major injury was either death within 24 h, injury severity score (ISS) ≥16, intensive care unit (ICU) stay ≥1 day or amount of blood transfused ≥2 units.5
Polytrauma always involves young, productive individuals and represents a substantial burden in the society, from both financial view and human perspectives. The presence of multiple injuries leads to significant disability with decreased chance of return to work and thus significant effect on economic state.6
It is apparent that bedside ultrasonography is a very helpful adjunct for the diagnosis of many emergent and life-threatening conditions. Emergency physicians have begun to apply this technology. Widespread use of limited bedside ultrasonography by emergency physicians will improve the diagnostic accuracy and efficiency, increase the quality of care, and proves to be a cost-effective technique for the practice of emergency medicine.7
Multiple investigators have concluded that the escalation in CT use is associated with clear and quantifiable cancer risks and several major specialty organizations have therefore called for a review of widespread CT use in trauma. In 2014 the American College of Surgeons listed avoidance of routine whole body trauma CT as one of its five choosing wisely recommendations.8
This study aims to improve the management processes of unstable polytrauma patients by early detection of injury causes, the accuracy of RUSH in Egyptian polytrauma patients and their outcomes. We seek to reduce the costs, radiation risks of unnecessary imaging exam and transposition of unstable patients for doing pan-computed tomography (pan-CT).
Methods
Inclusion criteria
This cross-sectional prospective study included unstable polytrauma patients admitted in Suez Canal University Hospital who (1) were applied advanced trauma life support (ATLS) guidelines and (2) treated for all the life threatening conditions and (3) had a follow-up time frame of 28 days.
The sample size was estimated using a predetermined area under the curve (AUC) for prediction of mortality among polytrauma patients = 0.844.9 The sample size was calculated for power of the study of 90% and an error of 0.05. An estimated drop out of 10% will be added. A series of equations are adopted to estimate the sample size using AUC. Computer-based software was used to calculate the required sample size.12 The least required sample size is 100 patients. Therefore 100 unstable polytrauma patients (defined as before) transferred to our hospital were included. All the polytrauma patients entered the resuscitation room once they arrived at the emergency room and excluded mixed or undefined types of shock from the sample size of the study.
Treatment
ATLS guidelines
ATLS guidelines were strictly followed for all the patients-ABCDE principle. Life threatening conditions were treated if founded.
-
A.
(Air way): Assess the airway and keep the neck immobilized in neutral position. Insert neck collar for all polytrauma patients.
-
B.
(Breathing): Assess breathing adequacy and airway patency by clinical observation.
-
C.
(Circulation): Assess the patient's circulation as we recheck the oxygen supply, airway patency and breathing adequacy.
-
D.
(Disability): Assessment neurological state by Glasgow coma score (GCS).
-
E.
(Exposure): Undress the patient to search for injuries; in-line immobilize patient with spinal injury; and complete primary survey.
Clinical and radiological survey
After ABCDE, all patients were subjected to full history (including age, gender, occupation, mode of trauma, and time of trauma, arrival and resuscitation) and secondary survey.
General examination of pulse, blood pressure, respiratory rate, temperature and oxygen saturation as well as local examination of head and neck, chest, abdomen, pelvis and extremities was conducted. Laboratory investigation included complete blood count, blood grouping & cross match, random blood sugar, arterial blood gases, serum creatinine and liver function test if needed.
All polytrauma patients underwent the following radiology:
The Rush protocol
-
(1)
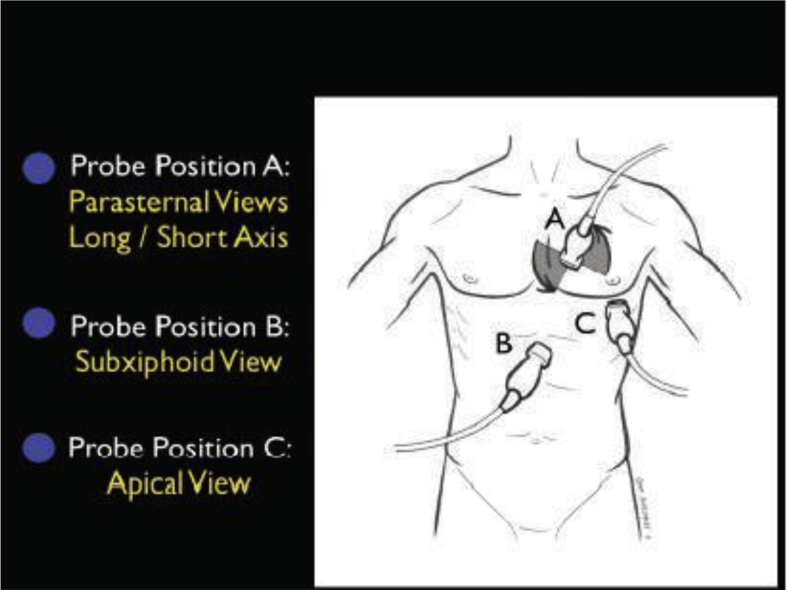
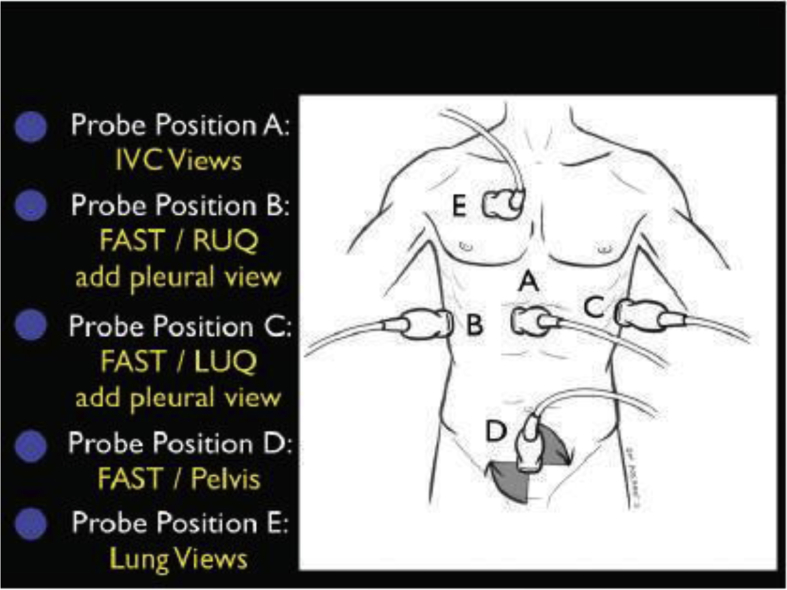
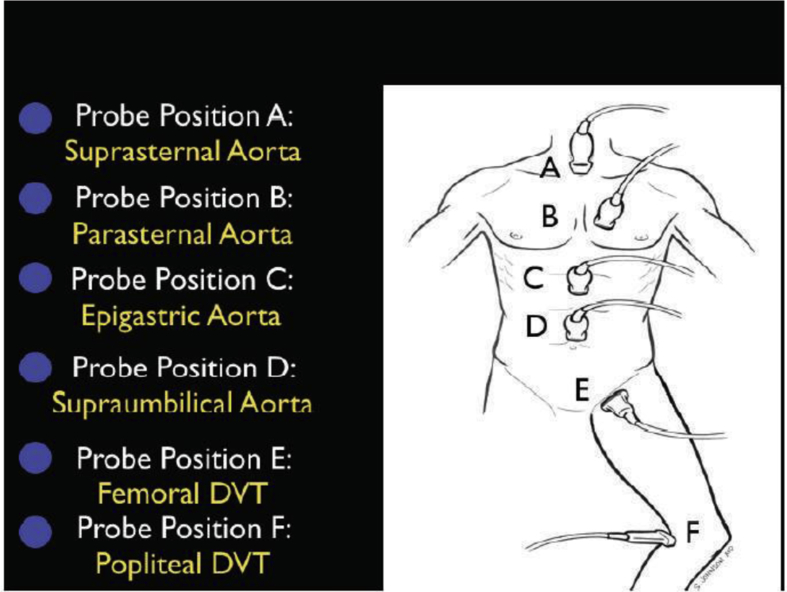
Step 1: The Pump. The first step in evaluation of the patient in shock is determination of cardiac status, termed for simplicity “the pump.” Imaging of the heart usually involves four classical views: parasternal long and short axis, subxiphoid, and apical (Figure 1). Step 2: The Tank. The second part of the RUSH protocol focuses on the determination of the effective intravascular volume status, which will be referred to as “the tank” (Figure 2). Step 3: The Pipes. The third and final step in the RUSH exam is to examine “the pipes,” looking first at the arterial side of the circulatory system, and secondly, at the venous side (Figure 3). Vascular catastrophes, such as a ruptured abdominal aortic aneurysm (AAA) or an aortic dissection, are life-threatening causes of hypotension. The survival of such patients may often be measured in minutes, and the ability to quickly diagnose these diseases is crucial. All the figures are cited from Reference 10.
-
(2)
Portable chest X-ray.
-
(3)
Portable pelvis X-ray
Fig. 1.
The RUSH exam. Step 1: Evaluation of “the pump”.
Fig. 2.
The RUSH exam. Step 2: Evaluation of “the tank”.
Fig. 3.
The RUSH exam. Step 3: Evaluation of “the pipes”.
After patient admission
After admission, all the patients were closely followed-up and received future treatments:
-
(1)
Recheck for any life threatening condition and treat if founded.
-
(2)
All patients were subjected to full history and examination and closely monitored.
-
(3)
The follow-up frame was 28 days inpatient ward or in ICU.
-
(4)
The progressive notes written by the staff of the emergency department and the ICU if needed, and the attending surgical registrars were used as the criteria of initial diagnosis. Comparing them to the injuries listed in the progress notes, investigation reports, and discharge summary lead to discovery of a number of new diagnoses.
Outcome
Fate of the patient was recorded “within 28 days' timeframe outcomes” whether:
-
(1)
Had surgical intervention,
-
(2)
Admitted to inpatient department under observation,
-
(3)
Admitted to intensive care unit,
-
(4)
Transferred and indication of transfer,
-
(5)
Discharged from emergency department,
-
(6)
Died at emergency room.
Ethical consideration
All patients give consent to participate in the study without affecting their course of treatment accordingly permission obtained from ethical committee of faculty of medicine in Suez Canal University.
-
(1)
Approval of research ethics committee.
-
(2)
Singing written informed consent from participants.
-
(3)
Confidentiality of data.
-
(4)
Explanation of our study to the participants.
-
(5)
An informed consent was taken from each patient or relatives.
Results
One hundred polytrauma patients were included in this study; 75% were males and 25% were females. The age of the patients ranged from 7 to 65 (mean SD 27.5 ± 17.8) years, respectively 31 in the <18 years age group, 59 in the 18–60 age group and 10 in the >60 age group. Adults aged 18–60 years (59%) were most frequently attacked by trauma. The most common mode of trauma was RTAs-86 patients (86%), followed by gunshot 8 (8%) and fall from height 6 (6%).
Clinical predictors for hypovolemia of the studied patients included respiratory rate, heart rate, systolic blood pressure, diastolic blood pressure, the mean arterial blood pressure and the GCS score. All of the detailed data are listed in Table 1. Table 2 shows the injury types based on different body regions.
Table 1.
Clinical predictors for hypovolemia.
| Clinical predictors for hypovolemia | Mean ± SD | t value | p value |
|---|---|---|---|
| Respiratory rate (breath/min) | 28.4 ± 7.6 | 4.3 | <0.001 |
| Heart rate (beats/min) | 107.6 ± 7.9 | 18.0 | <0.001 |
| Systolic blood pressure (mmHg) | 74.0 ± 6.5 | 18.5 | <0.001 |
| Diastolic blood pressure (mmHg) | 44.1 ± 15.6 | 14.2 | <0.001 |
| Mean arterial blood pressure (mmHg) | 53.9 ± 15.9 | 15.8 | <0.001 |
| Glasgow coma scale | 13.1 ± 2.5 | 5.3 | <0.001 |
Note: All the predictors are statistically significant for hypovolemia.
Table 2.
Type of injuries of polytrauma patients (total number of injuries = 219).
| Type of injuries | Frequency | Type of injuries | Frequency | Type of injuries | Frequency |
|---|---|---|---|---|---|
| Head | 71 (32.4%) | Face | 24 (11.0%) | Extremities | 75 (34.2%) |
| Fissure fracture | 8 | Orbital fracture | 5 | Clavicular fracture | 6 |
| Depressed fracture | 3 | Mandible fracture | 7 | Humeral fracture | 2 |
| Comminuted fracture | 3 | Le Forte fracture | 2 | Supracondylar fracture | 3 |
| Fracture base of the skull | 4 | Zygomatic fracture | 3 | Both-bone forearm fracture | 3 |
| Epidural hematoma | 12 | Nasal bone fracture | 4 | Distal radius fracture | 7 |
| Subdural hematoma | 6 | Maxillary fracture | 3 | Scaphoid fracture | 2 |
| Subarachnoid hemorrhage | 7 | Spine | 5 (2.3%) | Pelvic fracture | 6 |
| Brain contusion | 11 | Fissure fracture | 2 | Femoral fracture | 11 |
| Brain edema | 4 | Compressed fracture | 3 | Tibial fracture | 4 |
| Pnemocephales | 3 | Chest | 36 (16.4%) | Patellar fracture | 3 |
| Diffuse axonal injury | 3 | Unilateral rib fracture | 9 | Both-bone leg fracture | 8 |
| Subgleal hematoma | 7 | Bilateral rib fracture | 2 | Foot fracture | 4 |
| Abdomen and pelvis | 8 (3.7%) | Pneumothorax | 6 | Vascular injury | 2 |
| Splenic injury | 3 | Surgical emphysema | 3 | Nerve injury | 1 |
| Hepatic injury | 2 | Hemothorax | 5 | Cut tendon | 6 |
| Renal injury | 2 | Lung contusion | 10 | Skin loss | 5 |
| Diaphragmatic injury | 1 | Sternal fracture | 1 | Amputated extremities | 1 |
| Contusion and laxation | 1 |
The diagnostic cause of unstability in polytrauma patients by RUSH is hypovolemic shock (64%), obstructive shock (14%), distributive shock (12%) and then cardiogenic shock (10%) respectively (Table 3). The diagnostic reliability of RUSH of each shock type in relation to pan-CT in polytrauma patients is listed in Table 4 and the total accuracy of RUSH was 95.2%.
Table 3.
Diagnostic causes of instability polytrauma patients by RUSH.
| RUSH exam | Shock type |
|||
|---|---|---|---|---|
| Hypovolemic (n = 64) | Cardiogenic (n = 10) | Obstructive (n = 14) | Distributive (n = 12) | |
| Pump | Hyper-contractile heart | Hypo-contractile heart | Pericardial effusion | Hyper-contractile heart (early sepsis) |
| Small heart size | Dilated heart size | RV strain | Hypo-contractile heart (late sepsis) | |
| Hyper-contractile heart | ||||
| Tank | Flat IVC | Distended IVC | Distended IVC | Normal/small IVC |
| Flat IJV | Distended IJV | Distended IJV | Normal/small IJV | |
| Peritoneal fluid, pleural fluid | Lung rockets | Absent lung sliding (PTX) | Pleural fluid (empyema) | |
| Pleural effusions | Peritoneal fluid (peritonitis) | |||
| Ascites | ||||
| Pipes | AAA aortic dissection | Normal | DVT | Normal |
Note: Four patients were diagnosed during follow up after admission by RUSH and pan-CT.
Abbreviations: IVC: inferior vena cava; IJV: internal jugular vein; AAA: abdominal aortic aneurysm; RV: right ventricle; DVT: deep vein thrombosis.
Table 4.
Diagnostic reliability of RUSH of each shock type in relation to pan-CT in polytrauma patients.
| Reliability indices | Shock type |
|||
|---|---|---|---|---|
| Hypovolemic (n = 64) | Cardiogenic (n = 10) | Obstructive (n = 14) | Distributive (n = 12) | |
| Sensitivity | 92.2% | 100.0% | 92.9% | 91.7% |
| Specificity | 91.7% | 98.9% | 97.7% | 96.6% |
| PPV | 95.2% | 90.9% | 86.7% | 78.6% |
| NPV | 86.6% | 100.0% | 98.8% | 98.8% |
Note: The sensitivity, specificity, PPV and NPV of RUSH in different types of shock is 94.2%, 96.2%, 87.8% and 96.1% respectively, and thus the accuracy of RUSH was 95.2%.
Abbreviations: NPV: Negative predictive value, PPV: Positive predictive value.
Altogether 42% patients required surgical interventions and ICU admission. Table 5 shows other treatments and the corresponding proportion. Forty-three patients died, 53 fully recovered and 4 transferred to another hospital.
Table 5.
The 28-day outcome of polytrauma patients (n = 100).
| Variables | No. (%) |
|---|---|
| Interventions | |
| Surgical interventions and ICU admission | 42 (42%) |
| Surgical Interventions and inpatient admission | 23 (23%) |
| Inpatient admission under observation | 12 (12%) |
| ICU admission under observation | 19 (19%) |
| Transfer for another hospitala | 4 (4%) |
| Outcome | |
| Died | 43 (43%) |
| Discharged after complete recovery | 53 (53%) |
| Transfer to another hospital (not admitted)a | 4 (4%) |
Transfer to another hospital because no available beds in ICU or relatives refuse to complete the treatment in Suez Canal university hospital.
Discussion
Point of care or focused ultrasound is now an important bedside technique within critical care and emergency medicine to answer time-dependent focused clinical questions. For acute illness, it has some advantages over traditional imaging modalities. It is safe, rapid, non-invasive and comes to the patient's bedside. Bedside sonography has been considered as adjuvant to clinical examinations to rule in or rule out the main diagnoses in specific clinical settings. In general, most focused scans become more positive as the patient deteriorates.10
The present study was carried out on 100 unstable polytrauma patients attended to our hospital. All of them entered resuscitation room once they arrived at the emergency department. We followed the ABCDE principle and treat life threatening conditions if founded. After then patients were subjected to full history and secondary survey, ultrasonography and pan-CT according to clinical picture of the patients. The result of pan-CT scan were considered the standard for comparing with RUSH. Four patients were diagnosed during follow up after admission by RUSH and pan-CT.
Age and gender
In the present study, there were 75 males (75%) and 25 females (25%). Chalya and his colleges11 reported a male to female ratio of 64.6% vs 35.4%. This agrees with another study done by Tham et al.12 which reported male as the predominate gender in polytrauma patients (96.1%).
The mean age of our patients was (27.5 ± 17.8) years. This is in agree with Tham and his colleagues research12 which found that the majority of traumatized patients had a mean age of (32.5 ± 13.1) years. Also many studies reported that the commonest age group involved in accidents was between 20 and 29 years (25%–40%).11, 12 Another study found that the peak age of traumatic patients were in the 4th decade.5 The reason why the adult youth (age 20–40 years old) are involved in accidents can be explained by the fact that the majority of them are involved in productive activities and need to move fast enough from one place to another, which may be a predispose factor for RTAs or crashes. Polytrauma in young adults results in a serious economic burden to the country and family.
Injury mechanism
RTAs accounts for 86% of trauma causes, followed by gunshot (8%) and fall from height (6%). In another study conducted in Mwanza city, Tanzania, the mechanism of injury was RTAs in 62.5%, fall in 15.6%, assault in 11.5%, missed injuries in 18.94% and sports-related injuries in 1.0% patients.11 Similar observation was also noted in many studies.
Cause of unstability
The major cause of unstability in polytrauma patients diagnosed by RUSH is hypovolemic shock (64%), followed by obstructive shock, distributive shock and then cardiogenic shock. This is in agree with Seif et al.'s report10 in 2012, but not match the work by Taha et al.'s in 201713, whose second and third causes are respectively cardiogenic shock and obstructive shock. Anyway hypovolemic shock is still the dominant cause.
In the present study clinical predictors for hypovolemia included respiratory rate, heart rate, systolic blood pressure, diastolic blood pressure, mean arterial blood pressure and the GCS (all p ≤ 0.01, Table 1). In a study performed by Elbaih et al.,14 34% patient had systolic blood pressure below 90 mmHg, those with positive FAST 75% of patients were taken directly to surgical intervention without the need for CT.
Accuracy of RUSH
In addition, Stawicki et al.15 noted that the sensitivity, specificity, PPV and PNV for US and radiography were 86.2% vs 27.6%, 97.2% vs 100%, 89.3% vs 100%, 96.3% vs 83.5%. Moreover, US showed a high consistency with CT in determining the cause of unstability in polytrauma patients, especially with done US by expertise physicians.
In our study the diagnostic reliability of RUSH of each shock type in relation to pan-CT in polytrauma patients has been listed in Table 4; RUSH has a general accuracy of 95.2%. It is most accurate in detecting cardiogenic shock (sensitivity 100.0%, specificity 98.9%, PPV 90.9%, and NPV 100.0%). The result is in agree with Seif and their collage's study.10 In another work conducted by Atkinson et al.16 who prospectively determined the diagnostic accuracy of ultrasonography in 109 trauma patients, of their 25 cases confirmed by CT scan; only 13 (52%) were revealed by chest X-ray (sensitivity 52%; specificity 100%), while 23 (92%) were identified by US (sensitivity, 92%; specificity, 99.4%). We also noted that this is a study that used EFAST for missed chest injuries in Egypt.
In a retrospective study performed by Elbaih et al.14 in Ismailia 2016, 89.8% of patients had negative FAST finding and 10.1% had positive FAST; 3% of patients with negative FAST required therapeutic laparotomy due to instability and positive CT which showed retroperitoneal collection. This is a type that used FAST for blunt abdominal injuries only, not polytrauma patients.
Outcomes
There is a 43% mortality in the present study: the main cause is traumatic brain injury which was the most common associated injuries in unstable polytrauma patients, followed by blunt chest injuries and extremity injuries. Elbaih et al.14 revealed a similar overall mortality rate of 39%. Other 53% patients were discharged after complete recovery and 4% discharged for treatment to another hospital. For the transferred patients, a higher mortality is speculated due to the poor available tools for unstable polytrauma patients and difficulties during transportation from the event.
In disagree with Kauvar et al.'s study,18 regardless of the mechanism of injury, hemorrhage is the leading cause of death following trauma. Injury-induced hemorrhage accounts for the largest proportion of mortality within the first hour in trauma center care, causes 50% of injury-associated death within the first 24 h of trauma care. In mismatch with our study, Elbaih et al.17 studied 600 patients with acute polytrauma in Suez Canal University Hospitals and found that 48 patients were deceased (8%) due to circulatory failure secondary to cardiac penetrating injury in 5 case, massive hemorrhage in 32 cases, and sever lung laceration in 11 cases.
In the present study, 42% unstable polytrauma patients required surgical interventions and ICU admission, 23% needed surgical interventions and inpatient admission, 12% inpatient admission under observation, 19% ICU admission under observation and 4% transfer to another hospital (Table 5). According to Betz and his college,4 8.7% patients were admitted in the ICU, a much lower rate than our study (61%). They found that the need for ICU admission in polytrauma patients with unstability is still associated with a high mortality rate (p = 0.021).
The care of the injured patient remains one of the mainstays of emergency medicine practice. Emergency physicians play a vital role in the stabilization and diagnostic phases of trauma care. In hypotensive patient it is mandatory to rule out other sites of injuries that cause hemorrhagic shock as hemothorax, pelvic or long bone fractures, and to rule out other causes of shock as obstructive shock in cases of cardiac tamponade and pneumothorax, neurogenic shock, and cardiogenic shock. In cases of unstable polytrauma patients there are contraindication to transport these patients to done more investigations unless resuscitations are finished. Little studied have been done for the accuracy of RUSH in polytrauma, so this study is kind of innovative.
Limitations
Although we used a larger sample size than that used in Elbaih et al.,14 the sample size was still small and the study could not be blinded which might have introduced some bias into the results. Additionally, the accuracy of RUSH in polytrauma could not be precisely detected from history and diagnosis made based on clinical manifestations. In cases of unstable polytrauma patients there were contraindication to transport these patients to done more investigations like pan-CT unless resuscitation has been finished, so little studied were done for RUSH in polytrauma and comparison is limited. Also RUSH depends mainly on physician experience, but in our study all the cases were done by authors.
Conclusion
The most frequent cause of unstability in polytrauma patients diagnosed by RUSH is hypovolemic shock (64%). RUSH had a sensitivity, specificity, PPV and NPV in global different types of shock 94.2%, 96.2%, 87.8% and 96.1%respectively. Of the 100 patients, 43% patients died, 53% discharged after complete recovery and 4% discharged for transfer to another hospital. A high rate (42%) of surgical interventions and ICU admission was needed for unstable polytrauma patients.
Recommendations
In order to improve the management process in unstable polytrauma patients, we recommend the following:
-
1.
A high index of suspicion is required when dealing with all polytrauma patients especially the unstable and unconscious patients during primary and secondary survey.
-
2.
Bedside ultrasound should become more integrated in the practice of emergency medicine
-
3.
Application of polytrauma assessment sheet for all polytrauma patients.
-
4.
An experienced consultant/specialist should be available especially with good hand RUSH and should be redistribute to cover 24-h basis.
-
5.
RUSH represents an accurate, cost-effective, safe, and non-invasive method that allows an immediate exclusion over the pan-CT scan and clinical examination and highly recommended to be used as adjunct in the ATLS protocols.
-
6.
Pan-CT scan should be available on 24-h basis and can order easily by ER residences to improve radiological investigations especially if no expertise good hand RUSH available.
-
7.
Another lager study is recommended to confirm results of the present study because of its dependency on operator proficiency and other limitations.
-
8.
The widely used Point of care or Focused ultrasound must be applied and all emergency doctors must successfully complete RUSH course. A larger study is recommended to confirm results of the present study.
Footnotes
Peer review under responsibility of Daping Hospital and the Research Institute of Surgery of the Third Military Medical University.
References
- 1.Amin N.H., Jakoi A., Katsman A. Incidence of orthopedic surgery intervention in a level I urban trauma center with motorcycle trauma. J Trauma. 2011;71:948–951. doi: 10.1097/TA.0b013e31821e601d. [DOI] [PubMed] [Google Scholar]
- 2.Aldemir M., Taçyildiz I., Girgin S. Predicting factors for mortality in the penetrating abdominal trauma. Acta Chir Belg. 2004;104:429–434. [PubMed] [Google Scholar]
- 3.Butcher N., Balogh Z.J. The definition of polytrauma: the need for international consensus. Injury. 2009;40:S12–S22. doi: 10.1016/j.injury.2009.10.032. [DOI] [PubMed] [Google Scholar]
- 4.Betz M., Li G. Injury prevention and control. Emerg Med Clin North Am. 2007;25:901–914. doi: 10.1016/j.emc.2007.06.009. [DOI] [PubMed] [Google Scholar]
- 5.King R.W., Plewa M.C., Buderer N.M. Shock index as a marker for significant injury in trauma patients. Acad Emerg Med. 1996;3:1041–1045. doi: 10.1111/j.1553-2712.1996.tb03351.x. [DOI] [PubMed] [Google Scholar]
- 6.Søreide K. Epidemiology of major trauma. Br J Surg. 2009;96:697–698. doi: 10.1002/bjs.6643. [DOI] [PubMed] [Google Scholar]
- 7.Mateer J., Plummer D., Heller M. Model curriculum for physician training in emergency ultrasonography. Ann Emerg Med. 1994;23:95–102. doi: 10.1016/s0196-0644(94)70014-1. [DOI] [PubMed] [Google Scholar]
- 8.Birnbaum S., Brateman L., Hevezi J. American College of Radiology white paper on radiation dose in medicine. J Am Coll Radiol. 2007;4:272–284. doi: 10.1016/j.jacr.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 9.Dawson B., Trapp R.G. 4th ed. Lange Basic Science; USA: 2004. Basic & clinical biostatistics. [Google Scholar]
- 10.Seif D., Perera P., Mailhot T. Bedside ultrasound in resuscitation and the rapid ultrasound in shock protocol. Crit Care Res Pract. 2012;2012:503254. doi: 10.1155/2012/503254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chalya P.L., Mchembe M., Gilyoma J.M. Missed injuries in multiple trauma patients: a tertiary care experience in Tanzania. East Central African J Surg. 2010;15:39–46. [Google Scholar]
- 12.Tham K.Y., Seow E., Lau G. Pattern of injuries in helmeted motorcyclists in Singapore. Emerg Med J. 2004;21:478–482. [PMC free article] [PubMed] [Google Scholar]
- 13.Taha M., Elbaih A. Pathophysiology and management of different types of shock. Narayana Med J. 2017;6:14–39. [Google Scholar]
- 14.Elbaih A., Ali M., Attia Y. Accuracy of predictive factors and focused assessment with sonography for trauma (FAST) in management of adult blunt abdominal trauma and its outcome. Int J Surg Med. 2016;2:58–63. [Google Scholar]
- 15.Stawicki S.P., Braslow B.M., Panebianco N.L. Intensivist use of hand-carried ultrasonography to measure IVC collapsibility in estimating intravascular volume status: correlations with CVP. J Am Coll Surg. 2009;209:55–61. doi: 10.1016/j.jamcollsurg.2009.02.062. [DOI] [PubMed] [Google Scholar]
- 16.Atkinson P.R., McAuley D.J., Kendall R.J. Abdominal and cardiac evaluation with sonography in shock (ACES): an approach by emergency physicians for the use of ultrasound in patients with undifferentiated hypotension. Emerg Med J. 2009;26:87–91. doi: 10.1136/emj.2007.056242. [DOI] [PubMed] [Google Scholar]
- 17.Elbaih A.H., Abu-Elela S.T. Patterns and outcome of missed injuries in Egyptians polytrauma patients. Int J Surg Med. 2018;4:13–21. [Google Scholar]
- 18.Kauvar D.D., Lefering R., Wade C.E. Impact of hemorrhage on trauma outcome: an overview of epidemiology, clinical presentations and therapeutic considerations. J Trauma. 2006;60:S3–S11. doi: 10.1097/01.ta.0000199961.02677.19. [DOI] [PubMed] [Google Scholar]