Abstract
Purpose
The incidence of hip fractures is increasing within the aging population. Our objective was to identify and quantify the risk factors and develop a predictive model for the in-hospital mortality among hip fracture patients older than 65 years.
Methods
This is a prospective study conducted on 331 hip fracture patients older than 65 years admitted to our hospital from 2011 to 2014. Patients' demographics, prehospitalization residential status, prefracture comorbidity data, anti-aggregant and anticoagulant medication, preoperative hemoglobin value, type of fractures, type of treatments, time to surgery, and complications were recorded.
Results
The average age was 83 years, 73% female, and 57% of them sustained a femoral neck fracture. In 62.8% of patients, the number of pre-fracture baseline comorbidities was ≥2. The in-hospital mortality rate was 11.4%. In multivariate analysis, age over 90 years, congestive heart failure, asthma, rheumatologic disease, lung cancer, and not taking antiaggregant medication were independently associated with in-hospital mortality. A formula and risk stratification scoring for predicting the risk for in-hospital mortality was developed. Risk-adjustment model based on these variables had acceptable accuracy for predicting in-hospital mortality (c-statistic 0.77).
Conclusion
Advanced age, and five prefracture comorbidities have a strong association with in-hospital mortality in a hip fracture patient older than 65 years old. Our predictive model was specifically designed for the old hip fracture population. It has an accuracy similar to other risk models. The specificity, positive predictive value, and negative predictive value are high. In addition, it could discriminate a high risk patient from a low risk patient for in-hospital mortality.
Keywords: Hip fractures, In-hospital mortality, Prognostic factors, Elder population
Introduction
Mortality following hip fractures is high despite advances in surgical and regional anesthesia techniques. Several studies report that the mortality rates after hip fractures in the elderly range from 6% to 9% at 1-month follow-up, 13%–19% at 3 months and 26%–33% at 1 year.1, 2, 3, 4, 5
In-hospital mortality is a vital statistic measuring or recording the rate of death from any cause in hospitalized populations. Some hospitals and health administrators, including our country, have set the in-hospital mortality as a reliable quality indicator of healthcare.6, 7
Giannuolis et al.8 reported that there is a lack of consensus in the established protocols for optimisation of patient care, the definition of early and late surgery, the implementation of rehabilitation protocols, and the length of hospital stay. Thus, it is difficult to compare data from registries with different treatment pathways.
Factors associated with mortality after discharge have been described in published reports.9, 10, 11, 12, 13 Some of them are patient-related as age, sex, co-morbidities; and others are in-hospital-related as surgical delay, type of surgery, anesthetic treatment. Only few prospective14, 15, 16 and retrospective3, 17, 18 studies have reported factors related with the in-hospital mortality. And research regarding risk prediction models is limited.15, 18, 19
The objectives of this study were to analyze prospectively the prognostic factors for in-hospital mortality, and develop a predictive model for in-hospital mortality in hip fracture patients older than 65 years old.
Methods
Inclusion and exclusion criteria
A prospective observational study was designed to evaluate the prognostic factors after hip fractures in the elderly, which has been approved by our institutional ethics committee and informed consent was required. All consecutive patients older than 65 years who sustained a hip fracture admitted at our hospital between January 2011 and December 2014 were potentially eligible. Subjects were excluded from the study if the age was <65 years, found to have a pathological fracture, multiple trauma, bilateral hip fracture, or had a history of previous hip fracture.
At admission, age, sex and prior residence were recorded. Based on ICD-9 classification, fractures were categorized as femoral neck, pertrochanteric and subtrochanteric fractures.
Comorbidities
The presence of a comorbid condition was assigned to a patient when it was present in index or previous admission records. Otherwise, absence of the condition was assigned to the patient. In order to determine the associated comorbidities, we considered those with a greater influence on the prognosis hip fractures. Medical comorbidities included hypertension, atrial fibrilation, heart failure, coronary disease, epilepsy, Parkinson disease, asthma, chronic obstructive pulmonary disease, cerebral vascular disease, dementia, diabetes, rheumatic disease, lung cancer, renal disease, peripheral vascular disease, ulcer disease, liver disease, leukemia, lymphoma, metastatic solid tumor, and AIDS.20 The number of co-morbidities, Charlson comorbidity index (CCI),21 and age-adjusted CCI22 were scored. Anti-aggregant and anticoagulant medication were also recorded.
Preoperative cognitive function was evaluated by a mini-mental test score23 validated for the elderly, where the maximum score was 10 points and a result of 6 or less was suggestive of dementia.
Pre-fracture status of patients
Pre-fracture ambulation status was assessed using the Parker and Palmer score.24 Each item (walking ability indoors, outdoors, and shopping) was rated between 0 (unable) and 3 (full mobility with aids). Ambulation was considered independent when the score was 4 or greater, which indicated that the patient was able to ambulate indoors, outdoors and during shopping with or without walking aids. We graded pre-fracture functional level using the score described by Katz et al.,25 which is based on independence in 6 activities of daily living (ADL). Full independence was defined as the ability to do all 6 ADL without assistance; partial dependence as the ability to do 4 or 5 ADL without assistance; and total dependence as the ability to do 3 ADL or fewer without assistance.
Exam at admission and surgery
From the routine blood preoperative test, hemoglobin (Hb) was extracted. Patients received a blood transfusion if their hemoglobin fell below 80 g/L, or if they became symptomatic with a hemoglobin level of between 80 g/L and 100 g/L.
At admission, patients were examined by the emergency service, which focused on their associated medical pathology. After this initial evaluation, patients were managed on an orthopedic ward with conventional care. They were examined by an anesthesiologist, and an internist if the patient required preoperative stabilization and suitability of previous medical treatment. Time to surgery was defined as the difference between the admission date and operation date. Surgical delay was established by the anesthesiology and reanimation service based on the need for preoperative stabilization, anticoagulation or anti-aggregant treatment. The surgery was not delayed by treatment with 100 mg acetylsalicylic acid.
All procedures were performed in an operating room with laminar flow, with the patient under spinal anesthesia. The surgical procedures were based on facture type. Trochanteric fractures were treated with a proximal femoral nail, undisplaced cervical with screws, and displaced with cemented hemiarthroplasty. Antibiotic prophylaxis (cefazolin, 2 g previously, and 1 g every 8 h, 3 doses, postoperative intravenous; in allergic subjects, vancomycin 1 g previously, and 1 g in a single postoperative intravenous dose) and antithrombotic prophylaxis (enoxaparin 40 U subcutaneously every 24 h for 1 month after intervention) were identical in all cases. A routine 24 h postoperative test of Hb was extracted. Patients were moved to a chair on the first day after the intervention and started to walk using a frame on the second day, if possible. Surgical and medical complications were also collected.
Statistical analysis
Statistical analyses were conducted with SPSS software, version 18.0 (SPSS Inc., Chicago, USA). In order to determine whether the data were significantly different from the normal distribution, a Kolmogorov-Smirnov test was used. We present descriptive statistics (frequencies and medians, as appropriate). All baseline co-morbidities were dichotomous variables, that is, they were either present or absent.
For the purpose of statistical analysis, some variables were redefined. Age was stratified in three groups (less than 84, between 85 and 89, and greater than 90). Type of fracture was dichotomized in intracapsular (femoral neck), or extracapsular (pertrochanteric and subtrochanteric). Comorbidities were dichotomized in having two or fewer and three or more comorbidities. CCI was dichotomized in greater than 2, and equal or less than 2. Age-adjusted CCI was dichotomized in greater than 6, and equal or less than 6. Preoperative Hb was dichotomized in less than 100 g/L, and equal or greater than 100 g/L. Time to surgery was dichotomized in within 2 days, and more than 2 days.
We performed univariate analysis between potential independent association and the outcome of in-hospital mortality. For categorical data we used the chi-square test. For continuous variables, the t-test or non-parametric Mann-Whitney test were used.26 Multivariate analysis was conducted using logistic regression to adjust for possible confounding variables and to identify the independent predictors of outcomes. We start from the variables that showed a significant difference with in-hospital mortality in bivariate analysis. Due to collineartity, we have not entered in multivariate analysis the variables of number of co-morbidities, CCI, and age-adjusted CCI. An optimal multivariate analysis was obtained through a process of selection of backward stepwise variables based on the likelihood ratio test.27 Variables multicollinearity and analysis of influential values were performed. An odds ratio (OR) with 95% confidence interval for risk factors was estimated in the multivariate model. A p value of 0.05 or less was considered significant.
The goodness of fit of the logistic multivariate model was tested using Nagelkerke coefficient and Hosmer-Lemeshow statistic test,28 and overall predictive accuracy of the model was assessed using the c-statistic, which is equivalent to the area under the receiver operating characteristic (ROC) curve.28 As a general rule of thumb, c-statistics between 0.70 and 0.79 are considered acceptable and between 0.80 and 0.89 are considered excellent.29
Results
Over the period of our study, 386 hip fractures were admitted and treated in our hospital. Of them, 55 were excluded for study (35 under 65 years, 15 had a history of previous fracture, and 5 pathological fractures). The remaining 331patients were the subjects of this study.
The mean age was 83.7 years. There were 242 women (73.1%). In total, 286 (86.4%) patients lived in their own home, and 45 patients (13.6%) in a nursing home. Pre-fracture ambulation was dependent in 66 patients (19.9%), and functional level was dependence in 98 patients (29.6%). The most commonly encountered co-morbidities were hypertension, dementia and diabetes. In 208 patients, (62.8%) pre-fracture baseline co-morbidities were equal or greater than 2. Surgical treatment was performed in 310 patients (93.7%), with a mean time to surgery of 3.6 days. Of them, 106 patients (34.2%) were operated within 2 days after admission. No differences were noted between time to surgery and baseline co-morbidities equal or greater than 2 (p = 0.17).
During hospital admission, a total of 79 patients (23.9%) required a blood transfusion, with a mode of 2 packed red blood cells transfused. Regarding the blood transfusion and Hb value at admission, a patient with Hb level less than 100 g/L required preoperative blood transfusion in 23.3% of cases, pre and postoperative blood transfusion in 56.6%, and postoperative transfusion in 20.1%. Detailed data are shown in Table 1.
Table 1.
Characteristics of the study population [data are expressed as n (%)].
| Variables | In-hospital mortality |
p value | OR (95% CI) | ||
|---|---|---|---|---|---|
| Yes | No | ||||
| No. of patients | 331 | 38 | 293 | ||
| Age (years)a* | 83.7 (67–98) | 87.7 (81–97) | 83.2 (67–98) | <0.001 | |
| Age (years)c | |||||
| ≤ 84 | 171 (51.7) | 13 (34.2) | 158 (53.9) | 0.05 | |
| 85-89 | 87 (26.3) | 12 (31.6) | 75 (25.6) | ||
| ≥ 90 | 73 (22.1) | 13 (34.2) | 60 (20.5) | ||
| Sexc | |||||
| Male | 242 (73.1) | 15 (39.5) | 74 (25.3) | 0.07 | |
| Female | 89 (26.9) | 23 (60.5) | 219 (74.7) | ||
| Residencec | |||||
| Home | 286 (86.4) | 33 (86.8) | 253 (86.4) | 0.61 | |
| Nursing | 45 (13.6) | 5 (13.2) | 40 (13.7) | ||
| Fracture patternc | |||||
| Femoral neck | 191 (57.7) | 17 (44.7) | 174 (59.4) | 0.21 | |
| Pertrochanteric | 124 (37.5) | 19 (50.0) | 105 (35.8) | ||
| Subtrochanteric | 16 (4.8) | 2 (5.3) | 14 (4.8) | ||
| Fracture patternc | |||||
| Intracapsular | 191 (57.7) | 17 (44.7) | 174 (59.4) | 0.11 | |
| Extracapsular | 140 (42.3) | 21 (55.3) | 119 (40.6) | ||
| Parker and Palmer scorea* | 5.1 (1–9) | 3.4 (1–9) | 6.3 (4–9) | <0.001 | |
| Dependent mobilityc | 66 (19.9) | 23 (60.5) | 43 (14.7) | <0.001 | 8.9 (4.3–18.4) |
| Katz scorea* | 4.7 (0–6) | 3.5 (0–6) | 5.4 (3–6) | <0.001 | |
| Dependence patientsc | 98 (29.6) | 28 (73.7) | 70 (23.9) | <0.001 | 8.9 (4.1–19.2) |
| Hemoglobin (g/L)a* | 125 (91–142) | 117 (91–128) | 123 (109–142) | 0.004 | |
| Hemoglobin (g/L)c | |||||
| <100 | 30 (9.1) | 9 (23.7) | 21 (7.2) | 0.003 | 4.0 (1.6–9.5) |
| ≥100 | 301 (90.9) | 29 (76.3) | 272 (92.8) | ||
| Anticoagulant medicationc | 23 (7.0) | 3 (7.9) | 20 (6.8) | 0.73 | |
| Antiaggregant medicationc | 83 (25.1) | 2 (5.3) | 81 (27.7) | <0.001 | 0.14 (0.03–0.61) |
| Time to surgery (days)b* | 3.6 ± 2.1 | 4.1 ± 2.8 | 3.5 ± 2.0 | 0.36 | |
| Time to surgery > 2 daysc | 204/310 (65.8) | 15/24 (62.5) | 189/286 (66.1) | 0.44 | |
| Treatmentc | |||||
| Surgical | 310 (93.6) | 24 (63.1) | 286 (97.6) | <0.001 | 23.8 (8.7–64.6) |
| Non-surgical | 21 (6.4) | 14 (36.9) | 7 (2.4) | ||
| Surgical treatmentc | |||||
| Cemented hemiarthroplasty | 177 (57.0) | 15 (62.5) | 162 (56.6) | 0.47 | |
| Screws | 16 (5.1) | 0 | 16 (5.5) | ||
| Proximal femoral nail | 117 (37.9) | 9 (37.5) | 108 (37.9) | ||
* Means and ranges.
Student's t-test.
Mann-Whitney U test.
Chi-square test.
In 139/331 patients (42.0%), there was at least one complication. The most common overall complications were for medical reason, respiratory disease being the most prevalent. Medical complications were pneumonia in 32 patients (9.7%), urinary tract infection in 29 (8.8%), congestive heart failure in 17 (5.1%), pulmonary bronchitis in 17 (5.1%), renal failure in 9 (2.7%), ileus in 7 (2,1%), atrial fibrilation in 6 (1.8%), DVT in 6 (1.8%), stroke in 5 (1.5%), pulmonary embolism in 4 (1.2%), intestinal ischemia in 3 (0.9%), myocardial infarction in 3 (0.9%), ulcer disease in 2 (0.6%). Surgical complications occurred in 4 patients (1.2%), all wound infections: 3 superficial and 1 deep. There was significant difference in the complication rate between patients who had surgery within 2 days and those with more than 2 days (33.0% versus 50.9%, p = 0.001).
Overall, 38 patients died in-hospital. The in-patient mortality rate was 11.5%. There were 23 women (60.5%) and the mean age of death group was 87.7 years. At admission, 33 patients (86.8%) lived in their own home, and 5 patients (13.2%) in a nursing home. Pre-fracture ambulation was dependent in 23 patients (60.5%), and functional level was dependence in 28 patients (73.7%). The most commonly encountered comorbidities were hypertension, congestive heart failure, dementia, and rheumatic diseases. In 32 patients (84.2%) pre-fracture baseline comorbidities were equal or greater than 2. Surgical treatment was performed in 24 patients (63.2%), with a mean time to surgery of 4.1 days. Of them, 9 patients (37.5%) were operated within 2 days after admission. A total of 22 patients (57.9%) required a blood transfusion, with a mode of 4 packed red blood cells transfused. There were complications in 25 patients (65.8%), all medical. These complications were pneumonia in 8, pulmonary embolism in 4, stroke in 3, intestinal ischemia in 3, myocardial infarction in 3, gastric ulcer in 2, and acute renal failure in 2. There was no association between sustaining a complication and risk of mortality (p = 0.42). The mode from admission to in-hospital death was 8 days, and the mean value was 12.1 days (range 8–28 days) (Table 2).
Table 2.
Comorbidities at admission [data are expressed as n (%)].
| Comorbidities | In-hospital mortality |
p value a | OR (95% CI) | ||
|---|---|---|---|---|---|
| Yes | No | ||||
| No. of patients | 331 | 38 | 293 | ||
| Hypertensive disease | 211 (63.8) | 24 (63.2) | 187 (63.8) | 1.0 | |
| Atrial fibrillation | 53 (16.0) | 8 (21.1) | 45 (15.4) | 0.35 | 3.3 (1.6–6.8) |
| Congestive heart failure | 63 (19.0) | 15 (39.5) | 48 (16.4) | 0.002 | |
| Ischemic heart disease | 55 (16.6) | 9 (23.7) | 46 (15.7) | 0.24 | |
| Cerebrovascular disease | 50 (15.1) | 8 (21.1) | 42 (14.3) | 0.33 | |
| Dementia | 97 (29.3) | 11 (29.0) | 86 (29.4) | 1.0 | |
| Epilepsy | 5 (1.5) | 1 (2.6) | 4 (1.4) | 0.45 | |
| Parkinson disease | 23 (7.0) | 3 (7.9) | 20 (6.8) | 0.73 | |
| Chronic obstructive pulmonary disease | 38 (11.5) | 7 (18.4) | 31 (10.6) | 0.17 | |
| Asthma | 11 (3.3) | 5 (13.2) | 6 (2.1) | 0.004 | 7.2 (2.0–25.0) |
| Diabetes | 83 (25.1) | 9 (23.7) | 74 (25.3) | 1.0 | |
| Rheumatologic disease | 15 (4.5) | 11 (29.0) | 4 (1.4) | <0.001 | 29.4 (8.7–98.7) |
| Renal disease | 21 (6.3) | 0 | 21 (7.2) | 0.14 | |
| Lung cancer | 10 (3.0) | 6 (15.8) | 4 (1.4) | <0.001 | 13.5 (3.6–50.5) |
| Peripheral vascular disease | 2 (0.6) | 0 | 2 (0.7) | ||
| Ulcer disease | 4 (1.2) | 1 (2.6) | 3 (1.0) | ||
| Liver disease | 1 (0.3) | 0 | 1 (0.3) | ||
| Leukemia | 0 | 0 | 0 | ||
| Lynfoma | 1 (0.3) | 0 | 1 (0.3) | ||
| Metastatic solid tumor | 0 | 0 | 0 | ||
| AIDS | 0 | 0 | 0 | ||
| Number of comorbidities* | 3.5 (1–7) | 4.5 (3–7) | 3.1 (1–7) | <0.001b | |
| Number of comorbidities> 2 | 208 (62.8) | 32 (84.2) | 176 (60.1) | 0.002 | 3.5 (1.4–8.7) |
| CCI* | 2.4 (1–7) | 3.9 (3–7) | 2.5 (1–7) | <0.001 | |
| CCI > 2 | 129 (39.0) | 26 (68.4) | 103 (35.2) | <0.001 | 3.9 (1.9–8.2) |
| Age-adjusted CCI* | 5.3 (2–10) | 6.4 (4–10) | 5.2 (2–10) | <0.001b | |
| Age-adjusted CCI > 6 | 132 (39.9) | 29 (76.3) | 103 (35.2) | <0.001 | 5.9 (2.7–3.0) |
*Means and ranges.
CCI: Charlson Comorbidity Index.
Chi square test.
Student's t-test.
In multivariate analysis, the significant independent variables for increased in-hospital mortality were age, congestive heart failure, asthma, rheumatologic disease, lung cancer, and not-taking anti-aggregant medication (Table 3).
Table 3.
Multivariate analysis for in-hospital mortality.
| Variables | OR | 95% CI | p value |
|---|---|---|---|
| Age | 1.2 | 1.1–1.3 | 0.004 |
| Sex (Female/Male) | |||
| 2.5 | 0.8–8.1 | 0.112 | |
| Congestive heart failure (No/Yes) | |||
| 6.2 | 1.8–20.9 | 0.003 | |
| Asthma (No/Yes) | |||
| 101.3 | 12.0–851.5 | <0.001 | |
| Rheumatologic disease (No/Yes) | |||
| 73.4 | 13.1–410.1 | <0.001 | |
| Lung cancer (No/Yes) | |||
| 74.9 | 9.1–619.1 | <0.001 | |
| Anti-aggregant medication (No/Yes) | |||
| 150.6 | 4.7–4814.7 | 0.005 |
After univariate and multivariate analysis, we then developed a formula for predicting the risk for in-hospital mortality, as follows.
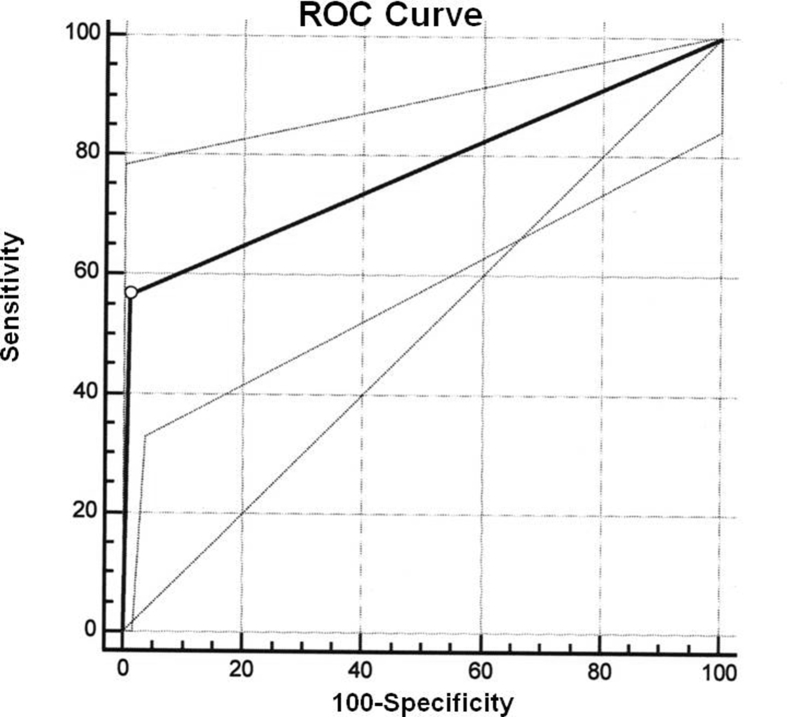
If age is between 85 and 89 the value is 1, and otherwise the value is 0. If age is equal or greater than 90 the value is 1, and otherwise the value is 0. If sex is male the value is 1, and otherwise the value is 0. If congestive heart failure (CHF) is a baseline co-morbidity the value is 1, otherwise the value is 0. If asthma (A) is a baseline co-morbidity the value is 1, otherwise the value is 0. If rheumatologic disease (RD) is a baseline co-morbidity the value is 1, otherwise the value is 0. If lung cancer (LC) is a baseline co-morbidity the value is 1, otherwise the value is 0. If the patient does not take antiaggregant medication the value is 1, otherwise the value is 0. A p value > 0.5 identify those patients with a high risk of in-hospital mortality. In our cohort, the Hosmer-Lemeshow test has a p = 0.93, and the c-statistic 0.77 (95% CI: 0.72–0.82) (Fig. 1). The clinical test values of our model are showed in Table 4.
Fig. 1.
Receiver-operating characteristic (ROC) curve and corresponding area under the curve (AUC) with 95% CI for in-hospital mortality in patients with hip fracture.
Table 4.
Model predicted values.
| 95% CI | ||
|---|---|---|
| Sensitivity (%) | 56.7 | 37.4–74.5 |
| Specificity (%) | 99.0 | 97.0–99.8 |
| True positive (%) | 0.05 | |
| True negative (%) | 87.3 | |
| False positive (%) | 0.009 | |
| False negative (%) | 0.03 | |
| Positive predictive value (%) | 85.0 | |
| Negative predictive value (%) | 95.7 | |
| Positive likelihood ratio | 56.7 | 17.1–177.4 |
| Negative likelihood ratio | 0.43 | 0.3–0.7 |
| 1/Negative likelihood ratio | 2.28 | 1.4–3.3 |
Due to the potential difficulty in using this complex equation in clinical practice, a risk stratification scoring system has been built (Table 5, Table 6).
Table 5.
Risk score of in-hospital mortality after hip fracture.
| Variables | Points |
|---|---|
| Age | |
| 60-69 | 0 |
| 70-79 | 2 |
| 80-89 | 4 |
| 90-99 | 6 |
| 100-109 | 8 |
| Sex | |
| Female | 0 |
| Male | 1 |
| Congestive heart failure | |
| No | 0 |
| Yes | 2 |
| Asthma | |
| No | 0 |
| Yes | 6 |
| Rheumatologic disease | |
| No | 0 |
| Yes | 6 |
| Lung cancer | |
| No | 0 |
| Yes | 6 |
| Anti-aggregant medication | |
| Yes | 0 |
| No | 7 |
Table 6.
Risk score and the incidence of estimated death.
| Point total | Estimate of risk (%) |
|---|---|
| ≤10 | ≤1 |
| 11 | 2.2 |
| 12 | 4.6 |
| 13 | 9.4 |
| 14 | 18.3 |
| 15 | 32.6 |
| 16 | 51.1 |
| 17 | 69.3 |
| 18 | 83.0 |
| 19 | 91.3 |
| ≥20 | >95.5 |
Discussion
The rate of in-hospital mortality in our study was 11.5%. And it is greater than the previously reported rates published in the last 5 years: Belmont et al.14 reported 4.5% rate in 9286 hip fractures, Frost et al.15 6% rate in 1504, Alzahrani et al.16 5% rate in 2178, Chatterton et al.17 6.5% rate in 4426, Johansen et al.30 5.2% rate in 1050, and Tarrant et al.31 4.6% rate in 437. In our country, the rate of in-hospital mortality is around 5%. Sanchez-Hernandez et al.32 showed 5.1% rate in 216 hip fractures managed with conventional care, which was reduced to 2.8% after a multidisciplinary hip fracture program. And Mesa-Lampré et al.33 published 6.9% rate in 494 hip fractures managed in an orthogeriatric unit.
Older age and male gender have been related with increased mortality in many studies. Belmont et al.14 showed 2.3 OR in male sex. Frost et al.15 reported 8.7 OR in patients >90 years, and 2.4 OR in male sex. Chatterton et al.17 published 4.1 OR in patients ≥91 years, and 2.0 OR in male sex. Librero3 reported 8.3 OR in patients >90 years, and 1.0 OR in male sex. In our study, age over 90 had 6.3 OR, and male sex had 2.6 OR for in-hospital mortality.
With regard to the types of fractures, Chatterton et al.17 showed association between intracapsular fracture and in-hospital mortality in univariate analysis with 1.4 OR, but this significance was not reproduced on multivariable analysis. We did not find this association in our cohort, and this was consistent with other study.16
Mental status had no association with in-hospital mortality in our cohort. However, Frost et al.15 reported this association between patients with dementia and those without dementia (24% versus 14%; p = 0.008).
Comorbidities have been described as a main factor with influence on postoperative morbidity and mortality. However, the association with in-hospital mortality following hip-fracture has not been well-documented, and the results are conflicting. Belmont et al.14 reported dialysis as the single greatest predictor in his analysis, with a greater than sixfold increased odds of mortality. Frost et al.15 showed that a number of comorbidities equal or greater than 1 had 2.3 OR for in-hospital mortality. Jiang et al.19 published that the number, type and mix of pre-fracture baseline comorbidities as factors for in-hospital mortality. Chatterton et al.17 reported only the number of comorbidities is independently and significantly associated with increased odds of in-hospital mortality. Neuhaus et al.18 showed the association between a greater value of Charlson index/age-adjusted Charlson index and in-hospital mortality. And similar results were published by Librero et al.3
In our study, congestive heart failure, asthma, rheumatologic disease, lung cancer, not taking antiaggregant medication, number of comorbidities equal or greater than 2, CCI greater than 2, and age-adjusted CCI greater than 6 were associated with in-hospital mortality. In the multivariate analysis, the independent comorbidities for in-hospital mortality after hip fracture in patients older than 65 years were congestive heart failure, asthma, rheumatologic disease, lung cancer, and not taking anti-aggregant medication.
Alzharani et al.16 found greater relative risk of in-hospital mortality for patients admitted from a long-term care facility compared with those who were living independently. We did not find this association in our study. But patients who died in-hospital needed assistance for ambulation and ADL.
Greater mortality is reported in patients with hip fracture non-operatively treated.34, 35 Gregory et al.36 published a 30-days mortality rate of 34% in 22 patients with displaced femoral neck fractures managed non-operatively for medical problems, compared to 4% in patients managed operatively. In our cohort, in-hospital mortality was 66% in patients managed non-operatively due to medical problems, and 7.7% in patients managed operatively, with 23.8 OR for in-hospital mortality if the patient was managed non-operatively.
Timing of surgery for hip fractures and mortality is a long-running controversy with studies showing contradictory results. There are studies that find an association between early surgery within 2 days from admission and mortality,15, 37, 38, 39 but others did not find this association.4, 40, 41 Chatterton et al.17 reported a higher 30-day mortality in patients who had surgery greater than 48 h, but they could not demonstrate a significant relationship. Neither Belmont et al.14 showed this association, although they reported more complications in patients with delayed surgery greater than 2 days. Librero et al.3 published a retrospective population-based cohort study of 56,500 patients of 60-years-old and over with hip fracture in the Spanish National Health System, and they did not find association between time to surgery and in-hospital mortality. In our cohort, time to surgery was similar between patients who died in-hospital and those who did not, but in patients with delayed surgery there were more complications.
To our knowledge, six prediction models for 30-day mortality following hip fracture surgery have been published in the literature. But only three of them were specifically designed for the hip fracture population. Jiang et al.19 developed a multivariate risk model based on a cohort of hip fracture patients. The c-statistic was 0.83. Predicting factors were aged, gender, long-term care residence and ten comorbidities. They established the risk of in-hospital mortality from <1% for patients in the lowest quartile of risk to >15% for those in the highest quartile. Maxwell et al.42 developed a logistic regression from the Nottingham Hip Fracture Score (NFHS), including age, gender, mini-mental test score and number of comorbidities. Between 0 and 4 points is scored for each variable, the total of points resulting in the NHFS. They put forward a formula to predict 30-day mortality. The c-statistic was 0.77. Holt et al.43 included age, ASA score, gender, pre-fracture residence and mobility, and fracture type, as variables associated with 30 and 120-day mortality after hip fracture surgery, using data from the Scottish Hip Fracture Audit. With a logistic regression model they proposed a formula to calculate the predicted mortality. The c-statistic was 0.76. Karres et al.44 evaluated 6 risk models for prediction mortality following hip fracture surgery. The best discrimination was demonstrated by the models that were specifically designed for the hip fracture population. Up to now, NFHS shows most promise of all models. But none of them showed AUC >0.80. They recommended further study to determine the best risk model for predicting mortality following hip fracture surgery.
Our predictive model was specifically designed for hip population. Independent predictive mortality variables were age, and five comorbidities. We added sex as a confusion factor, even is not significant in univariate and multivariate analysis, to build the model. It has a c-statistic of 0.77, lower than 0.80. It has high specificity, high positive predictive value, and high negative predictive value. And it is more than 2-fold increased risk to be classified properly as a patient with low risk for in-hospital mortality. Despite being a recent risk model, the initial results allow us to be optimistic for the future.
The main limitation of the study is the sample size. We have 38 patients with in-hospital mortality for hip fracture. Although, predictive models benefits from large sample size to avoid overfitting, we think that the importance of our model lies in the scarcity of studies about in-hospital mortality after hip fracture. Future multicenter research would increase the sample size, diminish model overfitting, validate our model, and compare our results with other models, especially with the NFHS risk model.
Footnotes
Peer review under responsibility of Daping Hospital and the Research Institute of Surgery of the Third Military Medical University.
References
- 1.Fernandez M.A., Griffin X.L., Costa M.L. Hip fracture surgery: improving the quality of the evidence base. Bone Joint J. 2015;97-B:875–879. doi: 10.1302/0301-620X.97B7.35996. [DOI] [PubMed] [Google Scholar]
- 2.Luger T.J., Kammerlander C., Gosch M. Neuroaxial versus general anaesthesia in geriatric patients for hip fracture surgery: does it matter? Osteoporos Int. 2010;21:S555–S572. doi: 10.1007/s00198-010-1399-7. [DOI] [PubMed] [Google Scholar]
- 3.Librero J., Peiró S., Leutscher E. Timing of surgery for hip fracture and in-hospital mortality: a retrospective population-based cohort study in the Spanish National Health System. BMC Health Serv Res. 2012;12:15. doi: 10.1186/1472-6963-12-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Castronuovo E., Pezzotti P., Franzo A. Early and late mortality in elderly patients after hip fracture: a cohort study using administrative health databases in the Lazio region, Italy. BMC Geriatr. 2011;11:37. doi: 10.1186/1471-2318-11-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Haentjens P., Magaziner J., Colón-Emeric C.S. Meta-analysis: excess mortality after hip fracture among older women and men. Ann Intern Med. 2010;152:380–390. doi: 10.1059/0003-4819-152-6-201003160-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marzo de . 2012. Indicadores de calidad para hospitales del Sistema Nacional de Salud.http://www.calidadasistencial.es/images/gestion/biblioteca/335.pdf [Google Scholar]
- 7.Department of Health and Human Services . AHRQ Pub.; Rockville: 2007. Agency for Healthcare Research and Quality. Guide to Inpatient Quality Indicators: Quality of Care in Hospitals–volume, Mortality, and Utilization. Version 3.1; pp. 56–57.https://www.ahrq.gov/downloads/pub/inpatqi/iqi_guide.pdf [Google Scholar]
- 8.Giannoulis D., Calori G.M., Giannoudis P.V. Thirty-day mortality after hip fractures: has anything changed? Eur J Orthop Surg Traumatol. 2016;26:365–370. doi: 10.1007/s00590-016-1744-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Panula J., Pihlajamäki H., Mattila V.M. Mortality and cause of death in hip fracture patients aged 65 or older: a population-based study. BMC Muscoskel Disord. 2011;12:105. doi: 10.1186/1471-2474-12-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Smith T., Pelpola K., Ball M. Pre-operative indicators for mortality following hip fracture surgery: a systematic review and meta-analysis. Age Ageing. 2014;43:464–471. doi: 10.1093/ageing/afu065. [DOI] [PubMed] [Google Scholar]
- 11.Hu F., Jiang C., Shen J. Preoperative predictors for mortality following hip fracture surgery: a systematic review and meta-analysis. Injury. 2012;43:676–685. doi: 10.1016/j.injury.2011.05.017. [DOI] [PubMed] [Google Scholar]
- 12.Navarrete F.E., Baixauli F., Fenollosa B. Hip fractures in the elderly: mortality predictive factors at one year from surgery. Rev Esp Cir Ortop Traumatol. 2009;53:237–241. [Google Scholar]
- 13.Sánchez-Crespo M.R., Bolloque R., Pascual-Carra A. Relationship between one-year mortality in hip fractures and surgical delay. Rev Esp Cir Ortop Traumatol. 2010;54:34–38. [Google Scholar]
- 14.Belmont P., Garcia E., Romano D. Risk factors for complications and in-hospital mortality following hip fractures: a study using the National Trauma Data Bank. Arch Orthop Trauma Surg. 2014;134:597–604. doi: 10.1007/s00402-014-1959-y. [DOI] [PubMed] [Google Scholar]
- 15.Frost S.A., Nguyen N.D., Black D.A. Risk factors for in-hospital post-hip fracture mortality. Bone. 2011;49:553–558. doi: 10.1016/j.bone.2011.06.002. [DOI] [PubMed] [Google Scholar]
- 16.Alzahrani K., Gandhi R., Davis A. In-hospital mortality following hip fracture care in southern Ontario. Can J Surg. 2010;53:294–298. [PMC free article] [PubMed] [Google Scholar]
- 17.Chatterton B.D., Moores T.S., Ahmad S. Cause of death and factors associated with early in-hospital mortality after hip fracture. Bone Joint J. 2015;97-B:246–251. doi: 10.1302/0301-620X.97B2.35248. [DOI] [PubMed] [Google Scholar]
- 18.Neuhaus V., King J., Hageman M.G. Charlson comorbidity indices and in-hospital deaths in patients with hip fractures. Clin Orthop Relat Res. 2013;471:1712–1719. doi: 10.1007/s11999-012-2705-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jiang H.X., Majumdar S.R., Dick D.A. Development and initial validation of a risk score for predicting in-hospital and 1-year mortality in patients with hip fractures. J Bone Miner Res. 2005;20:494–500. doi: 10.1359/JBMR.041133. [DOI] [PubMed] [Google Scholar]
- 20.Avellana Zaragoza J.A., Ferrández Portal L., Areosa Sastre A. Elsevier: Sociedad Española de Geriatría y Gerontología; Madrid: 2007. Sociedad Española de Geriatría y Gerontología, Sociedad Española de Cirugía Ortopédica y Traumatología. Anciano afecto de fractura de cadera: guía de buena práctica clínica en geriatría.https://www.segg.es/media/descargas/Acreditacion%20de%20Calidad%20SEGG/Residencias/guia_fractura_cadera.pdf [Google Scholar]
- 21.Charlson M., Szatrowski T.P., Peterson J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47:1245–1251. doi: 10.1016/0895-4356(94)90129-5. [DOI] [PubMed] [Google Scholar]
- 22.Charlson M.E., Pompei P., Ales K.L. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 23.Hodkinson H.M. Evaluation of a mental test score for assessment of mental impairment in the elderly. Age Ageing. 1972;41(Suppl 3):i35–i40. doi: 10.1093/ageing/afs148. 2012. [DOI] [PubMed] [Google Scholar]
- 24.Parker M.J., Palmer C.R. A new mobility score for predicting mortality after hip fracture. J Bone Jt Surg Br. 1993;75:797–798. doi: 10.1302/0301-620X.75B5.8376443. [DOI] [PubMed] [Google Scholar]
- 25.Katz S., Ford A.B., Moskowitz R.W. Studies of illness in the aged. The index of ADL: a standardized measure of biological and psychological function. JAMA. 1963;185:914–919. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 26.Zhang Z. Univariate description and bivariate statistical inference: the first step delving into data. Ann Transl Med. 2016;4:91. doi: 10.21037/atm.2016.02.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhang Z. Variable selection with stepwise and best subset approaches. Ann Transl Med. 2016;4:136. doi: 10.21037/atm.2016.03.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hosmer D.W., Lemeshow S. second ed. John Wiley and Sons; New York, NY: 1989. Applied Logistic Regression. [Google Scholar]
- 29.Hanley J.A., McNeil B.J. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982;143:29–36. doi: 10.1148/radiology.143.1.7063747. [DOI] [PubMed] [Google Scholar]
- 30.Johansen A., Mansor M., Beck S. Outcome following hip fracture: post-discharge residence and long-term mortality. Age Ageing. 2010;39:653–656. doi: 10.1093/ageing/afq074. [DOI] [PubMed] [Google Scholar]
- 31.Tarrant S.M., Hardy B.M., Byth P.L. Preventable mortality in geriatric hip fracture inpatients. Bone Jt J. 2014;96-B:1178–1184. doi: 10.1302/0301-620X.96B9.32814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sánchez-Hernández N., Sáez-López P., Paniagua-Tejo S. Results following the implementation of a clinical pathway in the process of care to elderly patients with osteoporotic hip fracture in a second level hospital. Rev Esp Cir Ortop Traumatol. 2016;60:1–11. doi: 10.1016/j.recot.2015.08.001. [DOI] [PubMed] [Google Scholar]
- 33.Mesa-Lampré M.P., Canales-Cortés V., Castro-Vilela M.E. Initial experiences of an orthogeriatric unit. Rev Esp Cir Ortop Traumatol. 2015;59:429–438. doi: 10.1016/j.recot.2015.02.007. [DOI] [PubMed] [Google Scholar]
- 34.Khan S.K., Kalra S., Khanna A. Timing of surgery for hip fractures: a systematic review of 52 published studies involving 291,413 patients. Injury. 2009;40:692–697. doi: 10.1016/j.injury.2009.01.010. [DOI] [PubMed] [Google Scholar]
- 35.Rodriguez-Fernandez P., Adarraga-Cansino D., Carpintero P. Effects of delayed hip fracture surgery on mortality and morbidity in elderly patients. Clin Orthop Relat Res. 2011;469:3218–3221. doi: 10.1007/s11999-010-1756-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gregory J.J., Kostakopoulou K., Cool W.P. One-year outcome for elderly patients with displaced intracapsular fractures of the femoral neck managed non-operatively. Injury. 2010;41:1273–1276. doi: 10.1016/j.injury.2010.06.009. [DOI] [PubMed] [Google Scholar]
- 37.Daugaard C.L., Jørgensen H.L., Riis T. Is mortality after hip fracture associated with surgical delay or admission during weekends and public holidays? A retrospective study of 38,020 patients. Acta Orthop. 2012;83:609–613. doi: 10.3109/17453674.2012.747926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nyholm A.M., Gromov K., Palm H. Time to surgery is associated with thirty-day and ninety-day mortality after proximal femoral fracture: a retrospective observational study on prospectively collected data from the Danish Fracture Database Collaborators. J Bone Jt Surg Am. 2015;97:1333–1339. doi: 10.2106/JBJS.O.00029. [DOI] [PubMed] [Google Scholar]
- 39.Shiga T., Wajima Z., Ohe Y. Is operative delay associated with increased mortality of hip fracture patients? Systematic review, meta-analysis, and meta-regression. Can J Anaesth. 2008;55:146–154. doi: 10.1007/BF03016088. [DOI] [PubMed] [Google Scholar]
- 40.Nordström P., Gustafson Y., Michaëlsson K. Length of hospital stay after hip fracture and short term risk of death after discharge: a total cohort study in Sweden. BMJ. 2015;350:h696. doi: 10.1136/bmj.h696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lizaur-Utrilla A., Martinez-Mendez D., Collados-Maestre I. Early surgery within 2 days for hip fracture is not reliable as healthcare quality indicator. Injury. 2016;47:1530–1535. doi: 10.1016/j.injury.2016.04.040. [DOI] [PubMed] [Google Scholar]
- 42.Maxwell M.J., Moran C.G., Moppett I.K. Development and validation of a preoperative scoring system to predict 30 day mortality in patients undergoing hip fracture surgery. Br J Anaesth. 2008;101:511–517. doi: 10.1093/bja/aen236. [DOI] [PubMed] [Google Scholar]
- 43.Holt G., Smith R., Duncan K. Early mortality after surgical fixation of hip fractures in the elderly: an analysis of data from the scottish hip fracture audit. J Bone Jt Surg Br. 2008;90:1357–1363. doi: 10.1302/0301-620X.90B10.21328. [DOI] [PubMed] [Google Scholar]
- 44.Karres J., Heesakkers N.A., Ultee J.M. Predicting 30-day mortality following hip fracture surgery: evaluation of six risk prediction models. Injury. 2015;46:371–377. doi: 10.1016/j.injury.2014.11.004. [DOI] [PubMed] [Google Scholar]