Abstract
Purpose
Orbital decompression and lower eyelid retraction surgery are traditionally performed separately in staged fashion, which may be unnecessary. Herein, we evaluate the safety and efficacy of combined orbital decompression and lower eyelid retraction surgery.
Methods
Retrospective analysis of patients undergoing combined orbital decompression and lower eyelid retraction surgery in patients with or without Graves orbitopathy, by one surgeon from 2016 to 2017. Patients with previous orbital or lower eyelid surgery were excluded. Surgical technique for orbital decompression included eyelid crease lateral-wall decompression, transconjunctival inferolateral-wall decompression, or transcaruncular medial-wall decompression, or combination. Surgical technique for lower eyelid retraction surgery described previously. Analysis included 34 surgeries (19 patients). Preoperative and postoperative photographs at longest follow-up visit were standardized and analyzed.
Results
Etiologies of lower eyelid retraction included thyroid eye disease (13 patients) and inherited (6 patients). Etiologies of proptosis included thyroid eye disease (13 patients) and inherited with shallow orbits and/or poor maxilla (6 patients). All 34 eyelids demonstrated improvement of lower eyelid position. The mean improvement of marginal reflex distance was 2.4 mm (range, 1.7–2.9 mm). There was one case of mild overcorrection and once case of prolonged chemosis. The average follow-up was 9 months (range, 6 months to 1 year).
Conclusions
This study demonstrates improvement of lower lid position in patients undergoing simultaneous orbital decompression and correction of lower eyelid retraction, irrespective of the etiology of lower eyelid retraction and proptosis or orbital decompression technique. Combined procedures may reduce the number of total procedures, patient anxiety, recovery time, and costs, without compromising the results.
Keywords: Eyelid retraction surgery, Orbital decompression, Thyroid eye disease, Proptosis, Sclera show
Introduction
Exophthalmos and eyelid retraction are typical signs of Graves' orbitopathy but can also occur in patients without thyroid eye disease.1, 2, 3 Because the globe position can affect lower eyelid position, the traditional approach has been staged surgeries with orbital decompression performed first followed later by lower eyelid retraction correction.4 However, multiple staged operations have disadvantages including substantial time commitment by the patient, increased costs to the patient, increased patient anxiety, and additional incisions and healing, resulting in decreased patient satisfaction.
There have been 2 previous studies that described simultaneous orbital decompression and lower eyelid retraction correction. Norris et al.5 reported the benefit of concurrent inferior retractor recession at the time of orbital decompression when closing a swinging-eyelid flap. Kim et al.6 described correction of lower eyelid retraction using a cellular human dermis during orbital decompression, using swinging eyelid approach.
In this study, the author evaluates the safety and efficacy of combined orbital decompression and lower eyelid retraction in patients with or without thyroid eye disease, with no restriction on the technique of orbital decompression.
Methods
In this retrospective study, charts of consecutive patients undergoing combined orbital decompression and lower eyelid retraction surgery in patients with or without Graves orbitopathy, by one surgeon (M.T.) in private practice from March 2016 to February 2017, were reviewed. Patients with previous orbital or lower eyelid surgery were excluded. Informed consent was obtained for each procedure, and the review adhered to the standards of the Declaration of Helsinki and was compliant with the Health Insurance Portability and Accountability Act, adherent to Institutional Review Board (IRB) approval standards.
Surgical technique for orbital decompression has been described previously,1, 2 which included eyelid crease approach lateral wall decompression, transconjunctival inferolateral wall decompression, or transcaruncular medial wall decompression, or combination. Orbital decompression was customized to the individual patient/anatomy and graded based on amount of axial globe reduction needed as follows: inferolateral wall if small amount of decompression required followed by additional lateral wall decompression followed by additional medial wall decompression. For bilateral cases, orbital decompression was done on both eyes in one setting.
Surgical technique for correction of lower eyelid retraction included transconjunctival lower eyelid retractor lysis, canthoplasty, and frost temporary tarsorrhaphy, with or without subperiosteal midface-suborbicularis oculi fat (SOOF) lifting and scar lysis, with or without internal eyelid spacer graft [AlloDerm (LifeCell Corporation, Woodlands, TX)] placement, as described in previous reports.7, 8, 9 In brief, midface lifting is performed if additional lower eyelid anterior lamella (skin) is necessary while spacer graft is used if there is middle lamella shortage.
Analysis included 34 surgeries in 19 patients (15 females, 4 males). Patients with less than 6-months follow-up were excluded. Preoperative and postoperative photographs at longest follow-up visit were used for analysis. All photographs were obtained by the surgeon (M.T.) in standardized fashion with head in straight position and eyes looking directly into the camera. Measurements of the corneal diameter and distance from pupil center to lower lid margin were obtained, standardized, and compared, per previous protocol (Fig. 1).9 All clinical photographs were obtained with written permission by the patient/guardian. Success was measured by patient satisfaction questionnaire and reduction/elimination of sclera show.
Fig. 1.
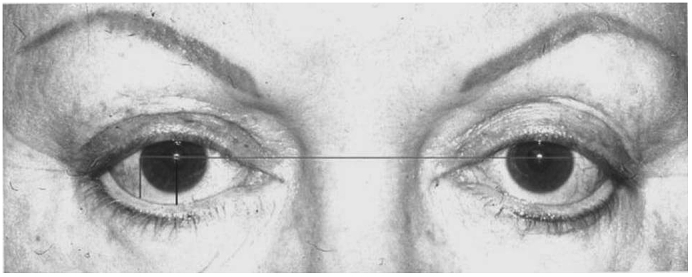
The distances used in our calculations were the corneal diameter of respective sides along with the center of pupil to lower lid margin (central LD) and lateral limbus to lower lid margin (lateral LD) as shown in this figure. (LD: Lid dimension).
Results
Etiologies of lower eyelid retraction included thyroid eye disease (13 patients) and inherited (6 patients). Etiologies of proptosis included thyroid eye disease (13 patients) and inherited with shallow orbits and/or poor maxilla (6 patients, Table 1). Mean age was 42 years old (range, 18–56 years old). Lower eyelid internal spacer graft (Alloderm) was placed in 5 patients. Midface-SOOF lifting was performed in 13 patients. 4 patients underwent lateral wall decompression only (via upper eyelid crease incision), 2 patients underwent medial wall decompression only (via caruncle incision), 4 patients underwent balanced lateral wall and medial wall decompression, 5 patients underwent transconjunctival inferolateral wall (orbit basin) decompression, and 4 patients underwent transconjunctival inferolateral wall (orbit basin) plus transcaruncular medial wall decompression (Table 1). All 19 patients (34 procedures) demonstrated improvement of lower eyelid position and were satisfied with improved eye appearance and dry eye symptoms and elimination or reduction of sclera show. Representative examples are shown in Fig. 2, Fig. 3, Fig. 4, Fig. 5, Fig. 6. Eight eyelids had residual sclera show but significantly improved. There was one case of mild overcorrection. No significant complications, including diplopia, were recorded. There was 1 case of prolonged inferior chemosis, requiring pressure eye patching for relief. The mean preoperative margin reflex distance 2 (MRD2) (central cornea to inferior eyelid margin) was 6.8 mm. The mean postoperative MRD2 was 4.4. The mean improvement or change in eyelid height was 2.4 mm (range, 1.7–2.9 mm). The average follow-up after surgery was 9 months (range, 6 months to 1 year).
Table 1.
Orbital decompression technique: lateral wall done via eyelid crease, inferolateral wall done via transconjunctival, medial wall done via transcaruncular.
| Patient | Etiology of proptosis-retraction | Orbital decompression walls | Lower eyelid retraction: SOOF lift | Lower eyelid retraction: spacer graft | Complications |
|---|---|---|---|---|---|
| 1 | Thyroid eye disease | Lateral + Medial | No | No | None |
| 2 | Thyroid eye disease | Lateral + Medial | No | No | None |
| 3 | Thyroid eye disease | Lateral + Medial | Yes | No | None |
| 4 | Thyroid eye disease | Lateral + Medial | Yes | No | None |
| 5 | Thyroid eye disease | Lateral | Yes | Yes | None |
| 6 | Thyroid eye disease | Lateral | No | No | None |
| 7 | Thyroid eye disease | Lateral | Yes | Yes | None |
| 8 | Thyroid eye disease | Lateral | Yes | No | None |
| 9 | Thyroid eye disease | Medial | Yes | No | None |
| 10 | Thyroid eye disease | Inferolateral | Yes | Yes | None |
| 11 | Thyroid eye disease | Inferolateral | Yes | No | None |
| 12 | Thyroid eye disease | Inferolateral + Medial | Yes | Yes | None |
| 13 | Thyroid eye disease | Inferolateral + Medial | No | No | None |
| 14 | Inherited | Lateral + Medial | Yes | No | None |
| 15 | Inherited | Inferolateral | Yes | Yes | None |
| 16 | Inherited | Inferolateral | Yes | No | None |
| 17 | Inherited | Inferolateral + Medial | No | No | None |
| 18 | Inherited | Inferolateral + Medial | Yes | No | Mild eyelid overcorrection |
| 19 | Inherited | Medial | No | No | Prolonged chemosis |
SOOF: Suborbicularis oculi fat.
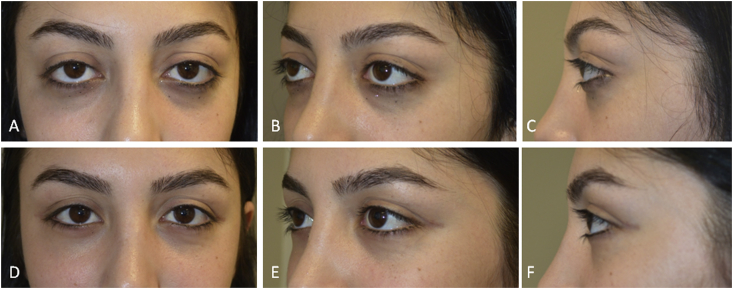
Fig. 2.
25-year-old female, with Graves disease and significant proptosis and lower eyelid retraction. She underwent balanced orbital decompression surgery (lateral wall through upper eyelid crease and medial wall via caruncle) along with transconjunctival lower eyelid retractors lysis, closed canthoplasty, and temporary tarsorrhaphy. A–C) Preoperative; D–F) 6 months postoperative photographs (Patient #1 in Table 1).
Fig. 3.
18-year-old female, with Graves disease and exophthalmos and lower eyelid retraction. She underwent balanced orbital decompression surgery (lateral wall through upper eyelid crease and medial wall via caruncle) along with transconjunctival lower eyelid retractors lysis, closed canthoplasty, and temporary tarsorrhaphy. A–C) Preoperative; D–F) 6 months postoperative photographs (Patient #2 in Table 1).
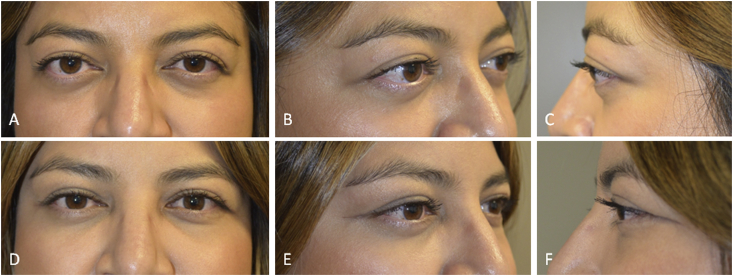
Fig. 4.
34-year-old female, with Graves disease and exophthalmos and lower eyelid retraction. She underwent bilateral balanced lateral and medial wall decompression (lateral wall through upper eyelid crease and medial wall via caruncle) with intraconal fat removal and transconjunctival lower eyelid retractors lysis, tear trough implant placement, midface/suborbicularis oculi fat (SOOF) lift, closed canthoplasty, and temporary tarsorrhaphy. A–C) Preoperative; D–F) 6 months postoperative photographs (Patient #3 in Table 1).
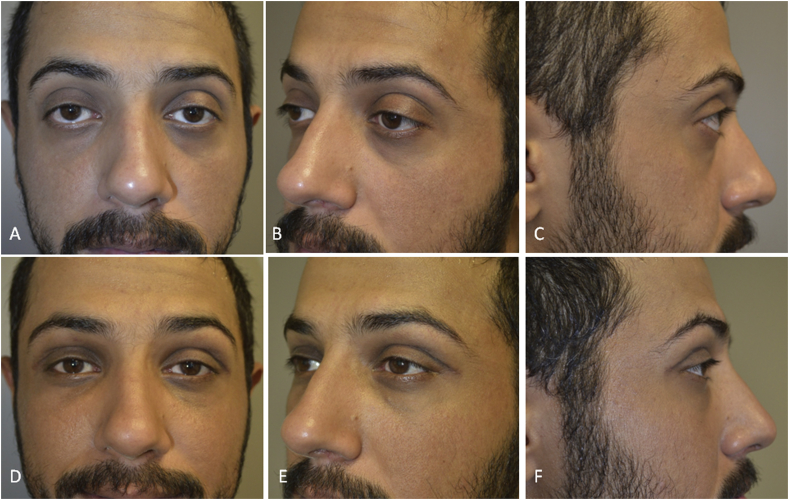
Fig. 5.
31-year-old Middle-Eastern male, complained of “frog eyes” and dry eyes, secondary to congenital shallow orbits, congenital malar eminence hypoplasia and lower eyelid retraction with sclera show. He underwent bilateral balanced lateral and medial wall decompression (lateral wall through upper eyelid crease and medial wall via caruncle) with intraconal fat removal and transconjunctival lower eyelid retractors lysis, tear trough implant placement, midface/suborbicularis oculi fat (SOOF) lift, closed canthoplasty, and temporary tarsorrhaphy, followed later by upper eyelid filler injection. A–C) Preoperative; D–F) 6 months postoperative photographs (Patient #14 in Table 1).
Fig. 6.

53-year-old African-American male, complained of bulging eyes and dry eyes, secondary to shallow orbits and malar eminence hypoplasia and lower eyelid retraction. He underwent inferolateral and medial wall decompression (inferolateral wall through transconjunctival approach and medial wall via caruncle) with intraconal fat removal, plus transconjunctival lower eyelid retractors lysis and open canthoplasty. A) Preoperative; B) 6 months postoperative photographs (Patient #17 in Table 1).
Discussion
Although orbital decompression for exophthalmos alone may improve lower eyelid retraction,10 it is rarely adequate to sufficiently correct the lower eyelid position and eliminate sclera show. Norris et al.5 reported the added benefit of concurrent inferior retractors recession with orbital decompression surgery when closing a swinging-eyelid flap. Recent study by Kim et al.6 compared orbital decompression alone vs. simultaneous orbital decompression and lower eyelid retractors recession vs. simultaneous orbital decompression and lower eyelid surgery with Alloderm spacer graft placement, via swinging eyelid approach, and they also reported significantly improved lower eyelid position when lower eyelid retraction was corrected concurrent with orbital decompression, greater with graft placement.
In this study, the data support the safety and efficacy of combined lower eyelid retraction surgery (with or without internal spacer graft) and orbital decompression, irrespective of etiology of lower eyelid retraction and exophthalmos and irrespective on technique of orbital decompression surgery. Therefore, the benefit of added lower eyelid retraction surgery is not dependent on the incision(s) used for orbital decompression, nor is it dependent on which wall(s) are decompressed. Furthermore, as reported previously,7 the result of lower eyelid retraction surgery may not be dependent on use of internal spacer graft either. The need for spacer graft should be individualized, based on specific criteria, as outlined in previous study.7
There is great patient anxiety, time commitment, healing, and cost with staged orbit and eyelid operations. It is obviously advantageous to have fewer operations. This study is useful to understand the benefits of combined lower eyelid retraction and orbital decompression surgery, without compromise in safety or functional/aesthetic results. In fact, it can even be argued that if the operations were performed separately, the second operation may be complicated by adhesion and contracture of the initial incision site if there was overlap of the operated areas.
There are important limitations to this study that must be taken into account when considering the implications of the data. The patients were not randomized. There were different incisions and walls used for orbital decompression, even though the orbital floor was not decompressed which alone can affect globe/eyelid position. The etiology of eyelid retraction and exophthalmos were varied including thyroid and non-thyroid cases. The lower eyelid correction included some patients that had spacer graft and/or midface lift, while some did not. Due to the retrospective design and different preoperative factors for the surgical decision of each group, there could have been a selection bias. A prospective, comparative controlled study in the future will be helpful in elucidating our findings. Furthermore, although good quality photographic documentation was available at regular intervals for all patients, allowing quantitative and unbiased evaluation, measurements taken from photographs have inherent inaccuracy. Lastly, concurrent lower eyelid retraction surgery at the time of orbital decompression is not recommended for patients with vertical strabismus who would need to undergo inferior rectus operation after orbital decompression.
In conclusion, this study demonstrates improvement of lower lid position in patients undergoing simultaneous orbital decompression and correction of lower eyelid retraction, irrespective of the etiology of lower eyelid retraction and proptosis and irrespective of orbital decompression technique. The results are comparable to previous studies with staged surgeries. The author proposes staged orbital decompression and lower eyelid retraction surgery may be unnecessary, and that lower eyelid retraction correction performed at the time of orbital decompression may reduce the number of total procedures, reduce patient anxiety, reduce recovery time, reduce costs, without compromising the results.
Footnotes
Financial support: None.
Proprietary interests: None.
Peer review under responsibility of the Iranian Society of Ophthalmology.
Author obtained the inform consents from the patients for publishing the photos.
References
- 1.Taban M. Expanding role of orbital decompression in aesthetic surgery. Aesthetic Surg J. 2017;37(4):389–395. doi: 10.1093/asj/sjw248. [DOI] [PubMed] [Google Scholar]
- 2.Goldberg R.A., Hwang M.M., Garbutt M.V., Shorr N. Orbital decompression for non-Graves' orbitopathy: a consideration of extended indications for decompression. Ophthalmic Plast Reconstr Surg. 1995;11(4):245–253. [PubMed] [Google Scholar]
- 3.Lane C.M. Cosmetic orbital surgery. Eye. 2006;20(10):1220–1223. doi: 10.1038/sj.eye.6702386. 2. [DOI] [PubMed] [Google Scholar]
- 4.Shorr N., Seiff S.R. The four stages of surgical rehabilitation of the patient with dysthyroid ophthalmopathy. Ophthalmology. 1986;93(4):476–483. doi: 10.1016/s0161-6420(86)33712-6. [DOI] [PubMed] [Google Scholar]
- 5.Norris J.H., Ross J.J., O'Reilly P., Malhotra R. A review of combined orbital decompression and lower eyelid recession surgery for lower eyelid retraction in thyroid orbitopathy. Br J Ophthalmol. 2011;95(12):1664–1669. doi: 10.1136/bjophthalmol-2011-300698. [DOI] [PubMed] [Google Scholar]
- 6.Kim K.Y., Woo Y.J., Jang S.Y., Lee E.J., Yoon J.S. Correction of lower eyelid retraction using acellular human dermis during orbital decompression. Ophthalmic Plast Reconstr Surg. 2017;33(3):168–172. doi: 10.1097/IOP.0000000000000683. [DOI] [PubMed] [Google Scholar]
- 7.Taban M.R. Lower eyelid retraction surgery without internal spacer graft. Aesthetic Surg J. 2017;37(2):133–136. doi: 10.1093/asj/sjw146. [DOI] [PubMed] [Google Scholar]
- 8.Shorr N. Madame Butterfly procedure with hard palate graft: management of post-blepharoplasty round eye and scleral show. Facial Plast Surg. 1994;10(1):90–118. doi: 10.1055/s-2008-1064559. [DOI] [PubMed] [Google Scholar]
- 9.Taban M., Douglas R., Li T., Goldberg R.A., Shorr N. Efficacy of thick acellular human dermis (alloderm) for lower eyelid reconstruction. Arch Facial Plast Surg. 2005;7(1):38–44. doi: 10.1001/archfaci.7.1.38. [DOI] [PubMed] [Google Scholar]
- 10.Goncalves A.C., Gupta S., Monteiro M.L., Douglas R.S. Customized minimally invasive orbital decompression surgery improves lower eyelid retraction and contour in thyroid eye disease. Ophthalmic Plast Reconstr Surg. 2017;33(6):446–451. doi: 10.1097/IOP.0000000000000825. [DOI] [PubMed] [Google Scholar]