Abstract
Purpose
To evaluate the impact of correct anatomical slab segmentation on foveal avascular zone (FAZ) dimensions in the superficial capillary plexus (SCP) and deep capillary plexus (DCP) using optical coherence tomography angiography (OCTA).
Methods
Participants with healthy retinas were recruited, and 5 × 5 mm OCTA images were acquired using the Canon HS-100 Angio eXpert module. FAZ size was measured in automatically (AS, manufacturer-based) and manually (MS, anatomical-based) segmented OCTA slabs by two experienced graders. FAZ dimensions, inter-rater agreement, and correlation to demographic and retinal parameters were evaluated.
Results
A total of 38 eyes from 20 healthy adult subjects were included in this cross-sectional study. While in AS slabs, the FAZ in the SCP was smaller than in the DCP, in MS images, it was the opposite. MS had a relevant impact on inter-rater agreement of FAZ measurements in the SCP. The FAZ area in both plexus correlated inversely with the central retinal thickness (CRT), irrespective of the segmentation applied. Furthermore, an enlargement of FAZ size in the DCP with increasing age was found. Finally, the FAZ in female participants was significantly larger than in their male counterparts, regardless of the evaluated plexus and chosen segmentation.
Conclusions
Correct anatomical slab segmentation has a significant impact on FAZ size measurements. Not adjusting the segmentation boundaries represents a significant source of error for measuring FAZ area and confounds comparisons across studies as well as OCTA devices.
Keywords: Foveal avascular zone, Optical coherence tomography, Optical coherence tomography angiography, Slab segmentation
Introduction
The foveal avascular zone (FAZ), the capillary-free area within the macula, plays an important role for central vision.1 Changes in the FAZ size can indicate alterations of the microcirculation state of the fovea.2 This biomarker might even have prognostic significance as enlargement of the FAZ, which can be seen in ischemic diseases such as diabetic retinopathy or retinal vein occlusion, and has been shown to be associated with poor visual outcome.3, 4, 5 Therefore, the adequate and precise measurement of FAZ dimensions is of clinical interest.
During the last 50 years, fundus fluorescein angiography (FA) has been the most popular method to evaluate the retinal capillary perfusion and to obtain FAZ measurements.6 However, FA is an invasive operation and requires intravenous administration of the contrast agent fluorescein, for which adverse reactions have been reported. Hence, follow-up examinations to monitor and compare FAZ over time are difficult to obtain.
The introduction of optical coherence tomography (OCT) after the turn of the millennium has revolutionized retinal imaging.7 OCT has become an established non-invasive technique for providing rapidly performed, high-resolution, cross-sectional images of the posterior pole. As OCT devices became faster over time, it is now possible to create flow maps of the retinal microvasculature non-invasively by discrimination of static and non-static (erythrocyte motion) signals. This technological extension is known as OCT angiography (OCTA).8
By now, several devices are commercially available and have been evaluated for image quality, speed, and reproducibility, which are all important characteristics. Moreover, these devices have been assessed with regard to correct segmentation of the different capillary plexus within the retina.9 Herein, we investigated the impact of correct anatomical slab segmentation on FAZ dimensions in the superficial capillary plexus (SCP) as well as deep capillary plexus (DCP) in eyes of healthy adults.
Methods
A cross-sectional study was conducted during the period from March 2017 until May 2017 to measure the FAZ area in healthy adults. The setup of our study was in accordance with the Declaration of Helsinki. Approval by the Institutional Review Board (IRB) at the University of Lübeck (vote reference number 17-008) was given. Informed consent was obtained individually by each participant. Ethnically, all participants were Caucasian and underwent a thorough ophthalmologic examination including best corrected visual acuity (BCVA) in Snellen, slit-lamp biomicroscopy, and OCTA.
Only healthy participants with a BCVA of at least 20/25 and age-appropriate, normal ocular findings without prior ophthalmic surgery were included in our study. Furthermore, the maximal permissible spherical and cylindrical aberration was ±2 and ±1 diopters (D), respectively.
OCTA was performed using the Canon HS-100 (Angio eXpert, OCTA Version 2.0, Tokyo, Japan) without prior pupil dilatation, and 5 × 5 mm macular scans of both eyes were acquired. The device functions at a rate of 70.000 A-scans per second and offers an axial optical resolution of 3 μm. The scanning laser ophthalmoscopy (SLO)-assisted tracking allows better image quality with reduced motion artifacts.
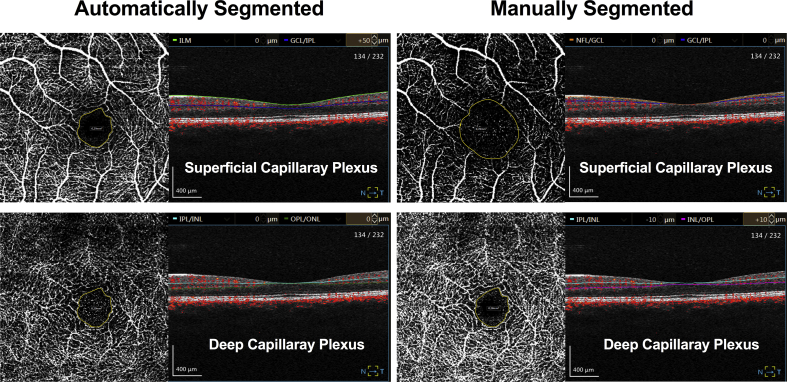
After acquisition, all images were automatically segmented (AS) according to the manufacturer's default settings as well as manually segmented (MS) according to the anatomical-based recommendations published by Spaide and Curcio in all B-scans (Table 1 and Fig. 1).9
Table 1.
Automated and manual segmentation strategies including segmentation values.
| Reference | Vascular plexus | Slab boundary | Anatomic basis | Offseta (μm) | |
|---|---|---|---|---|---|
| Automatically segmented (AS) | Angio eXpert V2.0 | Superficial | Top | ILM | |
| Bottom | GCL | +50 | |||
| Deep | Bottom | IPL | |||
| Bottom | OPL | ||||
| Manually segmented (MS) | Spaide and Curcio | Superficial | Top | ILM | |
| Middle | IPL | ||||
| Deep | Bottom | IPL | −10 | ||
| Top | OPL | +10 |
GCL: Ganglion cell layer; ILM: Internal limiting membrane; IPL: Inner plexiform layer; OPL: Outer plexiform layer.
Offset is the number of μm below (+) or above (−) stated anatomic structure.
Fig. 1.
Optical coherence tomography angiography (OCTA) images of the respective plexus based on the particular slab segmentation.
The FAZ area was manually measured in mm2 by two experienced graders (F.R. and M.K.) in every OCTA image (MS and AS) using the built-in measurement tool of the device. The outline of the innermost macular arcades was manually marked, and the integrated software automatically calculated the enclosed area. The graders were allowed to adjust the brightness and contrast of the images to optimize the measurements.
Data were analyzed using IBM SPSS (Version 24.0, Chicago, IL, USA). The Shapiro-Wilk test was used to check for normality of all obtained data. Inter-rater agreement between OCTA graders was evaluated using concordance correlation coefficient (CCC). Finally, we correlated the various FAZ measurements among each other as well as the foveal thickness by Spearman's correlation analysis. Age- and gender-specific differences were analyzed by linear regression and Mann-Whitney U test. Results with P < 0.05 were considered statistically significant.
Results
A total of 38 eyes from 20 healthy adult subjects were included in this cross-sectional study. These eyes had no relevant artefacts for measurement of FAZ. However, two eyes had to be excluded due to motion artefacts which did not allow adequate measurement of the FAZ. Demographics as well as central retinal thickness (CRT) measurements are reported in Table 2.
Table 2.
Demographics and optical coherence tomography (OCT) measurements.
| Parameter | Mean ± SD | Median (Min; Max) |
|---|---|---|
| Age (years) | 30.66 ± 7.92 | 28.5 (23; 55) |
| Sex (F/M) | 12 (60%)/8 (40%) | |
| Central Retinal Thickness (CRT) (μm) | 278 ± 26 | 277 (246; 347) |
F: Female; M: Male; SD: Standard deviation.
FAZ measurements for the respective plexus and segmentation are listed in Table 3. Based on the Shapiro-Wilk test, our data did not show a normal distribution. Therefore, non-parametric analyses were performed.
Table 3.
Optical coherence tomography angiography (OCTA) foveal avascular zone (FAZ) dimensions.
| FAZ superficial plexus (mm2) Mean ± SD Median (Min; Max) |
AS 0.294 ± 0.099 0.275 (0.13; 0.53) |
MS 0.668 ± 0.239 0.650 (0.25; 1.19) |
Wilcoxon signed rank test P < 0.001 |
| FAZ deep plexus (mm2) Mean ± SD Median (Min; Max) |
AS 0.317 ± 0.119 0.313 (0.10; 0.53) |
MS 0.285 ± 0.108 0.273 (0.08; 0.49) |
Wilcoxon signed rank test P = 0.010 |
| Wilcoxon signed rank test | P = 0.027 | P < 0.001 |
FAZ: Foveal avascular zone; AS: Automatically segmented; MS: Manually segmented.
In AS measurements, the FAZ in the deep plexus was significantly larger than in the superficial one (P = 0.027), whereas in MS measurements, it was the reverse (P < 0.001). While the FAZ in the superficial plexus was quantified significantly larger in MS measurements than in the AS ones (P < 0.001), the FAZ in the deep plexus was measured significantly smaller (P = 0.010).
Evaluating FAZ measurements of both graders with regard to inter-rater reliability by CCC analysis showed that the agreement was the highest for the AS measurements of the FAZ in the superficial plexus and the lowest for the MS measurements of the FAZ in the superficial plexus (Table 4).
Table 4.
Inter-rater agreement as concordance correlation coefficient (CCC), Grader 1 vs. Grader 2.
| FAZ | Grader 1 | Grader 2 | CCC | 95% CI | |
|---|---|---|---|---|---|
| AS | Superficial plexus (mm2) | 0.314 ± 0.110 0.310 (0.08; 0.61) |
0.274 ± 0.095 0.255 (0.12; 0.49) |
0.811 | 0.686 to 0.889 |
| Deep plexus (mm2) | 0.354 ± 0.141 0.340 (0.06; 0.68) |
0.281 ± 0.113 0.295 (0.08; 0.50) |
0.630 | 0.439 to 0.767 | |
| MS | Superficial plexus (mm2) | 0.639 ± 0.276 0.615 (0.15; 1.35) |
0.697 ± 0.277 0.660 (0.20; 1.37) |
0.483 | 0.204 to 0.689 |
| Deep plexus (mm2) | 0.264 ± 0.110 0.245 (0.06; 0.46) |
0.306 ± 0.117 0.300 (0.07; 0.55) |
0.732 | 0.557 to 0.844 | |
FAZ: Foveal avascular zone; AS: Automatically segmented; MS: Manually segmented; CCC: Concordance correlation coefficient; CI: Confidence interval.
Correlating the FAZ measurements among each other, we noted a very strong positive correlation between FAZ AS-Superficial and AS-Deep (r = 0.88; P < 0.01) as well as a strong positive correlation between FAZ MS-Superficial and MS-Deep (r = 0.61; P < 0.01) in the same eye (Table 5).
Table 5.
Spearman correlation analysis of foveal avascular zone (FAZ) measurements in the same eye.
| FAZ area measurements | FAZ area measurements | Correlation coefficient (P-value) |
|---|---|---|
| AS-Superficial | AS-Deep | 0.88 (P < 0.01) |
| MS-Superficial | MS-Deep | 0.61 (P < 0.01) |
| AS-Superficial | MS-Superficial | 0.63 (P < 0.01) |
| AS-Deep | MS-Deep | 0.80 (P < 0.01) |
FAZ: Foveal avascular zone; AS: Automatically segmented; MS: Manually segmented.
Comparing values based on the slab segmentation, a strong positive correlation between FAZ AS-Superficial and MS-Superficial (r = 0.63; P < 0.01) as well as a very strong positive correlation between FAZ AS-Deep and MS-Deep (r = 0.8; P < 0.01) was found.
With regard to foveal thickness, all FAZ measurements showed a significant negative correlation (Table 6).
Table 6.
Spearman correlation analysis of foveal thickness and foveal avascular zone (FAZ) measurements in the same eye.
| Foveal thickness correlated to | Correlation coefficient (P-value) |
|---|---|
| FAZ AS-Superficial | −0.822 (P < 0.01) |
| FAZ MS-Superficial | −0.585 (P < 0.01) |
| FAZ AS-Deep | −0.718 (P < 0.01) |
| FAZ MS-Deep | −0.791 (P < 0.01) |
FAZ: Foveal avascular zone; AS: Automatically segmented; MS: Manually segmented.
Age-dependent linear regression analysis revealed that the older the individual, the bigger the FAZ area (Table 7). However, only measurements of the deep retinal plexus showed a statistically significant correlation.
Table 7.
Age-dependent linear regression analysis.
| FAZ area measurements | Regression coefficient (P-value) |
|---|---|
| AS-Superficial | 0.297 (0.49) |
| MS-Superficial | 0.207 (0.60) |
| AS-Deep | 0.735 (0.03) |
| MS-Deep | 0.693 (0.04) |
FAZ: Foveal avascular zone; AS: Automatically segmented; MS: Manually segmented.
Gender-specific analysis showed that female individuals had a significantly greater FAZ than male individuals for both retinal plexus independent of the applied segmentation protocol (Table 8).
Table 8.
Gender-specific analysis.
| FAZ (mm2) | Female (23 eyes) |
Male (15 eyes) |
Mann-Whitney U Test |
||
|---|---|---|---|---|---|
| Mean ± SD | Median (Min; Max) | Mean ± SD | Median (Min; Max) | ||
| AS-Superficial | 0.34 ± 0.09 | 0.33 (0.16; 0.53) | 0.23 ± 0.06 | 0.23 (0.13; 0.33) | P < 0.01 |
| MS-Superficial | 0.75 ± 0.21 | 0.76 (0.38; 1.19) | 0.54 ± 0.22 | 0.53 (0.25; 1.14) | P < 0.01 |
| AS-Deep | 0.37 ± 0.10 | 0.37 (0.20; 0.53) | 0.24 ± 0.11 | 0.22 (0.10; 0.47) | P < 0.01 |
| MS-Deep | 0.33 ± 0.11 | 0.32 (0.08; 0.49) | 0.22 ± 0.06 | 0.20 (0.14; 0.38) | P < 0.01 |
FAZ: Foveal avascular zone; As: Automatically segmented; MS: Manually segmented.
Discussion
Various studies have characterized the FAZ size and shape in healthy people using OCTA.10, 11, 12, 13 All of these studies used the manufacturer's default settings for slab segmentation into SCP and DCP. However, Spaide and Curcio recently pointed out that the default settings of the commonly used OCTA manufacturers incorrectly segment the central macula of normal eyes.9 As a consequence, images of the SCP and DCP within the central macula are not accurately characterized. Furthermore, Ghasemi Falavarjani et al. also highlighted the relevance of slab segmentation on OCTA measurements.14 Therefore, we aimed at evaluating the impact of correct anatomical segmentation on findings of previous OCTA studies with regard to FAZ dimensions.
Interestingly, previous studies reported the FAZ in the SCP to be smaller than in the DCP. Yet, histological sections of human and macaque eyes clearly indicate that the terminations of the DCP reach further into the center than those of the SCP.9, 15 Therefore, the FAZ in the SCP should be larger than in the DCP as seen in our study after manual segmentation.
Our data suggests that the mean FAZ area ranges from 0.639 ± 0.276 mm2 (Grader 1) to 0.697 ± 0.277 mm2 (Grader 2) in the SCP and from 0.264 ± 0.110 mm2 (Grader 1) to 0.306 ± 0.117 mm2 (Grader 2) in the DCP. The CCC revealed that adjusting the slab segmentation according to correct anatomical boundaries resulted in more disagreement (0.811–0.483) between the two graders with regard to the FAZ in the SCP. Based on the morphology and shape of inner retinal layers the borders of the FAZ in the SCP are not well defined. As the thickness of retinal layers containing the DCP is not as much affected by the existence of the foveal pit, the FAZ in the DCP can be measured more easily. Since the automated slab segmentation according to manufacturer's default settings considers varying amounts of the DCP to be within the SCP, the inter-rater agreement was much higher. In the future, a grader-independent, automatic deep learning based approach for quantification of the FAZ in anatomically segmented slabs might improve reliability.
As it has been reported previously by Linderman et al., we found larger FAZ dimensions in females, although this is in contrast to data from Shahlaee et al.11, 16
Similarly, our observation of an enlargement of the FAZ in the DCP with increasing age is in agreement with that of Iafe et al., but conflicts with the study of Tan et al.17, 18 Age-related increase of the FAZ could be due to atrophic and occlusive changes in the macular capillaries. These differences could be due to different sex, age, and ethnical distribution.
Other studies have investigated the relationship of FAZ dimensions and foveal morphology. Tick et al. found a significant inverse correlation between FAZ dimensions and CRT using FA as well as OCT.1 A similar correlation was found by Shahlaee et al. by OCTA.11 The explanation is given through foveal development and the findings of Springer and Hendrickson, who suggested that the organization of foveal layers is influenced by FAZ size and intraocular pressure.19, 20
Still, it remains debatable whether the current OCTA nomenclature and grouping into two plexus should be reformed, as some recent studies revealed the presence of 2–4 distinct vascular plexuses in the retina, depending on location relative to the optic disc and fovea.21, 22 Yet, others would recommend reporting a single FAZ using a full-thickness retinal slab, which will also be consistent with the original description of the FAZ on fluorescein angiogram, instead of separating individual capillary plexuses. However, until these considerations are incorporated into guidelines and taken into account by manufacturers, correct anatomical segmentation should be performed.
There are several important limitations to this study. The small number of patients and the narrow range of age are important limiting factors. Furthermore, manual measurement of the FAZ area might be subject to inter-grader variability, especially in the SCP because of poorly defined borders. Although not within the scope of the present study, accuracy of the FAZ measurements could have been optimized by taking axial length values into account and correcting image sizes.23
In conclusion, we demonstrate that correct anatomical slab segmentation has a significant impact on FAZ size measurements. Not adjusting the segmentation boundaries represents a significant source of error for measuring FAZ area. While this may not be critical for longitudinal studies comparing multiple scans from one person, these errors limit the ability to compare or combine FAZ area measurements across studies and OCTA devices used.
Acknowledgement
The authors would like to thank “Eyetec GmbH” for providing the “HS-100 OCT” device and “Canon Europe” for evaluating the “Angio eXpert” OCTA module.
Footnotes
Disclosure: No funding was received. The authors do not have any commercial or proprietary interests related to this work.
Peer review under responsibility of the Iranian Society of Ophthalmology.
References
- 1.Tick S., Rossant F., Ghorbel I. Foveal shape and structure in a normal population. Invest Ophthalmol Vis Sci. 2011;52(8):5105–5110. doi: 10.1167/iovs.10-7005. [DOI] [PubMed] [Google Scholar]
- 2.Tan P.E.Z., Yu P.K., Balaratnasingam C. Quantitative confocal imaging of the retinal microvasculature in the human retina. Invest Ophthalmol Vis Sci. 2012;53(9):5728–5736. doi: 10.1167/iovs.12-10017. [DOI] [PubMed] [Google Scholar]
- 3.Minnella A.M., Savastano M.C., Federici M., Falsini B., Caporossi A. Superficial and deep vascular structure of the retina in diabetic macular ischaemia: OCT angiography. Acta Ophthalmol (Copenh) September 2016 doi: 10.1111/aos.13099. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 4.Casselholmde Salles M., Kvanta A., Amrén U., Epstein D. Optical coherence tomography angiography in central retinal vein occlusion: correlation between the foveal avascular zone and visual acuity. Invest Ophthalmol Vis Sci. 2016;57(9) doi: 10.1167/iovs.15-18819. OCT242-246. [DOI] [PubMed] [Google Scholar]
- 5.Balaratnasingam C., Inoue M., Ahn S. Visual acuity is correlated with the area of the foveal avascular zone in diabetic retinopathy and retinal vein occlusion. Ophthalmology. 2016;123(11):2352–2367. doi: 10.1016/j.ophtha.2016.07.008. [DOI] [PubMed] [Google Scholar]
- 6.Novotny H.R., Alvis D.L. A method of photographing fluorescence in circulating blood in the human retina. Circulation. 1961;24:82–86. doi: 10.1161/01.cir.24.1.82. [DOI] [PubMed] [Google Scholar]
- 7.Swanson E.A., Izatt J.A., Hee M.R. In vivo retinal imaging by optical coherence tomography. Opt Lett. 1993;18(21):1864–1866. doi: 10.1364/ol.18.001864. [DOI] [PubMed] [Google Scholar]
- 8.Kashani A.H., Chen C.L., Gahm J.K. Optical coherence tomography angiography: a comprehensive review of current methods and clinical applications. Prog Retin Eye Res. 2017;60:66–100. doi: 10.1016/j.preteyeres.2017.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Spaide R.F., Curcio C.A. Evaluation of segmentation of the superficial and deep vascular layers of the retina by optical coherence tomography angiography instruments in normal eyes. JAMA Ophthalmol. 2017;135(3):259–262. doi: 10.1001/jamaophthalmol.2016.5327. [DOI] [PubMed] [Google Scholar]
- 10.Hussain N., Hussain A. Diametric measurement of foveal avascular zone in healthy young adults using optical coherence tomography angiography. Int J Retina Vitr. 2016;2:27. doi: 10.1186/s40942-016-0053-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shahlaee A., Pefkianaki M., Hsu J., Ho A.C. Measurement of foveal avascular zone dimensions and its reliability in healthy eyes using optical coherence tomography angiography. Am J Ophthalmol. 2016;161:50–55.e1. doi: 10.1016/j.ajo.2015.09.026. [DOI] [PubMed] [Google Scholar]
- 12.Shiihara H., Otsuka H., Terasaki H. Reproducibility and differences in area of foveal avascular zone measured by three different optical coherence tomographic angiography instruments. Sci Rep. 2017;7(1):9853. doi: 10.1038/s41598-017-09255-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ghassemi F., Mirshahi R., Bazvand F., Fadakar K., Faghihi H., Sabour S. The quantitative measurements of foveal avascular zone using optical coherence tomography angiography in normal volunteers. J Curr Ophthalmol. 2017;29(4):293–299. doi: 10.1016/j.joco.2017.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ghasemi Falavarjani K., Al-Sheikh M., Akil H., Sadda S.R. Image artefacts in swept-source optical coherence tomography angiography. Br J Ophthalmol. 2017;101(5):564–568. doi: 10.1136/bjophthalmol-2016-309104. [DOI] [PubMed] [Google Scholar]
- 15.Snodderly D.M., Weinhaus R.S., Choi J.C. Neural-vascular relationships in central retina of macaque monkeys (Macaca fascicularis) J Neurosci Off J Soc Neurosci. 1992;12(4):1169–1193. doi: 10.1523/JNEUROSCI.12-04-01169.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Linderman R., Salmon A.E., Strampe M., Russillo M., Khan J., Carroll J. Assessing the accuracy of foveal avascular zone measurements using optical coherence tomography angiography: segmentation and scaling. Transl Vis Sci Technol. 2017;6(3):16. doi: 10.1167/tvst.6.3.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Iafe N.A., Phasukkijwatana N., Chen X., Sarraf D. Retinal capillary density and foveal avascular zone area are age-dependent: quantitative analysis using optical coherence tomography angiography. Invest Ophthalmol Vis Sci. 2016;57(13):5780–5787. doi: 10.1167/iovs.16-20045. [DOI] [PubMed] [Google Scholar]
- 18.Tan C.S., Lim L.W., Chow V.S. Optical coherence tomography angiography evaluation of the parafoveal vasculature and its relationship with ocular factors. Invest Ophthalmol Vis Sci. 2016;57(9) doi: 10.1167/iovs.15-18869. OCT224-234. [DOI] [PubMed] [Google Scholar]
- 19.Springer A.D., Hendrickson A.E. Development of the primate area of high acuity. 1. Use of finite element analysis models to identify mechanical variables affecting pit formation. Vis Neurosci. 2004;21(1):53–62. doi: 10.1017/s0952523804041057. [DOI] [PubMed] [Google Scholar]
- 20.Springer A.D., Hendrickson A.E. Development of the primate area of high acuity. 2. Quantitative morphological changes associated with retinal and pars plana growth. Vis Neurosci. 2004;21(5):775–790. doi: 10.1017/S0952523804215115. [DOI] [PubMed] [Google Scholar]
- 21.Garrity S.T., Iafe N.A., Phasukkijwatana N., Chen X., Sarraf D. Quantitative analysis of three distinct retinal capillary plexuses in healthy eyes using optical coherence tomography angiography. Invest Ophthalmol Vis Sci. 2017;58(12):5548–5555. doi: 10.1167/iovs.17-22036. [DOI] [PubMed] [Google Scholar]
- 22.Campbell J.P., Zhang M., Hwang T.S. Detailed vascular anatomy of the human retina by projection-resolved optical coherence tomography angiography. Sci Rep. 2017;7:42201. doi: 10.1038/srep42201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sampson D.M., Gong P., An D. Axial length variation impacts on superficial retinal vessel density and foveal avascular zone area measurements using optical coherence tomography angiography. Invest Ophthalmol Vis Sci. 2017;58(7):3065–3072. doi: 10.1167/iovs.17-21551. [DOI] [PubMed] [Google Scholar]