Abstract
Purpose
The present study aims to estimate the prevalence of non-compliance and improper drop administration technique among glaucoma patients and describe common obstacles to medication compliance.
Methods
A hospital-based cross-sectional study, using standardized questionnaire and direct observation by study personnel was conducted among glaucoma patients aged 18 years and above at a tertiary care charitable eye hospital in North India. 151 consecutive glaucoma patients on medical therapy following up at the glaucoma clinics for at least 6 months were recruited. Non-compliance was defined as missing at-least one drop of medication per week and (or) the inability to accurately describe the medication regimen. Study personnel also assessed drop administration technique during application of eye drops by patients treating ophthalmologist-provided information, including measures of disease stability. Factors such as socioeconomic status, presence of caregiver, and number of medications with their effect on compliance were studied using chi-square statistics.
Results
Among 151 patients interviewed, around 49% of patients reported problems in using glaucoma medications, with 16% of them reporting total non-compliance. 35% of patients demonstrated improper drop administration technique. Forgetfulness was cited as the main reason for being non-compliant and had a significant association with non-compliance (P = 0.00). Paying patients were more compliant as compared to subsidized patients (P = 0.05). Disease was more stable in compliant patients compared to non-compliant patients (P = 0.05). No other factor had significant association with compliance (P > 0.05).
Conclusions
Over 50% of the patients surveyed were non-compliant, and 35% demonstrated improper administration technique. Glaucoma patients should be educated on the importance of compliance and aids that minimize forgetfulness, and delivery systems facilitating the delivery of medications to the eye could be considered to enhance patient adherence.
Keywords: Adherence, Glaucoma, Medication, North India
Introduction
Glaucoma contributes to 0.6 million disability-adjusted life years (DALYs) or 1.96% of the overall burden of diseases in India.1 A recent population-based study using modern techniques for detecting glaucoma suggested 11.2 million persons aged 40 years and older are affected due to glaucoma in India.2 Around 27.6 million persons were estimated to have some form of primary angle closure disease. Blindness among primary angle closure glaucoma (PACG) patients affects twice the number than those with primary open angle glaucoma (POAG).2 It is estimated that every eighth individual aged 40 years and over to be affected due to glaucoma or is at risk in the country.2
Glaucoma progression is associated with elevated intraocular pressure (IOP), and lowering IOP has been shown to inhibit the progression of glaucomatous optic nerve damage.3 Topical medications are an effective initial therapy in many patients, but studies have shown that it is often necessary to use multiple topical medications to achieve target IOP. However, a complicating factor to glaucoma treatment is that a large population of patients has been shown to have poor compliance. In a study in South India, 42% of the patients reported one or more problems in using their glaucoma medications, and around 6% of patients reporting less than 100% adherence to their medications during the week before.4
Various barriers to glaucoma treatment compliance exist, and these can be categorized into provider factors, situational/environmental factors, medication regimen factors, and patient factors.5 Glaucoma medication compliance can be determined using self-report, physician report, direct observation, electronic medication monitors, and pharmacy data.6 Self-reported compliance is probably the most commonly employed measure of compliance used in the clinical care of patients. The purpose of this study was to assess barriers to compliance to topical anti-glaucoma medications among glaucoma patients using self-reported compliance, and provide information for improving compliance in tertiary ophthalmic care settings.
Methods
A hospital based cross-sectional study was conducted among glaucoma patients aged 18 years and over at the Glaucoma Clinic at Dr. Shroff's Charity Eye Hospital, from June 2015–Jan 2016. Dr. Shroff's Charity Eye Hospital is a tertiary referral center providing general and subspecialty services and training. The study used a semi-structured questionnaire (See Annexure 1) to assess patient reported problems and adherence to glaucoma medications. However, the method of drop administration was observed by study personnel among patients or care-givers. The questions included demographic profile (socioeconomic status calculation with Kuppuswamy scale7) and sections on barriers to compliance, patient views on glaucoma medications, number of medications, duration of treatment, and disease stability measured by visual field changes over time by treating glaucoma specialist's observation (who were masked to the nature of compliance of the patient).
The study was approved by Institutional Ethics Committee of the hospital, and the patients who received treatment at the hospital participated in the survey. The survey questions were distributed by trained clinical staff to patients who were over 18 years of age presenting to the hospital out-patient department, diagnosed with glaucoma, and had been started on medications. Patients who were on medications for less than six months were excluded from the study. Verbal consent was taken from each of the 151 patients participating in the survey.
The collected data was cleaned, edited, and coded in MS-Excel and analyzed using SPSS (Statistical Package for Social Scientist; version 20, IBM USA). Descriptive statistics in the form of frequencies and percentages were then calculated. The factors associated with non-compliance were explained between independent and dependent variable using chi-square statistics. Statistical significance was considered when the P-value stood at <0.05.
In this study, ‘non-compliance’ stands for missing any of the drops in the last week (both partial and total non-compliance). ‘Partial compliance’ was defined as those missing at least one drop of medication per week and (or) the inability to accurately describe the medication regimen, and ‘total non-compliance’ was defined as not taking any prescribed glaucoma medication for one week. ‘Full compliance’ meant patient's adherence to regimen and was not missing any medication for the last one week. In addition to this, improper drop administration technique was also noted, whether the patient touched the bottle tip to the eye or if the drop missed the eye. In this study, mean defect in best eye on visual field was considered mild [better than −6 Decibel (dB)], moderate (−6 to −12 dB), and severe (worse than −12 dB).
Doctor's perception of disease stability- A patient was defined as being stable if they had stable optic disc findings on subsequent disc photographs, no visual field progression, and IOP maintained in the target range. The disease was termed unstable/progressing if the patient had progression of disc findings (progressive cupping of optic disc, broadening or deepening of retinal nerve fiber layer defects or disc hemorrhage) with progression of glaucomatous field defects on visual field associated with IOP higher than the target pressure.
Results
A total of 151 patients were interviewed. The average age of the participants was 56.11 years, ranging from 18 years to 90 years. Most (66.23%) of the participants were over the age of 50 years, and two-thirds of them were males. Few (16.56%) of the participants were illiterate, though a majority (35.76%) were educated in the university. Most of the participants belonged to either middle or upper lower class as per Kuppuswamy scale.
A significant majority (75.50%) had bilateral involvement of glaucoma in their eyes, and those affected with either eye had almost equal representation in the left or right eye. Most of the patients were on treatment duration of 5 years or less, and around 28% reported a history of glaucoma in the family (Table 1).
Table 1.
Sociodemographic characteristics of participants.
| Sociodemographic data | Number (%) |
|---|---|
| Age | |
| 18–20 years | 2 (1.32) |
| 21–30 years | 4 (2.65) |
| 31–40 years | 12 (7.95) |
| 41–50 years | 39 (25.83) |
| 51–60 years | 34 (26.49) |
| 61–70 years | 40 (26.49) |
| >70 years | 20 (13.25) |
| Sex | |
| Male | 94 (62.5) |
| Female | 57 (37.75) |
| Education | |
| Illiterate | 25 (16.56) |
| Middle-school | 24 (15.89) |
| High school (Class IX, X) | 26 (17.22) |
| Intermediate (Class XI, XII) | 22 (14.57) |
| University & above | 54 (35.76) |
| Socioeconomic class | |
| Lower income | 24 (14.57) |
| Lower middle income | 44 (29.14) |
| Upper middle income | 79 (52.32) |
| Upper income | 6 (3.97) |
| Eyes treated | |
| Bilateral | 114 (75.50) |
| RE | 19 (12.58) |
| LE | 18 (11.92) |
| Duration of treatment | |
| <5 years | 103 (68.21) |
| >5–10 years | 33 (21.85) |
| >10–15 years | 8 (5.30) |
| >15 years | 7 (14.64) |
| Mean defect in best eye | |
| Mild (better than −6 dB) | 91 (60.26) |
| Moderate (−6 to −12 dB) | 31 (20.53) |
| Severe (worse than −12 dB) | 29 (19.21) |
| Family members with glaucoma | 28 (18.54) |
| Patient category | |
| General | 79 (52.31) |
| Paying | 72 (47.68) |
| Total | 151 (100%) |
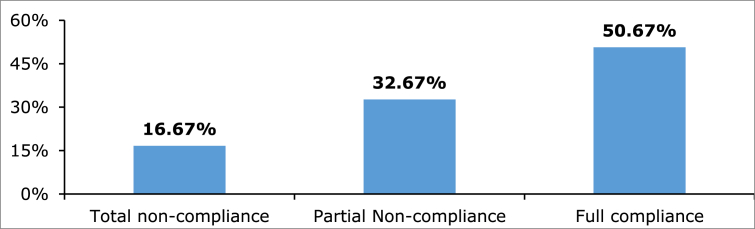
Fifty-four patients (35.76%) were observed to conduct improper drop administration technique. Forty-nine patients touched the eye while instilling the drop, and 5 patients missed the eye. Around 49.33% of the interviewed patients mentioned missing at least some form of the prescribed medication in the past 1 week, with 16.67% of these patients having total non-compliance (Fig. 1). The most cited reason for non-compliance was forgetfulness, followed by outstation travel. Seven patients mentioned costs as one of the problems, while another 7 mentioned the unavailability of the prescribed drug as reasons for non-compliance (Table 2).
Fig. 1.
Level of compliance to anti-glaucoma medications (n-151). The figure describes the patients' level of compliance to anti-glaucoma medications as total non-compliance, partial non-compliance, and full compliance (number-151).
Table 2.
Main reasons given by participants for missing their doses in the week before.
| Reason | Partial non-compliance | Total non-compliance | Total |
|---|---|---|---|
| Forgetfulness | 28 | 5 | 33 (44.59%) |
| Outstation travel | 7 | 3 | 10 (13.51%) |
| Others | 2 | 7 | 9 (12.16%) |
| Run out of drops | 4 | 0 | 4 (5.41%) |
| Cost of medicine | 2 | 5 | 7 (9.46%) |
| Unavailability of drugs | 4 | 3 | 7 (9.46%) |
| Discomfort | 0 | 2 | 2 (2.70%) |
| Laziness | 2 | 0 | 2 (2.70%) |
| TOTAL | 49 | 25 | 74 (100%) |
The level of compliance was compared between various groups of patients. The results showed that only three parameters, i.e. doctors perception of stability of the disease (stable/unstable), cause of non-compliance, and patient category (paying/subsidized) were found to have a significant effect (P < 0.05) on non-compliance. The rest of the variables, such as age (P = 1.00), gender (P = 0.88), education (P = 0.10), socioeconomic status (P = 0.162), improper administration technique (P = 0.61), treatment period (P = 1.00), number of medications (P = 0.632), side-effect of medications (P = 0.54), scheduling difficulty (P = 0.66), presence of caregiver (P = 0.99), and visual defect severity (P = 1.00) did not show any significant effect on non-compliance (Table 3).
Table 3.
Associated factors that determine non-compliance.
| ANOVA | df | SS | MS | F | Significance F | |||
| Regression | 16 | 37.73509934 | 2.358444 | 9.74336E+31 | 0 | |||
| Residual | 134 | 3.24356E-30 | 2.42E-32 | |||||
| Total | 150 | 37.73509934 | ||||||
| Coefficients | Standard error | t Stat | P-value | Lower 95% | Upper 95% | Lower 95.0% | Upper 95.0% | |
| Patient Category- P = Paying; G = Subsidized | 0.0 | 0.0 | −1.9 | 0.06 | 0.0 | 0.0 | 0.0 | 0.0 |
| Age | 0.0 | 0.0 | 0.0 | 1.00 | 0.0 | 0.0 | 0.0 | 0.0 |
| Sex | 0.0 | 0.0 | 0.1 | 0.88 | 0.0 | 0.0 | 0.0 | 0.0 |
| Education | 0.0 | 0.0 | −1.7 | 0.10 | 0.0 | 0.0 | 0.0 | 0.0 |
| Improper drop administration | 0.0 | 0.0 | −0.5 | 0.61 | 0.0 | 0.0 | 0.0 | 0.0 |
| Method of improper technique (A. Missed the eye, B. Contaminated bottle tip, C-Both) | 0.0 | 0.0 | 0.4 | 0.66 | 0.0 | 0.0 | 0.0 | 0.0 |
| Difficulty scheduling | 0.0 | 0.0 | 0.4 | 0.66 | 0.0 | 0.0 | 0.0 | 0.0 |
| Cause of non-compliance | 1.0 | 0.0 | 0.4 | 0.00 | 1.0 | 1.0 | 1.0 | 1.0 |
| Caregiver | 0.0 | 0.0 | 0.0 | 0.99 | 0.0 | 0.0 | 0.0 | 0.0 |
| Side effects | 0.0 | 0.0 | −0.6 | 0.54 | 0.0 | 0.0 | 0.0 | 0.0 |
| No. of administrations | 0.0 | 0.0 | 0.0 | 0.97 | 0.0 | 0.0 | 0.0 | 0.0 |
| How do you feel about drops | 0.0 | 0.0 | −0.6 | 0.54 | 0.0 | 0.0 | 0.0 | 0.0 |
| Treatment duration | 0.0 | 0.0 | 0.0 | 1.00 | 0.0 | 0.0 | 0.0 | 0.0 |
| Family members with glaucoma | 0.0 | 0.0 | −1.0 | 0.34 | 0.0 | 0.0 | 0.0 | 0.0 |
| Mean deviation of visual field | 0.0 | 0.0 | 0.0 | 1.00 | 0.0 | 0.0 | 0.0 | 0.0 |
| Doctor's preception | 0.0 | 0.0 | −0.1 | 0.88 | 0.0 | 0.0 | 0.0 | 0.0 |
ANOVA: Analysis of variance, df: Degrees of freedom, SS: Sum of squares, MS: Mean sum of squares, F: F-statistic, t stat: t-statistic.
Discussion
Glaucoma is the leading cause of irreversible blindness in India. Poor glaucoma awareness8, 9 and under-utilization of ophthalmic services in the country adds to the existing glaucoma burden.10 In such circumstances, the need for increasing compliance of anti-glaucoma medications becomes imperative to manage this condition. This article reports using a sample of 151 patients through interviews and direct observation to explore the factors associated with treatment compliance to glaucoma medications in a tertiary eye care center in North India.
The persistence with glaucoma medications have been found to be varying across several studies. In this study, around 49% of the interviewed patients reported either partial or total non-compliance with their glaucoma medications. However, in other developed and developing countries in Asia, the non-compliance rates have been found to be varied: Israel (29%),11 Hong Kong (63.4%),12 Taiwan (75.8%),13 Saudi Arabia (19.4%),14 and Pakistan (65.5%).15 The prevalence noted in the present study is in concordance with an earlier study done on glaucoma medication compliance in South India.4 The two previous studies on non-compliance conducted in North India reported non-compliance rates of 18% and 58%, respectively.16, 17 It is worrying to note that the earlier study in South India was done in 2009, and even though our study has been conducted seven years later, the percentage of non-compliance among patients with glaucoma remains high. This points to the fact that the knowledge of the ill-effects of medication non-compliance among glaucoma patients remains low, and there is need to ensure that patient education and community awareness on glaucoma needs to be focused in our country.
Review of the studies from Asia show that difficulty opening the bottle,11 presence of a family member,11 older age,4, 14 and belonging to a rural area4, 13 influenced non-compliance rates. Among studies from India, including this present study, factors influencing non-compliance were dose forgetfulness16, 17 and cost.17 Being a developing nation with most of the patients without insurance coverage, we expected cost as a major cause of non-compliance. However, we noted forgetfulness to be the leading cause. Hence, proper counseling of patients regarding the need for compliance with the treatment should be emphasized by eye care providers. Studies18, 19, 20 have shown that electronic reminders could improve adherence to chronic conditions, such as glaucoma. Thus, some of the measures that could probably improve compliance are: making patients and relatives aware about the disease and its sequelae, development of support system to remind patient about drops, and use of electronic reminders such as short message service (SMS) and social media applications.
Although a greater number of patients belonged to middle and lower socioeconomic status as per Kuppuswamy scale, we noted an equal number of patients under paying and subsidized category clinics. Thus, the patients with lower socioeconomic status also opted for paid clinics in our study. There is a possibility that these categories of patients are more concerned about the disease and its implications. This, in turn, may explain higher compliance among paying patients.
The patients who were compliant were noted to be stable in terms of glaucoma progression by the treating ophthalmologist, as compared to the non-compliant patients. Non-compliance to drops leads to glaucoma progression due to inadequate IOP control and subsequent optic nerve damage.21 Konstas et al.22 have reported progression of visual field and disc cupping in non-compliant patients. However, in an evidence based review by Olthoff et al.,23 no strong evidence supporting a relation between non-compliance and progression of visual field (VF) loss was found.
36 percent of our patients were noted to conduct improper drop administration technique. Poor aim can result in under-treatment and disease progression. On the contrary, repeated attempts can lead to excess medication administration and over-treatment, with higher medication costs and increased risk of side effects.23 Contact of the tip of the eye drop container to the eye or skin has consequences that range from contamination24, 25, 26 to trauma. A recent review article concludes that the aids named “Eyot” and “inverted, funnel-shaped guide” have positive objective and/or subjective study outcomes on eye drop instillation.27 Elderly patients and those with musculoskeletal comorbidities may benefit most from instillation aids.28 We also recommend eye drop administration aids to minimize improper drop administration technique.
As a follow-up measure in the hospital, to take care of the problem of non-compliance, we have incorporated counselors to explain glaucoma and the need for compliance to anti-glaucoma medications to patients. The importance of the caregiver is also emphasized to the patients. We also recommended developing patient reminder systems to increase compliance to the hospital authorities.
The study has a few limitations. As described in several studies, the method of using self-report through use of questionnaires could result in an overestimation of the results on compliance. Second, the study was conducted among patients who reported to a clinic for glaucoma treatment. Future research should look at the barriers of medication compliance using a community-based study on patients who have reported to such clinics and later have not returned for follow-up examinations. Lastly, this study was conducted at a single glaucoma clinic in North India; hence the generalizability of the study is limited.
Notwithstanding these limitations, our study has several strengths. The measures of non-compliance through improper administration technique were observed by study personnel of the patients/caregivers putting the eye drops. Around 43% of the study participants reported being from a lower socioeconomic background, which reflects the fact that the hospital is a charitable health facility with tertiary care facilities catering to lower, middle, and upper income category of the Indian population at large. Trained clinical staff administered the questionnaire used on the patients during the interviews.
Our study found a substantial level of non-compliance among patients reporting to a glaucoma clinic in North India. Among the 49% of patients who reported less than 100% adherence to their glaucoma medications in the previous week, around 16% reported total non-compliance. There is need for doctors and glaucoma clinics to pay more attention to the issue of medication non-compliance among patients reporting to health facilities. A support system to remind patients about glaucoma medications is required.
Acknowledgement
As this study did not involve any intervention or experimental component, a waiver for ethics approval was received from the Institutional Ethics Committee of Dr. Shroff's Charity Eye Hospital where this study was conducted.
Footnotes
Conflict of interest: None.
Peer review under responsibility of the Iranian Society of Ophthalmology.
Supplementary data related to this article can be found at https://doi.org/10.1016/j.joco.2017.09.002.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.World Health Organization . Department of Measurement and Health Information, World Health Organization; Geneva: 2009. Estimated DALYs by Causes and Member States. [Google Scholar]
- 2.George R., Ve S.R., Vijaya L. Glaucoma in India: estimated burden of disease. J Glaucoma. 2010;19(6):391–397. doi: 10.1097/IJG.0b013e3181c4ac5b. [DOI] [PubMed] [Google Scholar]
- 3.Schwartz G.F., Burk C., Bennett T., Patel V.D. Adherence and persistence with glaucoma therapy: brimonidine/timolol versus dorzolamide/timolol and various two-bottle combinations. J Clin Exp Ophthalmol. 2012;3:248. [Google Scholar]
- 4.Sleath B.L., Krishnadas R., Cho M. Patient reported barriers to glaucoma medication access, use, and adherence in Southern India. Indian J Ophthalmol. 2009;57(1):63. doi: 10.4103/0301-4738.44495. 38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tsai J.C., McClure C.A., Ramos S.E., Schlundt D.G., Pichert J.W. Compliance barriers in glaucoma: a systematic classification. J Glaucoma. 2003;12(5):393–398. doi: 10.1097/00061198-200310000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Robin A., Grover D.S. Compliance and adherence in glaucoma management. Indian J Ophthalmol. 2011;59(Suppl 1):S93–S96. doi: 10.4103/0301-4738.73693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Oberoi S.S. Updating income ranges for Kuppuswamy's socio-economic status scale for the year 2014. Indian J Public Health. 2015;59(2):156–157. doi: 10.4103/0019-557X.157540. [DOI] [PubMed] [Google Scholar]
- 8.Sathyamangalam R.V., Paul P.G., Ronnie G. Determinants of glaucoma awareness and knowledge in urban Chennai. Indian J Ophthalmol. 2009;57(5):355–360. doi: 10.4103/0301-4738.55073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Krishnaiah S., Kovai V., Srinivas M., Shamanna B.R., Rao G.N., Thomas R. Awareness of glaucoma in the rural population of Southern India. Indian J Ophthalmol. 2005;53(3):205–208. doi: 10.4103/0301-4738.16685. [DOI] [PubMed] [Google Scholar]
- 10.Ramakrishnan R., Nirmalan P.K., Krishnadas R. Glaucoma in a rural population of Southern India: the aravind comprehensive eye survey. Ophthalmology. 2003;110(8):1484–1490. doi: 10.1016/S0161-6420(03)00564-5. [DOI] [PubMed] [Google Scholar]
- 11.Castel O.C., Keinan-Boker L., Geyer O., Milman U., Karkabi K. Factors associated with adherence to glaucoma pharmacotherapy in the primary care setting. Fam Pract. 2014;31(4):453–461. doi: 10.1093/fampra/cmu031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pong J.C.F., Lai J.S.M., Tham C.C.Y., Lam D.S.C. Compliance with topical antiglaucoma medications. HKJ Opthalmol. 2003;9(1):12–15. [Google Scholar]
- 13.Hwang D.K., Liu C.J., Pu C.Y., Chou Y.J., Chou P. Persistence of topical glaucoma medication: a nationwide population-based cohort study in Taiwan. JAMA Ophthalmol. 2014;132(12):1446–1452. doi: 10.1001/jamaophthalmol.2014.3333. [DOI] [PubMed] [Google Scholar]
- 14.Essam O.A., Mousa A.B.A., Humaid A.S.S., Suliman A.H.S.S., Wairimu G.P., Ahmed M. Compliance of glaucoma patients to ocular hypotensive medications among the Saudi population. J Ocular Pharmacol Ther. 2016;32(1):50–54. doi: 10.1089/jop.2015.0052. [DOI] [PubMed] [Google Scholar]
- 15.Ahmad I., Khan B.S., Rehman M. Causes of non-compliance in patients with open angle glaucoma. Opthalmology Update. 2015;13(1):7–9. [Google Scholar]
- 16.Virani S., Rewri P., Dhar M. Difficulties with self instillation of eye drops and its impact on intraocular pressure in glaucoma patients. J Clin Ophthalmol Res. 2015;3(2):87–90. [Google Scholar]
- 17.Tripathi S., Gupta S., Arora V. Socio-demographic determinants of glaucoma medications compliance: a North Indian cross sectional study. Indian J Clin Exp Ophthalmol. 2017;3(1):53–56. [Google Scholar]
- 18.Ho L.Y., Camejo L., Kahook M.Y., Noecker R. Effect of audible and visual reminders on adherence in glaucoma patients using a commercially available dosing aid. Clin Ophthalmol. 2008;2(4):769–772. doi: 10.2147/opth.s3284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Laster S.F., Martin J.L., Fleming J.B. The effect of a medication alarm device on patient compliance with topical pilocarpine. J Am Optom Assoc. 1996;67(11):654–658. [PubMed] [Google Scholar]
- 20.Vervloet M., Linn A.J., Van Weert J.C., de Bakker D.H., Bouvy M.L., Van Diik L. The effectiveness of interventions using electronic reminders to improve adherence to chronic medication: a systematic review of the literature. J Am Med Inform Assoc. 2012;19(5):696–704. doi: 10.1136/amiajnl-2011-000748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Olthoff C.M.1, Schouten J.S., van de Borne B.W., Webers C.A. Noncompliance with ocular hypotensive treatment in patients with glaucoma or ocular hypertension an evidence-based review. Ophthalmology. 2005 Jun;112(6):953–961. doi: 10.1016/j.ophtha.2004.12.035. [DOI] [PubMed] [Google Scholar]
- 22.Konstas A.G.P., Maskaleris G., Gratsonidis S., Sardelli C. Compliance and viewpoint of glaucoma patients in Greece. Eye (Lond) 2000;14 pt(5):752–756. doi: 10.1038/eye.2000.197. [DOI] [PubMed] [Google Scholar]
- 23.Ostergaard Laursen S., Bjerrum P. Timolol eye drop-induced severe bronchospasm. Acta Med Scand. 1982;211(6):505–506. doi: 10.1111/j.0954-6820.1982.tb01990.x. [DOI] [PubMed] [Google Scholar]
- 24.Geyer O., Bottone E.J., Podos S.M., Schumer R.A., Asbell P.A. Microbial contamination of medications used to treat glaucoma. Br J Ophthalmol. 1995;79(4):376–379. doi: 10.1136/bjo.79.4.376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schein O.D., Hibberd P.L., Starck T., Baker A.S., Kenyon K.R. Microbial contamination of in-use ocular medications. Arch Ophthalmol. 1992;110(1):82–85. doi: 10.1001/archopht.1992.01080130084030. [DOI] [PubMed] [Google Scholar]
- 26.Teuchner B., Wagner J., Bechrakis N.E., Orth-Holler D., Nagl M. Microbial contamination of glaucoma eyedrops used by patients compared with ocular medications used in the hospital. Med (Baltimore) 2015;94(8):e583. doi: 10.1097/MD.0000000000000583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Solomon A., Chowers I., Raiskup F., Siganos C.S., Frucht-Prey J. Inadvertent conjunctival trauma related to contact with drug container tips: a masquerade syndrome. Ophthalmology. 2003;110(4):796–800. doi: 10.1016/S0161-6420(02)01967-X. [DOI] [PubMed] [Google Scholar]
- 28.Davies I., Williams A.M., Muir K.W. Aids for eye drop administration. Surv Ophthalmol. 2017;62(3):332–345. doi: 10.1016/j.survophthal.2016.12.009. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.