Abstract
Regional odontodysplasia (RO) is a rare nonhereditary developmental condition usually affecting maxilla and female patients. A few number of articles have used the cone beam computed tomography (CBCT) to describe imaging findings in RO. Thus, this article aims to report unusual imaging findings in a Brazilian child who presented with mandibular RO. A healthy 8-year-old boy was referred for evaluation of an anterior mandibular gingival enlargement. Radiographically, all right mandibular teeth showed wide pulp chambers and shortened roots with thin dentinal walls and open apices, featuring a “ghost teeth“ appearance, which indicated a diagnosis of RO. Missing teeth and altered radiopacity were observed. Cone beam computed tomography provided great insight into RO, allowing to identify gubernaculum tracts (GTs) associated with RO teeth. Fractal analysis of the bone surrounding RO teeth revealed an altered trabecular pattern.
Clinical significance
This case describes a rare developmental teeth-related pathology in a boy who showed unusual features on imaging exams. The CBCT provided the observation of RO tooth-related GTs, probably a new finding added to the international literature regarding RO, as well as the pulp chamber volume characterization of an affected tooth not published yet. In addition, it was observed an altered fractal pattern of the mandibular bone adjacent to RO teeth, which has not been described to date.
How to cite this article: de Sa Cavalcante D, Fonteles CSR, Ribeiro TR, Kurita LM, Pimenta AVM, Carvalho FSR, Costa FWG. Mandibular Regional Odontodysplasia in an 8-year-old Boy showing Teeth Disorders, Gubernaculum Tracts, and Altered Bone Fractal Pattern. Int J Clin Pediatr Dent 2018;11(2):128-134.
Keywords: Cone beam computed tomography, Fractal analysis, Gubernaculum tracts, Mandible, Regional odonto-dysplasia.
INTRODUCTION
Tooth anomalies encompass a heterogeneous group of dental disorders related to genetic, epigenetic, and environmental factor interaction during the morpho- or histodifferentiation stages of tooth development.1 General tooth dysplasia is a dental condition associated with specific disorders of root development, including double teeth, dentin dysplasia type I, hypophosphatasia, and RO.2 This latter is a rare nonhereditary developmental condition usually localized, although it can be generalized or associated with a syndrome that exhibits clinical, and characteristic imaging features.3 Although teeth alterations without other extraoral findings are the usual clinical presentation of RO, it has been reported RO teeth simultaneously with epidermal nevus syndrome,4,5 hypo-phosphatasia,6 hydrocephalus,7 and Hallermann-Streiff syndrome.8 These associations with systemic conditions reinforce the uncertain etiology of the RO, which has been related to other factors, such as a viral infection,9 use of inappropriate medication during pregnancy,10 trauma, nutritional deficiency, infection, and metabolic abnormalities.11
Teeth affected by RO show clinical and radiograph aspects useful as diagnostic criteria.11 Intraoral inspection may reveal hypoplastic malformed teeth with a yellowish/brownish discoloration.12 Plane radiographs are commonly requested for dental evaluation in RO. Panoramic radiograph showed a characteristically unilateral pattern without tendency to cross the midline and a predominant maxillary involvement. Radiographically, the affected teeth have a poor definition between hard dental tissues, as well as aspects resembling an arrested development including large pulp chambers (ghostlike appearance) and short roots with open apices.13-17
Imaging exams may also demonstrate delayed eruption of affected teeth, failure in the dental eruption process, tooth agenesis,18 or even altered mandibular radioden-sity.19 These features are important for the differential diagnosis with hereditary conditions, including dentin dysplasia, dentinogenesis imperfecta, and amelogenesis imperfecta.20
Conventional radiographs possess restrictions in terms of imaging details and three-dimensional evaluation. In RO, CT is a useful exam to provide a tri-dimensional tooth morphology, assessment of the pulp chamber volume, tissue density, and localization of dysplasia and hypocal-cification.21 However, there is only one published case of RO evaluated on CBCT to date.8
Thus, the aim of this paper is to describe teeth imaging findings observed on panoramic radiograph and CBCT from a male patient with mandibular RO, bone fractal properties not published yet, and to add a new feature of this condition.
CASE REPORT
An 8-year-old boy was referred to the Pediatric Dental Clinic at the Federal University of Ceará (Fortaleza, Ceará, Brazil) for the evaluation of a gingival enlargement of unknown duration situated in the anterior mandibular region associated with tooth pain. The patient showed normal stature and no other physical abnormalities. History of trauma, infectious diseases, or nutritional disorders was absent. Medical abnormalities or dental alterations were not observed among other members of his family. Intraoral examination revealed right mandibular malformed and hypoplastic teeth, deciduous teeth (inferior central incisors) associated with a localized gingival enlargement covered by a fibrous tissue, and teeth 83, 84, and 85 affected by caries. All other teeth were present and normal. At the first visit, clinical data were collected to establish the treatment plan and imaging exams were analyzed. However, after the return visit, the patient did not attend for dental follow-up.
Panoramic radiograph (Fig. 1) showed primary mandibular teeth (81, 82, 83, 84, and 85), tooth 46 and dental germs (43, 44, and 45) with “ghost teeth” appearance due to the presence of extensive pulp chamber demarcated by thin layer of mineralized tissue in which it was not possible to observe a clear definition of enamel and dentin. In addition, it was revealed agenesis of lower incisor teeth (41 and 42) and images suggesting dental caries on teeth 84, 85, and 46.
Fig. 1:

Panoramic radiograph in which deciduous and permanent teeth in the right hemimandibular show large pulp chambers. Agenesis of teeth 41 and 42 is observed, as well as images suggestive of caries on teeth 84, 85, and 46
A CBCT scan revealed: (1) a hypodense area suggestive of a periapical lesion associated with tooth 81, which did not show signs of dental caries (Fig. 2A); (2) remarkable difference in the pulp chamber space when comparing deciduous teeth 84 and 74 (Figs 2B and C); (3) crows of the affected teeth surrounded by large hypodense areas (Fig. 3A); (4) presence of GTs associated with unerupted teeth 43 and 45 (Fig. 3). In order to provide pulp chamber volume, it was used the semi-automated segmentation tool of the free access ITK-SNAP 3.4.0® software (Cognitica, Philadelphia, USA). It was observed that the volume of the RO-positive tooth pulp chamber (Fig. 4) was approximately 25% greater than the volume of the opposite unaffected tooth (Fig. 5). In addition, RO tooth was of approximately 28% shorter length than the corresponding contralateral tooth (Fig. 6).
Figs 2A to C:
Transverse images of CBCT showing the tooth 82 with a “ghost tooth” aspect associated with a hypodense image (white arrow) suggestive of periapical lesion (A); in addition, a significant difference between the space of the pulp chambers of primary teeth 84 (B) and 74 (C)
Figs 3A and B:

Presence of GTs (white arrows) associated with tooth germs 43 and 45. Also, enlargement of the pericoronal follicle space relative to the tooth germ 43
Figs 4A to D:
Window of the ITK-SNAP program in which the space of the pulp chamber of the healthy tooth 33 was segmented and rendered, getting a volume of 96.33 mm3. Axial, sagittal, three-dimensional, and coronal views are shown
Figs 5A to D:
Window of the ITK-SNAP program showing the three-dimensional reconstruction of the space of the pulp chamber of the tooth 43 with OR, which obtained a volume of 128.7 mm3. Axial, sagittal, three-dimensional, and coronal views are shown
Fig. 6:
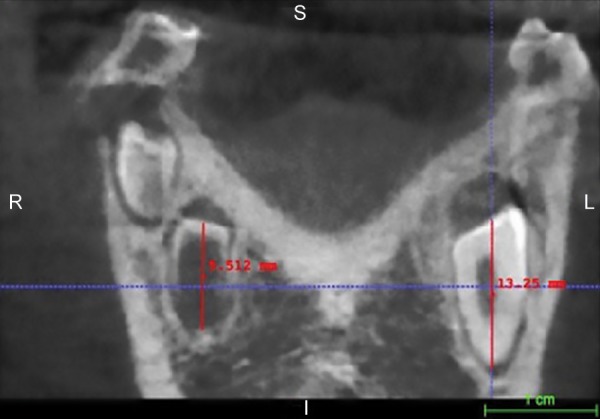
Linear measurements performed in the ITK-SNAP program in which the RO tooth presented a length of 9.512 mm while its contralateral tooth showed a length of 13.25 mm
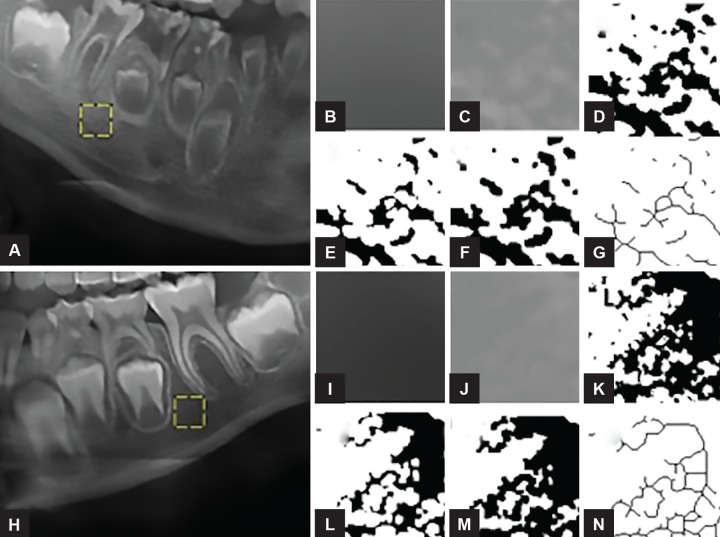
Imaging exams also showed an intense radiopacity pattern in the region of the trabecular bone surrounding adjacent RO teeth in comparison with the unaffected con-tralateral region. Thus, a fractal analysis was performed aiming to analyze the mandibular trabecular pattern of both regions (Fig. 7). ImageJ version 1.38x software (US National Institutes of Health, http://rsb.info.nih.gov/ nih-image) was used to perform this analysis. Initially, a region of interest (ROI) of 100 × 100 pixels above the mandibular canal was selected between the mesial roots of the tooth 46 and the unerupted tooth 45. This ROI was similarly selected for both right and left mandibular sides. Then, the procedures for calculating the fractal dimension followed the methodology described by White and Rudolph.22 The bone surrounding RO teeth had a fractal dimension value of 1,171, differing from the unaffected bone (value of 1.309), which indicates an altered bone microarchitecture in the mandibular region containing the RO teeth.
Figs 7A to N:
Sequence to obtain the fractal dimension. Regions of interest represented by yellow boxes (A,H) were cropped, duplicated, and a Gaussian filter with a sigma value of 35 (B,I) was applied. Then, the blurred image was subtracted from the original image and 128 was added (C, J). The resulting image was binarized (D, K), eroded (E, L), dilated (F, M) and skeletonized (G, N) in order to calculate the fractal dimension value
DISCUSSION
The RO is a rare developmental dental anomaly with an estimated prevalence of less than 1:1,000,000, and approximately 140 cases have been published to date.13,15 According to Crawford and Aldred,11 this condition probably was firstly described in 1934 by Hitchin under the term “arrested tooth development.” Zegarelli et al23 introduced the term “odontodysplasia” followed by Pindborg, who designed the term “regional” in order to reflect the clinical finding of involvement in a region or a segment of the affected jaw.11 Since its first publication, a few number of Brazilian studies have been performed. A PubMed search of the literature using the keywords “regional odontodysplasia” and “Brazil” disclosed only 10 publications to date, which emphasizes the importance of the present report.
As recorded at the dental appointment for patient evaluating, RO-related teeth are often small, discolored, hypocalcified, and hypoplastic, which reflect their abnormal development regarding dental hard tissues originated from the embryonic layers ectoderm and mesoderm.16 In addition, this case is uncommon since RO has been published mainly among females (1.7:1) and with a predilection to maxillary localization (1.6:1).24 Presently, it was reported a right mandibular RO in a young boy. According to Babu et al,20 there have been only four published cases of RO-positive teeth in mandibular site. In jaws, the third and fourth quadrants have been described as the lower involved regions followed by the first and second quadrants.24
In the field of the oral and maxillofacial radiology, imaging findings are strong diagnostic criteria for RO,11 typically featuring remarkable alterations in dental tissues of deciduous and/or permanent teeth. This case showed teeth with hypoplastic, hypocalcified crown, poor contrast between dental tissues demonstrated by a low radiodensity, shortened roots with wide open apices, pericoronal radiolucency representing an enlarged dental follicle, and large pulp chambers giving a “ghost teeth” appearance.11,17,21,23,25,26 In addition, it was observed the absence of right permanent mandibular central and lateral incisors, an unusual finding according to Tervonen et al.24 These authors compiled epidemiological data of RO published in the international literature up to 2002 and found only 10.7% of missing teeth in the studied sample of 138 cases. Similarly to the present case, Ganguly and Ramesh27 reported an unusual case of mandibular RO associated with the absence of left lower and lateral incisors which was observed on periapical radiographs.
It has been considered that unknown local factors affecting the tooth-forming tissues during development are probably involved in RO origin.28 We believe this fact may explain the occurrence of GTs in RO, which were firstly described in the present report. GT consists of an intraosseous tooth-related eruption pathway containing a fibrous tissue band (gubernacular cord) that communicates the tooth bud follicle with its overlying oral mucosa, appearing in the lingual alveolar bone of the deciduous related tooth.29-31 In the present case, CBCT characterized the gubernacular cord-containing pathway as a tooth bud-related hypodense channel as described by Ide et al.31 Interestingly, these authors reported a case of a mandibular adenomatoid odontogenic tumor arising in an 11-year-old girl which was associated with a GT on computed tomography. Oda et al32 showed a close spatial relationship and/or association between odontomas and the GT on CBCTs, noticeable in exams of individuals less than 20 years of age (>96%). Indeed, benign odontogenic tumors represent a heterogeneous group of lesions developed from the various components of the odontogenic apparatus,33 which encompass some similarity with RO regarding etiopathogenesis. In addition, the present case emphasizes the importance of CBCT to accurately detect GT, since panoramic radiography usually does not reveal this finding.30
Conventional radiographs usually describe teeth affected by RO with a typical hypoplastic morphology, encompassing large pulp chambers enclosed by thin layers of enamel and dentin.14 The digital imaging and communications (DICOM) files originated from CBCT scans and subsequently analyzed by ITK-SNAP software would be more advantageous in order to accurately provide a detailed pulp chamber description as performed in the present case. The use of ITK-SNAP as a valid tool for a tri-dimensional evaluation has been observed in several studies, including volumetric assessment of Stafne’s defects,28 forensic anthropology population characterization,34,35 monitoring of endodontic treatment outcome in periapical lesions,36 and orthodontics purposes.37,38 Throughout ITK-SNAP software, a morphological difference between mandibular RO tooth and its nonaffected contralateral tooth was presently evident, since affected tooth showed a pulp chamber volume 25% greater than the normal tooth. Clinically, this finding may predispose to dental fragility, as well as to enhance the occurrence and progression of periapical lesions. In addition, the same tooth evaluated in the present case showed a reduction in length (approximately 28%) when compared with the tooth 33. This aspect may reflect the clinical evidence of a delayed tooth development since RO tooth resembled Nolla’s stage 6, while normal tooth matched Nolla’s stage 7.39,40
Another interesting and rare finding observed in the present case was the mandibular bone altered radiopacity adjacent to the RO teeth. This finding was first reported by Ansari et al19 in a 9-year-old nonsyndromic girl who presented a “ghostly” appearance in the right mandible on panoramic radiography; thus, this case is the second one regarding adjacent RO teeth-related sclerotic bone with coarse and irregular trabeculae. Among syndromes featuring RO, there has been published only one case revealing a mandibular bone pattern abnormality to date, which was published by some of the present authors.8 Damasceno et al8 showed an altered maxillomandibular trabecular pattern associated with a generalized odontodysplasia on CBCT of a 5-year-old girl diagnosed with Hallermann-Streiff syndrome. In both situations (syndromic and nonsyn-dromic RO), a combination of some aspects appears to explain the altered radiopacity in areas surrounding the altered teeth: (1) since teeth displaying RO features do not have a normal development, it may be reasonable disturbance on the alveolar ridge formation process followed by an alteration in the alveolar bone density;19 (2) an abnormal periosteal appositional bone formation or a defective endosteal resorption could alter the mandibular bone trabeculae organization.41 In a clinical point of view, this radiographically altered bone should be carefully analyzed when planning osseointegrated implants placement.17
In order to provide new additional information to the current literature regarding RO and its possible effect on the mandibular bone pattern, it was performed a comparative fractal analysis in the present case. Fractal analysis to evaluate bone microarchitecture has been conducted in panoramic radiograph studies. Presently, fractal dimension was calculated by the box-counting method as published by White and Rudolph.22 It has been demonstrated that this methodology is able to show differences in bone density on panoramic radiographs of patients with osteoporosis,42,43 hyperparathyroidism,44 sickle cell anemia,45 chronic kidney disease,46 and osteogenesis imperfecta.47 Apparently, it is the first study using fractal analysis for characterization purposes in a mandibular case of OR. In this patient, a reduced fractal dimension value was obtained in the trabecular bone area affected by RO when compared with the corresponding nonaffected counter lateral mandibular region. This finding reflects an apparent trabecular bone scarcity, which agrees with Ansari et al19 who described the opaque appearance on the panoramic radiograph as a lower density of the alveolar bone around the affected teeth.
In brief, this case describes a rare developmental teeth-related pathology in a boy who showed unusual features on imaging exams, including mandibular involvement and missing permanent teeth. Cone beam computed tomography provided the observation of RO tooth-related GTs, probably a new finding added to the international literature regarding RO, as well as the pulp chamber volume characterization of an affected tooth not published yet. In addition, it was observed an altered fractal pattern of the mandibular bone adjacent to RO teeth, which has not been described to date.
CONCLUSION
The case is unusual, in that the RO occurred in the mandible. Findings in CBCT and panoramic radiograph revealed peculiarities not yet reported in articles. Therefore, it is important to identify and describe these imaging characteristics, in order to add new information to the current international literature.
CLINICAL SIGNIFICANCE
This case describes a rare developmental teeth-related pathology in a boy who showed unusual features on imaging exams. The CBCT provided the observation of RO tooth-related GTs, probably a new finding added to the international literature regarding RO, as well as the pulp chamber volume characterization of an affected tooth not published yet. In addition, it was observed an altered fractal pattern of the mandibular bone adjacent to RO teeth, which has not been described to date.
Footnotes
Source of support: Nil
Conflict of interest: None
REFERENCES
- 1.Laganà G, Venza N, Borzabadi-Farahani A, Fabi F, Danesi C, Cozza P. Dental anomalies: prevalence and associations between them in a large sample of non-orthodontic subjects, a cross-sectional study. BMC Oral Health. 2017 Mar;17(1):62. doi: 10.1186/s12903-017-0352-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Luder HU. Malformations of the tooth root in humans. Front Physiol. 2015 Oct;27(6):307. doi: 10.3389/fphys.2015.00307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mathew A, Dauravu LM, Reddy SN, Kumar KR, Venkatara-mana V. Ghost teeth: regional odontodysplasia of maxillary first molar associated with eruption disorders in a 10-year-old girl. J Pharm Bioallied Sci. 2015 Aug;7(Suppl 2):S800–S803. doi: 10.4103/0975-7406.163570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Slootweg PJ, Meuwissen PR. Regional odontodysplasia in epidermal nevus syndrome. J Oral Pathol. 1985 Mar;14(3):256–262. doi: 10.1111/j.1600-0714.1985.tb00489.x. [DOI] [PubMed] [Google Scholar]
- 5.Prakash SM, Gupta S, Kamarthi N, Goel S. Inflammatory linear verrucous epidermal nevus and regional odontodysplasia: a rare sorority. Indian J Dent. 2015 Oct-Dec;6(4):203–206. doi: 10.4103/0975-962X.160348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Russell K, Yacobi R. Generalized odontodysplasia concomitant with mild hypophosphatasia—a case report. J Can Dent Assoc. 1993 Feb;59(2):187–190. [PubMed] [Google Scholar]
- 7.Dahllöf G, Lindskog S, Theorell K, Ussisoo R. Concomitant regional odontodysplasia and hydrocephalus. Oral Surg Oral Med Oral Pathol. 1987 Mar;63(3):354–357. doi: 10.1016/0030-4220(87)90204-0. [DOI] [PubMed] [Google Scholar]
- 8.Damasceno JX, Couto JL, Alves KS, Chaves CM Jr, Costa FW, Pimenta Ade M, Fonteles CS. Generalized odontodysplasia in a 5-year-old patient with Hallermann-Streiff syndrome: clinical aspects, cone beam computed tomography findings, and conservative clinical approach. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014 Aug;118(2):e58–e64. doi: 10.1016/j.oooo.2014.04.013. [DOI] [PubMed] [Google Scholar]
- 9.Reade PC, Radden BG, Barke JJ. Regional odontodyspla-sia. A review and a report of two cases. Aust Dent J. 1974 Jun;19(3):152–161. doi: 10.1111/j.1834-7819.1974.tb05032.x. [DOI] [PubMed] [Google Scholar]
- 10.Lustmann J, Ulmansky M. Structural changes in odonto-dysplasia. Oral Surg Oral Med Oral Pathol. 1976 Feb;41(2):193–202. doi: 10.1016/0030-4220(76)90231-0. [DOI] [PubMed] [Google Scholar]
- 11.Crawford PJ, Aldred MJ. Regional odontodysplasia: a bibliography. J Oral Pathol Med. 1989 May;18(5):251–263. doi: 10.1111/j.1600-0714.1989.tb00394.x. [DOI] [PubMed] [Google Scholar]
- 12.Al-Tuwirqi A, Lambie D, Seow WK. Regional odontodyspla-sia: literature review and report of an unusual case located in the mandible. Pediatr Dent. 2014 Jan;36(1):62–67. [PubMed] [Google Scholar]
- 13.Jahanimoghadam F, Pishbin L, Rad M. Clinical, radiographic, and histologic evaluation of regional odontodysplasia: a case report with 5-year follow-up. J Dent (Shiraz) 2016 Jun;17(2):159–163. [PMC free article] [PubMed] [Google Scholar]
- 14.Spini TH, Sargenti-Neto S, Cardoso SV, Souza KC, de Souza SO, de Faria PR, Loyola AM. Progressive dental development in regional odontodysplasia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007 Sep;104(3):e40–e45. doi: 10.1016/j.tripleo.2007.02.027. [DOI] [PubMed] [Google Scholar]
- 15.Rashidian A, Afsharian Zadeh M, Azarshab M, Zarrabian T. Regional odontodysplasia: report of a case. J Dent (Shiraz) 2013 Dec;14(4):197–200. [PMC free article] [PubMed] [Google Scholar]
- 16.Thimma Reddy BV, Vinay Reddy KK, Sunil B, Pujita R, Kiran K, Kranthi KR. Regional odontodysplasia. J Indian Soc Pedod Prev Dent. 2010 Oct-Dec;28(4):315–318. doi: 10.4103/0970-4388.76166. [DOI] [PubMed] [Google Scholar]
- 17.Hamdan MA, Sawair FA, Rajab LD, Hamdan AM, Al-Omari IK. Regional odontodysplasia: a review of the literature and report of a case. Int J Paediatr Dent. 2004 Sep;14(5):363–370. doi: 10.1111/j.1365-263X.2004.00548.x. [DOI] [PubMed] [Google Scholar]
- 18.Fanibunda KB, Soames JV. Odontodysplasia, gingival manifestations, and accompanying abnormalities. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996 Jan;81(1):84–88. doi: 10.1016/s1079-2104(96)80154-5. [DOI] [PubMed] [Google Scholar]
- 19.Ansari G, Reid JS, Fung DE, Creanor SL. Regional odon-todysplasia: report of four cases. Int J Paediatr Dent. 1997 Jun;7(2):107–113. doi: 10.1111/j.1365-263x.1997.tb00288.x. [DOI] [PubMed] [Google Scholar]
- 20.Babu NS, Smriti RJ, Pratima DB. Regional odontodyspla-sia: report of an unusual case involving mandibular arch. Contemp Clin Dent. 2015 Apr-Jun;6(2):237–239. doi: 10.4103/0976-237X.156054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Matsuyama J, Tanaka R, Iizawa F, Sano T, Kinoshita-Kawano S, Hayashi-Sakai S, Mitomi T. Clinical and radiographic findings and usefulness of computed tomographic assessment in two children with regional odontodysplasia. Case Rep Dent. 2014 Aug;2014:764393. doi: 10.1155/2014/764393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.White SC, Rudolph DJ. Alterations of the trabecular pattern of the jaws in patients with osteoporosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999 Nov;88(5):628–635. doi: 10.1016/s1079-2104(99)70097-1. [DOI] [PubMed] [Google Scholar]
- 23.Zegarelli EV, Kutscher AH, Applebaum E, Archard HO. Odontodysplasia. Oral Surg Oral Med Oral Pathol. 1963 Feb;16:187–193. doi: 10.1016/0030-4220(63)90031-8. [DOI] [PubMed] [Google Scholar]
- 24.Tervonen SA, Stratmann U, Mokrys K, Reichart PA. Regional odontodysplasia: a review of the literature and report of four cases. Clin Oral Investig. 2004 Jun;8(2):45–51. doi: 10.1007/s00784-003-0245-0. [DOI] [PubMed] [Google Scholar]
- 25.van der Wal JE, Rittersma J, Baart JA, van der Waal I. Regional odontodysplasia: report of three cases. Int J Oral Maxillofac Surg. 1993 Dec;22(6):356–358. doi: 10.1016/s0901-5027(05)80667-8. [DOI] [PubMed] [Google Scholar]
- 26.Ibrahim Mostafa M, Samir Taha N, Ismail Mehrez MA. Generalised versus regional odontodysplasia: diagnosis, transitional management, and long-term follow-up—a report of 2 cases. Case Rep Dent. 2013 Feb;2013:519704. doi: 10.1155/2013/519704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ganguly R, Ramesh A. Regional odontodysplasia: a case of progressive tooth development. J Indian Soc Pedod Prev Dent. 2012 Apr-Jun;30(2):176–178. doi: 10.4103/0970-4388.100010. [DOI] [PubMed] [Google Scholar]
- 28.Gerlach RF, Jorge J Jr, de Almeida OP, Coletta RD, Zaia AA. Regional odontodysplasia. Report of two cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998 Mar;85(3):308–313. doi: 10.1016/s1079-2104(98)90014-2. [DOI] [PubMed] [Google Scholar]
- 29.Carollo DA, Hoffman RL, Brodie AG. Histology and function of the dental gubernacular cord. Angle Orthod. 1971 Oct;41(4):300–307. doi: 10.1043/0003-3219(1971)041<0300:HAFOTD>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 30.Nishida I, Oda M, Tanaka T, Kito S, Seta Y, Yada N, Fujita Y, Saeki K, Morikawa K, Matsumoto-Takeda S et al. Detection and imaging characteristics of the gubernacular tract in children on cone beam and multidetector computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015 Aug;120(2):e109–e117. doi: 10.1016/j.oooo.2015.05.001. [DOI] [PubMed] [Google Scholar]
- 31.Ide F, Mishima K, Kikuchi K, Horie N, Yamachika S, Satomura K, Shimoyama T, Sakashita H, Saito I, Kusama K. Development and growth of adenomatoid odontogenic tumor related to formation and eruption of teeth. Head Neck Pathol. 2011 Jun;5(2):123–132. doi: 10.1007/s12105-011-0253-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Oda M, Miyamoto I, Nishida I, Tanaka T, Kito S, Seta Y, Yada N, Saeki K, Matsumoto-Takeda S, Wakasugi-Sato N et al. A spatial association between odontomas and the gubernaculum tracts. Oral Surg Oral Med Oral Pathol Oral Radiol. 2016 Jan;121(1):91–95. doi: 10.1016/j.oooo.2015.10.014. [DOI] [PubMed] [Google Scholar]
- 33.Ringer E, Kolokythas A. Bone margin analysis for benign odontogenic tumors. Oral Maxillofac Surg Clin North Am. 2017 Aug;29(3):293–300. doi: 10.1016/j.coms.2017.03.006. [DOI] [PubMed] [Google Scholar]
- 34.Ge ZP, Yang P, Li G, Zhang JZ, Ma XC. Age estimation based on pulp cavity/chamber volume of 13 types of tooth from cone beam computed tomography images. Int J Legal Med. 2016 Jul;130(4):1159–1167. doi: 10.1007/s00414-016-1384-6. [DOI] [PubMed] [Google Scholar]
- 35.Ge ZP, Ma RH, Li G, Zhang JZ, Ma XC. Age estimation based on pulp chamber volume of first molars from cone-beam computed tomography images. Forensic Sci Int. 2015 Aug;253:133.e1–133.e7. doi: 10.1016/j.forsciint.2015.05.004. [DOI] [PubMed] [Google Scholar]
- 36.Villoria EM, Lenzi AR, Soares RV, Souki BQ, Sigurdsson A, Marques AP, Fidel SR. Post-processing open-source software for the CBCT monitoring of periapical lesions healing following endodontic treatment: technical report of two cases. Dentomaxillofac Radiol. 2017 Jan;46(1):20160293. doi: 10.1259/dmfr.20160293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cevidanes LH, Ruellas AC, Jomier J, Nguyen T, Pieper S, Budin F, Styner M, Paniagua B. Incorporating 3-dimensional models in online articles. Am J Orthod Dentofacial Orthop. 2015 May;147(5 Suppl):S195–S204. doi: 10.1016/j.ajodo.2015.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cevidanes LH, Styner M, Proffit WR. Three-dimensional superimposition of the skull base for the longitudinal evaluation of the effects of growth and of treatment. Orthod Fr. 2009 Dec;80(4):347–357. doi: 10.1051/orthodfr/2009021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Maber M, Liversidge HM, Hector MP. Accuracy of age estimation of radiographic methods using developing teeth. Forensic Sci Int. 2006 May;159(Suppl 1):S68–S73. doi: 10.1016/j.forsciint.2006.02.019. [DOI] [PubMed] [Google Scholar]
- 40.Nolla CM. The development of the permanent teeth. J Dent Child. 1960 Nov;27(4):254–266. [Google Scholar]
- 41.Kaissi AA, Handelbauer A, Klaushofer K, Grill F. Mid-diaphyseal endosteal thickening with subsequent medullary narrowing in a patient with Hallermann-Streiff syndrome. J Clin Med Res. 2011 Dec;3(6):328–330. doi: 10.4021/jocmr704e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Arsan B, Köse TE, Çene E, Özcan İ. Assessment of the tra-becular structure of mandibular condyles in patients with temporomandibular disorders using fractal analysis. Oral Surg Oral Med Oral Pathol Oral Radiol. 2017 Mar;123(3):382–391. doi: 10.1016/j.oooo.2016.11.005. [DOI] [PubMed] [Google Scholar]
- 43.Kavitha MS, An SY, An CH, Huh KH, Yi WJ, Heo MS, Lee SS, Choi SC. Texture analysis of mandibular cortical bone on digital dental panoramic radiographs for the diagnosis of osteoporosis in Korean women. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015 Mar;119(3):346–356. doi: 10.1016/j.oooo.2014.11.009. [DOI] [PubMed] [Google Scholar]
- 44.Ergün S, Saracjoglu A, Güneri P, Ozpinar B. Application of fractal analysis in hyperparathyroidism. Dentomaxillofac Radiol. 2009 Jul;38(5):281–288. doi: 10.1259/dmfr/24986192. [DOI] [PubMed] [Google Scholar]
- 45.Demirbaş AK, Ergün S, Güneri P, Aktener BO, Boyacioğlu H. Mandibular bone changes in sickle cell anemia: fractal analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008 Jul;106(1):e41–e48. doi: 10.1016/j.tripleo.2008.03.007. [DOI] [PubMed] [Google Scholar]
- 46.Gumussoy I, Miloglu O, Cankaya E, Bayrakdar IS. Fractal properties of the trabecular pattern of the mandible in chronic renal failure. Dentomaxillofac Radiol. 2016 May;45(5):20150389. doi: 10.1259/dmfr.20150389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Apolinário AC, Sindeaux R, de Souza Figueiredo PT, Gui-marães AT, Acevedo AC, Castro LC, de Paula AP, de Paula LM, de Melo NS, Leite AF. Dental panoramic indices and fractal dimension measurements in osteogenesis imperfecta children under pamidronate treatment. Dentomaxillofac Radiol. 2016 Mar;45(4):20150400. doi: 10.1259/dmfr.20150400. [DOI] [PMC free article] [PubMed] [Google Scholar]