13.1 Introduction
The most complex group of glycosphingolipids are the gangliosides. They contain oligosaccharide head groups with one or more residues of sialic acid. These are amphipathic compounds with a negative charge at pH 7.0. The gangliosides represents 5-8% of the total lipids in brain, and some 20 different types have been identified differing in the number of relative position of the hexose and sialic acid residues.
This is the basis of their classification. According to Svennerholm nomenclature a specific code G refers to “ganglion”, M, D, T and Q refer to the number of sialic acid moieties (mono-, di-, tri- and quadri-, respectively). The arabic numbers and small letters refer to the sequence of migration as determined by thin layer chromatography.
Gangliosides are highly concentrated in the ganglion cells of the central nervous system, particulary in the nerve endings. The CNS is unique among human tissues because more than one-half of the sialic acid is in ceramide-lipid-bound form. Lesser amounts of gangliosides are present in the surface membranes of the cells of most extraneural tissues. Gangliosides have been implicated in a varriety of specific biological processes in the nervous system, including cell adhesion and cell recognition, signal transduction, and regulation of receptor function and growth modulation.
13.2 Anti-ganglioside antibodies
Antibodies to antigens of myelin and axons are associated with several distinct syndromes of peripheral neuropathy. The antibodies are usually of polyclonal origin but are sometimes restricted to a single immunoglobulin class and may also occur as a monoclonal gammopathy. It is of note that unlike in most other organ-specific autoimmune diseases antibodies in peripheral neuropathy appear to recognize glycolipid antigens rather than protein antigen of myelin or axon.
Anti-ganglioside antibodies (anti-glycolipid antibodies) and peripheral neurophaty
Monoclonal antibodies to GM1 gangliosides are associated primarily with disorders affecting motor nerves. They were first described in patients with IgM monoclonal gammopathy and lower motor neuron syndrome and multifocal motor neuropathy (MMN).
Polyclonal anti-GM1 antibodies are found in a subset of patients with a variant of Guillain-Barre syndrome (GBS) characterized by a predominantly axonal neuropathy. They are found in MMN also, but there are predominantly or even exclusively of the IgM class while in GBS all three Ig classes are represented.
A common feature of both GBS and MMN is their association with conduction block of motor nerves, which may in part be caused by a direct action of the anti-ganglioside antibodies on ion channel function.
13.3 The Guillain-Barré syndrome
Acute GBS is clinically characterized by a rapidly progressive motor weakness of limb muscles and loss of reflexes while sensory symptoms occur less frequently. Increased serum titres of anti-GM1 antibodies have been reported in 22-30% of patients with GBS. These are polyclonal antibodies of all Ig subclasses and their titre is highest during the acute phase and decreases in the course of the disease.
A close antigenic relationship of Campylobacter lipopolysaccharides from stool isolates of GBS patients and oligosaccharides of certain gangliosides has been demonstrated supporting the concept of molecular mimicry (Table 2). This is a mechanism by which the host may generate an immune response to an initiating factor, such as an infectious organism or a tumor cell, which shares antigenic determinants with affected tissue of the host. For example, shared antigens between Campylobacter Jejuni and nerve fibres have been proposed to underlie some forms of GBS. GBS is considered to be a post-infectious disease because approximately two-third of patients report some form of preceding infectious illness. In a different study infections with C. Jejuni, Cytomegalovirus, Epstein-Barr virus and Mycoplasma Pneumoniae were shown to be significantly associated with GBS. The variability of GBS may, at least partly, be caused by a difference in the pathogen causing the preceding infection.
Table 2.
Glycolipid-mimicking structures identified on neuropathy-associated microorganisms
| Microorganism | Glycolipid (ganglioside) mimicked |
|---|---|
| Campylobacter jejuni | GM1, GM1b, GD1a, Ga1Nac-GD1a, GQ1b, GT1a |
| Haemophilus influenzae | GM1, GT1a |
| Mycoplasma pneumoniae | Galactocerebroside |
| Cytomegalovirus | GM2 |
13.4 Multifocal motor neuropathy
MMN is clinically characterized by slowly progressive asymmetric weakness of distal or proximal limb muscles and affects males more frequently than females. Its diagnostic hallmark is multifocal conduction block of motor nerves. The syndrome may easily be confused with motor neuron diseases like spinal muscular atrophy or amyotrophic lateral sclerosis.
Anti-GM1 antibodies in MMN are predominantly of the IgM class and titres are increased in 40-70% of patients, although an increased titre is not mandatory for the diagnosis.
13.5 Miller-Fisher syndrome
Increased titres of IgG antibodies directed to the ganglioside GQ1b are detectable in more than 90% of reported patients with the diagnosis of Miller-Fisher syndrome (MFS), a variant of GBS presenting with ophtalmoplegia, loss of tendon reflexes and sensory ataxia.
The pathogenic role of the ganglioside antibodies is still not clear, but there may be a contribution by a complement-mediated mechanism of immune injury. GM1 have complement-activating capacity, and the complement activation product has been found on the outer side of the Schwann cell and at the node of Ranvier. In a mouse model it was found that ganglioside antibodies are bound to peripheral nerve nodes of Ranvier and activate the complement cascade, but without inducing acute conduction block.
Because only some patients with preceding infections and ganglioside antibodies develop GBS, host susceptibility factors must be important for the development of the disease.
13.6 Laboratory methods
All laboratory methods lack specificity and sensitivity. Different ELISA methods, blot-techniques and immunochromatographic procedures are used for ganglioside antibodies measurement (detection). The most significant drawback of all methods is that the interpretation of results depends on the purity of the ganglioside fractions as antigens and assay conditions.
The methodology of anti-ganglioside antibodies assays is important because anti-glycolipid antibodies often bind to their targets with low avidity. False negative results occur if assay methodology fails to preserve the antibody-antigen bond or generates a low signal-to-noise ratio. Several methodological steps seem to improve the reliability of the enzyme-linked immunosorbent assay (ELISA) techniques that are commonly utilized for particular anti-ganglioside antibody measurement. The sensitivity of the assay is increased by taking measures to preserve the antigen-antibody bond. These include incubation for longer time (at least 4 hours), conducting the assay at 4° C, and avoiding the use of detergent in washing buffers. The specificity of the ELISA assay is improved by using human serum albumin or normal goat serum instead of bovine serum albumin for blocking non-specific binding sites in wells. Human serum occasionally has antibody activity to bovine serum albumin and can produce false positive or negative results depending on the type of controls used. Some attempts to recommend standard methodology have been made, although many laboratories have established local in-house immunodetection protocols based on elements previously published assay methods.
13.7 Conclusion
Anti-ganglioside antibody tests for possible immune-mediated neuropathy have become widely available in recent years. They have become popular because of their potential to identify subsets of patients within the large group of idiopathic neuropathies that have lacked specific clinical definition. However, testing for serum antibodies is never the first step but an additional diagnostic measure after careful clinical and electrophysiological evaluation.
Figure1.
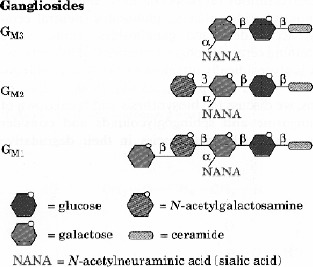
Schematic ganglioside structure
Table 1.
Antiganglioside antibodies and related neuropathies
| Antibody | Ig-class | Function | Neuropathy |
|---|---|---|---|
| Anti-GM1 | IgM | Conduction block | MMN |
| Anti-GM1 | |||
| Anti-GD1a | IgG, IgA, IgM | Conduction block | GBS |
| Anti-GT1b | |||
| Anti-GQ1b | IgG | Distal motor cond. block | MFS |
| Anti-GD1b | IgG | Sensory neuronal loss | Sensory neuropathy |
References
- 1.Willison HJ, Yuki N: Peripheral neuropathies and anti-glycolipid antibodies. Brain 2002;125(12):2591-2625. [DOI] [PubMed] [Google Scholar]
- 2.Kornberg AJ, Pestronk A: The clinical and diagnostic role of anti-GM1 antibody testing. Muscle&Nerve; 1994;17:100-104. [DOI] [PubMed] [Google Scholar]
- 3.Renaud S, Leppert D, Steck AJ. Clinical and biological aspects of antibodies in immune neuropathies. Conrad K, Humbel RL, Meurer M, Shoenfeld Y, Tan EM. (Eds): Autoantigens and Autoantibodies: Diagnostic tools and clues to understanding autoimmunity. Report on the 5th Dresden Symposium on Autoantibodies held in Dresden on October 18-21, 2000. Pabst Science Publishers; 2000: 566-579 [Google Scholar]
- 4.Steck AJ. Auto-antibody tests in peripheral neuropathies: pros and cons. J Neurol 2000;247: 423-428. [DOI] [PubMed] [Google Scholar]


