Abstract
Introduction:
Opioid analgesic prescriptions are driving trends in drug overdoses, but little is known about prescribing patterns among medical specialties. We conducted this study to examine the opioid-prescribing patterns of the medical specialties over time.
Methods:
IMS Health’s National Prescription Audit (NPA) estimated the annual counts of pharmaceutical prescriptions dispensed in the U.S. during 2007–2012. We grouped NPA prescriber specialty data by practice type for ease of analysis, and measured the distribution of total prescriptions and opioid prescriptions by specialty. We calculated the percentage of all prescriptions dispensed that were opioids, and evaluated changes in that rate by specialty during 2007–2012. The analysis was conducted in 2013.
Results:
In 2012, U.S. pharmacies and long-term care facilities dispensed 4.2 billion prescriptions, 289 million (6.8%) of which were opioids. Primary care specialties accounted for nearly half of all dispensed opioid prescriptions. The rate of opioid prescribing was highest for specialists in pain medicine (48.6%); surgery (36.5%); and physical medicine/rehabilitation (35.5%). The rate of opioid prescribing rose during 2007–2010 but leveled thereafter as most specialties reduced opioid use. The greatest percentage increase in opioid-prescribing rates during 2007–2012 occurred among physical medicine/rehabilitation specialists (+12.0%). The largest percentage drops in opioid-prescribing rates occurred in emergency medicine (−8.9%) and dentistry (−5.7%).
Conclusions:
The data indicate diverging trends in opioid prescribing among medical specialties in the U.S. during 2007–2012. Engaging the medical specialties individually is critical for continued improvement in the safe and effective treatment of pain.
Introduction
In the U.S., drug overdose deaths rose every year between 1999 and 2012,1 driven by prescription opioid analgesics.2 Primary care physicians prescribe the bulk of opioids.3 However, certain specialties, such as orthopedic surgery and dentistry, prescribe opioids at a higher rate than primary care physicians.4 Other medical specialties, such as emergency medicine, have documented large increases in opioid prescribing.5 There has not been a national comparison of the opioid-prescribing rates of the medical specialties over time. We used a recent commercial database to describe distributions and changes in opioid prescribing by medical specialty. We were interested in whether the recent emphasis on safe pain treatment had reduced opioid utilization among specialties with historically high or recently rising opioid-prescribing rates.
Methods
IMS Health’s National Prescription Audit (NPA) estimated the annual counts of all prescriptions dispensed nationally during 2007–2012. Prescriptions, including refills, dispensed at retail pharmacies, mail-order pharmacies, and long-term care facilities were included. The NPA sample included 67% of the approximately 57,000 pharmacies nationwide and captured nearly 80% of retail prescription dispensations in the U.S. NPA sampling methods are proprietary, and CIs for national estimates are not available. All opioid analgesics including buprenorphine were included. Opioid-containing cough and cold medications were excluded.
The NPA includes prescriber specialty data, and we grouped specialties by similarity of practice to clarify data interpretation (e.g., general practice, preventive medicine, and osteopathic medicine were grouped together as general practice) (Table 1). We calculated the total prescriptions and opioid prescriptions dispensed for the most recent year available, 2012. We defined the opioid-prescribing rate as the percentage of all prescriptions that were opioid analgesics and calculated annual rates and absolute rate changes during 2007–2012. We also used U.S. Census data to calculate opioid prescriptions per capita. We conducted this analysis in 2013.
Table 1. Opioid-Prescribing Rates by Specialty, IMS Health, U.S., 2012.
| Opioid Rx
n, millions (%) |
Total
Rx n, millions (%) |
Opioid Rx/Total
Rx % |
|
|---|---|---|---|
| Specialty | |||
| Family practice | 52.5 (18.2) | 946.9 (22.3) | 5.6 |
| Internal medicine | 43.6(15.1) | 913.9 (21.5) | 4.8 |
| Non-physician Prescribera | 32.2 (11.2) | 447.3 (10.5) | 7.2 |
| General practiceb | 32.2 (11.2) | 431.2 (10.1) | 7.5 |
| Surgeryc | 28.3 (9.8) | 77.6 (1.8) | 36.5 |
| Dentistry | 18.5 (6.4) | 64.0 (1.5) | 29.0 |
| Pain medicined | 14.5 (5.0) | 29.8 (0.7) | 48.6 |
| Emergency medicine | 12.5 (4.3) | 60.5 (1.4) | 20.7 |
| Physical med and rehab | 9.3 (3.2) | 26.1 (0.6) | 35.5 |
| All Otherse | 45.3 (15.7) | 1251.5 (29.5) | 3.6 |
| Total | 289.0 (100.0) | 4248.7 (100.0) | 6.8 |
Non-physician prescriber: nurse practitioner and physician’s assistant.
General practice: osteopathic medicine, general practice, and preventive medicine.
Surgery: general, orthopedic, plastic, cardiothoracic, vascular, colorectal, spinal, and neurologic.
Pain medicine: anesthesiology and pain medicine.
All others: cardiology, critical care, dermatology, endocrinology, gastroenterology, geriatrics, hematology, infectious disease, neurology, obstetrics and gynecology, oncology, otolaryngology, palliative care, pathology, pediatrics, podiatry, psychiatry, pulmonology, radiology, rheumatology, urology, veterinary, and “unspecified” specialty types.
Rx, prescriptions.
Results
In 2012, U.S. pharmacies (retail and mail order) and long-term care facilities dispensed 4.2 billion prescriptions, 289 million (6.8%) of which were opioid analgesics. Nine specialty groups accounted for 70.5% of all prescriptions and 84.3% of opioid prescriptions (Table 1). Three primary care specialty groups (family practice, internal medicine, and general practice) accounted for nearly half (44.5%) of all dispensed opioid prescriptions. Non-physician prescribers, physician assistants, and nurse practitioners contributed 10.5% of all prescriptions and 11.2% of opioid prescriptions. The rate of opioid prescribing was highest in the specialties of pain medicine (48.6%); surgery (36.5%); and physical medicine/ rehabilitation (35.5%).
During 2007–2012, total prescriptions per capita rose 3.5% (Table 2). Over the same period, opioid prescriptions per capita rose 7.3%. Overall, during 2007–2012, the opioid-prescribing rate increased by 3.7%. However, the growth in opioid prescribing stabilized in 2010, and both opioid prescriptions per capita and opioid-prescribing rates remained level during 2010–2012.
Table 2. Prescriptions Dispensed by Type, IMS Health, U.S., 2007–2012.
| 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | Change from 2007 to 2012 (%) |
|
|---|---|---|---|---|---|---|---|
| Opioid Rx
dispensed (millions) |
258.8 | 270.9 | 277.4 | 284.7 | 286.3 | 289.0 | 11.7 |
| Total Rx dispensed (millions) |
3,946.6 | 4,017.2 | 4,110.3 | 4,160.1 | 4,193.1 | 4,248.7 | 7.7 |
| Opioid Rx/total Rx (%) | 6.6 | 6.7 | 6.7 | 6.8 | 6.8 | 6.8 | 3.7 |
| Opioid Rx per capita | 0.86 | 0.89 | 0.90 | 0.92 | 0.92 | 0.92 | 7.3 |
| Total Rx per capita | 13.1 | 13.2 | 13.4 | 13.4 | 13.5 | 13.5 | 3.5 |
Rx, prescriptions.
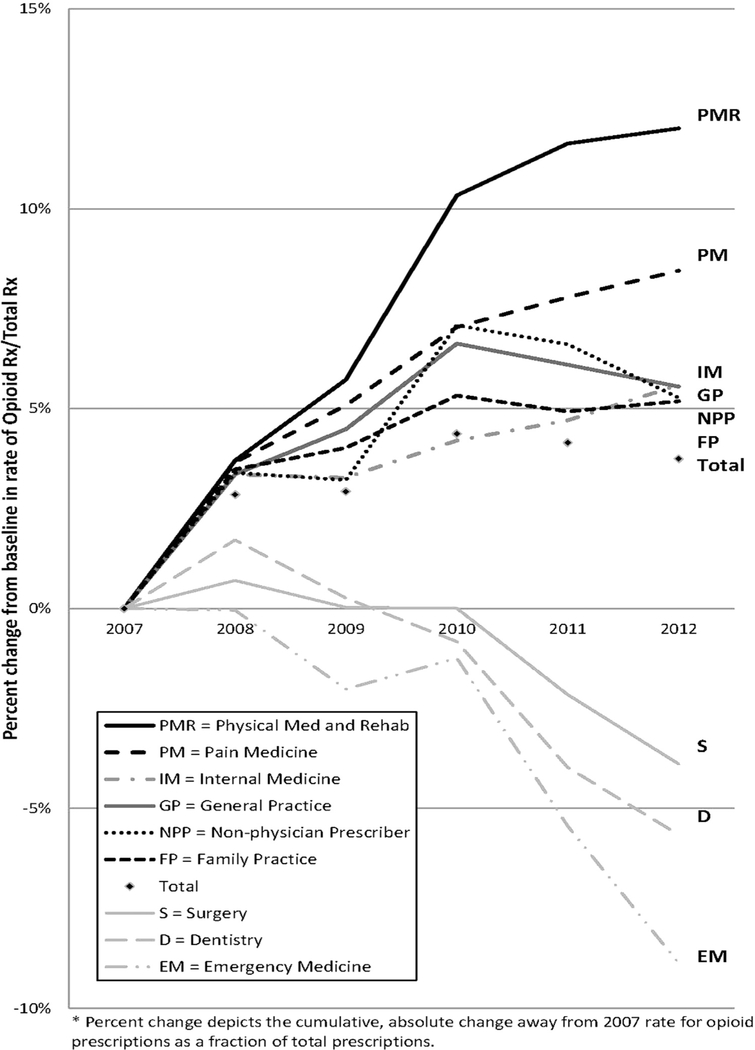
The greatest increase in the opioid-prescribing rate during 2007–2012 occurred among physical medicine/ rehabilitation specialists (+12.0%) (Figure 1). The opioid-prescribing rate for the specialties of pain medicine (+8.5%); family practice (+5.2%); general practice (+5.6%); and internal medicine (+5.6%) also increased more than the average opioid rate growth. Non-physician prescribers also had above-average growth in opioid-prescribing rates (+6.2% for nurse practitioners and +4.2% for physician assistants). All specialties except pain medicine, physical medicine/rehabilitation, and internal medicine reduced their prescribing rates after 2010. The largest drops in opioid-prescribing rates occurred in emergency medicine (−8.9%); dentistry (−5.7%); and surgery (−3.9%). All other specialties combined (not shown) saw a 2.2% drop in opioid-prescribing rates.
Figure 1.
Change in rate of opioid prescribing by specialty, 2007–2012*.
Discussion
The data from 2012 indicate that primary care specialties generated nearly half of dispensed opioid prescriptions, contributed more than half of all prescriptions, and prescribed opioids at a rate near the national average. Not surprisingly, specialties typically associated with the treatment of painful conditions such as pain medicine, physical medicine/rehabilitation, emergency medicine, surgery, and dentistry had high rates of opioid prescribing. Non-physician prescribers, an often overlooked group, contributed more than 11% of the opioid prescriptions, making them the third-largest opioid-pre-scribing group in this study.
The trends seen during 2007–2012 indicate a changing pattern of opioid prescribing in the U.S. The growth in opioid prescribing outpaced the growth in both total prescriptions and the U.S. population over the full study period. However, rates for both total and opioid prescriptions per capita stabilized after 2010. General practice and non-physician prescribers initially had above-average growth in the opioid-prescribing rate, but their rates dropped after 2010. Several specialties traditionally associated with high rates of opioid pre-scribing such as surgery, dentistry, and emergency medicine showed declines both before and after 2010. Only the specialties more likely to manage chronic pain (family practice, internal medicine, pain medicine, and physical medicine/rehabilitation) showed steady upward growth in their rates of opioid prescribing during 2007–2012. This persistent growth is concerning, as research has previously linked pain medicine and physical medicine/rehabilitation specialties to an increased risk of overdose death among their patients.6
The reasons for the 2010–2012 stabilization in prescription dispensation are not fully understood. Changes in the U.S. national pharmaceutical market may reflect macroeconomic phenomena that are beyond the scope of this study. However, during this period, a number of activities, such as an increase in the use of state prescription drug monitoring programs, changes to pain clinic licensing laws, and adjustments of insurance reimbursement policies, might have reduced inappropriate opioid prescribing.7–9 The stabilization in opioid prescribing might have contributed to the slight decline in opioid analgesic overdose mortality observed during 2010–2012.1
Limitations
This study has several limitations. IMS determines prescriber specialty by matching a Drug Enforcement Administration number, National Provider Identification number, or name and ZIP code to the American Medical Association database. Therefore, specialty assignation might not capture all providers, might poorly reflect practice settings, and may not track provider specialty changes. Furthermore, we grouped several specialties together for clarity of interpretation, but in doing so might have obscured differences among the combined specialties. Finally, the use of prescribing rates alone fails to capture changes in daily dosage or prescription duration, data that were not available for this analysis.
Conclusions
Despite these limitations, this study offers several important insights into opioid-prescribing behavior. The inflection point in the opioid-prescribing rate in 2010 is perhaps a sign that cautious use of opioid analgesics is becoming a priority among most medical specialties. The ongoing engagement of primary care physicians and non-physician prescribers, who together comprise the source of more than half of all opioid analgesic prescriptions, will be necessary to ensure continued improvement in safe, effective pain treatment. Specialties showing uninterrupted growth in opioid-based pain management, such as pain medicine and physical medicine/rehabilitation, should consider additional steps to support appropriate opioid-prescribing practices and the use of non-opioid and non-drug treatment options among their members.10 Finally, the reasons for the declines in opioid-prescribing rates among practitioners of emergency medicine, surgery, and dentistry should be explored. Understanding the factors that led to this decline could assist in developing efforts to further improve prescribing practice. Additional years of data will be needed to determine with certainty if the inflection in prescribing seen in 2010 was due to transient economic factors or is the beginning of an era of improved pain management, judicious opioid utilization, and decreased overdose deaths.
Acknowledgments
CDC funded this study and supported the staff responsible for the design and conduct of the study; the collection, analysis, and interpretation of the data; and the preparation, review, and approval of the manuscript. The views expressed in this article are those of the authors and do not necessarily reflect the official position of CDC or the U.S. Food and Drug Administration.
Footnotes
No financial disclosures were reported by the authors of this paper.
References
- 1.Warner M, Hedegaard H, Chen LH. NCHS Health E-Stat. Hyattsville, MD: National Centers for Health Statistics; 2014. Trends in drug-poisoning deaths involving opioid analgesics and heroin: United States, 1999–2012. www.cdc.gov/nchs/data/hestat/drug_poisoning/drug_ poisoning_deaths_1999-2012.pdf. [Google Scholar]
- 2.Jones CM, Mack KA, Paulozzi LJ. Pharmaceutical overdose deaths, United States, 2010. JAMA 2013;309(7):657–659. http://dx.doi.org/ 10.1001/jama.2013.272. [DOI] [PubMed] [Google Scholar]
- 3.Volkow ND, McLellan TA, Cotto JH, Karithanom M, Weiss SR. Characteristics of opioid prescriptions in 2009. JAMA 2011;305(13): 1299–1301. http://dx.doi.org/10.1001/jama.2011.401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ringwalt C, Gugelmann H, Garrettson M, et al. Differential prescribing of opioid analgesics according to physician specialty for Medicaid patients with chronic noncancer pain diagnoses. Pain Res Manag 2014;19(4):179–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chang HY, Daubresse M, Kruszewski SP, Alexander GC. Prevalence and treatment of pain in EDs in the United States, 2000 to 2010. Am J Emerg Med 2014;32(5):421–431. http://dx.doi.org/10.1016/j.ajem. 2014.01.015. [DOI] [PubMed] [Google Scholar]
- 6.Porucznik CA, Johnson EM, Rolfs RT, Sauer BC. Specialty of prescribers associated with prescription opioid fatalities in Utah, 2002–2010. Pain Med 2014;15(1):73–78. http://dx.doi.org/10.1111/pme.12247. [DOI] [PubMed] [Google Scholar]
- 7.Kreiner P, Nikitin R, Shields TP. Bureau of justice assistance prescription drug monitoring program performance measures report: January, 2009 through June 2012 Washington, DC: U.S. Department of Justice, Bureau of Justice Assistance; www.pdmpexcellence.org/sites/all/pdfs/BJA%20PDMP%20Performance%20Measures%20Report%20Jan%202009%20to%20June%202012%20FInal_with%20feedback.pdf. [Google Scholar]
- 8.State regulation of pain clinics and legislative trends relative to regulating pain clinics. National Alliance for Model State Drug Laws Website www.namsdl.org/NAMSDL%20Part%202%20Revised%20April%204%202014.pdf. 2014.
- 9.State Medicaid interventions for preventing prescription drug abuse and overdose: a report for the National Association of Medicaid Directors. Mercer Inc.; www.medicaiddirectors.org/node/1071. October 1, 2014. [Google Scholar]
- 10.Chou R, Fanciullo GJ, Fine PG, et al. American Pain Society-American Academy of Pain Medicine Opioids Guidelines Panel. Clinical guide-lines for the use of chronic opioid therapy in chronic noncancer pain. J Pain 2009;10(2):113–130. [DOI] [PMC free article] [PubMed] [Google Scholar]