Abstract
Background:
Fatigue is one of the most common issues related to cancer. Social support has direct effects on health status and coping with illness. This study investigated the relationship between the perception of social support and fatigue in patients with cancer.
Materials and Methods:
This descriptive/correlational study was conducted in Omid Hospital in Isfahan, Iran in 2014. One hundred and twenty-five cancer patients receiving chemotherapy were included in the study. Study participants were selected using consecutive sampling. Data were collected using the Cancer Fatigue Scale (CFS), Perceived Social Support Scale, and a demographic characteristics questionnaire. The collected data were analyzed using descriptive and analytical statistical tests in SPSS software.
Results:
Mean (SD) of patients’ fatigue and perceived social support scores were 40.63 (11.59) out of 100 and 49.33 (7.85) out of 100, respectively. The Pearson correlation coefficient showed an inverse relationship between fatigue and social support, however, this relationship was not significant. Multiple regression test was used to detect which dimension of perceived social support was a better predictor of the reduction in fatigue score. This test showed that the best predictor was informational support (B = −0.35, p = 0.004).
Conclusions:
Results showed a negative relationship between fatigue and perceived social support in cancer patients undergoing chemotherapy. Therefore, social support interventions can help reduce fatigue.
Keywords: Cancer, fatigue, Iran, social support
Introduction
Cancer as a life-threatening illness affects individuals’ health status.[1] The diagnosis of cancer is associated with a high level of psychological stress,[2] and is a crisis for patients and their families [3] due to its resulting emotional, physical, and social issues. The symptoms and side-effects of cancer decrease patients’ physical well-being and quality of life (QOL).[4,5] Fatigue is a common distressing symptom in patients with cancer,[6] and its prevalence ranged from 50% to 90% in a study reported by Donovan et al.[7] This symptom causes limitation in physical activity [8,9] and interferes with professional, family, and social roles.[10,11] The underlying mechanisms of fatigue are not clear, but its multidimensional and different factors such as psychological, environmental, and physical factors contribute to its occurrence;[12] however, no particular therapies have been found to address it.[13]
Prue et al. found that fatigue may remain for months or even years after completion of treatment, especially among patients who underwent chemotherapy.[14] Many patients have reported high scores for fatigue, but it was poorly managed in them.[15] The best strategy for managing fatigue is identifying the factors that reduce fatigue in these patients and help them overcome stressful situations.[1] Some studies have examined the effect of pharmacological intervention on cancer-related fatigue (CRF).[16,17,18] There are very few pharmacological options for the management of CRF and limited evidence of their effectiveness.[19] Some researchers have proposed that nonpharmacological intervention may reduce CRF.[20,21]
Tabrizi and Alizadeh found that CRF in patients is associated with their demographic characteristics, and stated that forming self-help groups as social support might be essential to reducing fatigue.[22] Numerous studies have been carried out on this issue. Some studies showed that social support has buffering effects [13] and helps patients cope with stressful situations [23] and overcome their challenges.[24] Others showed that social support has a direct effect on QOL [25,26] and can assist in the management of symptoms that patients with cancer experience,[27] and also showed that there was no significant relationship between perceived social support and fatigue.[28] Some studies in Iran have also investigated CRF.[22,29,30] The findings of Hajloo et al. showed the significant role of disease stage, illness perception, unmet needs, and fatigue in predicting the QOL of patients.[29] They also found that, in addition to providing physical care, attention to the psychological component in the lives of cancer patients is important in improving their QOL.[29] Chehrehgosha et al. stated that, in addition to physical care and nursing interventions, psychological interventions also play a significant role in the all-inclusive management of cancer patients’ problems, in particular, fatigue.[30]
Although there have been a large number of studies on fatigue and its management, few studies have been conducted to investigate the relationship between fatigue and social support in cancer patients, and no research has been conducted in this regard in Iran.
The provision of effective social support for patients might motivate patients to better cope with unbearable conditions, provide them with the practical and factual assistance they need, and teach them how to cope with symptoms. This study was conducted for evaluating the levels of fatigue and social support in patients receiving chemotherapy and to determine the relationship between fatigue and social support.
Materials and Methods
This correlational study was conducted among cancer patients receiving chemotherapy in a professional cancer treatment center in Isfahan, Iran between April and December 2014. Based on type I error of α= 0.05, power of 80%, and minimum of 0.2 estimate of correlation coefficient between fatigue and social support, a sample size of 125 participants was determined.[31] The participants were selected using consecutive sampling method. Sampling was conducted in the chemotherapy units of Omid Hospital. Every patient who met the inclusion criteria was selected until the required sample size was achieved. The inclusion criteria consisted of being Iranian and older than 18 years of age (people under the age of 18 years may have fewer connections with the outside environment due to family ties) and speaking Persian. This study was conducted among patients with different kinds of cancer who were undergoing chemotherapy and had no cognitive or physical disorders. If a patient was unable or unwilling to continue the study, he/she was excluded from the study.
In this study, a three-part questionnaire was used to collect data. The first part included questions on demographic characteristics and factors related to the disease and treatment that may affect fatigue and social support. This section included seven demographic questions on age (years), gender (male/female), level of education (illiterate, primary school, high school, secondary school, college), course of chemotherapy (1, 2, 3, 4, and more), marital status (married, single, divorced, or widowed), income (less than 150 $, 150 to 300 $, and more than 300 $), and disease duration (month).
The second part consisted of the Cancer Fatigue Scale (CFS) which examines fatigue in patients with cancer.[31] This scale was translated and used for the first time in Iran by Haghighat et al. in 2003.[32] It comprises 15 items in the three physical, cognitive, and emotional dimensions. Each item is scored based on a 5-point Likert scale ranging from 1 to 5 (not at all to very much). The total score of the inventory ranges between 15 and 75. Cronbach's alpha coefficient was calculated to determine the reliability of this tool (α = 0.95). In the current study, the Cronbach's alpha coefficient of the CFS was 0.91.
In the third part, the Perceived Social Support Scale was used to examine social support in these patients. This tool was developed by Davari in 2011[28] and includes 30 items in the emotional, informational, and instrumental dimensions. Each item is scored based on a 4-point Likert scale ranging from 1 to 4 (never to always). The total score of the scale ranges between 30 and 120. The validity of these instruments was determined through content and face validity. Cronbach's alpha coefficient was calculated to determine the reliability of the Perceived Social Support Scale (α = 87%). In addition to Cronbach's alpha coefficient, test-retest was also performed to assess reliability (r = 0.89). The reliability of the CFS in the physical, cognitive, and emotional dimensions and the total score of fatigue were determined using Cronbach's alpha coefficient (α = 0.92, α = 0.85, α = 0.89, and α = 0.95, respectively).
Researchers referred to chemotherapy wards and selected participants among patients who were hospitalized in the wards and were undergoing chemotherapy or were referred for chemotherapy. Patients who agreed to participate in the study were invited to take part in an interview to complete the questionnaire.
Some participants preferred to complete the questionnaire themselves alone. In such cases, the researchers provided them with the questionnaire. Data were collected in a private environment in the hospital wards after coordination with the wards’ chief nurses.
Statistical analysis of the data was conducted using SPSS software (version 20, IBM Corporation, Armonk, NY, USA). Six questionnaires were excluded from statistical calculations and 119 questionnaires were used for statistical analysis. Descriptive statistics (frequency, mean, and SD) were employed to calculate the fatigue score and perceived social support score and their dimensions. After conducting Kolmogorov–Smirnov test for goodness-of-fit to determine the type of distribution, Pearson correlation coefficient test was used to determine the correlation between social support and fatigue scores. Multiple regression test was adopted to determine which dimension of social support was a stronger predictor of fatigue score.
Ethical considerations
Approval to conduct the study was granted by the ethics committee of Isfahan University of Medical Sciences (ethics code: 291023). The researchers explained the research goals to the participants and obtained their written informed consent. All participants were informed that participating in the study was voluntary and were ensured of the confidentiality of their personal information.
Results
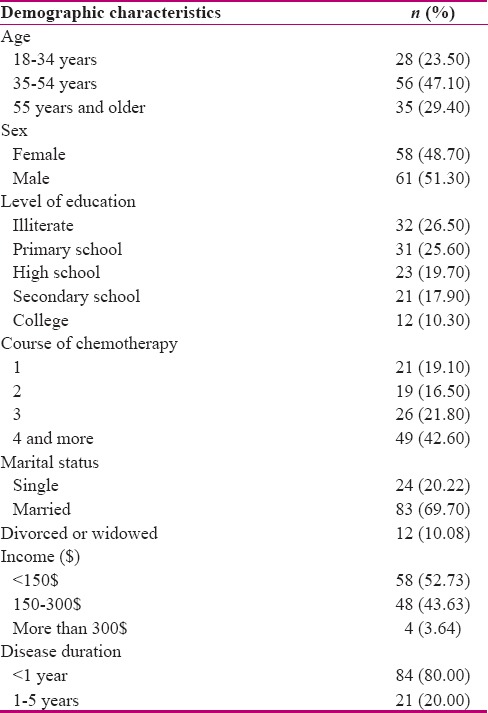
The mean (SD) score of participants’ age was 45.72 (14.11). Half of the patients were men (51.30%). Most of the participants were married (69.70%), illiterate (26.50%), and housewives (37.60%), and had an income of less than 150 $ (52.70%). Disease duration was less than 1 year (80%) in most participants. Most were hospitalized for chemotherapy (60.90%) and were undergoing course 4 or higher (42.60%)[Table 1].
Table 1.
Demographic characteristics of the patients
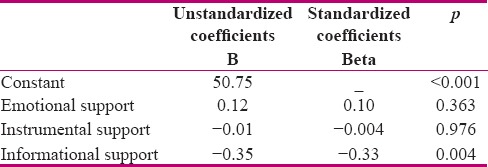
The mean (SD) score of fatigue was 40.63 (11.59) out of 100. The mean score of fatigue differed in different dimensions, and the highest mean was related to the physical dimension [44.34 (12.67) out of 100]. The mean (SD) score of social support was 49.33 (7.85) out of 100. The mean scores of informational and instrumental dimensions were less than that of the emotional dimension. There was an inverse relationship between total social support and fatigue scores, but this relationship was not significant (r = −0.18, p = 0.057). Moreover, the Pearson correlation coefficient showed an inverse and significant association between informational support and physical fatigue (r = −0.34, p = 0.001), cognitive fatigue (r = −0.21, p = 0.018), and total fatigue scores (r = −0.28, p = 0.002) [Table 2]. Multiple regression test was used to detect which dimension of perceived social support was a better predictor of the reduction of fatigue score. Results showed that the best predictor was informational support (p = 0.004) [Table 3].
Table 2.
Pearson correlation coefficient between social support and fatigue
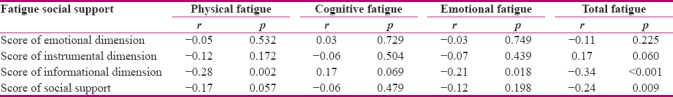
Table 3.
Regression coefficient of social support dimensions and beta according to fatigue score
Discussion
The objective of the current study was to assess the relation between CRF and perceived social support in cancer patients undergoing chemotherapy. Based on the findings, the mean score of fatigue in patients receiving chemotherapy was less than average, which is in line with the findings of Santin et al.[14] This may be due to disease duration that was less than 1 year in most participants. Hofman et al. reported variation in the level of fatigue in different studies.[33] The severity of CRF over time depends on many factors, including the treatment regimen, type of cancer, assessment technique, and patient population.[33]
In the current study, the rate of fatigue experienced by patients in the physical dimension was higher than that in other dimensions. Haghighat et al. also reported varying degrees of fatigue, and that the most commonly experienced fatigue was in the physical dimension.[32] Kelley and Kelley reported that most patients with fatigue reported significant impairment in their ability to complete a variety of daily activities, including preparing food, cleaning the house, and light lifting, and social activities with friends and family.[34] However, findings showed that effective interventions, such as social support, are urgently needed to reduce CRF and have the potential of improving physical functioning, QOL, and emotional and psychological health.[35] The present study findings showed that the mean score of perceived social support was approximately moderate [49.33 (7.85) out of 100]. In line with our findings, Pinar et al. reported that the mean score of social support in most patients with genital cancer was moderate,[36] whereas the results of the studies of Zabalegui et al.[37] and Karakoc and Yurtsever [24] showed that most participants experienced high social support. Furthermore, the results of the study by Faghani et al. showed that participants received a high level of social support.[38] This contrast may be related to sample size and the characteristics of study participants. The sample size of the current study was smaller than other studies. Moreover, patients with depression or physical limitations were not included in this study, and the majority of patients had a disease duration of less than 1 year, whereas other studies reported that more problematic patients with cancer receive more social support.[38] Findings in this study showed that patients received more emotional support compared to instrumental and informational support. The findings of Karakoc and Yurtsever are consistent with this finding.[24] Another study indicated that emotional support was most desired by cancer patients and directly correlated with the positive outcome of the disease.[39]
It seems that in patients with cancer the first and most common support provided by the family, relatives, and health personnel is emotional support. Emotional support includes empathy, listening, providing a sense of comfort, and communicating affection and love.
The mean instrumental support in this study was less than the average. In the study by Tzonkova, patients with cancer were forced to face and fight the disease alone without having instrumental or informational support from their relatives and friends, or having such support offered to them in extremely rare cases. Instrumental support is seen as a tangible aid that is offered regarding the disease. It includes transportation to and from the hospital, help with housework, and paying the bills.[40] Results of the present study may be due to low income of friends and relatives and the lack of sufficient financial support from support groups.
Low informational support is probably related to the fact that patients with cancer are not informed of their disease, because in Iran families do not have the tendency to talk about cancer diagnosis with their patients.[41] This is also observed in other cultures; the fear of saddening or harming the patient is a barrier to providing information about diagnosis to patients.[42] Moreover, many factors such as income [36] and educational level [43] correlated positively with perceived social support, and in the present study, most participants were illiterate and had low income. Another possible explanation for this result can be found in the specifics of this type of support. It requires knowledge in the field of medicine and relevant experience and practice. A previous study has showed that high informational support reduces fear [44] and distress,[45] and thus, providing informational support to patients is very useful.[46]
In the present study, there was an inverse relationship between total social support and fatigue, which was not significant. This suggests that, although the relationship between social support and fatigue is not strong, social support has an inverse relationship with fatigue.
There was an inverse and significant relationship between total social support and fatigue in the physical dimension of fatigue, which implies that with increase in social support in patients their fatigue decreases in the physical dimension. Results of the study by Karakoc and Yurtsever are consistent with this finding.[24] CRF is associated with significant levels of psychological distress and imposes a financial burden by limiting a patient's ability to work effectively. This economic effect can extend to caregivers and family members who may have to reduce their working hours to provide care for a patient with CRF.[33] This suggests that psychosocial interventions such as social support can improve the patient's condition even in the physical aspect, and subsequently, may increase the patient's QOL. Multiple regression test was used to detect which dimension of perceived social support was a better predictor of the reduction of fatigue score. Results showed that the best predictor was informational support.
Results of the study by Aghayousefi et al. indicated that education and knowledge of the disease has an effective role in reducing fatigue in patients with cancer.[47] Furthermore, informational support includes counseling, referral, and feedback for a given problem.[40]
Further research is needed to better understand the nature of the relationship between social support and fatigue symptoms in patients with cancer. For example, it would be interesting to compare this relationship between different gender and age groups, as well as patients with different disease durations.
The results of this study suggest that social support may be beneficial to patients with cancer. Further, informational support that incorporates family and friends and nursing staff from the patients’ social support network may be of the most benefit to fatigue and physical problems among patients with cancer. Patients’ fatigue could be reduced through increasing their awareness. Based on the results of this study, it is recommended that more specific studies be conducted regarding the different dimensions of social support such as the impact of informational support on the problems of patients with cancer.
In studies on the psychosocial impact of cancer, it is important to evaluate the findings with regard to individual characteristics and to make comparisons whenever possible. It is suggested that studies with larger sample sizes be conducted to determine the effect of social support on fatigue. This study was conducted in one center and with a small sample size, and the small sample size may have an impact on the findings. In addition, disease duration was less than 1 year in most participants; therefore, another study in patients with longer disease duration is recommended. Notwithstanding its limitations, this study is the first investigation of the association between social support and fatigue of patients with cancer in Iran.
Conclusion
Results showed that there was an inverse significant association between informational supports and fatigue in its physical dimension. Moreover, the best predictor of the reduction in fatigue score was informational support. Thus, it is suggested that health care providers, in addition to providing informational support and information about disease symptoms management, help patients identify sources of support and participate in support networks.
Furthermore, the use of the family-center care plan to increase support and the participation of a family member in the care process, especially for patients who perceived a lower level of social support, are recommended.
Financial support and sponsorship
Isfahan University of Medical Sciences, Isfahan, Iran.
Conflicts of interest
Nothing to declare.
Acknowledgement
The authors wish to thank all the individuals who kindly participated in this study and Isfahan University of Medical Sciences for supporting this work. The project number was 291023.
References
- 1.Usta YY. Importance of social support in cancer patients. Asian Pac J Cancer Prev. 2012;13:3569–72. doi: 10.7314/apjcp.2012.13.8.3569. [DOI] [PubMed] [Google Scholar]
- 2.Homeberm F. cancer related fatigue: Epidemiology, pathogenesis, diagnosis, and treatment. Dtsch Arztebl Int. 2012;109:161–71. doi: 10.3238/arztebl.2012.0161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Joulaee A, Joolaee S, Kadivar M, Hajibabaee F. Living with breast cancer: Iranian women's lived experiences. Int Nurs Rev. 2012;59:362–8. doi: 10.1111/j.1466-7657.2012.00979.x. [DOI] [PubMed] [Google Scholar]
- 4.Bower JE, Bak K, Berger A, Breitbart W, Escalante CP, Ganz PA, et al. Screening, assessment, and management of fatigue in adult survivors of cancer: An American Society of Clinical oncology clinical practice guideline adaptation. J Clin Oncol. 2014;32:1840–50. doi: 10.1200/JCO.2013.53.4495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fabi A, Falcicchio C, Giannarelli D, Maggi G, Cognetti F, Pugliese P. The course of cancer related fatigue up to ten years in early breast cancer patients: What impact in clinical practice? Breast. 2017;34:44–52. doi: 10.1016/j.breast.2017.04.012. [DOI] [PubMed] [Google Scholar]
- 6.Evans S, Seidman L, Sternlieb B, Casillas J, Zeltzer L, Tsao J. Clinical case report: Yoga for fatigue in five young adult survivors of childhood cancer. J Adolesc Young Adult Oncol. 2017;6:96–101. doi: 10.1089/jayao.2016.0013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Donovan KA, Stein KD, Lee M, Leach CR, Ilozumba O, Jacobsen PB. Systematic review of the multidimensional fatigue symptom inventory-short form. Support Care Cancer. 2015;23:191–212. doi: 10.1007/s00520-014-2389-7. [DOI] [PubMed] [Google Scholar]
- 8.Molassiotis A, Zheng Y, Denton-Cardew L, Swindell R, Brunton L. Symptoms experienced by cancer patients during the first year from diagnosis: patient and informal caregiver ratings and agreement. Palliat Support Care. 2010;8:313–24. doi: 10.1017/S1478951510000118. [DOI] [PubMed] [Google Scholar]
- 9.Purcell A, Fleming J, Bennett S, McGuane K, Burmeister B, Haines T. A multidimensional examination of correlates of fatigue during radiotherapy. Cancer. 2010;116:529–37. doi: 10.1002/cncr.24731. [DOI] [PubMed] [Google Scholar]
- 10.Barton DL, Liu H, Dakhil SR, Linquist B, Sloan JA, Nichols CR, et al. Wisconsin Ginseng (Panax quinquefolius) to improve cancer-related fatigue: A randomized, double-blind trial, N07C2. J Natl Cancer Instt. 2013;105:1230–8. doi: 10.1093/jnci/djt181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cheville AL. Cancer-related fatigue. Phys Med Rehabil Clin N Am. 2009;20:405–16. doi: 10.1016/j.pmr.2008.12.005. [DOI] [PubMed] [Google Scholar]
- 12.Vries U, Reif K, Petermann F. Tumorbedingte Fatigue und ihre psychosozialen Belastungen. Der Internist. 2011;11:1317–24. doi: 10.1007/s00108-011-2921-5. [DOI] [PubMed] [Google Scholar]
- 13.Wang XS, Zhao F, Fisch MJ, O'mara AM, Cella D, Mendoza TR, et al. Prevalence and characteristics of moderate to severe fatigue: A multicenter study in cancer patients and survivors. Cancer. 2014;120:425–32. doi: 10.1002/cncr.28434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Prue G, Allen J, Gracey J, Rankin J, Cramp F. Fatigue in gynecological cancer patients during and after anticancer treatment. J Pain Symptom Manage. 2010;39:197–210. doi: 10.1016/j.jpainsymman.2009.06.011. [DOI] [PubMed] [Google Scholar]
- 15.Santin O, Murray L, Prue G, Gavin A, Gormley G, Donnelly M. Self-reported psychosocial needs and health-related quality of life of colorectal cancer survivors. Eur J Oncol Nurs. 2015;19:336–42. doi: 10.1016/j.ejon.2015.01.009. [DOI] [PubMed] [Google Scholar]
- 16.Barak Y, Magalashvili D, Dolgopiat MD, Ladkani D, Nitzani D, Mazor Z, et al. Effect of alfacalcidol on fatigue in MS patients: A randomized, double-blind study (S23.004) Neurology. 2014;82:S23.004–S23.004. [Google Scholar]
- 17.Morrow GR, Shelke AR, Roscoe JA, Hickok JT, Mustian K. Management of cancer-related fatigue. Cancer Invest. 2005;23:229–39. doi: 10.1081/cnv-200055960. [DOI] [PubMed] [Google Scholar]
- 18.Yennurajalingam S, Frisbee-Hume S, Palmer JL, Delgado-Guay MO, Bull J, Phan AT, et al. Reduction of cancer-related fatigue with dexamethasone: A double-blind, randomized, placebo-controlled trial in patients with advanced cancer. J Clin Oncol. 2013;31:3076–82. doi: 10.1200/JCO.2012.44.4661. [DOI] [PubMed] [Google Scholar]
- 19.Finnegan-John J, Molassiotis A, Richardson A, Ream E. A systematic review of complementary and alternative medicine interventions for the management of cancer-related fatigue. Integrative Cancer Ther. 2013;12:276–90. doi: 10.1177/1534735413485816. [DOI] [PubMed] [Google Scholar]
- 20.Eickmeyer SM, Gamble GL, Shahpar S, Do KD. The role and efficacy of exercise in persons with cancer. Pm R. 2012;4:874, 81. doi: 10.1016/j.pmrj.2012.09.588. [DOI] [PubMed] [Google Scholar]
- 21.Tsai HF, Chen YR, Chung MH, Liao YM, Chi MJ, Chang CC, et al. Effectiveness of music intervention in ameliorating cancer patients’ anxiety, depression, pain, and fatigue: A meta-analysis. Cancer Nurs. 2014;37:E35–E50. doi: 10.1097/NCC.0000000000000116. [DOI] [PubMed] [Google Scholar]
- 22.Moghaddam Tabrizi F, Alizadeh S. Cancer Related Fatigue in Breast Cancer Survivors: In Correlation to Demographic Factors. Maedica. 2017;12:106. [PMC free article] [PubMed] [Google Scholar]
- 23.Rizalar S, Ozbas A, Akyolcu N, Gungor B. Effect of perceived social support on psychosocial adjustment of Turkish patients with breast cancer. Asian Pac J Cancer Prev. 2014;15:3429–34. doi: 10.7314/apjcp.2014.15.8.3429. [DOI] [PubMed] [Google Scholar]
- 24.Karakoc T, Yurtsever S. Relationship between social support and fatigue in geriatric patients receiving outpatient chemotherapy. Eur J Oncol Nurs. 2010;14:61–7. doi: 10.1016/j.ejon.2009.07.001. [DOI] [PubMed] [Google Scholar]
- 25.Eom CS, Shin DW, Kim SY, Yang HK, Jo HS, Kweon SS, et al. Impact of perceived social support on the mental health and health-related quality of life in cancer patients: Results from a nationwide, multicenter survey in South Korea. Psycho-Oncology. 2013;22:1283–90. doi: 10.1002/pon.3133. [DOI] [PubMed] [Google Scholar]
- 26.Filazoglu G, Griva K. Coping and social support and health related quality of life in women with breast cancer in Turkey. Psychol Health Med. 2008;13:559–73. doi: 10.1080/13548500701767353. [DOI] [PubMed] [Google Scholar]
- 27.Ekmann A, Avlund K, Osler M, Lund R. Do negative aspects of social relations influence fatigue. A cross-sectional study on a non-clinical sample of middle-aged Danish men? J Psychosomatic Res. 2012;73:277–82. doi: 10.1016/j.jpsychores.2012.08.005. [DOI] [PubMed] [Google Scholar]
- 28.Davari E. Investigation of Perceived Social Support on Quality of Life in Patients with Heart Failure in Hamedan Heart Professional center. Hamedan University of Medical Sciences; 2011. [Persian thesis] [Google Scholar]
- 29.Hajloo N, Barahmand O, Adili A, Fathi M. The role of disease stage illness perceptions, unmet needs and fatigue in predicting quality of life in patients with cancer. Health Psychol. 2016;5:79–95. [Google Scholar]
- 30.Chehrehgosha M, Dastourpour M, Sanagu A, Mohamadi A. Cancer-related Fatigue and its Relationship with Demographic and Clinical Characteristics. Hakim Jorjani J. 2013;1:24–31. [Google Scholar]
- 31.Hann D, Baker F, Denniston M, Gesme D, Reding D, Flynn T, et al. The influence of social support on depressive symptoms in cancer patients: Age and gender differences. J Psychosomatic Res. 2002;52:279–83. doi: 10.1016/s0022-3999(01)00235-5. [DOI] [PubMed] [Google Scholar]
- 32.Haghighat S, Akbari ME, Holakouei K, Rahimi A, Montazeri A. Factors predicting fatigue in breast cancer patients. Support Care Cancer. 2003;11:533–8. doi: 10.1007/s00520-003-0473-5. [DOI] [PubMed] [Google Scholar]
- 33.Hofman M, Ryan JL, Figueroa-Moseley CD, Jean-Pierre P, Morrow GR. Cancer-related fatigue: The scale of the problem. Oncologist. 2007;12(Suppl 1):4–10. doi: 10.1634/theoncologist.12-S1-4. [DOI] [PubMed] [Google Scholar]
- 34.Kelley GA, Kelley KS. Exercise and cancer-related fatigue in adults: A systematic review of previous systematic reviews with meta-analyses. BMC Cancer. 2017;17:693. doi: 10.1186/s12885-017-3687-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vardy J, Dhillon HM, Pond GR, Rourke SB, Xu W, Dodd A, et al. Cognitive function and fatigue after diagnosis of colorectal cancer. Ann Oncol. 2014;25:2404–12. doi: 10.1093/annonc/mdu448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pinar G, Okdem S, Buyukgonenc L, Ayhan A. The relationship between social support and the level of anxiety, depression, and quality of life of Turkish women with gynecologic cancer. Cancer Nurs. 2012;35:229–35. doi: 10.1097/NCC.0b013e31822c47bd. [DOI] [PubMed] [Google Scholar]
- 37.Zabalegui A, Cabrera E, Navarro M, Cebria MI. Perceived social support and coping strategies in advanced cancer patients. J Res Nurs. 2013;18:409–20. [Google Scholar]
- 38.Faghani S, Rahmani A, Parizad N, Mohajjel-Aghdam A-R, Hassankhani H, Mohammadpoorasl A. Social support and its predictors among Iranian cancer survivors. Asian Pac J Cancer Prev. 2014;15:9767–71. doi: 10.7314/apjcp.2014.15.22.9767. [DOI] [PubMed] [Google Scholar]
- 39.Kinsinger SW, Laurenceau JP, Carver CS, Antoni MH. Perceived partner support and psychosexual adjustment to breast cancer. Psychol Health. 2011;26:121571–88. doi: 10.1080/08870446.2010.533771. [DOI] [PubMed] [Google Scholar]
- 40.Tzonkov BV. Perceived Social Support in Cancer Survivors: Some Preliminary Results, Clinical Cases and Studies. Psychol Thought. 2013;6:90–6. [Google Scholar]
- 41.Ehsani M, Taleghani F, Hematti S, Abazari P. Perceptions of patients, families, physicians and nurses regarding challenges in cancer disclosure: A descriptive qualitative study. Eur J Oncol Nurs. 2016;25:55–61. doi: 10.1016/j.ejon.2016.09.003. [DOI] [PubMed] [Google Scholar]
- 42.Lichtenthal WG, Corner GW, Slivjak ET, Roberts KE, Li Y, Breitbart W, et al. A pilot randomized controlled trial of cognitive bias modification to reduce fear of breast cancer recurrence. Cancer. 2017;123:1424–33. doi: 10.1002/cncr.30478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wiener CH, Cassisi JE, Paulson D, Husson O, Gupta RA. Information support, illness perceptions, and distress in survivors of differentiated thyroid cancer. J Health Psychol. 2017;21:1956–65. doi: 10.1177/1359105317692143. [DOI] [PubMed] [Google Scholar]
- 44.Boltong A, Ledwick M, Babb K, Sutton C, Ugalde A. Exploring the rationale, experience and impact of using Cancer Information and Support (CIS) services: An international qualitative study. Support Care Cancer. 2017;25:1–8. doi: 10.1007/s00520-016-3513-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ehsani M, Taleghani F, Hematti S, Abazari P. Perceptions of patients, families, physicians and nurses regarding challenges in cancer disclosure: A descriptive qualitative study. Eur J Oncol Nurs. 2016;25:55–61. doi: 10.1016/j.ejon.2016.09.003. [DOI] [PubMed] [Google Scholar]
- 46.Drageset S, Lindstrøm TC. Coping with a possible breast cancer diagnosis: Demographic factors and social support. J Adv Nurs. 2005;51:217–26. doi: 10.1111/j.1365-2648.2005.03495.x. [DOI] [PubMed] [Google Scholar]
- 47.Aghayousefi, AR Dehestani M. Sharifi Saki S. Effectiveness of Cognitive – Behavioral Education in Reduction of Exhaustion of Cancer of Women Suffering from Breast Cancer Health. Psychology. 2016;5:5–17. [Google Scholar]


