Abstract
Background and Purpose
Gait speed does not adequately predict whether stroke survivors will be active in the community. This may be because traditional single-task gait speed does not sufficiently reproduce the demands of walking in the real world. This study assessed whether dual-task gait speed accounts for variance in daily ambulatory activity above what can be predicted with habitual (single-task) gait speed in community-dwelling stroke survivors.
Methods
Twenty-eight community-dwelling individuals, 58.2 years (SD=16.6), 8.9 months post stroke (IQR=3.7-19.4), completed a gait and cognitive task in single- and dual-task conditions. Daily ambulatory activity was captured using a physical activity monitor. A regression analysis examined R-squared changes with single and dual-task gait speed.
Results
Single-task gait speed explained 15.3% of the variance in daily ambulatory activity (P=0.04). Adding dual-task gait speed to the regression model increased the variance explained by an additional 20.6% (P=0.04).
Conclusions
Gait speed assessed under attention-demanding conditions may improve explanation of variance in daily ambulatory activity after stroke.
Indexing terms: Stroke, Cognition, Gait, Physical Activity
Subject terms: Cerebrovascular Disease/Stroke, Rehabilitation, Lifestyle
Introduction
Ambulatory activity in the home and community is a critical indicator of a person’s functional mobility and health status.1 Despite achievement of full-community ambulator status, many independently ambulatory stroke survivors take fewer steps per day than age-related averages and the recommended step activity needed for health benefits.2 Although there is evidence that habitual gait speed is associated with daily ambulatory activity after stroke,3 the strength of this relationship is variable and may overestimate walking activity in chronic stroke survivors.4
One factor that has been overlooked is the incongruence between our everyday environment (dynamic, unpredictable) and the clinic environment in which gait speed is typically assessed (stationary, predictable). The purpose of this exploratory analysis was to identify whether gait speed under attention-demanding conditions (dual-task walking) accounts for additional variance in ambulatory activity, above and beyond traditional single-task gait speed.
Methods
The sample comprised 28 community-dwelling adults, 18 years or older, within 3 years of stroke, who could walk continuously for 50 meters without assistance of another person and follow 3-step commands. Exclusion criteria were greater than 1 fall in last 12 months, speech deficits, pre- or co-existing neurological conditions, uncorrected hearing or visual impairments, and orthopedic conditions affecting gait. Study procedures were approved by the Institutional Review Board and participants provided informed consent. The data that support the findings of this study are available from the corresponding author upon reasonable request.
Participants completed assessments to characterize cognition, motor impairment, functional mobility, walking endurance, and balance self-efficacy. A classic dual-task paradigm was used to assess cognitive-motor dual-task performance, involving performance of each task in isolation (single-task) and in combination (dual-task). The cognitive task was the auditory Stroop task,5 which engages executive functions.6 Single-task performance of the Stroop task was recorded in sitting. Reaction time and response accuracy were measured.
The gait task required participants to walk continuously on a level surface for at least 48 meters providing, on average, 39 steady-state strides for spatiotemporal analysis. Gait data were acquired using a 5-node wireless ambulatory system (LEGSys™) (n=25) while walking along a 30-m walkway with a single turn at one end or during 6 continuous passes (n=3) over an 8-m instrumented walkway (GAITRite®).
Spontaneous daily ambulatory activity was captured over at least two consecutive days using an unobtrusive physical activity monitoring system (PAMSys™). The inertial sensors identified postural positions and movements over the two-day observation period, which yields optimum compromise between reliability and adherence.7 The participants were instructed to remove the activity monitor during sleeping hours and for bathing. Validated signal processing algorithms were used to identify physical activity of the user.8
To examine whether dual-task gait speed accounts for variance in daily ambulatory activity (steps per day) above what can be predicted with single-task gait speed, we entered the variables sequentially into a regression to identify significant changes in R-squared value. Since scatterplots of the relationships between gait speed and steps per day suggested a non-linear relationship, we used a polynomial regression, residual plots and parameter estimates to determine best curve fit for both single-task and dual-task gait speed in separate models prior to sequential regression models to determine which terms would be appropriate in the full model. The quadratic term significantly improved model fit for dual-task gait speed (R2 change=15.9%, P=0.01; Figure 1) but not single-task gait speed (R2 change=10.1%, P=0.06). Therefore, we used both the linear and quadratic terms for dual-task gait speed but retained only the linear term for single-task gait speed in the overall regression analysis.9 To assess the final regression model fit, we examined the residual plots and parameter estimates. Although there was one potential outlier for the multivariate model, there were no violations of the standard assumptions for linear regression.
Figure 1.
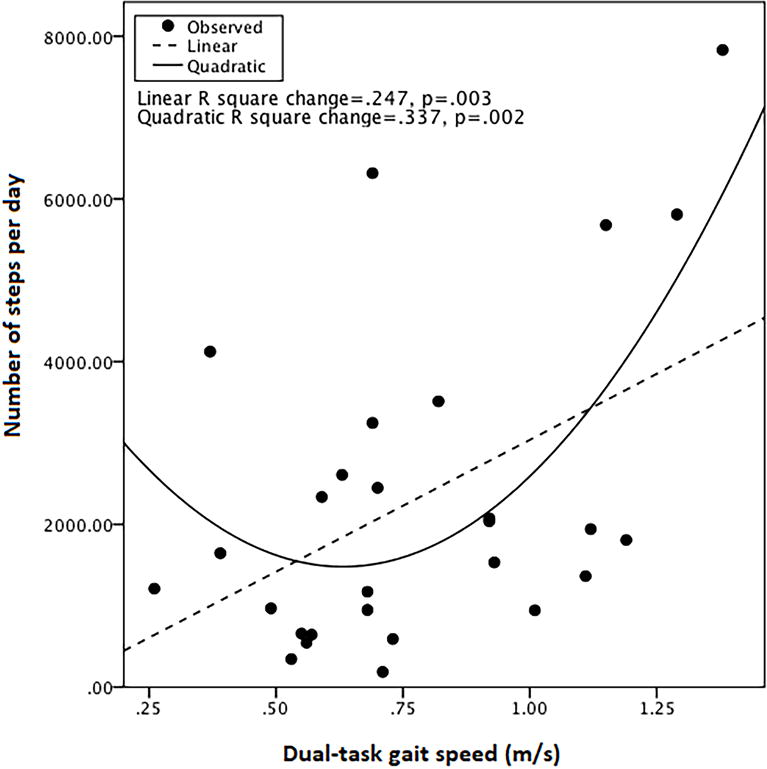
Test of model fit for dual-task gait speed and steps per day
Results
The 28 participants (61% male) were, on average, 58.2 (SD=16.6) years old and 8.9 months post stroke (IQR=3.7-19.4). The majority (71%) had ischemic strokes of left hemisphere (54%). Forty-three percent of the participants used an assistive device and 29% used bracing to walk. Additional characteristics are summarized in Table 1.
Table 1.
Participant characteristics
| Mean/Median | SD/IQR | |
|---|---|---|
| Montreal Cognitive Assessment (max. 30) | 26.0 | 24.0-27.0 |
| Lower Extremity Fugl-Meyer Assessment (max. 34) | 26.4 | 5.6 |
| 6-minute Walk Test (m) | 312.6 | 133.6 |
| Timed Up and Go Test (s) | 13.6 | 10.5-18.7 |
| Activities-specific Balance Confidence Scale (max. 100) | 67.9 | 20.7 |
Gait speed in the dual-task condition (mean=0.77 m/s; SD=0.29) was significantly slower than in the single-task condition (mean=0.82 m/s; SD=0.30), P=0.03. There was no difference in Stroop reaction time between single and dual-task conditions. However, Stroop-task accuracy was significantly worse in the dual-task condition (median=94%, IQR=78.5-100%) than the single-task condition (median=100%, IQR=90.5-100%), P=0.001. The physical activity monitor was worn, on average, for 2.5 days and 10.5 (SD=3.5) hours per day. There was no significant difference in daily step count between days 1 and 2, (P>0.05) and the ICC2,1 was 0.81.
The regression analysis indicated that single-task gait speed explained 15.3% of the variance in the number of steps per day (P=0.04). Adding dual-task gait speed increased the R-squared value by 20.6% (P=0.04) (Table 2). Together, single and dual-task gait speed explained 35.9% (adjusted R2=27.9%) of the variance in daily ambulatory activity. Since single-task gait speed became non-significant in the combined model, excluding single-task gait speed from the regression produced similar R-squared values as model 2 (Table 2).
Table 2.
Regression model summary
| Model | R | R Square | Adjusted R Square | Std. Error of the Estimate | Change Statistics | Std. Coefficients for Single-Task Gait Speed | ||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| R Square Change | Sig. F Change | Beta | Sig. | |||||
| 1 | .391a | .153 | .120 | 1860.83 | .153 | .040 | .391 | 0.04 |
| 2 | .599b | .359 | .279 | 1684.93 | .206 | .035 | −.110 | 0.84 |
| 3 | .598c | .358 | .306 | 1652.36 | .358 | .004 | – | – |
. Predictors: (Constant), Single-Task Gait Speed (m/s)
. Predictors: (Constant), Single-Task Gait Speed (m/s), Dual-Task Gait Speed (m/s), (Dual-Task Gait Speed * Dual-Task Gait Speed)
. Predictors: (Constant), Dual-Task Gait Speed (m/s), (Dual-Task Gait Speed * Dual-Task Gait Speed)
Discussion
Consistent with our expectation, including dual-task gait speed with single-task gait speed explained a larger proportion of the variance in everyday ambulatory activity than single-task gait speed alone. Furthermore, the proportion of the variance explained in this sample by including dual-task gait speed or by dual-task gait speed alone is greater than that reported for single-task gait speed previously.10 This may be, in part, because dual-task gait speed more accurately reproduces the demands of walking in the real world, where one often performs mental operations (e.g., engaging in conversation) while walking.
The observed curvilinear relationship between dual-task gait speed and steps per day was an unexpected finding and may be due to the specific distribution of our sample. Specifically, there was a small cluster of participants at the higher end of the gait speed continuum but on the low end of the steps-per-day continuum, while other fast walkers were high on the steps-per-day axis. This appears to be driving the observed curvilinear relationship (Figure 1). This finding is consistent with those of Robinson et al,11 who found more variability in self-reported walking-related activities in stroke-survivors with gait speed greater than 0.8 m/s.
Generalizability of the current findings is limited to a specific subpopulation of community-dwelling stroke survivors that are relatively young, with few comorbidities, mild or no cognitive impairment, low to moderate fall risk, and within 3 years of stroke. Daily ambulatory activity was measured over 2-3 consecutive days; this relatively short timeframe may not provide sufficient consistency to characterize habitual walking activity.12 However, the ICC2,1 value of 0.81 indicates good agreement13 between step activity over the assessment period. Although the PAMSys™ provided objective data to quantify daily step activity, we cannot determine if the participants were walking in their home or community. This is a limitation of physical activity monitoring in general and is not exclusive to this study.
Conclusions
Dual-task gait speed may improve explanation of the variance in daily ambulatory activity in community-dwelling stroke survivors. Future research should consider assessing the contribution of dual-task gait speed in predicting physical activity after stroke.
Supplementary Material
Acknowledgments
Sources of Funding
This research was supported in part by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (1R21HD076157-01A1).
Footnotes
Disclosures
None.
References
- 1.Chan CB, Spangler E, Valcour J, Tudor-Locke C. Cross-sectional relationship of pedometer-determined ambulatory activity to indicators of health. Obesity Research. 2003;11:1563–1570. doi: 10.1038/oby.2003.208. [DOI] [PubMed] [Google Scholar]
- 2.Michael K, Macko RF. Ambulatory activity intensity profiles, fitness, and fatigue in chronic stroke. Topics in stroke rehabilitation. 2007;14:5–12. doi: 10.1310/tsr1402-5. [DOI] [PubMed] [Google Scholar]
- 3.Bowden MG, Balasubramanian CK, Behrman AL, Kautz SA. Validation of a speed-based classification system using quantitative measures of walking performance poststroke. Neurorehabil Neural Repair. 2008;22:672–675. doi: 10.1177/1545968308318837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fulk GD, He Y, Boyne P, Dunning K. Predicting home and community walking activity poststroke. Stroke. 2017;48:406–411. doi: 10.1161/STROKEAHA.116.015309. [DOI] [PubMed] [Google Scholar]
- 5.Cohen G, Martin M. Hemisphere differences in an auditory stroop test. Percept Psychophys. 1975;17:79–83. [Google Scholar]
- 6.Siu K-C, Catena RD, Chou L-S, Van Donkelaar P, Woollacott MH. Effects of a secondary task on obstacle avoidance in healthy young adults. Exp Brain Res. 2008;184:115–120. doi: 10.1007/s00221-007-1087-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.de Bruin ED, Najafi B, Murer K, Uebelhart D, Aminian K. Quantification of everyday motor function in a geriatric population. J Rehabil Res Dev. 2007;44:417–428. doi: 10.1682/jrrd.2006.01.0003. [DOI] [PubMed] [Google Scholar]
- 8.Aminian K, Najafi B. Capturing human motion using body-fixed sensors: Outdoor measurement and clinical applications. Computer animation and virtual worlds. 2004;15:79–94. [Google Scholar]
- 9.Peixoto JL. Hierarchical variable selection in polynomial regression models. The American Statistician. 1987;41:311–313. [Google Scholar]
- 10.Mudge S, Stott NS. Timed walking tests correlate with daily step activity in persons with stroke. Archives of physical medicine and rehabilitation. 2009;90:296–301. doi: 10.1016/j.apmr.2008.07.025. [DOI] [PubMed] [Google Scholar]
- 11.Robinson CA, Shumway-Cook A, Matsuda PN, Ciol MA. Understanding physical factors associated with participation in community ambulation following stroke. Disabil Rehabil. 2011;33:1033–1042. doi: 10.3109/09638288.2010.520803. [DOI] [PubMed] [Google Scholar]
- 12.Berlin JE, Storti KL, Brach JS. Using activity monitors to measure physical activity in free-living conditions. Physical therapy. 2006;86:1137–1145. [PubMed] [Google Scholar]
- 13.Portney L, Watkins M. Foundations of clinical research: Application to practice. Stamford, USA: Appleton & Lange; 1993. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


