Abstract
Background/Aims
Dietary therapy is increasingly used to manage gastrointestinal (GI) symptoms in patients with irritable bowel syndrome (IBS). We aim to gauge United States gastroenterologists’ perceptions of dietary therapies for IBS.
Methods
We distributed a 22-question survey to members of the American College of Gastroenterology. The survey was developed by gastroenterologists and survey methodologists. We collected information pertaining to demographics, providers’ interpretation of their patients’ views on dietary therapy, and gastroenterologists’ perceptions on dietary therapy, and nutritional counseling in IBS.
Results
One thousand five hundred and sixty-two (14%) surveys were collected. Nearly 60% of participants reported that patients commonly associate food with GI symptoms. IBS patients most commonly use a trial and error approach followed by a lactose-free and gluten-free diet, and rarely use a low fermentable oligosaccharides, disaccharides, monosaccharides, and polyols (FODMAP) diet on their own. Over half of providers recommend diet therapy to > 75% of IBS patients and most commonly recommend a low FODMAP diet. Only 21% of gastroenterologists commonly refer IBS patients to registered dietitians, and only 30% use GI dietitians. Female providers were more likely than males to recommend dietary changes as the primary mode of therapy (OR, 1.43 [1.09–1.88]; P = 0.009).
Conclusions
Our national survey identified enthusiasm for diet treatment of IBS. While patients infrequently tried a low FODMAP diet on their own, GI providers commonly recommended this diet. Only a minority of GI providers refer their IBS patients to a registered dietitian for nutrition counseling and few refer patients to dietitians with specialized GI training. Female providers were more enthusiastic about diet therapies than males.
Keywords: Dietitian, Diet therapy, Irritable bowel syndrome
Introduction
Irritable bowel syndrome (IBS) is a chronic, functional gastrointestinal (GI) disorder characterized by recurring episodes of abdominal pain, bloating, and changes in stool quality and quantity. It represents one of the most commonly diagnosed GI disorders with a prevalence of 10–20% worldwide.1–4 IBS is associated with a high morbidity and accounts for billions of dollars in direct and indirect medical costs in the United States (US).5,6 The pathogenesis of this disorder is exceedingly complex and likely multifactorial, secondary to abnormalities in motility, visceral sensation, brain-gut interactions, intestinal permeability, immune activation, neuroendocrine function, bile acids, and the gut microbiome. While true food allergies are uncommon in IBS, several studies have indicated that IBS patients attribute exacerbations of their GI symptoms to the ingestion of particular foods, including certain carbohydrates, fruits and vegetables, dairy products, beans, and legumes.7–12
Several dietary manipulations have subsequently been investigated in the treatment of IBS, including high-fiber diets, gluten-free diets, lactose-reduced diets, low fat diets, and diets low in fermentable oligosaccharides, disaccharides, monosaccharides, and polyols (FODMAPs).13–19 FODMAPs are short-chain carbohydrates that are poorly or incompletely absorbed in the small intestine and subsequently fermented by the colonic microbiota, leading to the production of short-chain fatty acids and gases such as hydrogen, carbon dioxide, and methane.7,20 They are found in foods such as wheat, garlic, onions, sweeteners, and some fruits and vegetables. Gluten, on the other hand, is a storage protein commonly found in wheat, rye, and barley.
Despite the widespread interest in the role that diet plays in IBS, data reflecting the national views of gastroenterologists on dietary therapy is limited. In addition, there is a paucity of studies evaluating whether or not provider gender plays a role in how dietary therapy is prescribed. While female representation in gastro-enterology is increasing, the field remains predominantly male, and it is unclear how this affects dietary practices.21
The purpose of this study is to describe how gastroenterologists currently approach the use of dietary therapy in the management of IBS patients. More specifically, we hoped to determine whether or not providers’ recommendations regarding dietary interventions differed from patients’ pre-consultative dietary behaviors, as well as aimed to identify any specific practice patterns that may warrant additional education and review. In addition, we sought to determine whether demographic factors such as provider gender, years of experience, or type of practice setting affected overall views and recommendations regarding dietary therapy.
Materials and Methods
Overview
We developed a 22-item multiple-choice survey to assess how gastroenterologists approach the dietary management of IBS. Other secondary outcomes of this study were to obtain providers’ reports of their patients’ views on dietary therapy, to determine the frequency with which gastroenterologists recommend specific diets, to assess the value of registered dietitians and other modalities of nutritional education in IBS management, to investigate the barriers to delivering effective dietary interventions to patients with IBS, and to assess how these variables were affected by gender differences among survey participants.
Survey Design
The survey was developed by 2 practicing gastroenterologists, one gastroenterology fellow, 3 registered dietitians, and one survey methodologist. The survey was reviewed by each of these individuals and modified until all stakeholders agreed on the survey content. The survey was then pilot tested among 25 gastroenterologists in different community and academic settings, as well as among 3 different advanced practice practitioners (nurse practitioners and physician’s assistants) prior to distribution. Feedback from these providers was used to further modify the survey instrument.
The survey comprised of 4 main sections. The first section collected basic demographic information, including an assessment of participant gender, board certification, years of training in gastroenterology, primary practice site, region of practice, and percentage of outpatient clinic time spent treating patients with IBS. The second section included questions specifically related to the provider’s interpretation of their patients’ perceptions regarding foods that provoke GI symptoms and their patients’ initial self-management of their IBS. The third section pertained to gastroenterologists’ approach to the dietary management of IBS, including an inquiry into how physicians are prescribing specific diets and their subsequent views of the efficacy of these interventions. The fourth section assessed which resources are being utilized for nutritional advice and counseling (including the use of registered dietitians), and what barriers exist to providing effective dietary interventions to IBS patients (ie, complexity of the diet, potential expense of the diet, insurance coverage for dietician visits, meal preparation time, etc). The entire survey instrument can be found in the Appendix.
Study Population
The finalized survey was distributed electronically to all practicing gastroenterologists and gastroenterologists in training who were active members of the American College of Gastroenterology (ACG). The survey was administered using the principles established by the Tailored Design Method22 and was ultimately disbursed by the University of Minnesota using the Qualtrics web survey system in August 2015. A notification email regarding an upcoming survey was sent to members of the ACG 5 days prior to the final survey distribution. A reminder email was also sent to complete the survey one day prior to the conclusion of the survey period. A lottery system for gift cards was used as an incentive to complete the survey.
Statistical Methods
Survey responses were summarized using simple proportions. Multivariate logistic regression analyses were performed to examine the association of provider gender with responses adjusting for years out of training, primary practice site, and percentage of outpatient practice time devoted to the management of IBS. Odds ratios (ORs) and confidence intervals were subsequently calculated for the relationship between gender and applicable variables (recommending diet as primary therapy, delivering nutritional advice via mobile apps, using continuing medical education (CME) courses on diet therapy to train physicians, etc). Statistical significance was defined as a two-sided P-value of < 0.05 for all tests. Analyses were performed using SAS (v9.3; SAS Institute, Cary, North Carolina, USA).
Results
Participant Demographics
A total of 10 952 surveys were emailed to physician members of the ACG. Out of these emails, 424 emails bounced and 10 528 emails were successfully delivered. There were a total of 1417 complete responses and 145 partial responses, totaling 1562 received surveys (14.3% response rate). The majority of respondents were men (75.0% men vs 24.1% women), which is in concordance with the overall membership of the ACG and traditional gender disparities within the field of gastroenterology.21,23 Other characteristics of the population of respondents were similar to the overall membership of the ACG. The vast majority of respondents were board certified in gastroenterology (84.0%) and had completed their GI training over 20 years prior (36.7%). The survey population represented a geographically diverse group of US providers (South 33.2%, Northeast 27.1%, Midwest 23.1%, and West 16.6%). GI physicians who participated in this survey were most likely to practice either in an academic (41.9%) or a private GI setting (32.4%). Survey respondents also indicated that they spend a substantial proportion of their time caring for patients with IBS. For instance, over three-quarters of GI providers spend 10–50% of their time in the clinic caring for IBS patients. Additional characteristics of the study population are described in Table 1.
Table 1.
Respondent Demographics
| Physician factor | Respondents (n [%]) |
|---|---|
| Gender | |
| Male | 1175/1549 (75.9) |
| Female | 374/1549 (24.1) |
| Level of training | |
| Board certified/eligible gastroenterologist | 1289/1535 (84.0) |
| Fellow-in-training | 246/1535 (16.0) |
| Years out from GI training | |
| Less than 1 yr | 95/1282 (7.4) |
| 1–5 yr | 310/1282 (24.2) |
| 6–10 yr | 169/1282 (13.2) |
| 11–15 yr | 102/1282 (8.0) |
| 16–20 yr | 135/1282 (10.5) |
| Over 20 yr | 471/1282 (36.7) |
| Primary practice site | |
| Academic | 627/1498 (41.9) |
| Multi-specialty group | 342/1498 (22.8) |
| GI solo | 486/1498 (32.4) |
| Veterans association | 43/1498 (2.9) |
| Region of practice | |
| Northeast | 418/1544 (27.1) |
| Midwest | 357/1544 (23.1) |
| South | 513/1544 (33.2) |
| West | 256/1544 (16.6) |
| Percentage of outpatient clinic time spent treating Patients with IBS | |
| Less than 10% | 148/1514 (9.8) |
| 10–25% | 699/1514 (46.2) |
| 26–50% | 490/1514 (32.4) |
| 51–75% | 146/1514 (9.6) |
| More than 75% | 31/1514 (2.0) |
GI, gastrointestinal; IBS, irritable bowel syndrome.
“n” is variable secondary to partial survey responses and exclusion of fellows-in-training from answering certain demographic questions.
Patient’s Approach to the Self-management of Irritable Bowel Syndrome
Nearly 60% of surveyed gastroenterologists reported that their patients “usually” (45.6%) or “almost always” (13.6%) describe an association between consuming food and the development of GI symptoms. Another 37.1% reported that their patients “sometimes” describe this association. Similarly, survey participants indicated that over half of IBS patients “usually” (38.8%) or “almost always” (13.8%) attempt to self-manage their IBS symptoms prior to seeking advice from a gastroenterologist. We also asked GI providers to report how often their patients had tried different diet interventions, including a “trial and error” approach, lactose restriction, gluten restriction, low fat, or a low FODMAP diet, prior to seeing them for the first time. From highest to lowest, the proportion of providers who indicated that their patients had “usually” or “almost always” tried each diet were: trial and error (50%), lactose-reduced (33%), gluten-free (24%), low fat (6%), and low FODMAP (2%). Consistent with that, 70% of GI providers reported that their IBS patients had either “rarely” or “almost never” tried a low FODMAP diet before their initial visit (Table 2).
Table 2.
How Often Will Patients Have Tried the Following Diets Before Being Seen by a Gastroenterologist?
| Almost never | Rarely | Sometimes | Usually | Almost always | Total responses | |
|---|---|---|---|---|---|---|
| Trial and error | 53 (3.6) | 117 (8.1) | 562 (38.7) | 539 (37.1) | 181 (12.5) | 1452 |
| Lactose-free | 31 (2.1) | 184 (12.4) | 787 (52.8) | 409 (27.4) | 79 (5.3) | 1490 |
| Gluten-free | 45 (3.0) | 245 (16.4) | 839 (56.3) | 309 (20.7) | 53 (3.6) | 1491 |
| Low fat | 329 (22.2) | 708 (47.9) | 349 (23.6) | 80 (5.4) | 13 (0.9) | 1479 |
| Low FODMAP | 737 (49.6) | 532 (35.8) | 184 (12.4) | 25 (1.7) | 8 (0.5) | 1486 |
FODMAP, fermentable oligosaccharides, disaccharides, monosaccharides, and polyols.
Total number of gastroenterologists responding that their patients will have used the following diets to self-manage their irritable bowel syndrome (IBS). The number within each parenthesis indicates the percentage of total respondents.
Physician’s Perceptions of Dietary Interventions for Irritable Bowel Syndrome
Our survey population endorsed substantial confidence in diet therapies for IBS. Three-quarters of surveyed providers reported that they recommend diet therapies to at least half of their IBS patients, and over half of providers recommend diet therapies to over 75% of their IBS patients. Over half of surveyed gastroenterologists viewed diet modification as a primary (rather than secondary) management strategy for IBS. When asked about the effectiveness of diet therapies relative to other available treatments for IBS, we were surprised to find that over 90% of survey respondents indicated that diet was “about the same” (45%), “better” (41%), or “much better” (5%). Three-quarters of respondents felt that scientific evidence was “important” or “very important” to their decision of whether or not to recommend diet therapies.
Physicians were also questioned regarding how often they recommend specific diet interventions to their IBS patients, including lactose reduced, gluten-free, low FODMAP, high fiber, and low fat diets. From highest to lowest, the proportion of providers who recommended each diet “usually” or “almost always” were: low FODMAP (77%), high fiber (45%), lactose-reduced (45%), low fat (18%), and gluten-free (12%). Though most providers did not routinely recommend a gluten-free diet, 41% of providers admitted that they recommend it “sometimes” (Table 3).
Table 3.
How Often Do Gastroenterologists Recommend the Following Diets to Irritable Bowel Syndrome Patients?
| Almost never | Rarely | Sometimes | Usually | Almost always | Total responses | |
|---|---|---|---|---|---|---|
| High fiber | 81 (5.5) | 193 (13.2) | 531 (36.2) | 454 (31.0) | 207 (14.1) | 1466 |
| Lactose-free | 45 (3.1) | 124 (8.4) | 643 (43.9) | 430 (29.3) | 224 (15.3) | 1466 |
| Gluten-free | 218 (14.9) | 461 (31.5) | 607 (41.5) | 136 (9.3) | 41 (2.8) | 1463 |
| Low fat | 261 (17.8) | 449 (30.7) | 484 (33.1) | 195 (13.3) | 75 (5.1) | 1464 |
| Low FODMAP | 41 (2.8) | 128 (8.7) | 456 (31.1) | 505 (34.4) | 338 (23.0) | 1468 |
FODMAP, fermentable oligosaccharides, disaccharides, monosaccharides, and polyols.
Total number of gastroenterologists responding how often they prescribe the following diets for irritable bowel syndrome (IBS) patients. The number within each parenthesis indicates the percentage of total respondents.
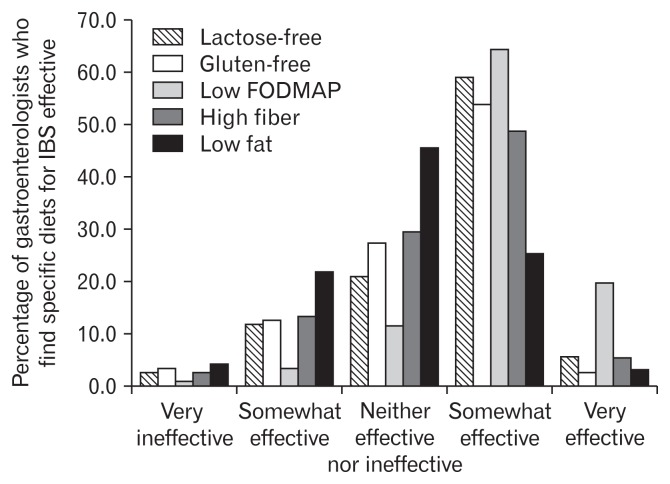
Providers perceived a low FODMAP diet to be the most effective dietary therapy for their IBS patients, with 85% of gastroenterologists reporting the low FODMAP diet to be “very effective” (20%) or “somewhat effective” (65%). A majority of surveyed gastroenterologists found a lactose-free diet (65%), a gluten-free diet (57%), and a high fiber diet (54%) to be “very effective” or “somewhat effective” for their IBS patients. A low fat diet was perceived to be the least effective dietary therapy for IBS, with only 28% of respondents finding the diet to be “very effective” or “somewhat effective” (Fig. 1).
Figure 1.
How often do gastroenterologists find specific dietary therapies effective for the treatment of irritable bowel syndrome (IBS)? FODMAP, fermentable oligosaccharides, disaccharides, monosaccharides, and polyols.
In multivariate analysis, female gastroenterologists were more likely than male gastroenterologists to recommend a low FOD-MAP diet (P < 0.001) or a gluten-free diet (P = 0.001) for their IBS patients. When adjusting for years out of training, primary practice site, and outpatient time treating IBS patients, this relationship was only significant for a gluten-free diet (P = 0.002). Female GI providers were also more likely to find a lactose-reduced diet (P = 0.001), gluten-free diet (P < 0.001), low FODMAP diet (P < 0.001), and low fat diet (P = 0.035) to be effective dietary therapy for IBS than were male providers. However, when adjusting for years out of training, primary practice site, and outpatient time treating IBS patients, female gastroenterologists were only more likely to find a gluten free diet (P < 0.001) and a low FODMAP diet (P = 0.004) to be more effective. Female gastroenterologists were also more likely than males to recommend dietary interventions as the primary mode of therapy for IBS (OR, 1.43 [1.09–1.88]; P = 0.009) (Table 4).
Table 4.
Provider Gender Differences in the Use of Dietary Therapy for Irritable Bowel Syndrome Patients
| Dietary therapy factor | Adjusted OR | 95% CI | P-value |
|---|---|---|---|
| Recommend dietary therapy as primary therapy | |||
| Male | 1.00 | ||
| Female | 1.43 | 1.09–1.88 | 0.009 |
| Deliver nutritional advice via an app for smartphone/tablet | |||
| Male | 1.00 | ||
| Female | 1.89 | 1.22–2.92 | 0.004 |
| Reporting that CME courses to train GI physicians would enhance delivery of dietary therapy to IBS patients | |||
| Male | 1.00 | ||
| Female | 1.52 | 1.18–1.97 | 0.001 |
CME, continuing medical education; GI, gastrointestinal; IBS, irritable bowel syndrome.
Dietary Counseling and Nutritional Advice
More than half of surveyed gastroenterologists were “comfortable” (38%) or “very comfortable” (18%) with providing dietary counseling to their IBS patients. Fewer than 10% were “not very comfortable” or “not at all comfortable” with this task. The most commonly used modalities to provide nutritional advice included educational handouts (81%), referral to a dietitian (70%), and verbal instructions (52%). Books (7%) and apps for smart phones/tablets (9%) were the least popular educational modalities.
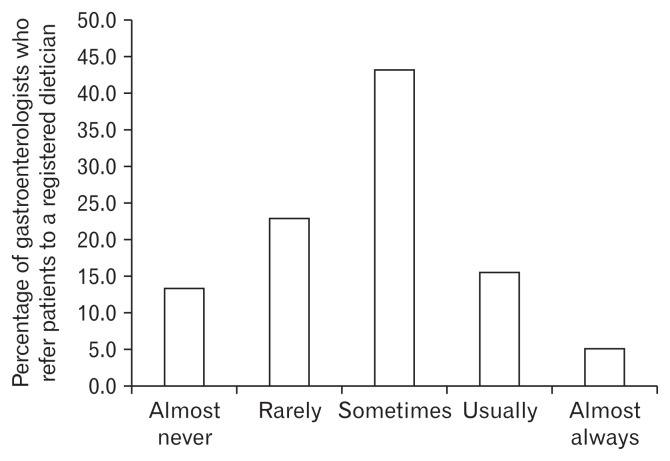
Only 21% of study participants reported that they “usually” or “almost always” referred their IBS patients to a registered dietitian for nutritional counseling (Fig. 2). When ordering a consultation with a dietitian, over 50% of gastroenterologists utilized a general dietitian. Only 30% referred their patients to a more specialized GI dietitian. Interestingly, 78% of respondents said that they believed that a registered dietitian with an IBS focus would enhance the delivery of dietary therapy to their IBS patients. When patients were ultimately referred to a registered dietitian, 51% of gastroen-terologists indicated that they “usually” or “almost always” provide specific diet recommendations to the dietitian. In addition to the enrichment provided by registered dietitians, surveyed gastroenterologists also reported that written handouts (74.7%), educational websites (72.4%), payer coverage of dietary consults and therapy (70.9%), and nutrition classes (65.4%) would help to enhance the delivery of dietary therapy to IBS patients.
Figure 2.
How often do gastroenterologists refer their irritable bowel syndrome patients to a registered dietitian?
In multivariate analysis, female GI providers were more likely than males to believe that access to a registered dietitian knowledgeable about IBS to be important in the decision of whether or not to recommend dietary therapy (P = 0.014). Female gastroenterologists were also more likely to recommend books (P = 0.012), refer patients to a dietitian (P = 0.018), and recommend an app for a smart phone/tablet (P = 0.002) than were male physicians. When adjusting for years out of training, primary practice site, and outpatient time treating IBS, this difference was only significant for using an app on a smart phone/tablet (OR, 1.89 [1.22–2.92]; P = 0.004). Female GI physicians were more likely than male GI physicians to believe that nutrition classes (P < 0.001), CME courses to train GI physicians (P < 0.001), and increased availability of registered dietitians with an IBS focus (P = 0.005) could enhance the delivery of dietary therapy to patients. When adjusting for years out of training, primary practice site, and outpatient time treating IBS patients, this relationship was only significant for CME courses (OR, 1.52 [1.18–1.97]; P = 0.001) (Table 4).
There were several factors that surveyed gastroenterologists believed to be potential barriers to providing effective dietary interventions to their IBS patients. The most significant of which included the complexity of dietary therapy (39.1% and 11.4% of physicians indicated that this is usually or always a hindrance) and the insurance coverage for dietitian visits (24.1% and 16.9% of physicians believed this to usually or almost always be a barrier).
Discussion
Our survey of over 1500 members of the ACG represents the largest survey to address gastroenterologists’ perceptions and practices surrounding food in the management of IBS. The association between food intake and GI symptoms is commonly based on previously published surveys of IBS patients.9 Similarly, our study found that GI providers believe that almost 60% of IBS patients relate their GI symptoms to eating a meal. This common association may account for why such a large proportion of IBS patients have tried diet manipulations to relieve their intestinal discomfort prior to seeking the advice of a gastroenterologist.
We were surprised with how favorably US GI providers viewed diet therapies compared to other available treatments for IBS patients. Over 90% of respondents felt that diet therapies were at least as good or better than other existing pharmacologic therapies for IBS. It is difficult to know whether this sentiment reflects the effectiveness of diet therapies, the marginal efficacy of available medical treatments, or a bit of both. Recent randomized, controlled trials suggest that diet therapies provide adequate relief to 50–70% of IBS sufferers.17,19,24,25 This compares quite favorably to the efficacy of Food and Drug Administration approved medical therapies for IBS, which typically provide adequate relief of GI symptoms in 20–60% of patients.26–31
Given these findings, perhaps it should not be surprising that more than three-quarters of GI providers recommended diet changes to the majority of their IBS patients. Our survey did not assess the quality of the diet instruction provided to IBS patients. An interesting survey study recently reported that while 98% of doctors claimed to provide dietary advice to their inflammatory bowel disease (IBD) patients, only 26% of surveyed IBD patients reported that they received dietary advice from their IBD doctor.32 Our study also identified some interesting disconnects between IBS patients and GI providers. Surveyed gastroenterologists indicated that their IBS patients most often took a “trial and error” approach to their diet, followed by pursuing a lactose-reduced diet. Almost a quarter of GI providers reported that their IBS patients had tried a gluten-free diet before seeking consultation, while their IBS patients had rarely tried a low FODMAP diet. On the other hand, GI providers most commonly recommended the low FODMAP diet to their IBS patients, with over 85% of survey respondents recommending this diet at least “sometimes.” GI providers were less enthusiastic about a gluten-free diet. One explanation for why gastroenterologists uncommonly recommend the lactose-free and gluten-free diets may be that their patients have already tried these diets on their own and are now requiring more guidance with the complex low FODMAP diet. These observations are also interesting as there is mounting evidence to support a role for both the low FODMAP diet and a gluten free diet in IBS patients.15,16,33
Multiple observational and randomized controlled trials have demonstrated that a low FODMAP diet may reduce the frequency and severity of GI symptoms in IBS patients.19,24,25,34,35 However, it is important to note that long-term efficacy and safety data are currently lacking and many of the existing studies have significant methodological limitations.8 Of course, this statement could fairly be applied to all dietary interventions offered to IBS patients, and many of the previous criticisms of the low FODMAP diet trials have recently been addressed in a study by Staudacher et al.36 The results of our study indicate that the majority of US GI providers are conscious of this growing body of evidence in support of the low FODMAP diet and are now frequently recommending this diet to their IBS patients.
Gluten has been shown to induce GI symptoms in some IBS patients without celiac disease, and this has sparked interest in an entity currently referred to as non-celiac gluten sensitivity (NCGS). Several studies have found that a gluten-free diet may improve GI symptoms and frequency of bowel movements in patients with IBS and diarrhea.15,16 However, some controversy still exists regarding the significance of NCGS as a discrete entity, with some studies suggesting that symptoms provoked by gluten may largely be secondary to concurrent FODMAP ingestion.33 For those patients that do experience symptom improvement with a gluten-free diet, this is likely to be driven by several factors, including restriction of proteins such as gluten or amylase trypsin inhibitors, restriction of poorly absorbed carbohydrates such as fructans, or the nocebo effect. Thus, the term “non-celiac gluten sensitivity” misrepresents this diverse population of patients, which might more accurately be referred to as “non-celiac wheat intolerance.”
This study also revealed noteworthy information regarding gastroenterologists’ perceptions of dietary education for IBS. Interestingly, the comfort level of surveyed GI providers in delivering dietary counseling to IBS patients was somewhat mixed, with around half of physicians reporting comfort with this task and the other half expressing reservations. Of note, it is unclear if physicians’ answer to this question affected their subsequent responses to other questions about the specific dietary therapies they prescribe. In addition, only a minority of physicians would frequently refer their IBS patients to a registered dietitian for supplemental nutritional advice. This is somewhat concerning, as recent studies showed registered dietitians to be superior to non-trained providers in successfully implementing dietary interventions in IBS.34,37
Several discrepancies also existed regarding gastroenterologists’ preferences in choosing a specific dietitian. The majority of physicians would refer their IBS patients to a general dietitian outside of their GI group, whereas few physicians would use a specialized GI dietitian. However, over 70% of gastroenterologists believed having direct access to registered dietitians with an IBS focus would enhance the delivery of dietary therapy. When considering complex, multi-step, highly restrictive interventions like the low FODMAP diet, the distinction between a general dietitian who may or may not have experience in caring for patients with GI disorders and a GI dietitian is particularly important. The results of our study indicate that gastroenterologists infrequently utilize specially trained GI dietitians and instead are opting to refer patients to general dietitians, even though the majority believes that GI dietitians would be of benefit to their IBS patients. This could imply that the choice to refer IBS patients to general dietitians may be more of a reflection of availability and access to GI dietitians than actual preference for general dietitians. On the other hand, the limited use of GI dietitians may also be a reflection of the severity of IBS cases that certain physicians encounter. For instance, a registered, general dietitian may be adequate for dietary education in mild to moderate cases of IBS, whereas specialized GI dietitians may be necessary in more severe or complicated scenarios. However, this is beyond the spectrum of our study and would require further investigation. It is also important for gastroenterologists to emphasize to their patients that the low FODMAP diet is not a strict lifetime diet, and it extends across 3 distinct stages: restriction, reintroduction, and maintenance. This requires a considerable amount of time and investment by patients and providers, illustrating gastroenterologists’ increasing need for access to dietitians with adequate interest and training in nutritional interventions for GI conditions.
In addition to referring patients to registered dietitians, surveyed gastroenterologists commonly used educational handouts to help deliver nutritional advice to IBS patients. Printed information sheets represent one of the simplest methods of delivering nutritional advice. However, providers are cautioned against using a handout as a lone means of educating patients about complex interventions like the low FODMAP diet. Patients should ideally be referred to a GI dietitian, but if this is not feasible, other educational material (such as handouts) should be provided to help guide patients through the elimination, reintroduction, and maintenance phases of the plan. Educational websites and apps for smart phones are other newer tools with the advantages of engaging comprehensive education and symptom monitoring capabilities38; however, fewer than half of GI providers felt that such means would enhance their ability to provide dietary therapies to their IBS patients. This may be secondary to a lack of awareness of such resources, or perhaps it is a reflection of how well patients are responding to the more traditional methods of verbal communication combined with instructional handouts.
Of the subgroup analyses we conducted, comparisons between perceptions and practices of female vs male providers merits special attention. Our survey identified a significant difference in the dietary management of IBS patients between female and male GI providers. For instance, when adjusting for confounding variables, females were more likely to use dietary interventions as the primary mode of therapy for IBS patients than were males. Female GI providers were also more likely to prescribe a gluten-free diet and to find both a gluten-free diet and a low FODMAP diet more efficacious than were males. While the reasons for this are unclear, it is interesting to wonder if there are inherent gender differences in the way men and women perceive nontraditional treatments such as diet therapies versus more traditional medical therapies. Or perhaps women are more diet conscious than men, leading them to prescribe certain diets with a higher frequency. Female GI physicians were also more likely than males to recommend using an app on a smart phone or tablet to help deliver dietary advice. Similarly, a recent study by Elavsky et al39 also found that individuals who use mobile apps for nutrition, weight loss, and fitness are more likely to be female. Further research is needed to determine whether gender discrepancies in the use of health related mobile apps are consistent, or if these findings could potentially influence the development of future dietary applications.
Another interesting observation was the marked variability in regional response rates to our survey, with the majority of responders residing in the Southern regions of the US. Although this was unlikely to lead to bias in those recommending dietary solutions, additional research may be warranted to determine if this is a stable finding, as it could potentially indicate the need to modify survey methodology on a regional basis in the future. Our study also has a number of potential limitations, which should be taken into consideration when interpreting the results. One particular limitation is the potential for response bias. For example, the GI providers choosing to participate in this study may have had a particular interest in IBS or increased background knowledge of dietary interventions. Though response bias is possible, we would point out that our response rate of 14% and sample size of over 1500 US GI providers represents the largest survey addressing dietary therapies for IBS conducted to date. In addition, our survey was only distributed to gastroenterologists and did not include input from actual patients, primary care physicians, or nurse practitioners. Results pertaining to patients’ dietary practices were rather extrapolated from the beliefs of the surveyed gastroenterologists. Primary care physicians and mid-level practitioners are often the principle providers for a number of patients with IBS, and further studies would be needed to determine if any differences exist between the practice patterns of these primary providers and those of gastroenterologists.
Another limitation of any survey study is whether participants’ responses to questions accurately reflect their actions in clinical practice. This survey was administered using a web-based platform, and it is possible that this may have introduced bias by excluding GI providers without access to the Internet. In the age of electronic health records, this seems unlikely to have significantly affected our results. Finally, this survey was conducted in 2015. It would be very interesting to repeat the survey again to see if perceptions and practices regarding dietary therapies for IBS have changed or evolved. Given the substantial number of published studies on the low FODMAP diet since this time, we would anticipate an even greater awareness and utilization of this diet in clinical practice.
A complex relationship exists between diet and the provocation of GI symptoms in IBS patients, and there is an ever-expanding body of evidence to support a role for dietary therapy in this population. Overall, GI providers who participated in this survey expressed a favorable view of the value and effectiveness of dietary intervention in IBS patients. However, a discrepancy was identified between the initial type of diet utilized by patients and that which was recommended by physicians. There is increasing evidence to support the efficacy of the low FODMAP diet in IBS patients, and our observed disconnect highlights the need for increased patient education on this topic. Overall, this survey has highlighted the nationwide practice patterns of gastroenterologists regarding dietary therapies for IBS patients. It has additionally illustrated the need for dietitians knowledgeable in the dietary management of IBS.
Supplementary Information
Acknowlegements
We thank Scott Lunos (statistical analyses), Todd Rockwood (survey content, design, and methodology), Barb Benson (survey content expert), Shelly Wymer (preparation and transmission of the electronic survey), and start-up grant of Department of Medicine, University of Minnesota Medical School.
Footnotes
Financial support: None.
Conflicts of interest: None.
Author contributions: Adrienne Lenhart: original manuscript writing and editing and data interpretation; Courtney Ferch: survey design and methodology; Michael Shaw: survey design and methodology, data interpretation, statistical analysis, and manuscript editing; and William D Chey: survey design and methodology, data interpretation, manuscript editing, and supervision.
References
- 1.Mayer EA. Clinical practice. Irritable bowel syndrome. N Engl J Med. 2008;358:1692–1699. doi: 10.1056/NEJMcp0801447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lovell RM, Ford AC. Global prevalence of and risk factors for irritable bowel syndrome: a meta-analysis. Clin Gastroenterol Hepatol. 2012;10:712–721. doi: 10.1016/j.cgh.2012.02.029. [DOI] [PubMed] [Google Scholar]
- 3.Jones R. Treatment of irritable bowel syndrome in primary care. BMJ. 2008;337:a2213. doi: 10.1136/bmj.a2213. [DOI] [PubMed] [Google Scholar]
- 4.Drossman DA, Camilleri M, Mayer E, Whitehead WE. AGA technical review on irritable bowel syndrome. Gastroenterology. 2002;123:2108–2131. doi: 10.1053/gast.2002.37095. [DOI] [PubMed] [Google Scholar]
- 5.Cash B, Sullivan S, Barghout V. Total costs of IBS: employer and managed care perspective. Am J Manag Care. 2005;11(1 suppl):S7–S16. [PubMed] [Google Scholar]
- 6.Talley NJ, Gabriel SE, Harmsen WS, Zinsmeister AR, Evans RW. Medical costs in community subjects with irritable bowel syndrome. Gastroenterology. 1995;109:1736–1741. doi: 10.1016/0016-5085(95)90738-6. [DOI] [PubMed] [Google Scholar]
- 7.Chey WD. Food: the main course to wellness and illness in patients with irritable bowel syndrome. Am J Gastroenterol. 2016;111:366–371. doi: 10.1038/ajg.2016.12. [DOI] [PubMed] [Google Scholar]
- 8.Krogsgaard LR, Lyngesen M, Bytzer P. Systematic review: quality of trials on the symptomatic effects of the low FODMAP diet for irritable bowel syndrome. Aliment Pharmacol Ther. 2017;45:1506–1513. doi: 10.1111/apt.14065. [DOI] [PubMed] [Google Scholar]
- 9.Böhn L, Störsrud S, Törnblom H, Bengtsson U, Simrén M. Self-reported food-related gastrointestinal symptoms in IBS are common and associated with more severe symptoms and reduced quality of life. Am J Gastroenterol. 2013;108:634–641. doi: 10.1038/ajg.2013.105. [DOI] [PubMed] [Google Scholar]
- 10.Locke GR, 3rd, Zinsmeister AR, Talley NJ, Fett SL, Melton LJ. Risk factors for irritable bowel syndrome: role of analgesics and food sensitivities. Am J Gastroenterol. 2000;95:157–165. doi: 10.1111/j.1572-0241.2000.01678.x. [DOI] [PubMed] [Google Scholar]
- 11.Monsbakken KW, Vandvik PO, Farup PG. Perceived food intolerance in subjects with irritable bowel syndrome-- etiology, prevalence and consequences. Eur J Clin Nutr. 2006;60:667–672. doi: 10.1038/sj.ejcn.1602367. [DOI] [PubMed] [Google Scholar]
- 12.Simrén M, Månsson A, Langkilde AM, et al. Food-related gastrointestinal symptoms in the irritable bowel syndrome. Digestion. 2001;63:108–115. doi: 10.1159/000051878. [DOI] [PubMed] [Google Scholar]
- 13.Moayvedi P, Quigley EM, Lacy BE, et al. The effect of fiber supplementation on irritable bowel syndrome: a systematic review and meta-analysis. Am J Gastroenterol. 2014;109:1367–1374. doi: 10.1038/ajg.2014.195. [DOI] [PubMed] [Google Scholar]
- 14.Moayyedi P, Quigly EM, Lacy BE, et al. The effect of dietary intervention on irritable bowel syndrome: a systematic review. Clin Transl Gastroenterol. 2015;6:e107. doi: 10.1038/ctg.2015.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vazquez-Roque MI, Camilleri M, Smyrk T, et al. A controlled trial of gluten-free diet in patients with irritable bowel syndrome-diarrhea: effects on bowel frequency and intestinal function. Gastroenterology. 2013;144:903–911.33. doi: 10.1053/j.gastro.2013.01.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Aziz I, Trott N, Briggs R, North JR, Hadjivassiliou M, Sanders DS. Efficacy of a gluten-free diet in subjects with irritable bowel syndrome-diarrhea unaware of their HLA-DQ2/8 genotype. Clin Gastroenterol Hepatol. 2016;14:696–703. e1. doi: 10.1016/j.cgh.2015.12.031. [DOI] [PubMed] [Google Scholar]
- 17.Staudacher HM, Lomer MC, Anderson JL, et al. Fermentable carbohydrate restriction reduces luminal bifidobacteria and gastrointestinal symptoms in patients with irritable bowel syndrome. J Nutr. 2012;142:1510–1518. doi: 10.3945/jn.112.159285. [DOI] [PubMed] [Google Scholar]
- 18.de Roest RH, Dobbs BR, Chapman BA, et al. The low FODMAP diet improves gastrointestinal symptoms in patients with irritable bowel syndrome: a prospective study. Int J Clin Pract. 2013;67:895–903. doi: 10.1111/ijcp.12128. [DOI] [PubMed] [Google Scholar]
- 19.Böhn L, Störsrud S, Liljebo T, et al. Diet low in FODMAPs reduces symptoms of irritable bowel syndrome as well as traditional dietary advice: a randomized controlled trial. Gastroenterology. 2015;149:1399–1407. e2. doi: 10.1053/j.gastro.2015.07.054. [DOI] [PubMed] [Google Scholar]
- 20.Shepherd SJ, Lomer MC, Gibson PR. Short-chain carbohydrates and functional gastrointestinal disorders. Am J Gastroenterol. 2013;108:707–717. doi: 10.1038/ajg.2013.96. [DOI] [PubMed] [Google Scholar]
- 21.Brotherton SE, Etzel SI. Graduate medical education, 2014–2015. JAMA. 2015;314:2436–2454. doi: 10.1001/jama.2015.10473. [DOI] [PubMed] [Google Scholar]
- 22.Dillman DA, Smyth JD, Melani L. Internet, mail, and mixed-mode surveys: the tailored design method. 3rd edn. Hoboken, NJ: John Wiley & Sons; 2009. [Google Scholar]
- 23.Diamond SJ, Thomas CR, Jr, Desai S, et al. Gender differences in publication productivity, academic rank, and career duration among U.S. academic gastroenterology faculty. Acad Med. 2016;91:1158–1163. doi: 10.1097/ACM.0000000000001219. [DOI] [PubMed] [Google Scholar]
- 24.Halmos EP, Power VA, Shepherd SJ, Gibson PR, Muir JG. A diet low in FODMAPs reduces symptoms of irritable bowel syndrome. Gastroenterology. 2014;146:67–75. e5. doi: 10.1053/j.gastro.2013.09.046. [DOI] [PubMed] [Google Scholar]
- 25.Eswaran SL, Chey WD, Han-Markey T, Ball S, Jackson K. A randomized, controlled trial comparing the low FODMAP diet vs. modified NICE guidelines in US adults with IBS-D. Am J Gastroenterol. 2016;111:1824–1832. doi: 10.1038/ajg.2016.434. [DOI] [PubMed] [Google Scholar]
- 26.Camilleri M, Lembo AJ, Lavins BJ, et al. Comparison of adequate relief with symptom, global, and responder endpoints in linaclotide phase 3 trials in IBS-C. United European Gastroenterol J. 2015;3:53–62. doi: 10.1177/2050640614555946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chey WD, Chey WY, Heath AT, et al. Long-term efficacy and safety of alosetron in women with severe diarrhea-predominant irritable bowel syndrome. Am J Gastroenterol. 2004;99:2195–2203. doi: 10.1111/j.1572-0241.2004.30509.x. [DOI] [PubMed] [Google Scholar]
- 28.Camilleri M, Northcutt AR, Kong S, Dukes GE, McSorley D, Mangel AW. Efficacy and safety of alosetron in women with irritable bowel syndrome: a randomised, placebo-controlled trial. Lancet. 2000;355:1035–1040. doi: 10.1016/S0140-6736(00)02033-X. [DOI] [PubMed] [Google Scholar]
- 29.Chey WD, Dove LS, Andrae DA, Covington PS. Early response predicts a sustained response to eluxadoline in patients with irritable bowel syndrome with diarrhea in two phase 3 studies. Aliment Pharmacol Ther. 2017;45:1319–1328. doi: 10.1111/apt.14031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Drossman DA, Chey WD, Johanson JF, et al. Clinical trial: lubiprostone in patients with constipation-associated irritable bowel syndrome--results of two randomized, placebo-controlled studies. Aliment Pharmacol Ther. 2009;29:329–341. doi: 10.1111/j.1365-2036.2008.03881.x. [DOI] [PubMed] [Google Scholar]
- 31.Chey WD, Lembo AJ, Lavins BJ, et al. Linaclotide for irritable bowel syndrome with constipation: a 26-week, randomized, double-blind, placebo-controlled trial to evaluate efficacy and safety. Am J Gastroenterol. 2012;107:1702–1712. doi: 10.1038/ajg.2012.254. [DOI] [PubMed] [Google Scholar]
- 32.Holt DQ, Strauss BJ, Moore GT. Patients with inflammatory bowel disease and their treating clinicians have different views regarding diet. J Hum Nutr Diet. 2017;30:66–72. doi: 10.1111/jhn.12400. [DOI] [PubMed] [Google Scholar]
- 33.Biesiekierski JR, Newnham ED, Irving PM, et al. Gluten causes gastrointestinal syptoms in subjects without celiac disease: a double-blind randomized placebo-controlled trial. Am J Gastroenterol. 2011;106:508–514. doi: 10.1038/ajg.2010.487. [DOI] [PubMed] [Google Scholar]
- 34.Whigham L, Joyce T, Harper G, et al. Clinical effectiveness and economic costs of group versus one-to-one education for short-chain fermentable carbohydrate restriction (low FODMAP diet) in the management of irritable bowel syndrome. J Hum Nutr Diet. 2015;28:687–696. doi: 10.1111/jhn.12318. [DOI] [PubMed] [Google Scholar]
- 35.Ong DK, Mitchell SB, Barrett JS, et al. Manipulation of dietary short chain carbohydrates alters the pattern of gas production and genesis of symptoms in irritable bowel syndrome. J Gastroenterol Hepatol. 2010;25:1366–1373. doi: 10.1111/j.1440-1746.2010.06370.x. [DOI] [PubMed] [Google Scholar]
- 36.Staudacher HM, Lomer MCE, Farquharson FM, et al. A diet low in FODMAPs reduces symptoms in patients with irritable bowel syndrome and a probiotic restores bifidobacterium species: a randomized controlled trial. Gastroenterology. 2017;153:936–947. doi: 10.1053/j.gastro.2017.06.010. [DOI] [PubMed] [Google Scholar]
- 37.O’Keeffe M, Lomer MC. Who should deliver the low FODMAP diet and what educational methods are optimal: a review. J Gastroenterol Hepatol. 2017;32(suppl 1):23–26. doi: 10.1111/jgh.13690. [DOI] [PubMed] [Google Scholar]
- 38.Ankersen DV, Carlsen K, Marker D, Munkholm P, Burisch J. Using eHealth strategies in delivering dietary and other therapies in patients with irritable bowel syndrome and inflammatory bowel disease. J Gastroenterol Hepatol. 2017;32(suppl 1):27–31. doi: 10.1111/jgh.13691. [DOI] [PubMed] [Google Scholar]
- 39.Elavsky S, Smahel D, Machackova H. Who are mobile app users from healthy lifestyle websites? Analysis of patterns of app use and user characteristics. Transl Behav Med. 2017;7:891–901. doi: 10.1007/s13142-017-0525-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.