Abstract
Classical hairy cell leukemia (HCL-c) is a rare lymphoid neoplasm. BRAFV600E mutation, detected in more than 80% of the cases, is described as a driver mutation, but additional genetic abnormalities appear to be necessary for the disease progression. For cases of HCL-c harboring a wild-type BRAF gene, the differential diagnosis of the variant form of HCL (HCL-v) or splenic diffuse red pulp lymphoma (SDRPL) is complex. We selected a panel of 21 relevant genes based on a literature review of whole exome sequencing studies (BRAF, MAP2K1, DUSP2, MAPK15, ARID1A, ARID1B, EZH2, KDM6A, CREBBP, TP53, CDKN1B, XPO1, KLF2, CXCR4, NOTH1, NOTCH2, MYD88, ANXA1, U2AF1, BCOR, and ABCA8). We analyzed 20 HCL-c and 4 HCL-v patients. The analysis of diagnostic samples mutations in BRAF (n = 18), KLF2 (n = 4), MAP2K1 (n = 3), KDM6A (n = 2), CDKN1B (n = 2), ARID1A (n = 2), CREBBP (n = 2) NOTCH1 (n = 1) and ARID1B (n = 1). BRAFV600E was found in 90% (18/20) of HCL-c patients. In HCL-c patients with BRAFV600E, other mutations were found in 33% (6/18) of cases. All 4 HCL-v patients had mutations in epigenetic regulatory genes: KDM6A (n = 2), CREBBP (n = 1) or ARID1A (n = 1). The analysis of sequential samples (at diagnosis and relapse) from 5 patients (2 HCL-c and 3 HCL-v), showed the presence of 2 new subclonal mutations (BCORE1430X and XPO1E571K) in one patient and variations of the mutated allele frequency in 2 other cases. In the HCL-v disease, we described new mutations targeting KDM6A that encode a lysine demethylase protein. This opens new perspectives for personalized medicine for this group of patients.
Keywords: hairy cell leukemia, next-generation sequencing, gene mutation, hairy cell leukemia variant, epigenetic regulation genes
INTRODUCTION
Classical Hairy cell leukemia (HCL-c) is a rare lymphoid neoplasm with an incidence rate estimated at 0.3 per 100,000 people in United States between 2011 and 2012, and 0.2 per 100,000 people for the variant form of Hairy cell leukemia (HCL-v) [1]. The diagnosis of HCL-c is based on the typical hairy morphology of lymphocytes and the identification of BRAFV600E mutation [2–4]. The BRAFV600E mutation has been described as a driver mutation and detected in the hematopoietic stem cells (HSC) from HCL-c patients [5]. However, additional genetic abnormalities seem to be necessary to induce the disease. Tumor hairy cells display additional genetic alterations that are absent in HSC harboring BRAFV600E. Whole-exome sequencing (WES) studies have highlighted additional BRAFV600E single nucleotide variants (SNV) [4, 6–8]. Some of these SNVs are probably passenger mutations, but others, because of their recurrence, appear to be more relevant to the disease.
The BRAFV600E mutation is absent in some HCL-c patients [9, 10]. In these cases, the distinction between HCL-c and the variant form of hairy cell leukemia (HCL-v) or splenic diffuse red pulp lymphoma (SRDPL) can be complex. In HCL-c patients, the absence of BRAFV600E has been associated with an unmutated immunoglobulin heavy chain variable (IGHV) gene, the preferential use of the VH4-34 gene (7–11% of cases), mutations targeting MAP2K1 (6/7 cases) and a poor prognosis [6, 10, 11]. HCL-v was introduced as provisional entity in the WHO classification of tumors in 2008 and 2016 [2, 3]. There are common characteristics between HCL-c and HCL-v, such as circulating villous lymphocytes and a histologic infiltration of the spleen with the involvement of the red pulp and atrophy of the white pulp [12]. The essential difference between the two diseases is the five-year overall survival rate: 78–92% for HCL-c and 57% for HCL-v [1, 13]. HCL-v diagnosis is essential because guidelines of care-management between HCL-c and HCL-v are different [14, 15]. The distinction between HCL-c and HCL-v is based on cytology with the presence of constant prominent nucleoli in HCL-v cells, as well as the immunophenotype. Classical hairy cells co-express CD103, CD123, CD25 and CD11c with an HCL score (one point given for each positive markers) ≥3 in 98% of cases [16]. The variant form lacks CD25 and has an HCL score <3. SDRPL, classified as a provisional entity by the WHO in 2008 and 2016, is a splenic hairy cell proliferation that is similar to HCL but quite distinct from splenic marginal zone lymphoma (SMZL) [17–19]. The distinction between HCL-v and SDRPL can be challenging because of an overlap in pathologies of the two cancers.
The next generation sequencing (NGS) approach and the sequencing of targeted genes have already proven to be useful for the diagnosis, classification and prognosis of lymphoid neoplasms [20]. Therefore, in the aim to develop a genomic diagnostic tool to distinguish these entities, we designed a panel of relevant target genes for HCL based on a literature review of WES studies [4, 6–8] and analyzed retrospectively HCL-c and HCL-v well-defined cases.
RESULTS
Single nucleotide variants (SNVs) featured in diagnosis samples
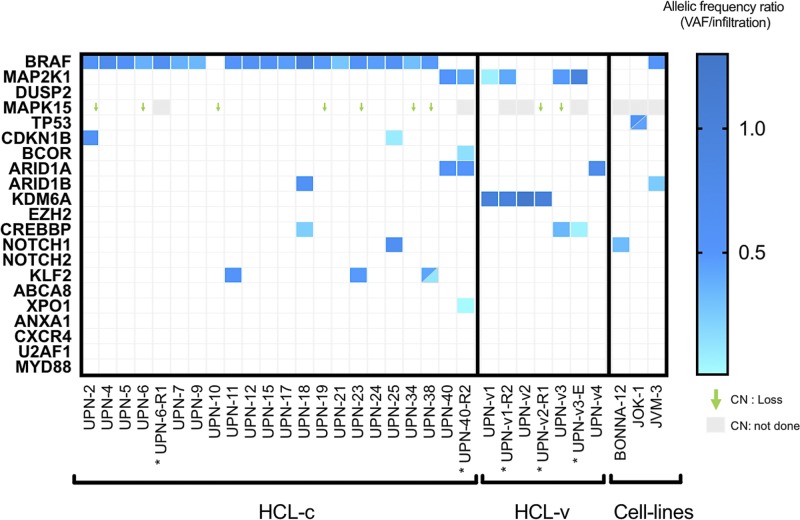
The Trichopanel was relevant for 96% (23/24) of patients. No SNVs were found in one patient (UPN-10) for any of the 21 targeted genes. The Trichopanel library sequencing yielded a median overall depth per sample of 322X [89X-533X] with 97.25% of targeted bases covered by 20 or more reads (Supplementary Table 2). For the samples obtained at diagnosis, a total of 891 variants (median per sample 37.5 [6–52]) were detected, then filtered on quality. Synonymous variations, intronic variations, and small nucleotide polymorphism (SNP) were excluded. Functional relevance was analyzed in silico using three validated algorithms (SIFT®, CADD® and polyphen2®) (Supplementary Table 5). After screening, 35 non-synonymous SNVs were validated with a range of 0–3 variants per samples (Figure 1 and Supplementary Table 5). Finally, the Trichopanel identified relevant mutations in BRAF (n = 18), KLF2 (n = 4), MAP2K1 (n = 3), KDM6A (n = 2), CDKN1B (n = 2), ARID1A (n = 2), CREBBP (n = 2), NOTCH1 (n = 1) and ARID1B (n = 1) (Figure 1).
Figure 1. Heat-map representation of mutations and CNV distribution in HCL-c and HCL-v.
Each column represents one patient (UPN), and each row is one gene of the Trichopanel. The intensity of color is proportional to the rVAF (dark blue, rVAF value close to 1; light blue, rVAF value < 0.3). Gray represents relapse/evolution samples. Mutations and rVAF details are provided in the Supplementary Table 4. The gene copy number variation was reported for the relevant gene MAPK15, CN not done in gray. Abbreviations: CN, copy number; HCL-c, hairy cell leukemia classic form; HCL-v, variant form. * Relapse/evolution samples.
Cell lines and patient characteristics
The Trichopanel was validated by the sequencing of three cell lines (BONNA-12, JOK-1 and JVM-3). In agreement with previously published data, we found no BRAFV600E mutations in these cell lines, but other mutations were found (e.g., NOTCH1T2466M in BONNA-12, BRAFK601N in JVM-3 [21]) (COSMIC Cell lines project http://cancer.sanger.ac.uk/cell_lines). In addition, several new SNVs were found: TP53Y234H/TP53R213Q in JOK-1 and ARID1BP1435L in JVM-3. (Figure 1, Supplementary Table 4).
Patient characteristics of our cohort are summarized in Table 1 and in Supplementary Table 1. In total, 24 patients were analyzed (20 HCL-c and four HCL-v), and all patients provided samples at the time of diagnosis. For 5 patients, samples taken at the time of diagnosis and relapse/follow-up were investigated. In HCL-c patients, 88.2% (15/17) were treated with the first-line drug cladribine (n = 12), interferon a (n = 2) or pentostatine (n = 1). Forty percent (6/15) of those patients progressed with a median of 25 months [0–166.5]. Of the two untreated patients, one had no treatment criteria (UPN-19, 38.5 months of follow up), and the other (UPN-17) died on the day of the diagnosis.
Table 1. Patient characteristics of the cohort.
| n = patients | HCL-c (n = 20) | HCL-v (n = 4) | TOTAL (n = 24) |
|---|---|---|---|
| Diagnosis samples | 20 | 4 | 24 |
| Relapse/Evolution samples | 2 | 3 | 5 |
| Diagnosis age (years) (Median [min-max]) | 54.5 [42–92] | 69.5 [64–82] | 60.5 [42–92] |
| Sex Ratio Male/Female | 15/5 | 4/0 | 19/5 |
| Folow up (month) (Median [min-max]) | 37.1 [0.0–218.5] | 19.9 [8.9–31.4] | 32.3 [0.0–218.5] |
| Neutropenia (%, n) | 82.3% (14/17) | 0% (0/4) | 66.7% (14/21) |
| Monocytopenia (%, n) | 87.5% (14/16) | 0% (0/4) | 70% (14/20) |
| Anemia (%, n) | 47% (8/17) | 75% (3/4) | 52.4% (11/21) |
| Treatment (%, n) | 88.2% (15/17) | 50% (2/4) | 82.8% (18/22) |
| TFS (month) (Median [min-max]) | 1.4 [0.0–30.0] | 6.05 [2.0–19.87] | 1.7 [0.0–30.0] |
| Relapses (%, n) | 40.0% (6/15) | 50% (2/4) | 44.4% (8/18) |
| PFS (month) (Median [min-max]) | 25.0 [0.0–166.5] | 15.1 [4.1–26.0] | 25.0 [0.0–166.5] |
Definitions: Neutropenia: absolute polynuclear cells count (PNN) <1.5 × 109/L; Monocytopenia: absolute monocytes count <0.20 × 109/L; Anemia: hemoglobinemia rate <120 g/L (female) <130 g/L (male).
Abbreviations: PFS: Progression Free Survival, TFS: Treatment Free Suvival.
Of the HCL-v patients, two (UPN-v1 and UPN-v2) were treated with Rituximab plus cladribine or cladribine alone; they progressed rapidly at 4.1 and 26 months respectively. The remaining HLC-v patients (UPN-v3 and UPN-v4) were untreated because of palliative care and the absence of treatment criteria, respectively (follow up of 8.5 months).
HCL-c patients at diagnosis have recurrent gene mutations
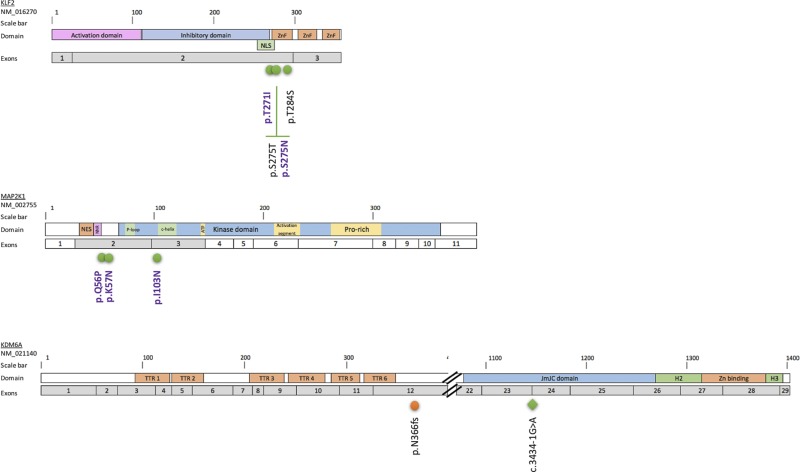
The BRAFV600E mutation was found in 90% (18/20) of HCL-c patients. For the two patients without the BRAFV600E mutation, one (UPN-40) had a mutation in MAP2K1, and the other (UPN-10) had no alternative mutations in any of the targeted genes. The frequency of the BRAFV600E allele was compatible with heterozygosity, with a median rVAF of 0.48 ± 0.12 (Figure 1 and Supplementary Table 5). In addition to BRAFV600E, mutations in KLF2 (n = 3), CDKN1B (n = 2), NOTCH1 (n = 1), ARID1B (n = 1) and CREBBP (n = 1) were found in 33% (6/18) of cases. KLF2 missense mutations found in three patients were localized in two specific domains, the zinc finger domain and the nuclear localization signal (Figure 2). CDKN1B mutations were found in two patients; these mutations were stop-gain and stop-loss mutations. One mutation had a rVAF compatible with heterozygosity (UPN-2; rVAF = 0.58), and the other was consistent with a sub-clonal mutation (UPN-25; rVAF = 0.09) (Supplementary Table 5).
Figure 2. Localization of the KLF2, MAP2K1 and KDM6A mutations in the corresponding proteins.
Distribution of mutations along the KLF2, MAP2K1 and KDM6A proteins. The exons targeted by the Trichopanel are represented in gray. Mutations are indicated as follows: green circles, missense mutations; blue circles, non-sense mutations; orange circles, deletions; green diamond, splicing variant. The SNVs previously described in HCL [8] or SMZL [25, 26] are in violet. Abbreviations: Helical domain (H), Jumonji domain (JmJC), nuclear export signal (NES), nuclear localization signal (NLS), negative regulatory region (NNR), Prolin-rich domain (Pro-rich), tetratricopeptids repeats (TTR), Zinc binding domain(Zn), Zinc fingers domain (ZnF).
Epigenetic mutations are recurrent in HCL-v patients
The MAP2K1I103N and MAP2K1Q56P mutations were found in two of four HCL-v patients (UPN-v1 and UPN-v3, respectively). All HCL-v patients had SNVs in epigenetic regulatory genes including KDM6A (n = 2), CREBBP (n = 1) and ARID1A (n = 1) (Figure 1 and Supplementary Table 5). The two KDM6A mutations were potentially deleterious (UPN-v1 and UPN-v2). One was a frameshift deletion, and the other was a splicing variant leading to a loss of exon 24 as confirmed by RNA sequencing (Figure 2 and Supplementary Figure 1B). The calculated rVAF were 1.01 and 0.99, respectively, in these two male patients, in agreement with the location of KDM6A in the X chromosome.
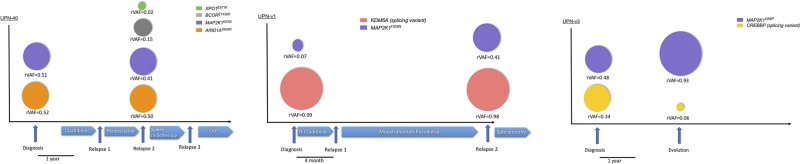
Sub-clonal mutations and variant allele frequency changes are found at the disease relapse
We analyzed serial samples from five patients (two HCL-c and three HCL-v) at diagnosis and relapse (Figure 3). For one HCL-c patient (UPN-6), we observed the same mutational pattern in the two samples. In the second case (UPN-40), two new sub-clonal mutations (BCORE1430X and XPO1E571K) were characterized. In the three HCL-v patients (two treated and one untreated), no new mutations were observed but variations of the rVAF were identified in two cases. UPN-v1 had an increased allele frequency of MAP2K1I103N (rVAF = 0.07 at diagnosis and 0.41 at relapse). UPN-v3 had a decreased allele frequency of the CREBBP splicing variant (rVAF = 0.34 to 0.06). This patient was left untreated between the first and the second samples.
Figure 3. The mutations described at diagnosis are either maintained or evolving at relapse.
Representation of the relevant HCL-c (UPN-40) and HCL-v patients (UPNv1 and UPN-v3) tested at diagnosis and at relapse. For each patient, color-coded circles estimate the rVAF of the indicated mutations. Relevant times points and treatment are indicated by arrows. Abbreviations: CEP Cisplatin-Endoxan-Epirubicin, R-Cladribine: Rituximab + cladribine.
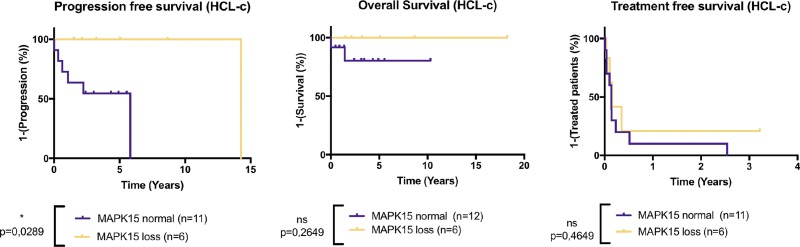
MAPK15 gene loss is the most frequent abnormality of CNVs
CNV analysis highlighted various abnormalities: the most frequent CNV was a loss of one copy of MAPK15 found in 37.5% of patients (9/24) (Figure 1). According to the MAPK15 CNV status, there were no significant differences for TFS and OS in HCL-c patients, but PFS was significantly better in HCL-c patients with a MAPK15 deletion (Figure 4). Four patients had a loss of EZH2 gene copy (UPN-18, UPN-40, UPN-v1 and UPN-v2). On the basis of their karyotypes, two of them had an abnormal chromosome 7q (one deletion and one rearrangement) involving the loss of BRAF (7q34) (Supplementary Table 1).
Figure 4. MAPK15 deletion improves the progression-free survival in HCL-c patients.
Kaplan-Meier representation of Treatment-free survival (TFS), Progression-free survival (PFS) and Overall survival (OS) of HCL-c according to MAPK15 copy loss status. p-values were calculated with Log-rank Test. In the “MAPK15 normal” group, patients were given first-line treatment with Interferon n = 1, pentostatine n = 2 or cladribine n = 5. In the “MAPK15 loss” group, patients were given first-line treatment with Interferon n = 1 or cladribine n = 6. MAPK15 loss is associated with significantly improved PFS in HLC-c patients, and no significant differences were observed in TFS and OS.
DISCUSSION
HCL cell lines are atypical. As expected, none had the BRAFV600E mutation [23], suggesting that a hairy cell phenotype-like can be observed without this driver mutation. In contrast, other mutations were found in TP53, NOTCH1, ARID1B and BRAF with an allele frequency compatible with their complex karyotype (Supplementary Table 4). JVM-3 is a B prolymphocytic leukemia-derived cell line and harbors BRAFK601N [22]. This mutation is found in rare cases of melanoma and leads to MAPK pathway activation [24]. Altogether, the cell line data show that JVM-3 could be a model for studying HCL.
Consistent with the literature, BRAFV600E mutations were found in 90% (18/20) of HCL-c patients [4, 10]. The proportion of HCL-c patients with BRAFWT differs according to the studies, ranging from 0 to 20% [4, 10]. Some alternative BRAFV600E mutations were found in exon 11 [9]. In this study, the two HCL-c patients with BRAFWT had no alternative BRAF mutations in exons 11 or 15. For these patients, the diagnosis of the classical form was confirmed by immunophenotyping, the HCL score (4/4), and the hairy cell morphology without prominent nucleoli. These criteria indicate that BRAFV600E is not the unique driver mutation in all HCL-c cases. IGHV-4-34 gene rearrangements are associated with BRAFWT in HCL-c patients [10]. In this study, IGHV status was not examined.
One third of the HCL-c patients had mutations in addition to BRAF mutations (one to two additional altered genes per patient). In all patients with these additional mutations (6/6), rVAFs were close to 0.50 (0.47 ± 0.16), confirming the early-onset of the mutation and the hypothesis in which mutations in addition to BRAF are necessary to the disease [5]. Two HCL-c patients with BRAFV600E (UPN-25 and UPN-38) had additional sub-clonal mutations in CDKN1BW76X (rVAF = 0.09) and KLF2T284S (rVAF = 0.16), respectively. The characterization of these sub-clonal mutations could be necessary for the management of future treatment and to avoid the promotion of a sub-clone during the relapse.
The Trichopanel detected KLF2 mutations in 15% (3/20) of HCL-c patients. This percentage is comparable with those reported in the literature, reported in 10–16% of cases [25, 26]. KLF2, involved in three patients, plays a key role in B-cell homing to lymph nodes and inhibition of the NF-κB pathway26,27. KLF2275N, KLF2275T and KFL2T271I mutations found in those patients are localized within the zinc finger domain or the nuclear localization signal (NLS). These mutations have been described in splenic zone marginal lymphoma (SMZL) as possibly deleterious mutations [25, 26]. Moreover, mutations involving the NLS lead to cytoplasmic relocalization of KFL2 and affect transcription factor activity [26]. In a murine model, KLF2 gene knock-out is not sufficient to induce lymphoma but results in deregulation of B-cell differentiation and trafficking [27, 28]. Thus, mutations in KLF2 in HCL-c patients could explain both the extra-nodal localization of hairy cells and NF-κB pathway upregulation [29]. One patient (UPN-38) had two mutations in KLF2: KFL2T271I (rVAF = 0.42) and KLF2T284S (rVAF = 0.16). Multiple KLF2 mutations (2–5) have been described previously in eleven patients with HLC-c (n = 1), extra-nodal marginal zone lymphoma (=1), Burkitt lymphoma (n = 1), SMZL (n = 1) and diffuse large B cell lymphoma (n = 7), and in most cases, the KLF2 mutations were located on separated alleles [26]. The effects of KLF2 mutations on HCL are still unclear and further studies are necessary.
Alterations of cell cycle and apoptosis are common in hematologic neoplasms. In this study, two HCL-c patients had CDKN1B mutations (2/20, 10%), and none had TP53 mutations. These data are consistent with previously published data in which CDKN1B mutations are found in 11–16% of HCL-c patients [7, 30]. In HCL-c patients, the frequency of TP53 mutations differs considerably from one study to another, ranging from 0–2% [30, 31] to 27% [32]. In our study, patients with CDKN1BW76X and CDKN1BX199S mutations had an atypical HCL immunophenotype with the expression of CD10. CD10 expression in HCL is rare (10–20% of cases) [33]. Currently, no studies have reported a correlation between CDKN1B mutation and CD10 expression.
In three of the six patients with BRAFWT (2 HCL-c and 4 HCL-v), we found mutations in MAP2K1. This finding is consistent with previously published data in which 48% of HCL (classical and variant form) patients with BRAFWT had MAP2K1 mutations [6]. More precisely, MAP2K1 activating mutations are found in 86% (6/7) of BRAFWT-containing HCL-c patients and 42% (10/24) of HCL-v patients [6]. BRAF and MAP2K1 mutations are mutually exclusive in HCL [6]. The mutations MAP2K1Q56P and MAP2K1K57N (UPN-v3 and UPN-40, respectively) that we found are close to the negative regulatory domain of the protein and lead to ERK phosphorylation [34, 35]. Interestingly, although the presence of MAP2K1K57N would improve of the sensitivity of cells to MEK inhibitors, MAP2K1Q56P could generate resistance [35, 36]. MAP2K1I103N (in UPN-v1) is localized close to the C-terminal helix of the protein [34]. Currently, this mutation is not described as an MEK activator but could confer resistance to MEK inhibitors by impairing the allosteric binding of the drug [35]. In the UPN-v1 patient, the MAP2K1I103N mutation was sub-clonal at the initial diagnosis (rVAF = 0.07) and considerably increased at the time of relapse (rVAF = 0.41). Altogether, these data showed that MAP2K1I103N would not confer a proliferative or survival advantage at time of diagnosis but could induce a bad-responder phenotype, even in the absence of MEK inhibitor. Indeed, UPN-v1 was treated with cladribine-rituximab and then moxetumomab-pasudotox as a second line of treatment. The detection of these mutations seems essential in the future clinical management of HCL patients.
No TP53 mutations were found in HCL-v patients, even at relapse. TP53 mutations have been described in nearly 30% of HCL-v cases [13, 31].
Finally, we described new KDM6A mutations in HCL-v patients. Both patients were hemizygous for the mutations as KDM6A is located on chromosome X. The presence of tumor suppressor genes on the chromosome X has been used to explain the imbalanced male/female sex ratio in cancers [37]. Moreover, HCL is known to have a 5:1 male/female sex ratio [3]. KDM6A (also known as Ubiquitously Transcribed Tetratricopeptide Repeat Protein X-Linked (UTX)) encodes a lysine demethylase protein that removes di- and tri-methyl groups from lysine 27 of Histone 3 (H3K27). Disruptive KDM6A mutations have been found in multiple myeloma, bladder neoplasms and T cell acute lymphoblastic leukemia (T-ALL) [38]. KDM6A mutations leading to a loss of function were previously described in 3 HCL-c patients [6, 7, 39]. Two were atypical patients, and one had a stop-gain mutation in KDM6A found in the relapse sample, possibly due to vemurafenib treatment [7]. Another patient had the BRAFWT allele with an unmutated immunoglobulin heavy gene VH4-34 [6]. This sub-type of HCL is considered to be bad responder to classical drug therapies [31]. A disruptive KDM6A mutation was also recently found in one SDRPL patient and in one HCL-v patient [30, 39]. In our series, one patient with a KDM6A mutation was non-responsive to first and second line therapies.
Those mutations and the two mutations found in our series result in the loss of the highly conserved C-terminal region of KDM6A (including Jumomji and zinc binding domains) which is essential for its demethylase activity [40]. Loss of KDM6A activity may sensitize tumor cells to demethylating agents such as EZH2 inhibitors [41]. Indeed, KDM6A inactivation (KDM6AR1279X) in T-ALL cell lines showed an improvement in the sensitivity to DZNEP, an epigenetic compound that targets methylation of H3K27 [42].
As already described in chronic lymphocytic leukemia [43], the analysis of diagnosis/relapse samples highlighted the heterogeneity of tumor cells and their sub-clonal evolution during the course of the disease. BCOR was recently described as a new recurrent gene altered in SDRPL. Mutations were found in 6/42 SRDPL and loss of BCOR expression in 4 other cases [39]. In our series, a BCOR mutation (BCORE1430X) was found at the relapse of patient UPN-40 as a sub-clonal stop-gain mutation (rVAF = 0.15).
XPO1 encodes for exportin 1, a protein that plays a key role in the nuclear export of tumor suppressors such as p53, p27 and Iκ-B, an inhibitor of the NF-κB pathway [44]. A hotspot XPO1E571K mutation has been found in primary mediastinal B-cell lymphoma, classical Hodgkin lymphoma (HL-c) and chronic lymphocytic leukemia (CLL) [45–47]. One patient (UPN-40) presented the XPO1E571K hotspot mutation at relapse. The significance of the presence of a sub-clonal XPO1E571K mutation at relapse is unknown.
The MAPK15 gene encodes extracellular regulated kinase 8 (ERK8), a recently identified member of the MAPK family. This gene is located in chromosome 8. Its activity is still unclear, but it appears to play an oncogenic role. ERK8 stabilizes c-JUN and regulates autophagy and cell transformation [48, 49]. Overexpression of MAPK15 was described in solid neoplasms [49, 50]. Thanks to this effect on MAPK pathway, MAPK15 loss could potentially antagonize the constitutive activation of MAPK pathway in BRAFV600E hairy cells. Further investigations of the link between BRAFV600E and MAPK15 are necessary. Here, we found that loss of MAPK15 copy number improved PFS in HCL-c patients without repercussion on OS (Figure 4).
MATERIALS AND METHODS
Patients and patient samples
We studied three cell lines (BONNA-12, JOK-1, JVM3 (obtained from German Collection of Microorganisms and Cell Culture or offered by Toulouse University Hospital) 20 HCL-c and 4 HCL-v patients from an initial diagnosis and 2 HCL-c and 3 HCL-v patients with relapsing disease. Mononuclear cells were obtained from peripheral blood (17 samples), bone marrow aspirates (10 samples) or 2 biopsy specimens (spleen and nodule). The HCL-c disease was diagnosed in accordance with the WHO 2016 classification [3] by combination of clinical criteria, cytology, presence of BRAFV600E and immunophenotyping. The HCL-v disease was diagnosed by clinical criteria, hairy cell morphology with constant prominent nucleoli, the absence of BRAFV600E, and immunophenotyping (Supplementary Table 1). Informed consent was obtained from patients, and the procedures were conducted in accordance with the Helsinki Declaration and the policy of the CHU de Caen.
Next generation sequencing
The PBMC fraction was collected after gradient density separation (histopaque®). DNA was extracted with the automated device MagnaPur® (Roche Lifescience) according to the manufacturer's recommendations. Library design was performed with the Ion Ampliseq Designer™ software. The DNA library (Ion Ampliseq™ Library kit), template preparation/chip loading (Ion Chef™ system + Ion PGM™ Hi-Q Chef Kit Reagent) and sequencing (Ion Torrent PGM™) were performed according to the manufacturer's recommendations (ThermoFisher Scientific). The Trichopanel design covers 71,020 bases using 712 amplicons (Supplementary Table 2). The analyzed genes belong to nine functional groups: MAPK signaling pathway (BRAF, MAP2K1, DUSP2, MAPK15), epigenetic regulation (ARID1A, ARID1B, EZH2, KDM6A, CREBBP), cell cycle/apoptosis (TP53, CDKN1B, XPO1), homing (KLF2, CXCR4), NOTCH pathway (NOTCH1, NOTCH2), NF-κB pathway (MYD88), inflammation (ANXA1), splicing (U2AF1), differentiation (BCOR) and extracellular transport (ABCA8), according to published WES data [4, 6–8]. Data analysis was performed with Torrent suiteTM software, and then, variant analysis was performed using an in-house generated bioinformatic pipeline (Generate reports®) as previously described [20]. The ratio of variant allele frequency (VAF), rVAF, was calculated as the percentage of VAF on divided by the percentage of tumor infiltration. Splicing prediction was performed using an in-house generated bioinformatic pipeline (Alamut® Visual 2.9 interactive Biosoftware) as previously described [51] (Supplementary Figure 1A). Functional relevance was analyzed in silico using three validated algorithms (SIFT®, CADD® and polyphen2®).
Copy number variation (CNV) analysis of the regions sequenced by the Trichopanel was performed as previously described [52], and patients' data were normalized to DNA samples from eight healthy patients.
Sanger sequencing
Primer sequences for PCR amplification were designed with the Primer3 software (v4.0.0, http://primer3.ut.ee) (Supplementary Table 3). Sequencing was performed on an ABI Prism31000 device (ThermoFisher Scientific) according to the manufacturer's recommendations.
Immunophenotyping
Multiparameter flow cytometric immunophenotyping was performed on a FACS CANTO II or a FACSCalibur (Becton Dickinson, (BD)), and the data were used to characterize hairy cells (HC) and to quantify tumor infiltration (See Supplementary Methods).
Statistical analysis
Statistical representations of the Kaplan–Meir test on Treatment Free Survival (TFS), Progression Free Survival (PFS) and Overall Survival (OS) were performed using GraphPad Prism version 7.00, and p-values were calculated with Log-rank Test. TFS was calculated from the date of diagnosis to date of first treatment or last patient follow-up. OS was calculated from the date of diagnosis to date of death or last patient follow-up. PFS was calculated from the date of diagnosis until disease progression, relapse, death or last patient follow-up. p values < 0.05 were considered statistically significant.
CONCLUSIONS
The use of the Trichopanel has a potential benefit in the diagnosis and the prognosis of HCL-c and HCL-v patients, who need to be confirmed in a larger cohort. This is a relatively easy tool for routine analysis. The KDM6A loss of function mutation described in this study needs to be further investigated in order to determine the role of demethylating agents in those patients.
SUPPLEMENTARY MATERIALS FIGURES AND TABLES
Acknowledgments
The authors thank members of A. Martins's team (INSERM U1245, Université de Rouen, France) for the analysis of splicing prediction with the Alamut® software. The authors thank M. Decamp (CHU de Caen, France) for cell lines and patient karyotypes.
Abbreviations
- CNV
copy number variation
- HCL-c
classical hairy cell leukemia
- HCL-v
hairy cell leukemia-variant
- SDRPL
splenic diffuse red pulp lymphoma
- SMZL
splenic marginal zone lymphoma
- SNV
single nucleotide variation
Footnotes
Author contributions
BS, FJ and XT conceived and planned the study; EM and CM performed the experiments; EM, PB, P-JV, BS, FJ and XT interpreted the data; GD reviewed clinical data; VS, EC and DN performed and reviewed the biological HCL diagnosis (cytology, immunophenotyping and molecular analysis); EM wrote the manuscript with the support of PB, P-JV, GD, BS, FJ and XT.
CONFLICTS OF INTEREST
All of the authors declare no conflicts of interest
FUNDING
This work was supported by the A.R.E.H.B. association, CHU Caen, France.
REFERENCES
- 1.Teras LR, DeSantis CE, Cerhan JR, Morton LM, Jemal A, Flowers CR. US Lymphoid Malignancy Statistics by World Health Organization Subtypes. CA Cancer J Clin. 2016;2016;66:443–59. doi: 10.3322/caac.21357. [DOI] [PubMed] [Google Scholar]
- 2.Swerdlow SH, Campo E, Lee Harris N, Jaffe ES, Pileri SA, Stein H, Thiele J, Vardiman JW. WHO Classification of tumours of Haematopoietic and Lymphoid Tissues. Lyon, France: IARC Press; 2008. [Google Scholar]
- 3.Swerdlow SH, Campo E, Pileri SA, Harris NL, Stein H, Siebert R, Advani R, Ghielmini M, Salles GA, Zelenetz AD, Jaffe ES. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 2016;127:2375–90. doi: 10.1182/blood-2016-01-643569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tiacci E, Trifonov V, Schiavoni G, Holmes A, Kern W, Martelli MP, Pucciarini A, Bigerna B, Pacini R, Wells VA, Sportoletti P, Pettirossi V, Mannucci R, et al. BRAF mutations in hairy-cell leukemia. N Engl J Med. 2011;364:2305–2315. doi: 10.1056/NEJMoa1014209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chung SS, Kim E, Park JH, Chung YR, Lito P, Teruya-Feldstein J, Hu W, Beguelin W, Monette S, Duy C, Rampal R, Telis L, Patel M, et al. Hematopoietic stem cell origin of BRAFV600E mutations in hairy cell leukemia. Sci Transl Med. 2014;6:238ra71–238ra71. doi: 10.1126/scitranslmed.3008004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Waterfall JJ, Arons E, Walker RL, Pineda M, Roth L, Killian JK, Abaan OD, Davis SR, Kreitman RJ, Meltzer PS. High prevalence of MAP2K1 mutations in variant and IGHV4-34–expressing hairy-cell leukemias. Nat Genet. 2013;46:8–10. doi: 10.1038/ng.2828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dietrich S, Hüllein J, Lee SC, Hutter B, Gonzalez D, Jayne S, Dyer MJ, Oleś M, Else M, Liu X, Słabicki M, Wu B, Troussard X, et al. Recurrent CDKN1B (p27) mutations in hairy cell leukemia. Blood. 2015;126:1005–1008. doi: 10.1182/blood-2015-04-643361. [DOI] [PubMed] [Google Scholar]
- 8.Weston-Bell NJ, Tapper W, Gibson J, Bryant D, Moreno Y, John M, Ennis S, Kluin-Nelemans HC, Collins AR, Sahota SS. Exome Sequencing in Classic Hairy Cell Leukaemia Reveals Widespread Variation in Acquired Somatic Mutations between Individual Tumours Apart from the Signature BRAF V(600)E Lesion. Richards KL, editor. PLoS One. 2016;11:e0149162. doi: 10.1371/journal.pone.0149162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tschernitz S, Flossbach L, Bonengel M, Roth S, Rosenwald A, Geissinger E. Alternative BRAF mutations in BRAF V600E-negative hairy cell leukaemias. Br J Haematol. 2014;165:529–33. doi: 10.1111/bjh.12735. [DOI] [PubMed] [Google Scholar]
- 10.Xi L, Arons E, Navarro W, Calvo KR, Stetler-Stevenson M, Raffeld M, Kreitman RJ. Both variant and IGHV4-34–expressing hairy cell leukemia lack the BRAF V600E mutation. Blood. 2012;119:3330–3332. doi: 10.1182/blood-2011-09-379339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Arons E, Kreitman RJ. Molecular variant of hairy cell leukemia with poor prognosis. Leuk Lymphoma. 2011;52:99–102. doi: 10.3109/10428194.2011.565841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Matutes E, Martínez-Trillos A, Campo E. Hairy cell leukaemia-variant: Disease features and treatment. Best Pract Res Clin Haematol. 2015;28:253–63. doi: 10.1016/j.beha.2015.09.002. [DOI] [PubMed] [Google Scholar]
- 13.Hockley SL, Else M, Morilla A, Wotherspoon A, Dearden C, Catovsky D, Gonzalez D, Matutes E. The prognostic impact of clinical and molecular features in hairy cell leukaemia variant and splenic marginal zone lymphoma. Br J Haematol. 2012;158:347–54. doi: 10.1111/j.1365-2141.2012.09163.x. [DOI] [PubMed] [Google Scholar]
- 14.Robak T, Matutes E, Catovsky D, Zinzani PL, Buske C. Hairy cell leukaemia: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2015;26:v100–7. doi: 10.1093/annonc/mdv200. [DOI] [PubMed] [Google Scholar]
- 15.Grever MR, Abdel-Wahab O, Andritsos LA, Banerji V, Barrientos J, Blachly JS, Call TG, Catovsky D, Dearden C, Demeter J, Else M, Forconi F, Gozzetti A, et al. Consensus guidelines for the diagnosis and management of patients with classic hairy cell leukemia. Blood. 2017;129:553–560. doi: 10.1182/blood-2016-01-689422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Matutes E, Morilla R, Owusu-Ankomah K, Houliham H, Meeus P, Catovsky D. The immunophenotype of hairy cell leukemia (HCL). Proposal for a scoring system to distinguish HCL from B-cell disorders with hairy or villous lymphocytes. Leuk Lymphoma. 1994;14:57–61. [PubMed] [Google Scholar]
- 17.Baseggio L, Traverse-Glehen A, Callet-Bauchu E, Morel D, Magaud JP, Berger F, Salles G, Felman P. Relevance of a scoring system including CD11c expression in the identification of splenic diffuse red pulp small B-cell lymphoma (SRPL) Hematol Oncol. 2011;29:47–51. doi: 10.1002/hon.957. [DOI] [PubMed] [Google Scholar]
- 18.Traverse-Glehen A, Baseggio L, Callet-Bauchu E, Morel D, Gazzo S, Ffrench M, Verney A, Rolland D, Thieblemont C, Magaud JP, Salles G, Coiffier B, Berger F, et al. Splenic red pulp lymphoma with numerous basophilic villous lymphocytes: a distinct clinicopathologic and molecular entity? Blood. 2008;111:2253–2260. doi: 10.1182/blood-2007-07-098848. [DOI] [PubMed] [Google Scholar]
- 19.Traverse-Glehen A, Verney A, Gazzo S, Jallades L, Chabane K, Hayette S, Coiffier B, Callet-Bauchu E, Ffrench M, Felman P, Berger F, Baseggio L, Salles G. Splenic diffuse red pulp lymphoma has a distinct pattern of somatic mutations amongst B-cell malignancies. Leuk Lymphoma. 2016;58:1–10. doi: 10.1080/10428194.2016.1196813. [DOI] [PubMed] [Google Scholar]
- 20.Dubois S, Viailly PJ, Mareschal S, Bohers E, Bertrand P, Ruminy P, Maingonnat C, Jais JP, Peyrouze P, Figeac M, Molina TJ, Desmots F, Fest T, et al. Next Generation Sequencing in Diffuse Large B Cell Lymphoma Highlights Molecular Divergence and Therapeutic Opportunities: a LYSA Study. Clin Cancer Res. 2016;22:2919–2928. doi: 10.1158/1078-0432.CCR-15-2305. [DOI] [PubMed] [Google Scholar]
- 21.Nayak L, Goduni L, Takami Y, Sharma N, Kapil P, Jain MK, Mahabeleshwar GH. Kruppel-Like Factor 2 Is a Transcriptional Regulator of Chronic and Acute Inflammation. Am J Pathol. 2013;182:1669–704. doi: 10.1016/j.ajpath.2013.01.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jebaraj BM, Kienle D, Bühler A, Winkler D, Döhner H, Stilgenbauer S, Zenz T. BRAF mutations in chronic lymphocytic leukemia. Leuk Lymphoma. 2013;54:1177–82. doi: 10.3109/10428194.2012.742525. [DOI] [PubMed] [Google Scholar]
- 23.Tiacci E, Pucciarini A, Bigerna B, Pettirossi V, Strozzini F, Martelli MP, Tabarrini A, Drexler HG, Falini B. Absence of BRAF-V600E in the human cell lines BONNA-12, ESKOL, HAIR-M, and HC-1 questions their origin from hairy cell leukemia. Blood. 2012;119:5332–5333. doi: 10.1182/blood-2011-12-400374. [DOI] [PubMed] [Google Scholar]
- 24.Yao Z, Torres NM, Tao A, Gao Y, Luo L, Li Q, de Stanchina E, Abdel-Wahab O, Solit DB, Poulikakos PI, Rosen N. BRAF Mutants Evade ERK-Dependent Feedback by Different Mechanisms that Determine Their Sensitivity to Pharmacologic Inhibition. Cancer Cell. 2015;28:370–83. doi: 10.1016/j.ccell.2015.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Clipson A, Wang M, de Leval L, Ashton-Key M, Wotherspoon A, Vassiliou G, Bolli N, Grove C, Moody S, Escudero-Ibarz L, Gundem G, Brugger K, Xue X, et al. KLF2 mutation is the most frequent somatic change in splenic marginal zone lymphoma and identifies a subset with distinct genotype. Leukemia. 2015;29:1177–85. doi: 10.1038/leu.2014.330. [DOI] [PubMed] [Google Scholar]
- 26.Piva R, Deaglio S, Famà R, Buonincontri R, Scarfò I, Bruscaggin A, Mereu E, Serra S, Spina V, Brusa D, Garaffo G, Monti S, Dal Bo M, et al. The Krüppel-like factor 2 transcription factor gene is recurrently mutated in splenic marginal zone lymphoma. Leukemia. 2015;29:503–7. doi: 10.1038/leu.2014.294. [DOI] [PubMed] [Google Scholar]
- 27.Hart GT, Wang X, Hogquist KA, Jameson SC. Kruppel-like factor 2 (KLF2) regulates B-cell reactivity, subset differentiation, and trafficking molecule expression. Proc Natl Acad Sci. 2011;108:716–21. doi: 10.1073/pnas.1013168108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Winkelmann R, Sandrock L, Porstner M, Roth E, Mathews M, Hobeika E, Reth M, Kahn ML, Schuh W, Jack HM. B cell homeostasis and plasma cell homing controlled by Kruppel-like factor 2. Proc Natl Acad Sci. 2011;108:710–5. doi: 10.1073/pnas.1012858108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nagel S, Ehrentraut S, Meyer C, Kaufmann M, Drexler HG, MacLeod RA. NFkB is activated by multiple mechanisms in hairy cell leukemia: NFkB IS Activated by Multiple Mechanisms. Genes Chromosomes Cancer. 2015;54:418–32. doi: 10.1002/gcc.22253. [DOI] [PubMed] [Google Scholar]
- 30.Durham BH, Getta B, Dietrich S, Taylor J, Won H, Bogenberger JM, Scott S, Kim E, Chung YR, Chung SS, Hüllein J, Walther T, Wang L, et al. Genomic analysis of hairy cell leukemia identifies novel recurrent genetic alterations. Blood. 2017;130:1644–8. doi: 10.1182/blood-2017-01-765107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Forconi F, Sozzi E, Cencini E, Zaja F, Intermesoli T, Stelitano C, Rigacci L, Gherlinzoni F, Cantaffa R, Baraldi A, Gallamini A, Zaccaria A, Pulsoni A, et al. Hairy cell leukemias with unmutated IGHV genes define the minor subset refractory to single-agent cladribine and with more aggressive behavior. Blood. 2009;114:4696–702. doi: 10.1182/blood-2009-03-212449. [DOI] [PubMed] [Google Scholar]
- 32.König EA, Kusser WC, Day C, Porzsolt F, Glickman BW, Messer G, Schmid M, De Chatel R, Marcsek ZL, Demeter J. p53 mutations in hairy cell leukemia. Leukemia. 2000;14:706–11. doi: 10.1038/sj.leu.2401721. [DOI] [PubMed] [Google Scholar]
- 33.Jasionowski TM, Hartung L, Greenwood JH, Perkins SL, Bahler DW. Analysis of CD10+ Hairy Cell Leukemia. Am J Clin Pathol. 2003;120:228–35. doi: 10.1309/QVJD31TEG9UJ18BQ. [DOI] [PubMed] [Google Scholar]
- 34.Bromberg-White JL, Andersen NJ, Duesbery NS. MEK genomics in development and disease. Brief Funct Genomics. 2012;11:300–10. doi: 10.1093/bfgp/els022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Emery CM, Vijayendrana KG, Zipserc MC, Sawyera AM, Niua L, Kima JJ, Hattona C, Choprad R, Oberholzera PA, Karpovac MB, MacConailla LE, Zhang J, Gray NS, et al. MEK1 mutations confer resistance to MEK and B-RAF inhibition. PNAS. 2009;106:20411–6. doi: 10.1073/pnas.0905833106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Marks JL, Gong Y, Chitale D, Golas B, McLellan MD, Kasai Y, Ding L, Mardis ER, Wilson RK, Solit D, Levine R, Michel K, Thomas RK, et al. Novel MEK1 Mutation Identified by Mutational Analysis of Epidermal Growth Factor Receptor Signaling Pathway Genes in Lung Adenocarcinoma. Cancer Res. 2008;68:5524–8. doi: 10.1158/0008-5472.CAN-08-0099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dunford A, Weinstock DM, Savova V, Schumacher SE, Cleary JP, Yoda A, Sullivan TJ, Hess JM, Gimelbrant AA, Beroukhim R, Lawrence MS, Getz G, Lane AA. Tumor-suppressor genes that escape from X-inactivation contribute to cancer sex bias. Nat Genet. 2016;49:10–6. doi: 10.1038/ng.3726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.van Haaften G, Dalgliesh GL, Davies H, Chen L, Bignell G, Greenman C, Edkins S, Hardy C, O'Meara S, Teague J, Butler A, Hinton J, Latimer C, et al. Somatic mutations of the histone H3K27 demethylase gene UTX in human cancer. Nat Genet. 2009;41:521–3. doi: 10.1038/ng.349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jallades L, Baseggio L, Sujobert P, Huet S, Chabane K, Callet-Bauchu E, Verney A, Hayette S, Desvignes JP, Salgado D, Levy N, Béroud C, Felman P, et al. Exome sequencing identifies recurrent BCOR gene alterations and the absence of KLF2, TNFAIP3 and MYD88 mutations in splenic diffuse red pulp small B-cell lymphoma. Haematologica. 2017;14:1758–66. doi: 10.3324/haematol.2016.160192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sengoku T, Yokoyama S. Structural basis for histone H3 Lys 27 demethylation by UTX/KDM6A. Genes Dev. 2011;25:2266–77. doi: 10.1101/gad.172296.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ler LD, Ghosh S, Chai X, Thike AA, Heng HL, Siew EY, Dey S, Koh LK, Lim JQ, Lim WK, Myint SS, Loh JL, Ong P, et al. Loss of tumor suppressor KDM6A amplifies PRC2-regulated transcriptional repression in bladder cancer and can be targeted through inhibition of EZH2. Sci Transl Med. 2017. p. 9. [DOI] [PubMed]
- 42.Van der Meulen J, Sanghvi V, Mavrakis K, Durinck K, Fang F, Matthijssens F, Rondou P, Rosen M, Pieters T, Vandenberghe P, Delabesse E, Lammens T, De Moerloose B, et al. The H3K27me3 demethylase UTX is a gender-specific tumor suppressor in T-cell acute lymphoblastic leukemia. Blood. 2015;125:13–21. doi: 10.1182/blood-2014-05-577270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Schuh A, Becq J, Humphray S, Alexa A, Burns A, Clifford R, Feller SM, Grocock R, Henderson S, Khrebtukova I, Kingsbury Z, Luo S, McBride D, et al. Monitoring chronic lymphocytic leukemia progression by whole genome sequencing reveals heterogeneous clonal evolution patterns. Blood. 2012;120:4191–6. doi: 10.1182/blood-2012-05-433540. [DOI] [PubMed] [Google Scholar]
- 44.Camus V, Miloudi H, Taly A, Sola B, Jardin F. XPO1 in B cell hematological malignancies: from recurrent somatic mutations to targeted therapy. J Hematol Oncol. 2017;10 doi: 10.1186/s13045-017-0412-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Camus V, Stamatoullas A, Mareschal S, Viailly PJ, Sarafan-Vasseur N, Bohers E, Dubois S, Picquenot JM, Ruminy P, Maingonnat C, Bertrand P, Cornic M, Tallon-Simon V, et al. Detection and prognostic value of recurrent exportin 1 mutations in tumor and cell-free circulating DNA of patients with classical Hodgkin lymphoma. Haematologica. 2016;101:1094–101. doi: 10.3324/haematol.2016.145102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jardin F, Pujals A, Pelletier L, Bohers E, Camus V, Mareschal S, Dubois S, Sola B, Ochmann M, Lemonnier F, Viailly PJ, Bertrand P, Maingonnat C, et al. Recurrent mutations of the exportin 1 gene (XPO1) and their impact on selective inhibitor of nuclear export compounds sensitivity in primary mediastinal B-cell lymphoma: XPO1 Mutations in Primary Mediastinal B-Cell Lymphoma. Am J Hematol. 2016;91:923–30. doi: 10.1002/ajh.24451. [DOI] [PubMed] [Google Scholar]
- 47.Jeromin S, Weissmann S, Haferlach C, Dicker F, Bayer K, Grossmann V, Alpermann T, Roller A, Kohlmann A, Haferlach T, Kern W, Schnittger S. SF3B1 mutations correlated to cytogenetics and mutations in NOTCH1, FBXW7, MYD88, XPO1 and TP53 in 1160 untreated CLL patients. Leukemia. 2014;28:108–17. doi: 10.1038/leu.2013.263. [DOI] [PubMed] [Google Scholar]
- 48.Colecchia D, Rossi M, Sasdelli F, Sanzone S, Strambi A, Chiariello M. MAPK15 mediates BCR-ABL1-induced autophagy and regulates oncogene-dependent cell proliferation and tumor formation. Autophagy. 2015;11:1790–802. doi: 10.1080/15548627.2015.1084454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jin DH, Lee J, Kim KM, Kim S, Kim DH, Park J. Overexpression of MAPK15 in gastric cancer is associated with copy number gain and contributes to the stability of c-Jun. Oncotarget. 2015;6:20190–20203. doi: 10.18632/oncotarget.4171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Iavarone C, Acunzo M, Carlomagno F, Catania A, Melillo RM, Carlomagno SM, Santoro M, Chiariello M. Activation of the Erk8 Mitogen-activated Protein (MAP) Kinase by RET/PTC3, a Constitutively Active Form of the RET Proto-oncogene. J Biol Chem. 2006;281:10567–76. doi: 10.1074/jbc.M513397200. [DOI] [PubMed] [Google Scholar]
- 51.Théry JC, Krieger S, Gaildrat P, Révillion F, Buisine MP, Killian A, Duponchel C, Rousselin A, Vaur D, Peyrat JP, Berthet P, Frebourg T, Martins A, et al. Contribution of bioinformatics predictions and functional splicing assays to the interpretation of unclassified variants of the BRCA genes. Eur J Hum Genet. 2011;19:1052. doi: 10.1038/ejhg.2011.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Boeva V, Popova T, Lienard M, Toffoli S, Kamal M, Le Tourneau C, Gentien D, Servant N, Gestraud P, Rio Frio T, Hupe P, Barillot E, Laes JF. Multi-factor data normalization enables the detection of copy number aberrations in amplicon sequencing data. Bioinformatics. 2014;30:3443–50. doi: 10.1093/bioinformatics/btu436. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.